Abstract
Objective/Background
This report presents a superior mesenteric artery (SMA) embolism managed by percutaneous mechanical thrombectomy (PMT).
Methods
A 61 year old woman diagnosed with SMA embolism was admitted. Emboli were found in the middle and distal segments of the SMA on abdominal computed tomography angiography. Under local anaesthesia, a 6 F Rotarex system was used to remove the emboli via left brachial artery access. Emboli were successfully removed and patency was restored to the SMA and its branches.
Results
Post-operatively, the patient's symptoms were significantly relieved. No post-operative complications were observed and no discomfort was documented during follow-up.
Conclusion
Endovascular treatment of SMA embolism using PMT is a feasible and alternative option.
Keywords: Acute mesenteric ischaemia, Embolism, Endovascular treatment, Percutaneous mechanical thrombectomy, Superior mesenteric artery
Highlights
-
•
A patient with superior mesenteric artery (SMA) embolism was managed by endovascular treatment.
-
•
The emboli in the SMA were successfully removed using percutaneous mechanical thrombectomy.
-
•
Symptoms were relieved quickly and significantly.
Introduction
Acute mesenteric ischaemia (AMI) is an acute, critical disease caused by loss of the mesenteric circulation. Owing to the insidious onset and rapid development of AMI and because there have been no breakthroughs in the clinical diagnosis or treatment, the prognosis of AMI is very poor. The overall mortality rate can reach 60–80%.1 The main pathogenesis of AMI is superior mesenteric artery (SMA) embolism, accounting for approximately 40–50% of cases.2 Emboli most frequently originate in the heart and are common in patients with atrial fibrillation.3 The early diagnosis and treatment of AMI is crucial to its prognosis. Delayed treatment might lead to intestinal ischaemia and necrosis.4 Traditional treatment has mainly been confined to open or laparoscopic thrombectomy. With the development of endovascular techniques, methods of percutaneous catheter directed thrombolysis and mechanical thrombectomy have been gradually adopted. The present paper reports the treatment of SMA embolism with percutaneous mechanical thrombectomy (PMT).
Case Report
After experiencing the sudden onset of 12 hours of abdominal pain, a 61 year old woman was admitted to Beijing Friendship Hospital, Beijing, China. The patient had a history of hypertension, diabetes mellitus, coronary heart disease, and atrial fibrillation. Physical examination indicated slight abdominal distension, no gastrointestinal peristalsis, obvious tenderness around the navel and lower abdomen with mild rebound tenderness, no muscle tension, no shifting dullness, and the absence of bowel sounds. There were no obvious abnormalities in the vital signs, and body temperature was normal, however an electrocardiogram revealed atrial fibrillation. Contrast abdominal computed tomography (CT) angiography (CTA) showed a filling defect in the middle and distal segments of the SMA (Fig. 1). The results of laboratory tests, including white blood cell count, haemoglobin, and tests for liver and kidney function were normal. According to the pre-operative examination, there were no signs of intestinal necrosis. PMT was performed the same day as an emergency procedure. Informed consent was obtained from the patient before surgery.
Figure 1.

Contrast enhanced abdominal computed tomography angiography revealed a filling defect in the middle and distal segments of the superior mesenteric artery.
Surgical technique
Under local anaesthesia, left brachial artery access was established with a 5 F sheath. Next, a guidewire and an angiographic catheter were inserted into the abdominal aorta. Angiography revealed the emboli were in the mid-distal area of the SMA, but that its branches were normal (Fig. 2). After administration of heparin (50 mg intravenously [IV]), a 90 cm 6 F sheath was inserted into the abdominal aorta to replace the 5 F sheath, and a vertebral catheter was passed into the SMA. Then, the long sheath was placed into the proximal SMA. A 0.018″ guidewire was placed in the SMA through the thrombus, reaching the distal end. Along the guidewire, a 6 F Rotarex system (Straub Medical, Wangs, Switzerland) was inserted to the target lesion and the emboli were removed (Fig. 3). After withdrawing the Rotarex, a repeat angiogram indicated that the original thrombus was removed and that blood flow was normal (Fig. 4). After slowly injecting urokinase (250,000 IU via sheath), a vascular closure device (Starclose; Abbott Vascular, Temecula, CA, USA) was used to seal the brachial access. The operation was successful, and the patient had no adverse reactions.
