Abstract
Background
The diagnosis of multiple sclerosis (MS) is currently based solely on clinical and magnetic resonance imaging features. However, histopathological studies have revealed four different patterns of lesion pathology in patients diagnosed with MS, suggesting that MS may be a pathologically heterogeneous syndrome rather than a single disease entity.
Objective
The aim of this study was to investigate whether patients with pattern I MS differ from patients with pattern II or III MS with regard to cerebrospinal fluid (CSF) findings, especially with reference to intrathecal IgG synthesis, which is found in most patients with MS but is frequently missing in MS mimics such as aquaporin-4-IgG-positive neuromyelitis optica spectrum disorders and myelin oligodendrocyte glycoprotein-IgG-positive encephalomyelitis.
Methods
Findings from 68 lumbar punctures in patients who underwent brain biopsy as part of their diagnostic work-up and who could be unequivocally classified as having pattern I, pattern II or pattern III MS were analysed retrospectively.
Results
Oligoclonal bands (OCBs) were present in 88.2% of samples from pattern I MS patients but in only 27% of samples from patients with pattern II or pattern III MS (P < 0.00004); moreover, OCBs were present only transiently in some of the latter patients. A polyspecific intrathecal IgG response to measles, rubella and/or varicella zoster virus (so-called MRZ reaction) was previously reported in 60–80% of MS patients, but was absent in all pattern II or III MS patients tested (P < 0.00001 vs. previous cohorts). In contrast, the albumin CSF/serum ratio (QAlb), a marker of blood–CSF barrier function, was more frequently elevated in samples from pattern II and III MS patients (P < 0.002). Accordingly, QAlb values and albumin and total protein levels were higher in pattern II and III MS samples than in pattern I MS samples (P < 0.005, P < 0.009 and P < 0.006, respectively).
Conclusions
Patients with pattern II or pattern III MS differ significantly from patients with pattern I MS as well as from previous, histologically non-classified MS cohorts with regard to both intrathecal IgG synthesis and blood–CSF barrier function. Our findings strongly corroborate the notion that pattern II and pattern III MS are entities distinct from pattern I MS.
Keywords: Multiple sclerosis, Histopathology, Pattern I lesions, Pattern II lesions, Pattern III lesions, Cerebrospinal fluid, Oligoclonal bands, Intrathecal IgG synthesis, Blood-CSF barrier dysfunction, Total protein, QIgG, QAlb
Background
Histopathological studies have demonstrated at least three different lesion patterns in early disease stages from patients diagnosed with multiple sclerosis (MS), termed patterns I, II and III [1, 2]. Pattern I lesions show T cell and macrophage infiltration. Pattern II is defined by additional antibody and complement deposition, suggesting a contribution of humoral mechanisms to disease pathology. Pattern III is characterized by distal oligodendrogliopathy with dysregulated myelin protein expression and oligodendrocyte apoptosis, but still occurs on an inflammatory background. A fourth pattern, defined by oligodendrocyte degeneration in the periplaque white matter, has been described in few autopsy cases of primary-progressive MS, but is rare. These findings raise the possibility that MS, a diagnosis currently based mainly on phenotypical, namely clinical and radiological features [3], may in fact be a pathologically heterogeneous syndrome rather than a single disease entity. Importantly, two recent studies demonstrated intraindividual homogeneity and persistence of pattern I, II and III lesions over time [4, 5], further corroborating the notion that lesion pathology may rather define pathogenetically distinct entities than reflect stage-dependent processes in the development of lesions.
Intrathecal IgG synthesis, as detected qualitatively by isoelectric focusing (IEF) of cerebrospinal fluid (CSF) and serum or quantitatively by calculation of the immunoglobulin CSF/serum ratio (QIgG), is present in 90–98% of MS patients, usually remains detectable over the entire course of disease and is considered a diagnostic mainstay in MS [6–9].
In this study, we retrospectively compared the CSF profiles of patients who underwent brain biopsy as part of their diagnostic work-up and who could be unequivocally classified as having pattern I, pattern II or pattern III lesions, respectively.
Methods
Patients
Results from 68 routine lumbar punctures in 33 patients with histopathologically confirmed MS (16 × pattern II, 7 × pattern III, 10 × pattern I [1, 2]) were analysed for OCB frequency and OCB patterns; CSF and serum IgG, IgM and IgA; CSF and serum albumin; IgG, IgM and IgA CSF/serum ratios (QIgG, QIgM, QIgA); albumin CSF/serum ratio (QAlb); intrathecal IgG response to measles (M), rubella (R) and varicella zoster (Z) (MRZ reaction [MRZR]) [10–14]; CSF total protein (TP) and CSF l-lactate levels; and CSF white cell counts and white cell differentiation. All patients had undergone brain biopsy as part of their diagnostic work-up. All biopsies were histopathologically classified at the Department of Neuropathology, University of Göttingen, Germany (WB, IM, FK), as previously described [1, 2]. All patients were classified based on brain lesions; none was classified based on brainstem, spinal cord or optic nerve lesions. All had early active disease and none had primary-progressive disease or pattern IV lesions. The median age at the time of first lumbar puncture was 36 years (range 13–63). The sex ratio (m:f) was 1:1.75. All patients were of Caucasian origin. Available serum samples were retrospectively tested for aquaporin 4 (AQP4)-IgG and myelin oligodendrocyte glycoprotein (MOG)-IgG using a cell-based assay (CBA) employing formalin HEK293 cells transfected with full-length human M1-AQP4 and M23-AQP4 [15, 16] or full-length human MOG [17, 18], respectively. All analyses were done retrospectively, in no case were brain, blood or CSF specimens obtained for the present study. AQP4-IgG and MOG-IgG testing and retrospective analysis of the patients’ CSF results was performed in an anonymized fashion.
Evaluation of the humoral immune response
Oligoclonal IgG bands (OCBs) were evaluated according to an international consensus [9]: IEF pattern 1 = no OCBs in CSF or serum; IEF pattern 2 = CSF-restricted OCBs; IEF pattern 3 = CSF-restricted OCBs and additional identical bands in CSF and serum (combination of patterns 2 and 4); IEF pattern 4 = identical OCBs in CSF and serum (‘mirror pattern’); and IEF pattern 5 = monoclonal bands in CSF and serum. Only IEF patterns 2 and 3 indicate intrathecal IgG synthesis. Quantitative expressions of the intrathecal humoral immune response were based on calculation of the CSF/serum ratios for IgG (QIgG), IgM (QIgM) and IgA (QIgA) with QIg = IgCSF[mg/L]/Igserum[g/L]. The upper limits of the respective reference ranges, Qlim(IgG), Qlim(IgM) and Qlim(IgA), were calculated against QAlb according to Reiber’s revised hyperbolic functions [10]. Values for QIg > Qlim(Ig) were considered to indicate intrathecal immunoglobulin synthesis [10]. The fraction (in %) of intrathecally produced Ig (IgIF) and the absolute amount of locally, i.e. intrathecally, produced Ig (IgGloc) were calculated according to the following formulas: IgIF[%] = [QIg − Qlim(Ig)] × Igserum × 100 and Igloc[mg/L] = [QIg − Qlim(Ig)] × Igserum, respectively [10]. Antibody indices (AI) were calculated according to Reiber’s formula: AI = Qspec/QIgG, or AI = Qspec/Qlim(IgG) if (Qlim > QIgG), with Qspec = IgGspec(CSF)/IgGspec(serum). Taking into account the relatively small sample size of the pattern I MS subgroup, we also compared the results for pattern II and pattern III MS with data from ‘classical’ landmark studies on OCB and MRZR findings in (histologically non-classified) MS [14, 19].
Evaluation of blood-CSF barrier function
The CSF/serum albumin quotient, QAlb = AlbCSF[mg/L]/Albserum[g/L], was used to assess the blood–CSF barrier function. As the upper reference limit of QAlb is age dependent, Qlim(Alb) was calculated as 4 + (a/15), with a representing the patient’s age, according to Reiber et al. [20]. Dysfunction of the blood–CSF barrier was defined as QAlb > Qlim(Alb).
Cytological examination, total CSF protein and l-lactate
A white cell count >5/μL was classified as ‘increased’. An age-dependent upper reference range for CSF l-lactate was applied (0–15 years of age, 1.8 mmol/L; 16–50 years, 2.1 mmol/L; >50 years, 2.6 mmol/L [21, 22]). As upper reference limit for total CSF protein, 450 mg/L was used.
Statistics
Fisher’s exact test and Mann–Whitney U test were used to detect differences between groups. Spearman’s rho was calculated to test for correlations. P values <0.05 were considered statistically significant. Due to the exploratory nature of this study, no corrections for multiple comparisons were performed. Reiber diagrams were generated using the Protein Statistics in CSF analysis V3.0 software (Comed, Soest, Germany). The study was approved by the institutional review boards of the University of Göttingen and the University of Heidelberg. All CSF parameters evaluated in this study are routinely tested in Germany as part of the diagnostic workup of patients with suspected MS in Germany and are recommended by the guidelines of the German Society of Neurology and by the guidelines of the Germany Society of CSF Analysis and Clinical Neurochemistry [21].
Results
Epidemiology and autoantibody status
Epidemiological data for all subgroups are given in Table 1. All serum samples available for retrospective testing (n = 13) were negative for AQP4-IgG and MOG-IgG [18].
Table 1.
