Abstract
Globally, dental caries is one of the most prevalent diseases and is more common in children living in deprived areas. Dental caries is preventable, and guidance in the United Kingdom recommends parental supervised brushing (PSB): a collection of behaviors—including twice-daily toothbrushing with fluoridated toothpaste—that should begin upon eruption of the first tooth (approximately 6 to 12 mo of age) and for which children need to be helped or supervised by an adult until at least 7 y of age. The aim of this study was to explore parents’ experiences of toothbrushing with their young children and to establish barriers and facilitators to PSB at individual, interpersonal, and environmental levels according to the theoretical domains framework. Qualitative semistructured interviews guided by the framework were conducted with 27 parents of young children (<7 y) in 2 deprived areas of the United Kingdom. Framework analysis was used. Parents were not aware of national guidance concerning their active involvement in toothbrushing; however, they did have detailed knowledge of toothbrushing practices for children, and their intentions were to brush their children’s teeth themselves twice every day as part of a family routine. Nonetheless, parents’ difficulties experienced in managing their children’s challenging behavior and the environmental context of their stressful lives meant that many parents adopted a role of simply reminding their children to brush or watching them brush. As such, the main barriers to PSB among parents living in deprived areas were skills in managing their children’s behavior and environmental influences on family life. The results of our study have clear implications for the development of appropriate interventions to address the modifiable barriers to improve parental adoption of PSB.
Knowledge Transfer Statement: The results of this study will be used to develop a behavior change intervention to encourage parental supervised brushing. The intervention—which is likely to be delivered through health practitioners rather than dental teams—will be developed to reduce dental caries among young children and will require evaluation in terms of its clinical and cost effectiveness.
Keywords: dental caries, caregivers, oral health, child - preschool, socio-economic factors, oral hygiene
Introduction
Globally, dental caries is one of the most prevalent diseases, with an estimated 621 million children with untreated caries in their primary teeth, reaching peak prevalence at 6 y of age (Kassebaum et al. 2015). The consequences of dental caries for children include pain, loss of sleep, problems with eating and speaking, and time off from school (American Academy of Pediatric Dentsitry 2014; Gilchrist et al. 2015). The Global Burden of Disease Study 2010 found that in the United Kingdom an average of 2.2 h of children’s healthy life was lost for every child aged 5 to 9 y because of poor oral health. In comparison, the disability associated with vision loss is an average of 1.6 h and for diabetes mellitus 1.5 h (Murray et al. 2013). The financial impact is also significant: treating oral diseases in the National Health Service in England costs £3.4 billion annually (in addition to an estimated £2.3 billion spent in the private sector). Dental extractions under general anesthesia are also costly, with an estimated cost in 2011 to 2012 of around £23 million (Public Health England 2014b). Reducing the prevalence of dental caries in children is a UK public health priority (Department of Health 2012).
The relationship between dental caries and socioeconomic status has been confirmed to be strong and consistent (Schwendicke et al. 2015). The 2013 UK Child Dental Health Survey revealed that 31% of 5-y-olds had obvious caries experience, with wide variation in the proportion affected between children who were of low income and eligible for free school meals (41% of 5-y-olds) and those who were not eligible (29% of 5-y-olds; Pitts et al. 2015). The relationship between ethnicity and dental caries is more complex. Higher levels of dental caries are generally seen in the primary teeth of children of Pakistani, Bangladeshi, and East European origin even after adjusting for socioeconomic status, probably due to diet and oral health behaviors (Conway et al. 2007; Marcenes et al. 2013).
Caries is preventable, and one of the most effective ways of preventing caries is regular toothbrushing with fluoride toothpaste (Marinho et al. 2003). Oral health guidance in the United Kingdom recommends parental supervised brushing (PSB): a collection of behaviors—including twice daily toothbrushing with fluoridated toothpaste—that should begin upon eruption of the first tooth (approximately 6 to 12 mo of age) and for which “children need to be helped or supervised by an adult . . . until at least seven years of age” (Public Health England 2014a; Scottish Intercollegiate Guidelines Network 138 2014). However, reports suggest that this guidance is not being translated into practice, as the most recent national data suggest that a large proportion of UK children (50% of 5-y-olds) brush their teeth without any adult involvement (White et al. 2006). This is a significant problem. Observational studies have found that caries experience at 6 y is strongly associated with low frequency of toothbrushing, late initiation of brushing, and lack of parental involvement in brushing (Duijster et al. 2014).
To develop effective interventions, it is important to identify barriers and facilitators, also referred to as determinants, that parents report as influencing implementation of PSB. A range of barriers have been identified—including lack of knowledge and understanding of the importance of primary teeth, the cost and availability of toothbrushes/toothpaste, difficulty establishing a routine, the influence of family, and managing child behavior (Wong et al. 2005; Amin and Harrison 2009; de Jong-Lenters et al. 2014; Elison et al. 2014; Prowse et al. 2014; Trubey et al. 2015). However, there are some limitations with the research in this area. First, with the exception of a study by Elison and colleagues (2014), PSB has not been the primary focus of previous studies that have examined a range of oral health practices. Of studies specifically on PSB, participants were largely limited to parents of white ethnic origin, children 3 to 6 y, and children without caries, and they tended to be from families of middle to high socioeconomic status. Finally, most studies lack a theoretical framework for exploring determinants of behavior, and this may mean that they fail to consider the full range of influences within the context of PSB.
