Abstract
Objectives
Evidence-based guidelines recommend that HIV care providers offer retention-in-care services, but data are needed to assess service provision.
Methods
We surveyed a probability sample of 1234 HIV care providers to estimate the percentage of providers whose practices offered 5 recommended retention services and describe providers’ perceptions of barriers to care among patients.
Results
An estimated 21% of providers’ practices offered all 5 retention services. Providers at smaller (<50 versus >400 patients), private, and non-Ryan White HIV/AIDS Program (RWHAP)-funded practices, and practices without on-site case management were significantly less likely to provide patient navigation services or do systematic monitoring of retention. Providers’ most commonly perceived barriers to care among patients were mental health (40%), substance abuse (36%), and transportation (34%) issues.
Conclusion
Deficiencies in the provision of key retention services are substantial. New strategies may be needed to increase the delivery of recommended retention services, especially among private, non-RWHAP-funded, and smaller facilities.
Keywords: HIV, delivery of health care, retention in care, HIV care providers, Medical Monitoring Project
Introduction
The US National HIV/AIDS Strategy (NHAS) updated to 2020 emphasizes the importance of monitoring and improving outcomes at all stages of the HIV care continuum, including the percentage of persons living with HIV who are diagnosed, engaged in care, on treatment, and virally suppressed.1 According to national and local care continuum estimates, most persons living with HIV who are not virally suppressed have been diagnosed with HIV but are not engaged (linked and retained) in HIV care.2–5 Recently released guidelines and recommendations from HIV physician groups and federal agencies on HIV prevention and care in clinical settings endorse evidence-based strategies to retain patients in HIV care.6–10 Recommended retention strategies include providing colocated care and ancillary services, identifying and addressing individuals’ barriers to care, providing patient or peer navigation services, and using HIV surveillance data and clinical data to identify and locate persons out of care.8 Several recent systematic literature reviews support using multiple strategies in combination to retain and reengage persons in HIV care.11–13
The extent to which HIV care providers’ practices are following recommendations to enhance patient engagement and retention in care is unknown. In 2013, the Medical Monitoring Project (MMP) constructed a national probability sample of HIV care providers working in a variety of clinical care settings across the United States and Puerto Rico. Using these data, we estimated the percentage of HIV care providers in the United States who offer recommended retention-in-care services in their practice and described providers’ perceptions about reasons why patients miss scheduled follow-up visits.
Methods
We analyzed data collected from the MMP 2013–2014 Provider Survey, which was conducted in the geographic areas and HIV care facilities sampled for MMP in 2012.14,15 The Provider Survey used a complex 2-stage sample design, in which the US states and territories were sampled, followed by facilities providing HIV care in those jurisdictions. All 17 sampled jurisdictions (16 states and Puerto Rico) agreed to participate in MMP. Of 622 sampled facilities, 505 (81%) agreed to participate in the survey by providing contact information for all HIV care providers (defined as providers who order CD4 count or HIV viral load tests and/or prescribe antiretroviral medications). Providers (physicians, physician assistants, and nurse practitioners) were eligible to participate if they had completed professional training and had provided HIV care between January and April 2012. The final sample consisted of 2208 HIV care providers from 391 of 622 sampled facilities (63% overall facility cooperation rate), all of whom were invited to participate in the survey. Of 2208 providers sampled, 2023 (92%) were determined to be eligible and 1234 of the eligible providers returned surveys (American Association for Public Opinion Research, Response Rate 3,16 adjusted provider response rate, 64%). The data were weighted based on the probability of selection, and nonresponse adjustments were made to sampling weights based on provider and practice factors associated with nonresponse, for example, provider profession, number of HIV care providers in the practice, and whether or not the provider worked at a private practice.