Epidemiological findings
| Units | Pattern I MS | Patterns II + III MS | Pattern II MS | Pattern III MS | AQP4-Ab+ NMO [48] | |
|---|---|---|---|---|---|---|
| Patients | N | 10 | 23 | 16 | 7 | 89 |
| Samples | N | 19 | 49 | 30 | 19 | 211 |
| Age at first LP | Years | 30 (13–47) | 36 (20–63) | 35 (20–51) | 38 (26–63) | 39.5 (14–79) |
| Sex ratio | m:f | 1:1 | 1:2.3 | 1:2.2 | 1:2.5 | 1:12.1 |
LP lumbar puncture, m male, f female
Results in AQP4-IgG-positive NMO as observed in a previous study [48] are given in the last column for comparison. Note the marked difference in the sex ratios between pattern II MS and NMO. Years are given as median and range
Oligoclonal bands
CSF-restricted OCB were found in 15/17 (88.2%) samples from patients with pattern I MS, but were negative in 27/37 (73%) of samples from patients with pattern II or pattern III MS (P < 0.00004) (Fig. 1). Overall, only 7/22 (31.8%) pattern II and III patients, but 8/10 (80%) pattern I MS patients, had OCB at least once (P < 0.021). Moreover, OCBs were only transiently positive in 2 of the 7 only OCB-positive pattern II and III patients (patient 1, pattern II: lumbar puncture (LP) #1 positive, LP #2 negative; patient 2, pattern III: LP #1 positive, LP #2 negative). If only persisting OCB are taken into account, only 22.7% (5/22) patients with pattern II or III MS were positive for OCB (P < 0.006) (Table 2). Of note, QIgG was negative at the time of OCB determination in the two cases with transient OCB, indicating very low levels of intrathecal IgG synthesis in these patients. Identical OCB in serum and CSF without additional CSF-restricted bands (the so-called mirror pattern or IEF pattern 4), suggesting possible systemic inflammation, were found in a single patient with pattern II MS but were absent in all other patients. IEF pattern 5, indicating monoclonal gammopathy, was present in a single pattern II MS patient (still detectable in a second sample taken 24 months later) and transiently in one pattern III patient (negative follow-up sample obtained 36 days later). Comparison of the pattern II or pattern III MS patients’ data with data from a reference paper on CSF in MS [19] confirmed the marked difference in OCB frequency (P < 0.000001) (see Table 9 for details).
Fig. 1.
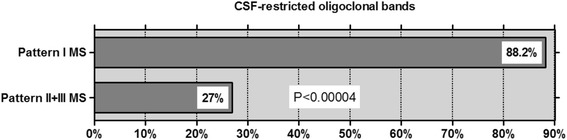
Frequency of CSF-restricted oligoclonal bands (OCBs) results from 54 LPs in patients with pattern I MS compared to patients with pattern II or pattern III MS. Note that OCBs were present only transiently in 2/7 OCB-positive pattern II/III patients
Table 2.
Frequency of intrathecal total IgG synthesis; oligoclonal IgG pattern; IgG CSF/serum ratios; intrathecal IgG fractions; absolute amount of locally produced IgG; and CSF and serum IgG concentrations
| Units | Pattern I MS | Pattern II + III MS | Pattern II MS | Pattern III MS | AQP4-IgG+ NMO [48] | MOG-IgG+ EM [35] | |
|---|---|---|---|---|---|---|---|
| CSF-restricted OCB | Samples | 15/17 (88.2) | 10/37 (27) | 9/25 (36) | 1/12 (8.3) | 29/177 (16.4) | 8/47 (17) |
| CSF-restricted OCB | Patients | 8/10 (80) | 7/22 (31.8) | 6/16 (37.5) | 1/6 (16.7) | 22/80 (27.5) | 6/45 (13) |
| CSF-restricted OCB, without transient OCB | Patients | 8/10 (80) | 5/22 (22.7) | 5/16 (31.3) | 0/6 (0) | 16/80 (20) | 6/45 (13) |
| OCB, IEF pattern 1 | Samples | 2/15 (13.3) | 24/35 (68.6) | 13/23 (56.5) | 11/12 (91.7) | 127/177 (71.8) | n.d. |
| OCB, IEF pattern 2 | Samples | 13/15 (86.7) | 7/35 (20) | 6/23 (26.1) | 1/12 (8.3) | 19/177 (10.7) | n.d. |
| OCB, IEF pattern 3 | Samples | 0/15 (0) | 1/35 (2.9) | 1/23 (4.3) | 0/12 (0) | 10/177 (5.6) | n.d. |
| OCB, IEF pattern 4 | Samples | 0/15 (0) | 1/35 (2.9) | 1/23 (4.3) | 0/12 (0) | 20/177 (11.3) | n.d. |
| OCB, IEF pattern 5 | Samples | 0/15 (0) | 3/35 (8.6) | 2/23 (8.7) | 1/12 (8.3) | 1/177 (0.6) | n.d. |
| QIgG > Qlim(IgG) | Patients | 3/10 (30) | 4/21 (19) | 4/14 (28.6) | 0/7 (0) | n.d. | n.d. |
| QIgG > Qlim(IgG) | Samples | 7/17 (41.2) | 5/41 (12.2) | 5/24 (20.8) | 0/17 (0) | 13/143 (9) | n.d. |
| QIgG, all LPs | – | 3.6 (1.9–9.35; 17) | 4.75 (1.3–21.5; 42) | 4.8 (1.3–21.5; 25) | 4.7 (1.98–12.6; 17) | 3.9 (0.2–58.1; 135) | n.d. |
| QIgG, if positive | – | 3.63 (2.6–9.35; 7) | 5.03 (3.2–8.8; 5) | 5.03 (3.2–8.8; 5) | n.a. | 5.7 (2.5–58.1; 12) | n.d. |
| IgGloc, all LPs | mg/L | 0 (0–75.76; 17) | 0 (0–51.17; 41) | 0 (0–51.17; 24) | 0 (0–0; 17) | 0 (0–441.4; 135) | n.d. |
| IgGloc, QIgG positives | mg/L | 5.91 (2.31–75.76; 7) | 16.75 (11.79–51.17; 5) | 16.75 (11.79–51.17; 5) | n.a. | 13.9 (1.3–441.4; 12) | n.d. |
| IgGIF, all LPs | % | 0 (0–0.58; 17) | 0 (0–0.59; 41) | 0 (0–0.59; 24) | 0 (0–0; 17) | 0 (0–90.6; 135) | n.d. |
| IgGIF, QIgG positives | % | 0.14 (0.06–0.58; 7) | 0.47 (0.22–0.59; 5) | 0.47 (0.22–0.59; 5) | n.a. | 32.5 (2.8–90.6; 12) | n.d. |
| IgG CSF, all LPs | mg/L | 39.9 (11–130; 17) | 43.7 (11.4–146; 41) | 46 (11.4–109; 24) | 37.7 (21–146; 17) | 37.9 (2.4–487; 136) | n.d. |
| IgG CSF, QIgG positives | mg/L | 39.9 (16.8–130; 7) | 53.3 (22.9–109; 5) | 53.3 (22.9–109; 5) | n.a. | 70.6 (20.5–487; 12) | n.d. |
| IgG serum, all LPs | g/L | 10 (3.9–28.04; 17) | 8.75 (5.55–28.9; 41) | 10.39 (5.55–24.8; 24) | 7.5 (6.15–28.9; 17) | 10 (1.9–55.8; 134) | n.d. |
| IgG serum, QIgG positives | g/L | 9.21 (3.9–15.3; 7) | 8.75 (7.1–12.4; 5) | 8.75 (7.1–12.4; 5) | n.a. | 10.7 (2.4–18; 12) | n.d. |
n.a. not applicable, n.d. no data
Concentrations, ratios and fractions are reported as medians; range and total sample numbers examined are given in brackets
Table 9.
Summary of differences in CSF parameters between various MS subgroups as observed in the present study
| Parameter | Diagnostic groups | Results | P values |
|---|---|---|---|
| CSF-restricted OCB, all LPs | Pattern I | 15/17 (88.2) | P < 0.00004 |
| Patterns II + III | 10/37 (27) | ||
| Reiber et al. [19] | 262/267 (98) | P < 0.000001 | |
| Patterns II + III | 10/37 (27) | ||
| Pattern I | 15/17 (88.2) | P < 0.0001 | |
| Pattern II | 9/25 (36) | ||
| Pattern III | 1/12 (8.3) | ||
| CSF-restricted OCB, patients | Pattern I | 8/10 (80) | P < 0.03 |
| Patterns II + III | 7/22 (31.8) | ||
| Reiber et al. [19] | 262/267 (98) | P < 0.000001 | |
| Patterns II + III | 7/22 (31.8) | ||
| CSF-restricted OCB, patients, w/o transient OCBs | Pattern I | 8/10 (80) | P < 0.006 |
| Patterns II + III | 5/22 (22.7) | ||
| Reiber et al. [19] | 262/267 (98) | P < 0.00001 | |
| Patterns II + III | 5/22 (22.7) | ||
| MRZ reaction (≥2 AIs >1.5), all LPs | Jarius et al. [23] | 397/546 (69) | P < 0.000001 |
| Patterns II + III | 0/12 (0) | ||
| M and/or R and/or Z >1.5, all LPs | Reiber et al. [19] | 158/177 (89) | P < 0.000001 |
| Patterns II + III | 0/12 (0) | ||
| QIgG > Qlim(lgG), all LPs | Pattern I | 7/17 (41.2) | P < 0.03 |
| Patterns II + III | 5/41 (12.2) | ||
| QAlb > Qlim(Alb), all LPs | Pattern I | 4/17 (23.5) | P < 0.002 |
| Patterns II + III | 30/43 (69.8) | ||
| Pattern I | 4/17 (23.5) | P = 0.002 | |
| Pattern II | 16/26 (61.5) | ||
| Pattern III | 14/17 (82.4) | ||
| QAlb, all LPs | Pattern I | 4.81 (3.01–10.8; 17) | P < 0.005 |
| Patterns II + III | 8.39 (2.1–33.9; 42) | ||
| Albumin CSF, all LPs | Pattern I | 204 (95–517; 17) | P < 0.009 |
| Patterns II + III | 331 (81.2–726; 41) | ||
| Total CSF protein elevated, all LPs | Pattern I | 3/15 (20) | P < 0.003 |
| Patterns II + III | 29/43 (67.4) | ||
| Total CSF protein, all LPs | Pattern I | 375 (187–750; 15) | P < 0.007 |
| Patterns II + III | 550 (168–1930; 43) | ||
| Albuminocytological dissociation, all LPs | Pattern I | 1/8 (12.5) | P < 0.04 |
| Patterns II + III | 13/21 (61.9) |
IgG, IgM and IgA CSF/serum ratios
While 7/17 (41.2) samples from patients with pattern I MS showed elevated QIgG levels, only 5/41 (12.2) of samples from patients with pattern II or pattern III MS did so (P < 0.021) (Table 2). Intrathecal production of IgM as indicated by elevated QIgM was rare and was found both in patients with pattern I MS (3/9; 33.3%) and in patients with pattern II MS (3/12; 25%). QIgA levels were elevated in a few pattern I patients (2/8; 25%), in a single pattern II patient and in none of the pattern III patients (1/17; 5.9%). Data on both the fractions and the absolute amounts of intrathecally produced IgG, IgM and IgA can be found in Tables 2 and 3. Plots of QIgG, QIgA and QIgM, respectively, against QAlb as a measure of blood–CSF barrier function are shown in Fig. 2.
