Abstract
Aims
To examine parental concerns about child growth and factors that drive parents’ decisions whether to intervene medically with their child’s height.
Methods
Parents of 9- to 14-year-old pediatric primary care patients of various heights, oversampled for those with short stature, participated in exploratory focus groups and nominal group technique sessions. Growth concerns expressed by the groups were incorporated into a survey, completed by 1,820 parents, and rated for their degree of impact on medical decision-making. Ordinal logistic regression modeled concern scores against parent traits. Explanatory focus groups clarified the survey results.
Results
Research team consensus and factor analysis organized the 22 distinct concerns expressed by the parent groups into 7 categories. Categories rated as having the greatest influence on parental decision-making involved: treatment efficacy and side effects, child health and psychosocial function. Level of concern was highly associated with parental education and parenting style.
Conclusion
Psychosocial issues are influential, but parental decision-making is most impacted by concerns about treatment and child health. By discussing the real risks and benefits of hormone treatment and addressing parents’ perceptions of what is needed for physical and psychosocial health, clinicians can be highly effective educators to assure that treatment is used only as medically indicated.
Keywords: Growth, Short children, Clinical decision-making, Parent, Growth hormone treatment
Introduction
Because short stature is not a disease, multiple medical and psychosocial factors influence management decisions. Guidelines proposed thus far for the evaluation of children with short stature are based mostly on clinical experience and theoretical considerations [1]; evidence supporting what constitutes the best subspecialist referral strategies is lacking, with controversy persisting over medical necessity, optimal criteria, cost effectiveness and outcomes of evaluation and intervention [2, 3]. The absence of clear, evidence-based guidelines leaves room for greater influence by nonmedical factors on management decisions. Gender, racial and sociodemographic disparities have been documented in the diagnostic evaluation, subspecialist referral and growth hormone (GH) treatment of children with short stature [4–6], lending credence to the notion that nonmedical considerations impact stature-related management decisions.
Parents and clinicians share in the medical decision-making. Evidence shows that the degree of parental concern influences rates of both subspecialist referral by primary care providers [7] and prescription of GH by endocrinologists [8–10] independent of objective measures of the child’s growth. A study aimed at understanding the parents’ role in medical decision-making used conjoint analysis and six attributes of ‘growth augmentation therapy’ selected by the investigators as pertinent to parental preferences [11].
To learn what influences the decisions of parents who do not, as well as of those who do, seek medical care for a short child, we studied parents of patients from primary care settings. We used a mixed qualitative-quantitative approach to explore the breadth of concerns that may lead parents to seek medical care for a short child, and to determine each concern’s relative importance to parental decision-making. We also sought to understand which parental traits were associated with their concerns about child growth.
Subjects and Methods
The study was granted exemption by the Institutional Review Board of the Children’s Hospital of Philadelphia (CHOP; IRB protocol No. 10-007612). A 4-phase, mixed qualitative-quantitative method allowed parents to explore, prioritize and explain their concerns about child growth. This approach was similar to the ‘teen-centered method’ and ‘parent-centered method’ previously applied to exploring factors that influence adolescents’ interactions with the health care system [12, 13] and parents’ perceptions of factors affecting diabetes management for their children [14]. Table 1 summarizes the study method, subject recruitment and participants in each phase.
Table 1.
Study design: a mixed qualitative-quantitative approach
| Phase Activity | Objective | Subject recruitment | Number of sessions | Number of parents | |
|---|---|---|---|---|---|
| White | Black | ||||
| 1 Exploratory focus groups | To explore the broad range of factors that influence the decision | Phone calls to parents from a randomized list of children of any height, aged 9–14 years, from 9 primary care pediatric offices | 13 | 31 | 40 |
| 2 Nominal group technique | To generate and prioritize key factors that influence the decision; to populate the survey | 10 | 39 | 24 | |
| 3 One-time survey | To allow for subgroup and regression analyses | In-person convenience sampling of parents of children (of any height and age) at 4 primary care pediatric offices | 1,820 surveys completed | 733 | 856 |
| 4 Explanatory focus groups | To explain why and how the key factors influence the decision | Same as in phases 1 and 2 | 12 | 38 | 39 |
Participants and Study Design
Parents of randomly selected children of any height, aged 9–14 years, from 9 pediatric primary care offices were recruited to participate in the first 2 phases of the study (table 1). Phase 1 involved 13 exploratory focus groups, in which parents were prompted by open-ended questions to express in their own words the issues and their underlying meanings that affect their willingness to seek specialist care and treatment for a short child. While exploratory focus groups provide breadth and depth of ideas, discussions often focus on the most timely or emotionally charged issues, even though more mundane ones actually may play a greater role in parental decision-making. Thus, phase 2 consisted of 10 nominal group technique sessions in which parents were asked: ‘If you had a child with short stature, what factors most affect the likelihood that you would seek specialist care and GH treatment?’ After each group volunteered the list of pertinent factors, they were asked to anonymously provide (i.e. write on a card) the top 10 reasons, ranked by priority. Tabulation of these rankings provided the most salient factors for the group as a whole, and was used to populate the survey of phase 3.
