Abstract
Background
The frequency of non-cardiac chest pain (CP) hospitalization after acute myocardial infarction (AMI) is unknown, and its significance from patients’ perspectives is not studied.
Objectives
To assess the frequency of non-cardiac CP admissions after AMI and its association with patients’ self-reported health status.
Methods
We identified cardiac and non-cardiac CP hospitalizations in the year after AMI from the 24-center TRIUMPH registry. Hierarchical repeated measures regression was used to identify the association of these hospitalizations with patients’ self-reported health status using the Seattle Angina Questionnaire Quality of Life domain (SAQ QoL) and Short Form 12 (SF-12) physical (PCS) and mental (MCS) component summary scores.
Results
Of 3099 patients, 318 (10.3%) were hospitalized with CP, of whom 92 (28.9%) were hospitalized for non-cardiac CP. Compared with patients not hospitalized with CP, non-cardiac CP hospitalization was associated with poorer health status (SAQ QoL adjusted differences: −8.9 points [95% CI −12.1, −5.6]; SF-12 PCS: −2.5 points [95% CI −4.2, −0.8] and SF-12 MCS: −3.5 points [95% CI −5.1, −1.9]). SAQ QoL for patients hospitalized with non-cardiac CP was similar to patients hospitalized with cardiac CP (adjusted difference: 0.6 points [95% CI −3.2, 4.5]; SF-12 PCS (0.9 points [95% CI −1.1, 2.9]), but was worse with regards to SF-12 MCS (adjusted difference: −2.0 points [95% CI −3.9, −0.2]).
Conclusions
Non-cardiac CP accounted for a third of CP hospitalizations within one year of AMI and was associated with similar disease-specific QoL as well general physical and mental health status impairment compared with cardiac CP hospitalization.
Keywords: chest pain, non-cardiac, angina, rehospitalization and health status outcomes
Prior studies have reported that 1 in 4 patients experience recurrent chest pain (CP) after acute myocardial infarction (AMI)1,2. Although these patients may experience angina secondary to incomplete revascularization or recurrent ischemic events, others present with non-cardiac CP syndromes that can be difficult for them to distinguish from angina or a recurrent acute coronary syndrome3,4. In fact, prior studies have indicated that 90% of patients diagnosed with non-cardiac CP in the general population continue to complain of chest pain at 2 years.5 This often leads to recurrent evaluations, which are associated with high resource utilization and cost3,6–8. Although substantial effort has been directed toward protocols to efficiently risk stratify patients presenting to the hospital with CP9,10, many of these patients are still hospitalized for further evaluation. Moreover, since the Centers for Medicare and Medicaid Services now reduce payments to hospitals with high readmission rates in the 30 days following AMI11, understanding the frequency and impact of non-cardiac CP hospitalizations post AMI has become increasingly important.
Currently, the frequency of non-cardiac CP after AMI and its association with health-related quality of life is unknown. To identify the incidence of hospitalization with non-cardiac CP in the first year after AMI, and to determine its association with patients’ health status, we analyzed data from the 24-center Translational Research Investigating Underlying Disparities in Acute Myocardial Infarction Patients’ Health Status (TRIUMPH) study. TRIUMPH collected detailed data about patient characteristics and health status, as well as physician-adjudicated hospitalization data. To contextualize these results, we also examined the health status outcomes associated with cardiac CP hospitalization, and compared the impact of non-cardiac and cardiac CP hospitalization on health status outcomes. Finding a high frequency of non-cardiac CP admissions, and a strong association with health status, would underscore the importance of further studying and developing treatment strategies and protocols for this condition.
METHODS
TRIUMPH Study
A total of 4340 patients were enrolled in the TRIUMPH study between April 11, 2005 and December 31, 2008. Patients were ≥18 years of age, with elevated cardiac biomarkers (troponin or creatine kinase-MB fraction assessed within 24 hours of admission), and supporting evidence of an AMI (electrocardiographic ST-segment changes or prolonged ischemic signs/symptoms). Each patient underwent a standardized interview by research staff to document sociodemographic and clinical data, as previously described. Patients were then contacted for follow-up interviews at 1, 6 and 12-months after AMI. All patients signed an informed consent after Institutional Review Board approval was obtained at each participating center. Funding support for the TRIUMPH Registry from the National Heart Lung and Blood Institute (P50 HL077113). The authors are solely responsible for the design and conduct of this study, all study analyses, the drafting and editing of the paper and its final contents.
A separate informed consent was obtained from TRIUMPH participants to collect their rehospitalization records for adjudication. During telephone interviews at 1, 6 and 12 months, patients were asked to report any admissions to any hospital. Any reported admissions led to retrieval of all hospital records over the year after AMI from the reported hospital. These documents were independently reviewed by at least two members of a physician adjudication panel to determine cause of hospitalization and document in-hospital processes of care. In the event that the initial two reviewers disagreed on the cause for hospitalization, a third reviewer independently reviewed the documents to ascertain the cause of hospitalization.
Study Population
Of the 4340 patients enrolled in TRIUMPH, 24 died before discharge from the index AMI hospitalization and 310 did not consent to release of medical records for the rehospitalization follow-up study. Among the remaining 4006 patients, 631 did not complete any follow-up interviews and 248 did not have physician-adjudicated hospitalization data, most often due to refusal of the admitting hospital to provide the medical records. We further excluded 28 patients who had only a hospitalization for staged percutaneous coronary intervention (PCI), yielding 3099 eligible patients participating in the follow-up rehospitalization study with complete follow-up data during the year after their AMI hospitalization.
Definitions and Adjudication Process
Each CP hospitalization was classified as non-cardiac or cardiac by the physician adjudication panel. Patients were classified as having a non-cardiac CP hospitalization if they were admitted with atypical or non-cardiac description of CP12,13 and the following conditions were absent: elevated cardiac biomarkers, evidence of myocardial ischemia on non-invasive stress tests, flow limiting epicardial coronary stenosis (>70%) or abnormal fractional flow reserve (<0.80). Specifically, patients with normal myocardial perfusion on stress myocardial perfusion imaging or normal wall motion on stress echocardiography who described atypical or non-cardiac chest pain were classified as having non-cardiac CP. The treating physician’s diagnosis of non-cardiac CP was also used to identify non-cardiac CP hospitalizations. Cardiac CP was categorized according to standard definitions of stable angina, unstable angina, NSTEMI and STEMI after reviewing hospital records. The adjudicators specifically focused upon in-hospital testing, including cardiac biomarkers, ECG findings, stress testing and angiographic findings of severe epicardial stenoses or fractional flow reserve <0.80, and the treating physician’s diagnoses. Specific cardiac chest pain definitions are listed in Supplementary Table 1. Any patient with no hospitalizations, cardiac hospitalizations unrelated to CP or with hospitalization for non-cardiac reasons in the first year after AMI was categorized as not having had a CP hospitalization. Any patient admitted for both cardiac and non-cardiac chest pain during follow-up was classified in the cardiac chest pain group.