Table 3.
Frequency of intrathecal IgM and IgA synthesis; IgM and IgA CSF/serum ratios; intrathecal IgM and IgA fractions; amount of locally produced IgM and IgA; and absolute CSF and serum IgM and IgA concentrations
| Units | Pattern I MS | Pattern II + III MS | Pattern II MS | Pattern III MS | AQP4-IgG+ NMO [48] | |
|---|---|---|---|---|---|---|
| QIgM > Qlim(IgM) | Patients | 3/9 (33.3) | 3/17 (17.6) | 3/12 (25) | 0/5 (0) | n.d. |
| QIgM > Qlim(IgM), LPs | Samples | 3/16 (18.8) | 5/30 (16.7) | 5/20 (25) | 0/10 (0) | 13/96 (14%) |
| QIgM, all LPs | – | 0.58 (0.26–1.5; 15) | 0.65 (0.1–14.1; 26) | 0.8 (0.1–14.1; 17) | 0.6 (0.5–5.8; 9) | 0.9 (0–40.5; 97) |
| QIgM, if positive | – | 0.8 (0.58–1.5; 3) | 9.8 (3.5–14.1; 5) | 9.8 (3.5–14.1; 5) | n.a. | 8.3 (1.2–40.5; 13) |
| IgMloc, all LPs | mg/L | 0 (0–0.27; 16) | 0 (0–9.24; 29) | 0 (0–9.24; 19) | 0 (0–0; 10) | 0 (0–35.3; 95) |
| IgMloc, QIgM positives | mg/L | 0.12 (0.05–0.27; 3) | 6.41 (0.86–9.24; 5) | 6.41 (0.86–9.24; 5) | n.a. | 0.9 (0–35.3; 13) |
| IgMIF, all LPs | % | 0 (0–0.12; 16) | 0 (0–0.86; 30) | 0 (0–0.86; 20) | 0 (0–0; 10) | 0 (0-95.8; 95) |
| IgMIF, QIgM positives | % | 0.1 (0.09-0.12; 3) | 0.71 (0.17–0.86; 5) | 0.71 (0.17–0.86; 5) | n.a. | 15.3 (2.3–95.8; 13) |
| IgM CSF, all LPs | mg/L | 1 (0.4–3; 15) | 1.05 (0.2–17.8; 26) | 1.2 (0.2–17.8; 17) | 0.9 (0.54–11; 9) | 0.7 (0–36.9; 100) |
| IgM CSF, QIgM positives | mg/L | 1.2 (0.42–3; 3) | 9 (5.4–17.8; 5) | 9 (5.4–17.8; 5) | n.a. | n.d. |
| IgM serum, all LPs | g/L | 1.68 (0.56–3.75; 16) | 1.6 (0.38–3.68; 29) | 1.45 (0.38–3.68; 20) | 1.7 (0.9–2.2; 9) | 0.96 (0.13–2.85; 99) |
| IgM serum, QIgM positives | g/L | 1.51 (0.72–2; 3) | 1.1 (0.64–1.5; 5) | 1.1 (0.64–1.5; 5) | n.a. | n.d. |
| QIgA > Qlim(IgA) | Patients | 2/8 (25) | 1/17 (5.9) | 1/12 (8.3) | 0/5 (0) | n.d. |
| QIgA > Qlim(IgA) | Samples | 2/15 (13.3) | 1/29 (3.4) | 1/19 (5.3) | 0/10 (0) | 5/88 (6%) |
| QIgA, all LPs | – | 1.77 (1.01–5.7; 13) | 2.5 (0.82–9.1; 29) | 2.4 (1–6.6; 19) | 3.3 (0.82–9.1; 10) | 2.1 (0–40.4; 88) |
| QIgA, if positive | – | 3.22 (1.73–4.7; 2) | 1 (1–1; 1) | 1 (1–1; 1) | n.a. | 5.1 (3.7–20.2; 5) |
| IgAloc, all LPs | mg/L | 0 (0–3.72; 15) | 0 (0–0.08; 29) | 0 (0–0.08; 19) | 0 (0–0; 10) | 0 (0–3.2; 86) |
| IgAloc, QIgA positives | mg/L | 2.015 (0.31–3.72; 2) | 0.08 (0.08–0.08; 1) | 0.08 (0.08–0.08; 1) | n.a. | 0.3 (0.03–3.2; 5) |
| IgAIF, all LPs | % | 0 (0–0.73; 15) | 0 (0–0.08; 29) | 0 (0–0.08; 19) | 0 (0–0; 10) | 0 (0–7.5; 86) |
| IgAIF, QIgA positives | % | 0.425 (0.12–0.73; 2) | 0.08 (0.08–0.08; 1) | 0.08 (0.08–0.08; 1) | n.a. | 5.6 (0.5–7.5; 5) |
| IgA CSF, all LPs | mg/L | 2.7 (1.4–16.6; 13) | 4.55 (0.24–19.9; 30) | 3.45 (0.24–17.5; 20) | 8.5 (3.1–19.9; 10) | 4.7 (0–131; 95) |
| IgA CSF, QIgA positives | mg/L | 3.79 (2.5–5.08; 2) | 1.1 (1.1–1.1; 1) | 1.1 (1.1–1.1; 1) | n.a. | n.d. |
| IgA serum, all LPs | g/L | 1.53 (0.9–2.9; 15) | 1.88 (0.53–3.8; 29) | 1.55 (0.53–3; 19) | 2.6 (1.2–3.8; 10) | 0.96 (0.13–2.85; 99) |
| IgA serum, QIgA positives | g/L | 1.26 (1.08–1.45; 2) | 1.1 (1.1–1.1; 1) | 1.1 (1.1–1.1; 1) | n.a. | n.d. |
n.a. not applicable, n.d. no data
Concentrations, ratios and fractions are reported as medians; range and total sample numbers examined are given in brackets
Fig. 2.
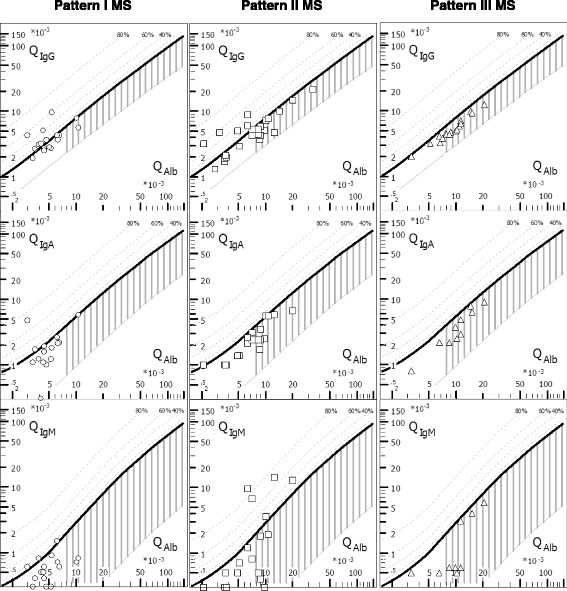
CSF/serum quotient diagrams for IgG, IgM and IgA (‘Reibergrams’). Individual CSF/serum ratios of IgG, IgA and IgM are plotted against CSF/serum albumin ratios. Values above the upper hyperbolic discrimination line, Qlim, indicate intrathecal synthesis of the respective immunoglobulin (Ig) class. Individual intrathecal fractions, IgIF, can be directly read by interpolation from the percentiles above Qlim (median values are given in Tables 2 and 3). Vertical dashed lines indicate the median Qlim(Alb). IgG/A/M immunoglobulin G/A/M, QIgG/A/M CSF/serum IgG/A/M ratios, QAlb CSF/serum albumin ratio
Immunoglobulin class patterns
Intrathecal Ig production, if present, was restricted to one immunoglobulin class in most cases (cf. Table 4 for details). A two-class immune reaction, defined as intrathecal production of either IgG and IgM, or IgM and IgA, or IgG and IgA, was present in only four samples (Table 4). None of the samples showed a three-class immune response, defined as combined elevation of QIgG, QIgM and QIgA. Of note, three pattern II patients showed an isolated IgM reaction at least once (patient 1, intrathecal IgM, IgG and IgA fractions, 83, 47 and 0%, respectively, at first lumbar puncture; 73, 0 and 0% 10 days later; and 71, 0 and 0% 14 days later; patient 2, 37, 0 and 0%; patient 3, 17, 0 and 0% at first puncture, no intrathecal IgM, IgG and IgA synthesis at repeat puncture at day 34 and day 815).
