Abstract
Introduction
This case highlights the complexity of upper limb revascularization after a subclavian artery traumatic injury and strengthens the role of a hybrid/multi-disciplinary approach to such injuries.
Report
A 45-year-old male patient presented with an acute right upper limb following a traumatic injury to the right subclavian artery due to a motor vehicle accident (MVA). Associated injuries included an unstable cervical spine injury, a large open right clavicular injury, and a brain injury, which limited the potential revascularisation options available. The arm was revascularised using a hybrid endovascular/open surgical approach, namely embolization of the proximal subclavian artery (just distal to vertebral artery) and a right common femoral artery to distal axillary artery bypass using prosthetic material.
Discussion
Blunt injuries to the subclavian artery are often high impact, complex and associated with multiple injuries to surrounding structures, which limit the role of standard procedures used in the elective setting. This case highlights the role of multidisciplinary team involvement, using a hybrid approach and a novel distal inflow site to restore upper limb perfusion.
Keywords: Upper limb, Ischemia, Trauma, Revascularization
Highlights
-
•
Major vascular trauma often requires a multidisciplinary team approach.
-
•
Prompt decision is required even if it involves unusual methods of treatment.
-
•
A combined hybrid endovascular/open surgical treatment should be considered.
Introduction
Traumatic vascular injuries of the subclavian and proximal axillary arteries are potentially devastating, yet they account for a minority of vascular injuries presenting to trauma centres.1 The skeletal protection afforded to the subclavian artery means that any injury to the artery is usually high impact and associated with significant damage to surrounding structures, which often complicates repair.2 We report a case of a complex proximal right subclavian artery traumatic injury associated with a number of other injuries that posed a number of issues with regard to limb revascularisation.
Report
A 45-year-old male patient was admitted following a motor vehicle accident (motorcycle vs. lamp-post). He had a pulseless electrical activity (PEA) arrest on the scene secondary to tension pneumothorax, which was decompressed, and cardiopulmonary resuscitation (CPR) carried out for 10 minutes with return to spontaneous ventilation. The patient was intubated at the scene and bilateral thoracostomies were performed prior to transfer, which resulted in the return of spontaneous ventilation. On arrival to the trauma centre, the patient was haemodynamically stable and had a large open wound overlying the proximal extent of the right clavicle. The right hand was cold with an associated pulseless right upper limb. The patient underwent a trauma series computerised tomography (CT) scan.
The CT findings included a right proximal subclavian artery disruption with no distal filling, a mediastinal haematoma, and traumatic subarachnoid haemorrhage with basal ganglia contusion, a C6 fracture with associated fractures of the scapula, sternum and the right clavicle. There were also significant open right tibia and fibula fractures and a small liver laceration.
The unstable nature of the C6 fracture allied to the open wound precluded a carotid subclavian bypass procedure and it was felt that a total endovascular solution (insertion of a covered stent) would not be successful due to the length of the occlusion seen on CT. As such, a combined endovascular and open surgical procedure to revascularise the right arm was performed (embolization of the right subclavian artery origin and right femoral to distal axillary artery bypass).
Under general anaesthesia and with a cervical collar in situ, a longitudinal right groin incision was made and the common femoral artery exposed. Due to the site of the open wound, the axillary artery was approached laterally. An incision was made within the deltopectoral grove, allowing identification of the coracoid process. A coracoid osteotomy was performed by the orthopaedic surgeon, the coracoid was pre drilled and detached as if to do a Latarjet procedure.3
On this occasion it was not necessary to release pectoralis minor. Inferior reflection of the coracoid tip and its muscular attachments provided free access to the second part of the axillary artery.