Providers were recruited with a modified version of Dillman’s Tailored Design Method,17 which involved mailing individualized recruitment packets to all of the providers in participating practices. The recruitment packets included a letter from the Centers for Disease Control and Prevention (CDC) explaining the purpose of the survey, instructions for completing the self-administered survey via paper or a Web-based response system, and a $20 cash incentive. The recruitment materials explained the voluntary nature of the survey, and written informed consent was not obtained. As a public health surveillance activity, the MMP Provider Survey was determined to be nonresearch in accordance with federal human subjects’ protections in the Code of Federal Regulations and CDC guidelines for defining public health research and nonresearch.18,19 Nonresponders were sent 3 additional mailings at set intervals over the following 7 weeks. Survey distribution and follow-up was conducted in waves comprising 8 individual cycles at 1 week intervals spanning 17 weeks between June 2013 and January 2014.
The provider survey instrument consisted of 61 questions covering 7 general content areas (provider demographics, professional characteristics, practice characteristics, general characteristics of their HIV patients, patient management practices, sources of information used for current guidelines and continuing education, and provision of antiretroviral prophylaxis for HIV-negative patients) and required approximately 30 minutes to complete. For this analysis, we focused on providers’ reports about retention services (appointment reminders, patient navigation services, follow-up on missed visits, reinforcement of the importance of follow-up visits, and systematic monitoring of retention in care) offered to patients within their practices (Figure 1). We investigated bivariate associations between all 5 retention services being offered within one’s practice and practice characteristics ascertained from facility data collected from clinic administrators for MMP. Practice characteristics evaluated included receipt of Ryan White HIV/AIDS Program (RWHAP) funding (yes or no), practice type (private or nonprivate), geographic location of practice (urban or nonurban), practice size (based on estimated HIV patient caseload), and provision of on-site case management services (yes or no). We also examined associations between the 2 retention services offered least often, systematic monitoring of retention in care and patient navigation services, with these practice characteristics.
Figure 1.
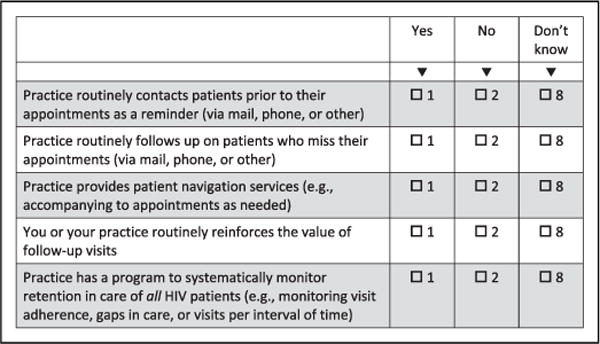
Questions about retention services provided to patients within provider’s practice, Medical Monitoring Project 2013–2014 Provider Survey. Do you agree with the following statements about services provided to patients at your practice?
We investigated providers’ perceptions of their patients’ barriers to care, measured as each provider’s assessment of how frequently (never, rarely, sometimes, often, or very often) their patients miss scheduled visits due to the following reasons: child care problems, drug or alcohol abuse, emotional or psychological barriers related to HIV (eg, stigma, denial), homelessness, incarceration or legal detention, mental health problems, reluctance to admit not following provider’s advice, too sick to travel to clinic, and transportation problems. Reasons for missed follow-up visits were considered endorsed if the provider responded that patients “often” or “very often” missed visits due to that particular reason.
We computed weighted estimates of percentages and corresponding 95% confidence intervals describing the population of HIV providers, whether their practice provided each of the 5 retention services, and their perceptions about why patients miss follow-up visits. Rao-Scott chi-square tests were performed to test bivariate associations between practice characteristics and offering all 5 retention services and offering the individual services of patient navigation and systematic monitoring of retention in care. All estimates incorporated the survey weights, and variance estimates were computed using Taylor Series Linearization to reflect the complex features of the MMP provider sample. We used SAS/STAT (version 9.4; SAS Institute Inc) procedures for the analysis of complex sample survey data and considered estimates with a coefficient of variation >0.3 unreliable.