Table 4.
Immunoglobulin class response patterns
| Units | Pattern I MS | Pattern II + III MS | Pattern II MS | Pattern III MS | AQP4-IgG+ NMO [48] | |
|---|---|---|---|---|---|---|
| Three-class reaction | Samples | 0/16 (0) | 0/32 (0) | 0/21 (0) | 0/11 (0) | 0/87 (0%) |
| Two-class reaction | Samples | 2/16 (12.5) | 2/32 (6.3) | 2/21 (9.5) | 0/11 (0) | 5/87 (5.7%) |
| IgG + IgM | Samples | 1 | 1 | 1 | 0 | 1/87 (1.1%) |
| IgG + IgA | Samples | 1 | 1 | 1 | 0 | 1/87 (1.1%) |
| IgM + IgA | Samples | 0 | 0 | 0 | 0 | 3/87 (3.4%) |
| One-class reaction | Samples | 5/16 (31.3) | 6/32 (18.8) | 6/21 (28.6) | 0/11 (0) | 13/87 (14.9%) |
| Only IgG | Samples | 4 | 2 | 2 | 0 | 5/87 (5.7%) |
| Only IgM | Samples | 1 | 4 | 4 | 0 | 7/87 (8%) |
| Only IgA | Samples | 0 | 0 | 0 | 0 | 1/87 (1.1%) |
Concentrations, ratios and fractions are reported as medians; range and total sample numbers examined are given in brackets
QIgG/A/M=CSF/serum IgG/A/M ratios
MRZ reaction
A positive MRZR, as defined by at least two positive IgG-AIs, which has been reported in the literature to be present in around 70% of patients with MS [10–14, 23], was absent in all samples from patients with pattern II or pattern III MS examined (P < 0.000002 compared to unselected MS patients [23]). Only two patients with pattern I MS had been tested for MRZR (positive in 1/2, 50%), precluding statistical comparisons. A positive AI against at least one of the three constituents (measles virus, rubella virus, varicella zoster virus), which has been reported in the literature to be present in 89% (158/177) [19] to 94% (94/100) [14] of patients with MS, was absent in 91% (10/11) of samples from pattern II and III patients (P < 0.000001 vs. references [19] and [14]). MRZR was re-tested in two patients (one with pattern II and one with pattern III MS) later in the disease course and remained negative in both cases. Only a single patient with pattern III MS had a positive AI for measles virus; however, a follow-up examination 1 month later was negative. See Table 5 for details.
Table 5.
Frequency of intrathecal IgG synthesis to infectious agents
| Units | MS, according to literature [14] | Pattern I MS | Pattern II + III MS | Pattern II MS | Pattern III MS | AQP4-IgG+ NMO [13, 23, 43, 55, 56] | MOG-IgG+ EM [35] | |
|---|---|---|---|---|---|---|---|---|
| MRZ reaction (≥2 AIs >1.5) | Patients | 72/100 (72) | 1/2 (50) | 0/10 (0) | 0/7 (0) | 0/3 (0) | 1/42 (2.4) | 0/11 (0) |
| Samples | 72/100 (72) | 1/2 (50) | 0/12 (0) | 0/8 (0) | 0/4 (0) | 1/42 (2.4) | 0/11 (0) | |
| M and/or R and/or Z >1.5 | Samples | 158/177 (89) | 1/2 (50) | 1/11 (9.1) | 0/8 (0) | 1/3 (33.3) | n.d. | n.d. |
| Measles virus AI >1.5 | Samples | 138/177 (78) | 1/2 (50) | 1/10 (10) | 0/8 (0) | 1/4 (25) | 1/42 (2.4) | 0/11 (0) |
| Rubella virus AI >1.5 | Samples | 106/177 (60) | 1/2 (50) | 0/9 (0) | 0/8 (0) | 0/4 (0) | 0/42 (0) | 0/11 (0) |
| Zoster virus AI >1.5 | Samples | 97/177 (55) | 0/2 (0) | 0/9 (0) | 0/8 (0) | 0/4 (0) | 1/42 (2.4) | 0/11 (0) |
| Herpes simplex virus AI >1.5 | Samples | 26/94 (28) | n.d. | 0/4 (0) | 0/4 (0) | 0/1 (0) | n.d. | n.d. |
| Epstein–Barr virus AI >1.5 | Samples | n.d. | 0/2 (0) | 0/2 (0) | n.d. | n.d. | n.d. | 0/2 (0) |
| Borrelia burgdorferi AI >1.5 | Samples | 0/1 (0) | 0/3 (0) | 0/6 (0) | 0/2 (0) | n.d. | 0/1 (0) | 0/3 (0) |
| Toxoplasma gondii AI >1.5 | Samples | n.d. | 0/1 (0) | 0/1 (0) | n.d. | n.d. | n.d. | 0/1 (0) |
| TPHA AI >1.5 | Samples | n.d. | 0/1 (0) | 0/1 (0) | n.d. | n.d. | n.d. | 0/1 (0) |
n.a. not applicable AI antibody index, M measles virus, R rubella virus, TPHA Treponema pallidum haemagglutination assay, Z varicella zoster virus
Blood–CSF barrier integrity
A disrupted blood–CSF barrier function was found in only 4/17 (23.5) of samples from patients with pattern I MS but in 30/43 (69.8) of samples from patients with pattern II or pattern III MS (P < 0.002). Accordingly, median QAlb values and median albumin CSF concentrations were higher in pattern II or III samples than in pattern I samples (P < 0.005 for QAlb, P < 0.009 for CSF albumin). See Table 6 for details.
Table 6.
Blood–CSF barrier function and albumin levels
| Units | Pattern I MS | Pattern II + III MS | Pattern II MS | Pattern III MS | AQP4-IgG+ NMO [48] | |
|---|---|---|---|---|---|---|
| QAlb > Qlim(Alb) | Patients | 4/10 (40) | 15/22 (68.2) | 9/15 (60) | 6/7 (85.7) | n.d. |
| QAlb > Qlim(Alb) | Samples | 4/17 (23.5) | 30/43 (69.8) | 16/26 (61.5) | 14/17 (82.4) | 75/147 (51%) |
| QAlb, all LPs | – | 4.81 (3.01–10.8; 17) | 8.39 (2.1–33.9; 42) | 7.3 (2.1–33.9; 25) | 9 (3.3–20.7; 17) | 7 (2.3–57.1; 137) |
| QAlb, QAlb pos. | – | 8.53 (6.3–10.8; 4) | 9.8 (6.4–33.9; 29) | 9 (6.4–33.9; 15) | 10.25 (6.8––20.7; 14) | 11.8 (5.63–57.14; 70) |
| Albumin CSF, all LPs | mg/L | 204 (95–517; 17) | 331 (81.2–726; 41) | 255.5 (81.2–599; 24) | 368 (137–726; 17) | 284 (83.6–1890; 139) |
| Albumin CSF, QAlb pos. | mg/L | 366 (251–517; 4) | 371.5 (227–726; 28) | 312 (227–599; 14) | 431 (282–726; 14) | 437 (219–1890) |
| Albumin serum, all LPs | g/L | 40.6 (29.3–49.5; 17) | 40 (22.6–51.8; 41) | 39.85 (22.6–51.4; 24) | 41.2 (32.7–51.8; 17) | 40.7 (19.7–67.9; 133) |
| Albumin serum, QAlb pos. | g/L | 43.15 (37.7–47.9; 4) | 39.5 (22.6–50.9; 27) | 35.55 (22.6–46.8; 14) | 39.9 (32.7–50.9; 13) | 39 (19.7–55.9) |
| Combined intrathecal IgG synthesis and disturbed blood–CSF barrier function | ||||||
| Patients, at least once | N (%) | 3/10 (30) | 4/20 (20) | 3/13 (23.1) | 1/7 (14.3) | n.d. |
| All LPs | N (%) | 3/17 (17.6) | 5/43 (11.6) | 4/26 (15.4) | 1/17 (5.9) | 13/74 (17.6%) |
n.d. no data
QAlb = CSF/serum albumin ratio. Concentrations and ratios are reported as medians; range and total sample numbers examined are given in brackets
Cellular immune response
CSF pleocytosis was slightly less frequent in pattern II MS samples (6/26; 23.1%) than in pattern I (5/13; 38.5%) and pattern III (10/14; 71.4%) samples (P < 0.02). However, median CSF white cell count (WCC) were low in all three subgroups, with only 3/49 (6.1%) of samples showing cell counts >40 cells/μL (see Table 7 for details). In patients with pleocytosis, CSF white cells included lymphocytes in all samples examined and monocytes in most, with no significant differences between the groups. Neutrophil granulocytes were present only in five samples from patients with pleocytosis, and the levels were very low (1 × pattern I MS: 7 cells/μL, 5% neutrophils; 1 × pattern II MS: 6 cells/μL, 3% neutrophils; 3 × pattern III MS: 17, 13 and 7 cells/μL, 1–3% neutrophils) and possibly related to slight blood contamination in one case (722 erythrocytes/μL). Eosinophils were present in only two patients with pleocytosis (1 × pattern II MS: 69 cells/μL, 13% eosinophils, absent both in a previous sample and in a follow-up sample, AQP4-IgG: negative; 1 × pattern III MS: 7 cells/μL, 5% eosinophils; no erythrocytes in both cases). Sixty-two percent (13/21) of pattern II/III MS samples without pleocytosis showed an elevated QAlb and, thus, an albuminocytological dissociation, but only 12.5% (1/8) of pattern I MS samples (P < 0.04; see Table 7 for details).
Table 7.
