Abstract
Cognitive Behavioral Therapy (CBT) is an evidence-based treatment for dental anxiety; however, access to therapy is limited. The current study aimed to develop a self-help CBT resource for reducing dental anxiety in children, and to assess the feasibility of conducting a trial to evaluate the treatment efficacy and cost-effectiveness of such an intervention. A mixed methods design was employed. Within phase 1, a qualitative “person-based” approach informed the development of the self-help CBT resource. This also employed guidelines for the development and evaluation of complex interventions. Within phase 2, children, aged between 9 and 16 y, who had elevated self-reported dental anxiety and were attending a community dental service or dental hospital, were invited to use the CBT resource. Children completed questionnaires, which assessed their dental anxiety and health-related quality of life (HRQoL) prior to and following their use of the resource. Recruitment and completion rates were recorded. Acceptability of the CBT resource was explored using interviews and focus groups with children, parents/carers and dental professionals. For this analysis, the authors adhered to the Mixed Methods Appraisal Tool criteria. There were 24 families and 25 dental professionals participating in the development and qualitative evaluation of the CBT resource for children with dental anxiety. A total of 56 children agreed to trial the CBT resource (66% response rate) and 48 of these children completed the study (86% completion rate). There was a significant reduction in dental anxiety (mean score difference = 7.7, t = 7.9, df = 45, P < 0.001, Cohen’s d ES = 1.2) and an increase in HRQoL following the use of the CBT resource (mean score difference = -0.03, t = 2.14, df = 46, P < 0.05, Cohen’s d ES = 0.3). The self-help approach had high levels of acceptability to stakeholders. These findings provide preliminary evidence for the effectiveness and acceptability of the resource in reducing dental anxiety in children and support the further evaluation of this approach in a randomized control trial.
Knowledge Transfer Statement: This study details the development of a guided self-help Cognitive Behavioral Therapy resource for the management of dental anxiety in children and provides preliminary evidence for the feasibility and acceptability of this approach with children aged between 9 and 16 y. The results of this study will inform the design of a definitive trial to examine the treatment- and cost-effectiveness of the resource for reducing dental anxiety in children.
Keywords: child dentistry, feasibility studies, evidence-based practice, comprehensive dental care, early intervention, patient care
Introduction
Dental anxiety commonly develops in childhood, and over one-third of children report some fear of visiting the dentist (Taani et al. 2005). Dental fear can prevent children from regularly engaging with dental services and completing dental treatment, which can have a negative impact on the oral health status and quality of life of these children (Nicolas et al. 2010; Taani 2002; Townend et al. 2000). Dental anxiety often continues into adulthood, with children who experience anxiety more likely to become symptomatic, rather than proactive, users of dental services when adults (Poulton et al. 2001).
Treating people with dental anxiety can be time consuming, challenging and can place financial demands on dental practices and services (Moore and Brodsgaard 2001). Children with anxiety are therefore a key group referred by dental practitioners to specialist services for pharmacological interventions (e.g., sedation, general anesthetic) (Harris et al. 2008). Referrals to specialist services often mean that patients have to travel further to access dental care and also cause longer delays in receiving dental treatment. Dental patients with anxiety may also become dependent on pharmacological approaches for the management of their care, particularly if they do not receive treatment for their anxiety (McGoldrick et al. 2001). Therefore, there is the potential for significant long-term benefits if early access to psychological interventions is available to reduce dental anxiety.
Meta-analyses have demonstrated the effectiveness of Cognitive Behavioral Therapy (CBT) in a range of anxiety disorders in children (James et al. 2015), and a series of systematic reviews have shown its efficacy in reducing dental anxiety (Armfield and Heaton 2013; Gordon et al. 2013). The approach incorporates cognitive and behavioral techniques to modify unhelpful thoughts and behaviors that maintain anxiety. Although there is evidence to support the use of CBT in the treatment of anxiety, access to this therapy is often limited (Chavira et al. 2004; Merikangas et al. 2011). “Pure self-help” (where an individual works through an intervention unsupported) and “guided self-help” CBT (where a healthcare practitioner supports the individual to work through an intervention) provide alternatives to traditional therapist-led CBT therapy and can be used as part of a “stepped care” approach to treatment (Bower and Gilbody 2005). The Five Areas model of CBT (Williams and Garland 2002), which focuses on the patient’s life situation, altered thinking, altered behavior, altered emotions and altered physical symptoms associated with their anxiety, offers an accessible model for the assessment and management of dental anxiety that can be applied in the clinical setting. This model has been used to theoretically inform a series of self-help resources for patients with a variety of common mental health problems (Williams 2012).
When developing an intervention, it is important that the preferences and needs of users are examined to maximize the relevance and acceptability of the intervention (Yardley et al. 2015). Therefore, the aim of this study was to involve children, parents/carers and dental team members in the development of a CBT self-help resource for reducing dental anxiety in children and to investigate the feasibility of evaluating the effectiveness of this resource in a randomized control trial. The research was undertaken in 2 phases and the specific research objectives for each phase were as follows:
Study phase 1:
Develop a child-centered, guided, self-help CBT resource plus guidance notes for parents/carers and a training package for practitioners.
Study phase 2:
Collect data on recruitment, retention and completion rates for the CBT resource
Examine effect size changes, variability in levels of dental anxiety, and quality of life following the use of the CBT self-help approach in children to determine the required sample size for a future trial.
Explore acceptability of the CBT resource to children, parents/carers and dental team members.
Determine whether preliminary evidence from the feasibility study supports continuation to a large-scale, randomized control trial.
Study Phase 1: Development of the CBT Resource
Materials and Methods
This research was informed by guidance for developing and evaluating complex interventions, and the study consisted of a development phase and feasibility study (Craig et al. 2008). The study adhered to the EQUATOR Network research review guidance (“Mixed Methods Appraisal Tool”) (Pace et al. 2012) and “RATS” checklist (“Relevance of study question,” “Appropriateness of qualitative method,” “Transparency of procedures,” and “Soundness of interpretative research”) (Clark 2003). Ethical approval for the research was granted by the NRES Committee York and Humber: Leeds West REC (13/YH/0163). Informed written assent/consent was obtained from children, parents/carers and professionals, and anonymity of the data was explained to the participants.
Design
The development of the self-help CBT resource was guided by the Five Areas model of CBT (Williams and Garland 2002), which focuses on enhancing the coping skills of individuals with anxiety using a mixture of cognitive and behavioral techniques. The “person-based” approach (Yardley et al. 2015) was employed to complement the theory-driven approach. This approach focuses on understanding and accommodating the perspectives and needs of people who will use an intervention, and thus involves iterative in-depth qualitative research with stakeholders throughout development of the intervention (Yardley et al. 2015). Therefore, children with dental anxiety, parents/carers and dental professionals were all involved in the development of the CBT self-help resource. Dyadic interviews were conducted with children and parents/carers and interviews/focus groups were undertaken with dental team members. Dyadic interviews and focus groups have the advantage that comments from one participant (e.g., a parent) can encourage responses from the other participant (e.g., the child), allowing for the stimulation of ideas (Morgan et al. 2013).
Children’s personal experiences of dental anxiety (e.g., their thoughts, behaviors, physical symptoms, feelings, and situational triggers) were explored during the interviews to ensure development of a young person-centered CBT resource (Morgan et al. 2016). During these interviews, participants were asked what they thought should be included in the CBT self-help resource (e.g., what they thought would help reduce their dental anxiety), and were asked to provide feedback on different format and delivery options (e.g., pure self-help vs. guided self-help). Participants were shown draft versions of the resource and iterative modifications were made based on the feedback provided. Data collection and analysis were conducted concurrently until data saturation occurred and no new themes emerged. Interviews were audio recorded and transcribed verbatim.
