Abstract
Specific amino acids within the V3 loop of HIV-1 CRF01_AE envelope glycoprotein that are involved in the interaction with CCR5/CXCR4 coreceptors, are not well characterized. We generated V3 mutants using polymerase chain reaction (PCR)-based site-directed mutagenesis of HIV-1 CRF01_AE R5-env plasmids at specific positions. Mutant viruses were produced by env-pseudotyped virus assay, tested for coreceptor usage using U373.R5 and U373.X4 cells, and viral entry was assessed with luciferase activity measurement. All viruses, harboring either single or double mutations, used the CCR5 coreceptor. However, those containing a single substitution at positions 7, 11, 18, and 32 and those with mutations at positions 5/32 and 18/32 had reduced infectivity. Only virus with arginine substitution at position 11 seemed to be involved in CXCR4 coreceptor usage. Our results suggest that some V3 positions may be necessary for the binding to coreceptor, but not for the switch of coreceptor usage.
Keywords: : HIV-1, CRF01_AE, V3, coreceptor usage, CCR5
Introduction
Human Immunodeficiency Virus type 1 (HIV-1) enters target cells following interactions of the envelope glycoprotein (gp120) with CD4 cellular receptor and coreceptors, in particular CCR5 or CXCR4.1–3 Based on the use of coreceptor, HIV-1 variants are classified as CCR5 tropic (R5), CXCR4 tropic (X4), and dual/mixed tropic (D/M) viruses.4 The third variable region (V3 loop) of HIV-1 envelope is important for interaction with coreceptors5,6 and specific V3 amino acids and total of net charge are essential to the coreceptor interaction (CCR5 and/or CXCR4).7,8 Several studies based on HIV-1 subtype B and C suggested that alterations in V3 region, including insertions or mutations on either side of the base, stem, or crown, selectively mediated the coreceptor usage and only a few amino acid changes within V3 region are needed for virus to switch from using CCR5 to CXCR4.9–16 Moreover, Svicher et al. showed that beyond the classical positions 11, 24, and 25, other V3 genetic determinants can modulate HIV-1 subtype B CCR5 or CXCR4 coreceptor usage.17
In a previous study, we developed the Support Vector Machine combined with a feature selector using Logistic Model Trees (SVM/LMT) to predict the coreceptor usage of HIV-1 CRF01_AE viruses.18 Nine specific positions (5, 7, 11, 13, 14, 18, 19, 27, and 32) in V3 sequences were identified as involved in prediction of CCR5 or CXCR4 usage. However, the role of these selected positions in coreceptor interaction of CRF01_AE viruses needed to be validated in a phenotypic assay. We present, in this study, the analysis of the effect of different amino acid substitutions at these selected positions on the interaction with CCR5 or CXCR4 coreceptor.
Materials and Methods
Selection of mutants
Nine positions within the V3 loop were identified from our previous study: 5, 7, 11, 13, 14, 18, 19, 27, and 32.18 Moreover, Random Forest based model was also selected as a classifier since it is nonparametric, interpretable, efficient, and offers high predictive performance, especially in many problems of protein function predictions.19,20 It was used to classify the coreceptor usage of HIV-1 CRF01_AE, select, and rank important positions within the V3 loop. The specific positions provided by this model were 5, 6, 7, 11, 12, 18, 22, 27, and 32 that can differentiate CCR5 and CXCR4 coreceptor usage (unpublished data). Combining both models, we identified the positions of interest for this study. They were positions 5, 7, 11, 12, 18, 27, and 32.
The mutant amino acids were chosen based on their frequency among the sequences of CXCR4-using CRF01_AE strains available in the Los Alamos HIV Sequence Database. The nine single mutations selected were S5Y, N7K, S11R, T12V, T12F, Q18R, I27V, I27T, and S32R. All possible double mutations combining the single mutations were created and led to 34 patterns. Among them, seven double mutations predicted by the SVM/LMT method to confer CXCR4 usage were selected.