The first 2 phases focused on parents of 9- to 14-year-old patients because the peripubertal period is the time of greatest patient-family concern about growth and the age at which gender-based disparities in subspecialist referral for short stature become evident [5]. The parent groups were stratified by race (entered into their child’s electronic health record at a clinical encounter according to parent self-classification), but were not limited by patient gender, to capture a greater breadth of ideas. To ensure the inclusion of views of parents of short children, recruitment oversampled (i.e. 3–4 of the 10–12 participants for each group) parents of children with height <10th percentile. The groups were not isolated by height status, because group discussions by all parents of short children may serve to raise parental anxiety about their child’s health and health care, while discussions by all parents of nonshort children may not elicit fruitful information as height may not have been a concern for them. Because no identifying information or patient height data was collected during the sessions, the relative group attendance by parents of short versus nonshort children remains unknown. Similarly, although the anonymity required by the design of the parent groups precluded the collection of sociodemographic data, the groups were recruited from urban and nonurban practices to try to capture a variety of social perspectives.
Nonmedical personnel facilitated all parent groups to avoid influencing, even subconsciously, parent comments. The moderators were trained in group dynamics and facilitation techniques to make every participant feel equally comfortable with sharing their thoughts and to prevent a dominant or swaying participant from carrying away the group discussion. The moderators used a standard script developed by the research team. Transcripts were analyzed by 2 investigators (A.G. and P.C.) for themes, which were presented to the entire research team for further analysis and development of the next study phase.
Growth concerns expressed by the parent groups were incorporated into the quantitative survey of phase 3. The survey, available in English or Spanish, was completed anonymously during summer 2012 by parents of children evaluated at 4 pediatric primary care offices (2 urban and 2 nonurban) affiliated with a tertiary care pediatric hospital. Recruitment was conducted without regard to height or age of the children, and different pediatric practices were selected to prevent contamination of the survey results by parents who may have participated in the previous group discussions. Full details of the subject recruitment and methodologies of the first 3 phases were reported previously [15]. The fourth phase included 12 explanatory focus groups, composed of parents recruited from the same population used for the first 2 phases and designed to explore the meanings and ramifications of the survey results. Like in the first 2 phases, nonmedical facilitators trained in the study techniques moderated the explanatory focus groups by using a standard script developed by the entire research team.
Survey Creation
In addition to questions about sociodemographic background, respondent height and their children’s growth, the survey included questions to identify the parenting style of the respondent. The parenting style was determined using a short version of the Parenting Dimensions Inventory (PDI-S) [16], an 11-item, self-administered instrument that assesses control, support and structure in a general parenting context. The 2 scales, nurturance and amount of control, are part of the longer PDI [17] and were used to classify parents into one of 4 groups based on the work of Baumrind [18] and Maccoby and Martin [19]: authoritative (high nurturance, high control), authoritarian (low nurturance, high control), indulgent (high nurturance, low control) and uninvolved (low nurturance, low control).
To better understand parental concerns about height, the survey asked: ‘Parents vary in how much medical care they seek for their children, such as getting testing and treatment. Imagine you have a short child (even if you don’t have one in real life). How much of an impact would each of the following issues make on your decision whether to do something medical for that child’s height?’ This was followed by a list of the distinct concerns expressed by parents in the first 2 study phases. Using a 5-point Likert scale, respondents scored the degree of impact that each concern would have on their medical decision-making.
The survey was beta-tested on parents of patients in the outpatient diabetes clinic and translated into Spanish, as previously described [15].
Data Collection and Analyses
Survey data were managed using REDCap (Research Electronic Data Capture; Vanderbilt University, Nashville, Tenn., USA) tools hosted at CHOP. Probabilistic samples of randomly selected surveys (10% of the 1,820 surveys) were manually reviewed to test the fidelity of the data entry. Concern scores were excluded from analysis as unreliable if a respondent had selected all of the same answer to each of the concern questions (n = 237; 13% of 1,820 total).
Research team consensus and confirmatory factor analysis of the survey responses organized the distinct concerns expressed by the parent groups into categories. The mean Likert score of the individual concerns within each category was calculated as the summary score for that category. The ordinal logistic regression modeling of each concern category score by respondent traits was then analyzed. Survey results were statistically analyzed using JMP software (SAS Institute Inc., Cary, N.C., USA), whereas transcripts from the parent groups were analyzed qualitatively using NVivo software (2008; QSR International, Melbourne, Vic., Australia).