The design of the self-help resource was led by a commissioned design company, utilizing professional writers and designers.
Participants
As described previously, young people aged 11 to 16 y with dental anxiety and their parents/carers were purposively sampled to provide a range of views (Morgan et al. 2016). The criteria used for sampling included: gender; age; dental setting (primary/secondary care) deprivation; and ethnicity. Parents of children who had been diagnosed as dentally anxious by the dental clinician, were approached by the researcher.The researcher confirmed the presence of dental anxiety with each participant. Participants were recruited from 2 general dental practices: the community dental service, and a National Health Service (NHS) pediatric dentistry unit, located within the South Yorkshire region of the UK. The age range was selected to recruit participants of sufficient cognitive development who would be able to provide a detailed account of their previous anxiety experiences using the specified CBT framework (James et al. 2015). A sampling matrix was used to monitor the recruitment of participants. Children with severe communication difficulties or who did not speak English were excluded. Of the parents of the 17 children who were approached, 13 children (n = 10 female) aged between 11 and 15 y and their parents/carers agreed to participate in this phase of the study.
A purposive sample of dental team members were also recruited from a diverse range of settings (e.g., primary dental care practices, community dental services and dental hospitals), as outlined within the study protocol (Marshman et al. 2016). A total of 19 dental team members (13 GDPs, 2 pediatric dentists, 2 dental nurses, 1 community dentist, 1 dental therapist) participated.
Materials
The topic resource for the interviews with children and their parents/carers was based on the Five Areas CBT model (Williams and Garland 2002) developed by one of the researchers (C.W.) and included questions on past experiences of dental anxiety (e.g., to identify unhelpful thoughts, feelings, behaviors, physical symptoms and situational/contextual factors that need to be addressed within the CBT self-help resource). The topic resource for the dental team members included questions about their previous experiences of managing dental anxiety (e.g., to identify practitioners’ needs). Topic resources also examined stakeholders’ preferences for the content, format and delivery of the resources.
Analysis
Framework analysis (using the Five Areas CBT model) was used to analyze the qualitative data generated from interviews with children and parents/carers. This pragmatic approach to qualitative research draws on both inductive and deductive processes (Ritchie and Spencer 1994). The framework analysis involved the following stages: 1) familiarization with the data, 2) coding and identifying an analytic framework, 3) indexing (applying the analytic framework), 4) charting, and 5) mapping and interpretation. The data generated from interviews with dental team members were analyzed using thematic analysis, and a hybrid approach of inductive and deductive coding and theme development was employed (Braun and Clarke 2006). Data analysis was guided by an essentialist approach, which aims to report the experiences of participants (Braun and Clarke 2006). Data was entered into Excel spreadsheets and 2 researchers analyzed the qualitative data to promote rigor in the analysis (e.g., reliability of coding). Each researcher independently read and reviewed the transcripts to identify important and repeating ideas that emerged from the data. Any disagreements in interpretation were resolved through discussion.
Results and Summary
Four themes specifically related to the development of the CBT resource were identified from the stakeholder interviews, which included: “pure vs. guided self-help,” “supporting everyone involved,” “facilitators: engaging, informative and accessible,” and “potential barriers.” Details of how these data informed the development of the CBT resources are provided in Table 1. Table 2 details how the Five Areas model of CBT also guided the development of the CBT resources.
Table 1.
Summary of Themes that Informed the Development of the CBT Self-help Resource.
| Themes/Sub-themes that Emerged from Stakeholder Interviews | How This Informed the Content/Format/Delivery of the CBT Resource |
|---|---|
|
Theme 1: “pure vs. guided self-help”
• “Advantages and disadvantages of a pure self-help approach” (e.g., less practitioner time required; however, reliance on high levels of motivation, low levels of perceived value/ efficacy). • “Advantages and disadvantages of a guided approach” (e.g., would require more time but higher levels of perceived value/efficacy, time required needs to be feasible). • “Relationship building” (e.g., the resource should help build positive and trusting patient–dentist relationships; therefore, the dentist should have some involvement in the delivery of the resources). |
• The analysis of this data revealed stakeholders had a preference for the guided self-help approach delivered by the patient’s dentist; thus, a guided CBT resource was developed. • The CBT self-help resource includes a variety of tools that facilitate effective communication and positive relationships between the patient and the dentist (e.g., dentist message). • The CBT self-help resource was designed so that it could be used flexibly by practitioners: Practitioners can focus on reading/working through specific “self-contained” and “brief” sections of the resource that are most helpful for their patient and are most feasible for them to work through in their particular dental setting. |
|
Theme 2: “supporting everyone involved”
• “Parents/carers’ difficulties and challenges” (e.g., helplessness, responsibility/pressure, negative emotions). • “Ways in which parents/carers have tried to manage their child’s anxiety” (e.g., withholding information, persuasion/pressure, reassurance, distraction, positive reinforcement). • “Parent’s need for support” (e.g., better understanding of child’s anxiety, know what they can do to help their child). • “Needs of dental team” (e.g., Help with understanding patients’ anxiety and what can be done in practice to help manage anxiety, specific information about how to introduce the CBT book e.g., a script). |
A supporting parent resource was developed, which aimed to help parents/carers: • Understand their child’s dental anxiety and reflect on how helpful/unhelpful their own thoughts and behaviors might be. • Develop ways of supporting their children with their anxiety. A supporting resource for the dental team was developed, which included the following: • Information about to use the guided CBT resource with patients (e.g., scripts for introducing the CBT self-help resource, etc.). • General tips and techniques for the management of dental anxiety. An assessment tool was also included within the “dentist message” section of the children’s CBT resource to help dental practitioners better understand their patients’ anxiety/needs. |
|
Theme 3: “facilitators: engaging, informative and accessible”
• “Informative” (e.g., information on treatments, equipment, procedures) • “Simple and age-appropriate” • “Interactive” (e.g., activities to complete) • “Mixed formats” (e.g., online and paper-based) |
A paper-based, CBT self-help resource was produced so that the resource could be used easily by patients and dentists within dental clinics. However, as a result of this feedback, we have also developed an online portal where the CBT resource and supporting resources can be accessed for free (www.llttf.com/dental). A number of activities and illustrations are included within the resource to optimize engagement, and children, parents/carers and dental team members were all involved in the development and revision of the content/presentation of material to ensure the CBT resource was age appropriate and accessible. |
|
Theme 4: “potential barriers”
• “Too much information” • “Not enough time” |
The CBT self-help resource is designed so that it could be used flexibly with patients and dentists to overcome this possible barrier. Therefore, it is not necessary for patients or dentists to require large amounts of time to read/work through the whole CBT resource in one sitting. |
Table 2.
