Abstract
Introduction
Primary angiosarcomas of the aorta are rare and because of their non-specific presentation, the initial diagnosis is often very difficult.
Report
A 66 year old woman, initially suffering from night sweats and general malaise, is presented. A computerized tomography (CT) scan was performed which showed a filling defect of the descending aorta. This defect later caused embolic occlusion of the celiac vessels. The patient underwent surgical resection of the filling defect of the descending aorta and an embolectomy of the celiac vessels. The defect was histopathologically diagnosed as an angiosarcoma. The clinical presentation, diagnostic pitfalls, histopathological diagnosis, and the therapeutic management are discussed.
Discussion
In this case report, the importance of carefully diagnosing an angiosarcoma is highlighted as the consequences could be rapid metastasization or embolization.
Keywords: Angiosarcoma, Descending aorta, Malignancy, Primary aortic tumor
Highlights
-
•
An angiosarcoma of the descending aorta was diagnosed, which is a rare malignancy.
-
•
This malignancy is very hard to diagnose therefore long-term survival is uncertain.
-
•
This malignancy is very aggressive for both local and distant recurrence.
-
•
This case report reflects the difficulty in diagnosing this malignancy.
-
•
It also shows the rapid progression of this disease.
Introduction
Primary malignant tumors of the aorta, first described in 1873,1 are extremely rare and exhibit considerable histological heterogeneity.2 The symptoms and radiological appearance of these tumors are often non-specific. The diagnosis is often established after resection of the tumor.3, 4 The most common histological entities that have been described are sarcomas without classification.4
This is a case report of a patient who initially presented with night sweats and general malaise, who's CT scan showed a filling defect of the descending aorta, which, after resection, was later diagnosed as an angiosarcoma.
Case Report
A 66 year old woman, with no significant medical history, presented to her general practitioner with progressive general malaise that had lasted 6 months. She intentionally lost 10 kilograms because she was overweight. For 1 week, she had suffered from fever, night sweats, and fatigue in the lower limbs. She had no history of tuberculosis and, although living in an endemic Q-fever area, she had had no contact with sheep or goats. After 2 weeks she was referred to a rheumatologist who found an increased white cell count of 25.2 × 109/L (normal range 4–11 × 109/L), an increased C-reactive protein (CRP) level of 42 mg/L (normal range <10), and an increased erythrocyte sediment rate of 48 mm/hour (normal range <30 mm/hour). With the differential diagnosis of an unknown autoimmune disease she was treated with prednisone. As the symptoms persisted after 3 weeks, she was admitted to the department of internal medicine at a rural hospital. The initial differential diagnosis included an unknown generalized infection. Therefore, blood cultures were taken, which were negative and remained negative. The blood levels at that time were: an increased CRP of 106 mg/L, an increased white cell count of 20.6 × 109/L, and negative Q fever and lues. A computerized tomography (CT) scan showed a filling defect of the descending aorta and the coeliac trunk (Fig. 1), which was interpreted as a possibly infected thrombosis and was treated with gentamicin and vancomycin. To prevent further growth of a possible thrombus, the patient was treated with therapeutic Nadroparin (Aspen Pharma Trading, Dublin, Ireland). The CT findings suggested positron emission tomography (PET), which showed a hotspot at the filling defect of the descending aorta and a small hotspot in the right tibia, considered to be septic emboli. A magnetic resonance imaging (MRI) scan of the tibia was performed. The differential diagnosis of the lesion in the tibia was inflammation or a malignancy.
Figure 1.
CT scan showing an irregular abnormality in the descending aorta and occlusion of the celiac trunk.
The patient was referred to the department of vascular surgery of a tertiary referral hospital. Here the antibiotic was discontinued. On admission, no abdominal abnormalities were found on physical examination. The symptoms of the patient were persistent, but unchanged from the initial presentation. A multidisciplinary treatment team, including a cardiothoracic surgeon, a vascular surgeon, and a microbiologist recommended a magnetic resonance angiogram (MRA). This showed a non-enhancing lesion in the descending aorta without vessel wall involvement, concluding that the filling defect of the descending aorta was less suspicious of malignancy. Seven days after the referral, the patient developed acute abdominal pain. A CT scan was performed, which showed complete occlusion of the celiac trunk as well as infarctions in the left lobe of the liver, spleen, and both kidneys. To prevent further embolization and to limit any ischemia-reperfusion injury, urgent surgical intervention was performed. Because the MRA showed a non-enhancing lesion without vessel wall involvement, the defect was considered to be resectable, therefore endovascular recanalization and stenting was not considered before surgery.