Results
Descriptive Statistics for Provider Population
Table 1 provides weighted estimates describing the population of HIV providers and characteristics of practices in which they work. Nearly 59% of providers were at least 50 years old, 57% were male, and 63% were white. Most HIV providers were physicians, board certified in infectious diseases (45%) or another specialty (30%), 15% were nurse practitioners, 5% physician’s assistants, and 5% nonboard-certified physicians. Nearly 58% were HIV specialists, and 83% provided primary care. Among all HIV providers, 48% worked at RWHAP-funded practices and 42% worked in private practices (which may or may not have received Ryan White funds). Nearly 69% of providers worked at practices located in large metropolitan areas. With respect to the size of the practice, 29% worked in small practices (<50 patients), 45% worked in medium-sized practices (50–400 patients), and 25% worked in large practices (>400 patients). Nearly 51% of providers worked in practices offering on-site case management.
Table 1.
Estimated Provider and Practice Characteristics of HIV Adult Medical Care Providers in the United States—Medical Monitoring Project 2013–2014 Provider Survey.a,b
| Demographics | n | wt % | 95% CI |
|---|---|---|---|
| Age, years | |||
| <40 | 211 | 17.5 | 12.9–22.2 |
| 40–49 | 326 | 24.0 | 21.2–26.8 |
| 50–59 | 453 | 38.4 | 32.3–44.6 |
| 60+ | 204 | 20.1 | 14.8–25.3 |
| Gender | |||
| Male | 620 | 56.5 | 49.6–63.5 |
| Female | 585 | 43.5 | 36.5–50.4 |
| Race/ethnicity | |||
| Black/African American | 89 | 10.8 | 3.8–17.7 |
| Hispanic/Latinoc | 158 | 10.7 | 3.5–17.8 |
| Otherd | 179 | 15.6 | 10.7–20.6 |
| White | 783 | 62.9 | 55.8–70.0 |
| Qualifications and experience | |||
| Certification type | |||
| Non-board-certified physiciane | 61 | 4.8 | 2.2–7.4 |
| ID board-certified physiciane | 564 | 44.5 | 37.3–51.7 |
| Other board-certified physiciane | 319 | 30.0 | 22.8–37.3 |
| Nurse practitioner | 217 | 15.2 | 10.3–20.1 |
| Physician assistant | 63 | 5.4 | 2.6–8.2 |
| HIV specialistf | 865 | 57.8 | 51.2–64.4 |
| Provides primary careg | 1094 | 83.1 | 78.4–87.8 |
| Practice characteristics | |||
| Practice receives Ryan White HIV/AIDS Program funding | 784 | 47.5 | 35.4–59.6 |
| Private practice | 300 | 41.9 | 33.3–50.6 |
| Practice located in a large metropolitan areah | 1001 | 68.7 | 60.3–77.1 |
| Size of practice, number of HIV patients served | |||
| Small: <50 patients | 124 | 29.4 | 21.7–37.0 |
| Medium: 50–400 patients | 376 | 45.2 | 37.1–53.3 |
| Large: >400 patients | 734 | 25.4 | 20.4–30.5 |
| Practice uses an electronic medical record | 759 | 62.2 | 48.9–75.5 |
| Practice uses an integrated team approach to HIV carei | 874 | 54.0 | 45.6–62.6 |
| Practice provides on-site case management | 850 | 50.8 | 41.5–60.1 |
Abbreviations: CI, confidence interval; wt, weighted.
N = 1234.
Numbers=may not add to total and percentage may not total 100% because of missing data. Values exclude “don’t know” responses
Hispanic or Latinos can be of any race. Providers are classified in only 1 race/ethnicity category.
Includes American Indian/Alaska Native, Asian, Native Hawaiian/Other Pacific Islander, and multiple races.
Doctor of Medicine (MD) or Doctor of Osteopathic Medicine (DO).
American Academy of HIV Medicine (AAHIVM) specialist certification (AAHIVS) detailed at http://www.aahivm.org/aahivs.
Point of first contact, comprehensive care, emphasis on prevention and coordination of care.
Based on urban influence codes.