Outcome Measures
The primary outcome was disease-specific health status, which was evaluated using the quality of life domain of the disease-specific Seattle Angina Questionnaire (SAQ QoL). The SAQ is a 19-item self-administered instrument, with a 4-week recall period, that quantifies coronary artery disease-specific health status14. The SAQ is a 19-item self-administered instrument, with a 4-week recall period, that quantifies coronary artery disease-specific health status14. At each follow-up telephone interview, the SAQ and the SF-12 were administered by trained study nurses to record patients self-reported health status. The SAQ has well-established validity, reliability and is more sensitive to clinical change than generic health status measures. SAQ scores are also independently associated with costs, morbidity and mortality among CAD patients15–17. Scores range from 0–100, where higher scores indicate better function, fewer symptoms and better quality of life. The SAQ asks patients to report CP, tightness or angina, but does not specifically distinguish between pain of an anginal character and other causes of CP. Accordingly, it is likely to effectively quantify the health status impact of CP regardless of its etiology.
As a secondary outcome, we also evaluated general health status using the generic Short Form 12 (SF-12)18. The SF-12 consists of 12 questions assessing two domains, the physical component (PCS) and the mental component (MCS) scores, which provide an assessment of patients’ overall physical and mental function. A score of 50 is normalized to the mean health status of the US population and each 10 points represents 1 standard deviation from that mean. The lower the score, the worse the patient perceives his or her generic health status, and lower scores have been shown to correlate with a greater likelihood for admissions due to cardiac causes and death19–21.
Statistical Analyses
We compared the baseline demographics, clinical characteristics and treatments of patients with non-cardiac CP hospitalization, cardiac CP hospitalization and those with no CP hospitalizations during the follow-up period. Continuous variables were reported as the mean ± standard deviation and differences were compared using one way analysis of variance. Categorical variables were compared using chi-square tests.
To understand the association between CP hospitalization and patients’ health status (comparing patients hospitalized with non-cardiac CP vs. no CP hospitalizations, and those with cardiac CP hospitalization vs. no CP hospitalizations; Figure 1), we then fit 3 hierarchical repeated measure linear models to assess the association between CP hospitalization and each of the three health status outcomes: the disease-specific SAQ QoL and the generic SF-12 PCS and MCS domains. This repeated measures approach included all follow-up health status assessments (1, 6 and 12 months). In order to compare the relative health status impact of non-cardiac versus cardiac CP, we also directly compared the difference in health status scores among patients hospitalized with cardiac vs. non-cardiac CP. All models adjusted for important potential confounders that were identified based upon either clinical judgment or a statistically significant difference between groups (p<0.05) in univariate analyses. Patients’ baseline health status scores were included in each analysis examining that same health status outcome, along with age, race, sex, smoking status, prior coronary artery bypass grafting (CABG), peripheral arterial disease, diabetes mellitus, insurance status (insurance vs. no insurance), Patient Health Questionnaire-9 depression scale score22,23, Perceived Stress Scale-4 score24, working status, marital status, in-hospital revascularization during index admission (percutaneous coronary intervention [PCI] vs. none, CABG vs. none), number of diseased vessels on coronary angiography during index hospitalization, ST-elevation MI (STEMI) vs. non ST-elevation MI (NSTEMI) and cardiac rehabilitation during follow-up. Finally, to contextualize the association of non-cardiac CP with health status outcomes, we used the same multivariable modeling to compare health status outcomes again between patients hospitalized with non-cardiac and cardiac CP.
Figure 1. Patient population.
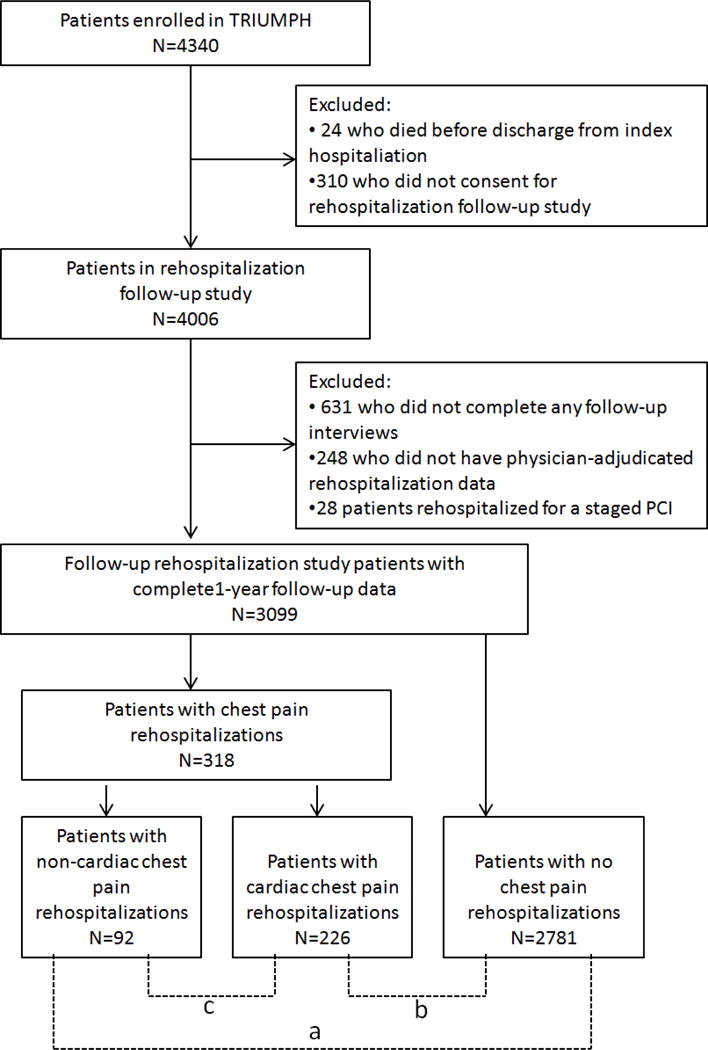
The proportions of patients with complete follow-up who experienced hospitalization for non-cardiac CP, cardiac CP or had no CP hospitalizations are presented. The dotted lines demonstrate the comparisons of patients with: a) non-cardiac CP vs. CP hospitalization, b) cardiac CP vs. no CP hospitalization, and c) non-cardiac CP vs. cardiac CP hospitalization.
* a, b and c are the comparisons made between different rehospitalizations
In addition, we performed a time-to-rehospitalization analysis using the Kaplan-Maier method to and present these curves to show the timing of rehospitalization events among the different groups across the follow-up period. Finally, to identify additional independent predictors of health status in follow-up after AMI, we examined the relationship between covariates in the multivariable linear regression models and each health status outcome.