CBT Framework and Techniques Used in the “Your Teeth. You Are in Control” Self-help CBT Resource.
| Five Areas Model of CBT: Main Areas Targeted | Information/Activities included in the CBT Resource “Your Teeth. You are in Control” and Supporting Resources |
|---|---|
| 1) Altered thoughts and 2) altered feelings | The CBT self-help resource: • Explains how dental anxiety is common to normalize children’s feelings (e.g., “Not everyone loves their dentist” section). • Explains the common unhelpful thoughts that children with dental anxiety experience (using data provided by children in qualitative interviews) and how they can challenge these unhelpful thoughts. • Provides information on cognitive techniques/tools that children can use when at the dental clinic (e.g., “Here’s how to take control” section). • Contains procedural and treatment information (e.g., “The facts” section). • Encourages children to reflect on their experiences and reappraise their anxiety (e.g., “Now you’ve finished” section). |
| 3) Altered behaviors and 4) physical symptoms | The CBT self-help resource: • Provides information on specific behavioral techniques/tools children can use (e.g., “Here’s how to take control” section). • Encourages patients and dentists to develop a shared treatment plan (e.g., “Now make a plan” section). • Includes a communication tool that can be used by patients to communicate information about their anxiety to the dentist (“Dentist message” section). • Encourages children to write down the specific cognitive and behavioral techniques they are going to use next time they visit the dentist (e.g., “Preparing for next time” section). • Encourages the use of positive reinforcement to increase probability that helpful behaviors, such as attending the dentist and/or receiving treatment, will be repeated (e.g., “Time for a reward” section). |
| 5) Situational influences of dental anxiety (e.g., improving the patient–dentist relationship, dealing with parental anxiety) | The CBT self-help resource: • Requires patients and dentists to work through parts of the resource together to build up trust and a beneficial patient–dentist relationship. • Contains supporting resources for dental team members and parents/carers to facilitate a “team approach” to the management of children’s dental anxiety. |
The results from the qualitative interviews with children led to the development of the content for a child-centered resource, and included sections about: 1) how dental anxiety is common (to normalize feelings of anxiety), 2) the common “unhelpful thoughts” often experienced by children with dental anxiety (using data provided by children in qualitative interviews), 3) how to challenge these unhelpful thoughts, 4) procedural and treatment information, and 5) cognitive and behavioral techniques/activities that can be used by children when at the dental clinic.
Children expressed a preference for the resource to be made available in a mixture of formats (paper-based and online). The resultant resource entitled, “Your teeth. You are in control” has been produced as an A5 booklet and is available online free of charge at www.llttf.com/dental.
Parents/carers and dental team members felt they would find value in information that could help them to better understand the dental anxiety felt by children, and wanted practical tips on how to help the child feel less anxious. As a result, complementary resources for parents/carers and dental team members were developed, which include a resource for parents/carers and a dental team practice resource. These supporting resources are also available as A5 booklets, summary sheets, and can also be accessed online from www.llttf.com/dental. A clinical protocol and communication script were also developed to support the practitioners’ implementation of the guided CBT approach.
Children and other stakeholders advised against developing resources that included too much information and that would take too long to work through. Therefore, various drafts of the resources were shown to children, parents/carers and dental team members to ensure the most important and relevant information was included in the resource, that the resource was concise, and that sections could be completed quickly and while in the dental appointment, if required.
Study Phase 2: Feasibility Study
Materials and Methods
Following the development of the CBT self-help resource, a feasibility study was undertaken to determine whether further evaluation of the resource was warranted and possible. This phase of the study utilized a mixed methods approach. A protocol providing detailed methodology related to the feasibility study has been published previously (Marshman et al. 2016). Informed written assent and consent were obtained from children and parents/carers/professionals, respectively, before their involvement in the research, and data anonymity was explained to participants.
Design and intervention
Patients were recruited from 2 community dental clinics in Derbyshire and 1 dental hospital in the South Yorkshire region of the UK. New patients presenting at these clinics were given a “screening slip” at reception that asked them to indicate whether they were worried about going to the dentist. Patients who met all of the inclusion criteria and their parents/carers were invited to participate at this initial new patient visit.
At the next visit, children and parents/carers who had indicated a desire to participate in the study were provided with the CBT self-help resource. The resource was explained to children and their parents/carers, and children were asked to read the CBT self-help resource and complete the relevant sections (e.g., their “message to the dentist”) before their next appointment. Baseline dental anxiety and quality of life questionnaires were also completed by the child at this visit (T1). During the next 2 appointments, the clinician worked through and discussed specific sections of the CBT self-help resource with the patients and treated the child as medically necessary (e.g., fissures sealants, extractions, restorations). At the end of their third appointment, patients completed the follow-up dental anxiety and quality of life questionnaire (T2). Further appointments (if required) were scheduled in accordance with patients’ clinical needs.
Participants
This phase of the study had specific inclusion criteria and children had to be: aged between 9 and 16 y; English speaking; respond “a little bit worried” or “very worried” to the screening question “Please tell us how you feel about going to the dentist”; require a course of dental treatment that would involve at least 3 separate visits; and not have an acute dental problem that required urgent dental treatment. Lancaster and colleagues (2004) recommend a minimum sample size of 30 to estimate a parameter such as a standard deviation (which is required to inform on sample size calculations for a future trial). Among the dental team members, 4 pediatric dentists, 2 dental nurses and 1 dental therapist based in a community dental service and a pediatric dental hospital delivered the guided CBT self-help approach.
Materials
A clinical protocol and a communication script were developed to support the practitioners’ implementation of the guided CBT approach. Dental anxiety was assessed using the 8-item Modified Child Dental Anxiety Scale (MCDAS) (Humphris et al. 1998), which assesses children’s concerns in relation to specific dental procedures (examination, scale and polish, injection, filling, extraction, inhalation sedation, and general anesthesia) and how the child feels generally when they visit the dentist. For this, 5-point Likert scale was used—a measure that has demonstrated good internal consistency (Cronbach alpha coefficient = 0.84) (Humphris et al. 1998)—and total scores ranged from 8 (little or no dental anxiety) to 40 (extreme dental anxiety). Two global change questions were employed to assess self-reported change in dental anxiety (e.g., “Has how you feel about going to the dentist changed since your first visit to the dental hospital?” and “Has how you feel about going to the dentist changed since you started using the green booklet?”). Again, a 5-point Likert response scale was used (1 = “I feel a lot less worried” to 5 = “I feel a lot more worried”).
HRQoL was assessed using the Child Health Utility 9D (CHU-9D) questionnaire (Stevens 2010). Children were asked to rate how they felt that day, and 9 domains were assessed (worried, sad, pain, tired, annoyed, school work/homework, sleep, daily routine, able to join in activities). Each domain has 5 response options, and utility weights were calculated from the responses. The UK tariff generates utility weights between 0.33 and 1 (perfect health), with a higher utility reflecting higher HRQoL. The CHU-9D has demonstrated an acceptable level of internal consistency (Cronbach alpha coefficient = 0.78) (Furber and Segal 2015).
Analysis
Descriptive data on recruitment, retention, and completion rates is presented. Wilcoxon signed-rank tests were undertaken to analyze differences in individual items on the MCDAS, which assess anxiety related to specific dental procedures (e.g., tooth extraction, inhalation sedation, injection, and filling). Paired t-tests were used to compare baseline and follow-up total MCDAS scores and CHU-9D utility scores. Effect sizes were calculated using Cohen’s d Effect Size (ES) statistic. To calculate total anxiety and utility scores for cases who had missing data, median scores for the specific MCDAS/CHU-9D items were imputed for cases where there was less than 50% of data missing from the total scale. Participants’ responses to the global change questions are also reported.
Acceptability of the CBT Resource
Qualitative research was employed, because it is particularly useful for exploring issues concerning acceptability, implementation and practicality of an intervention and for exploring possible mechanisms of change (O’Cathain et al. 2015).
Design
Interviews were undertaken with children and parents/carers once children had completed the intervention. Children were given the option to be interviewed with their parent or separately. Interviews with dental professionals were also undertaken to examine their perspectives and experiences of using the CBT self-help resource. Data collection and analysis were conducted concurrently until data saturation occurred and no new ideas emerged. Interviews were audio recorded and transcribed verbatim.
Participants
A purposive sample of children who had taken part in the feasibility study (e.g., range of ages, gender, dental setting (primary/secondary care) deprivation, engagement with resource) were invited to participate, with their parents/carers, to obtain a diverse range of experiences and perspectives. Twelve families were approached and 11 families participated in this phase of the research (one family declined due to other commitments). The characteristics of the participants are detailed in Table 3. Children were aged between 10 and 15 y, the majority were female (n = 7, 64%). Eleven mothers and 2 fathers participated.