Prediction of coreceptor usage
All single and double V3 mutations were assessed for typical features of X4 viruses based on different methods, including 11/25 rule,7 net charge rule,8 and two free genotypic tools (Geno2pheno[coreceptor], and PSSM [both R5X4 and SINSI matrices], http://coreceptor.geno2pheno.org and https://indra.mullins.microbiol.washington.edu/webpssm, respectively).
V3 site-directed mutagenesis
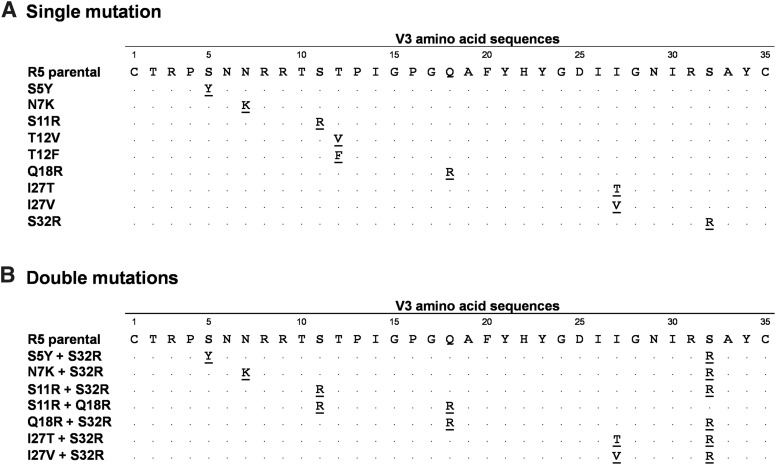
The parental env gene (R5) was previously selected from the viral quasispecies of an HIV-1-infected patient (patient ID: HDR932), and cloned in the expression vector PCI. It was previously determined as CCR5-using with a phenotypic assay based on env-pseudotyped virus (unpublished data). The GenBank reference number of the HIV-1 CRF01_AE env sequence (R5 parental sequence; wild-type [WT] sequence) is KU994848. Mutants at positions 5, 7, 11, 12, 18, 27, and 32 were obtained by site-directed mutagenesis using mutagenic primers (Eurogentec, Belgium). We designed 16 patterns of mutations involving either one position or two positions (Fig. 1). DNA fragments containing the desired mutation were amplified by polymerase chain reaction (PCR) with the Phusion® High-Fidelity DNA polymerase (New England BioLabs, MA) using two nonoverlapping 5′-phosphorylated primers. PCR were performed in a total reaction volume of 50 μl as follows: denaturation at 98°C for 30 s; 30 cycles at 98°C for 10 s, 50°C for 30 s, 72°C for 2.5 min; and final extension at 72°C for 10 min. Following amplification, the DNA products were treated with 10 units DpnI (New England BioLabs, MA) for 1 h at 37°C to digest the parental template. The DNA products were then purified and 100 ng were ligated to themselves by using T4 DNA ligase (New England BioLabs, MA) at 4°C overnight. The ligation products were transformed into ElectroMAX™ DH5α-E™ cells (Invitrogen, CA) by electroporation and spread on LB medium with ampicillin. Ten to 20 single colonies were analyzed by V3 sequencing to confirm the mutation at selected positions. A single colony was selected to isolate the plasmid DNA and to produce the mutant viruses.
FIG. 1.
V3 amino acid sequences of mutants with (A) single mutation or (B) double mutations. Positions in V3 are identified by the number above the R5 parental (WT) sequence. The dots mean that amino acid is similar to the amino acid present in the R5 parental (WT) sequence. Mutations are identified by the bold and underlined amino acid letter codes. WT, wild type.
Cells
The 293T cells were maintained in Dulbecco's modified Eagle's medium (DMEM) supplemented with 10% fetal bovine serum (FBS) and 1% penicillin–streptomycin (ATB). U373.R5 and U373.X4 cells were maintained in DMEM medium supplemented with 10% FBS, 1% ATB, 10 μg/ml puromycin, and 100 μg/ml hygromycin B.