The theoretical domains framework (TDF; Francis et al. 2012) identifies 12 key domains of behavioral determinants, including knowledge, skills, intentions, goals, social influences, and beliefs about capabilities that are thought to influence behavior. It provides a useful framework for understanding a range of behavioral determinants at different levels of influence (individual, interpersonal, and environmental) and relationships within and across these levels. The TDF has been successfully used to identify important determinants of behavior among health practitioners and members of the public (Francis et al. 2012) in contexts including dental behaviors (Bonetti and Clarkson 2010; Gnich et al. 2015), but it has not yet been applied to parents.
The aim of this study was to explore parents’ experiences of toothbrushing with their young children and to establish barriers and facilitators to PSB among those living in deprived areas of the United Kingdom. These barriers and facilitators are described at individual, interpersonal, and environmental levels through the TDF (Francis et al. 2012).
The findings of this study will inform the development of an intervention to address the modifiable barriers to improve parental adoption of PSB.
Methods
Overview
The study involved a qualitative exploration based on semistructured interviews guided by the TDF with parents of young children living in 2 deprived areas of the United Kingdom.
Participants
Parents of children <7 y old from Barnsley or Bradford were invited to participate. Barnsley and Bradford are both in the 10% most deprived local authorities in England. Epidemiologic data suggest a higher prevalence of dental caries in Barnsley and Bradford: the average number of decayed, missing, and filled teeth (d3mft) in 5-y-olds were 1.61 and 1.98, respectively, in 2011 to 2012, as compared with the average of 0.94 in England (Public Health England 2013).
Ethical Approval
Ethical approval was obtained from National Research Ethics Committee, North of Scotland (14/NS/0093).
Recruitment
Participants were purposively sampled through a maximum variation approach to ensure inclusion of the following: parents (or caregivers with parental responsibility) living in deprived areas; of different sexes, ethnicities, and first languages; with children of varied ages and dental attendance patterns, with and without dental caries. These characteristics were based on factors identified in the literature as being influential (Godson and Williams 1996; Sasahara et al 1998; Pani et al 2012; Marcenes et al. 2013; Pitts et al. 2015). Potential participants were identified from previous research projects, children’s centers, and community dental clinics to identify a diverse group of participants who lived in areas of high deprivation. Recruitment continued until saturation was achieved and no new data emerged (Sandelowski 1995).
Thirty-six parents were identified in Bradford from those who had previously participated in research projects. These parents were sent an information sheet and then contacted by a researcher by telephone. Seventeen parents were reached by telephone. Thirteen parents gave initial consent and agreed to participate.
An independent organization that represents the views of the public (Healthwatch Barnsley) was approached to identify children’s centers located in deprived areas of Barnsley that may be amenable to involvement in research. One center agreed to facilitate the interviews and issued participant information sheets to suitable parents. Interviews were arranged at the children’s center for 11 parents wishing to proceed.
Seven parents with children attending the Bradford and Barnsley Community Dental Services were approached by their dentists. They were given brief verbal information about the study and a written information sheet, and they agreed to be contacted by a researcher by telephone. Contact was made with 6 parents by telephone, and 3 agreed to participate.
Reasons for nonparticipation included reluctance to take part in a qualitative interview, being “too busy,” and having family events such as moving or illness.
Procedure
Written informed consent was obtained from all participants, who were asked to self-report their ethnicity per classification of the UK Office for National Statistics. A topic guide based on the TDF was used to identify determinants of behavior, although it was not so rigidly applied as to restrict participants from generating new ideas. Interviews were conducted by 4 trained researchers from different disciplines in either English or Urdu. The topic guide was modified as the interviews progressed in response to evolving findings. Interviews were recorded, transcribed verbatim in English, and made anonymous. Data were collected between June 2014 and February 2015.
Analysis
Qualitative framework analysis was used as guided by the TDF. Framework analysis is a pragmatic approach to qualitative research that draws on both inductive and deductive processes; it is designed to be rigorous and valid and to produce easily interpreted results and readily implemented findings (Ritchie and Spencer 1994). The analysis involved the following stages.
Stage 1: identifying initial themes
First, 5 interviews were conducted, the transcripts read, and notes made independently by 3 researchers (H.J.R., S.M.A., and Z.M.) on the general fit to the TDF, the specific content of each TDF domain, its component constructs, and the data that emerged. These notes were discussed and disagreements resolved before discussion with a fourth analyst (R.R.C.M.). R.R.C.M. and S.M.A. had experience using the TDF.
Stage 2: labeling the data
Each section of these 5 transcripts was labeled independently by 2 researchers (H.J.R. and S.M.A.) with an index number to represent the TDF domain to which the data related and to which of its component constructs. This was discussed with Z.M. and R.R.C.M., and further discussions were held to clarify the boundaries between the domains.