Multiple clinicians work together to augment the provider visit by providing previsit, postvisit, or between-visit contact with HIV-infected patients. Team members may include nurses, social workers, case managers, mental health providers, substance abuse counselors, and/or adherence counselors.
Retention-in-Care Services
The majority of providers worked in practices that reinforced the importance of follow-up visits (96%), used appointment reminders (89%), and followed up on missed visits (82%; Table 2). However, only 53% of providers worked in practices that conducted systematic monitoring of retention in care, and only 33% worked in practices that provided patient navigation services. An estimated 21% of providers worked in practices that provided all 5 retention services, 55% worked in practices that provided at least 4 retention services, and 84% worked in practices that provided at least 3 retention services (Figure 2).
Table 2.
Percentage of HIV Care Providers Whose Practice Offers Retention-in-Care Services—Medical Monitoring Project 2013–2014 Provider Survey.a
| Type of Retention Service | n | wt. % | 95% CI |
|---|---|---|---|
| Reinforcing importance of follow-up visits | 1192 | 95.9 | 93.5–98.4 |
| Appointment reminders | 1071 | 88.6 | 85.5–91.7 |
| Missed visit follow-up | 961 | 82.1 | 78.2–86.1 |
| Systematic monitoring of retention in care | 767 | 53.4 | 43.8–63.1 |
| Patient navigation services | 486 | 33.1 | 26.5–39.6 |
Abbreviations: CI, confidence interval; wt, weighted.
N = 1234.
Figure 2.
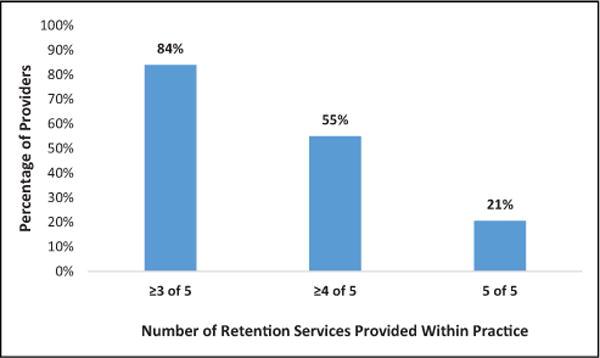
Percentage of HIV care providers whose practice offers at least 3 of 5, at least 4 of 5, and all 5 retention services, a Medical Monitoring Project 2013–2014 Provider Survey (N =1234). a Retention services included appointment reminders, missed visit follow-up, patient navigation services, reinforcing importance of follow-up visits, and systematic monitoring of retention in care.
Providers who worked in RWHAP-funded practices were considerably more likely than those in non-RWHAP-funded practices to report that their practice offered all 5 retention services (34% versus 9%), systematically monitored retention in care (77% versus 31%), and offered patient navigation services (45% versus 23%; Table 3). Providers who worked in nonprivate practices (versus private), large practices (versus medium or small), and practices that provided (versus did not provide) on-site case management were also more likely to report that their practice offered all 5 retention services, systematically monitored retention in care, and provided patient navigation services. Urban versus nonurban facility location was not associated with provision of retention services.
Table 3.