CSF white cell counts
| Units | Pattern I MS | Pattern II + III MS | Pattern II MS | Pattern III MS | AQP4-IgG+ NMO [48] | |
|---|---|---|---|---|---|---|
| Pleocytosis | Samples | 5/13 (38.5) | 16/40 (40) | 6/26 (23.1) | 10/14 (71.4) | 98/194 (50.5) |
| WCC, all LPs | Cells/μL | 5 (1–23; 13) | 3 (0–267; 40) | 2 (0–267; 26) | 8.5 (3–24; 14) | 6 (0–380; 182) |
| WCC, if elevated | Cells/μL | 11 (6–23; 5) | 14.5 (6–267; 16) | 40 (6–267; 6) | 10.5 (7–24; 10) | 19 (6–380; 98) |
| WCC, >40 cells/μL | Samples | 0/13 (0) | 3/36 (8.3) | 3/22 (13.6) | 0/14 (0) | 28/194 (14.4) |
| WCC, >40 cells/μL | Cells/μL | n.a. | 69 (55–267; 3) | 69 (55–267; 3) | n.a. | 94 (43–380; 28) |
| Albuminocytological dissociation | Samples | 1/8 (12.5) | 13/21 (61.9) | 10/18 (55.6) | 3/3 (100) | 27/75 (33.3) |
n.a. not applicable
WCC = white cell count
WCC in the various groups are reported as medians; range and total sample numbers examined are given in brackets
Total CSF protein
Total protein (TP) in the CSF was more frequently elevated in samples from patients with pattern II or III MS samples (29/43; 67.4%) than in pattern I MS (3/15; 20%) (P < 0.003). Accordingly, median TP CSF levels were higher in pattern II or III MS samples (median 550 mg/dl, range 168–1930) than in pattern I MS samples (median 375, range 187–750) (P < 0.006), with the highest levels detected in pattern III samples (median 640, range 260–1277). TP CSF levels >750 mg/dl were present in 8/43 (18.6%) samples from patients with pattern II or III MS, but were not detected in any of the pattern I MS patients. As expected, TP CSF and QAlb were strongly correlated both in the total cohort and within each of the three subgroups (P < 0.0001).
CSF l-lactate
A trend towards higher median l-lactate level was noted in pattern II and III MS (1.9 mmol/L, range 0.8–3.3) compared with pattern I MS (1.3 mmol/L, range 1.1–2.35). Similarly, a higher proportion of patients with pattern II or III MS than patients with pattern I MS had elevated l-lactate levels at least once, but the difference was not statistically significant. See Table 8 for details.
Table 8.
CSF total protein and CSF l-lactate
| Units | Pattern I MS | Pattern II + III MS | Pattern II MS | Pattern III MS | AQP4-IgG+ NMO [48] | |
|---|---|---|---|---|---|---|
| CSF TP elevated | Patients | 3/9 (33.3) | 14/20 (70) | 8/13 (61.5) | 6/7 (85.7) | n.d. |
| CSF TP elevated | Samples | 3/15 (20) | 29/43 (67.4) | 15/26 (57.7) | 14/17 (82.4) | 80/152 (52.6) |
| CSF TP, all LPs | mg/L | 375 (187–750; 15) | 550 (168–1930; 43) | 501 (168–1930; 26) | 640 (260–1277; 17) | 473 (198–3620; 147) |
| CSF TP, if elevated | mg/L | 724 (532–750; 3) | 622 (470–1930; 29) | 571 (471–1930; 15) | 693 (470–1277; 14) | 780 (45.4–3620; 68) |
| CSF TP, >750 mg/L | mg/L | 0/15 (0) | 8/43 (18.6) | 4/26 (15.4) | 4/17 (23.5) | 41/147 (28) |
| CSF lactate elevated | Patients | 2/8 (25) | 6/14 (42.9) | 5/11 (45.5) | 1/3 (33.3) | n.d. |
| CSF lactate elevated | Samples | 2/9 (22.2) | 7/28 (25) | 6/20 (30) | 1/8 (12.5) | 27/83 (32.5) |
| CSF lactate, all LPs | mmol/L | 1.3 (1.1–2.35; 11) | 1.9 (0.8–3.3; 28) | 1.85 (0.8–3.3; 20) | 1.9 (1.36–2.9; 8) | 1.97 (0.87–6.8; 80) |
| CSF lactate, if elevated | mmol/L | 2.175 (2–2.35; 2) | 2.5 (2.2–3.3; 7) | 2.4 (2.2–3.3; 6) | 2.9 (2.9–2.9; 1) | 2.9 (2.1–6.8; 27) |
| CSF lactate, >3 mmol/L | mmol/L | 0/11 (0) | 1/28 (3.6) | 1/20 (5) | 0/8 (0) | 27/80 (33.8) |
n.d. no data
Concentrations are reported as medians; range and total sample numbers examined are given in brackets
Abnormal vs. normal results
Overall, 65/68 (95.6%) LPs showed some abnormality (either intrathecal IgG, IgM or IgA synthesis; disturbed blood–CSF barrier function; or elevated WCC, TP or l-lactate levels); the only three samples with normal results were all from patients with pattern II MS.
A summary of the statistically significant differences between groups can be found in Table 9.
Discussion
In this study, we systematically analysed the results from 68 lumbar punctures in patients who were histopathologically diagnosed with pattern I, pattern II or pattern III MS according to previously published criteria [2]. The most striking finding was the lack of intrathecal IgG synthesis in the vast majority of samples from pattern II or pattern III MS patients. Intrathecal IgG synthesis is considered a diagnostic mainstay of MS. While previous studies reported a frequency of OCB in MS of 90–98% in European patients, 73% of samples from pattern II or pattern III MS patients, including all pattern III patients, were negative in the present European cohort. Moreover, OCBs were positive only transiently in the only two patients with non-pattern I lesions and follow-up data. Transient OCBs have been reported in other neuroinflammatory diseases such as neuromyelitis optica (NMO), acute disseminated encephalomyelitis or CNS infection, whereas OCBs are thought to persist over the entire disease course of MS [24, 25]. Similarly, the polyspecific, intrathecal antiviral IgG response as defined by at least two elevated CSF/serum antibody indices to measles, rubella and/or (so-called MRZ reaction) varicella zoster virus, which is seen in around 70% of patients with MS (and considered to represent non-specific bystander B-cell activation) [10–14, 23], was missing in all patients with pattern II or III lesions tested. Some 91% of the pattern II and III MS samples did not even show a monospecific IgG response to one of the constituents of the MRZR; in contrast, a reaction to at least one of the three viral agents has been found in 89–94% of MS patients [14, 19]. Together, this strongly suggests that patients with pattern II and pattern III lesions are immunopathophysiologically distinct from patients with ‘pattern I MS’ as well as from previous MS cohorts [8, 10, 19].
This notion is further supported by the finding of additional, significant differences in CSF profiles between patients with pattern I lesions and patients with pattern II or III lesions. The latter group significantly more frequently had signs of compromised blood–CSF barrier function, had significantly higher CSF albumin concentrations and significantly higher and more frequently elevated CSF total protein levels (Tables 6 and 9; Fig. 3). In addition, an albuminocytological dissociation was more commonly seen in patients with type II or III lesions.
Fig. 3.
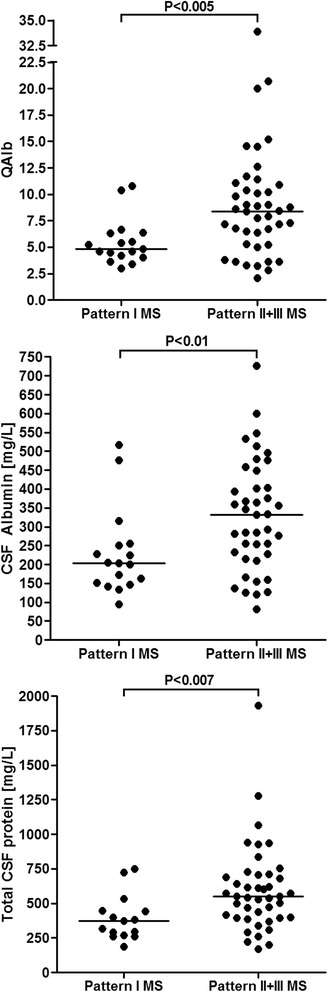
Albumin CSF/serum ratios, CSF albumin concentrations, and CSF total protein concentrations. QAlb CSF/serum albumin ratio
Although intraindividual persistence of a single lesion type over time has been shown in a larger cohort of biopsied patients [4, 5], there is an ongoing discussion on whether the various histopathological lesion patterns identified in MS really represent different entities or rather different stages of the same disease. Given that OCBs are a constant feature in MS, which once acquired does not normally vanish [24, 25] (except in rare patients treated with natalizumab [26, 27], a drug not used in any of our patients), the lack of OCB positivity or persistence in most pattern II and III patients provides particularly strong evidence in favour of the former hypothesis.