Sensitivity Analyses
We also evaluated for potential bias related to missing follow-up data. A total of 1189 patients with missing follow-up data over the 1-year follow-up period, who were not included in our primary analysis, were included in a sensitivity analysis along with the 3099 patients who had complete follow-up data. We generated a propensity score for likelihood of having complete follow-up data, including all baseline demographic, clinical and treatment variables in a non-parsimonious logistic regression model. Multivariable modeling for health status outcomes and predictors of non-cardiac CP hospitalization were then repeated to determine whether missing follow-up data influenced our results after weighting using the inverse of the propensity score to participate in follow-up. Essentially, this analysis assigns greater weight to the outcomes of a patient who had complete follow-up who was statistically most similar to a patient without complete follow-up, and less weighting to the outcomes of a patient with propensity score consistent with high likelihood of follow-up.
To study the association between timing of rehospitalizations, type (cardiac, non-cardiac and none), and health status we conducted further sensitivity analyses in which the patients were identified who were hospitalized for evaluation of chest pain symptoms within 1 month after the 30-day and 6 month assessments. These patients were categorized according to the type of chest pain and were compared to patients who were not hospitalized with chest pain over the follow-up period. Scores on each health status measure across these groups are presented in Supplementary Table 2, but across measures, health status was significantly worse among patients who were hospitalized with non-cardiac and cardiac chest pain within a month after assessment, in comparison to patients who had no hospitalizations for chest pain.
RESULTS
Patient characteristics
The baseline characteristics of patients with non-cardiac CP, cardiac CP and no CP hospitalizations are presented in Table 1. Briefly, compared to patients with no CP hospitalization and with non-cardiac chest pain hospitalization, patients with cardiac CP hospitalization were more likely to be non-white, to have cardiac comorbidities (including diabetes, hypertension, prior MI, prior PCI and prior CABG), to be depressed and less likely to work full or part time. Moreover, no differences were found in access to care metrics at baseline or at 6 or 12 months post AMI.
Table 1.
Patient characteristics
| Non-cardiac CP hospitalization (n = 92) |
Cardiac CP hospitalization (n = 226) |
No CP hospitalization (n = 2781) |
P-Value | |
|---|---|---|---|---|
|
| ||||
| Age (years, mean ± SD) | 58.2 ± 11.7 | 58.7 ± 11.7 | 59.4 ± 12.0 | 0.447 |
|
| ||||
| Male | 55 (59.8%) | 128 (56.6%) | 1886 (67.8%) | < 0.001 |
|
| ||||
| White race | 61 (66.3%) | 142 (62.8%) | 1955 (70.5%) | 0.004 |
|
| ||||
| BMI (kg/m2, mean ± SD) | 29.1 ± 6.3 | 29.7 ± 7.0 | 29.6 ± 6.4 | 0.742 |
|
Socioeconomic Data | ||||
| College Education | 48 (52.2%) | 119 (53.1%) | 1366 (49.4%) | 0.497 |
|
| ||||
| Payor | 0.002 | |||
| Commercial/PPO | 36 (40.4%) | 80 (36.2%) | 1184 (43.3%) | |
| HMO | 3 (3.4%) | 20 (9.0%) | 304 (11.1%) | |
| Medicare | 25 (28.1%) | 40 (18.1%) | 495 (18.1%) | |
| Medicaid | 2 (2.2%) | 19 (8.6%) | 127 (4.6%) | |
| VA | 0 (0.0%) | 0 (0.0%) | 37 (1.4%) | |
| Other | 2 (2.2%) | 9 (4.1%) | 96 (3.5%) | |
| None/Self-Pay | 21 (23.6%) | 53 (24.0%) | 489 (17.9%) | |
|
| ||||
| Avoided Care Due to Costs in Past Year | 21 (22.8%) | 57 (25.9%) | 657 (24.0%) | 0.787 |
|
| ||||
| Financial Situation at the end of the month | < 0.001 | |||
| Some money left over | 38 (41.8%) | 75 (33.5%) | 1218 (44.5%) | |
| Just enough to make ends meet | 30 (33.0%) | 81 (36.2%) | 1004 (36.7%) | |
| Not enough to make ends meet | 23 (25.3%) | 68 (30.4%) | 514 (18.8%) | |
|
| ||||
| Baseline ENRICHD Social Support Score (points, mean ± SD) | 21.7 ± 4.8 | 21.3 ± 5.0 | 22.1 ± 4.3 | 0.015 |
|
| ||||
| Married or common law marriage | 39 (42.9%) | 95 (42.0%) | 1541 (55.5%) | < 0.001 |
|
| ||||
| Work full or part time | 49 (53.3%) | 84 (37.5%) | 1423 (51.7%) | < 0.001 |
|
Access to Care | ||||
| Difficultly obtaining an outpatient appointment (baseline) | 4 (15.4%) | 3 (30.0%) | 73 (23.0%) | 0.556 |
|
| ||||
| Difficultly obtaining care due to inability to find a physician (baseline) | 1 (3.8%) | 1 (10.0%) | 59 (18.6%) | 0.098 |
|
| ||||
| Currently Have a Doctor (6 months) | 161 (91.0%) | 67 (85.9%) | 1758 (88.3%) | 0.438 |
|
| ||||
| Currently Have a Doctor (12 months) | 149 (87.1%) | 67 (88.2%) | 1784 (87.8%) | 0.959 |
|
Past Medical History | ||||
| Diabetes | 27 (29.3%) | 92 (40.7%) | 783 (28.2%) | < 0.001 |
|
| ||||
| Hypertension | 63 (68.5%) | 173 (76.5%) | 1828 (65.7%) | 0.004 |
|
| ||||
| Prior MI | 20 (21.7%) | 67 (29.6%) | 534 (19.2%) | < 0.001 |
|
| ||||