Stage 3: sorting the data by theme
Data with the same index number were brought together by S.M.A. and discussed by 4 analysts (H.J.R., S.M.A., Z.M., and R.R.C.M.).
Stage 4: synthesizing the data
Thematic charts were created for each TDF domain, retaining the context and language used in the data. These thematic charts were discussed (Z.M., S.M.A., H.J.R., R.R.C.M., P.F.D., K.A.G.B.) and modifications made. The remaining interviews were then conducted and transcripts labeled and sorted by Z.M. and S.M.A. Subsequently, interactions among levels (individual, interpersonal, and environmental) and domains and explanations for these interactions were discussed and agreed.
Results
In total, saturation was reached after 27 interviews had been conducted across Bradford and Barnsley. Of the 27 interviews, 13 took place at participants’ homes, 11 at a children’s center, 2 at a research institute, and 1 by telephone. Participants were 22 mothers, 2 fathers, and 3 grandmothers. Of these, 15 were of white British ethnicity, 10 Pakistani, 1 Polish, and 1 Russian. The majority of interviews were conducted in English (n = 23), with the remaining 4 conducted in Urdu. Most participants had >1 child (n = 16) with a third having ≥3 children (n = 9). Twenty-one participants had taken their children to visit the dentist (Table). Based on the postcode and the Index of Multiple Deprivation 2010, the majority (n = 18) lived in the “most deprived” areas of England, 7 in areas categorized as “more deprived,” and 2 in areas of “average” deprivation.
Table.
Characteristics of the Participants from the 2 Settings of Bradford and Barnsley.
| Russian (n = 1) | White British (n = 15) | Polish (n = 1) | Pakistani (n = 10) | ||||
|---|---|---|---|---|---|---|---|
| Age, y | Attended Dentist | Never Attended | Attended Dentist | Attended Dentist | Never Attended | Attended Dentist | Total |
| 0 to 2 | 0 | 1 | 2 | 0 | 2 | 1 | 6 |
| 2 to 4 | 0 | 1 | 8 | 0 | 2 | 3 | 14 |
| 4 to 6 | 1 | 0 | 3 | 1 | 0 | 2 | 7 |
| Total | 1 | 2 | 13 | 1 | 4 | 6 | 27 |
In summary, parents were not aware of national guidance concerning toothbrushing; however, they did have detailed knowledge of toothbrushing practices for children, and their intentions were to brush their children’s teeth twice every day as part of a family routine. However, difficulties experienced managing their children’s challenging behavior and the environmental context of their stressful lives meant that many parents adopted a role of simply reminding their children to brush or watching them brush, but this did not always occur, particularly at busy times of the day and weekends, when routines were not enforced. As a consequence, the extent of the toothbrushing for some children was a “quick brush” of their own front teeth, as parents observed children often missing brushing their “back teeth.”
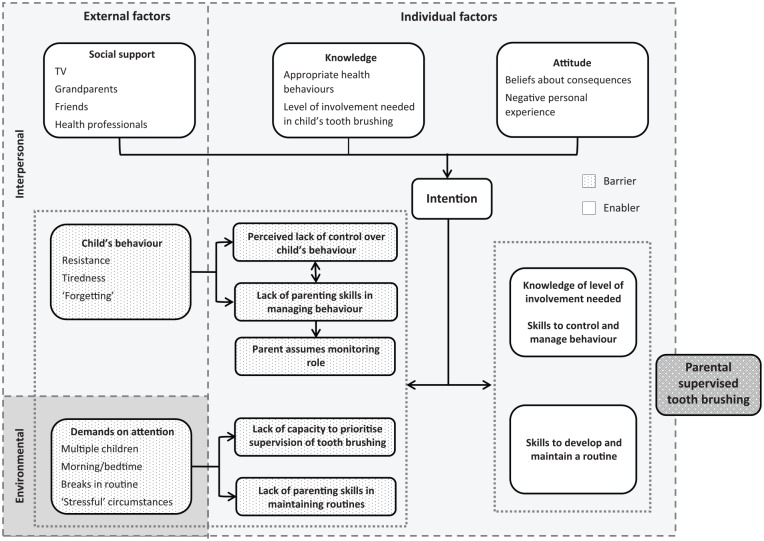
The main barriers and facilitators are summarized in the Figure: the distinctions among the individual, interpersonal, and environmental levels of influence are highlighted and the interactions among domains indicated. Reported barriers and facilitators did not appear to vary by ethnicity.
Figure.
Conceptual diagram of barriers and facilitators of parental supervised brushing.
The detailed results are now described according to the TDF and focused on PSB, with illustrative quotes presented.
Parents’ Knowledge of Toothbrushing
Parents knew that brushing with a fluoride toothpaste was important for good oral health, and they generally had detailed knowledge of appropriate behaviors for young children, including the age at which brushing should commence, frequency of brushing, and use of fluoride toothpaste.