Results
Survey Respondent Characteristics
The surveys were completed by 1,820 of the 2,185 parents approached (83% response rate). Females composed 87% of both the parents approached and the survey respondents. The surveys were collected in practices located in nonurban (51%) and urban (49%) areas, and 7% were completed in Spanish. The respondent characteristics were described previously in detail [15]. Of note, the highest educational level completed by the respondents was a master’s or doctorate degree for 21%, a college degree for 29%, some college education for 15%, graduation from high school for 20% or trade school for 9%, and partial high school for 6%. Thirteen percent of the respondents indicated that they were concerned that at least one of their children was too short, and of those respondents, 7% (about 1% of all survey respondents) reported that they had a child who was treated with GH. This prevalence was consistent with the FDA’s approved indication for GH treatment of idiopathic short stature (ISS), defined as a height below −2.25 SD (i.e. the shortest 1.2% of the population). The respondent characteristics were further categorized into each of the 4 parenting styles (table 2).
Table 2.
Percentages of respondents, by trait, that were categorized into each parenting style group
| Respondent traits | Parenting style (n = 1,554)1
|
p value1 | |||
|---|---|---|---|---|---|
| uninvolved (n = 250) |
indulgent (n = 167) |
authoritarian (n = 657) |
authoritative (n = 480) |
||
| Gender | <0.0001 | ||||
| Female | 15 | 11 | 42 | 33 | |
| Male | 26 | 11 | 43 | 20 | |
|
| |||||
| Race/ethnicity | <0.0001 | ||||
| Asian | 28 | 12 | 41 | 20 | |
| Black or African-American | 12 | 7 | 48 | 34 | |
| White or Caucasian | 18 | 15 | 36 | 31 | |
| Hispanic or Latino | 24 | 10 | 45 | 21 | |
| Other | 16 | 12 | 44 | 28 | |
|
| |||||
| Chosen survey language | 0.0013 | ||||
| English | 16 | 11 | 42 | 32 | |
| Spanish | 31 | 13 | 48 | 8 | |
|
| |||||
| Primary care practice | 0.0026 | ||||
| Nonurban (2 sites) | 17 | 13 | 41 | 29 | |
| Urban (2 sites) | 15 | 8 | 44 | 33 | |
|
| |||||
| Highest level of education completed | <0.0001 | ||||
| Partial high school | 22 | 3 | 45 | 30 | |
| High school graduate | 15 | 6 | 49 | 30 | |
| Trade school graduate | 8 | 7 | 50 | 36 | |
| Partial college | 14 | 10 | 46 | 30 | |
| College graduate | 17 | 10 | 42 | 31 | |
| Master’s or doctorate degree | 19 | 20 | 30 | 31 | |
|
| |||||
| Current employment status | 0.0264 | ||||
| Full time (>35 h/week) | 18 | 11 | 40 | 32 | |
| Part time | 15 | 12 | 45 | 28 | |
| Unemployed | 17 | 6 | 48 | 29 | |
| Homemaker | 15 | 13 | 41 | 30 | |
| Student | 9 | 16 | 42 | 33 | |
| Retired | 15 | 0 | 77 | 8 | |
| Disabled | 11 | 5 | 38 | 46 | |
| Other | 12 | 8 | 23 | 58 | |
|
| |||||
| Total annual household income | 0.0002 | ||||
| Less than USD 25,000 | 17 | 7 | 45 | 30 | |
| USD 25,000–49,999 | 14 | 7 | 47 | 32 | |
| USD 50,000–74,999 | 14 | 12 | 44 | 30 | |
| USD 75,000–99,999 | 12 | 14 | 42 | 32 | |
| USD 100,000–149,999 | 14 | 14 | 38 | 34 | |
| USD 150,000 or more | 23 | 17 | 32 | 28 | |
|
| |||||
| Insurance | 0.0022 | ||||
| Private | 16 | 13 | 41 | 30 | |
| Government | 14 | 7 | 45 | 34 | |
| Self-pay | 23 | 12 | 42 | 23 | |
|
| |||||
| Number of children living in household | 0.0215 | ||||
| 0 | 20 | 9 | 52 | 18 | |
| 1 | 16 | 13 | 37 | 34 | |
| 2 | 17 | 11 | 41 | 32 | |
| 3 or 4 | 14 | 9 | 49 | 28 | |
| 5 or more | 16 | 2 | 61 | 20 | |
|
| |||||
| Concerned that at least one of their children was too short | 0.0488 | ||||
| No | 15 | 11 | 43 | 32 | |
| Yes | 22 | 12 | 38 | 27 | |
Pearson’s χ2 test was performed to examine the association between each respondent trait and parenting style by univariable analysis.
These values are based on the highest number of responses collected for each variable. The total number ranged from 1,503 to 1,554.
Parental Concerns
The parent groups expressed 22 distinct concerns that could influence a parent’s decision to seek medical care for a short child, which were organized into 7 categories by research team consensus and confirmatory factor analysis. Table 3 lists all 7 categories with their specific survey items and illustrative parent comments from the explanatory groups in phase 4 of this study. Figure 1 shows the proportion of parents who rated each concern category as having a big or extreme impact on their decision to take medical action for a child’s short stature. Treatment characteristics and health were the 2 concern categories that were the most important drivers of decisions to seek treatment; they were different from all other categories (p < 0.0001; using the Bowker test for symmetry).
