Abstract
Regular physical activity produces resistance to the negative health consequences of stressor exposure. One way that exercise may confer stress resistance is by reducing the impact of stress on diurnal rhythms and sleep; disruptions of which contribute to stress-related disease including mood disorders. Given the link between diurnal rhythm disruptions and stress-related disorders and that exercise both promotes stress resistance and is a powerful non-photic biological entrainment cue, we tested if wheel running could reduce stress-induced disruptions of sleep/wake behavior and diurnal rhythms. Adult, male F344 rats with or without access to running wheels were instrumented for biotelemetric recording of diurnal rhythms of locomotor activity, heart rate, core body temperature (CBT), and sleep (i.e. REM, NREM, and WAKE) in the presence of a 12hr light/dark cycle. Following 6 weeks of sedentary or exercise conditions, rats were exposed to an acute stressor known to disrupt diurnal rhythms and produce behaviors associated with mood disorders. Prior to stressor exposure, exercise rats had higher CBT, more locomotor activity during the dark cycle, and greater %REM during the light cycle relative to sedentary rats. NREM and REM sleep were consolidated immediately following peak running to a greater extent in exercise, compared to sedentary rats. In response to stressor exposure, exercise rats expressed higher stress-induced hyperthermia than sedentary rats. Stressor exposure disrupted diurnal rhythms in sedentary rats; and wheel running reduced these effects. Improvements in sleep and reduced diurnal rhythm disruptions following stress could contribute to the health promoting and stress protective effects of exercise.
Keywords: Voluntary Exercise, Sleep, Activity, Diurnal, Temperature
Introduction
Disruptions in circadian/diurnal rhythms contribute to the development and symptom severity of mood disorders (Breslau et al. 2004; Emens et al. 2009; Germain et al. 2003; Hasler et al. 2010; Kyung Lee et al. 2010; Ohayon et al. 2001; Papadimitriou et al. 2005; van Liempt et al. 2012). Depressed individuals, for example, have disrupted sleep/wake behavior (Hasler et al. 2010; Kyung Lee & Douglass 2010; Ohayon & Roth 2001) and circadian temperature rhythms (Avery et al. 1982; Hasler et al. 2010; Monk et al. 1994; Posener et al. 2000; Souetre et al. 1989). Disrupted sleep is an independent risk factor for the development of depression (Kronfeld-Schor et al. 2012; Mallon et al. 2000; Riemann et al. 2001; Roberts et al. 2000) and insomniacs, compared to controls, were more likely to develop depression at one-year follow-up (Ford et al. 1989). Given that disruptions in sleep/wake behavior and circadian physiology contribute to the development of stress-related mood disorders, identifying behavioral factors that can mitigate these stress-induced disruptions in sleep/wake behavior and diurnal/circadian rhythms will aid in reducing their burden on society.
One such behavioral factor is regular physical activity, which is effective at preventing and treating stress-related mood disorders including depression (Babyak et al. 2000; Blumenthal et al. 2007; Dunn et al. 2005), anxiety (Barbour et al. 2007; Newman et al. 2007), and post-traumatic stress disorder (Manger et al. 2005; Newman & Motta 2007). Pre-clinical studies also demonstrate similar stress-protective effects of regular physical activity (Duman et al. 2008; Greenwood et al. 2011; Greenwood et al. 2003; Vollert et al. 2011). Regular physical activity is a behavioral factor that, when voluntary, will naturally align with the light/dark cycle (Verwey et al. 2013) and is an endogenous zeitgeber that can entrain sleep/wake behavior (Edgar et al. 1991). Prior data indicate that voluntary exercise can hasten the re-entrainment of the sleep/wake cycle in humans following a 4-day phase-shift (Yamanaka et al. 2010) and improve sleep in rodent models (Blanco-Centurion et al. 2006; Lancel et al. 2003). Importantly, exercise-induced increases in sleep quality are associated with a decreased suicide risk in depressed patients (Davidson et al. 2013). Taken together, these studies support the possibility that voluntary exercise may protect against stress-induced disruptions in diurnal physiological rhythms through reinforced entrainment of sleep/wake behavior and diurnal physiological rhythms.
The purpose of the current experiment was to investigate the impact of long-term voluntary exercise on diurnal rhythms of sleep/wake behavior and physiology and to examine whether this behavioral intervention could alleviate stress-induced disruptions to sleep/wake patterns and diurnal physiological rhythms. We hypothesized that prior wheel running would improve sleep and attenuate the disruptions in sleep/wake behavior and physiological rhythms following acute stressor exposure.
Methods
Animals
Adult male F344 rats (n = 16, Harlan Laboratories) weighing 200g–230g, postnatal day 50 at arrival; were housed with controlled temperature (22°C) and humidity. We selected the F344 rodent strain for several reasons: 1) F344 rats are an inbred strain known to respond to stressors in a consistent fashion and allow us to minimize group size. 2) The F344 rat is also a consistently mid-high range voluntary wheel runner (Greenwood et al. 2005b; Greenwood et al. 2003; Speaker et al. 2014). The goal of this study was to explore the potential protective effects of exercise on stress-induced disruptions in sleep and physiology, thus by using the F344 rat, we were ensured that we would maximize the impact of stressor exposure and achieve consistent wheel running distances, thus allowing us to minimize group sizes and variability of both dependent and independent measures. The animals were maintained on a 12:12 hour light/dark cycle (lights on 0400–1600 hours). All rats were housed in Nalgene Plexiglas cages (45 × 25.2 × 14.7 cm) and were allowed to acclimate to the housing conditions for one week. Rats had ad libitum access to food and water and were weighed once per week. All experimental procedures were performed during the inactive cycle and animals were handled during the 1 week acclimation period. Animal discomfort was minimized during all procedures. Experimental protocols for these studies were approved by the University of Colorado Animal Care and Use Committee.
Exercise Protocol
Rats in the running group had running wheels (1.1 m circumference; Mini Mitter, Bend, OR) mounted on the inside of their home cage. Wheels in the home cage were also locked during acclimatization and for one week (Week 4) following surgical implantation of the telemetry transmitters. All rats were allowed to exercise for 6 weeks prior to stressor exposure, not including the week recovering from surgical transmitter implant. The 6-week duration of exercise was chosen because previous studies demonstrate that 6 weeks of wheel running is necessary to prevent increased shock-elicited fear and deficits in shuttle box escape learning caused by exposure to inescapable tail shock (Greenwood et al. 2005a). Revolutions were automatically recorded by the Activity Wheel Monitor or Vital View software (Mini Mitter, Bend, OR) and distance was calculated by multiplying wheel circumference (1.081m) by the number of wheel revolutions.
Stress Protocol
Rats were exposed to 100 inescapable tail shocks as previously described (Greenwood et al. 2005a; Thompson et al. 2013). On the day of exposure to tail shock, all rats were taken to a separate room, placed in Plexiglass restraining tubes (23.4cm long and 7.0cm in diameter) and exposed to 100, 5-s, 1.5mA inescapable tail shocks. All rats were exposed to inescapable tail shocks at the same time on the day of stress exposure. Shocks were delivered at random with an average interval of 60-s between shocks and occurred during the inactive (light) cycle between 0800 and 1100 h. After exposure to inescapable tail shock all rats were immediately returned to their home cages where continuous uninterrupted biotelemetry recording continued for 6 days.
Biotelemetry Surgeries
The F40-EET biotelemetry transmitters (Data Sciences International, St. Paul Minnesota.) were implanted into animals as previously described (Greenwood et al. 2014; Thompson et al. 2014). Briefly, animals were fully anesthetized and unresponsive following ketamine (i.p. 75.0 mg/kg), and medetomidine (i.p. 0.5 mg/kg). Animals were shaved and prepped for surgery. A midline incision was made approximately 5.0 cm in length on the ventral abdominal wall. The F40-EET transmitter was placed on the intestines, the biopotential leads were passed through the ventral abdominal wall and then the F40-EET transmitter was sutured to the ventral abdominal wall. Once the transmitter was sutured into place, the ECG leads were positioned to measure cardiac electrical activity. Finally, the EEG leads were placed as previously described (Olivadoti et al. 2008). Briefly, insulated leads were passed subcutaneously to the base of the skull, where they were attached to pan head stainless steel screws (Plastics One Inc.) which served as electroencephalographic (EEG) recording electrodes. Using sterile technique, a hole was drilled to secure the screws in place at stereotaxic coordinates relative to bregma: anterior 2.0; lateral 2.5 and posterior −5.5; lateral 3.0. Once screws and leads were in place, they were embedded in dental acrylic to ensure the integrity of the recording signal. Immediately following surgery rats were given meloxicam (i.p. 1.0 mg/kg) for analgesia after which they recovered on a heating pad at 37° C until ambulatory. Once ambulatory, rats were placed in their home cages and given one 2.0 mg rimadyl tablet (Bio-Serv, product# MD150-2) and several fruity bites (Bio-Serv, product# F6038). Animals were allowed to recover for one week following surgery where running wheels were locked for the exercise group.