When I think about healthy teeth I think about brushing twice a day and less sugar and no sugar before bedtime. (father of a 3-y-old child)
He were 5 months old when he got his front 2 teeth, so I’ve been doing it since then. (mother of a 4-y-old child)
I use Colgate 0-3 year olds, I read it’s better ’cause it contains fluoride in it. (mother of 3- and 4-y-old children)
This detailed knowledge was therefore an enabling factor at an individual level, although parents were often not aware of the guidance about the need to help their child brush until 7 y of age, which represents a barrier to effective PSB.
I don’t think they’ve ever told us that under the age of 7 you should brush your kids teeth—I’ve not been told that by my dentist. (father of a 3-y-old)
Beliefs and Emotions about the Consequences of Poor Oral Health Behaviors and Motivation to Maintain Good Oral Health for Their Children
Parents stated the consequences of not brushing their children’s teeth, including the sequelae of dental caries such as pain, sleepless nights, dental infections, poor appearance of teeth, and the need for dental treatment.
Well they’d just end up rotting and going bad and they’d have more dental appointments. (mother of 3-y-old twins)
Parents described their own negative experiences of these sequelae, particularly about traumatic episodes at the dentist and the dental anxiety that resulted.
I’ll still probably have to go with them to the bathroom to make sure because I know I had a tooth problem and I suffered with it quite a bit so I don’t want my kids to go through the same pain. (mother of 3- and 4-y-old children)
I’ve had a few bad experiences at the dentist so I like to make sure everybody has good teeth. (mother of 4- and 6-y-old children)
Halitosis was an additional consequence described of children not brushing their teeth.
You can actually smell their breath like when they are talking to you and if they’ve not brushed their teeth it really, really smells. (mother of 2- and 4-y-old children)
Parents’ concerns about these consequences resulted in emotions of fear and worry:
I know a lot of people that are absolutely terrified of the dentist. They show lots of things on TV about gum diseases and that’s the main thing I’m actually scared of. (mother of 2- and 4-y-old children)
I worry a lot because of my middle child’s teeth. (mother of a 3-mo-old baby, 3- and 8-y-old children)
These domains acted at an individual level as potential facilitators, motivating parents to want their children to attain good oral health and resulting in an intention to ensure that their children brushed twice daily with a fluoride toothpaste.
Social Influences on Toothbrushing
As illustrated in the previous section, the main sources of external social influences on parents were from the television, particularly from adverts for adult toothpastes. Other social influences came from grandparents. There was variation reported regarding the influence of grandparents, from being positive role models for their grandchildren to being a barrier to PSB when parents tried to insist on toothbrushing being performed in a certain way.
With their grandma and grandad they get away with murder anyway so if they don’t want to brush their teeth they are like why are you forcing them! I can’t say nothing to them, it’s a big family. (mother of 2-, 4-, and 6-y-old children)
Her grandad does, he’s always in the bathroom and he’s always reminding her, he’s brilliant doing his. (mother of a 5-y-old child)
While parents reported not routinely discussing toothbrushing with friends, they did report observing the state of their friends’ children’s teeth and made internal comparisons of their own toothbrushing practices as parents.
My mate was saying about her daughter who’s the same age as mine about 7, and she was saying something about you know if on a day when she’s really busy and the kids are tired she just tells them to go to bed! And I go do you tell them to brush their teeth and she goes no! (mother of a 6-y-old)
Social Role of Parents in Children’s Toothbrushing
Mothers were largely perceived (by both mothers and fathers) to have overall responsibility within the family for children’s toothbrushing practices. While this was a consistent finding, the nature of the toothbrushing practices that parents adopted differed.
’Cause I’m their mum and it’s what mums do! (mother of 3-y-old twins)
Roles varied from those where mothers were actively engaged in the brushing of the children’s teeth themselves (per the national guidance) to those where mothers simply reminded their children to brush or were in the bathroom with them as they brushed. Parenting skills and styles appeared to determine the nature of the role.
My youngest one she’s 3 so I don’t even trust her with the toothbrush, she plays with her toothbrush but when it is brushing time I do the brushing. I would be like you’re not going to get your teddy tonight so I would use other things to encourage her and eventually she realized brushing is not a big deal, just gets done in 2 minutes. (mother of 3- and 7-y-old children)
She likes doing it. She enjoys being sat in the bath and then she likes to brush her teeth. It’s unbelievable to say she’s only 2, she doesn’t like me doing it, she just kicks off, she does what she likes. (mother of a 2-y-old child)
Parental Skills Involved in Toothbrushing and Behavior Regulation
Two types of skills were identified as being important for brushing children’s teeth: manual skills of the individual parent in brushing and interpersonal skills in the management of young children’s behavior, with the latter being the most problematic. Regarding the manual skills of toothbrushing, while some concerns were expressed by parents about hurting their children, especially when starting to brush their teeth as babies, parents generally felt that they had the necessary manual skills to do this.