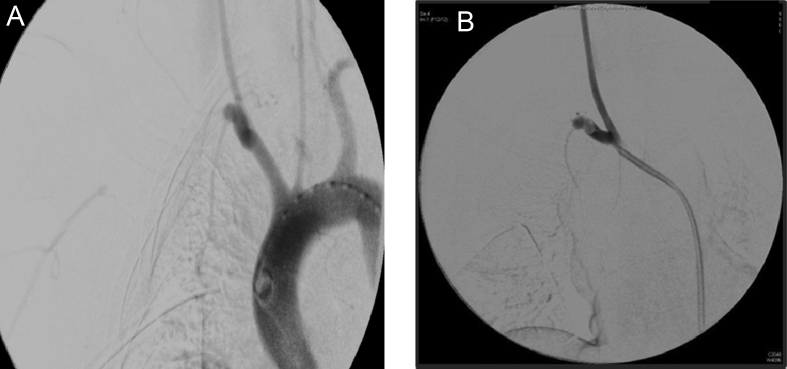
The right common femoral artery was punctured and a 6F sheath inserted. A catheter was positioned within the aortic arch and an angiogram confirmed the disruption of the origin of the subclavian artery (Fig. 1A). The brachiocephalic trunk was cannulated and an Amplatzer™ vascular plug type 1 (16 mm; St Jude Medical, ST. Paul, MN, USA) placed (Fig. 1B). A subcutaneous tunnel was then fashioned along the right side of the abdominal wall and thorax (lateral from the site of chest drain insertion) and an 8-mm ringed ePTFE graft (Maquet) was passed through the tunnel. An end to side anastomosis was performed sequentially at both the common femoral artery and the axillary artery under cover of 2000 IU of heparin. The distal aspect of the subclavian artery proximal to the axillary anastomosis was ligated. The coracoid process was then reattached to the scapula and soft tissue coverage achieved over the proximal anastomosis. Collatamp G (Tribute Pharmaceuticals), a gentamicin impregnated haemostatic agent, was placed within both wounds and the skin closed. A full fasciotomy of all compartments of the right arm was performed. The patient was then transferred to the neurological critical care unit with a warm hand and palpable radial pulse.
Figure 1.
(A) Pre-occlusion of the subclavian artery with an Amplatzer™plug. (B) Post-occlusion of the subclavian artery with an Amplatzer™plug.
The patient had a convoluted prolonged recovery period post-operatively. The patient had a 9-week stay within the tertiary trauma centre. During this period, his stay was complicated with a herpes simplex virus 1 (HSV1) pneumonia, with an associated slow respiratory wean requiring tracheostomy, and readmission to critical care unit with lung collapse. The patient suffered a traumatic rhabdomyolysis responding to conventional treatment. Neurological improvement was slow, with a right upper limb paresis due to a diffuse brachial plexus injury (confirmed by subsequent MRI), partial Horner's and right third cranial nerve palsy. Rehabilitation was commenced with regards to speech and language therapy, with speaking valve trials, and physiotherapy. The patient was transferred to a local district hospital, after 65 days, for continued rehabilitation requirements.
Discussion
Upper extremity injuries comprise 30% of total vascular injuries (although subclavian artery injuries are uncommon due to their localization) and have the potential to cause major functional impairment, limb loss or death. The close proximity of complex anatomical structures allied to the protective bony skeleton makes access and subsequent control and repair one of the most challenging situations facing a vascular/trauma surgeon.
Given the initial clinical findings of this patient at presentation it was felt that the arterial supply to the arm was insufficient and given that the patient was intubated a thorough neurological examination was unable to be performed. However, it is recognised that significant injury to the brachial plexus is an indication of poor limb related outcomes4 and indeed in this case, the patient was ultimately found, once extubated, to have a significant plexus injury with associated arm paralysis and complex pain. Eventually, in these types of cases upper limb amputation rates ultimately approach 30%.
The optimal repair for any arterial injury is either primary repair or an anatomical autogenous vein bypass with perceived better patency rates and the associated reduced risks of infection. The multitude of injuries usually associated with subclavian artery injuries often precludes such an approach. More recently, there has been a trend towards endovascular strategies to deal with trauma as a whole, notably embolization techniques but also the use of covered stents. Indeed, endovascular repair of injured axillosubclavian arteries has been described in penetrating and blunt trauma using covered stents often requiring a through and through wire to achieve this.5 However, complete vessel transection is technically more challenging from an endovascular perspective, mainly due to difficulty with crossing the complete transection and its associated haematoma.