Data Acquisition and Analysis
The F40-EET transmitter allows in vivo real-time measurement of locomotor activity (LA), heart rate (HR), core body temperature (CBT) and electroencephalogram (EEG) in freely behaving animals. Biotelemetry recordings were acquired/analyzed using Dataquest ART 4.3 Gold Acquisition/Analysis Software (Data Sciences International, St. Paul, MN) as previously described (Greenwood et al. 2014; Thompson et al. 2013; Thompson et al. 2014; Thompson et al. 2012). Locomotor activity, heart rate and EEG were recorded at 500 Hz. Analysis of the sleep/wake cycles was performed using the automated Neuroscore 2.1.0 software (Data Sciences International, St. Paul, MN). The trace EEG signal was subjected to fast Fourier Transformation (FFT), yielding spectra between 0.5 and 30 Hz in 0.5-Hz frequency bins. The delta frequency band was defined at 0.5–4.5 Hz and the theta frequency band was defined as 6.0–9.0 Hz as previously described (Olivadoti & Opp 2008). Arousal state was scored in 10-sec epochs and classified as NREMS, REMS, or WAKE on the basis of state-dependent changes in multiple parameters, including the EEG, locomotor activity, heart rate and CBT as previously described (Olivadoti & Opp 2008). Briefly, wakefulness was defined on the basis of a low amplitude, mixed frequency (delta≈theta) EEG accompanied by body movements. Increases in CBT during wakefulness are associated with activity. NREM sleep was identified by increased absolute EEG amplitude with integrated values for the delta frequency band greater than those for the theta frequency and lack of body movements. CBT declines upon entry into NREM sleep until it reaches a regulated asymptote. REM sleep was characterized by a low amplitude EEG with integrated values for the delta frequency band less than those for the theta frequency band. Any epochs containing artifact or electrical noise were marked and excluded from subsequent spectral analysis. Time spent in NREM/REM/WAKE was calculated as a percentage (%) of time spent in a specific behavioral state per hour (i.e. % REM, % NREM, or % WAKE). Additionally, average bout durations of NREM/REM/WAKE were calculated as an average per hour. Finally, for NREM/REM/WAKE the total number of episodes per hour (#) was also calculated. All sleep/wake data were averaged into 20-min, 1-hour or 12-hour intervals for statistical analysis. The sedentary and exercise groups had 8 animals per group, however; two animals had to be eliminated from the exercise group due to animal destruction of the transmitter leads and a subsequent failure of accurate data collection from the transmitters.
Power analyses were also performed on the EEG after peak wheel running during the baseline period and for several hours following stress exposure and no significant differences were found (data not shown), which is consistent with the prior literature in young rats (Blanco-Centurion & Shiromani 2006). Briefly, Fast Fourier Transformations were performed on the trace EEG signal in order to generate two different frequency bands (delta 0.5–4.5 Hz, theta 6.0–9.0 Hz) and obtain the absolute power for signals (Campbell 2009). Average values for the absolute power were then compared via ANOVA to investigate potential differences due to exercise.
Experimental Design
Rats were allowed to acclimate to housing conditions for one week before the running wheels were unlocked (Figure 1A). On day 0, seven days after arrival to the colony, the wheels were unlocked and these rats were allowed to freely run on wheels for the remainder of the experiment (exercise group), except for one week following surgical implantation of the transmitters. The sedentary group was housed in sedentary cages with no access to running wheels. On experimental days 28 and 29, rats were implanted with biotelemetry devices and following recovery rats again either remained sedentary or were allowed access to their wheels for 2 weeks (days 35–49) during which time baseline measures (BL) were also captured in control conditions where rats were completely undisturbed in their home cages for 96 hours (days 45–48) to measure diurnal/circadian rhythms and the day/night differences (i.e. diurnal differences for BL shown in figure 7) were obtained by averaging these four days together. On day 50, all rats were exposed to acute stress (~0800–1000). After stressor exposure, rats were immediately returned to their home cages and again completely undisturbed for 6 days (experimental days 51–56) in order to record real-time recovery from the stress-induced diurnal physiological rhythm disruptions.
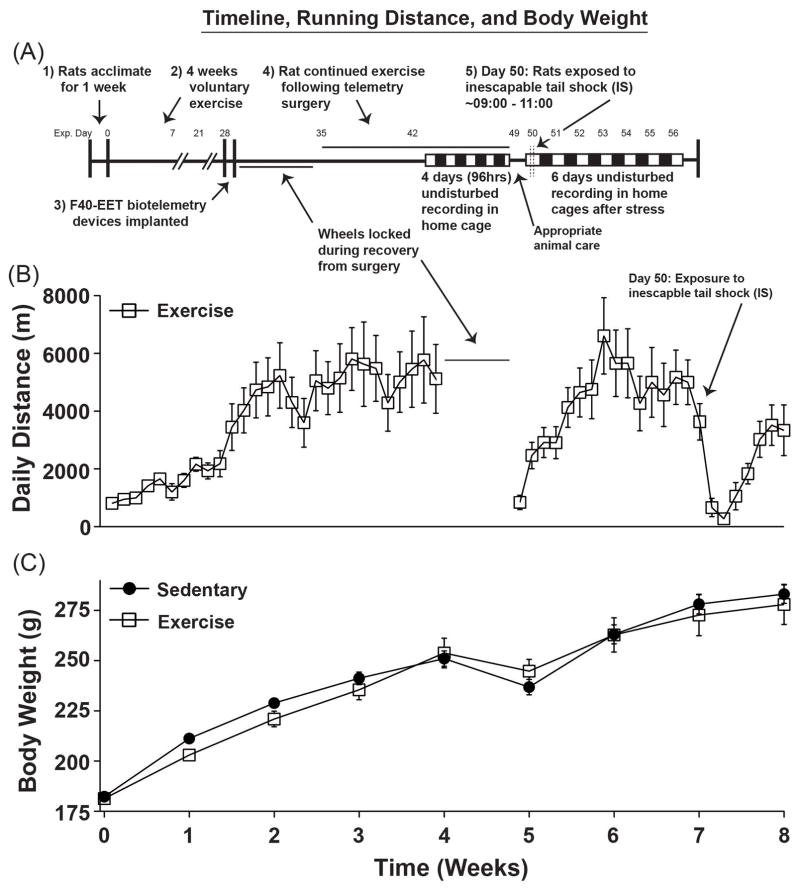
Figure 1.
The experimental timeline, total daily running distances, and body weights are shown. (A) Animals were either sedentary or had access to running wheels (exercise) for 4 weeks prior to telemeter implantation. For the exercise group, the wheels were locked during recovery, but were unlocked for the remainder of the study following recovery from surgery. After stress exposure, all animals were allowed to recover from stress exposure completely undisturbed in their home cages for 6 subsequent days. (B) Total daily running distances across the entirety of the experiment are depicted. Wheels were locked during recovery from implantation of telemetry devices for animal safety. (C) Data are depicted in weekly increments demonstrating normal body weight gain across the experiment. Abbreviations are as follows: experimental (exp.), grams (g) and meters (m).
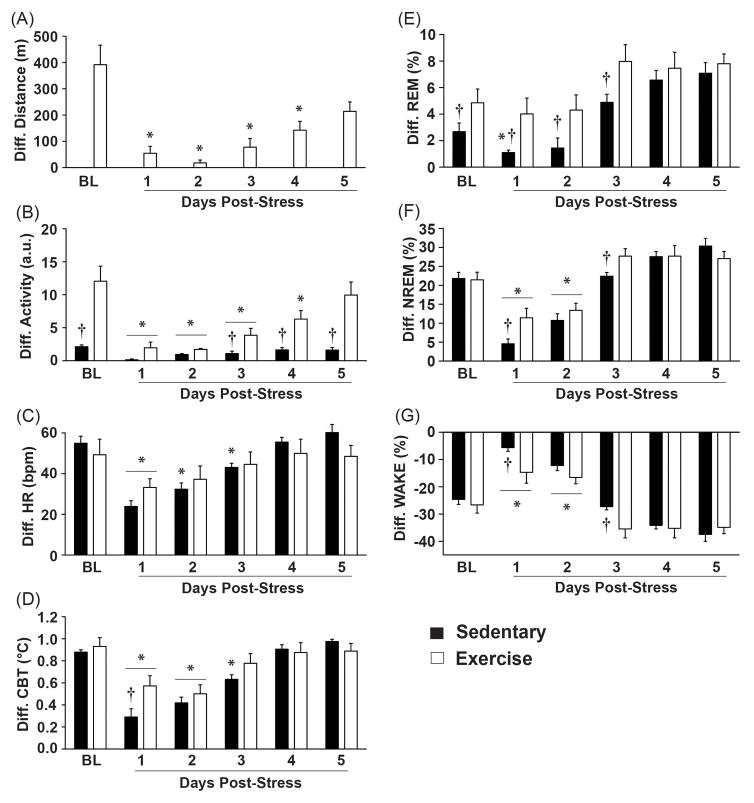
Figure 7.
Data are graphed as diurnal differences in order to identify whether exercise attenuated the stress-induced flattening of diurnal physiological rhythms and sleep/wake behavior. (A) Stress exposure reduced nightly wheel running for post-stress days 1–4, but returned to pre-stress levels by post-stress day 5. (B) Stress exposure significantly flattened the diurnal rhythms of locomotor activity in both groups for post-stress days 1–3, but this effect lasted until post-stress day 4 in the sedentary group. Both groups regained their pre-stress diurnal differences in locomotor activity by post-stress day 5 and the diurnal difference in locomotor activity between the exercise and sedentary groups was again evident at this time. (C) Stress exposure flattened the diurnal rhythms of heart rate in both groups for post-stress day 1, but this effect lasted until post-stress day 3 in the sedentary group. (D) Stress exposure flattened the diurnal rhythms in CBT in both groups until post-stress day 2, but this effect lasted until post-stress day 3 in the sedentary groups. Exercise attenuated the impact of stress on flattening of the diurnal rhythm of CBT on post-stress day 1 only, when compared with sedentary rats. (E) Stress exposure flattened the diurnal rhythm of REM sleep in sedentary rats only on post-stress day 1, but exercise reduced the stress-induced flattening of the diurnal rhythm in REM sleep. The differences in the diurnal rhythm of REM sleep between exercise and sedentary groups were evident both before stress and until post-stress day 3. (F) Stress exposure flattened the diurnal rhythms of NREM sleep in both groups until post-stress day 2. Exercise attenuated the impact of stress on the flattening of the diurnal rhythm of NREM sleep on post-stress day 1 only, when compared with sedentary rats. Although the effects of stress on flattening the diurnal rhythm of NREM sleep had dissipated in both groups by post-stress day 3, exercising rats had a greater diurnal rhythm in NREM sleep when compared to sedentary rats on post-stress day 3. (G) Consistent with the sleep data, stress exposure flattened the diurnal rhythm of WAKE until post-stress day 2. Exercise also reduced the impact of stress on flattening the diurnal rhythm of WAKE on post-stress day 1 only, when compared with the sedentary group. Abbreviations are as follows: arbitrary units (a.u.), pre-stress baseline (BL), beats per minute (bpm), degrees Celsius (°C), diurnal difference (Diff.) and meters (m). (*p < 0.05 effect of stress compared to baseline values; †p < 0.05 exercise compared to sedentary).