Percentage of HIV Care Providers Whose Practice Offers All 5 Retention Practices, Patient Navigation Services, and Systematic Monitoring of Retention in Care Stratified by Practice Characteristics—Medical Monitoring Project 2013–2014 Provider Survey.a
| All 5 Retention Services
|
Systematic Monitoring of Retention in Care
|
Patient Navigation Services
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| n | wt % | (95% CI) | n | wt % | (95% CI) | n | wt % | (95% CI) | |
| Practice characteristics | |||||||||
| Practice receives Ryan White HIV/AIDS Program fundingb | |||||||||
| Yes (n =784) | 239 | 33.6 | 26.2–41.0 | 575 | 77.0 | 69.1–84.9 | 364 | 44.7 | 37.3–52.2 |
| No (n = 343) | 36 | 8.6 | 4.2–12.9 | 131 | 31.0 | 22.3–39.6 | 77 | 23.3 | 13.3–33.3 |
| Private practiceb | |||||||||
| Yes (n =300) | 38 | 8.2 | 4.3–12.1 | 130 | 31.2 | 23.5–39.0 | 72 | 23.5 | 13.4–33.6 |
| No (n = 934) | 270 | 29.6 | 22.8–36.4 | 637 | 69.5 | 60.8–78.2 | 414 | 39.9 | 33.8–46.0 |
| Practice located in a large metro areac,d | |||||||||
| Yes (n =1001) | 231 | 20.2 | 14.5–25.8 | 612 | 55.0 | 47.6–62.5 | 389 | 35.1 | 28.6–41.7 |
| No (n =233) | 77 | 21.6 | 11.4–31.8 | 155 | 50.0 | 27.7–72.2 | 97 | 28.5 | 16.3–40.7 |
| Size of practice, number of HIV patients servedb | |||||||||
| Small: <50 patients (n =124) | 18 | 10.6 | 4.4–16.7 | 53 | 35.0 | 18.5–51.4 | 29 | 18.8 | 9.9–27.6 |
| Medium: 50–400 patients (n = 376) | 98 | 23.2 | 14.2–32.2 | 232 | 58.5 | 45.6–71.4 | 128 | 35.2 | 24.2–46.3 |
| Large: >400 patients (n = 734) | 192 | 27.6 | 22.4–32.8 | 482 | 65.8 | 60.8–70.9 | 329 | 45.6 | 41.0–50.3 |
| Practice provides on-site case managementb | |||||||||
| Yes (n =850) | 252 | 30.3 | 22.6–38.1 | 606 | 70.7 | 58.9–82.4 | 384 | 40.7 | 32.6–48.7 |
| No (n = 384) | 56 | 10.6 | 6.2–14.9 | 161 | 35.7 | 27.6–43.8 | 102 | 25.2 | 15.7–34.6 |
Abbreviations: CI, confidence interval; wt, weighted.
N = 1234.
Significant Rao-Scott chi-square test result for all 3 outcomes at P ≤ .01.
Nonsignificant Rao-Scott chi-square test result for all 3 outcomes at P ≤ .05.
Practice location based on urban influence codes.
Providers’ Perceived Reasons Why Patients Miss Scheduled Follow-up Visits
Mental health problems were reported by 41% of providers as often or very often being a reason for missed follow-up visits, followed by drug or alcohol abuse (36%), transportation problems (34%), and emotional or psychological barriers associated with HIV (30%; Table 4).
Table 4.
Percentage of HIV Care Providers Who Reported that Patients Often or Very Often Miss Scheduled Follow-up Visits Due to Specified Reasons—Medical Monitoring Project 2013–2014 Provider Survey.a
| n | wt. % | (95% CI) | |
|---|---|---|---|
| Mental health problems | 618 | 40.5 | 35.8–45.2 |
| Drug or alcohol abuse problems | 567 | 36.1 | 30.3–41.9 |
| Transportation problems | 511 | 33.9 | 28.3–39.5 |
| Emotional/psychological barriers related to HIV (e.g., stigma, denial, fear, or anger) | 467 | 30.1 | 24.8–35.3 |
| Reluctance to admit not following provider’s advice | 210 | 18.6 | 11.9–25.3 |
| Homelessness | 165 | 10.6 | 7.8–13.4 |
| Childcare problems | 138 | 8.4 | 5.7–11.1 |
| Incarceration or legal detention | 86 | 5.7 | 3.5–7.9 |
| Too sick to travel to clinic | 64 | 4.9 | 2.9–7.0 |
Abbreviations: CI, confidence interval; wt., weighted.
N =1234.