Table 3.
Seven categories of 22 distinct concerns raised by parents regarding a short child (illustrative comments from parent explanatory groups provide further insight into the specific concerns)
| Category | Distinct concern (specific survey item) | Illustrative comments from explanatory groups |
|---|---|---|
| Treatment characteristics | Whether the available treatment has been researched and what were the results. Concerns about side effects or fear of possible outcomes from available treatment. |
|
| Health | Health issues are causing the child’s short height. The child’s short height is causing health issues. The child is experiencing physical pain or discomfort as a result of their short height. The child’s doctor or nurse believes the child’s height may be a problem. |
|
| Psychosocial functioning | The child’s behavior has changed (feeling depressed, acting out). The child is bothered or concerned about their own height. The child is experiencing bullying or teasing. The child is treated differently than their peers because of their height. The child feels isolated or withdrawn from their peers as a result of their height. The child is not able to participate in activities with peers (such as playing sports, going on amusement park rides). The parent wants the child to be well adjusted and have a positive body image. |
|
| Physical appearance | The child is a ‘midget’ or a ‘dwarf’. The child’s growth is disproportionate (different body parts are growing at different rates). |
|
| Adult success | The child’s height would change the child’s behavior, happiness or fulfillment during adulthood. The child’s short height would limit the child’s career choice as an adult. |
|
| Comparison | The child’s growth chart percentile or their pattern on the growth chart may be worrisome. The child’s height is short compared to their peers. |
|
| Cultural/demographic features | The family’s religious beliefs. Whether the child is a boy or a girl. The child’s race or ethnicity. |
|
Fig. 1.
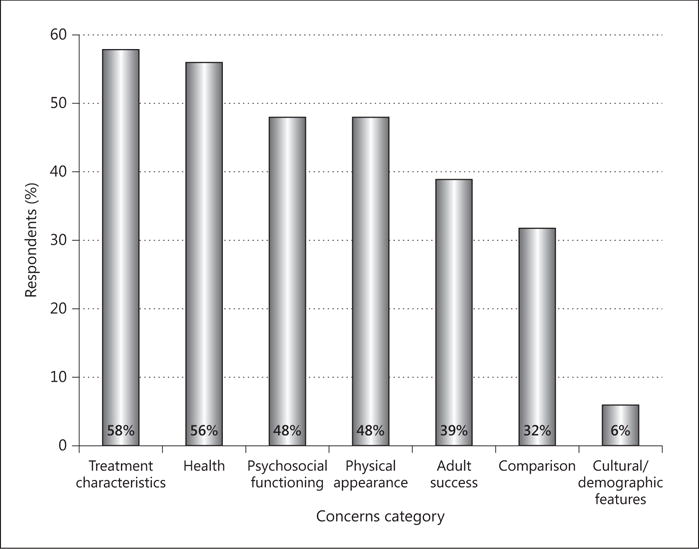
Percentages of parents who rated each concern category as having a big or extreme impact on their decision to seek medical care for a child’s short stature.
The level of impact on their decision-making that was ascribed by the respondents to each of the concern categories was related to the respondents’ traits (table 4). Educational level and parenting style had the strongest significance levels and were significant factors in the models for the greatest number of concern categories. For all 6 concern categories where educational level and parenting style were significant explanatory variables in the model, respondents with higher educational backgrounds and those with high nurturance (indulgent or authoritative parenting styles) were more likely to rate the concerns as having a greater impact on their decision to seek medical care for a short child.
Table 4.
Logistic regression modeling of each concern category score by respondent traits
| Traits | Concern categories
|
||||||
|---|---|---|---|---|---|---|---|
| treatment characteristics | health | psychosocial functioning | physical appearance | adult success | comparison to others | cultural/demographic features | |
| Respondent’s gender | 0.0338 | ||||||
| Race/ethnicity | 0.0287 | 0.0034 | 0.0356 | 0.0443 | 0.0060 | ||
| Spanish language | 0.0170 | ||||||
| Pediatric practice | 0.0005 | 0.0019 | 0.0011 | 0.0060 | 0.0456 | ||
| Educational level | <0.0001 | <0.0001 | 0.0002 | <0.0001 | <0.0001 | 0.0048 | |
| Employment status | 0.0002 | ||||||
| Total household annual income | 0.0010 | 0.0056 | 0.0032 | ||||
| Medical insurance | 0.0208 | ||||||
| Number of children living in the household | |||||||
| Respondent’s height | |||||||
| Concern about the height of respondent’s own child(ren) | 0.0359 | 0.0115 | |||||
| Parenting style | <0.0001 | <0.0001 | 0.0001 | 0.0018 | 0.0021 | 0.0145 | |
Only significant p values on modeling are shown.