Determination of viral coreceptor utilization
Mutant viruses were tested for coreceptor usage using U373 cells expressing either CCR5 or CXCR4. The plasmids containing single or double V3 mutations were cotransfected with pNL4.3Δenv.Luc plasmid backbone into 293T cells to produce mutant viruses. Cell-free supernatants were collected 72 h posttransfection and viral production was determined by quantification of p24 protein using the INNOTEST® HIV Antigen mAb (INNOGENETICS, Belgium). U373.R5 or U373.X4 cells were seeded in 96-well plates at the density of 14,000 cells/well 1 day prior infection. On the following day, the monolayers, about 70% confluent, were infected with mutant viruses (10 ng of p24). After 48 h, the viral entry was assessed by measuring the luciferase activity (as relative light units [RLUs]) using Bright-Glo™ Luciferase Assay System (Promega), according to the manufacturer's instructions. All infections were performed in triplicate. The WT virus, or parental virus, was also tested for coreceptor usage. HIV-1 LEA21 was used as CCR5-using virus positive control and NL4-3 as CXCR4-using virus positive control. Cells not infected with HIV-1 were used as negative control. The cutoff for positivity was defined as two times greater than the mean background of the U373 cells, measured on negative controls in all experiments. Coreceptor usage was determined as the RLU detected in U373 cells.
Statistical analysis
The infectivity was expressed in the mean Log RLU of luciferase activity in U373.R5 and U373.X4 cells. The results are presented as the mean ± SEM (standard error of mean) of triplicate infections. The infectivity of each mutant was compared with that of WT virus using Student t-test. Statistical analysis was performed using STATA software version 10.1. (StataCorp, TX). Differences were considered statistically significant if the p-value was ≤.05.
Results
The effect of V3 single mutations on coreceptor usage
Prediction of coreceptor usage using genotypic tools
Coreceptor usage of all V3 single mutations was predicted using available genotypic predictors (Table 1). Based on 11/25 rule, only virus with S11R mutation was predicted to have an X4 phenotype. Based on net charge rule, viruses with N7K, S11R, Q18R, and S32R mutations were predicted to have an X4 phenotype. Geno2pheno predicted X4 phenotype for viruses with N7K, S11R, and S32R mutations. Based on PSSM using X4R5 matrix, all single mutations, except T12V, T12F, and S32R, were predicted as X4, whereas using SINSI matrix only S11R mutation was predicted to have X4 phenotype.
Table 1.
Prediction of Coreceptor Usage of the V3 Mutants Using Different Genotypic Methods
| Geno2pheno[coreceptor] | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| V3 crown | 11/25 | Net charge | FPR, %a | FPR 1% | FPR 2.5% | FPR 5% | FPR 10% | FPR 15% | FPR 20% | PSSM (X4R5) | PSSM (SINSI) | SVM/LMT | Phenotypic result | |