Table 3.
Characteristics of Young People Purposively Sampled for Interviews in the Feasibility Study (Phase 2).
| Participant Group Number | Participant’s Details | Dental Setting Deprivation Quintile (1 = Least Deprived, 5 = Most Deprived) |
Dental Treatment | Engagement with Resource at First Visit (Written in Guide) |
|---|---|---|---|---|
| Participant group 1 | Male (15 y) and mother | 5 | Dental restorations and extractions | Yes, partly (able to discuss) |
| Participant group 2 | Female (12 y) and mother | 2 | Dental restorations and extractions | Not at all (no idea) |
| Participant group 3 | Female (13 y) and mother | 3 | Fissures sealants, extractions and restorations | Yes, partly (able to discuss) |
| Participant group 4 | Male (14 y) and mother | 2 | Dental restorations | Yes, partly (able to discuss) |
| Participant group 5 | Female (12 y) and mother | 1 | Fissure sealants, restorations and extractions | Yes, fully (written in guide) |
| Participant group 6 | Female (14 y), mother and father | 5 | Fissure sealants, restorations and extractions | Yes, fully (written in guide) |
| Participant group 7 | Female (10 y) and father | 4 | Fissure sealants and extractions | Yes, fully (written in guide) |
| Participant group 8 | Male (13 y) and mother | 3 | Dental restorations and extractions | Not at all (no idea) |
| Participant group 9 | Female (14 y) and mother | 1 | Fissures sealants and extractions | Yes, fully (written in guide) |
| Participant group 10 | Female (11 y) and mother | 4 | Fissures sealants and extractions | Yes, fully (written in guide) |
| Participant group 11 | Male (13 y) and mother | 3 | Fissure sealants and restorations | Yes, partly (able to discuss) |
Dental professionals’ perspectives and acceptability of the CBT approach were explored using interviews/focus groups. Dental team members who were involved in the development of a CBT self-help resource were asked about their perceived acceptability of a CBT-resource for the management of dental anxiety within the initial series of interview/focus groups. Additional interviews were conducted with dental professionals who had used the CBT self-help book with patients.
Materials
The topic resource for children was based on the Five Areas CBT model (Williams and Garland 2002) and explored changes in children’s experiences of dental anxiety as a result of the CBT intervention. It also covered the views of children and parents/carers about the usefulness of the resource (acceptability) and the barriers associated with the use of the CBT self-help approach (usability). The topic resource for dental health team members was guided by the Theory of Planned Behavior (Ajzen 1991) and explored factors that could influence practitioners’ future use of the CBT self-help approach and its acceptability.
Analysis
Framework analysis was used and a hybrid approach of inductive (data-driven) and deductive (theory-driven) coding and theme development was employed (Ritchie and Spencer 1994). After coding the first 3 transcripts the 2 researchers involved compared the codes they had applied and agreed on a set of codes to apply to all subsequent transcripts. Coding and indexing was done manually and an Excel spreadsheet was used to chart data. Initial themes were discussed with the research team and reflexive engagement with the data contributed to the development of the final themes. Any disagreements in interpretation were resolved through discussion.
Results
Recruitment and completion rates
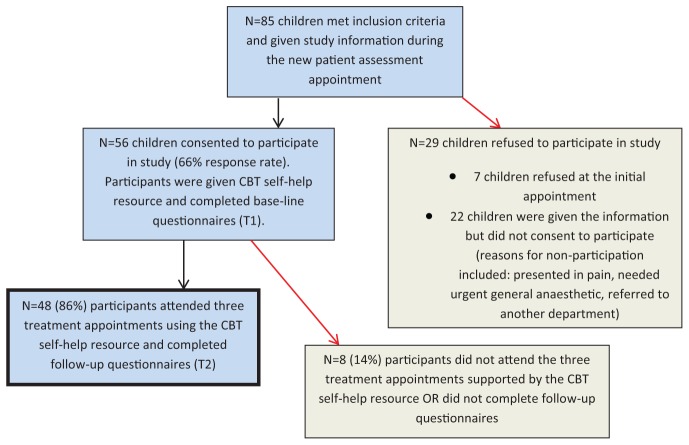
A total of 85 children were invited to participate in the feasibility study and trial the CBT resource. The recruitment rate (proportion of children invited to take part in the study who agreed to participate) and completion rate (proportion of children who agreed to participate who completed the study) was 66% and 86%, respectively (see Figure). A total of 48 patients completed the study. Table 4 provides a summary of the characteristics, dental setting (primary/secondary care) deprivation levels, treatment needs, and levels of engagement with the CBT resource for the study population.
Figure.
Flowchart of recruitment and completion rates in the feasibility study (phase 2). CBT, Cognitive Behavioral Therapy.
Table 4.
Data for Participants Who Completed the Feasibility Study (Phase 2).
| Variables | n / Mean |
|---|---|
| Participants completed CBT self-help resource | n = 48 |
| Mean age | Mean, 12.3 y (SD, 1.9 y) |
| Gender | |
| Male | n = 15 |
| Female | n = 33 |
| Ethnic Background | |
| White British | n = 45 |
| Any other group (English Caribbean & Asian Pakistani) | n = 3 |
| Dental Deprivation score | |
| 1st Quintile (least deprived) | n = 9 |
| 2nd Quintile | n = 5 |
| 3rd Quintile | n = 9 |
| 4th Quintile | n = 10 |
| 5th Quintile (most deprived) | n = 15 |
| PAST DENTAL HISTORY | |
| Past dental general anesthetic | |
| Yes | n = 16 |
| No | n = 30 |
| Not known | n = 2 |
| Previous inhalation sedation | |
| Yes | n = 4 |
| No | n = 44 |
| Reason for referral | |
| Caries | n = 36 |
| Orthodontic extractions | n = 10 |
| Trauma | n = 1 |
| Other | n = 1 |
| Engagement with CBT resource at “intervention appointment 1” visit | |
| Yes, fully (written in guide) | n = 26 |
| Yes, partly (able to discuss) | n = 15 |
| Not at all (no idea) | n = 6 |
| Data missing | n = 1 |
| Completed treatment following use of CBT self-help resource | |
| Yes | n = 43 |
| Treatment ongoing | n = 5 |
| Pharmacological intervention(s) | |
| Referral letter stated need for GA | n = 10 |
| Child received GA only | n = 3 |
| Referral letter stated need for sedation | n = 19 |
| Child received inhalation sedation only | n = 38 |
| Child received GA and inhalation sedation | n = 3 |
CBT, Cognitive Behavioral Therapy; GA, general anaesthetic.
Dental anxiety and quality of life
In response to the question to children, “Has how you feel about going to the dentist changed since your first visit to the dental hospital?”, 35 (73%) participants indicated they felt “A lot less worried” and 12 (25%) participants indicated they felt “A little less worried” (missing data for 1 participant). In response to the question, “Has how you feel about going to the dentist changed since you started using the green booklet?”, 29 (60%) participants indicated they felt “A lot less worried,” 17(35%) indicated they felt “A little less worried,” and 1 participant (2%) indicated their feelings had not changed (missing data for 1 participant).
The mean MCDAS score at baseline was 25.0 (SD, 6.5; range, 15 to 35) and at follow-up the mean score was 17.4 (SD, 6.1; range, 8 to 31). The results revealed a significant large reduction in dental anxiety following the CBT intervention (t = 7.9, df = 45, P < 0.001; 95% CI = 5.7 to 9.6; Cohen’s d ES = 1.2) (Cohen 1992).