Statistical Analysis
All data were analyzed with repeated measures ANOVA either as 20-min blocks (Figures 5 and 6), 1-hour blocks (Figures 2, 3), as diurnal differences (Figure 7) or as weeks (Figure 1), where the sedentary and exercise conditions were used as factors. The diurnal differences were calculated using the averages of the differences between the lights-on values and the lights-off values as previously described (Greenwood et al. 2014; Thompson et al. 2013; Thompson et al. 2014). Additionally, during stress exposure the 20-min block data (Figures 5 and 6) were collapsed into pre-stress (4 hours), during stress (2 hours) or post-stress exposure (14 hours). Finally, multiple linear regression analyses were performed to examine potential significant relationships between variables. When appropriate, post hoc analyses for multiple comparisons were performed using Fisher’s protected least significant differences (PLSD). Alpha was set to p < 0.05.
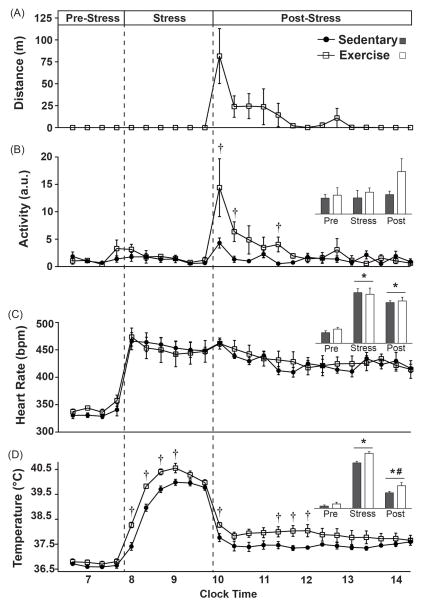
Figure 5.
Physiological data on the day of exposure to stress are graphed in 20-minute blocks (or averaged, insets) before stress in the home cage, during stress and immediately after stress upon return to the home cage. There were no differences between groups one hour prior to stressor exposure. (A) Wheel running and (B) locomotor activity were increased upon return to the home cage following stress, but there were no differences in locomotor activity during stress exposure. (C) Although stress increased heart rate, it did so equally and did not differ between groups upon return to the home cage following stress. (D) CBT was also elevated as a result of stress exposure, but CBT was higher in animals with prior access to running wheels during stress. CBT remained slightly elevated after return to the home cage following stress, but was slightly higher in exercising animals which may have been a result of the increased wheel running immediately following stress exposure. Abbreviations are as follows: arbitrary units (a.u.), beats per minute (bpm), degrees Celsius (°C) and meters (m). (*p < 0.05 compared to pre-stress values; #p < 0.05 compared to during stress values; †p < 0.05 exercise compared to sedentary).
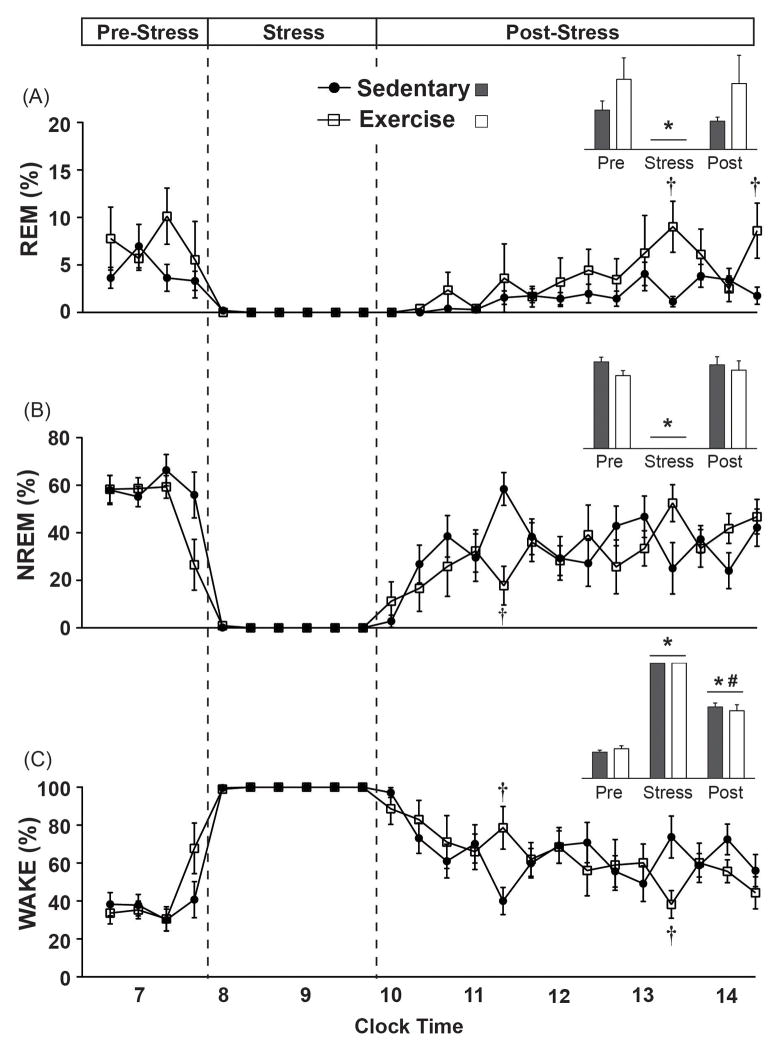
Figure 6.
Sleep/Wake behavior on the day of exposure to stress is graphed in 20-minute blocks (or averaged, insets) before stress in the home cage, during stress and immediately after stress upon return to the home cage. There were no differences between groups in the hour prior to stress exposure. (A) Stress exposure eliminated REM sleep in both groups, which initially remained reduced following stress, but was not reduced on average (inset). Several hours after stress exposure, exercising rats spent slightly more time in REM sleep when compared to sedentary rats. (B) Stress exposure also eliminated NREM sleep in both groups. Immediately following stress exposure, exercising rats spent slightly less time in NREM sleep and had a trend towards increased NREM sleep several hours later. (C) During stress exposure time spent in WAKE was increased to a maximum. Immediately following stress, exercising rats initially spent slightly more time in WAKE, but several hours later spent slightly less time in WAKE. (* p < 0.05 compared to pre-stress values; #p < 0.05 compared to during stress values; †p < 0.05 exercise compared to sedentary).
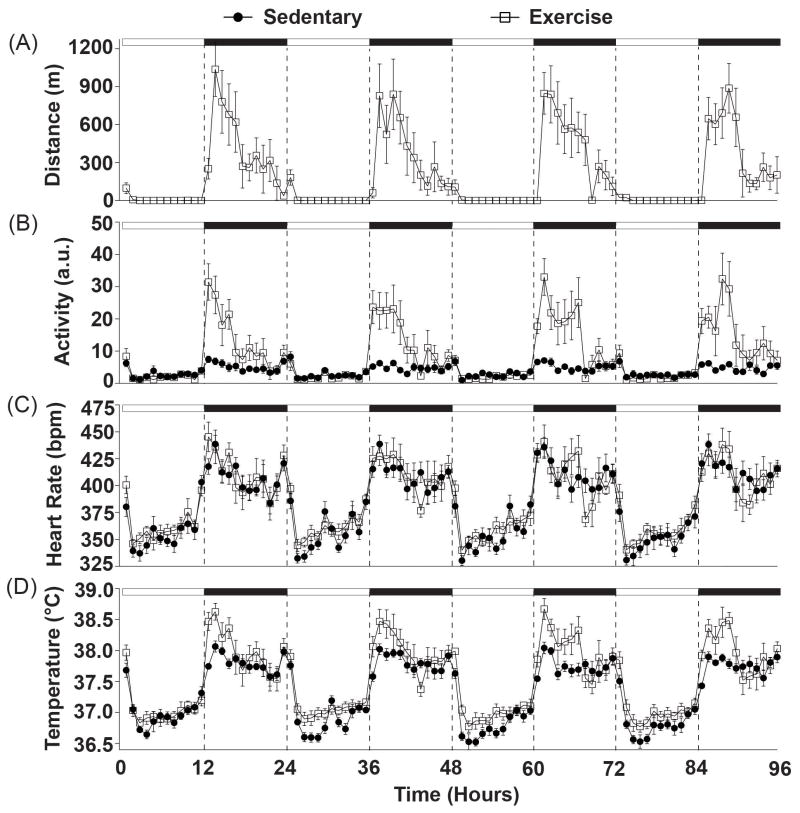
Figure 2.