| R5 parental (patient code: HDR932), WT | GPGQ | SD/R5 | 4/R5 | 84.8 | R5 | R5 | R5 | R5 | R5 | R5 | R5 | R5 | R5 | R5 |
| mutant P5 (S5Y) | GPGQ | SD/R5 | 4/R5 | 24.9 | R5 | R5 | R5 | R5 | R5 | R5 | X4 | R5 | R5 | R5 |
| mutant P7 (N7K) | GPGQ | SD/R5 | 5/X4 | 7.8 | R5 | R5 | R5 | X4 | X4 | X4 | X4 | R5 | R5 | R5 |
| mutant P11 (S11R) | GPGQ | RD/X4 | 5/X4 | 1.8 | R5 | X4 | X4 | X4 | X4 | X4 | X4 | X4 | R5 | R5/X4 |
| mutant P12 (T12V) | GPGQ | SD/R5 | 4/R5 | 99.4 | R5 | R5 | R5 | R5 | R5 | R5 | R5 | R5 | R5 | R5 |
| mutant P12 (T12F) | GPGQ | SD/R5 | 4/R5 | 91 | R5 | R5 | R5 | R5 | R5 | R5 | R5 | R5 | R5 | R5 |
| mutant P18 (Q18R) | GPGR | SD/R5 | 5/X4 | 31.3 | R5 | R5 | R5 | R5 | R5 | R5 | X4 | R5 | R5 | R5 |
| mutant P27 (I27T) | GPGQ | SD/R5 | 4/R5 | 87.1 | R5 | R5 | R5 | R5 | R5 | R5 | X4 | R5 | R5 | R5 |
| mutant P27 (I27V) | GPGQ | SD/R5 | 4/R5 | 84.8 | R5 | R5 | R5 | R5 | R5 | R5 | X4 | R5 | R5 | R5 |
| mutant P32 (S32R) | GPGQ | SD/R5 | 5/X4 | 6 | R5 | R5 | R5 | X4 | X4 | X4 | R5 | R5 | R5 | R5 |
| mutant (S5Y+S32R) | GPGQ | SD/R5 | 5/X4 | 2.4 | R5 | X4 | X4 | X4 | X4 | X4 | X4 | R5 | X4 | R5 |
| mutant (N7K+S32R) | GPGQ | SD/R5 | 6/X4 | 1.7 | R5 | X4 | X4 | X4 | X4 | X4 | X4 | R5 | X4 | Defective |
| mutant (S11R+S32R) | GPGQ | RD/X4 | 6/X4 | 0.7 | X4 | X4 | X4 | X4 | X4 | X4 | X4 | X4 | X4 | Defective |
| mutant (S11R+Q18R) | GPGR | RD/X4 | 6/X4 | 1.7 | R5 | X4 | X4 | X4 | X4 | X4 | X4 | X4 | X4 | Defective |
| mutant (Q18R+S32R) | GPGR | SD/R5 | 6/X4 | 2.6 | R5 | R5 | X4 | X4 | X4 | X4 | X4 | R5 | X4 | R5 |
| mutant (I27V+S32R) | GPGQ | SD/R5 | 5/X4 | 6 | R5 | R5 | R5 | X4 | X4 | X4 | X4 | R5 | X4 | R5 |
| mutant (I27T+S32R) | GPGQ | SD/R5 | 5/X4 | 6.8 | R5 | R5 | R5 | X4 | X4 | X4 | R5 | R5 | X4 | R5 |
%FPR: a value is calculated from Geno2pheno predictor. The value below %FPR cutoff is predictive for an X4 virus, whereas a value above %FPR cutoff reflects an R5 virus. Geno2pheno allows the user choose a %FPR cutoff as 1%, 2.5%, 5%, 10%, 15%, and 20%.
FPR, false positive rate.
Phenotypic assay to assess the coreceptor usage
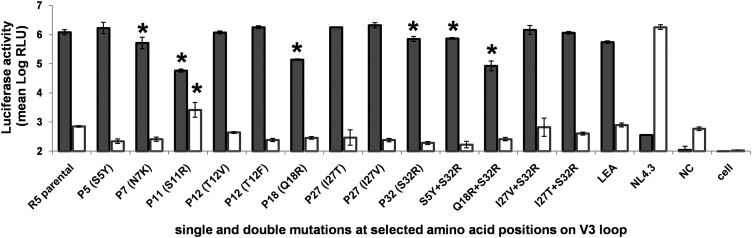
The infectivity of all V3 single mutation viruses in U373.R5 and U373.X4 cells are shown in Figure 2. The WT virus with original clone of R5-env infected only CCR5-expressing cells. All mutant viruses containing V3 single mutations used CCR5 as a coreceptor. Interestingly, the infectivity of viruses containing single mutation at position 7, 11, 18, and 32 was significantly decreased in CCR5-expressing cells (p < .05). When compared with WT virus, mutant N7K and S32R had a twofold reduction of infectivity in CCR5-expressing cells, whereas mutant Q18R showed ninefold reduction. The arginine substitution at position 11 also caused a 21-fold reduction in viral infectivity in CCR5-expressing cells. Notably, the amino acid substitution at position 5 (S5Y), position 12 (T12V and T12F), and position 27 (I27T and I27V) had no effect on infection of CCR5-expressing cells.