Wilcoxon signed-rank tests also revealed significant reductions in anxiety levels related to the following procedures: “injection” (baseline median = 5 “very worried,” follow-up median = 3 “fairly worried”; z = -4.86, P < 0.01); “filling” (baseline median = 4 “worried a lot,” follow-up median = 2 “very slightly worried,” z = -4.04, P < 0.01); “tooth taken out” (baseline median = 5 “very worried,” follow-up median = 3 “fairly worried,” z = -4.51, P < 0.01), and “mixture of gas and air” (baseline median = 3 “fairly worried,” follow-up median = 1 “relaxed/not worried,” z = -3.15, P < 0.01).
The mean CHU-9D utility score at baseline was 0.875 (SD, 0.09; range, 0.51 to 1.0) and at follow-up, 0.904 (SD, 0.08; range, 0.68 to 1.0). The results revealed a significant small improvement in quality of life following the CBT intervention (t = -2.14, df = 46, P < 0.05, 95% CI = -0.06 to -0.00, Cohen’s d ES = -0.3) (Cohen 1992). Children reported decreases in the impact on HRQoL between baseline to follow-up for: worry (81% to 56%), sadness (23% to 19%), annoyed (17% to 8%), tired (73% to 56%,), schoolwork (31% to 19%), sleep (27% to 25%), daily routine (21% to 10%) and joining in activities (38% to 19%). However, children reported an increase in the impact on HRQoL between baseline and follow-up for the pain domain (17% to 27%, respectively).
Acceptability of the Guided CBT Self-help Resource by Children and Parents/Carers
Framework analysis revealed 3 themes and 6 subthemes within the data, which are discussed below. The coding templates and analytic framework used to develop the final themes are included in the Appendix.
Theme 1: “a positive experience”
Children and parents/carers indicated that they were pleased that they had been offered the CBT resource and felt it had been useful in helping them and their child manage the child’s anxiety.
“An increased understanding”
Children particularly valued the information provided within the child CBT self-help resource (e.g., procedural information), which had increased the predictability of treatment and reduced their anxiety.
“I felt a little better when I knew what was happening and what the injections were” (Participant group 4, male 14 y).
“Less anxiety, more confidence”
Children indicated that they felt reduced levels of anxiety and worry following their use of the resource. Many of their worries and fears (e.g., “I can’t trust the dentist” and “it will be painful”) had been challenged as a result of new positive experiences and feelings of confidence when talking through their concerns with their dentists. Children and parents/carers discussed how using the resource had made them feel more confident so they could cope when they visit the dentist.
“He was really scared of going. Then, with the help of the lady dentist and the resource, he was happy to go. The last time it was, ‘You don’t have to go if you don’t want to go.’ ‘Yeah, I’m going. I’m going.’ So, big difference” (Participant group 1, mother).
However, some children felt they would still experience some anxiety in the future, for example, if they had to receive dental treatment without sedation.
“Additional benefits”
Many parents/carers felt the CBT resource had helped them better understand their child’s anxiety and allowed them to become more supportive when their child was anxious. Some parents/carers also reported reductions in their own dental anxiety as a result of supporting their child in using the CBT resource.
“I didn’t realize how much it would help me” (Participant group 1, mother).
Theme 2: “barriers to engagement”
Children found the child CBT self-help resource easy to follow and understand. However, children commonly reported that they had forgotten to complete sections of the resource before their appointment and forgotten to take the resource with them to the dentist; this indicates a potential barrier to engagement. Some children talked about how they would like to use the resource in the future; however, there was some uncertainty from children and parents/carers about how a general dentist would react to the guided self-help approach and this was cited as a reason why they might not use the resource in the future:
“I’m not saying they were bad or anything [general dentist] but they just don’t always have the time. I don’t know because it would probably help [using the resource]. It would probably speed things up” (Participant group 11, mother).
While parents/carers thought having separate supporting parent guidance was useful, few had actually read the parent guidance due to a lack of time. Parents/carers did, however, help children read through the child CBT resource and this appeared to be useful for both children and parents/carers.
“Overcoming barriers”
Children and parents/carers appreciated the guidance that dentists had provided, and this helped them work through key sections of the CBT resource. This “guided” approach was seen as central to the building of positive patient–dentist relationships. Children and parents/carers also recognized the value of dentists having worksheets available for occasions when children had not remembered to take their CBT resource to their appointment.
Theme 3: “the importance of communication and positive relationships”
“Communication and care”
A consistent finding was that the CBT resource helped children and parents/carers communicate with their dentist and develop a positive patient–dentist relationship. They viewed the action of their dentist giving them and the child the CBT self-help resource as a sign that the dentist was interested in exploring the child’s dental anxiety and that they wanted to help them. Children felt that using the resource enabled them to ask their dentist more questions than they would usually, and to talk about their anxiety more openly with the dentist.
“The message to the dentist” (Participant group 5, Female 13 y) “You like that bit?” (Interviewer) “Yeah…because you can tell the dentist how you feel and tell them things that you want to happen in the appointment and the things you don’t want” (Participant group 5, Female 13 y).
“It’s more that somebody’s actually taking an interest in taking time” (Participant group 4, mother).
Some children worried about returning to their local dentist with whom they did not have such a positive relationship:
“I think it’s because the dentist that we’ve got, they’re not, like, good, if I’m honest, because they don’t tell you stuff” (Participant group 3, female 12 y).
“Control and choice”
Agreeing on a stop signal—one of the activities suggested in the book—was particularly valued by children and parents/carers. Having a clear understanding of what would happen within the appointment allowed patients to feel more in control. Children also liked the cognitive and behavioral techniques (e.g., distraction, listening to music) and the choices that had been provided to them as result of using the resource:
“Normally, I’m really scared in the dentist and normally I’ll just say I don’t need to go. When I read some of this, I was, like, cool and then the dentist kept telling me that you do get to make decisions…then I felt more comfortable” (Participant group 4, Female, 14 y).
“They let her have her headphones in, basically, listen to music and she had full control of everything that she was doing and I think that were a big part of her confidence” (Participant group 2, mother).
Dental Professionals’ Acceptability of the Guided CBT Self-help Approach
In total, 25 dental professionals were interviewed; 19 dental team members who had been involved in the development of the CBT resource and 6 additional professionals (3 pediatric dentists, 1 pediatric dental therapist, 1 dental nurse who had experience using the CBT resource with patients, and 1 commissioner of dental services). Thus, the majority (80%) of professionals who provided data on the acceptability of the self-help resource had not used the self-help resource with patients.
The framework analysis revealed 4 themes and 6 sub-themes within the data, which are discussed below. The coding templates and analytic framework used to develop the final themes are included in the Appendix.
Theme 1: “the value of a CBT self-help resource”
“Anxiety management: an important part of our role”
Dental team members felt that managing anxiety of their patients was important and presented significant challenges.
“If we don’t help them now, they are going to grow up to be adults with a mouth full of rotten teeth who will need very difficult extractions, who are terrified to come in” (D4, GDP).
“It’s quite difficult, you know. Lots of the time, the parents/carers are anxious as well so there is no one really supporting you” (D7, GDP).
“Benefits of using a CBT self-help resource”
Dental team members were positive about the development of a resource that could aid them in the management of dental anxiety. Perceived benefits of using a CBT self-help approach included: 1) reducing children’s dental anxiety levels and their reliance on pharmacological approaches to managing their dental care, and 2) helping practitioners understand and manage dental anxiety.
“As a clinician this would be a really valuable aid …[…]… from a commissioning point of view, any aid that helps people on the ground to do something has got to be valuable …[…]… the best way to reduce a GA waiting list is not to put more money in. It’s to front load with a load of resources to stop it happening in the first place and then load it at the end to stop the recurrence” (D25, commissioner).