Discussion
The Institute of Medicine identified 6 traits as aspects of quality in health care, including patient-centered care, defined as ‘care that is respectful of and responsive to individual and patient preferences, needs and values’ and that ensures ‘that patient values guide all clinical decisions’ [20, 21]. This study’s parent-centered, mixed qualitative-quantitative approach drew upon the collective wisdom and experience of parents of primary care patients, rather than the assumptions of clinician investigators, to determine the pertinent factors for quantitative study. In so doing, this method captured a richer breadth of factors that were likely to more accurately reflect what parents consider in their decision-making regarding medical intervention for a child’s short stature. The survey further allowed the concerns to be ranked along their importance to parental decision-making, for both the population and sociodemographic subgroups. It identified educational level and parenting style as the 2 parent traits most clearly associated with parental concerns about child growth.
Treatment characteristics (i.e. proven efficacy and side effect risks) and growth-related health issues were the 2 categories rated by parents as those that would most strongly influence their decision to seek medical care for a child’s short stature. This has several ramifications for clinicians. First, in discussions with parents, it is important for clinicians to clearly distinguish between GH replacement for GH deficiency and pharmacologic GH treatment, such as for ISS, as the two clinical scenarios pose different risk-benefit considerations. Untreated GH deficiency has been associated with altered body composition (increased adiposity, decreased lean muscle mass), decreased bone mineralization, unfavorable plasma lipid and lipoprotein profiles and increased cardiovascular morbidity and mortality [22]. Thus, GH replacement for patients with GH deficiency provides health benefits beyond height. In other scenarios, GH treatment is pursued solely for height augmentation, either in a child with a health condition associated with short stature proven responsive to GH (e.g. Turner syndrome) or a healthy short child (i.e. ISS).
Like treatment benefits, safety considerations are also nuanced. Although GH has a generally safe profile [23], recent conflicting data from a European consortium study of adults who had been treated with GH in childhood (SAGhE) highlight our lack of definitive knowledge about the long-term safety effects from pediatric GH treatment (recombinant GH has been available only since 1985) [24–26]. As parents in our exploratory focus groups explained, parents often turn to the Internet for information about GH, in preparation for and/or as supplementation to their discussions with their children’s physicians [27]. A content analysis of websites related to GH and children revealed underreporting of risks and costs of treatment, via complete omission (39% of the websites for each) or downplaying [27]. With such biased information serving as a trusted resource, it is particularly incumbent upon clinicians to appropriately and adequately educate patient families so they can make properly informed decisions. To summarize these points, considering GH treatment is a nuanced decision best made with a clinician armed with medical knowledge and sensitive to parents’ spoken and unspoken concerns.
Parents rated concerns about the impact of short stature on psychosocial function as also strongly influencing their medical decision-making. Multiple studies found associations between tallness and markers of social and financial success [28], particularly for males [29], including in the realms of mating/dating, workplace, academia, politics and military [30–33]. Despite the social pressures on short individuals demonstrated, other studies countered that short stature does not preclude normal psychosocial adjustment in children or adults [34]. Similarly, some argue that many studies overestimate the impact of short stature on psychosocial outcome due to methodological flaws [35]. Consistent with these latter arguments, respondent height was not associated with concern scores in our study; the degree of parental adjustment precludes a direct relationship between parent height and their level of concern.
The appropriateness of GH treatment for healthy short children has been argued extensively in the literature [36–38] and likely will continue to be. Previous studies tried to determine whether short stature has a clinically significant impact on psychosocial health or function. Perhaps it is time to reframe the question: what are the factors, perceived or real, that drive some families to seek medical care for short stature? Clearly, psychosocial concerns influence height-related parental decision-making, since, in our survey, 48% of the respondents selected psychosocial function (current, in childhood) and 39% selected adult success (i.e. future psychosocial function) as having a big or extreme impact on their decision. Likewise, from the four US pediatric GH registries, 18% of GH recipients were treated for the ISS indication, which is purely for psychosocial reasons [39].
Almost half of respondents selected physical appearance as an important factor in their height-related decision-making. We were surprised by the use of the terms ‘midget’ and ‘dwarf’ by parents in the first 2 phases of our study, but due to the frequency with which the words were uttered, we felt compelled to incorporate them as an item in our survey, and afterwards to explicitly ask parents in the explanatory focus groups what is meant by those terms. The unifying concepts shared by parents, as evoked by those terms, were that they are pejorative and should no longer be used, but that they were a ready shorthand in referring to growth failure that is clearly due to an underlying medical condition and not just an extreme variant of healthy short stature. Likewise, disproportionate growth was unambiguously abnormal. Parents felt it would be important to seek medical care for these conditions, for health and pain reasons (some believed the joints must be painful on walking) more so than height. Of note, the salience of this category may reflect media influence, as the television shows Little People, Big World and The Little Couple aired during the study period.
The comparison category, relating child height to the growth chart, peers or family, was a more modest influence on parental decision-making. It highlighted the importance of contextual cues in raising parental concern, and the arbitrary nature of defining an ‘abnormal’ threshold in considering a continuous physical trait like height.