| Prior PCI | 15 (16.3%) | 66 (29.2%) | 522 (18.8%) | < 0.001 |
|
| ||||
| Prior CABG | 14 (15.2%) | 52 (23.0%) | 275 (9.9%) | < 0.001 |
|
| ||||
| Dyslipidemia | 47 (51.1%) | 120 (53.1%) | 1363 (49.0%) | 0.471 |
|
| ||||
| Chronic Kidney Disease | 2 (2.2%) | 19 (8.4%) | 182 (6.5%) | 0.125 |
|
| ||||
| Current smoking | 28 (30.4%) | 95 (42.0%) | 1076 (39.0%) | 0.382 |
|
| ||||
| Chronic Heart Failure | 9 (9.8%) | 20 (8.8%) | 182 (6.5%) | 0.215 |
|
| ||||
| Peripheral Vascular Disease | 2 (2.2%) | 18 (8.0%) | 126 (4.5%) | 0.045 |
|
| ||||
| Prior stroke | 7 (7.6%) | 16 (7.1%) | 119 (4.3%) | 0.049 |
|
Health-Status Scores | ||||
| PHQ-9 Depression Score (points, mean ± SD) | 5.8 ± 5.4 | 6.5 ± 5.7 | 5.0 ± 5.3 | < 0.001 |
|
| ||||
| Perceived Stress Scale Score (points, mean ± SD) | 5.2 ± 3.8 | 5.4 ± 4.2 | 4.4 ± 3.7 | < 0.001 |
|
AMI Index Hospitalization Information | ||||
| STEMI | 47 (51.1%) | 89 (39.4%) | 1224 (44.0%) | 0.480 |
|
| ||||
| In-hospital Revascularization Procedure | 0.064 | |||
| None | 19 (20.7%) | 53 (23.5%) | 680 (24.5%) | |
| PCI | 68 (73.9%) | 159 (70.4%) | 1803 (64.8%) | |
| CABG | 5 (5.4%) | 14 (6.2%) | 298 (10.7%) | |
|
| ||||
| Killip Class on Arrival | 0.168 | |||
| I | 86 (94.5%) | 198 (89.2%) | 2455 (89.3%) | |
| II | 5 (5.5%) | 24 (10.8%) | 237 (8.6%) | |
| III | 0 (0.0%) | 0 (0.0%) | 41 (1.5%) | |
| IV | 0 (0.0%) | 0 (0.0%) | 17 (0.6%) | |
|
| ||||
| In-Hospital Cardiogenic Shock | 2 (2.2%) | 5 (2.2%) | 75 (2.7%) | 0.955 |
|
| ||||
| Diseased Vessels | 0.096 | |||
| 0 | 6 (6.8%) | 9 (4.4%) | 228 (8.7%) | |
| 1 | 43 (48.9%) | 77 (37.7%) | 1127 (43.2%) | |
| 2 | 20 (22.7%) | 64 (31.4%) | 668 (25.6%) | |
| 3 | 19 (21.6%) | 54 (26.5%) | 583 (22.4%) | |
|
| ||||
| LV Systolic Function | 0.650 | |||
| Normal | 60 (65.2%) | 140 (61.9%) | 1744 (62.8%) | |
| Mild | 19 (20.7%) | 38 (16.8%) | 549 (19.8%) | |
| Moderate | 7 (7.6%) | 31 (13.7%) | 288 (10.4%) | |
| Severe | 6 (6.5%) | 17 (7.5%) | 196 (7.1%) | |
|
Medications at Discharge from Index Hospitalization | ||||
| Beta Blockers | 81 (88.0%) | 196 (86.7%) | 2529 (90.9%) | 0.081 |
|
| ||||
| Statins | 75 (81.5%) | 203 (89.8%) | 2460 (88.5%) | 0.097 |
|
| ||||
| Aspirin | 89 (96.7%) | 212 (93.8%) | 2636 (94.8%) | 0.621 |
|
| ||||
| Thienopyridine | 72 (78.3%) | 189 (83.6%) | 2103 (75.6%) | 0.022 |
|
| ||||
| ACE Inhibitor/ARB | 68 (73.9%) | 184 (81.4%) | 2054 (73.9%) | 0.043 |
|
Rehospitalization Information | ||||
| In-Hospital Cardiac Catheterization | 5 (5.4%) | 97 (42.9%) | 9 (5.3%) | < 0.001 |
|
| ||||
| In-Hospital PCI | 0 (0.0%) | 71 (31.4%) | 12 (7.1%) | < 0.001 |
Abbreviations: SD: standard deviation, BMI: Body mass index, MI: myocardial infarction, PCI: percutaneous coronary intervention, CABG: coronary artery bypass graft, STEMI: ST-Elevation myocardial infarction, ACE: Angiotensin converting enzyme and ARB: Angiotensin receptor blocker
We report that cardiac catheterization was performed on 43% vs 5% vs 5% of patients with cardiac CP hospitalization, non-cardiac CP hospitalization and no chest pain hospitalizations, respectively. PCI during 1-year follow-up was performed on 31% of patients with cardiac CP hospitalization vs 7% in patients with no chest pain hospitalizations. None of the patients with non-cardiac CP hospitalization received PCI.
Frequency of non-cardiac chest pain hospitalization
In the year following an AMI admission, 318 of 3099 (10.3%) patients were hospitalized for evaluation and management of CP. Of these, 92 (28.9%) were admitted for non-cardiac CP and the remaining 226 patients were hospitalized with cardiac CP; 70 (31%) with recurrent AMI, 131 (58.0%) with unstable angina and 25 (11.0%) with stable angina. The timing of cardiac and non-cardiac chest pain hospitalizations over the follow-up period are presented in Figure 2 and Supplementary Figure 4.
Figure 2.
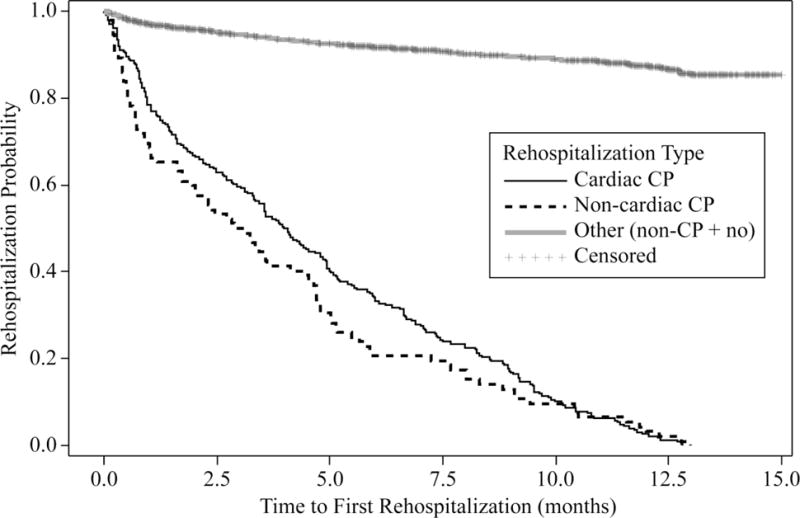
Kaplan-Meier curve showing time-to-rehospitalization among patients with with cardiac chest pain hospitalizatin, non-cardiac chest pain hospitalization or no chest pain hospitaliztions through 1 year of follow-up
Chest pain hospitalization and health status outcomes
Both non-cardiac CP and cardiac CP hospitalizations were associated with significantly worse disease-specific health status over the follow-up period as compared to patients without a CP hospitalization. After adjusting for patient characteristics, those hospitalized with non-cardiac CP had significantly lower SAQ QoL scores than those without a CP hospitalization (adjusted difference of −8.1 points, 95% CI −11.4, −4.8; Figure 3 and 4) similar to patients admitted with cardiac CP (adjusted difference of −9.5 points, 95% CI −11.7, −.73) as compared with those without a CP hospitalization. The SAQ QoL scores over the year after AMI was similar between those with non-cardiac and cardiac CP admissions (difference in adjusted scores of 0.6 points, 95% CI −3.2, 4.5).