Physiological data are graphed in 1-hr blocks collected during 96 hours (experimental days 45–48) of completely undisturbed monitoring in order to assess the effects of regular voluntary physical activity on diurnal physiological rhythms when compared with sedentary rats. Rats preferred to run on the wheels (A) during the early nocturnal phase (p < 0.01) and (B) had increased locomotor activity at that time when compared with sedentary rats (p < 0.01). (C) There were no differences in the heart rate after six weeks of prior wheel running, but (D) wheel running produced increases in CBT (p < 0.05) during the peak and nadir of the diurnal temperature cycle (p < 0.01). Abbreviations are as follows: arbitrary units (a.u.), beats per minute (bpm), degrees Celsius (°C) and meters (m).
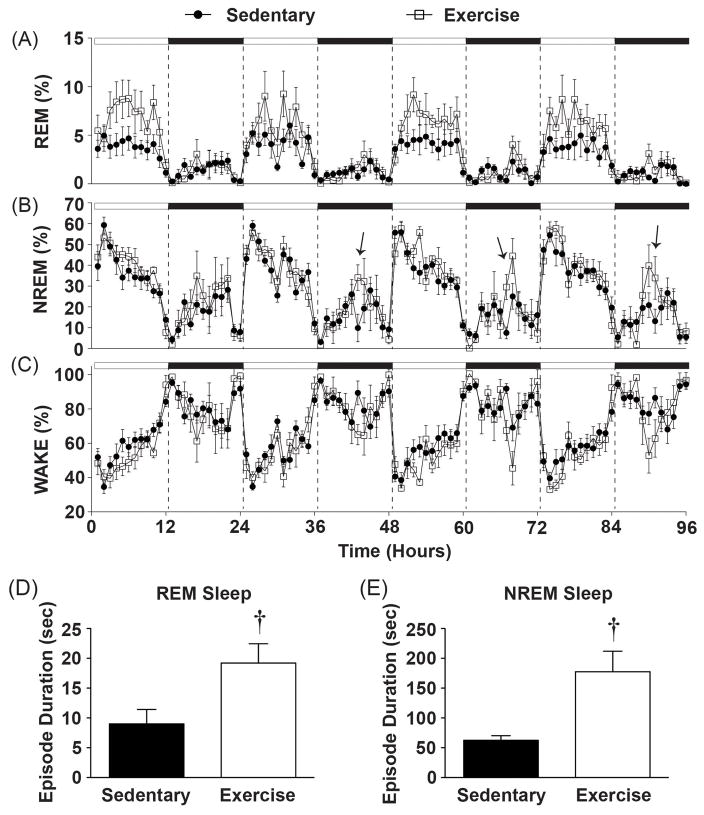
Figure 3.
Sleep data graphed in 1-hr blocks revealing that (A) Physically active rats had a significant increase in the time spent in REM sleep during the light cycle. (B) There were no significant differences in the time spent in NREM. (C) There were no significant differences in the time spent in the WAKE state. Importantly, immediately following peak wheel running (mid-dark cycle) exercising rats had on average (D) longer REM episode durations and E) NREM episode durations when compared with sedentary rats (see results for details). Arrows denote times when NREM sleep was significantly different in physically active vs. sedentary rats. (†p < 0.05 exercise compared to sedentary).
Results
Experimental Timeline and Total Running Distance
Figure 1 delineates the experimental timeline (Figure 1A), total daily distance run (Figure 1B), and average body weights (Figure 1C) throughout the experiment. Physically active rats increased total running distance prior to telemetry implantation (F(27, 135) = 8.137; p < 0.0001; main effect of time during weeks 0–4; Figure 1B). Surgery temporarily reduced the daily distance run (F(22, 110) = 10.122; p < 0.0001; main effect of time during weeks 5–8; Figure 1B), but running distance quickly recovered to pre-surgery levels before stress exposure. Prior to surgical implantation of the biotelemetry devices, there was a trend towards lower body weights in exercising rats across time (F(3, 36 ) = 2.47; p = 0.07; interaction between exercise and time during weeks 0–4; Figure 1C). Following implantation, physically active rats weighed slightly more than sedentary rats initially (Week 5), but as they continued exercise they weighed slightly less by week 8 (F(3, 36 ) = 4.528; p = 0.0086; interaction between exercise and time during weeks 5–8; Figure 1C) post-hoc analysis revealed no main effects of exercise on body weight from Weeks 5–8.
Voluntary Exercise Increases Locomotor Activity and Shifts Diurnal CBT Curve Higher
Diurnal variations in physiological parameters in physically active and sedentary rats are shown in Figures 2 and 3 during a 96-hour time period (experimental days 45–48) where rats remained completely undisturbed in their home cages. There was a significant effect of time on running wheel behavior in the physically active group (F(5, 95) = 6.135; p < 0.0001; Figure 2A), indicating that rats with wheels in their cages voluntarily ran primarily during the dark cycle. This wheel running behavior was consistent with more overall locomotor activity in physically active rats when compared to sedentary rats (F(1, 12) = 26.985; p = 0.0002; Figure 2B) and also occurred primarily during the dark cycle (F(95, 1141) = 5.996; p < 0.0001; interaction between exercise and time; Figures 2B).
After 6 weeks of voluntary exercise there was no statistically significant effect of physical activity on heart rate (Figure 2C) which is consistent with prior findings (Masini et al. 2011), however; several weeks earlier (Experimental days 35–38; 96-hours) physically active rats did have a larger increase in heart rate at the onset of the dark cycle when compared with sedentary rats (F(95, 1141) = 1.696; p < 0.0001; interaction between exercise and time; data not shown). These results raise the possibility that cardiovascular adaptations may have occurred between 4–6 weeks of voluntary wheel running.
Prior physical activity shifted the diurnal CBT curve higher (F(1, 12) = 6.351; p = 0.0269; main effect of exercise; Figure 2D) and this effect was most evident during the peak and nadir of the diurnal temperature cycle (F(95, 1140) = 2.03; p < 0.0001; interaction between exercise and time; Figure 2D).
Voluntary Exercise Alters Sleep/Wake Behavior in a Diurnal Specific Manner
Regular physical activity also entrained sleep/wake behavior. Voluntary exercise resulted in significantly more time spent in the REM sleep state during the light cycle (F(95, 1140) = 1.787; p < 0.0001; interaction between exercise and time; Figure 3A), but there was only a trend towards a greater number of REM bouts across the same time period (F(1, 12) = 3.856; p = 0.0731; main effect of exercise; data not shown). There were no differences in the average duration of REM bouts across the 96-hour period between sedentary and physically active rats.
Six weeks of physical activity had less impact on the percent of time spent in NREM sleep (Figure 3B), however exercise altered sleep architecture. Immediately following the peak of voluntary physical activity (mid-dark cycle), the exercise group had longer average NREM bout lengths for each of the four dark cycles of the 96-hour baseline period (F(95, 1140) = 1.592; p = 0.0004; interaction between exercise and time; data for NREM bout length across hours not shown) and had a greater number of NREM bouts (F(95, 1140) = 2.036; p < 0.0001; interaction between exercise and time; data not shown) when compared with the sedentary group.
A more in depth analysis of sleep architecture revealed that exercising rats had longer NREM bouts when compared to sedentary rats for the first hour immediately following peak wheel running, which was consistently 6 hours after lights off or mid-dark cycle (Figure 3B; see arrows). Figure 3E depicts the average of the first hour immediately after peak wheel running for each of the days of baseline recording for NREM bouts. These results demonstrate that physically active rats had longer average NREM bout durations at this time when compared to sedentary rats (F(1, 12) =14.012; p = 0.0028; main effect of exercise; Figure 3E), thus revealing greater consolidation of NREM sleep immediately following voluntary exercise. Although there were no overall statistical differences in average REM bout durations across the 96-hour undisturbed recording period as stated previously, it should be noted that exercising rats also had longer REM bouts immediately following cessation of peak wheel running which was also consistent with the 96-hour undisturbed recording period (F(1, 12) = 6.667; p = 0.0240; main effect of exercise; Figure 3D).
Finally, there was a trend towards reduced percent of time spent in WAKE across the 96-hour period in physically active animals although this did not reach significance (F(95, 1140) = 1.217; p = 0.0843; Figure 3C).
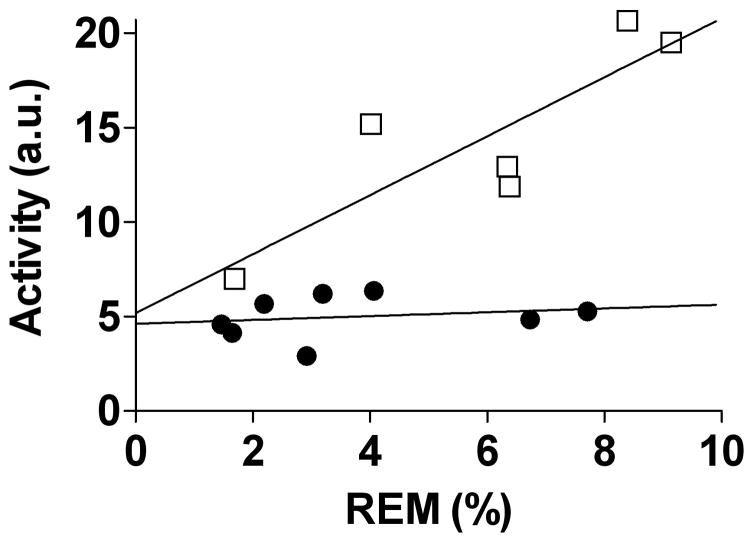
One intriguing finding, based on stepwise multiple regression analysis, was that higher nocturnal locomotor activity levels in exercising animals were positively correlated (y = 0.617x + (−1.61)) with more time spent in the REM sleep state (F(1, 5) = 18.966; p = 0.012; Figure 4, open squares) during the lights on period. Although there was a similar linear relationship between the average distance run (meters) during the dark cycle and time spent in the REM sleep state during the light cycle, this did not reach statistical significance (F(1, 5) = 2.729; p = 0.1739; data not shown). In contrast to the exercise group, there was no such relationship between nocturnal locomotor activity and time spent in REM sleep during the light cycle in the sedentary group (Figure 4, closed circles).