FIG. 2.
Effect of amino acid mutations on infectivity. Infectivity is expressed as RLUs detected in U373 cells expressing CCR5 (black bar) and CXCR4 (white bar). The results are presented as the mean ± SEM of triplicate infections. LEA and NL4.3 strains were used as positive controls for CCR5-using and CXCR4-using viruses, respectively. NC was pseudotyped virus defective in env resulting from cotransfection of empty PCI expression vector and pNL4.3Δenv.Luc. *p < .05. NC, negative control (defective virus); PCI, PCI expression vector; RLUs, relative light units.
Almost all single mutations had no effect on infection of CXCR4-expressing cells as compared with the WT env gene. Only the mutant with arginine substitution at position 11 (S11R) was able to use the CXCR4 coreceptor and showed a dual R5X4 tropism (p < .05).
The effect of V3 double mutations on coreceptor usage
Prediction of coreceptor usage using genotypic tools
Results of predictions using available genotypic tools of the effect of seven double mutations are shown in Table 1. Based on 11/25 rule, virus with double mutations at position 11/32 and 11/18 were predicted to have X4 phenotype. Based on net charge rule, the results showed that net charge was increased in all double mutations as related to CXCR4 usage. Almost all genotypic predictors, including Geno2pheno, PSSM (X4R5 matrix), and SVM/LMT, predicted the double mutants to have X4 phenotype. Based on PSSM using X4R5 matrix, all double mutants, except I27T+S32R, were predicted as X4, whereas using SINSI matrix only S11R+S32R and S11R+Q18R mutations were predicted to have X4 phenotype. Net charge rule and Geno2pheno (FPR10%) predicted that 7/7 mutants were X4 viruses.
Phenotypic assay to assess the coreceptor usage
The effect of V3 double mutations on coreceptor usage and infectivity of these mutant viruses are shown in Figure 2. The result showed that none of double mutations had an effect on infection of CXCR4-expressing cells. For CCR5 usage, the amino acid substitutions at positions 5 and 32 (S5Y+S32R) caused a twofold statistically significant reduction of viral infectivity as compared with WT virus (p < .05), and had the same profile as single mutation at position 32 alone (S32R). Thus, the addition of S5Y to S32R did not change the infectivity in CCR5-expressing cells. Double mutations at positions 18 and 32 (Q18R+S32R) led to a 14-fold statistically significant reduction in infectivity as compared with WT virus (p < .05) and individual single mutation either Q18R or S32R. This double mutant (Q18R+S32R) showed eightfold reduction of infectivity in CCR5-expressing cells as compared with the double mutant at S5Y+S32R. In contrast, the double mutations at positions 27 and 32 (I27V+S32R and I27T+S32R) showed no effect on infection of CCR5-expressing cells. Remarkably, the mutant viruses with double mutations at positions 7 and 32 (N7K+S32R), 11 and 32 (S11R+S32R), and 11 and 18 (S11R+Q18R) were defective in infectivity and also non-infectious in TZM-Bl cells (data not shown).
Discussion
Our study showed that all viruses with either single or double mutations used CCR5 coreceptor. However, viruses containing single substitution at positions 7, 11, 18, and 32 had reduced infectivity as compared with WT virus, and viruses with double mutations (at positions 5/32 and 18/32) had reduced infectivity as compared with viruses with individual mutation. Only virus with arginine substitution at position 11 used the CXCR4 coreceptor. In contrast to the various genotypic methods, which predicted the impact of single or double mutations for CXCR4-using viruses, none of them was confirmed in our phenotypic assay, all mutant viruses except one using only the CCR5 coreceptor. The discrepancy between the genotypic predictors and our assay was mainly observed with viruses harboring double mutations. This may be related to the presence of positively charged amino acids or high total net charge of V3 region, which lead the predictors voted for X4 phenotype. It had been previously reported that Geno2pheno and PSSM tools overestimate X4 phenotypes.22 In our study, none of the genotypic tools could fully predict correctly the coreceptor phenotype indicating that genotypic tools to predict coreceptor usage of HIV-1 CRF01_AE need to be improved.