Figure 3. Health status scores from baseline through 1 year of follow-up.
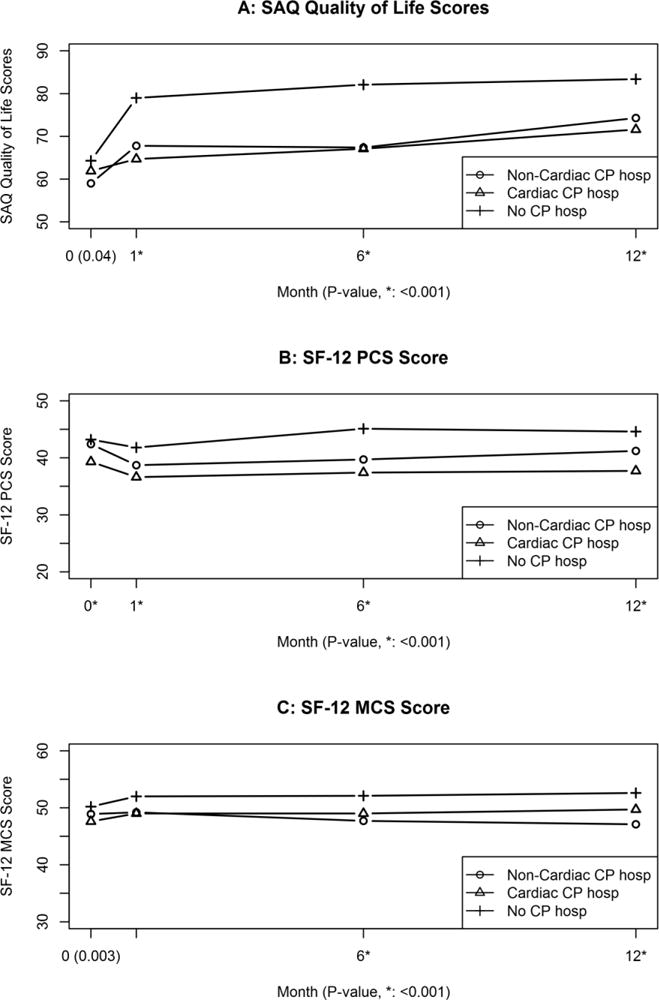
Panel A shows SAQ Quality of Life scores at baseline, 1, 6 and 12 months for patients with non-cardiac CP, cardiac CP and no CP. Panel B shows baseline, 1, 6 and 12 month scores on the SF-12 PCS scale, and Panel C shows baseline, 1, 6 and 12 month scores on the SF-12 MCS scale.
Figure 4.
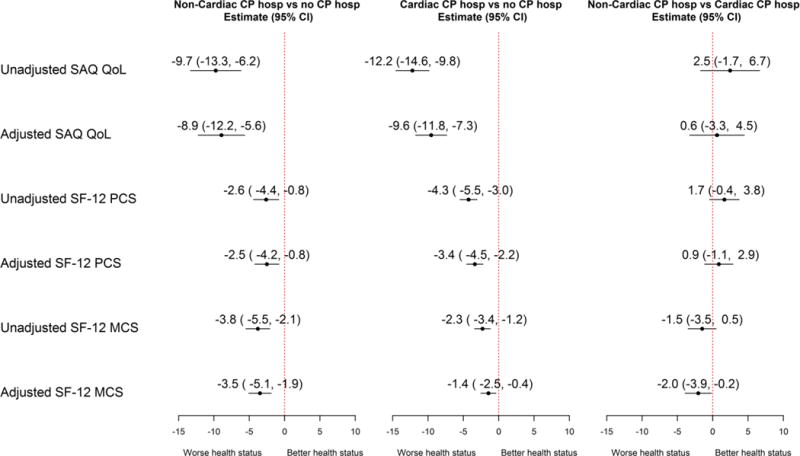
Association between cardiac or non-cardiac CP hospitalization and health status after acute myocardial infarction
Similarly, general health status was worse among patients hospitalized with non-cardiac CP than those who were not hospitalized with CP (Figure 3 and 4). Patients presenting with non-cardiac CP (adjusted difference in SF-12 PCS scores of −2.5 points, 95% CI −4.2, −0.8) or cardiac CP (adjusted difference in SF-12 PCS scores of −3.4 points, 95% CI −4.5, −2.2) reported poorer physical functioning than those without hospitalization for with CP. There were no significant differences in the adjusted SF-12 PCS scores when comparing patients with non-cardiac CP hospitalizations and those who had cardiac CP hospitalizations (difference of 0.9 points, 95% CI −1.1, 2.9).
Mental health scores, as assessed by the adjusted SF-12 MCS, were lower in patients hospitalized with non-cardiac CP in comparison as compared with those who were not hospitalized with CP (difference −3.5 points, 95% CI −5.1, −1.9). Patients hospitalized with cardiac CP also had lower SF-12 MCS scores compared with to patients who had no CP hospitalizations (−1.4 points, 95% CI −2.5, −0.4). In contrast to the other health status measures, patients with non-cardiac CP hospitalization had worse mental health status over the follow-up period than patients hospitalized with cardiac CP (SF-12 MCS adjusted difference −2.0 points, 95% CI −3.9, −0.2).
We repeated the multivariable modeling process, using the same model structure and covariates, for each SAQ subscale and the SAQ Overall Summary Score (Supplementary Figure 1). These results were consistent with findings on the SAQ QoL scale indicating worse health status among patients with either cardiac or non-cardiac chest pain.
Other clinical characteristics independently associated with health status in recovery after AMI are presented in Supplementary Figures 2a, 2b and 2c. Older age, current work employment, being married and in-hospital revascularization during the index hospitalization were associated with better quality of life. However, smoking, presenting with STEMI, female gender, depression and stress, having no insurance and history of CABG prior to the index AMI were all associated with worse quality of life.
Sensitivity analyses
After adjusting our analyses for the inverse of the propensity to have complete follow-up data, we found no significant differences in our results, suggesting that there was little bias due to missing follow-up data.
Adjudication process
Initially, two physicians adjudicated each chart and in case of disagreement the chart was sent to a third physician for review (blinded to initial two reviews). In case of continued disagreement among the three reviewers, more reviewers (blinded to initial reviews) were invited to help with the adjudication. We report that the agreement between the initial two reviewers was high for all the three groups studied (75% vs 71% vs 85% for cardiac CP vs non-cardiac CP vs no CP hospitalizations, respectively). In cardiac CP hospitalization group, 21% needed a third reviewer and only 4% needed a fourth reviewer. In the non-cardiac CP hospitalization group, 23%, 3% and 2% needed a third, fourth and fifth reviewer, respectively.
Mortality
Mortality in the first two years after AMI was numerically lower in those with non-cardiac CP hospitalization (although with low event rates) but not significantly different compared to those with cardiac CP hospitalization and those without chest pain hospitalizations (2 [2.2%] vs. 18 [8.0%] vs. 188 [6.8%], respectively, p=0.17). Moreover, the 2-year mortality rates were also not significantly different between non-cardiac CP and cardiac CP groups (p value of 0.07).