The term ‘multiple sclerosis’ refers to a clinicoradiologically defined syndrome. There is currently no proof that all patients presenting with acute CNS demyelination and dissemination in time and space share the same underlying pathogenesis. Instead, several lines of evidence suggest that the current ‘phenotypic’ definition of MS may cover more than one disease: (i) pathological studies have demonstrated histopathological heterogeneity among patients with MS [1, 4, 5]; (ii) clinical studies have shown differences in clinical presentation (‘spinal MS’), course (primary progressive MS without relapses vs. relapsing-remitting MS), severity and prognosis (‘benign MS’); (iii) MRI studies have suggested different lesion types in MS; and (iv) treatment trials have found ‘non-responders’, i.e. patients in whom drugs shown to be effective in the majority of patients with MS were of no benefit. In accordance with that hypothesis, numerous patients previously diagnosed as having variants of MS or ‘opticospinal MS’ based on the current clinicoradiological consensus criteria were found over the past decade to have newly discovered humorally mediated diseases, pathophysiologically distinct from MS, that are now termed AQP4-IgG-positive ‘neuromyelitis optica spectrum’ disorder (NMOSD) [28–33] and MOG-IgG-positive encephalomyelitis (EM) [17, 34–42]. Of note, many of patients with AQP4-IgG-positive NMO or MOG-IgG-positive EM had previously been wrongly diagnosed with MS due to a significant overlap in clinical presentation and clinical criteria and, in consequence, had been wrongly treated with drugs approved for MS but not for NMO or MOG-EM [17, 34–36, 43–47]. In a large European cohort, more than 40% of AQP4-IgG-positive patients with NMOSD had been previously misdiagnosed with MS [43]. Similarly, McDonald’s clinicoradiological criteria or Barkhofs’s radiological for MS were met by 33 and 15%, respectively, of all MOG-IgG-positive patients in a recent study [35]. Wrong diagnosis and, accordingly, false treatment for MS may have caused disease exacerbation and worse outcome in some of those patients, underlining the clinical importance of studies investigating potential heterogeneity in MS [45–47].
AQP4-IgG-positive NMO lesions, MOG-IgG-positive EM lesions and pattern II MS lesions share important histopathological similarities in that all three are characterized by antibody and complement deposits. It is therefore of particular note that many of the CSF findings from patients with pattern II lesions were more similar to what has been reported in AQP4-IgG-positive NMO [43, 48, 49] and MOG-IgG-positive EM [17, 34–36] than to what was found in patients with pattern I lesions in our study (Tables 1, 2, 3, 4, 5, 6, 7, and 8). However, the majority of patients with pattern II and pattern III lesions are negative for AQP4-IgG and MOG-IgG, as were all 10 patients with pattern II or III lesions and available serum samples in the present study [18, 50, 51], suggesting a potential role of other, so far unknown autoantibodies in this condition. In contrast, the CSF findings associated with pattern I lesions were much more in line with what one would expect in patients with typical MS.
Of interest, AQP4-IgG-positive NMO is characterized by a marked female predominance (male to female ratio ~1:10–12) [43]; in contrast, the male to female ratio was 1:2.2 in the pattern II patients and thus more similar to what has been reported in MS and in MOG-IgG-positive EM [35].
In Germany, ≥95% of all MS patients are positive for CSF-restricted OCB [8, 10, 19]. The fact that most pattern II and III patients had no CSF-restricted OCB in our study therefore implies that pattern II and III MS cannot account for the majority of patients with MS. With most pattern II and III patients belonging to the small subgroup of <5% of OCB-negative MS cases, pattern II MS and pattern III MS are probably rare conditions.
This seems to be in contrast to histopathological studies that reported a lower proportion of pattern I cases. However, there are several reasons why pattern II and III cases may be overrepresented in neuropathological cohorts:
As OCBs are considered a hallmark of MS, it seems reasonable to conceive that patients with clinical and radiological findings suggestive of MS but no OCB are more likely to undergo brain biopsy or autopsy than those with OCB. The lack of intrathecal IgG synthesis in patients with pattern II or pattern III lesions may thus result in overrepresentation of pattern II and pattern III patients in histopathological studies.
Tumefactive lesions are more commonly found in pattern II and III patients and certainly tend to prompt biopsies and autopsies more often than conventional lesions. Similarly, most pattern II and III patients in autopsy studies had died from highly active disease (in particular, patients with pattern III lesions, who often had died from fulminant disease within a few months from onset). However, fulminant and highly active disease definitely also tend to prompt biopsy and autopsy. This may again result in an overrepresentation of pattern II/III patients in biopsy/autopsy studies.
Some patients with pattern II lesions are positive for MOG-IgG [4, 18, 52]. MOG encephalomyelitis shows a strong clinical and paraclinical overlap with MS but also significant differences such as ADEM-like presentation, longitudinally extensive and bilateral ON, longitudinally extensive myelitis [17, 34–36]. Again, such ‘MS-atypical’ presentations may tend to prompt biopsy or autopsy and, thus, artificially increase the proportion of pattern II cases in biopsy/autopsy studies.
Our results indicate that the proportion of patients with type II and type III lesions may be particularly high among OCB-negative patients diagnosed with MS. While only 2–10% of patients with MS are negative for OCB according to the literature, this subset is not small in absolute numbers, given the high prevalence of MS in some Western populations (e.g. ~2.3 million patients worldwide; ~140,000 patients in Germany). Given that fact and considering that differences in pathophysiology may well translate into different treatment requirements, as already shown in AQP4-IgG-positive NMO [47] and suggested for MOG-IgG-positive EM [34, 35], studies aiming at enhancing our understanding of the immunopathophysiology of pattern II and III lesions seem highly warranted.
Importantly, the frequency of OCB has been reported to increase with latitude [53, 54]. Whether this implies a higher proportion of patients with ‘pattern I’ lesions at higher latitudes is currently unknown but deserves to be addressed in future studies.
We acknowledge that our study has both strengths and limitations. While we count the high number of CSF samples included (n = 68) and the high number of CSF parameters analysed among the strengths of our study, the retrospective and exploratory study design is a potential limitation. However, prospective studies would be extremely difficult or even impossible to perform given that brain biopsies are only very rarely performed in patients with MS and that lumbar puncture is not anymore required to make the diagnosis of MS according to the current international diagnostic criteria [3].
Conclusions
In summary, the present study provides additional, strong evidence for pattern I MS on the one hand and pattern II MS and pattern III MS on the other hand being distinct entities by demonstrating significant differences in CSF findings between patients with pattern I lesions and patients with pattern II or pattern III lesions, especially with regard to intrathecal IgG synthesis. Of particular note, the CSF profiles present in the pattern II/III subgroup were more similar to those reported in AQP4-IgG-positive NMO and MOG-IgG-positive EM than to those classically considered typical for MS. Further studies are now warranted to confirm our findings in larger, international cohorts. Such studies need to take into account the recently reported increase in frequency of CSF oligoclonal banding in MS with latitude [53, 54].
Acknowledgements
This work was supported by research grants from the Dietmar Hopp Stiftung to BW, from Merck Serono to BW, from the German Federal Ministry of Education and research-funded Competence Network Multiple Sclerosis (KKNMS) to BW, WB and IM, and by a research fellowship from the European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS) to SJ. The authors are thankful to Mrs. Anna Eschlbeck and to the Nikon Imaging Center for the excellent technical assistance. We acknowledge the financial support by Deutsche Forschungsgemeinschaft and Ruprecht-Karls-Universität Heidelberg within the funding programme Open Access Publishing.
Funding
The work of BW was supported by research grants from the Dietmar Hopp Stiftung and from Merck Serono. The work of BW, WB and IM was supported by the German Federal Ministry of Education and Research (BMBF/KKNMS, Competence Network Multiple Sclerosis). The work of SJ was supported by a research grant from the European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS).
Availability of data and materials
The datasets generated during and/or analysed during the current study are not publicly available due to local data protection requirements but are available from the corresponding author on reasonable request in an anonymized fashion.
Abbreviations
- AQP4
Aquaporin-4
- CNS
Central nervous system
- CSF
Cerebrospinal fluid
- EM
Encephalomyelitis
- IgA
Immunoglobulin A
- IgG
Immunoglobulin G
- IgM
Immunoglobulin M
- MOG
Myelin oligodendrocyte glycoprotein
- MRZR
Measles, rubella, zoster reaction
- MS
Multiple sclerosis
- NMO
Neuromyelitis optica
- NMOSD
NMO spectrum disorder
- OCBs
Oligoclonal bands
- QAlb
Albumin CSF/serum ratio
- QIgG/A/M
IgG/A/M CSF/serum ratio
- TP
Total protein
- TPHA
Treponema pallidum haemagglutination assay
- WCC
White cell count
Authors’ contributions
SJ conceived and designed the study, analysed the CSF data and wrote the manuscript. WB, FK and IM provided the histopathological data. WB, FK, IM, BW, FP and KR provided CSF and clinical data. All authors were involved in revising the manuscript for intellectual content. All authors read and approved the final draft before submission.
Ethics approval and consent to participate
The study was approved by the institutional review board of the University of Göttingen, and the patients gave written informed consent.
Consent for publication
Not applicable.
Competing interests
BW has received research grants, speaking fees and travel grants from Merck Serono, Biogen, Teva, Novartis, Sanofi Genzyme, Bayer Healthcare, Biotest and the Dietmar Hopp Foundation. KR has received research support from Novartis as well as speaking fees and travel grants from Guthy Jackson Charitable Foundation, Bayer Healthcare, Biogen Idec, Merck Serono, Sanofi Genzyme, Teva, Roche, and Novartis, none of which is related to the present study. FrP has received research support from Bayer, Novartis, Biogen Idec, Teva, Sanofi-Aventis/Genzyme, Merck Serono, Alexion, Chugai, Arthur Arnstein Stifung Berlin, Guthy Jackson Charitable Foundation and the US National Multiple Sclerosis Society; has received travel funding and/or speaker honoraria from Bayer, Novartis, Biogen Idec, Teva, Sanofi Aventis/Genzyme and Merck Serono; and has consulted for Sanofi Genzyme, Biogen Idec, and MedImmune; none of which is related to the present paper. The other authors report no competing interests. WB has received honoraria for lectures by Bayer Vital, Biogen, Merck Serono, Teva, Genzyme, Roche and Novartis. He is a member of scientific advisory boards for Teva, Biogen, Novartis and Genzyme. WB receives research support from Teva, Biogen, Genzyme and Novartis.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
W.B. and B.W. are equally contributing senior authors.