Only 6% of the survey respondents rated cultural/demographic features, including patient gender, race/ethnicity and family religious beliefs, as having a big or extreme impact on their height-related medical decision-making, although they featured more prominently during the parent group discussions. For example, multiple parents volunteered comments that an intervention would be ‘worth it’ for a boy but not a girl, thereby identifying patient gender as a direct modifier of their decision-making. Similarly, spirituality distinguished African-American from White parent group discussions, as the former frequently included comments that height was divinely ordained and, thus, to be accepted without tampering.
Regression modeling of the parent scores for each concern category revealed that of the respondent traits analyzed, parenting style and educational level were most strongly associated with greater concern. The influence of these factors on the concern scores may reflect differential attitudes about short stature and child rearing, medical access as well as awareness or knowledge about health care. Parents who were indulgent or authoritative responded more strongly to the various growth-related concerns – perhaps not surprisingly, since those are the more child-centered (high nurturance) parenting styles. Likewise, on our survey, higher educational level was associated with greater concern scores, consistent with a previous report that parents seeking endocrinology care for short children in a mid-sized, ethnically diverse US city had a higher educational background than the surrounding population [10]. Studies of patient preferences for involvement in medical decision-making found that people with a higher educational level tended to take a more active role in decision-making [40].
Despite the power of the mixed qualitative-quantitative method for revealing parent concerns, there were several limitations. Although a variety of situations may lead parents to be concerned about their child’s height, the questions and subsequent categories created by the research team were developed from insight of parents of children of various ages and heights who may or may not have had any previous experience seeking medical care for their child’s height. While this approach allowed us to capture ideas also representing parents of short children who decide against seeking medical care, the subgroup of parents who do seek subspecialist care may have heightened or altered concerns. For example, from clinical experience, several parents have sought GH treatment because they personally knew someone whose son was benefiting from GH and they did not want their own son to miss out on the opportunity, a concern not raised by the primary care population studied here. Response bias, the desire to give the socially preferred answer, may have been operant as another limitation. For example, multiple parents in the explanatory focus groups were surprised that only 6% of the survey respondents gave strong ratings to the cultural/demographic features category. As one parent offered: ‘People aren’t going to admit that in a survey’. Participant bias may seem like a third limitation, in that 87% of our survey respondents were female. However, 87% of the parents approached were female, reflecting the greater tendency for mothers to accompany their children to their primary care appointments. Fathers may have a behind-the-scenes role in family medical decision-making, which we could not capture.
Conclusions
There are many reasons why a parent may be sufficiently concerned about a child’s short height to seek medical attention. As the USA are moving towards value-and science-driven health care, this study provides insights to aid clinicians in enhancing the patient-centeredness, and hence quality, of care given to children and their families who are concerned about short stature. More specifically, clinicians should listen carefully to the patients’ and parents’ concerns and provide adequate, accurate information about the potential benefits and risks of treatment to allow them to participate in proper medical decision-making.
Acknowledgments
This work was supported by grants 1R01 HD57037 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD; A.G.) and UL1TR000003 from the National Center for Advancing Translational Sciences (NCATS; A.J.C.) of the National Institutes of Health (NIH). We want to thank the network of primary care clinicians, their patients and the families for their contribution to this project and clinical research facilitated through the Pediatric Research Consortium (PeRC) at the Children’s Hospital of Philadelphia, funded in part by the Agency for Healthcare Research and Quality. We also want to thank our research assistants Catherine Callo, Oni Hawkins and Jane Kovacs for recruiting parents to complete the surveys, and our focus group moderators Charles Adams, P.C., Kevin Gralewski, Stephen Oliver and Denise Outlaw. We are grateful to Thomas G. Power, PhD, Professor of Human Development at Washington State University, for allowing us to use his PDI-S in the survey and for his guidance and support in analyzing the data collected from the PDI-S.
Footnotes
An abstract of our data was presented at the Joint Meeting of the International Society of Endocrinology and the Endocrine Society (ICE/ENDO) 2014 in Chicago, Ill., USA.
Disclosure Statement
A.G. had a research grant for an investigator-initiated project from Genentech Inc. that ended in November 2012, and currently serves on the Steering Committee for the Pfizer International Growth Study Database. P.C., A.J.C., T.H.L. and K.R.G. have nothing to declare.