Predictors of non-cardiac chest pain hospitalization
We identified several independent predictors of both non-cardiac CP and cardiac CP hospitalization. Compared with patients without a hospitalization for CP, patients with a greater burden of angina at the time of their index AMI, women and diabetics were more likely to be admitted with cardiac CP, but these patient factors were not associated with admission for non-cardiac CP (Supplementary Figure 3). Current smokers were less likely to present with non-cardiac CP, while there was no difference in the likelihood of hospitalization with cardiac CP in follow-up between smokers and non-smokers. Married patients were less frequently admitted to the hospital for evaluation of chest pain regardless of etiology, while those with prior CABG (before their index AMI) were more likely to be hospitalized with both cardiac CP and non-cardiac CP. Individuals treated with PCI during the index hospitalization were more likely to be hospitalized with cardiac CP than those who did not undergo revascularization.
DISCUSSION
In an era of increasing attention on post-AMI rehospitalization25, understanding the frequency and types of CP hospitalization following AMI and the clinical significance of these CP hospitalizations is increasingly important. To our knowledge, there are no prior studies of the incidence and clinical implications of non-cardiac CP hospitalizations following AMI. We leveraged a multicenter AMI registry with carefully adjudicated data on all rehospitalizations in the first year after AMI to address this gap in knowledge. We found that hospitalization for CP within the first year after AMI occurred in 10% of patients, and that 1 in 3 patients hospitalized with CP presented with a non-cardiac etiology for their symptoms. Non-cardiac CP hospitalization was associated with poorer disease-specific and general health status throughout the first year of recovery as compared with those not admitted with recurrent CP and was associated with similar decrements in health status as compared with patients admitted for cardiac CP. In fact, although non-cardiac CP hospitalization was associated with slightly worse impairment of mental functioning than cardiac CP hospitalization, the difference was clinically modest and unlikely to be clinically significant.
Our study extends prior reports regarding the association of non-cardiac CP with patients’ perceived quality of life. Prior studies have examined patients without known coronary artery disease, often identified in the Emergency Department or in outpatient clinics. These reports have suggested that patients with non-cardiac CP may have poor health status26, and have similar or even greater levels of anxiety compared with those who have cardiac chest pain27–29. Importantly, it has been shown that many patients with non-cardiac CP are not reassured after being informed their chest pain is not of cardiac origin, often remaining anxious and seeking further medical evaluation8. Our report examines the relationship between non-cardiac CP and health status in a much higher risk population with recent AMI. Our data suggest a strong association between non-cardiac CP admissions and poorer health status in these patients with established CAD, indicating a clear need to better identify and treat the underlying causes of non-cardiac CP.
Non-cardiac CP has been shown to commonly occur with several conditions such as gastrointestinal, musculoskeletal and psychiatric disorders30. Gastrointestinal diagnoses such as reflux disease, esophageal spasm, and cholelithiasis have been found to be important causes of symptoms in patients presenting with non-cardiac CP3,4,31. In a small study of patients with coronary artery disease who had continued atypical CP despite medical therapy or revascularization, it was found that nearly two thirds had gastroesophageal reflux disease, and the majority of these patients experienced significant symptom relief with treatment4. Similarly, musculoskeletal CP is also a common, treatable cause of symptoms in a many patients with non-cardiac CP31–34. Moreover, psychiatric conditions are prevalent among patients with non-cardiac CP and include panic, anxiety, and depressive disorders35. Prior studies have shown that cognitive behavioral therapy is an effective treatment option for patients presenting with non-cardiac CP36,37. To date, however, no systematic strategies to pro-actively evaluate these potential etiologies of non-cardiac CP have been developed or tested. Given that as many as a third of CP admissions are not cardiac in etiology, systematically seeking to identify and intervene in high-risk patients might be a cost-effective intervention that may also improve patients’ health status recovery after an AMI. The use of prediction models on discharge to identify patients with high likelihood of rehospitalizations should be encouraged. Future studies should focus on developing protocols that aim to identify patients with non-cardiac chest pain that can be managed effectively in the outpatient setting to prevent extensive emergency room evaluations and admission to the hospital.
Several limitations of the present study should be considered in the interpretation of these data. First, we were not able to adjudicate the causes of patients’ non-cardiac CP and angina secondary to small vessel disease or microvascular disease cannot be excluded in the non-cardiac CP group. However, our definition of non-cardiac CP was consistent with prior studies and represents some of the first insights into the frequency and clinical importance of these symptoms in patients with established coronary artery disease. Future studies are needed to determine the frequency of various non-cardiac CP syndromes, such as panic disorder, musculoskeletal pain, and gastroesophageal reflux disease, among others. Second, not all TRIUMPH patients participated in the follow-up rehospitalization study, and patients were also excluded who were not able to complete the follow-up process. Since these patients may differ from those who participated throughout the entire follow-up period, selection bias cannot be excluded. However, our results weighted for the inverse of the propensity to have complete follow-up suggested no significant bias was introduced into our analyses by missing data. The TRIUMPH rehospitalization sub-study did not collect detailed information for emergency department encounters that did not lead to inpatient admission. Accordingly, we were unable to examine variability in hospitalization rates among all-comers with chest pain symptoms, and were unable to examine either the association between outpatient emergency department evaluations and health status or the predictors of inpatient vs. outpatient evaluation.” Moreover, follow-up health status assessments in TRIUMPH were conducted at 1-, 6- and 12-months after enrollment. Accordingly, for many hospitalizations there was no health status assessment in the month preceding hospital admission. Although our sensitivity analyses suggest an even stronger relationship between non-cardiac chest pain hospitalization and health status in the month before hospitalization, greater granularity as to the exact temporal relationships between chest pain syndromes and health status cannot be obtained from this study and future efforts to collect patients’ health status at more frequent interviews will be needed. TRIUMPH enrolled patients between 2005 and 2008 and thus the use of high sensitivity troponins and other advanced imaging modalities to risk stratify patients with chest pain might not reflect current practice. Finally, although we adjusted for potential confounders in the relationship between CP and health status outcomes, unmeasured and residual confounding cannot be excluded in this observational study.
CONCLUSIONS
We found that non-cardiac CP accounts for 1 in 3 CP hospitalizations in follow-up after AMI and is associated with impaired quality of life over the year after an AMI. Although the magnitude of the association of non-cardiac CP and cardiac CP with disease-specific quality of life and general physical functioning is similar, non-cardiac CP was associated with a slightly greater impairment in patients’ mental health which was clinically modest and unlikely to be clinically significant. In light of the significant health status impairment associated with non-cardiac CP, better describing the causes, prevention and treatment of non-cardiac CP is an important area for future research.