“It [anxiety] could be managed with the help of a self-help approach. I think that would be a huge advantage and I think for the patients longer term to be able to have their dental treatment done but without the anxiety and not having that reliance on sedation or general anesthetic” (D1, community dentist).
However, practitioners felt that it was important that the CBT resource could be used with patients within the time constraints of the NHS dental contract.
“I wouldn’t want it to be too complicated and I wouldn’t want it to be another kind of something that you would have to do long training” (D11, pediatric dentist).
Theme 2: “patient suitability and engagement”
It was recognized that there were some individuals for whom the CBT self-help approach may be less suitable. It was suggested that children who had complex needs (e.g., autism) could experience difficulties engaging, and this type of approach may not be sufficient to manage patients with high levels of dental anxiety.
“[Children with] mild autism and Asperger’s… perhaps haven’t engaged with it quite as well, found it harder…” (D21, pediatric dentist).
Some professionals also felt that a proportion of patients would not be interested in the resource because of a preference for (or reliance on) pharmacological interventions.
“Some patients, they just come in and say ‘I want sedation’” (D7, GDP).
“I think it’s to do with targeted stigma associated with psychology being a mental health issue…but if patients and parents/carers are open to it, I think it will be received really well” (D2, pediatric dentist).
“Parental involvement: beneficial but not essential”
Dental team members who had no experience in using the CBT resource felt that parental engagement would be central to the success of the CBT self-help approach. However, dental team members who had used the resource felt that this was less of an issue and suggested that this was because the CBT resource had incorporated an interactive/guided element, which enabled children who had not engaged with the resource at home to work through key sections with their dentist.
“A lot of these children want to feel better about the dentist…so I think a lot of them like to do the booklet and that’s it, it’s completely independent from the parents/carers a lot of the time” (D23, pediatric dentist).
Theme 3: “using the resource in the real world”
Some practitioners anticipated difficulties using a CBT self-help resource.
”Confidence”
Dentists interviewed felt that they would have the skills necessary to deliver the intervention. However, those individuals who had previous experience using the CBT resource felt it did take some time to adjust to this new way of working with anxious patients. The use of scripts was particularly valued by these individuals. Professionals also felt that additional online training could be provided to help develop people’s confidence in the using of the resource.
“A viable management approach?”
It was suggested that practitioners would value the use of a CBT resource with their patients if they found the resource could be feasibly delivered within their practice.
“If it was 5 min at the start of a filling appointment say, yes then I think I could do it” (D7, GDP).
However, some of those interviewed felt that a proportion of practitioners might doubt the efficacy of CBT or have low levels of motivation to treat dental anxiety and thus be reluctant to use the CBT self-help approach within their practice.
“There are certain individuals out there who just don’t believe in it” (D2, pediatric dentist).
Practitioners recommended the resource be evaluated in different dental settings so that the evidence base could be examined. Most of the practitioners were keen to use and evaluate the use of the CBT self-help resource with their patients on the condition that this could be implemented within the time constraints of their NHS clinics.
Theme 4: “the whole package”
It was felt that there were various ways in which the CBT self-help resource reduced dental anxiety. Dental team members suggested that one of the key mechanisms to change was the facilitation of positive patient–dentist relationships, which led to patients developing their trust in the dentist and subsequently feeling less anxious. Dental team members felt that working through the CBT resource with patients had enabled them to gain a better understanding of the patient’s anxiety and thus demonstrate more empathy when interacting with the patient.
“It’s the whole package that reduces their dental anxiety, but maybe that’s what it is… it’s been an opportunity to build up a positive relationship with the patient” (D21, pediatric dentist).
“Communication and care”
It was suggested that the self-help resource had acted as a communication aid between anxious patients and dentists. The importance of dentists’ characteristics and behaviors in reducing patients’ anxiety was highlighted within the interviews and many of those interviewed felt the CBT resource would fail if the practitioner delivering it did not interact with children in a positive manner (e.g., wasn’t friendly, caring and approachable).
“Until that child feels you’ll be looking after them as an individual and caring about what they want, then I think they are always going to be a bit resistant” (D6, GDP).
“It’s about, I believe, in building up trust and honesty” (D22, pediatric dental therapist).
Discussion
While there is some evidence that therapist-led CBT is an effective treatment for dental anxiety, there is a lack of research exploring the needs and preferences of children, parents/carers and dental team members in relation to the management of dental anxiety. It is important that users’ perspectives are fully considered in the intervention design process to maximize the relevance of the intervention for users and the likelihood that the intervention will be adopted by the target population. Therefore, within phase 1 of the research, children, parents/carers and dental team members were involved in developing a CBT resource aimed at reducing dental anxiety in children. One of the specific objectives of the project was to develop a child-centered resource that would be acceptable to key stakeholders, and this was achieved through a “person-based” approach to intervention development (Yardley et al. 2015). To ensure that the intervention was evidence-based, the Five Areas model of CBT (Williams and Garland 2002) was used to inform the development of the CBT self-help resource. One of the benefits of utilizing this specific CBT framework was the model’s inclusion of contextual and situational factors. Indeed, the findings from the qualitative interviews highlighted the significance of interpersonal relationships; specifically, patient–dentist communication and trust. Had an “individualistic” model driven the development of the intervention, these interpersonal factors may not have been fully considered.
Phase 2 of the research aimed to investigate the feasibility of evaluating the CBT resource in a randomized control trial (RCT). Therefore, data on recruitment and retention/completion rates associated with patients’ use of the CBT resource was collected. Two-thirds of children who were invited to participate agreed to take part in the study. Recruitment/response rates are important because they provide an indication of how many patients would need to be approached in a future trial to obtain the required sample size. The results from the feasibility study indicate that self-help will not be an appropriate management approach for all children with dental anxiety. Indeed, it is widely recognized that some patients with anxiety-related conditions will not opt for CBT-based interventions and that several psychosocial factors (e.g., motivation to change, complexity of life situation, psychological mindedness) may influence a patient’s willingness to engage or suitability for CBT (Blenkiron 1999). Within the current research, 86% of the patients who were recruited went on to complete the study, which is comparable with completion rates reported in CBT services for adults with dental anxiety (Kani et al. 2015).
The current findings suggest that the CBT self-help resource may be beneficial in reducing dental anxiety in children. This is consistent with a meta-analysis undertaken by Kvale et al. (2004), which revealed that behavioral interventions aimed at reducing dental anxiety have a large effect size overall (1.8). However, this meta-analysis focused on interventions for the management of dental anxiety in adults. The findings from the current study suggest that the CBT resource may be an effective intervention for children with dental anxiety. Standard deviation scores and effect sizes in the current study could also be used to inform a sample size calculation for a future trial. However, within a future trial, it will be important to establish whether the reduction in dental anxiety associated with the use of the self-help CBT resource is clinically meaningful. The improvement in HRQoL is also interesting and indicates that the CHU-9D measure may be an appropriate instrument to use in a future trial, as it has the required sensitivity to detect changes in HRQoL impacts associated with dental anxiety and oral health. The mean difference of 0.03 reported in this study is generally regarded as significant in utility measures (Drummond 2001).