References
- 1.Oostdijk W, Grote FK, de Muinck Keizer-Schrama SM, Wit JM. Diagnostic approach in children with short stature. Horm Res. 2009;72:206–217. doi: 10.1159/000236082. [DOI] [PubMed] [Google Scholar]
- 2.Craig D, Fayter D, Stirk L, Crott R. Growth monitoring for short stature: update of a systematic review and economic model. Health Technol Assess. 2011;15:iii–iv. 1–64. doi: 10.3310/hta15110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sisley S, Trujillo MV, Khoury J, Backeljauw P. Low incidence of pathology detection and high cost of screening in the evaluation of asymptomatic short children. J Pediatr. 2013;163:1045–1051. doi: 10.1016/j.jpeds.2013.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grimberg A, Feemster KA, Pati S, Ramos M, Grundmeier R, Cucchiara AJ, Stallings VA. Medically underserved girls receive less evaluation for short stature. Pediatrics. 2011;127:696–702. doi: 10.1542/peds.2010-1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grimberg A, Kutikov JK, Cucchiara AJ. Sex differences in patients referred for evaluation of poor growth. J Pediatr. 2005;146:212–216. doi: 10.1016/j.jpeds.2004.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grimberg A, Stewart E, Wajnrajch MP. Gender of pediatric recombinant human growth hormone recipients in the United States and globally. J Clin Endocrinol Metab. 2008;93:2050–2056. doi: 10.1210/jc.2007-2617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cuttler L, Marinova D, Mercer MB, Connors A, Meehan R, Silvers JB. Patient, physician, and consumer drivers: referrals for short stature and access to specialty drugs. Med Care. 2009;47:858–865. doi: 10.1097/MLR.0b013e31819e1f04. [DOI] [PubMed] [Google Scholar]
- 8.Silvers JB, Marinova D, Mercer MB, Connors A, Cuttler L. A national study of physician recommendations to initiate and discontinue growth hormone for short stature. Pediatrics. 2010;126:468–476. doi: 10.1542/peds.2009-3609. [DOI] [PubMed] [Google Scholar]
- 9.Hardin DS, Woo J, Butsch R, Huett B. Current prescribing practices and opinions about growth hormone therapy: results of a nationwide survey of paediatric endocrinologists. Clin Endocrinol (Oxf) 2007;66:85–94. doi: 10.1111/j.1365-2265.2006.02691.x. [DOI] [PubMed] [Google Scholar]
- 10.Finkelstein BS, Singh J, Silvers JB, Marrero U, Neuhauser D, Cuttler L. Patient attitudes and preferences regarding treatment: GH therapy for childhood short stature. Horm Res. 1999;51(suppl 1):67–72. doi: 10.1159/000053138. [DOI] [PubMed] [Google Scholar]
- 11.Singh J, Cuttler L, Shin M, Silvers JB, Neuhauser D. Medical decision-making and the patient: understanding preference patterns for growth hormone therapy using conjoint analysis. Med Care. 1998;36(suppl):AS31–AS45. doi: 10.1097/00005650-199808001-00005. [DOI] [PubMed] [Google Scholar]
- 12.Ginsburg KR, Alexander PM, Hunt J, Sullivan M, Zhao H, Cnaan A. Enhancing their likelihood for a positive future: the perspective of inner-city youth. Pediatrics. 2002;109:1136–1142. doi: 10.1542/peds.109.6.1136. [DOI] [PubMed] [Google Scholar]
- 13.Ginsburg KR, Slap GB, Cnaan A, Forke CM, Balsley CM, Rouselle DM. Adolescents’ perceptions of factors affecting their decisions to seek health care. JAMA. 1995;273:1913–1918. [PubMed] [Google Scholar]
- 14.Ginsburg KR, Howe CJ, Jawad AF, Buzby M, Ayala JM, Tuttle A, Murphy K. Parents’ perceptions of factors that affect successful diabetes management for their children. Pediatrics. 2005;116:1095–1104. doi: 10.1542/peds.2004-1981. [DOI] [PubMed] [Google Scholar]
- 15.Cousounis PA, Lipman TH, Ginsburg K, Cucchiara AJ, Grimberg A. How short is too short according to parents of primary care patients. Endocr Pract. 2014;20:1113–1121. doi: 10.4158/EP14052.OR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hood B, Power T, Hill L. Children’s appraisal of moderately stressful situations. Int J Behav Dev. 2009;33:167–177. [Google Scholar]
- 17.Slater MA, Power TG. Multidimensional assessment of parenting in single-parent families. In: Vincent JP, editor. Advances in Family Intervention, Assessment, and Theory. 4. Greenwich: JAI; 1987. p. 197. [Google Scholar]
- 18.Baumrind D. Effects of authoritative parental control on child behavior. Child Dev. 1966;37:887–907. [Google Scholar]
- 19.Maccoby E, Martin J. Socialization in the context of the family: parent-child interaction? In: Hetherington EM, editor. Handbook of Child Psychology. 4. New York: Wiley; 1983. [Google Scholar]
- 20.Institute of Medicine; Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington: National Academies Press; 2001. [Google Scholar]