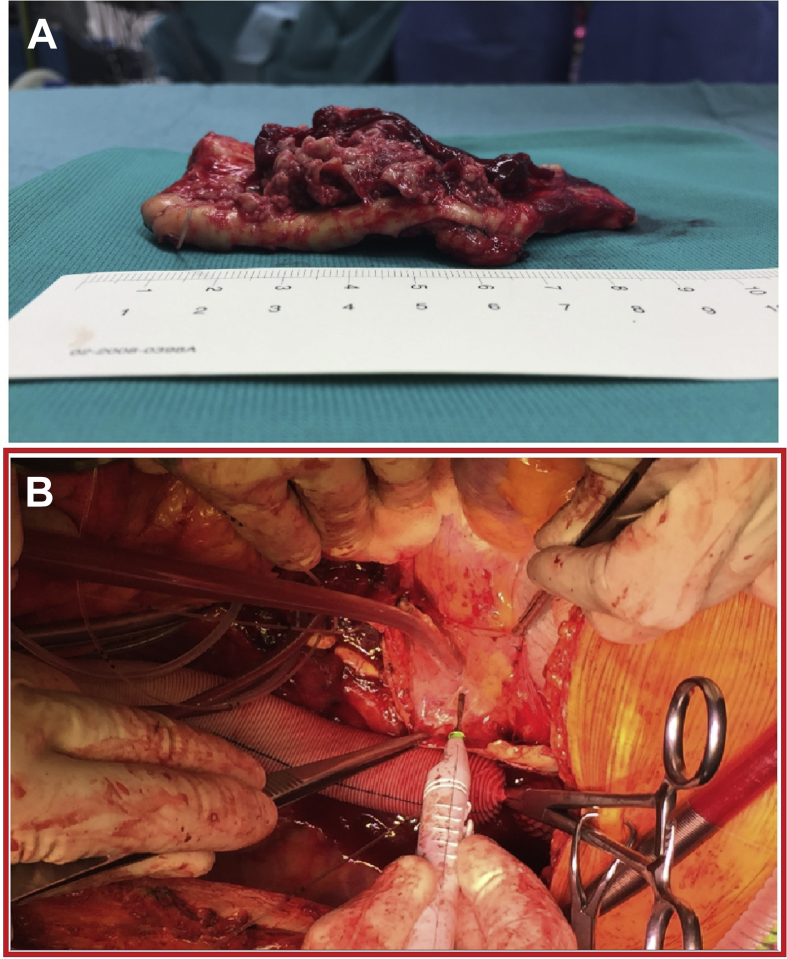
A left thoracophrenic-laparotomy was performed using left heart bypass with a Biomedicus pump (Medtronic inc. Minneapolis, MN, USA). The distal part of the thoraco-abdominal aorta, from the 8th thoracic vertebrae down to the celiac trunk, was resected (Fig. 2A). An embolectomy of the celiac trunk was performed. An interposition graft (Intergard prosthesis ø 22 mm, Maquet Getinge group, Intervascular, Athelia, La Ciotat, France) was inserted between the two ends of the aorta with an oblique anastomosis at the celiac trunk (Fig. 2B). The tumor appeared to have spread beyond the vascular wall into some of the intercostal arteries. After 4 days on intensive care, the patient returned to the ward, recovered without complications, and was discharged in good health 10 days after the operation. The total hospital stay was approximately 5 weeks.
Figure 2.
(A) Filling defect of the descending aorta resected from the 8th thoracic vertebrae to the celiac trunk. (B) Interposition graft inserted between the two ends of the aorta with an oblique anastomosis at the celiac trunk.
Histological examination revealed an epithelioid angiosarcoma. The tumor was present at the proximal resection edge and the embolus was shown to be a malignant tumor of the same kind. The tumor was staged pT4N0M1. Treatment was taken over by an oncologist, who conducted new PET, CT, and MRI scans to determine the course of treatment. In the PET/CT, a few weeks after the surgery, new abnormalities were found in the right femur and os ilium, suspicious of metastasis. The patient underwent palliative treatment.