There were a number of challenging factors with this case that prevented such revascularization options. Firstly, the presumed unstable cervical spine fracture and the subsequent need for immobilisation (hard collar) prevented movement of the neck making appropriate carotid artery exposure virtually impossible, thus precluding a carotid-axillary bypass. Furthermore, the open wound over the right clavicle was extensive and not only limiting tunnelling options but would significantly increase the risk of graft infection. Owing to the multiple injuries suffered by the patient, the mediastinal blood and the distinct possibility of turning a relatively stable haemodynamic situation into an unstable one, a sternotomy with inline bypass from the origin of the proximal subclavian artery was felt to be extremely high risk in this acute stage. Similar concerns, specifically with regard to haemodynamic stability also precluded a total endovascular solution using a covered stent. A femoral to axillary bypass procedure was thus considered as a strategy given that, if required, a more definitive procedure could be performed in a more elective setting. Indeed, this was the initial plan but the subsequent realisation of the extent of the brachial plexus injury and the associated flaccid, painful arm meant that a more definitive procedure was not undertaken. Surveillance of the graft was not performed for similar reasons. Although extra-anatomical bypasses are felt to have poorer long term patency, this is often in the context of atherosclerotic disease and anecdotally in those patients with good arterial “run off” (e.g. in the management of infected aortic grafts), such grafts tend to have much better longer term patency rates with reported patency rates reaching almost 90% in the mid to long term.6
Secondly, the ability to access the axillary artery at the level of the coracoid process allowed us to circumvent the open wound and limit exposure of the graft to a possible infected area. This was facilitated by an orthopaedic surgeon with an interest in the upper limb and highlights the need for a multidisciplinary input when dealing with such complex cases. In this case the multidisciplinary team consisted of a vascular surgeon, an upper limb orthopaedic surgeon, a plastic surgeon, an interventional radiologist alongside anaesthetic and intensive care colleagues which lends weight to the role of major trauma centres within the UK.
Thirdly, the subclavian artery injury was 2–3 cm distal to its origin, which allowed placement of the Amplatzer™ vascular plug type 1 (16 mm; St Jude Medical) without encroaching onto the origin of the right common carotid artery. Although we gave a small amount of heparin intraoperatively (after discussion with our neurosurgical team), in the immediate post-operative period no anticoagulation was given and a single antiplatelet agent was introduced once the intracranial bleeding risk had been reduced. The ischemic time was not taken in consideration as its effect on muscle function was masked by the concomitant brachial plexus injury (Table 1).
Table 1.
Potential revascularisation strategy.
| Potential revascularisation strategy | Reason not undertaken |
|---|---|
| Sternotomy and primary subclavian repair/bypass | Concerns with sternotomy precipitating significant bleeding with decompression of the haematoma surrounding the subclavian artery injury |
| Right carotid subclavian bypass | Presumed unstable cervical spine fracture which prevented movement of the neck to optimise carotid exposure The bypass graft would pass through a potentially infected area in keeping with the large open wound overlying the clavicle |
| Axillary–axillary bypass | Concerns with tunnelling a synthetic graft through the centre of the large open wound overlying the right clavicle |
Conclusion
Upper limb vascular trauma is diverse; the key for a good outcome is the prompt decision and the collaboration of various teams to deliver the fastest and the most appropriate way of treatment, even if this involves an unorthodox method of treatment. Extra-anatomical bypass allied with a hybrid endovascular approach to dealing with such injuries is a feasible treatment strategy.
Conflict of Interest
None.
Funding
None.
References
- 1.Franga D.L., Hawkins M.L., Mondy J.S. Management of subclavian and axillary artery injuries: spanning the range of current therapy. Am Surg. 2005;71(4):303–307. [PubMed] [Google Scholar]
- 2.Siegel J.H., Smith J.A., Siddiqi S.Q. Change in velocity and energy dissipation on impact in motor vehicle crashes as a function of the direction of crash: key factors in the production of thoracic aortic injuries, their pattern of associated injuries and patient survival. A Crash Injury Research Engineering Network (CIREN) study. J Trauma. 2004;57(4):760–777. doi: 10.1097/01.ta.0000147502.50248.c4. discussion 777–8. [DOI] [PubMed] [Google Scholar]
- 3.Walch G., Boileau P. Latarjet-Bristow procedure for recurrent anterior instability. Tech Shoulder Elbow Surg. 2000;1:256–261. [Google Scholar]
- 4.RA1 Fitridge, Raptis S., Miller J.H., Faris I. Upper extremity arterial injuries: experience at the Royal Adelaide Hospital, 1969 to 1991. J Vasc Surg. 1994;20(6):941–946. doi: 10.1016/0741-5214(94)90231-3. [DOI] [PubMed] [Google Scholar]
- 5.Rohlffs F., Larena-Avl A.A., Petersen J.P., Debus E.S., Kölbel T. Through-and-through wire technique for endovascular damage control in traumatic proximal axillary artery transection. Vascular. 2015;23(1):99–101. doi: 10.1177/1708538114531259. [DOI] [PubMed] [Google Scholar]
- 6.Sharp W.J., Hoballah J.J., Mohan C.R., Kresowik T.F., Martinasevic M., Chalmers R.T. The management of the infected aortic prosthesis: a current decade of experience. J Vasc Surg. 1994;19(5):844–850. doi: 10.1016/s0741-5214(94)70009-5. [DOI] [PubMed] [Google Scholar]