Figure 4.
Multiple linear regression analysis revealed that exercising animals (open squares) with greater amounts of exercised induced locomotor activity spent more time in REM sleep throughout the 96-hour baseline period. The adjusted r2 = 0.782; p < 0.05 suggesting that the exercise induced variance in locomotor activity can account for 78% of the variance in REM sleep using the following equation: y = 0.617x + (−1.61). In contrast, the sedentary animals (closed circles) had no such relationship. Abbreviations are as follows: arbitrary units (a.u.), rapid eye movement (REM).
Exercise Alters Physiological Responses and Sleep/Wake Behavior in the Hours Following Acute Stress Exposure
Figures 5 and 6 depict the effects of the interaction between stress and exercise on physiology and sleep/wake behavior for the remaining light cycle (~5 hours) following stress exposure on experimental day 50. These data are depicted in twenty-minute blocks obtained in the home cage immediately prior to stressor exposure (pre-stress), during exposure to stress, and upon return to the home cage (post-stress). The averaged values of each time (pre-stress, stress, and post-stress) are shown in the graph insets. There were no statistical differences between groups in any measure immediately prior to stressor exposure (pre-stress). Struggling in the tail shock tubes can be accurately represented by locomotor activity during stress (Thompson et al. 2014). Struggling behavior during stress did not differ between groups (Figure 5B; during stress). Physically active rats, however, had increased locomotor activity following stress exposure when compared with the sedentary rats (F(13, 156) = 3.745; p < 0.0001; Figure 5B), which was consistent with increased wheel running following acute stress in the physically active animals (F(5, 13) = 3.967; p < 0.0001; Figure 5A).
Stressor exposure increased heart rate to the same extent in physically active and sedentary rats and it remained elevated above pre-stress levels upon return to the home cage for several hours (F(2, 24) = 86.067; p < 0.0001; main effect of stress; see Figure 5C inset for results of post hoc analysis). Similarly, CBT increased during stress and remained elevated following stress; though CBT following stress wasn’t as elevated as during stress (F(2, 24) = 478.375; p < 0.0001; main effect of stress; see Figure 5D inset for results of post hoc analysis).
The exercise group reached a higher CBT during stress when compared with the sedentary group (F(1, 12) = 15.576; p = 0.0019; main effect of exercise; see Figure 5D for results of post hoc analysis) although both groups had similar CBT’s by the end of stressor exposure (F(5, 60) = 4.499; p = 0.0015; interaction between exercise and time; Figure 5D). Physically active rats had higher CBT’s for several hours following acute stress (F(1, 12) = 5.237; p < 0.041; main effect of exercise; see Figure 5D for results of post hoc analysis).
Stress exposure reduced the time spent in REM sleep (F(2, 24) = 15.741; p < 0.0001; main effect of stress; see Figure 6A inset for results of post hoc analysis) and NREM sleep (F(2, 24) = 124.953; p < 0.0001; main effect of stress; see Figure 6B inset for results of post hoc analysis) to a minimum, but increased time spent in WAKE to a maximum (F(2, 24) = 373.845; p < 0.0001; main effect of stress; see Figure 6C inset for results of post hoc analysis).
Following stress, exercising rats spent slightly more time in REM sleep (F(13, 156) = 2.495; p = 0.004; interaction between exercise and time; see Figure 6A for results of post hoc analysis). In contrast, exercising rats spent less time in NREM sleep immediately following stress (F(13, 156) = 2.289; p = 0.0085; interaction between exercise and time; see Figure 6B for results of post hoc analysis). Consistent with the sleep data, exercising rats initially spent more time in WAKE immediately following stress exposure when compared to the sedentary rats but spent significantly less time in WAKE several hours later (F(13, 156) = 2.167; p = 0.013; interaction between exercise and time; see Figure 6C for results of post hoc analysis).
Voluntary Exercise Protects Against Stress-Induced Flattening of the Diurnal Rhythms of Sleep and Temperature
Stress exposure reduced the nightly running distances for post-stress days 1–4, which returned to pre-stress levels by post-stress day 5 (F(5, 25) = 7.205; p = 0.0003; main effect of stress; see Figure 7A for results of post hoc analysis). Exercising rats had greater levels of locomotor activity both before and after stress exposure (F(1, 12) = 29.943; p = 0.0001; main effect of exercise; see Figure 7B for results of post hoc analysis). Stress exposure significantly flattened the diurnal rhythm of locomotor activity in both groups for post-stress days 1–3 (F(5, 60) = 21.587; p < 0.0001; main effect of stress; see Figure 7B for results of post hoc analysis), but this effect lasted longer in the exercise group (F(5, 60) = 12.2294; p < 0.0001; interaction between exercise and stress; see Figure 7B for results of post hoc analysis) likely due to the large exercise effect on the diurnal difference of locomotor activity at baseline. Stress exposure also flattened the diurnal rhythm of heart rate in both groups for post-stress day 1 (F(5, 60) = 20.242; p < 0.0001; main effect of stress; see Figure 7C for results of post hoc analysis). Flattening of diurnal rhythm of heart rate persisted longer in the sedentary relative to the physically active group (F(5, 60) = 2.689; p = 0.0294; interaction between exercise and stress; see Figure 7C for results of post hoc analysis). Stress exposure significantly flattened the diurnal rhythm of CBT in both groups for post-stress days 1 and 2, but this effect persisted until post-stress day 3 in the sedentary group (F(5, 60) = 50.110; p < 0.0001; main effect of stress ; see Figure 7D for results of post hoc analysis). Exercise, however, attenuated the stress-induced flattening of the diurnal rhythm of CBT (F(5, 60) = 4.117; p = 0.0028; interaction between exercise and stress; see Figure 7D for results of post hoc analysis).
Stress exposure flattened the diurnal rhythm of REM sleep in the sedentary group, but stress had little effect on the diurnal rhythm of REM sleep in the exercise group (F(5, 60) =27.629; p < 0.0001; main effect of stress; see Figure 7E for results of post hoc analysis). This result was likely due to the pre-stress differences in the diurnal rhythms of REM sleep between exercising and sedentary groups (F(1, 12) = 5.160; p = 0.042; main effect of exercise; see Figure 7E for results of post hoc analysis). Stress exposure also flattened the diurnal rhythm of NREM sleep in both groups until post-stress day 2 (F(5, 60) = 67.542; p < 0.0001; main effect of stress; Figure 7E) and voluntary exercise also attenuated the magnitude of the stress-induced flattening of the diurnal rhythm of NREM sleep (F(5, 60) = 3.302; p = 0.010; interaction between exercise and stress; see Figure 7F for results of post hoc analysis). Consistent with the NREM data, stress exposure also disrupted the diurnal rhythm of WAKE until post-stress day 2 (F(5, 60) = 69.303; p < 0.0001; main effect of stress; see Figure 7F for results of post hoc analysis) and voluntary exercise attenuated the disruption of the diurnal rhythm of WAKE following stress exposure (F(5, 60) = 3.063; p = 0.015; interaction between exercise and stress; see Figure 7G for results of post hoc analysis).
Discussion
The results from this study support the hypothesis that prior wheel running improves sleep and attenuates the disruptions in sleep/wake behavior and physiological rhythms following acute stressor exposure. By using in vivo continuous wireless biotelemetry measurement of LA, HR, CBT and EEG in freely behaving animals, we found a significant linear relationship between increased nocturnal physical activity and increased time spent in REM sleep. Although prior studies have reported increased REM sleep following exercise (Blanco-Centurion & Shiromani 2006; Gambelunghe et al. 2001; Hanagasioglu et al. 1982; Lancel et al. 2003), our results suggest a direct relationship between increased locomotor activity for animals with access to a running wheel, and increased REM sleep. Thus increased physical activity is associated with changes in sleep architecture prior to stressor exposure.
Stressor exposure substantially disrupts REM sleep in sedentary rats which is consistent with earlier findings (Cheeta et al. 1997; Greenwood et al. 2014; Kant et al. 1995; Papale et al. 2005; Pawlyk et al. 2008; Rampin et al. 1991), but we show here for the first time that this effect was attenuated in exercising rats. Sufficient REM sleep appears to be important for recovery from stressful events or situations, especially in those with stress-related disorders (Germain & Nielsen 2003; Kyung Lee & Douglass 2010). In fact, victims of traffic accidents that slept more and had more consolidated REM sleep episodes didn’t go on to develop post-traumatic stress disorder (Mellman et al. 2007), which highlights the importance of sufficient REM sleep following aversive events. This idea is consistent with the finding that rats who lost REM rebound after stressor exposure to a traumatic event expressed the greatest stress sensitization (Greenwood et al. 2014; Thompson et al. 2014). In our study, wheel running attenuated the stress-induced diurnal disruption of REM sleep. It may be possible that exercise induced improvements in REM sleep underlie, in part, the preventative benefits of physical activity in affective disorders.