The feasibility study also explored the views of children, parents/carers and dental team members about the acceptability of the CBT self-help approach. Findings from the stakeholder interviews revealed children, parents/carers and dental professionals viewed the self-help book positively. The qualitative data suggested that the CBT self-help resource may operate on a number of different levels to reduce dental anxiety in children. The provision of preparatory information and the use of cognitive and behavioral strategies appeared to increase patients’ perceptions of control and reduce dental anxiety. The importance of adequate information provision and cognitive-behavioral strategies in the management of patients with mild to moderate dental anxiety has indeed been highlighted within the literature (Newton et al. 2012). The use of the CBT resource also appeared to facilitate positive patient–dentist relationships and improve communication. Effective patient–dentist communication plays a significant role in reducing dental anxiety (Zhou et al. 2011). It is possible that the efficacy of many self-help interventions could be partly attributable to this type of therapeutic alliance. Indeed, there is some evidence that therapeutic alliance is a key factor in developing feelings of safety and calmness in children with dental anxiety and that this can lead them to view dental staff in a more positive light (Shahnavaz et al. 2015). The findings from the current study also provided some evidence that parents/carers had learnt effective ways of supporting their children with their anxiety, highlighting the importance of promoting parental involvement in the development and implementation of child-centered interventions.
The final objective of the study was to determine whether preliminary evidence supports continuation to a large-scale, randomized control trial. The recruitment and retention rates within the current study and the reduction in children’s dental anxiety and improvement in HRQoL following their use of the CBT self-help resource provide promising results to suggest that this intervention may be a viable approach for the management of dental anxiety in children. These findings are consistent with previous research showing evidence for the effectiveness of guided self-help CBT in the treatment of child anxiety (Creswell et al. 2014). Therefore, it is proposed that further evaluation of the treatment efficacy and cost-effectiveness of the CBT self-help approach is warranted.
While there are challenges with undertaking mixed methods studies (e.g., resources required, integration of data), the mixed methods approach employed within the current study strengthened the quality of this research. Indeed, Medical Research Council guidance for the development and evaluation of complex interventions suggests that feasibility studies benefit from the inclusion of both quantitative and qualitative methods (Craig et al. 2008). To maximize the credibility and quality of the research undertaken, it is important that individuals are reflexive and consider how their personal experiences, perspectives and roles may influence the research process/findings. Within the current study, 3 members of the research team had a dual role within the research and were involved in both the design of the research and the delivery of the CBT intervention. It is therefore possible that their in-depth knowledge of the CBT self-help resource could have influenced their confidence in their implementation of the resource. To manage this potential issue, a communication script was developed to standardize the delivery of the CBT approach. In addition, to minimize the likelihood of social desirability bias within the study (e.g., patients feeling the need to provide positive feedback about the CBT self-help resource because they are aware their dentists are part of the research study and want to please them), all interviews and analyses were undertaken by members of the research team who had no clinical involvement in the child’s dental care. Children and parents/carers were also informed that their dental care would not be influenced by their participation in the research and that their responses would be anonymized.
There were a number of limitations to the study. Firstly, it was an uncontrolled treatment development and feasibility study and therefore the design of the study prevents examination of whether the improvements in dental anxiety and HRQoL were due to the intervention itself. It is possible that treatment effects (e.g., desensitization) contributed to the reduction in dental anxiety. Potential confounder variables (e.g., socioeconomic status) could also have influenced the results of the study, and these confounders should be considered in any future evaluation of the resource. However, the aim of this study was not to evaluate the effectiveness of the CBT self-help resource but to examine whether preliminary results suggest this intervention could and should be tested in a full-scale trial. Secondly, within the feasibility study, all of the patients with self-reported dental anxiety were invited to trial the resource. At baseline, MCDAS scores ranged from 15 to 35 and therefore, although no threshold scores were established to identify low/moderate/severe anxiety, this range of scores indicates that a proportion of patients had high levels of dental anxiety (maximum score possible was 40). It is recommended that CBT self-help be offered as a low intensity intervention as part of a stepped care approach for the management of mild to moderate anxiety, and it is recognized that patients with high dental anxiety are likely to require more complex interventions (Newton et al. 2012). Therefore, the inclusion of this group of patients in this study may have underestimated the treatment effectiveness of the guided CBT self-help resource. Thirdly, it is possible that a sampling bias could have influenced the results of the study. For example, it is plausible that the clinicians who volunteered to take part in the current study had a particular interest in the management of dental anxiety. However, a purposive recruitment strategy was employed to ensure that patients and professionals from a diverse range of backgrounds, and with a diverse range of experiences, were represented within the research.
Finally, it should be recognized that the CBT self-help resource was piloted in a community salaried dental service and a hospital pediatric dentistry clinic. Consequently, while general dental practitioner’s acceptability of the CBT self-help resource was explored within the current study, the feasibility of implementing the intervention in a primary dental care setting was not evaluated. Therefore, future evaluations would need to evaluate the CBT resources in different dental settings. A large proportion of adults who complete therapist-led CBT for dental anxiety go on to receive dental treatment without the need for sedation (Kani et al. 2015). However, future research is needed to investigate the possible longstanding benefits of this guided self-help CBT intervention and examine whether the use of this approach can improve children’s future engagement with dental services, reduce referrals to specialist services, and decrease reliance on pharmacological interventions for the management of dental anxiety.
Conclusion
The CBT self-help resource appears to be a feasible and acceptable intervention for the reduction of dental anxiety in children aged 9 to 16 y. The promising findings from this study warrant further evaluation of the resource and thus a randomized, controlled trial is needed to determine the treatment efficacy and cost-effectiveness of this self-help CBT intervention as compared with usual care. If the results of a further trial confirm the effectiveness of this self-help approach, this intervention would provide a viable alternative to the pharmacological management of dental anxiety in children.
Author Contributions
J. Porritt, contributed to conception, design, data acquisition, analysis, and interpretation, drafted and critically revised the manuscript; H. Rodd and A. Morgan, contributed to conception, design, data acquisition, analysis, and interpretation, critically revised the manuscript; C. Williams, contributed to conception, design, and data interpretation, critically revised the manuscript; E. Gupta, contributed to data analysis and interpretation, critically revised the manuscript; J. Kirby, contributed to design and data acquisition, critically revised the manuscript; C. Creswell, T. Newton, K. Stevens, and S. Baker, contributed to conception, design, and data interpretation, critically revised the manuscript; S. Prasad, contributed to design and data acquisition, critically revised the manuscript; Z. Marshman, contributed to conception, design, data analysis, and interpretation, drafted and critically revised the manuscript. All authors gave final approval and agree to be accountable for all aspects of the work.
Acknowledgments
The authors would like to thank the patients and patient representatives who contributed to the design of the study.
Footnotes
This paper presents independent research funded by the National Institute for Health Research (NIHR) under its Research for Patient Benefit (RfPB) Programme (Grant Reference Number PB-PG-1111-26029).
The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health. C.C. is funded by an NIHR Research Professorship (NIHR-RP-2014-04-018). C.W. is the author of a range of CBT-based resources that address anxiety, depression and other mental health problems. These are available commercially as books, cCBT products, and classes. He receives royalties, and is a shareholder and director of a company that commercialized these resources.
The other authors have declared no other competing interests.