First, I tell her to open her mouth, and I do the top of the teeth, the bottom row, the top row, then I tell her close your mouth and give me a big smile so she does then I do the front, so all the way around and then I tell her to spit it out and that’s it. (mother of 2- and 4-y-old children, talking about her 4-y-old)
For parents who reported difficulties with toothbrushing, the main barrier appeared to be lack of parenting skills to manage behavior should the children be unwilling. Parents described how they began to brush their children’s teeth as soon as they erupted, but parents noted that they often encountered challenging behavior from children once they reached 18 to 24 mo. Around this age, parents experienced their children 1) crying because they did not want their teeth brushed, 2) keeping their mouths closed to prevent their parents accessing their teeth, or 3) asserting their independence to want to brush their own teeth.
He closes his mouth and he throws a tantrum, I do try quite a few times. (mother of 2- and 4-y-old children, talking about her 2-y-old child)
Really bad tantrums, my 2-year-old. I try to help because he cannot brush his teeth properly, he’ll throw a tantrum, he throws the toothbrush at me, toothpaste at me and just lays on the floor and starts kicking his legs. (mother of 2- and 4-y-old children, talking about her 2-y-old)
At this stage, variation was seen parents’ responses to this behavior. Some parents continued brushing their children’s teeth themselves despite the resistance, and they regulated their children’s behavior by restraint or other techniques, including distraction with songs and the use of rewards or bribery.
He screams and he shouts. I have to hold him really tight and give them a good brush so that’s what I do with him. (mother of 1- and 3-y-old children, talking about her 3-y-old)
Other parents, however, tried to continue brushing their children’s teeth but found their children’s behavior too difficult to regulate and then “admitted defeat,” subsequently adopting a supervisory or monitoring role over their children’s toothbrushing, rather than having an active role in helping brush the teeth themselves per the national guidance.
I’ve tried to do it myself but then he just tenses his mouth shut, so I just leave him to his own devices. (grandmother with parental responsibility for a 3-y-old child)
Parents who adopted a monitoring or supervisory role were aware that the nature of these roles meant that their children spent very little time brushing and often neglected “their back teeth.”
Beliefs about Capabilities in Managing Their Children’s Behaviors
Beliefs about capabilities in managing children’s behavior were typically expressed in terms of ability to “control” children. There was variation in the degree of control: some parents perceived a lack of control over the interpersonal interaction with their children to be a barrier to helping them brush their children’s teeth.
Until she’ll open her mouth, there’s nothing I can do about it. (mother of 3-mo-old baby, 3- and 8-y-old children talking about her 3-y-old)
Other parents believed themselves to be in control:
The younger one I do hers. I brush her teeth in the morning and at night. They’re children you have to do it. Yes, I keep control of all of that. (mother of 1- and 3-y-old children)
The Nature of the Toothbrushing Behaviors, the Role of Memory, and Environmental Contexts
Three domains were interrelated: the nature of the behavior, memory, and environmental context. Parents consistently reported that toothbrushing was a routine behavior for their children:
It’s a night-time and morning thing you do anyway when you wake up, so it automatically goes to brushing your teeth. It’s not something I have to remind them to do; it’s just something they know—even my little one. (father of 2- and 4-y-old children)
However, they did report breaks in the routine and times when their children “forgot” to brush. Breaks in the routine often occurred at weekends, school holidays, and “sleepovers.”
It could be, for example, if friends come over for the night, coming to sleep over, then they just forget about it ’cause getting playing, playing, playing with their friends. (mother of 1-, 5-, and 8-y-old children)
Upon analysis of the instances when participants described “forgetting,” however, these events were typically not a function of memory or indeed a result of individual factors but of interpersonal or environmental influences, such as prioritizing activities (e.g., getting children into bed, eating breakfast, leaving the house for school), particularly for parents who had reported difficulties with their children’s toothbrushing behaviors. It appeared that the times when toothbrushing typically takes place were also especially busy times in family life.
Oh I just leave him sometimes or let him do what he wants to do basically ’cause mornings are busy. (mother of 4- and 6-y-old children talking about the 4-y-old)
Struggle in a sense of sometimes, maybe like, if they’re too tired at night and they’re half asleep and I’m brushing their teeth and they don’t really want to do it. (mother of 3- and 4-y-old children)
In addition, parents described their environment in terms of the “stressful” circumstances in which they lived that made day-to-day life a “struggle”—namely, several young children to look after, unemployment, debt, drug use, single parenthood, and domestic abuse—all of which explain why toothbrushing was understandably not a priority.
My 3 youngest get up and brush their own teeth. But my oldest, he hates his teeth being brushed. He did live at my mums so I don’t know if she’s scared him when she’s been brushing his teeth and that’s put him off. I struggled. (mother of 2-, 3-, 4-, and 5-y-old children)
So as they are getting ready to go out - have a wash, brush their teeth, get dressed, and then go. But when they go to their dad’s, he doesn’t bother, he doesn’t bother with anything so . . . (mother of 3- and 4-y-old children)
Because of my problems I’ve got so many people involved in [the child’s] care. My mum advised me because we care for him together and she does all that side of things. (mother of a 4-y-old child)
Discussion
The main barriers to the implementation of guidance on PSB were interpersonal difficulties of parents managing their children’s behavior within the environmental circumstances in which they lived. The likely consequences of these barriers include reduced duration, frequency, and efficacy of toothbrushing in children. Although the relative contribution of toothbrushing and dietary modification to the overall risk of dental caries is yet to be fully elucidated, the potential to improve implementation of PSB by modifying parents’ behaviors provides a significant opportunity to reduce the prevalence of dental caries in children living in deprived areas. However, as these health behaviors are the result of influences from multiple levels (individual, interpersonal, and environmental), interventions to change behaviors need to be developed to account for these influences.