We also discovered that 6 weeks of wheel running in freely behaving animals improves NREM sleep quality in a diurnally dependent manner. A similar pre-clinical study found that both young and old F344 rats had displayed slightly better NREM sleep quality after 8 weeks of exercise, although they used forced exercise in a slowly rotating wheel for only 50 minutes per night (Blanco-Centurion & Shiromani 2006). In another study using forced rota-rod running, light physical exercise for 45 minutes also resulted in improved NREM sleep immediately after exercise, which was the only time sleep was measured in this study (Gambelunghe et al. 2001). The current results and prior studies are also consistent with the clinical literature where it has been found that trained individuals have higher levels of NREM sleep compared with untrained controls. For example, female swimmers spent more time in NREM sleep at sleep onset following increased training as the swim season progressed (Taylor et al. 1997), suggesting a link between increased physical activity and increased need for NREM sleep especially at sleep onset. Another clinical study in females demonstrated that physical activity with concomitant increases in external temperatures also significantly increased time spent in NREM sleep (Horne et al. 1985), which reveals the potential connection between temperature and activity induced changes in NREM sleep. Thus the current results are in agreement with previous studies but also extend our understanding of wheel running, NREM sleep patterns, and how they relate to each other in a diurnally dependent manner. One current hypothesis of the function of NREM sleep is that it may help reorganize and strengthen synapses in response to daily activities (Tononi et al. 2012) and it is believed that during NREM sleep slow wave oscillations are occurring between the thalamus and the cortex (de Andres et al. 2011), however the specific purpose of NREM sleep remains poorly understood. Interestingly, there may be a connection between increased temperature and the induction of NREM sleep that could involve the pre-optic area of the hypothalamus (McGinty et al. 2001), which could account for the finding that physically active rats had better NREM sleep immediately after wheel running.
Stressor exposure also produced a disruption in the diurnal rhythm of NREM sleep in sedentary rats but this effect was attenuated in exercising rats. Our results are the first to demonstrate that prior wheel running can attenuate the stress-induced disruption of the diurnal rhythm of NREM sleep following stress exposure, thus based on previous work and our current findings, exercise both produces better quality of NREM sleep (Blanco-Centurion & Shiromani 2006; Gambelunghe et al. 2001) and protects NREM from stress-induced disruptions. Interestingly, Dang-Vu et al., 2015 recently reported that better NREM quality may decrease vulnerability to stress-induced sleep disruptions (Dang-Vu et al. 2015). It is well known that disruptions of diurnal rhythms are prevalent in those with stress-related disorders (Cole et al. 1990; Emens et al. 2009; Hasler et al. 2010; Scott et al. 1997) and that reducing their disruption may benefit health.
Prior to stressor exposure, voluntary exercise increased CBT body temperature both during the active (dark) and inactive (light), cycles. These results are consistent with prior literature demonstrating an effect of exercise on CBT (Blanco-Centurion & Shiromani 2006; Masini et al. 2011). Similar to the effect of stress on sleep/wake diurnal rhythms, stressor exposure flattened the diurnal rhythm of CBT in sedentary rats, and exercise attenuated this effect. Interestingly, this effect of regular physical activity on CBT could also contribute to many of the protective effects of exercise on the negative health consequences of stress, including mood disorders. For example, increasing body temperature alone can alleviate symptoms of depression in depressed patients (Hanusch et al. 2013; Koltyn et al. 1992) and depressed individuals have deficits in thermoregulatory cooling (Ward et al. 1986). Additionally, individuals who are exercise trained activate thermoregulatory cooling mechanisms more efficiently than untrained controls (Cramer et al. 2012; Ichinose-Kuwahara et al. 2010). Thus it seems plausible that the antidepressant-like effects of exercise may depend, in part, on alterations in thermoregulation; however the potential mechanisms remain poorly understood.
One possibility is that repeated low-intensity exercise bouts, such as that in voluntary wheel running, repeatedly increased CBT thus stimulating thermoregulatory centers in the brain. Two thermoregulatory centers that could be involved are the serotonergic neurons in the dorsal raphé nucleus and the pre-optic area of the hypothalamus. Lowry and colleagues have hypothesized that temperate sensitive serotonergic neurons in the dorsal raphé nucleus may contribute to antidepressant effects (Hale et al. 2013) and it is known that serotonergic neurons in the dorsal raphé nucleus are important for mediating the antidepressant-like effects of voluntary free wheel running (Greenwood et al. 2005b; Greenwood et al. 2003). Voluntary exercise can also activate preoptic neurons responsible for thermoregulation (Hasegawa et al. 2005) and activation of warm-sensitive neurons in the preoptic area can promote sleep onset (Kumar et al. 2011; McGinty et al. 1994). In fact, the preoptic area is important in both thermoregulation and sleep regulation as lesions of the preoptic area can decrease NREM sleep and increase REM sleep (Mendelson 1998). It could be possible that repeated increases in locomotor activity led to repeated increases in CBT, subsequently activating thermosensitive brain regions like the preoptic area (McGinty & Szymusiak 2001), thus improving sleep/wake behavior and facilitating a stress-protective phenotype.
Conclusions
Regular physical activity can both prevent and reduce the severity of stress-related disorders. Given the link between disruptions in sleep, diurnal rhythms and stress-related disorders (Breslau et al. 2004; Emens et al. 2009; Germain & Nielsen 2003; Hasler et al. 2010; Kyung Lee & Douglass 2010; Ohayon & Roth 2001; Papadimitriou & Linkowski 2005; van Liempt et al. 2012), it may be possible that the impacts of exercise on sleep and diurnal rhythms, contribute to these effects. Despite these associations, a thorough understanding of the role of sleep recovery in response to stressful situations remains elusive (Sanford et al. 2014); however our data add that exercise protects against the stress-induced flattening of diurnal rhythms of NREM/REM sleep and body temperature which could reduce the negative consequences of stress exposure and/or enhance recovery following aversive events. More research is needed to understand the specific patterns of sleep recovery following aversive events that are beneficial to physical and mental well-being.
Supplementary Material
Figure S1 – Data are graphed in 1-hour blocks from the first dark cycle (experimental day 51) until the sixth dark cycle (experimental day 56) following stress exposure. A) Rodents with access to running wheels regained their pre-stress levels of running distance around the sixth dark cycle after stress (F131, 655) = 5.477; p < 0.0001; main effect of time). B) Although stress reduced locomotor activity for both groups, rodents with access to running wheels continued to have higher levels of locomotor activity following several days of recovery (F(1, 12) = 18.057; p = 0.0011; main effect of exercise) and took longer to regain pre-stress levels of nocturnal locomotor activity when compared with the sedentary rodents (F(131, 1572) = 5.672; p < 0.0001; interaction between exercise and time) likely due to pre-existing higher levels of locomotor activity before stress exposure. C) Although there didn’t appear to be differences in heart rate between exercising and sedentary rodents prior to stress exposure (see Figure 2C), in the days following stress exposure there was a slight difference in heart rates between the two groups (F(131, 1572) = 1.699; p < 0.0001; interaction between exercise and time). D) Stress exposure altered the exercise induced CBT differences that were present prior to stress exposure, however; these exercise induced differences returned following 5–6 days of recovery from stress (F(131, 1572) = 2.177; p < 0.0001; interaction between exercise and time; Figure S1D). E) Exercising rodents continued to spend more time in REM sleep when compared to sedentary rodents (F(131, 1572) = 1.258; p = 0.0301; interaction between exercise and time) although this difference appeared reduced following 6 days of recovery after stress exposure. F) Although there were no substantial differences in the amount of time spent in NREM sleep prior to stress exposure, exercising rodents spent more time in NREM sleep following several days of recovery from stress exposure, primarily during the mid-dark cycles (F(131, 1572) = 1.394; p = 0.0031; interaction between exercise and time; see arrows). G) Consistent with the sleep data exercising rodents spent less time in WAKE when compared to sedentary rodents following stress exposure (F(131, 1572) = 1.410; p = 0.0023; interaction between exercise and time). Abbreviations are as follows: arbitrary units (a.u.), beats per minute (bpm), degrees Celsius (°C), and meters (m).
Acknowledgments
This study was generously supported by The National Institutes of Health (NIH RO1 MH068283) and by the Department of Defense Enabling Stress Resistance initiative (DARPA W911NF-10-1-0050).