In our study, the positions of interest 7 and 32 located at the base and position 18 located at the crown are known to play an important role in the interaction with CCR5 coreceptor.23–25 Mutations involving several of these positions may alter the interaction with CCR5 more than an individual mutation would. Virus containing mutations at positions 18 and 32 had indeed lower infectivity. However, we found that some combination of mutations (N7K+S32R, S11R+S32R, and S11R+Q18R) abolished viral infectivity in cells expressing either CCR5 or CXCR4. This may be due to the fact that these positions are involved in coreceptor binding, some mutations causing the functional loss for entry. However, these defective mutants may also be X4 if they have had compensatory mutations elsewhere in V3 loop; in particular, the S11R mutation which is required for CXCR4 usage.
The decreased infection of CCR5-expressing cells by virus containing V3 amino acid substitution at positions 7 (N7K), 11 (S11R), 18 (Q18R), 32 (S32R), S5Y+S32R, and Q18R+S32, may be due to changes in electrostatic interactions between the V3 loop and the coreceptor, since it was previously described that electrostatic potentials play a role in V3-CCR5 interaction.26,27 The substitution at positions 7 (N7K), 11 (S11R), 18 (Q18R), 32 (S32R) and double mutations corresponding to increase in positively charged amino acid (K or R) may be critical for the reduction of CCR5 usage. It was previously shown that mutation N7K decreases the binding affinity to the CCR5 N-terminus to V3 loop and increases the distance between position 7 and the sulfotyrosine at position 14 on CCR5, thus diminishing the interaction between these two important regions.17 It was also shown that mutations resulting in the acquisition of a positive charge, such as N7K, S11R, and Q32K, led to a remarkably unfavorable profile for CCR5 binding.17
In addition, a recent study showed that R5 and X4 variants within one host are genetically isolated and compartmentalized in different host cell types, and amino acid patterns of V1/V2 and C2/V3 regions of all R5 and X4 variants are also distinct.28 Moreover, the changes from R5 to X4 variants usually require more mutations as were reported in subtype B, C, and CRF07_BC.9,13,15,16 It was related to our study that either single or double mutations within V3 loop are not sufficient for coreceptor switching.
Taken together, the V3 amino acid substitutions at positions 7, 11, 18, and 32, including double mutations at 5/32 and 18/32 of HIV-1 CRF01_AE subtype, had an effect on interaction with CCR5, whereas substitutions at positions 5, 12, and 27 did not. Only arginine substitution at position 11 seemed to be involved in CXCR4 coreceptor usage. Mutations within the V3 region of HIV-1 CRF07_BC have been shown necessary, but not sufficient to allow for switch of coreceptor usage,16 suggesting that the effects of amino acid substitution on CXCR4 usage are context dependent, and that other regions of the envelope glycoprotein may be involved in the coreceptor usage. Other domains in gp120, including modifications of N-linked glycosylation sites, as well as in gp41 region, have been reported to influence the coreceptor usage and be involved in coreceptor switching.29–32 Similarly, our results suggest that some V3 positions are necessary for binding to coreceptor, but are not sufficient for switching coreceptor usage. Additional studies, including the impact of these mutations on the sensitivity to CCR5 blockers, including Maraviroc and other CC chemokines, would be informative and might help improve the genotypic approaches to better predict the coreceptor usage of CRF01_AE variants.