Previous studies have highlighted the importance of the family in childhood dental caries (Mattila et al. 2000) and parenting skills as being important for PSB (Huebner and Riedy 2010; de Jong-Lenters et al. 2014; Collett et al. 2016). A recent study also observed how parents who lacked the skills to carry out PSB tended to allow their children to brush their own teeth, rather than persist with parental involvement (Collett et al. 2016). However, this literature has tended to 1) focus on the need for PSB to be implemented in the home as a routine behavior (Trubey et al. 2014) or 2) cite poor family functioning (Duijster et al. 2014). The findings from this qualitative study suggest that parents perceive that they have established toothbrushing as an important routine behavior in family life but that the nature of the their involvement is less than optimal because of difficulties managing the behavior of young children. It appears that difficulties are due, not to a lack of memory, but to interpersonal skills to manage the behavior of children as they develop and the environmental influences within the circumstances in which families live. Interventions to promote greater involvement of parents in toothbrushing need to focus on practically supporting them to develop these skills, while acknowledging social, cultural, and environmental contexts (Greenhalgh et al. 2015). Incorporating training in PSB into parenting programs is one approach that would provide this support in a way that avoids “victim blaming” parents (Watt 2007). Worldwide, various group-based parenting programs are run that have been developed on the basis of behavior change theory to provide support to parents within their local communities. Parents suggested that when their children were around 18 to 24 mo, their parental skills were tested; as such, many of the parenting programs are aimed at parents of young children of this age. Further research is needed to develop a PSB intervention that could be incorporated into these programs and to evaluate the impact of the interventions on parents’ involvement in toothbrushing and, ultimately, dental caries prevalence.
The strengths of the study include 1) the diverse sample of parents involved who lived in deprived areas, 2) the recruiting of parents of children with and without caries, 3) the use of the TDF as a theoretical framework, and 4) robust data collection and analysis by a multidisciplinary team. The approach taken to sampling was chosen to include a range of parents, including those of different ethnicities and first languages and those living in deprived areas. This approach was taken owing to the relationship between dental caries and socioeconomic status (Schwendicke et al. 2015), the high prevalence of dental caries in the primary teeth of children of Pakistani or Bangladeshi origin (Conway et al. 2007; Marcenes et al. 2013), and because research has largely been limited to parents of white ethnic origin. Difficulties have been described in engaging South Asian parents in research (Macneill et al. 2013); however, their inclusion was facilitated by links to other research and public health projects and the availability of a trained interviewer who spoke Urdu. In this study, the Index of Multiple Deprivation was used as a composite area–based measure of deprivation; as such, it was not possible to determine the socioeconomic status of parents who participated. However, such deprivation indices have been shown to be sensitive to variations in oral health behaviors and to have a valuable role to examine how features of places and people influence oral health (Locker 2000).
The TDF was used to guide the study, and it resulted in insights not previously identified in earlier studies of PSB. The TDF was used in a study of parents concerning healthy eating (Curtis et al. 2015), and there were similar findings in terms of the central role of the mother in the health behavior, the importance of the interpersonal relationship between parent and child, and the potential for influences from grandparents to be both positive and negative. However, while the use of this framework can be considered a strength of this study, the potential limitations of this approach should also be considered. Concerns have been expressed about the use of the TDF making interviews too focused and restrictive (Francis et al. 2012), although in this case, there was good coverage of data across the domains, which suggests that it was an appropriate choice of theory for this study. During the interviews, data did emerge that were outside the topic guide and TDF, particularly about attendance at the dentist, but this was not judged to be relevant to the aim of the study. Further criticisms include the lack of specified relationships among the domains and the low agreement among those involved in the analysis (Francis et al. 2012). This was not a problem that we encountered. The interviews and data analysis were conducted by several researchers with a range of backgrounds (pediatric dentistry, dental public health, psychology, and health psychology), with discussions held at various stages in the analysis to develop consensus about the content of each domain (particularly where domains appeared to overlap) and to facilitate triangulation.
Conclusion
The results of our study have implications for the development of interventions to improve PSB that recognize the importance of 1) environmental influences, 2) developing parenting skills, and 3) the changing support needed by parents as their children mature. The findings of this study will inform the development of an intervention to improve implementation of guidance on PSB.
Author Contributions
Z. Marshman, contributed to conception, design, data acquisition, analysis, and interpretation, drafted and critically revised the manuscript; S.M. Ahern, contributed to design, data acquisition, analysis, and interpretation, drafted and critically revised the manuscript; R.R.C. McEachan, P.F. Day, contributed to conception, design, data analysis, and interpretation, critically revised the manuscript; H.J. Rogers, contributed to data acquisition and analysis, critically revised the manuscript; K.A. Gray-Burrows, contributed to data analysis and interpretation, critically revised the manuscript. All authors gave final approval and agree to be accountable for all aspects of the work.