Discussion
To our knowledge, these are the first national estimates on the provision of HIV retention-in-care services in clinical settings, and our findings suggest suboptimal delivery of recommended retention services in the United States. Only 1 in 5 HIV providers reported working in a practice that provided all 5 retention services, all of which are services recommended in recent HIV care guidelines.7–9 While a large majority reported working in practices that offered individual retention services such as appointment reminders and missed visit follow-up, just over half reported providing systematic monitoring of retention in care and only 1 in 3 reported providing patient navigation services. HIV providers at private, non-RWHAP-funded, and smaller facilities were even less likely to report that their facility provided all 5 retention services. Increasing provision of retention services within HIV care practices is needed to support the 2020 NHAS goal of increasing to 90% the percentage of persons with diagnosed HIV infection who are retained in HIV medical care.1
Optimizing HIV care continuum outcomes requires that providers proactively identify and address barriers to care engagement in addition to offering recommended retention services.7 We found that providers endorsed reasons for missed patient visits (ie, mental health, substance abuse, transportation, and emotional or psychological barriers related to HIV) that are similar to those reported by patients as reasons for poor engagement in care.20,21 Reasons for missed visits such as mental health, substance abuse, or stigma are complex and multidimensional in nature and are not easily addressed directly by HIV care providers during follow-up care visits. Nonetheless, HIV providers have an integral role in screening for and identifying patients at risk of missed visits and linking patients to support services.
Previous data have shown that RWHAP-funded facilities were more likely than non-RWHAP-funded facilities to provide case management, mental health, and substance abuse treatment services, and patients attending RWHAP-funded facilities were more likely to report receiving these services than patients attending non-RWHAP-funded facilities.22 Colocating support services in settings providing routine HIV medical care is the cornerstone of the medical home model endorsed by RWHAP.23 Expansion of the RWHAP medical home model might increase patient access to support services and foster enhanced engagement in care. In HIV practices where a medical home model cannot be implemented, administrators may consider colocating support staff (such as peer or patient navigators) who can refer or link patients to off-site support services. Similarly, HIV practices without colocated support services may consider strengthening linkages to RWHAP-funded service providers within existing referral networks to ensure that case management or patient navigation are provided to patients needing these services.
Guidelines from provider organizations and federal agencies emphasize the importance of implementing existing evidence-informed retention strategies in HIV practices as well as developing and disseminating new strategies to retain patients in HIV care.7,8 Organizations may consider leveraging existing resources, partnerships, and funded initiatives to increase implementation of evidence-informed retention interventions in HIV care practices. Several federally funded programs are focused on identifying and promoting innovative methods and strategies to retain and reengage persons in HIV medical care. Centers for Disease Control and Prevention recently funded demonstration projects to implement and evaluate innovative approaches to improve linkage to and reengagement in HIV care among persons living with HIV.24 Similarly, the Health Resources and Services Administration (HRSA) funds RWHAP Part C grantees through its Early Intervention Services and Capacity Development Grants programs to implement activities that establish or enhance infrastructure for improving the delivery of comprehensive HIV primary care services, including linkage or retention-in-care activities.25 Last, current HRSA Special Projects of National Significance initiatives are focused on identifying and disseminating evidence-informed interventions to improve outcomes along the HIV care continuum.26
Our analysis is subject to a few limitations. First, estimates of delivery of retention services are self-reported and may be subject to measurement error due to poor recall or social desirability. Provision of certain retention services may be performed by nonclinical staff, and thus providers may not have been aware of these services. However, provider awareness of services is important to measure, as it may reflect how often these services are promoted to patients. Next, estimates of retention services reflect the proportion of providers working in practices that offer each retention service, not the proportion of practices offering each service nor the overall proportion of HIV patients with access to these services. The proportion of patients with access to retention services may be higher than our provider-based estimates suggest, given that HIV care practices with larger patient volumes are more likely to provide these services. Nonetheless, our analyses provide valuable insight about HIV providers’ perceptions and characteristics of HIV practices where service delivery can be enhanced.