Acknowledgments
Authors would like to thank Dr. Woottichai Khamduang, faculty of Associated Medical Sciences, Chiang Mai University, for his support with statistical analysis. This work was supported by the National Research University project under the Thailand's Office of the Commission on Higher Education, Thailand and Program of Excellence for Education and Research in South countries (PEERS). The following reagents were obtained through the NIH AIDS Research and Reference Reagent Program, Division of AIDS, NIAID, NIH: pNL4.3.LUC.R-E- from N. Landau; TZM-bl cells from J.C. Kappes, X. Wu, and Tranzyme, Inc.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Dalgleish AG, Beverley PC, Clapham PR, Crawford DH, Greaves MF, Weiss RA: The CD4 (T4) antigen is an essential component of the receptor for the AIDS retrovirus. Nature 1984;312:763–767 [DOI] [PubMed] [Google Scholar]
- 2.Deng H, Liu R, Ellmeier W, et al. : Identification of a major co-receptor for primary isolates of HIV-1. Nature 1996;381:661–666 [DOI] [PubMed] [Google Scholar]
- 3.Feng Y, Broder CC, Kennedy PE, Berger EA: HIV-1 entry cofactor: Functional cDNA cloning of a seven-transmembrane, G protein-coupled receptor. Science 1996;272:872–877 [DOI] [PubMed] [Google Scholar]
- 4.Berger EA, Doms RW, Fenyo EM, et al. : A new classification for HIV-1. Nature 1998;391:240. [DOI] [PubMed] [Google Scholar]
- 5.Hartley O, Klasse PJ, Sattentau QJ, Moore JP: V3: HIV's switch-hitter. AIDS Res Hum Retroviruses 2005;21:171–189 [DOI] [PubMed] [Google Scholar]
- 6.Hwang SS, Boyle TJ, Lyerly HK, Cullen BR: Identification of the envelope V3 loop as the primary determinant of cell tropism in HIV-1. Science 1991;253:71–74 [DOI] [PubMed] [Google Scholar]
- 7.De Jong JJ, De Ronde A, Keulen W, Tersmette M, Goudsmit J: Minimal requirements for the human immunodeficiency virus type 1V3 domain to support the syncytium-inducing phenotype: Analysis by single amino acid substitution. J Virol 1992;66:6777–6780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fouchier RA, Groenink M, Kootstra NA, et al. : Phenotype-associated sequence variation in the third variable domain of the human immunodeficiency virus type 1 gp120 molecule. J Virol 1992;66:3183–3187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Coetzer M, Nedellec R, Cilliers T, Meyers T, Morris L, Mosier DE: Extreme genetic divergence is required for coreceptor switching in HIV-1 subtype C. J Acquir Immune Defic Syndr 2011;56:9–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Delobel P, Sandres-Saune K, Cazabat M, et al. : R5 to X4 switch of the predominant HIV-1 population in cellular reservoirs during effective highly active antiretroviral therapy. J Acquir Immune Defic Syndr 2005;38:382–392 [DOI] [PubMed] [Google Scholar]
- 11.Pastore C, Nedellec R, Ramos A, et al. : Conserved changes in envelope function during human immunodeficiency virus type 1 coreceptor switching. J Virol 2007;81:8165–8179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schwalbe B, Schreiber M: Effect of lysine to arginine mutagenesis in the V3 loop of HIV-1 gp120 on viral entry efficiency and neutralization. PLoS One 2015;10:e0119879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tsuchiya K, Ode H, Hayashida T, et al. : Arginine insertion and loss of N-linked glycosylation site in HIV-1 envelope V3 region confer CXCR4-tropism. Sci Rep 2013;3:2389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Waters LJ, Scourfield AT, Marcano M, et al. : The evolution of coreceptor tropism in HIV-infected patients interrupting suppressive antiretroviral therapy. Clin Infect Dis 2011;52:671–673 [DOI] [PubMed] [Google Scholar]