References
- Ajzen I. 1991. Theories of cognitive self-regulation. The theory of planned behavior. Organizational Behavior and Human Decision Processes. 50(2):179–211. [Google Scholar]
- Armfield JM, Heaton LJ. 2013. Management of fear and anxiety in the dental clinic: A review. Aust Dent J. 58(4):390–407. [DOI] [PubMed] [Google Scholar]
- Blenkiron P. 1999. Who is suitable for cognitive behavioural therapy? J R Soc Med. 92(5):222–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bower P, Gilbody S. 2005. Stepped care in psychological therapies: Access, effectiveness and efficiency. Brit J Psychiat. 186:11–17. [DOI] [PubMed] [Google Scholar]
- Braun V, Clarke V. 2006. Using thematic analysis in psychology. Qual Res Psychol. 3(2):77–101. [Google Scholar]
- Chavira DA, Stein MB, Bailey K, Stein MT. 2004. Child anxiety in primary care: Prevalent but untreated. Depress Anxiety. 20(4):155–164. [DOI] [PubMed] [Google Scholar]
- Clark JP. 2003. How to peer review a qualitative manuscript. In: Godlee F, Jefferson T, editors. In peer review in health sciences. London: BMJ Books; p. 219–235. [Google Scholar]
- Cohen J. 1992. A power primer. Psychol Bull. 112(1):155–159. [DOI] [PubMed] [Google Scholar]
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. 2008. Developing and evaluating complex interventions: The new medical research council guidance. Brit Med J. 337:a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creswell C, Waite P, Cooper P. 2014. Assessment and management of anxiety disorders in childhood and adolescence. Arch Dis Child. 99:674–678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drummond M. 2001. Introducing economic and quality of life measurements into clinical studies. Ann Med. 33(5):344–349. [DOI] [PubMed] [Google Scholar]
- Furber G, Segal L. 2015. The validity of the child health utility instrument (chu9d) as a routine outcome measure for use in child and adolescent mental health services. Health Qual Life Outcomes. 13:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon D, Heimberg RG, Tellez M, Ismail AI. 2013. A critical review of approaches to the treatment of dental anxiety in adults. J Anxiety Disord. 27(4):365–378. [DOI] [PubMed] [Google Scholar]
- Harris RV, Pender SM, Merry A, Leo A. 2008. Unravelling referral paths relating to the dental care of children: A study in liverpool. Prim Dent Care. 15(2):45–52. [DOI] [PubMed] [Google Scholar]
- Humphris GM, Wong HM, Lee GT. 1998. Preliminary validation and reliability of the modified child dental anxiety scale. Psychol Rep. 83(3 Pt 2):1179–1186. [DOI] [PubMed] [Google Scholar]
- James AC, James G, Cowdrey FA, Soler A, Choke A. 2015. Cognitive behavioural therapy for anxiety disorders in children and adolescents. Cochrane Database Syst Rev. 2:CD004690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kani E, Asimakopoulou K, Daly B, Hare J, Lewis J, Scambler S, Scott S, Newton JT. 2015. Characteristics of patients attending for cognitive behavioural therapy at one U.K. specialist unit for dental phobia and outcomes of treatment. Br Dent J. 219(10):501–506. [DOI] [PubMed] [Google Scholar]
- Kvale G, Berggren U, Milgrom P. 2004. Dental fear in adults: A meta-analysis of behavioral interventions. Community Dent Oral Epidemiol. 32(4):250–264. [DOI] [PubMed] [Google Scholar]
- Lancaster GA, Dodd S, Williamson PR. 2004. Design and analysis of pilot studies: Recommendations for good practice. J Eval Clin Pract. 10(2):307–312. [DOI] [PubMed] [Google Scholar]
- Marshman Z, Morgan A, Porritt J, Gupta E, Baker S, Creswell C, Newton T, Stevens K, Williams C, Prasad S, et al. 2016. Protocol for a feasibility study of a self-help cognitive behavioural therapy resource for the reduction of dental anxiety in young people. Pilot Feasibility Stud. 2:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGoldrick P, Levitt J, De Jongh A, Mason A, Evans D. 2001. Referrals to a secondary care dental clinic for anxious adult patients: Implications for treatment. Br Dent J. 191(12):686–688. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, He JP, Burstein M, Swendsen J, Avenevoli S, Case B, Georgiades K, Heaton L, Swanson S, Olfson M. 2011. Service utilization for lifetime mental disorders in U.S. Adolescents: Results of the national comorbidity survey-adolescent supplement (ncs-a). J Am Acad Child Adolesc Psychiatry. 50(1):32–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore R, Brodsgaard I. 2001. Dentists’ perceived stress and its relation to perceptions about anxious patients. Community Dent Oral Epidemiol. 29(1):73–80. [PubMed] [Google Scholar]
- Morgan A, Rodd H, Porritt J, Baker S, Creswell C, Newton T, Williams C, Marshman Z. 2016. Children’s experience of dental anxiety. Int J Paediatr Dent. doi: 10.1111/ipd.12238. [DOI] [PubMed] [Google Scholar]
- Morgan DL, Ataie J, Carder P, Hoffman K. 2013. Introducing dyadic interviews as a method for collecting qualitative data. Qual Health Res. 23(9):1276–1284. [DOI] [PubMed] [Google Scholar]
- Newton T, Asimakopoulou K, Daly B, Scambler S, Scott S. 2012. The management of dental anxiety: Time for a sense of proportion? Br Dent J. 213(6):271–274. [DOI] [PubMed] [Google Scholar]
- Nicolas E, Bessadet M, Collado V, Carrasco P, Rogerleroi V, Hennequin M. 2010. Factors affecting dental fear in French children aged 5-12 years. Int J Paediatr Dent. 20(5):366–373. [DOI] [PubMed] [Google Scholar]
- O’Cathain A, Hoddinott P, Lewin S, Thomas KJ, Young B, Adamson J, Jansen YJ, Mills N, Moore G, Donovan JL. 2015. Maximising the impact of qualitative research in feasibility studies for randomised controlled trials: Guidance for researchers. Pilot Feasibility Stud. 1:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pace R, Pluye P, Bartlett G, Macaulay AC, Salsberg J, Jagosh J, Seller R. 2012. Testing the reliability and efficiency of the pilot mixed methods appraisal tool (mmat) for systematic mixed studies review. Int J Nurs Stud. 49(1):47–53. [DOI] [PubMed] [Google Scholar]
- Poulton R, Waldie KE, Thomson WM, Locker D. 2001. Determinants of early- vs late-onset dental fear in a longitudinal-epidemiological study. Behav Res Ther. 39(7):777–785. [DOI] [PubMed] [Google Scholar]
- Ritchie J, Spencer L. 1994. Qualitative data analysis for applied policy research. In: Bryman A, Burgess R, editors. Analysing qualitative data. London: Routledge; p. 173–194. [Google Scholar]
- Shahnavaz S, Rutley S, Larsson K, Dahllöf G. 2015. Children and parents’ experiences of cognitive behavioral therapy for dental anxiety – a qualitative study. Int J Paediatr Dent. 25(5):317–326. [DOI] [PubMed] [Google Scholar]
- Stevens KJ. 2010. Working with children to develop dimensions for a preference-based, generic, pediatric, health-related quality-of-life measure. Qual Health Res. 20(3):340–351. [DOI] [PubMed] [Google Scholar]
- Taani DQ. 2002. Dental attendance and anxiety among public and private school children in jordan. Int Dent J. 52(1):25–29. [DOI] [PubMed] [Google Scholar]
- Taani DQ, El-Qaderi SS, Abu Alhaija ES. 2005. Dental anxiety in children and its relationship to dental caries and gingival condition. Int J Dent Hyg. 3(2):83–87. [DOI] [PubMed] [Google Scholar]
- Townend E, Dimigen G, Fung D. 2000. A clinical study of child dental anxiety. Behav Res Ther. 38(1):31–46. [DOI] [PubMed] [Google Scholar]
- Williams C. 2012. Overcoming anxiety, stress and panic: A five areas approach. Boca Raton: Crc Press. [Google Scholar]
- Williams C, Garland A. 2002. A cognitive-behavioural therapy assessment model for use in everyday clinical practice. Adv Psychiatr Treat. 8(3):172–179. [Google Scholar]
- Yardley L, Morrison L, Bradbury K, Muller I. 2015. The person-based approach to intervention development: Application to digital health-related behavior change interventions. J Med Internet Res. 17(1):e30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Y, Cameron E, Forbes G, Humphris G. 2011. Systematic review of the effect of dental staff behaviour on child dental patient anxiety and behaviour. Patient Educ Couns. 85(1):4–13. [DOI] [PubMed] [Google Scholar]