Supplementary Material
Acknowledgments
Funding: Funding support was received for the TRIUMPH Registry from the National Heart Lung and Blood Institute (P50 HL077113). Dr. Qintar is supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health under Award Number T32HL110837. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Dr. Chan is supported by a grant from the NHLBI (1R01HL123980).
Abbreviations
- CP
Chest pain
- SAQ
Seattle Angina Questionnaire
- SF-12 PCS
Short Form 12 physical component summary scores
- SF-12 MCS
Short Form 12 mental component summary scores
- TRIUMPH Study
Translational Research Investigating Underlying Disparities in Acute Myocardial Infarction Patients’ Health Status Study
Footnotes
Disclosures: Dr. Spertus owns the copyright for the Seattle Angina Questionnaire. All other authors have no disclosures.
Author Contributions:
Mohammed Qintar, MD: analysis of data, interpretation of data, drafting and revisions of manuscript.
Yuanyuan Tang, PhD: Statistical analyses, revisions of manuscript.
Donna M. Buchanan, PhD: interpretation of data, drafting and revisions of manuscript.
Paul S. Chan, MD, MSc: interpretation of data, drafting and revisions of manuscript.
Amit P. Amin, MD, MSc: interpretation of data, review and revisions of manuscript.
John A. Spertus, MD MPH: conception and design of study, funding of study, coordination of study, interpretation of data, drafting and revisions of manuscript.
Adam C. Salisbury, MD, MSc: conception and design of study, analysis of data, interpretation of data, drafting and revisions of manuscript.
References
- 1.Spertus JA, Dawson J, Masoudi FA, Krumholz HM, Reid KJ, Peterson ED, Rumsfeld JS, Cardiovascular Outcomes Research C Prevalence and predictors of angina pectoris one month after myocardial infarction. Am J Cardiol. 2006;98:282–288. doi: 10.1016/j.amjcard.2006.01.099. [DOI] [PubMed] [Google Scholar]
- 2.Longmore RB, Spertus JA, Alexander KP, Gosch K, Reid KJ, Masoudi FA, Krumholz HM, Rich MW. Angina frequency after myocardial infarction and quality of life in older versus younger adults: the Prospective Registry Evaluating Myocardial Infarction: Event and Recovery study. American heart journal. 2011;161:631–638. doi: 10.1016/j.ahj.2010.12.005. [DOI] [PubMed] [Google Scholar]
- 3.Leise MD, Locke GR, 3rd, Dierkhising RA, Zinsmeister AR, Reeder GS, Talley NJ. Patients dismissed from the hospital with a diagnosis of noncardiac chest pain: cardiac outcomes and health care utilization. Mayo Clin Proc. 2010;85:323–330. doi: 10.4065/mcp.2009.0428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singh S, Richter JE, Hewson EG, Sinclair JW, Hackshaw BT. The contribution of gastroesophageal reflux to chest pain in patients with coronary artery disease. Annals of internal medicine. 1992;117:824–830. doi: 10.7326/0003-4819-117-10-824. [DOI] [PubMed] [Google Scholar]
- 5.Eslick GD, Talley NJ. Natural history and predictors of outcome for non-cardiac chest pain: a prospective 4-year cohort study. Neurogastroenterology and motility: the official journal of the European Gastrointestinal Motility Society. 2008;20:989–997. doi: 10.1111/j.1365-2982.2008.01133.x. [DOI] [PubMed] [Google Scholar]
- 6.Prina LD, Decker WW, Weaver AL, High WA, Smars PA, Locke GR, 3rd, Reeder GS. Outcome of patients with a final diagnosis of chest pain of undetermined origin admitted under the suspicion of acute coronary syndrome: a report from the Rochester Epidemiology Project. Annals of emergency medicine. 2004;43:59–67. doi: 10.1016/s0196-0644(03)00601-2. [DOI] [PubMed] [Google Scholar]
- 7.Eslick GD, Jones MP, Talley NJ. Non-cardiac chest pain: prevalence, risk factors, impact and consulting–a population-based study. Alimentary pharmacology & therapeutics. 2003;17:1115–1124. doi: 10.1046/j.1365-2036.2003.01557.x. [DOI] [PubMed] [Google Scholar]
- 8.Hadlandsmyth K, Rosenbaum DL, Craft JM, Gervino EV, White KS. Health care utilisation in patients with non-cardiac chest pain: a longitudinal analysis of chest pain, anxiety and interoceptive fear. Psychology & health. 2013;28:849–861. doi: 10.1080/08870446.2012.762100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hoffmann U, Truong QA, Schoenfeld DA, Chou ET, Woodard PK, Nagurney JT, Pope JH, Hauser TH, White CS, Weiner SG, Kalanjian S, Mullins ME, Mikati I, Peacock WF, Zakroysky P, Hayden D, Goehler A, Lee H, Gazelle GS, Wiviott SD, Fleg JL, Udelson JE, Investigators R-I Coronary CT angiography versus standard evaluation in acute chest pain. N Engl J Med. 2012;367:299–308. doi: 10.1056/NEJMoa1201161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cullen MW, Reeder GS, Farkouh ME, Kopecky SL, Smars PA, Behrenbeck TR, Allison TG. Outcomes in patients with chest pain evaluated in a chest pain unit: the chest pain evaluation in the emergency room study cohort. American heart journal. 2011;161:871–877. doi: 10.1016/j.ahj.2011.02.008. [DOI] [PubMed] [Google Scholar]
- 11.Senate US. HR 3590: The Patient Protection and Affordable Care Act. 2009 [Google Scholar]
- 12.Diamond GA, Forrester JS. Analysis of probability as an aid in the clinical diagnosis of coronary-artery disease. N Engl J Med. 1979;300:1350–1358. doi: 10.1056/NEJM197906143002402. [DOI] [PubMed] [Google Scholar]
- 13.Diamond GA. A clinically relevant classification of chest discomfort. Journal of the American College of Cardiology. 1983;1:574–575. doi: 10.1016/s0735-1097(83)80093-x. [DOI] [PubMed] [Google Scholar]
- 14.Spertus JA, Winder JA, Dewhurst TA, Deyo RA, Fihn SD. Monitoring the quality of life in patients with coronary artery disease. The American journal of cardiology. 1994;74:1240–1244. doi: 10.1016/0002-9149(94)90555-x. [DOI] [PubMed] [Google Scholar]
- 15.Spertus JA, Jones P, McDonell M, Fan V, Fihn SD. Health status predicts long-term outcome in outpatients with coronary disease. Circulation. 2002;106:43–49. doi: 10.1161/01.cir.0000020688.24874.90. [DOI] [PubMed] [Google Scholar]
- 16.Mozaffarian D, Bryson CL, Spertus JA, McDonell MB, Fihn SD. Anginal symptoms consistently predict total mortality among outpatients with coronary artery disease. American heart journal. 2003;146:1015–1022. doi: 10.1016/S0002-8703(03)00436-8. [DOI] [PubMed] [Google Scholar]