- 15.Zhang H, Tully DC, Zhang T, Moriyama H, Thompson J, Wood C: Molecular determinants of HIV-1 subtype C coreceptor transition from R5 to R5X4. Virology 2010;407:68–79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang L, Ma L, Wang Z, et al. : Alterations in HIV-1 gp120V3 region are necessary but not sufficient for coreceptor switching in CRF07_BC in China. PLoS One 2014;9:e93426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Svicher V, Alteri C, Artese A, et al. : Identification and structural characterization of novel genetic elements in the HIV-1V3 loop regulating coreceptor usage. Antivir Ther 2011;16:1035–1045 [DOI] [PubMed] [Google Scholar]
- 18.Shoombuatong W, Hongjaisee S, Barin F, Chaijaruwanich J, Samleerat T: HIV-1 CRF01_AE coreceptor usage prediction using kernel methods based logistic model trees. Comput Biol Med 2012;42:885–889 [DOI] [PubMed] [Google Scholar]
- 19.Amaratunga D, Cabrera J, Lee YS: Enriched random forests. Bioinformatics 2008;24:2010–2014 [DOI] [PubMed] [Google Scholar]
- 20.Breiman L: Random forests. Machine Learn 2001;45:5–32 [Google Scholar]
- 21.Samleerat T, Thenin S, Jourdain G, et al. : Maternal neutralizing antibodies against a CRF01_AE primary isolate are associated with a low rate of intrapartum HIV-1 transmission. Virology 2009;387:388–394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mulinge M, Lemaire M, Servais JY, et al. : HIV-1 tropism determination using a phenotypic Env recombinant viral assay highlights overestimation of CXCR4-usage by genotypic prediction algorithms for CRRF01_AE and CRF02_AG. PLoS One 2013;8:e60566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Huang CC, Tang M, Zhang MY, et al. : Structure of a V3-containing HIV-1 gp120 core. Science 2005;310:1025–1028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hung CS, Vander Heyden N, Ratner L: Analysis of the critical domain in the V3 loop of human immunodeficiency virus type 1 gp120 involved in CCR5 utilization. J Virol 1999;73:8216–8226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang WK, Dudek T, Essex M, Lee TH: Hypervariable region 3 residues of HIV type 1 gp120 involved in CCR5 coreceptor utilization: Therapeutic and prophylactic implications. Proc Natl Acad Sci USA 1999;96:4558–4562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kalinina OV, Pfeifer N, Lengauer T: Modelling binding between CCR5 and CXCR4 receptors and their ligands suggests the surface electrostatic potential of the co-receptor to be a key player in the HIV-1 tropism. Retrovirology 2013;10:130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Morikis D, Rizos AK, Spandidos DA, Krambovitis E: Electrostatic modeling of peptides derived from the V3-loop of HIV-1 gp120: Implications of the interaction with chemokine receptor CCR5. Int J Mol Med 2007;19:343–351 [PubMed] [Google Scholar]
- 28.Zhou S, Bednar MM, Sturdevant CB, Hauser BM, Swanstrom R: Deep sequencing of the HIV-1 env gene reveals discrete X4 lineages and linkage disequilibrium between X4 and R5 viruses in the V1/V2 and V3 variable regions. J Virol 2016;90:7142–7158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dimonte S, Mercurio F, Svicher V, D'Arrigo R, Perno CF, Ceccherini-Silberstein F: Selected amino acid mutations in HIV-1 B subtype gp41 are associated with specific gp120v(3) signatures in the regulation of co-receptor usage. Retrovirology 2011;8:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Labrosse B, Treboute C, Brelot A, Alizon M: Cooperation of the V1/V2 and V3 domains of human immunodeficiency virus type 1 gp120 for interaction with the CXCR4 receptor. J Virol 2001;75:5457–5464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pollakis G, Kang S, Kliphuis A, Chalaby MI, Goudsmit J, Paxton WA: N-linked glycosylation of the HIV type-1 gp120 envelope glycoprotein as a major determinant of CCR5 and CXCR4 coreceptor utilization. J Biol Chem 2001;276:13433–13441 [DOI] [PubMed] [Google Scholar]
- 32.Thielen A, Sichtig N, Kaiser R, Lam J, Harrigan PR, Lengauer T: Improved prediction of HIV-1 coreceptor usage with sequence information from the second hypervariable loop of gp120. J Infect Dis 2010;202:1435–1443 [DOI] [PubMed] [Google Scholar]