Figure 2.
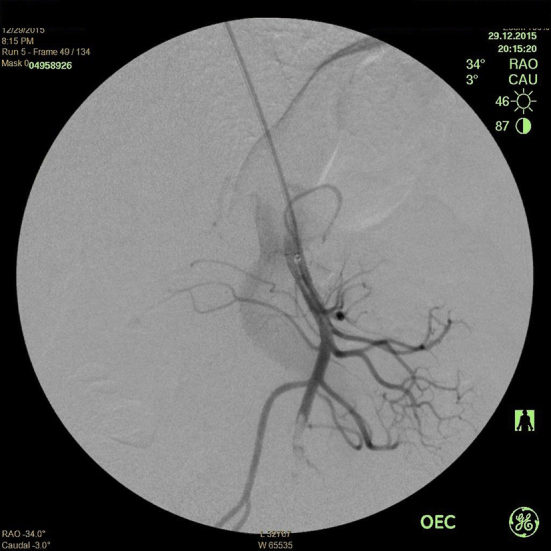
Angiography showed an embolism of the superior mesenteric artery.
Figure 3.

Operating with a 6 F Rotarex system.
Figure 4.

After the procedure, angiography showed that the original thrombus was completely removed.
Results
Post-operatively, the patient had stable vital signs and received a regimen of low molecular weight heparin sodium (Clexane, Sanofi, Paris, France; 60 mg IV twice daily) for anticoagulant therapy; alprostadil (10 μg IV daily) for vasodilator therapy; antibiotics; and parenteral nutrition. Abdominal pain was relieved significantly after the procedure. Physical examination carried out 12 h post-operatively indicated normal body temperature, soft abdomen, mild tenderness around the navel, and no rebound tenderness or muscle tension. White cell count, haemoglobin, and liver and kidney function were normal. The patient's flatulence and defecation were restored on days 2 and 5 post-operatively, respectively. Five days later, the patient began to eat normally. One week post-operatively, re-examination via enhanced abdominal CTA showed that the SMA and its branches were normal and patent (Fig. 5). The patient was discharged 10 days post-operatively, and took aspirin (100 mg daily) and warfarin (3 mg daily) orally. During a 6 month follow-up period, the patient had no complaints of discomfort; normal eating, flatulence, and defecation; and no bleeding reactions.
Figure 5.
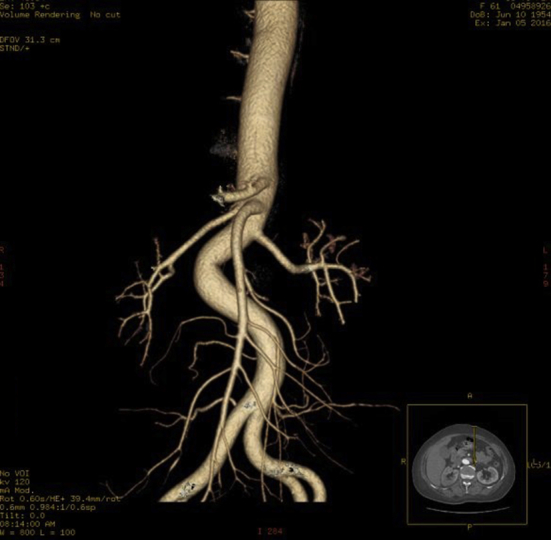
Abdominal three dimensional reconstruction of the superior mesenteric artery and its branches indicated blood flow patency.