Footnotes
Declaration of Interest
There are no financial conflicts of interest
References
- Avery DH, Wildschiodtz G, Rafaelsen OJ. Nocturnal temperature in affective disorder. Journal of affective disorders. 1982;4(1):61–71. doi: 10.1016/0165-0327(82)90020-9. [DOI] [PubMed] [Google Scholar]
- Babyak M, Blumenthal JA, Herman S, et al. Exercise treatment for major depression: maintenance of therapeutic benefit at 10 months. Psychosomatic medicine. 2000;62(5):633–8. doi: 10.1097/00006842-200009000-00006. [DOI] [PubMed] [Google Scholar]
- Barbour KA, Edenfield TM, Blumenthal JA. Exercise as a treatment for depression and other psychiatric disorders: a review. Journal of cardiopulmonary rehabilitation and prevention. 2007;27(6):359–67. doi: 10.1097/01.HCR.0000300262.69645.95. [DOI] [PubMed] [Google Scholar]
- Blanco-Centurion CA, Shiromani PJ. Beneficial effects of regular exercise on sleep in old F344 rats. Neurobiology of aging. 2006;27(12):1859–69. doi: 10.1016/j.neurobiolaging.2005.10.009. [DOI] [PubMed] [Google Scholar]
- Blumenthal JA, Babyak MA, Doraiswamy PM, et al. Exercise and pharmacotherapy in the treatment of major depressive disorder. Psychosomatic medicine. 2007;69(7):587–96. doi: 10.1097/PSY.0b013e318148c19a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau N, Roth T, Burduvali E, et al. Sleep in lifetime posttraumatic stress disorder: a community-based polysomnographic study. Archives of general psychiatry. 2004;61(5):508–16. doi: 10.1001/archpsyc.61.5.508. [DOI] [PubMed] [Google Scholar]
- Campbell IG. EEG recording and analysis for sleep research. In: Crawley Jacqueline N, et al., editors. Current protocols in neuroscience / editorial board, Jacqueline N. Crawley … [et al.] Unit 10. Chapter 10. 2009. p. 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheeta S, Ruigt G, van Proosdij J, et al. Changes in sleep architecture following chronic mild stress. Biological psychiatry. 1997;41(4):419–27. doi: 10.1016/S0006-3223(96)00058-3. [DOI] [PubMed] [Google Scholar]
- Cole RJ, Loving RT, Kripke DF. Psychiatric aspects of shiftwork. Occupational medicine. 1990;5(2):301–14. [PubMed] [Google Scholar]
- Cramer MN, Bain AR, Jay O. Local sweating on the forehead, but not forearm, is influenced by aerobic fitness independently of heat balance requirements during exercise. Experimental physiology. 2012;97(5):572–82. doi: 10.1113/expphysiol.2011.061374. [DOI] [PubMed] [Google Scholar]
- Dang-Vu TT, Salimi A, Boucetta S, et al. Sleep spindles predict stress-related increases in sleep disturbances. Frontiers in human neuroscience. 2015;9:68. doi: 10.3389/fnhum.2015.00068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson CL, Babson KA, Bonn-Miller MO, et al. The impact of exercise on suicide risk: examining pathways through depression, PTSD, and sleep in an inpatient sample of veterans. Suicide & life-threatening behavior. 2013;43(3):279–89. doi: 10.1111/sltb.12014. [DOI] [PubMed] [Google Scholar]
- de Andres I, Garzon M, Reinoso-Suarez F. Functional Anatomy of Non-REM Sleep. Frontiers in neurology. 2011;2:70. doi: 10.3389/fneur.2011.00070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duman CH, Schlesinger L, Russell DS, et al. Voluntary exercise produces antidepressant and anxiolytic behavioral effects in mice. Brain research. 2008;1199:148–58. doi: 10.1016/j.brainres.2007.12.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn AL, Trivedi MH, Kampert JB, et al. Exercise treatment for depression: efficacy and dose response. American journal of preventive medicine. 2005;28(1):1–8. doi: 10.1016/j.amepre.2004.09.003. [DOI] [PubMed] [Google Scholar]
- Edgar DM, Dement WC. Regularly scheduled voluntary exercise synchronizes the mouse circadian clock. The American journal of physiology. 1991;261(4 Pt 2):R928–33. doi: 10.1152/ajpregu.1991.261.4.R928. [DOI] [PubMed] [Google Scholar]
- Emens J, Lewy A, Kinzie JM, et al. Circadian misalignment in major depressive disorder. Psychiatry research. 2009;168(3):259–61. doi: 10.1016/j.psychres.2009.04.009. [DOI] [PubMed] [Google Scholar]
- Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA : the journal of the American Medical Association. 1989;262(11):1479–84. doi: 10.1001/jama.262.11.1479. [DOI] [PubMed] [Google Scholar]
- Gambelunghe C, Rossi R, Mariucci G, et al. Effects of light physical exercise on sleep regulation in rats. Medicine and science in sports and exercise. 2001;33(1):57–60. doi: 10.1097/00005768-200101000-00010. [DOI] [PubMed] [Google Scholar]
- Germain A, Nielsen TA. Sleep pathophysiology in posttraumatic stress disorder and idiopathic nightmare sufferers. Biological psychiatry. 2003;54(10):1092–8. doi: 10.1016/s0006-3223(03)00071-4. [DOI] [PubMed] [Google Scholar]
- Greenwood BN, Fleshner M. Exercise, stress resistance, and central serotonergic systems. Exercise and sport sciences reviews. 2011;39(3):140–9. doi: 10.1097/JES.0b013e31821f7e45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenwood BN, Foley TE, Burhans D, et al. The consequences of uncontrollable stress are sensitive to duration of prior wheel running. Brain research. 2005a;1033(2):164–78. doi: 10.1016/j.brainres.2004.11.037. [DOI] [PubMed] [Google Scholar]
- Greenwood BN, Foley TE, Day HE, et al. Wheel running alters serotonin (5-HT) transporter, 5-HT1A, 5-HT1B, and alpha 1b-adrenergic receptor mRNA in the rat raphe nuclei. Biological psychiatry. 2005b;57(5):559–68. doi: 10.1016/j.biopsych.2004.11.025. [DOI] [PubMed] [Google Scholar]
- Greenwood BN, Foley TE, Day HE, et al. Freewheel running prevents learned helplessness/behavioral depression: role of dorsal raphe serotonergic neurons. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2003;23(7):2889–98. doi: 10.1523/JNEUROSCI.23-07-02889.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenwood BN, Thompson RS, Opp MR, et al. Repeated exposure to conditioned fear stress increases anxiety and delays sleep recovery following exposure to an acute traumatic stressor. Frontiers in Psychiatry. 2014;5:146. doi: 10.3389/fpsyt.2014.00146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale MW, Raison CL, Lowry CA. Integrative physiology of depression and antidepressant drug action: implications for serotonergic mechanisms of action and novel therapeutic strategies for treatment of depression. Pharmacology & therapeutics. 2013;137(1):108–18. doi: 10.1016/j.pharmthera.2012.09.005. [DOI] [PubMed] [Google Scholar]
- Hanagasioglu M, Borbely AA. Effect of voluntary locomotor activity on sleep in the rat. Behavioural brain research. 1982;4(4):359–68. doi: 10.1016/0166-4328(82)90060-2. [DOI] [PubMed] [Google Scholar]
- Hanusch KU, Janssen CH, Billheimer D, et al. Whole-body hyperthermia for the treatment of major depression: associations with thermoregulatory cooling. The American journal of psychiatry. 2013;170(7):802–4. doi: 10.1176/appi.ajp.2013.12111395. [DOI] [PubMed] [Google Scholar]
- Hasegawa H, Ishiwata T, Saito T, et al. Inhibition of the preoptic area and anterior hypothalamus by tetrodotoxin alters thermoregulatory functions in exercising rats. Journal of applied physiology. 2005;98(4):1458–62. doi: 10.1152/japplphysiol.00916.2004. [DOI] [PubMed] [Google Scholar]
- Hasler BP, Buysse DJ, Kupfer DJ, et al. Phase relationships between core body temperature, melatonin, and sleep are associated with depression severity: further evidence for circadian misalignment in non-seasonal depression. Psychiatry research. 2010;178(1):205–7. doi: 10.1016/j.psychres.2010.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horne JA, Moore VJ. Sleep EEG effects of exercise with and without additional body cooling. Electroencephalography and clinical neurophysiology. 1985;60(1):33–8. doi: 10.1016/0013-4694(85)90948-4. [DOI] [PubMed] [Google Scholar]
- Ichinose-Kuwahara T, Inoue Y, Iseki Y, et al. Sex differences in the effects of physical training on sweat gland responses during a graded exercise. Experimental physiology. 2010;95(10):1026–32. doi: 10.1113/expphysiol.2010.053710. [DOI] [PubMed] [Google Scholar]
- Kant GJ, Pastel RH, Bauman RA, et al. Effects of chronic stress on sleep in rats. Physiology & behavior. 1995;57(2):359–65. doi: 10.1016/0031-9384(94)00241-v. [DOI] [PubMed] [Google Scholar]
- Koltyn KF, Robins HI, Schmitt CL, et al. Changes in mood state following whole-body hyperthermia. International journal of hyperthermia : the official journal of European Society for Hyperthermic Oncology, North American Hyperthermia Group. 1992;8(3):305–7. doi: 10.3109/02656739209021785. [DOI] [PubMed] [Google Scholar]
- Kronfeld-Schor N, Einat H. Circadian rhythms and depression: human psychopathology and animal models. Neuropharmacology. 2012;62(1):101–14. doi: 10.1016/j.neuropharm.2011.08.020. [DOI] [PubMed] [Google Scholar]
- Kumar D, Kumar VM, Mallick HN. Warm sensitive neurons of the preoptic area regulate ambient temperature related changes in sleep in the rat. Indian journal of physiology and pharmacology. 2011;55(3):262–71. [PubMed] [Google Scholar]
- Kyung Lee E, Douglass AB. Sleep in psychiatric disorders: where are we now? Canadian journal of psychiatry Revue canadienne de psychiatrie. 2010;55(7):403–12. doi: 10.1177/070674371005500703. [DOI] [PubMed] [Google Scholar]
- Lancel M, Droste SK, Sommer S, et al. Influence of regular voluntary exercise on spontaneous and social stress-affected sleep in mice. The European journal of neuroscience. 2003;17(10):2171–9. doi: 10.1046/j.1460-9568.2003.02658.x. [DOI] [PubMed] [Google Scholar]
- Mallon L, Broman JE, Hetta J. Relationship between insomnia, depression, and mortality: a 12-year follow-up of older adults in the community. International psychogeriatrics / IPA. 2000;12(3):295–306. doi: 10.1017/s1041610200006414. [DOI] [PubMed] [Google Scholar]
- Manger TA, Motta RW. The impact of an exercise program on posttraumatic stress disorder, anxiety, and depression. International journal of emergency mental health. 2005;7(1):49–57. [PubMed] [Google Scholar]