- 17.Arnold SV, Morrow DA, Lei Y, Cohen DJ, Mahoney EM, Braunwald E, Chan PS. Economic impact of angina after an acute coronary syndrome: insights from the MERLIN-TIMI 36 trial. Circulation Cardiovascular quality and outcomes. 2009;2:344–353. doi: 10.1161/CIRCOUTCOMES.108.829523. [DOI] [PubMed] [Google Scholar]
- 18.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Medical care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Piotrowicz K, Noyes K, Lyness JM, McNitt S, Andrews ML, Dick A, Hall WJ, Moss AJ, Zareba W. Physical functioning and mental well-being in association with health outcome in patients enrolled in the Multicenter Automatic Defibrillator Implantation Trial II. European heart journal. 2007;28:601–607. doi: 10.1093/eurheartj/ehl485. [DOI] [PubMed] [Google Scholar]
- 20.Rumsfeld JS, MaWhinney S, McCarthy M, Jr, Shroyer AL, VillaNueva CB, O’Brien M, Moritz TE, Henderson WG, Grover FL, Sethi GK, Hammermeister KE. Health-related quality of life as a predictor of mortality following coronary artery bypass graft surgery. Participants of the Department of Veterans Affairs Cooperative Study Group on Processes, Structures, and Outcomes of Care in Cardiac Surgery. JAMA: the journal of the American Medical Association. 1999;281:1298–1303. doi: 10.1001/jama.281.14.1298. [DOI] [PubMed] [Google Scholar]
- 21.Dorr DA, Jones SS, Burns L, Donnelly SM, Brunker CP, Wilcox A, Clayton PD. Use of health-related, quality-of-life metrics to predict mortality and hospitalizations in community-dwelling seniors. Journal of the American Geriatrics Society. 2006;54:667–673. doi: 10.1111/j.1532-5415.2006.00681.x. [DOI] [PubMed] [Google Scholar]
- 22.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. Journal of general internal medicine. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gilbody S, Richards D, Brealey S, Hewitt C. Screening for depression in medical settings with the Patient Health Questionnaire (PHQ): a diagnostic meta-analysis. Journal of general internal medicine. 2007;22:1596–1602. doi: 10.1007/s11606-007-0333-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of health and social behavior. 1983;24:385–396. [PubMed] [Google Scholar]
- 25.Krumholz HM, Lin Z, Drye EE, Desai MM, Han LF, Rapp MT, Mattera JA, Normand SL. An administrative claims measure suitable for profiling hospital performance based on 30-day all-cause readmission rates among patients with acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2011;4:243–252. doi: 10.1161/CIRCOUTCOMES.110.957498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Eslick GD. Health care seeking behaviors, psychological factors, and quality of life of noncardiac chest pain. Disease-a-month: DM. 2008;54:604–612. doi: 10.1016/j.disamonth.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 27.Webster R, Norman P, Goodacre S, Thompson A. The prevalence and correlates of psychological outcomes in patients with acute non-cardiac chest pain: a systematic review. Emergency medicine journal: EMJ. 2012;29:267–273. doi: 10.1136/emermed-2011-200526. [DOI] [PubMed] [Google Scholar]
- 28.Eken C, Oktay C, Bacanli A, Gulen B, Koparan C, Ugras SS, Cete Y. Anxiety and depressive disorders in patients presenting with chest pain to the emergency department: a comparison between cardiac and non-cardiac origin. The Journal of emergency medicine. 2010;39:144–150. doi: 10.1016/j.jemermed.2007.11.087. [DOI] [PubMed] [Google Scholar]
- 29.Robertson N, Javed N, Samani NJ, Khunti K. Psychological morbidity and illness appraisals of patients with cardiac and non-cardiac chest pain attending a rapid access chest pain clinic: a longitudinal cohort study. Heart. 2008;94:e12. doi: 10.1136/hrt.2006.100537. [DOI] [PubMed] [Google Scholar]
- 30.Husser D, Bollmann A, Kuhne C, Molling J, Klein HU. Evaluation of noncardiac chest pain: diagnostic approach, coping strategies and quality of life. European journal of pain. 2006;10:51–55. doi: 10.1016/j.ejpain.2005.01.011. [DOI] [PubMed] [Google Scholar]
- 31.Eslick GD, Coulshed DS, Talley NJ. Review article: the burden of illness of non-cardiac chest pain. Alimentary pharmacology & therapeutics. 2002;16:1217–1223. doi: 10.1046/j.1365-2036.2002.01296.x. [DOI] [PubMed] [Google Scholar]
- 32.Fruergaard P, Launbjerg J, Hesse B, Jorgensen F, Petri A, Eiken P, Aggestrup S, Elsborg L, Mellemgaard K. The diagnoses of patients admitted with acute chest pain but without myocardial infarction. European heart journal. 1996;17:1028–1034. doi: 10.1093/oxfordjournals.eurheartj.a014998. [DOI] [PubMed] [Google Scholar]
- 33.Rouan GW, Hedges JR, Toltzis R, Goldstein-Wayne B, Brand D, Goldman L. A chest pain clinic to improve the follow-up of patients released from an urban university teaching hospital emergency department. Annals of emergency medicine. 1987;16:1145–1150. doi: 10.1016/s0196-0644(87)80474-2. [DOI] [PubMed] [Google Scholar]
- 34.Wise CM, Semble EL, Dalton CB. Musculoskeletal chest wall syndromes in patients with noncardiac chest pain: a study of 100 patients. Archives of physical medicine and rehabilitation. 1992;73:147–149. [PubMed] [Google Scholar]
- 35.White KS, Raffa SD, Jakle KR, Stoddard JA, Barlow DH, Brown TA, Covino NA, Ullman E, Gervino EV. Morbidity of DSM-IV Axis I disorders in patients with noncardiac chest pain: Psychiatric morbidity linked with increased pain and health care utilization. Journal of consulting and clinical psychology. 2008;76:422–430. doi: 10.1037/0022-006X.76.3.422. [DOI] [PubMed] [Google Scholar]
- 36.Spinhoven P, Van der Does AJ, Van Dijk E, Van Rood YR. Heart-focused anxiety as a mediating variable in the treatment of noncardiac chest pain by cognitive-behavioral therapy and paroxetine. Journal of psychosomatic research. 2010;69:227–235. doi: 10.1016/j.jpsychores.2010.02.005. [DOI] [PubMed] [Google Scholar]
- 37.van Beek MH, Oude Voshaar RC, Beek AM, van Zijderveld GA, Visser S, Speckens AE, Batelaan N, van Balkom AJ. A brief cognitive-behavioral intervention for treating depression and panic disorder in patients with noncardiac chest pain: a 24-week randomized controlled trial. Depression and anxiety. 2013;30:670–678. doi: 10.1002/da.22106. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