Discussion
Primary angiosarcomas originate from the heart, aorta, or the great vessels. About 140 cases of primary malignant neoplasia of the aorta have been described in the literature, with the first being documented by Brodowski in 1873.1, 3
Primary malignant neoplasms of the aorta can be classified based on where they appear to arise from: the intima, media, or adventitia. The most common site is the intima, where a polypoid tumor forms with an intraluminal growth pattern, causing obstruction and embolization. Intimal tumors can also grow longitudinally with thickening of the arterial wall. Mural tumors often present later and with extravascular growth; they originate from the media or adventitia.3 Other neoplasms arising from the adventitia are tumors with extra-arterial growth and arterial obstruction, but these tumors are only present in advanced stages. The malignant neoplasms of the aorta that arise from endothelium are the angiosarcoma and endotheliosarcoma. The leiomyosarcoma arises from the smooth muscle cells of the media, and the fibrosarcoma arises from the adventitial fibroblasts.5 These malignancies are very aggressive for both local and distant recurrence.6 The most common location of primary malignant neoplasia of the aorta is the descending thoracic aorta. The second most common location is the visceral abdominal aorta, followed by the infrarenal aorta. The treatment for tumors arising from the visceral aorta is most difficult because of the early involvement of the visceral arteries.
Herein, a case is reported of an angiosarcoma of the descending aorta in a 66 year old woman. Although the reported observations involve a female patient, there is a male predominance for these neoplasms.3 Primary tumors of the veins are more often seen in women.
In this case, the woman suffered from non-specific symptoms. The symptoms that are usually mentioned in patients with malignant neoplasia of the aorta mostly originate from local occlusion of the aorta, such as symptoms of abdominal pain, lower extremity claudication, or secondary hypertension. The clinical presentation could also be related to embolization of the neoplasm, with metastases in the bones and skin, or to mesenteric infarction. The extension of the tumor in the visceral vessels could cause vascular insufficiency in the respective distribution.4, 5
Long-term survival is uncertain. Complete resection is very important, because the prognosis of patients with metastasis is extremely poor, as chemotherapy and radiotherapy are not effective.7 The 5 year survival is about 8%, with a mean survival of 14 months. The survival time of the patient in this case report is unknown because she is alive at present. As many as 80% of the patients have metastatic disease.5 In the case presented, the angiosarcoma of the descending aorta was not identified before embolization and metastases had developed.
In conclusion, angiosarcomas of the descending aorta are very rare, but should be suspected in patients in whom a filling defect of the descending aorta is seen on the CT scan. The diagnosis should be made before embolization of the process occurs, preventing metastasization and occlusion of the vessels. Symptoms usually present late. This case highlights the importance of careful consideration of the diagnosis when a filling defect in the descending aorta has been detected. If the present case is critically reviewed, it can be concluded that a pre-operative diagnostic work up of the filling defect of the descending aorta and the lesion in the tibia should have been prompted.
Conflict of Interest
None.
Funding
None.
References
- 1.Brodowski W. Primares sarkom der aorta thoracica nit verbretung des neugebildes in der unteren korperhalfte. Jahresb Leidtung Fortschr ges Med. 1873:243–246. [Google Scholar]
- 2.Thalheimer A., Fein M., Geissinger E., Franke S. Intimal angiosarcoma of the aorta: report of a case and review of the literature. J Vasc Surg. 2004;40(3):548–553. doi: 10.1016/j.jvs.2004.06.035. [DOI] [PubMed] [Google Scholar]
- 3.Hales S.L., Locke R., Sandison A., Jenkins M., Hamady M. Aortic angiosarcoma: a rare cause for leaking thoracic aneurysm. Cardiovasc Intervent Radiol. 2011;34(Suppl. 2):S20–S24. doi: 10.1007/s00270-009-9776-3. [DOI] [PubMed] [Google Scholar]
- 4.Böhner H., Luther B., Braunstein S., Beer S., Sandmann W. Primary malignant tumors of the aorta: clinical presentation, treatment, and course of different entities. J Vasc Surg. 2003;38(6):1430–1433. doi: 10.1016/s0741-5214(03)00935-2. [DOI] [PubMed] [Google Scholar]
- 5.Fatima J., Duncan A.A., Maleszewski J., Kalra M., Oderich G., Gloviczki P. Primary angiosarcoma of the aorta, great vessels and the heart. J Vasc Surg. 2013;57(3):756–764. doi: 10.1016/j.jvs.2012.09.023. [DOI] [PubMed] [Google Scholar]
- 6.Naughton P.A., Wandling M., Phade S., Garcia-Toca M., Carr J.C., Rodriguez H.E. Case report: intimal angiosarcoma causing abdominal aortic rupture. J Vasc Surg. 2010;53(3):818–821. doi: 10.1016/j.jvs.2010.10.090. [DOI] [PubMed] [Google Scholar]
- 7.Nakajima H., Kobayashi J., Matsuda H., Ishibashi-Ueda H. A primary angiosarcoma in the aorta. Interact Cardiovasc Thorac Surg. 2007;6:832–833. doi: 10.1510/icvts.2007.154575. [DOI] [PubMed] [Google Scholar]