Discussion
SMA embolism is the most common cause of AMI; this affliction has a rapid onset and lacks obvious clinical features in the early stage. The characteristics of the abdominal pain and the development of symptoms are similar to those of other acute abdominal conditions, which often leads to delay in treatment. Thus, early diagnosis is critical. When the acute abdominal symptoms of patients do not match the signs and laboratory test results, the possibility of AMI should be considered, especially when these symptoms occur in the presence of atrial fibrillation, arteriosclerosis, blood coagulation abnormalities, and other circulatory diseases. Once AMI is suspected, enhanced CT should be performed as soon as possible. The development of multislice CT diagnostic techniques promotes a more timely diagnosis. Given the advantages of speed and non-invasiveness, and the ability to simultaneously diagnose other acute abdominal conditions, CT has gradually replaced angiography. In addition, CT examination can also show intestinal wall oedema, free abdominal gas, fluid, and other signs, providing important evidence for treatment.5, 6
Early diagnosis and prompt treatment can restore blood flow through the SMA to prevent the progression of intestinal ischaemia. When there is no clear evidence of intestinal necrosis, endovascular treatment can be used to substitute open surgery as the preferred method of treatment.7, 8 Endovascular treatment has the advantages of minimal invasiveness, fewer post-operative complications, and lower mortality rates than open surgery.8, 9, 10 Arthurs et al. reported that patients with AMI receiving endovascular treatment and undergoing open surgery had mortality rates of 36% and 50%, respectively.7 Currently, the primary methods of endovascular treatment include catheter directed thrombolysis, percutaneous angioplasty, percutaneous thrombectomy and aspiration.11 Catheter directed thrombolysis uses an infusion catheter to inject intraluminally urokinase and other thrombolytic drugs into the target vessels. However, the drugs dissolve the thrombus with low efficiency that are not able to dissolve the clots quickly, so the prolonged treatment can cause intestinal ischaemia to develop.12 In addition, it is necessary to be alert to the occurrence of intestinal haemorrhage in thrombolytic therapy, which is not suitable for patients with contraindications to thrombolytic therapy. Angioplasty and stenting are used as a supplementary treatment of residual stenosis after thrombolysis to restore the lumen morphology and to reduce the recurrence rate. PMT breaks down the thrombi by mechanical means and removes the thrombi with aspiration. The advantages of PMT lie in the rapid clearance of the thrombi, no or reduced use of thrombolytic drugs after the operation, minimal invasiveness, and a low complication rate. Recently, it was reported that the Rotarex and Aspirex system was applied to successfully treat SMA embolism.12, 13
The present case was confirmed to be acute SMA embolism due to sudden abdominal symptoms, previous history of atrial fibrillation, and a CT diagnosis. In addition, there were no signs of peritonitis or intestinal necrosis by physical examination, laboratory tests, or CT. These conditions indicated an early stage of AMI, which made endovascular treatment rather than open surgery, possible. It was decided to perform PMT because it could remove the emboli and restore the circulation of the bowel rapidly compared with catheter directed thrombolysis. The other reason was that the embolism only involved the main trunk of the SMA, making it possible to suction all the emboli. The operative access should be determined by the SMA anatomy before the procedure. In this case, the SMA originated from the abdominal aorta at an acute angle; therefore, the brachial artery approach was chosen. When operating, the possibility of PMT induced vessel rupture should be considered, especially during application in small diameter vessels, which may have serious consequences. If rupture occurs during the procedure, covered stent or coil embolisation is feasible,13 while open surgery should also be prepared for. Therefore, it is advisable to choose a low profile system, maintain a good support with the guidewire, and to avoid rotating branches. Distal embolisation is another possible PMT complication. After thrombectomy, injecting urokinase through the catheter can dissolve distal microemboli, and it is thus possible to avoid distal embolisation.
Conclusion
To date, the application of PMT in treating AMI has not been well documented. Owing to the late introduction of PMT equipment and the high cost of surgery, the clinical application of PMT is greatly limited. To the authors' knowledge, this case may be the first report in China of the treatment of a patient with SMA embolism with a Rotarex. Although this is only one case report, according to the results of previously reported cases,12, 13 along with the present results, PMT could be an effective option for the treatment of acute SMA embolism.