Contributor Information
S. Jarius, Phone: ++49-6221-56-4747, Email: sven.jarius@med.uni-heidelberg.de
F.B. König, Email: fbkoenig@gmx.net
I. Metz, Email: imetz@gwdg.de
K. Ruprecht, Email: klemens.ruprecht@charite.de
F. Paul, Email: friedemann.paul@charite.de
W. Brück, Email: wbrueck@med.uni-goettingen.de
B. Wildemann, Email: brigitte.wildemann@med.uni-heidelberg.de
References
- 1.Lucchinetti CF, Bruck W, Lassmann H. Evidence for pathogenic heterogeneity in multiple sclerosis. Ann Neurol. 2004;56:308. doi: 10.1002/ana.20182. [DOI] [PubMed] [Google Scholar]
- 2.Lucchinetti C, Bruck W, Parisi J, Scheithauer B, Rodriguez M, Lassmann H. Heterogeneity of multiple sclerosis lesions: implications for the pathogenesis of demyelination. Ann Neurol. 2000;47:707–717. doi: 10.1002/1531-8249(200006)47:6<707::AID-ANA3>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 3.Polman CH, Reingold SC, Banwell B, Clanet M, Cohen JA, Filippi M, Fujihara K, Havrdova E, Hutchinson M, Kappos L, et al. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol. 2011;69:292–302. doi: 10.1002/ana.22366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Konig FB, Wildemann B, Nessler S, Zhou D, Hemmer B, Metz I, Hartung HP, Kieseier BC, Bruck W. Persistence of immunopathological and radiological traits in multiple sclerosis. Arch Neurol. 2008;65:1527–1532. doi: 10.1001/archneur.65.11.1527. [DOI] [PubMed] [Google Scholar]
- 5.Metz I, Weigand SD, Popescu BF, Frischer JM, Parisi JE, Guo Y, Lassmann H, Bruck W, Lucchinetti CF. Pathologic heterogeneity persists in early active multiple sclerosis lesions. Ann Neurol. 2014;75:728–738. doi: 10.1002/ana.24163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tumani H, Deisenhammer F, Giovannoni G, Gold R, Hartung HP, Hemmer B, Hohlfeld R, Otto M, Stangel M, Wildemann B, Zettl UK. Revised McDonald criteria: the persisting importance of cerebrospinal fluid analysis. Ann Neurol. 2011;70:520. doi: 10.1002/ana.22508. [DOI] [PubMed] [Google Scholar]
- 7.Franciotta D, Columba-Cabezas S, Andreoni L, Ravaglia S, Jarius S, Romagnolo S, Tavazzi E, Bergamaschi R, Zardini E, Aloisi F, Marchioni E. Oligoclonal IgG band patterns in inflammatory demyelinating human and mouse diseases. J Neuroimmunol. 2008;200:125–128. doi: 10.1016/j.jneuroim.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 8.Reiber H, Teut M, Pohl D, Rostasy KM, Hanefeld F. Paediatric and adult multiple sclerosis: age-related differences and time course of the neuroimmunological response in cerebrospinal fluid. Mult Scler. 2009;15:1466–1480. doi: 10.1177/1352458509348418. [DOI] [PubMed] [Google Scholar]
- 9.Andersson M, Alvarez-Cermeno J, Bernardi G, Cogato I, Fredman P, Frederiksen J, Fredrikson S, Gallo P, Grimaldi LM, Gronning M, et al. Cerebrospinal fluid in the diagnosis of multiple sclerosis: a consensus report. J Neurol Neurosurg Psychiatry. 1994;57:897–902. doi: 10.1136/jnnp.57.8.897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Reiber H. Cerebrospinal fluid—physiology, analysis and interpretation of protein patterns for diagnosis of neurological diseases. Mult Scler. 1998;4:99–107. doi: 10.1177/135245859800400302. [DOI] [PubMed] [Google Scholar]
- 11.Jarius S, Eichhorn P, Jacobi C, Wildemann B, Wick M, Voltz R. The intrathecal, polyspecific antiviral immune response: specific for MS or a general marker of CNS autoimmunity? J Neurol Sci. 2009;280:98–100. doi: 10.1016/j.jns.2008.08.002. [DOI] [PubMed] [Google Scholar]
- 12.Jarius S, Eichhorn P, Wildemann B, Wick M. Usefulness of antibody index assessment in cerebrospinal fluid from patients negative for total-IgG oligoclonal bands. Fluids Barriers CNS. 2012;9:14. doi: 10.1186/2045-8118-9-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jarius S, Franciotta D, Bergamaschi R, Rauer S, Wandinger KP, Petereit HF, Maurer M, Tumani H, Vincent A, Eichhorn P, et al. Polyspecific, antiviral immune response distinguishes multiple sclerosis and neuromyelitis optica. J Neurol Neurosurg Psychiatry. 2008;79:1134–1136. doi: 10.1136/jnnp.2007.133330. [DOI] [PubMed] [Google Scholar]
- 14.Felgenhauer K, Reiber H. The diagnostic significance of antibody specificity indices in multiple sclerosis and herpes virus induced diseases of the nervous system. Clin Investig. 1992;70:28–37. doi: 10.1007/BF00422934. [DOI] [PubMed] [Google Scholar]
- 15.Jarius S, Probst C, Borowski K, Franciotta D, Wildemann B, Stoecker W, Wandinger KP. Standardized method for the detection of antibodies to aquaporin-4 based on a highly sensitive immunofluorescence assay employing recombinant target antigen. J Neurol Sci. 2010;291:52–56. doi: 10.1016/j.jns.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 16.Jarius S, Paul F, Fechner K, Ruprecht K, Kleiter I, Franciotta D, Ringelstein M, Pache F, Aktas O, Wildemann B. Aquaporin-4 antibody testing: direct comparison of M1-AQP4-DNA-transfected cells with leaky scanning versus M23-AQP4-DNA-transfected cells as antigenic substrate. J Neuroinflammation. 2014;11:129. doi: 10.1186/1742-2094-11-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jarius S, Ruprecht K, Kleiter I, Borisow N, Asgari N, Pitarokoili K, Pache F, Stich O, Beume LA, Hummert MW, et al. MOG-IgG in NMO and related disorders: a multicenter study of 50 patients. Part 1: frequency, syndrome specificity, influence of disease activity, long-term course, association with AQP4-IgG, and origin. J Neuroinflammation. 2016;13:279. doi: 10.1186/s12974-016-0717-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jarius S, Metz I, Konig FB, Ruprecht K, Reindl M, Paul F, Bruck W, Wildemann B. Screening for MOG-IgG and 27 other anti-glial and anti-neuronal autoantibodies in ‘pattern II multiple sclerosis’ and brain biopsy findings in a MOG-IgG-positive case. Mult Scler. 2016;22:1541–1549. doi: 10.1177/1352458515622986. [DOI] [PubMed] [Google Scholar]
- 19.Reiber H, Ungefehr S, Jacobi C. The intrathecal, polyspecific and oligoclonal immune response in multiple sclerosis. Mult Scler. 1998;4:111–117. doi: 10.1177/135245859800400304. [DOI] [PubMed] [Google Scholar]
- 20.Reiber H. Flow rate of cerebrospinal fluid (CSF)—a concept common to normal blood-CSF barrier function and to dysfunction in neurological diseases. J Neurol Sci. 1994;122:189–203. doi: 10.1016/0022-510X(94)90298-4. [DOI] [PubMed] [Google Scholar]
- 21.Petereit HF, Sindern E, Wick M. CSF diagnostics. Guidelines and catalogue of methods of the German Society for Cerebrospinal Fluid Diagnostics and Clinical Neurochemistry. Heidelberg: Springer; 2007. [Google Scholar]
- 22.Wildemann B, Oschmann P, Reiber H. Laboratory diagnosis in neurology. Stuttgart, New York: Thieme; 2011. [Google Scholar]
- 23.Jarius S, Eichhorn P, Franciotta D, Petereit HF, Akman-Demir G, Wick M, Wildemann B. The MRZ reaction as a highly specific marker of multiple sclerosis: re-evaluation and structured review of the literature. J Neurol. 2017;264:453–466. doi: 10.1007/s00415-016-8360-4. [DOI] [PubMed] [Google Scholar]
- 24.Walsh MJ, Tourtellotte WW. Temporal invariance and clonal uniformity of brain and cerebrospinal IgG, IgA, and IgM in multiple sclerosis. J Exp Med. 1986;163:41–53. doi: 10.1084/jem.163.1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Petereit HF, Reske D. Expansion of antibody reactivity in the cerebrospinal fluid of multiple sclerosis patients—follow-up and clinical implications. Cerebrospinal Fluid Res. 2005;2:3. doi: 10.1186/1743-8454-2-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.von Glehn F, Farias AS, de Oliveira AC, Damasceno A, Longhini AL, Oliveira EC, Damasceno BP, Santos LM, Brandao CO. Disappearance of cerebrospinal fluid oligoclonal bands after natalizumab treatment of multiple sclerosis patients. Mult Scler. 2012;18:1038–1041. doi: 10.1177/1352458511428465. [DOI] [PubMed] [Google Scholar]
- 27.Harrer A, Tumani H, Niendorf S, Lauda F, Geis C, Weishaupt A, Kleinschnitz C, Rauer S, Kuhle J, Stangel M, et al. Cerebrospinal fluid parameters of B cell-related activity in patients with active disease during natalizumab therapy. Mult Scler. 2013;19:1209–1212. doi: 10.1177/1352458512463483. [DOI] [PubMed] [Google Scholar]