Conclusion
HIV provider organizations and federal agencies emphasize the importance of offering comprehensive retention services in HIV clinical care. However, implementation of systematic monitoring of retention in care and patient navigation services in providers’ practices is suboptimal, particularly among providers at private, non-RWHAP-funded, and smaller HIV care facilities. HIV care providers indicated that mental health concerns, substance abuse, lack of transportation, and psychological barriers related to HIV (eg, stigma or denial) were primary reasons why patients missed appointments. Development and dissemination of new tools and strategies, such as more formalized measurement of provision of retention services using quality-of-care indicators, may help increase delivery of recommended retention services.
Acknowledgments
We thank participating MMP providers, facilities, and project areas and staff from Altarum Institute. We also acknowledge the contributions of the Clinical Outcomes Team and the Behavioral and Clinical Surveillance Branch at CDC and the MMP Project Area Group Members (http://www.cdc.gov/hiv/statistics/systems/mmp/resources.html).
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Funding for the Medical Monitoring Project is provided by the Centers for Disease Control and Prevention.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention (CDC).
Portions of the analysis were presented at the 11th International Conference on HIV Treatment and Prevention Adherence in Hollywood, Florida, USA, May 2016.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.White House Office of National AIDS Policy. National HIV/AIDS strategy for the United States: updated to 2020. 2015 https://www.aids.gov/federal-resources/national-hiv-aids-strategy/nhas-update.pdf. Accessed July 27, 2017.
- 2.Centers for Disease Control and Prevention. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas—2013. HIV Surveill Suppl Rep. 2015;20(2):70. [Google Scholar]
- 3.Bradley H, Hall HI, Wolitski RJ, et al. Vital signs: HIV diagnosis, care, and treatment among persons living with HIV–United States, 2011. Mmwr Morb Mortal Wkly Rep. 2014;63(47):1113–1117. [PMC free article] [PubMed] [Google Scholar]
- 4.Wiewel EW, Braunstein SL, Xia Q, Shepard CW, Torian LV. Monitoring outcomes for newly diagnosed and prevalent HIV cases using a care continuum created with New York city surveillance data. J Acquir Immune Defic Syndr. 2015;68(2):217–226. doi: 10.1097/QAI.0000000000000424. [DOI] [PubMed] [Google Scholar]
- 5.Kay ES, Batey DS, Mugavero MJ. The HIV treatment cascade and care continuum: updates, goals, and recommendations for the future. Aids Res Ther. 2016;13:35. doi: 10.1186/s12981-016-0120-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aberg JA, Gallant JE, Ghanem KG, et al. Primary care guidelines for the management of persons infected with HIV: 2013 update by the HIV Medicine Association of the Infectious Diseases Society of America. Clin Infect Dis. 2014;58(1):1–10. doi: 10.1093/cid/cit757. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention, Health Resources and Services Administration, National Institutes of Health et al. Recommendations for HIV Prevention with Adults and Adolescents with HIV in the United States, 2014. 2014 http://stacks.cdc.gov/view/cdc/26062. Accessed March 21, 2016.
- 8.International Advisory Panel on HIV Care Continuum Optimization. IAPAC guidelines for optimizing the HIV care continuum for adults and adolescents. J Int Assoc Provid Aids Care. 2015;14(suppl 1):S3–S34. doi: 10.1177/2325957415613442. [DOI] [PubMed] [Google Scholar]
- 9.Marrazzo JM, del Rio C, Holtgrave DR, et al. HIV prevention in clinical care settings: 2014 recommendations of the International Antiviral Society-USA Panel. JAMA. 2014;312(4):390–409. doi: 10.1001/jama.2014.7999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.The Foundation for AIDS Research. Curbing the HIV epidemic by supporting effective engagement in HIV care. 2016 http://www.amfar.org/uploadedFiles/_amfarorg/Articles/On_The_Hill/2016/DC-2016-Engagement-Policy-Report_081916-October.pdf. Accessed July 27, 2017.