Acknowledgments
We thank the parents for taking part. We also thank the Public Health team at Barnsley Metropolitan Borough Council, Healthwatch Barnsley, Bradford and Barnsley Community Dental Services, and Born in Bradford for their help in recruiting participants. We further thank Dr. Francesca Soldani, consultant in pediatric dentistry for Bradford District Care Trust and Rotherham NHS Foundation Trust, for her help with recruitment and Dr. Stephanie Prady for her expertise in health inequalities.
Footnotes
This publication is independent research funded by the National Institute for Health Research. This study is part of the Healthy Children Healthy Families Theme of the NIHR CLAHRC Yorkshire and Humber. The views expressed in this publication are those of the authors and not necessarily those of the National Health Service, the National Institute for Health Research, or the Department of Health.
The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
References
- American Academy on Pediatric Dentistry. 2014. Policy on early childhood caries ECC: classifications, consequences, and preventive strategies. Pediatr Dent. 37(6 Suppl):15–16. [PubMed] [Google Scholar]
- Amin MS, Harrison RL. 2009. Understanding parents’ oral health behaviors for their young children. Qual Health Res. 19(1):116–127. [DOI] [PubMed] [Google Scholar]
- Bonetti D, Clarkson JE. 2010. The challenges of designing and evaluating complex interventions. Community Dent Health. 27(3):130–132. [PubMed] [Google Scholar]
- Collett BR, Huebner CE, Seminario AL, Wallace E, Gray KE, Speltz ML. 2016. Observed child and parent toothbrushing behaviors and child oral health. Int J Paediatr Dent. 26(3):184–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conway DI, Quarrell I, McCall DR, Gilmour H, Bedi R, Macpherson LM. 2007. Dental caries in 5-year-old children attending multi-ethnic schools in Greater Glasgow: the impact of ethnic background and levels of deprivation. Community Dent Health. 24(3):161–165. [PubMed] [Google Scholar]
- Curtis KE, Lahiri S, Brown KE. 2015. Targeting parents for childhood weight management: development of a theory-driven and user-centered healthy eating app. JMIR Mhealth Uhealth. 3(2):e69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Jong-Lenters M, Duijster D, Bruist MA, Thijssen J, de Ruiter C. 2014. The relationship between parenting, family interaction and childhood dental caries: a case-control study. Soc Sci Med. 116:49–55. [DOI] [PubMed] [Google Scholar]
- Department of Health. 2012. Healthy Lives, Healthy People: improving outcomes and supporting transparency. London (England): Department of Health. [Google Scholar]
- Duijster D, Verrips GH, van Loveren C. 2014. The role of family functioning in childhood dental caries. Community Dent Oral Epidemiol. 42(3):193–205. [DOI] [PubMed] [Google Scholar]
- Elison S, Norgate S, Dugdill L, Pine C. 2014. Maternally perceived barriers to and facilitators of establishing and maintaining tooth-brushing routines with infants and preschoolers. Int J Environ Res Public Health. 11(7):6808–6826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francis JJ, O’Connor D, Curran J. 2012. Theories of behaviour change synthesised into a set of theoretical groupings: introducing a thematic series on the theoretical domains framework. Implement Sci. 7:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilchrist F, Marshman Z, Deery C, Rodd HD. 2015. The impact of dental caries on children and young people: what they have to say? Int J Paediatr Dent. 25(5):327–338. [DOI] [PubMed] [Google Scholar]
- Gnich W, Bonetti D, Sherriff A, Sharma S, Conway DI, Macpherson LM. 2015. Use of the theoretical domains framework to further understanding of what influences application of fluoride varnish to children’s teeth: a national survey of general dental practitioners in Scotland. Community Dentist Oral Epidemiol. 43(3):272–281. [DOI] [PubMed] [Google Scholar]
- Godson JH, Williams SA. 1996. Oral health and health related behaviours among three-year-old children born to first and second generation Pakistani mothers in Bradford, UK. Community Dent Health. 13(1):27–33. [PubMed] [Google Scholar]
- Greenhalgh T, Clinch M, Afsar N, Choudhury Y, Sudra R, Campbell-Richards D, Claydon A, Hitman GA, Hanson P, Finer S, et al. 2015. Socio-cultural influences on the behaviour of South Asian women with diabetes in pregnancy: qualitative study using a multi-level theoretical approach. BMC Medicine. 13:120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huebner CE, Riedy CA. 2010. Behavioral determinants of brushing young children’s teeth: implications for anticipatory guidance. Pediatr Dentist. 32(1):48–55. [PMC free article] [PubMed] [Google Scholar]