- 28.Lennon VA, Kryzer TJ, Pittock SJ, Verkman AS, Hinson SR. IgG marker of optic-spinal multiple sclerosis binds to the aquaporin-4 water channel. J Exp Med. 2005;202:473–477. doi: 10.1084/jem.20050304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lennon VA, Wingerchuk DM, Kryzer TJ, Pittock SJ, Lucchinetti CF, Fujihara K, Nakashima I, Weinshenker BG. A serum autoantibody marker of neuromyelitis optica: distinction from multiple sclerosis. Lancet. 2004;364:2106–2112. doi: 10.1016/S0140-6736(04)17551-X. [DOI] [PubMed] [Google Scholar]
- 30.Levy M, Wildemann B, Jarius S, Orellano B, Sasidharan S, Weber MS, Stuve O. Immunopathogenesis of neuromyelitis optica. Adv Immunol. 2014;121:213–242. doi: 10.1016/B978-0-12-800100-4.00006-4. [DOI] [PubMed] [Google Scholar]
- 31.Jarius S, Paul F, Franciotta D, Waters P, Zipp F, Hohlfeld R, Vincent A, Wildemann B. Mechanisms of disease: aquaporin-4 antibodies in neuromyelitis optica. Nat Clin Pract Neurol. 2008;4:202–214. doi: 10.1038/ncpneuro0764. [DOI] [PubMed] [Google Scholar]
- 32.Jarius S, Wildemann B. AQP4 antibodies in neuromyelitis optica: diagnostic and pathogenetic relevance. Nat Rev Neurol. 2010;6:383–392. doi: 10.1038/nrneurol.2010.72. [DOI] [PubMed] [Google Scholar]
- 33.Jarius S, Wildemann B, Paul F. Neuromyelitis optica: clinical features, immunopathogenesis and treatment. Clin Exp Immunol. 2014;176:149–164. doi: 10.1111/cei.12271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jarius S, Kleiter I, Ruprecht K, Asgari N, Pitarokoili K, Borisow N, Hummert MW, Trebst C, Pache F, Winkelmann A, et al. MOG-IgG in NMO and related disorders: a multicenter study of 50 patients. Part 3: brainstem involvement—frequency, presentation and outcome. J Neuroinflammation. 2016;13:281. doi: 10.1186/s12974-016-0719-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jarius S, Ruprecht K, Kleiter I, Borisow N, Asgari N, Pitarokoili K, Pache F, Stich O, Beume LA, Hummert MW, et al. MOG-IgG in NMO and related disorders: a multicenter study of 50 patients. Part 2: epidemiology, clinical presentation, radiological and laboratory features, treatment responses, and long-term outcome. J Neuroinflammation. 2016;13:280. doi: 10.1186/s12974-016-0718-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pache F, Zimmermann H, Mikolajczak J, Schumacher S, Lacheta A, Oertel FC, Bellmann-Strobl J, Jarius S, Wildemann B, Reindl M, et al. MOG-IgG in NMO and related disorders: a multicenter study of 50 patients. Part 4: afferent visual system damage after optic neuritis in MOG-IgG-seropositive versus AQP4-IgG-seropositive patients. J Neuroinflammation. 2016;13:282. doi: 10.1186/s12974-016-0720-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mader S, Gredler V, Schanda K, Rostasy K, Dujmovic I, Pfaller K, Lutterotti A, Jarius S, Di Pauli F, Kuenz B, et al. Complement activating antibodies to myelin oligodendrocyte glycoprotein in neuromyelitis optica and related disorders. J Neuroinflammation. 2011;8:184. doi: 10.1186/1742-2094-8-184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jarius S, Wildemann B. The history of neuromyelitis optica. J Neuroinflammation. 2013;10:8. doi: 10.1186/1742-2094-10-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Brain WR. Critical review: disseminated sclerosis. QJM. 1930;23:343–391. doi: 10.1093/qjmed/os-23.91.343. [DOI] [Google Scholar]
- 40.Weinshenker BG, Wingerchuk DM, Nakashima I, Fujihara K, Lennon VA. OSMS is NMO, but not MS: proven clinically and pathologically. Lancet Neurol. 2006;5:110–111. doi: 10.1016/S1474-4422(06)70333-7. [DOI] [PubMed] [Google Scholar]
- 41.Zamvil SS, Slavin AJ. Does MOG Ig-positive AQP4-seronegative opticospinal inflammatory disease justify a diagnosis of NMO spectrum disorder? Neurol Neuroimmunol Neuroinflamm. 2015;2:e62. doi: 10.1212/NXI.0000000000000062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Reindl M, Jarius S, Rostasy K, Berger T. Myelin oligodendrocyte glycoprotein antibodies: How clinically useful are they? Curr Opin Neurol. 2017;30(3):295–301. [DOI] [PubMed]
- 43.Jarius S, Ruprecht K, Wildemann B, Kuempfel T, Ringelstein M, Geis C, Kleiter I, Kleinschnitz C, Berthele A, Brettschneider J, et al. Contrasting disease patterns in seropositive and seronegative neuromyelitis optica: a multicentre study of 175 patients. J Neuroinflammation. 2012;9:14. doi: 10.1186/1742-2094-9-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wildemann B, Jarius S, Schwarz A, Diem R, Viehöver A, Hähnel S, Reindl M, Korporal-Kuhnke M. Failure of alemtuzumab therapy to control MOG encephalomyelitis. Neurology. 2017;89(2):207–9. [DOI] [PubMed]
- 45.Palace J, Leite MI, Nairne A, Vincent A. Interferon Beta treatment in neuromyelitis optica: increase in relapses and aquaporin 4 antibody titers. Arch Neurol. 2010;67:1016–1017. doi: 10.1001/archneurol.2010.188. [DOI] [PubMed] [Google Scholar]
- 46.Uzawa A, Mori M, Hayakawa S, Masuda S, Kuwabara S. Different responses to interferon beta-1b treatment in patients with neuromyelitis optica and multiple sclerosis. Eur J Neurol. 2010;17:672–676. doi: 10.1111/j.1468-1331.2009.02897.x. [DOI] [PubMed] [Google Scholar]
- 47.Trebst C, Jarius S, Berthele A, Paul F, Schippling S, Wildemann B, Borisow N, Kleiter I, Aktas O, Kumpfel T. Update on the diagnosis and treatment of neuromyelitis optica: recommendations of the Neuromyelitis Optica study group (NEMOS) J Neurol. 2013;261:1–16. doi: 10.1007/s00415-013-7169-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jarius S, Paul F, Franciotta D, Ruprecht K, Ringelstein M, Bergamaschi R, Rommer P, Kleiter I, Stich O, Reuss R, et al. Cerebrospinal fluid findings in aquaporin-4 antibody positive neuromyelitis optica: results from 211 lumbar punctures. J Neurol Sci. 2011;306:82–90. doi: 10.1016/j.jns.2011.03.038. [DOI] [PubMed] [Google Scholar]
- 49.Jarius S, Franciotta D, Paul F, Ruprecht K, Bergamaschi R, Rommer PS, Reuss R, Probst C, Kristoferitsch W, Wandinger KP, Wildemann B. Cerebrospinal fluid antibodies to aquaporin-4 in neuromyelitis optica and related disorders: frequency, origin, and diagnostic relevance. J Neuroinflammation. 2010;7:52. doi: 10.1186/1742-2094-7-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kale N, Pittock SJ, Lennon VA, Thomsen K, Roemer S, McKeon A, Lucchinetti CF. Humoral pattern II multiple sclerosis pathology not associated with neuromyelitis Optica IgG. Arch Neurol. 2009;66:1298–1299. doi: 10.1001/archneurol.2009.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hahn S, Trendelenburg G, Scharf M, Denno Y, Brakopp S, Teegen B, Probst C, Wandinger KP, Buttmann M, Haarmann A, Szabados F, Vom Dahl M, Kümpfel T, Eichhorn P, Gold H, Paul F, Jarius S, Melzer N, Stöcker W, Komorowski L. Identification of the flotillin-1/2 heterocomplex as a target of autoantibodies in bona fide multiple sclerosis. J Neuroinflammation. 2017;14(1):123. [DOI] [PMC free article] [PubMed]
- 52.Spadaro M, Gerdes LA, Mayer MC, Ertl-Wagner B, Laurent S, Krumbholz M, Breithaupt C, Högen T, Straube A, Giese A, et al. Histopathology and clinical course of MOG-antibody-associated encephalomyelitis. Ann Clin Transl Neurol. 2015;2(3):295-301. [DOI] [PMC free article] [PubMed]
- 53.Dobson R, Ramagopalan S, Davis A, Giovannoni G. Cerebrospinal fluid oligoclonal bands in multiple sclerosis and clinically isolated syndromes: a meta-analysis of prevalence, prognosis and effect of latitude. J Neurol Neurosurg Psychiatry. 2013;84:909–914. doi: 10.1136/jnnp-2012-304695. [DOI] [PubMed] [Google Scholar]
- 54.Lechner-Scott J, Spencer B, de Malmanche T, Attia J, Fitzgerald M, Trojano M, Grand'Maison F, Gomez JA, Izquierdo G, Duquette P, et al. The frequency of CSF oligoclonal banding in multiple sclerosis increases with latitude. Mult Scler. 2012;18:974–982. doi: 10.1177/1352458511431729. [DOI] [PubMed] [Google Scholar]
- 55.Pohl D, Rostasy K, Jacobi C, Lange P, Nau R, Krone B, Hanefeld F. Intrathecal antibody production against Epstein-Barr and other neurotropic viruses in pediatric and adult onset multiple sclerosis. J Neurol. 2010;257:212–216. doi: 10.1007/s00415-009-5296-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Brecht I, Weissbrich B, Braun J, Toyka KV, Weishaupt A, Buttmann M. Intrathecal, polyspecific antiviral immune response in oligoclonal band negative multiple sclerosis. PLoS One. 2012;7:e40431. doi: 10.1371/journal.pone.0040431. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analysed during the current study are not publicly available due to local data protection requirements but are available from the corresponding author on reasonable request in an anonymized fashion.