- 11.Liau A, Crepaz N, Lyles CM, et al. Interventions to promote linkage to and utilization of HIV medical care among HIV-diagnosed persons: a qualitative systematic review, 1996–2011. AIDS Behav. 2013;17(6):1941–1962. doi: 10.1007/s10461-013-0435-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thompson MA, Mugavero MJ, Amico KR, et al. Guidelines for improving entry into and retention in care and antiretroviral adherence for persons with HIV: evidence-based recommendations from an International Association of Physicians in AIDS Care panel. Ann Intern Med. 2012;156(11):817–833. W284–W294. doi: 10.7326/0003-4819-156-11-201206050-00419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Higa DH, Crepaz N, Mullins MM. Identifying best practices for increasing linkage to, retention, and re-engagement in HIV medical care: findings from a systematic review, 1996–2014. AIDS Behav. 2016;20(5):951–966. doi: 10.1007/s10461-015-1204-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention. Behavioral and clinical characteristics of persons receiving medical care for HIV infection—Medical Monitoring Project, United States, 2011. HIV Surveillance Special Report. 2015;10 http://www.cdc.gov/hiv/library/reports/surveillance/#special. Accessed July 27, 2017. [Google Scholar]
- 15.Iachan R, Johnson CH, Harding RL, et al. Design and weighting methods for a nationally representative sample of HIV-infected adults receiving medical care in the United States-Medical Monitoring Project. Open AIDS J. 2016;10:164–181. doi: 10.2174/1874613601610010164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.The American Association for Public Opinion Research. Standard definitions: final dispositions of case codes and outcome rates for surveys. 8th. AAPOR; https://www.aapor.org/AAPOR_Main/media/publications/Standard-Definitions2015_8theditionwithchanges_April2015_logo.pdf. Published 2015. Accessed July 27, 2017. [Google Scholar]
- 17.Dillman D, Smyth J, Christian L. Internet, Phone, Mail, and Mixed-mode Surveys. Hoboken, NJ: John Wiley & Sons, Inc; 2014. [Google Scholar]
- 18.Protection of Human Subjects, US Federal Code Title 45 Part 46. http://www.hhs.gov/ohrp/humansubjects/guidance/45cfr46.html. Effective July 14, 2009. Last revised January 15, 2010. Accessed December 9, 2016. [PubMed]
- 19.Centers for Disease Control and Prevention. Distinguishing Public Health Research and Public Health Nonresearch. 2010 http://www.cdc.gov/od/science/integrity/docs/cdc-policy-distinguishing-public-health-research-nonresearch.pdf. Accessed July 27, 2017.
- 20.Beer L, Valverde EE, Raiford JL, Weiser J, White BL, Skarbinski J. Clinician perspectives on delaying initiation of antiretroviral therapy for clinically eligible HIV-infected patients. J Int Assoc Provid AIDS Care. 2015;14(3):245–254. doi: 10.1177/2325957414557267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tobias CR, Cunningham W, Cabral HD, et al. Living with HIV but without medical care: barriers to engagement. AIDS Patient Care Stds. 2007;21(6):426–434. doi: 10.1089/apc.2006.0138. [DOI] [PubMed] [Google Scholar]
- 22.Weiser J, Beer L, Frazier EL, et al. Service delivery and patient outcomes in Ryan White HIV/AIDS Program-funded and -non-funded health care facilities in the United States. JAMA Intern Med. 2015;175(10):1650–1659. doi: 10.1001/jamainternmed.2015.4095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Beane SN, Culyba RJ, DeMayo M, Armstrong W. Exploring the medical home in Ryan White HIV care settings: a pilot study. J Assoc Nurses AIDS Care. 2014;25(3):191–202. doi: 10.1016/j.jana.2013.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention. Organizations funded under CDC’s new awards for 12-1201. http://www.cdc.gov/hiv/funding/announcements/ps12-1201/categoryc.html. Accessed July 27, 2017.
- 25.Health Resources and Services Administration. Part C: Early Intervention Services and Capacity Development Program grants. http://hab.hrsa.gov/abouthab/partc.html. Accessed July 27, 2017.
- 26.Health Resources and Services Administration. Part F: Special Projects of National Significance (SPNS) program. http://hab.hrsa.gov/abouthab/partfspns.html. Accessed July 27, 2017.