- Kassebaum NJ, Bernabé E, Dahiya M, Bhandari B, Murray CJ, Marcenes W. 2015. Global burden of untreated caries: a systematic review and metaregression. J Dent Res. 94(5):650–658. [DOI] [PubMed] [Google Scholar]
- Locker D. 2000. Deprivation and oral health: a review. Community Dent Oral Epidemiol. 28(3):161–169. [DOI] [PubMed] [Google Scholar]
- Macneill V, Nwokoro C, Griffiths C, Grigg J, Seale C. 2013. Recruiting ethnic minority participants to a clinical trial: a qualitative study. BMJ Open. 3(4):e002750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcenes W, Muirhead VE, Murray S, Redshaw P, Bennett U, Wright D. 2013. Ethnic disparities in the oral health of three- to four-year-old children in East London. Br Dent J. 215(2):E4. [DOI] [PubMed] [Google Scholar]
- Marinho VC, Higgins JP, Sheiham A, Logan S. 2003. Fluoride toothpastes for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 1:CD002278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattila ML, Rautava P, Sillanpaa M, Paunio P. 2000. Caries in five-year-old children and associations with family-related factors. J Dent Res. 79(3):875–881. [DOI] [PubMed] [Google Scholar]
- Murray CJ, Richards MA, Newton JN, Fenton KA, Anderson HR, Atkinson C, Bennett D, Bernabé E, Blencowe H, Bourne R, et al. 2013. UK health performance: findings of the Global Burden of Disease Study 2010. Lancet. 381(9871):997–1020. [DOI] [PubMed] [Google Scholar]
- Pani SC, Badea L, Mirza S, Elbaage N. 2012. Differences in perceptions of early childhood oral health-related quality of life between fathers and mothers in Saudi Arabia. Int J Paediatr Dent. 22(4):244–249. [DOI] [PubMed] [Google Scholar]
- Pitts NB, Chadwick B, Anderson T. 2015. Children’s Dental Health Survey 2013. Report 2: Dental disease and damage in Children, England, Wales and Northern Ireland. London (England): Health and Social Care Information Centre; http://www.hscic.gov.uk/catalogue/PUB17137/CDHS2013-Report2-Dental-Disease.pdf. [Google Scholar]
- Prowse S, Schroth RJ, Wilson A, Edwards JM, Sarson J, Levi JA, Moffat ME. 2014. Diversity considerations for promoting early childhood oral health: a pilot study. Int J Dent. 2014:175084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Public Health England. 2013. National Dental Epidemiology Programme for England: oral health survey of five-year-old children 2012. A report on the prevalence and severity of dental decay. London (England): Public Health England. [Google Scholar]
- Public Health England. 2014a. Delivering better oral health: an evidence-based toolkit for prevention. 3rd ed. London (England): Public Health England. [Google Scholar]
- Public Health England. 2014b. Local authorities improving oral health: commissioning better oral health for children and young people. An evidence-informed toolkit for local authorities. London (England): Public Health England. [Google Scholar]
- Ritchie J, Spencer L. 1994. Qualitative data analysis for applied policy research. In: Bryman A, Burgess R. editors. Analyzing qualitative data. New York (NY): Routledge; p. 173–194. [Google Scholar]
- Sandelowski M. 1995. Sample size in qualitative research. Res Nurs Health. 18(2):179–183. [DOI] [PubMed] [Google Scholar]
- Sasahara H, Kawamura M, Kawabata K, Iwamoto Y. 1998. Relationship between mothers’ gingival condition and caries experience of their 3-year-old children. Int J Paediatr Dent. 8(4):261–267. [DOI] [PubMed] [Google Scholar]
- Schwendicke F, Dörfer CE, Schlattmann P, Page LF, Thomson WM, Paris S. 2015. Socioeconomic inequality and caries: a systematic review and meta-analysis. J Dent Res. 94(1):10–18. [DOI] [PubMed] [Google Scholar]
- Scottish Intercollegiate Guidelines Network 138. 2014. Dental interventions to prevent caries in children: a national clinical guideline. Edinburgh (Scotland): Scottish Intercollegiate Guidelines Network. [Google Scholar]
- Trubey RJ, Moore SC, Chestnutt IG. 2014. Parents’ reasons for brushing or not brushing their child’s teeth: a qualitative study. Int J Paediatr Dent. 24(2):104–112. [DOI] [PubMed] [Google Scholar]
- Trubey RJ, Moore SC, Chestnutt IG. 2015. Children’s toothbrushing frequency: the influence of parents’ rationale for brushing, habits and family routines. Caries Res. 49(2):157–164. [DOI] [PubMed] [Google Scholar]
- Watt RG. 2007. From victim blaming to upstream action: tackling the social determinants of oral health inequalities. Community Dent Oral Epidemiol. 35(1):1–11. [DOI] [PubMed] [Google Scholar]
- White DA, Chadwick BL, Nuttall NM, Chestnutt IG, Steele JG. 2006. Oral health habits amongst children in the United Kingdom in 2003. Br Dent J. 200(9):487–491. [DOI] [PubMed] [Google Scholar]
- Wong D, Perez-Spiess S, Julliard K. 2005. Attitudes of Chinese parents toward the oral health of their children with caries: a qualitative study. Pediatr Dent. 27(6):505–512. [PubMed] [Google Scholar]