- 21.Maizes V, Rakel D, Niemiec C. Integrative medicine and patient-centered care. Explore (NY) 2009;5:277–289. doi: 10.1016/j.explore.2009.06.008. [DOI] [PubMed] [Google Scholar]
- 22.Lanes R. Metabolic abnormalities in growth hormone deficiency. Pediatr Endocrinol Rev. 2004;2:209–215. [PubMed] [Google Scholar]
- 23.Allen DB. Safety of growth hormone treatment of children with idiopathic short stature: the US experience. Horm Res Paediatr. 2011;76(suppl 3):45–47. doi: 10.1159/000330159. [DOI] [PubMed] [Google Scholar]
- 24.Carel JC, Ecosse E, Landier F, Meguellati-Hakkas D, Kaguelidou F, Rey G, Coste J. Long-term mortality after recombinant growth hormone treatment for isolated growth hormone deficiency or childhood short stature: preliminary report of the French SAGhE study. J Clin Endocrinol Metab. 2012;97:416–425. doi: 10.1210/jc.2011-1995. [DOI] [PubMed] [Google Scholar]
- 25.Sävendahl L, Maes M, Albertsson-Wikland K, Borgström B, Carel JC, Henrard S, Speybroeck N, Thomas M, Zandwijken G, Hokken-Koelega A. Long-term mortality and causes of death in isolated GHD, ISS, and SGA patients treated with recombinant growth hormone during childhood in Belgium, the Netherlands, and Sweden: preliminary report of 3 countries participating in the EU SAGhE study. J Clin Endocrinol Metab. 2012;97:E213–E217. doi: 10.1210/jc.2011-2882. [DOI] [PubMed] [Google Scholar]
- 26.Poidvin A, Touzé E, Ecosse E, Landier F, Béjot Y, Giroud M, Rothwell PM, Carel JC, Coste J. Growth hormone treatment for childhood short stature and risk of stroke in early adulthood. Neurology. 2014;83:780–786. doi: 10.1212/WNL.0000000000000737. [DOI] [PubMed] [Google Scholar]
- 27.Cousounis P, Lipman TH, Ginsburg KR, Grimberg A. Internet informs parents about growth hormone. Horm Res Paediatr. 2013;80:86–91. doi: 10.1159/000351463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Deaton A, Arora R. Life at the top: the benefits of height. Econ Hum Biol. 2009;7:133–136. doi: 10.1016/j.ehb.2009.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hall SS. Size Matters: How Height Affects the Health, Happiness, and Success of Boys – and the Men They Become. Boston: Houghton Mifflin; 2006. [Google Scholar]
- 30.Stulp G, Mills M, Pollet TV, Barrett L. Nonlinear associations between stature and mate choice characteristics for American men and their spouses. Am J Hum Biol. 2014;26:530–537. doi: 10.1002/ajhb.22559. [DOI] [PubMed] [Google Scholar]
- 31.Judge TA, Cable DM. The effect of physical height on workplace success and income: preliminary test of a theoretical model. J Appl Psychol. 2004;89:428–441. doi: 10.1037/0021-9010.89.3.428. [DOI] [PubMed] [Google Scholar]
- 32.Hensley WE. Height as a measure of success in academe. Psychol J Hum Behav. 1993;30:40–46. [Google Scholar]
- 33.Tuvemo T, Jonsson B, Persson I. Intellectual and physical performance and morbidity in relation to height in a cohort of 18-year-old Swedish conscripts. Horm Res. 1999;52:186–191. doi: 10.1159/000023459. [DOI] [PubMed] [Google Scholar]
- 34.Lee JM, Appugliese D, Coleman SM, Kaciroti N, Corwyn RF, Bradley RH, Sandberg DE, Lumeng JC. Short stature in population-based cohort: social, emotional, and behavioral functioning. Pediatrics. 2009;124:903–910. doi: 10.1542/peds.2008-0085. [DOI] [PubMed] [Google Scholar]
- 35.Bullinger M, Kolttowska-Häggström M, Sandberg D, Chaplin J, Wollmann H, Noeker M, Brütt AL. Health-related quality of life of children and adolescents with growth hormone deficiency or idiopathic short stature – part 2: available results and future directions. Horm Res. 2009;72:74–81. doi: 10.1159/000232159. [DOI] [PubMed] [Google Scholar]
- 36.Allen DB, Cuttler L. Clinical practice. Short stature in childhood – challenges and choices. N Engl J Med. 2013;368:1220–1228. doi: 10.1056/NEJMcp1213178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bolt LL, Mul D. Growth hormone in short children: beyond medicine? Acta Paediatr. 2001;90:69–73. doi: 10.1080/080352501750064905. [DOI] [PubMed] [Google Scholar]
- 38.Sandberg DE, Colsman M. Growth hormone treatment of short stature: status of the quality of life rationale. Horm Res. 2005;63:275–283. doi: 10.1159/000086593. [DOI] [PubMed] [Google Scholar]
- 39.Grimberg A, Huerta-Saenz L, Grundmeier R, Ramos MJ, Pati S, Cucchiara AJ, Stallings VA. Gender bias in US pediatric growth hormone treatment. Sci Rep. 2015;5:11099. doi: 10.1038/srep11099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Say R, Murtagh M, Thomson R. Patients’ preference for involvement in medical decision making: a narrative review. Patient Educ Couns. 2006;60:102–114. doi: 10.1016/j.pec.2005.02.003. [DOI] [PubMed] [Google Scholar]