Conflict of Interest
None.
Funding
None.
References
- 1.Bradbury A.W., Brittenden J., McBride K., Ruckley C.V. Mesenteric ischaemia: a multidisciplinary approach. Br J Surg. 1995;82:1446–1459. doi: 10.1002/bjs.1800821105. [DOI] [PubMed] [Google Scholar]
- 2.Acosta S. Epidemiology of mesenteric vascular disease: clinical implications. Semin Vasc Surg. 2010;23:4–8. doi: 10.1053/j.semvascsurg.2009.12.001. [DOI] [PubMed] [Google Scholar]
- 3.Stanley J.C. Mesenteric arterial occlusive and aneurysmal disease. Cardiol Clin. 2002;20:611–622. doi: 10.1016/s0733-8651(02)00067-x. [DOI] [PubMed] [Google Scholar]
- 4.Inderbitzi R., Wagner H.E., Seiler C., Stirnemann P., Gertsch P. Acute mesenteric ischaemia. Eur J Surg. 1992;158:123–126. [PubMed] [Google Scholar]
- 5.Yun W.S., Lee K.K., Cho J., Kim H.K., Huh S. Treatment outcome in patients with acute superior mesenteric artery embolism. Ann Vasc Surg. 2013;27:613–620. doi: 10.1016/j.avsg.2012.07.022. [DOI] [PubMed] [Google Scholar]
- 6.Menke J. Diagnostic accuracy of multidetector CT in acute mesenteric ischemia: systematic review and meta-analysis. Radiology. 2010;256:93–101. doi: 10.1148/radiol.10091938. [DOI] [PubMed] [Google Scholar]
- 7.Arthurs Z.M., Titus J., Bannazadeh M., Eagleton M.J., Srivastava S., Sarac T.P. A comparison of endovascular revascularization with traditional therapy for the treatment of acute mesenteric ischemia. J Vasc Surg. 2011;53:698–704. doi: 10.1016/j.jvs.2010.09.049. [DOI] [PubMed] [Google Scholar]
- 8.Block T.A., Acosta S., Björck M. Endovascular and open surgery for acute occlusion of the superior mesenteric artery. J Vasc Surg. 2010;52:959–966. doi: 10.1016/j.jvs.2010.05.084. [DOI] [PubMed] [Google Scholar]
- 9.Schermerhorn M.L., Giles K.A., Hamdan A.D., Wyers M.C., Pomposelli F.B. Mesenteric revascularization: management and outcomes in the United States, 1988–2006. J Vasc Surg. 2009;50:341–348. doi: 10.1016/j.jvs.2009.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Raupach J., Lojik M., Chovanec V., Renc O., Strýček M., Dvořák P. Endovascular management of acute embolic occlusion of the superior mesenteric artery: a 12-year single-centre experience. Cardiovasc Intervent Radiol. 2016;39:195–203. doi: 10.1007/s00270-015-1156-6. [DOI] [PubMed] [Google Scholar]
- 11.Acosta S., Björck M. Modern treatment of acute mesenteric ischaemia. Br J Surg. 2014;101:e100–e108. doi: 10.1002/bjs.9330. [DOI] [PubMed] [Google Scholar]
- 12.Popovic P., Kuhelj D., Bunc M. Superior mesenteric artery embolism treated with percutaneous mechanical thrombectomy. Cardiovasc Intervent Radiol. 2011;34:67–69. doi: 10.1007/s00270-010-9921-z. [DOI] [PubMed] [Google Scholar]
- 13.Kuhelj D., Kavcic P., Popovic P. Percutaneous mechanical thrombectomy of superior mesenteric artery embolism. Radiol Oncol. 2013;47:239–243. doi: 10.2478/raon-2013-0029. [DOI] [PMC free article] [PubMed] [Google Scholar]