- Masini CV, Nyhuis TJ, Sasse SK, et al. Effects of voluntary wheel running on heart rate, body temperature, and locomotor activity in response to acute and repeated stressor exposures in rats. Stress. 2011;14(3):324–34. doi: 10.3109/10253890.2010.548013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGinty D, Szymusiak R. Brain structures and mechanisms involved in the generation of NREM sleep: focus on the preoptic hypothalamus. Sleep medicine reviews. 2001;5(4):323–42. doi: 10.1053/smrv.2001.0170. [DOI] [PubMed] [Google Scholar]
- McGinty D, Szymusiak R, Thomson D. Preoptic/anterior hypothalamic warming increases EEG delta frequency activity within non-rapid eye movement sleep. Brain research. 1994;667(2):273–7. doi: 10.1016/0006-8993(94)91506-7. [DOI] [PubMed] [Google Scholar]
- Mellman TA, Pigeon WR, Nowell PD, et al. Relationships between REM sleep findings and PTSD symptoms during the early aftermath of trauma. Journal of traumatic stress. 2007;20(5):893–901. doi: 10.1002/jts.20246. [DOI] [PubMed] [Google Scholar]
- Mendelson WB. Effects of parenterally administered triazolam on sleep in rats with lesions of the preoptic area. Pharmacology, biochemistry, and behavior. 1998;61(1):81–6. doi: 10.1016/s0091-3057(98)00080-x. [DOI] [PubMed] [Google Scholar]
- Monk TH, Buysse DJ, Frank E, et al. Nocturnal and circadian body temperatures of depressed outpatients during symptomatic and recovered states. Psychiatry research. 1994;51(3):297–311. doi: 10.1016/0165-1781(94)90016-7. [DOI] [PubMed] [Google Scholar]
- Newman CL, Motta RW. The effects of aerobic exercise on childhood PTSD, anxiety, and depression. International journal of emergency mental health. 2007;9(2):133–58. [PubMed] [Google Scholar]
- Ohayon MM, Roth T. What are the contributing factors for insomnia in the general population? Journal of psychosomatic research. 2001;51(6):745–55. doi: 10.1016/s0022-3999(01)00285-9. [DOI] [PubMed] [Google Scholar]
- Olivadoti MD, Opp MR. Effects of i.c.v administration of interleukin-1 on sleep and body temperature of interleukin-6-deficient mice. Neuroscience. 2008;153(1):338–48. doi: 10.1016/j.neuroscience.2008.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papadimitriou GN, Linkowski P. Sleep disturbance in anxiety disorders. International review of psychiatry. 2005;17(4):229–36. doi: 10.1080/09540260500104524. [DOI] [PubMed] [Google Scholar]
- Papale LA, Andersen ML, Antunes IB, et al. Sleep pattern in rats under different stress modalities. Brain research. 2005;1060(1–2):47–54. doi: 10.1016/j.brainres.2005.08.021. [DOI] [PubMed] [Google Scholar]
- Pawlyk AC, Morrison AR, Ross RJ, et al. Stress-induced changes in sleep in rodents: models and mechanisms. Neuroscience and biobehavioral reviews. 2008;32(1):99–117. doi: 10.1016/j.neubiorev.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Posener JA, DeBattista C, Williams GH, et al. 24-Hour monitoring of cortisol and corticotropin secretion in psychotic and nonpsychotic major depression. Archives of general psychiatry. 2000;57(8):755–60. doi: 10.1001/archpsyc.57.8.755. [DOI] [PubMed] [Google Scholar]
- Rampin C, Cespuglio R, Chastrette N, et al. Immobilisation stress induces a paradoxical sleep rebound in rat. Neuroscience letters. 1991;126(2):113–8. doi: 10.1016/0304-3940(91)90532-x. [DOI] [PubMed] [Google Scholar]
- Riemann D, Berger M, Voderholzer U. Sleep and depression--results from psychobiological studies: an overview. Biological psychology. 2001;57(1–3):67–103. doi: 10.1016/s0301-0511(01)00090-4. [DOI] [PubMed] [Google Scholar]
- Roberts RE, Shema SJ, Kaplan GA, et al. Sleep complaints and depression in an aging cohort: A prospective perspective. The American journal of psychiatry. 2000;157(1):81–8. doi: 10.1176/ajp.157.1.81. [DOI] [PubMed] [Google Scholar]
- Sanford LD, Suchecki D, Meerlo P. Stress, Arousal, and Sleep. Current topics in behavioral neurosciences. 2014 doi: 10.1007/7854_2014_314. [DOI] [PubMed] [Google Scholar]
- Scott AJ, Monk TH, Brink LL. Shiftwork as a Risk Factor for Depression: A Pilot Study. International journal of occupational and environmental health. 1997;3(Supplement 2):S2–S9. [PubMed] [Google Scholar]
- Souetre E, Salvati E, Belugou JL, et al. Circadian rhythms in depression and recovery: evidence for blunted amplitude as the main chronobiological abnormality. Psychiatry research. 1989;28(3):263–78. doi: 10.1016/0165-1781(89)90207-2. [DOI] [PubMed] [Google Scholar]
- Speaker KJ, Cox SS, Paton MM, et al. Six weeks of voluntary wheel running modulates inflammatory protein (MCP-1, IL-6, and IL-10) and DAMP (Hsp72) responses to acute stress in white adipose tissue of lean rats. Brain, behavior, and immunity. 2014;39:87–98. doi: 10.1016/j.bbi.2013.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor SR, Rogers GG, Driver HS. Effects of training volume on sleep, psychological, and selected physiological profiles of elite female swimmers. Medicine and science in sports and exercise. 1997;29(5):688–93. doi: 10.1097/00005768-199705000-00016. [DOI] [PubMed] [Google Scholar]
- Thompson RS, Christianson JP, Maslanik TM, et al. Effects of stressor controllability on diurnal physiological rhythms. Physiology & behavior. 2013;112–113:32–9. doi: 10.1016/j.physbeh.2013.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson RS, Strong PV, Clark PJ, et al. Repeated fear-induced diurnal rhythm disruptions predict PTSD-like sensitized physiological acute stress responses in F344 rats. Acta physiologica. 2014 doi: 10.1111/apha.12239. [DOI] [PubMed] [Google Scholar]
- Thompson RS, Strong PV, Fleshner M. Physiological Consequences of Repeated Exposures to Conditioned Fear. Behavioral Sciences. 2012;2(2):57–78. doi: 10.3390/bs2020057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tononi G, Cirelli C. Time to be SHY? Some comments on sleep and synaptic homeostasis. Neural plasticity. 2012;2012:415250. doi: 10.1155/2012/415250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Liempt S, Arends J, Cluitmans PJ, et al. Sympathetic activity and hypothalamo-pituitary-adrenal axis activity during sleep in post-traumatic stress disorder: A study assessing polysomnography with simultaneous blood sampling. Psychoneuroendocrinology. 2012 doi: 10.1016/j.psyneuen.2012.05.015. [DOI] [PubMed] [Google Scholar]
- Verwey M, Robinson B, Amir S. Recording and analysis of circadian rhythms in running-wheel activity in rodents. Journal of visualized experiments : JoVE. 2013;(71) doi: 10.3791/50186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vollert C, Zagaar M, Hovatta I, et al. Exercise prevents sleep deprivation-associated anxiety-like behavior in rats: potential role of oxidative stress mechanisms. Behavioural brain research. 2011;224(2):233–40. doi: 10.1016/j.bbr.2011.05.010. [DOI] [PubMed] [Google Scholar]
- Ward NG, Doerr HO. Skin conductance. A potentially sensitive and specific marker for depression. The Journal of nervous and mental disease. 1986;174(9):553–9. [PubMed] [Google Scholar]
- Yamanaka Y, Hashimoto S, Tanahashi Y, et al. Physical exercise accelerates reentrainment of human sleep-wake cycle but not of plasma melatonin rhythm to 8-h phase-advanced sleep schedule. American journal of physiology Regulatory, integrative and comparative physiology. 2010;298(3):R681–91. doi: 10.1152/ajpregu.00345.2009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1 – Data are graphed in 1-hour blocks from the first dark cycle (experimental day 51) until the sixth dark cycle (experimental day 56) following stress exposure. A) Rodents with access to running wheels regained their pre-stress levels of running distance around the sixth dark cycle after stress (F131, 655) = 5.477; p < 0.0001; main effect of time). B) Although stress reduced locomotor activity for both groups, rodents with access to running wheels continued to have higher levels of locomotor activity following several days of recovery (F(1, 12) = 18.057; p = 0.0011; main effect of exercise) and took longer to regain pre-stress levels of nocturnal locomotor activity when compared with the sedentary rodents (F(131, 1572) = 5.672; p < 0.0001; interaction between exercise and time) likely due to pre-existing higher levels of locomotor activity before stress exposure. C) Although there didn’t appear to be differences in heart rate between exercising and sedentary rodents prior to stress exposure (see Figure 2C), in the days following stress exposure there was a slight difference in heart rates between the two groups (F(131, 1572) = 1.699; p < 0.0001; interaction between exercise and time). D) Stress exposure altered the exercise induced CBT differences that were present prior to stress exposure, however; these exercise induced differences returned following 5–6 days of recovery from stress (F(131, 1572) = 2.177; p < 0.0001; interaction between exercise and time; Figure S1D). E) Exercising rodents continued to spend more time in REM sleep when compared to sedentary rodents (F(131, 1572) = 1.258; p = 0.0301; interaction between exercise and time) although this difference appeared reduced following 6 days of recovery after stress exposure. F) Although there were no substantial differences in the amount of time spent in NREM sleep prior to stress exposure, exercising rodents spent more time in NREM sleep following several days of recovery from stress exposure, primarily during the mid-dark cycles (F(131, 1572) = 1.394; p = 0.0031; interaction between exercise and time; see arrows). G) Consistent with the sleep data exercising rodents spent less time in WAKE when compared to sedentary rodents following stress exposure (F(131, 1572) = 1.410; p = 0.0023; interaction between exercise and time). Abbreviations are as follows: arbitrary units (a.u.), beats per minute (bpm), degrees Celsius (°C), and meters (m).