Abstract
Background
The role of non-infective inflammatory response (IR) in the aetiology of postoperative cognitive dysfunction (POCD) is still controversial. The aim of this controlled, prospective observational study was to assess the possible relationship between the grade of IR, defined by procalcitonin (PCT) changes, and development of POCD related to cardiac surgery.
Methods
Forty-two patients, who were ≥ 60 years of age and scheduled for elective cardiac surgery, were separated into the low inflammatory (LIR) and high inflammatory (HIR) response groups based on their PCT levels measured on the first postoperative day. A matched normative control group of 32 subjects was recruited from primary care practice. The PCT and C-reactive protein (CRP) levels were monitored daily during the first five postoperative days. The cognitive function and mood state were preoperatively tested with a set of five neurocognitive tests and two mood inventories and at the seventh postoperative day. The Reliable Change Index modified for practice (RCIp) using data from normative controls was applied to determine the significant decline in test performance.
Results
The LIR (n = 20) and HIR (n = 22) groups differed significantly in the PCT (p < 0.001) but not in the CRP time courses. The incidence of POCD at the first postoperative week was 35.7% in the cohort. The LIR and HIR groups did not vary in the RCIp Z scores of neurocognitive tests and frequencies of POCD (7 vs 8 cases, respectively, p > 0.05). Additionally, there was no difference in the mood states, anxiety levels and perioperative parameters known to influence the development of POCD.
Conclusions
In this study, the magnitude of the non-infective inflammatory response generated by on-pump cardiac surgery did not influence the development of POCD in the early postoperative period in elderly patients.
Keywords: Cardiac surgery, Cardiopulmonary bypass, Procalcitonin, C-reactive protein, Postoperative cognitive dysfunction, Reliable Change Index
Background
Postoperative cognitive dysfunction (POCD) is known to be an important complication of cardiac and non-cardiac surgeries with marked consequences for the quality of life, work ability and intermediate-term mortality [1–4]. POCD can be characterized by a combined or specific impairment of the working memory, executive function, attention or psychomotor speed [2, 5]. The manifestation of POCD seems to be independent of age; however, it varies among age groups in both the incidence and course [5, 6]. While young and middle-aged patients experience transient cognitive decline, which recovers within a short period, the rate of POCD is up to 50% higher in elderly patients for whom the symptoms are persistent from weeks to months [5–7]. Despite the relevant amount of data published in this field in the last two decades, the explicit incidence of POCD remains debated [8]. This is due to methodological diversities in the definition of POCD or the neurocognitive tests and statistical analyses used [1, 8–10]. Hence, the interpretations of predictors and risk factors of POCD are also unclear for the same reasons. However, advanced age and the extent of surgical trauma are the most established of all investigated factors [5, 11].
The exact pathogenesis of POCD is unknown. Nevertheless, it can be supposed that POCD is a result of interactions between preoperative (patient-related), perioperative and hospital-associated factors [2, 5]. There is a strong evidence that inflammation plays a key role in the development of cognitive decline and dementia in the elderly. Elevated C-reactive protein (CRP) and interleukin-6 (IL-6) were found to be predictors of these in the general population [12–15]. The potential causative factors of POCD, surgical trauma generated inflammatory response and blood-brain barrier (BBB) disruption have been the subject of several clinical investigations in cardiac and non-cardiac surgeries in the past [5, 16, 17]. These studies confirmed a definitive inflammatory response and BBB injury after cardiac surgery in both animal and human investigations [5, 16–18]. However, the direct relationship between inflammatory response and POCD remains controversial [2, 19].
Procalcitonin (PCT) is a widely used biomarker in the diagnosis and antibiotic treatment of sepsis and its quantification has become the part of clinical practice in this field in the last 15 years [20, 21]. Nonetheless, PCT has also been described to be an appropriate indicator of non-infective postoperative inflammatory response [22–24], and it may have prognostic value for some complications related to cardiac surgery [24–26].
The aim of this controlled, prospective observational study was to assess the association between different grades of postoperative inflammatory response characterized by levels of PCT and the frequency of POCD after on-pump cardiac surgery.
Methods
Subjects
Patients who were aged ≥ 60 years and scheduled for elective on-pump cardiac surgery were enrolled in the cardiac surgery group. To create an age-matched, normative control group, subjects aged ≥ 60 years were recruited from primary care practice. The exclusion criteria in the cardiac surgery group, as well as in the normative controls, were significant dementia (Mini Mental State Examination score < 24), a history of cerebrovascular disease, intracranial pathology or psychiatric disease, regular treatment with benzodiazepines or anti-inflammatory drugs (e.g., steroids or non-steroids), elevated baseline PCT or CRP levels, severe left ventricle dysfunction (ejection fraction < 35%) or any kind of organ failure. Surgery or hospitalization within the last 12 months was an additional exclusion criterion in the control group.
Anaesthetic procedure
Anaesthesia was performed using a midazolam bolus 0.05 mg/kg intravenously (IV), sufentanyl bolus 0.5 μg/kg IV, propofol bolus 1 mg/kg IV, or atracurium bolus 0.5 mg/kg IV for induction and then propofol 3–5 mg/kg/h continuous IV and sufentanyl boluses for maintenance of anaesthesia, including the cardiopulmonary bypass (CPB) period. Intraoperative monitoring of patients was based on anaesthesia standards extended with arterial blood pressure, central venous pressure, nasopharyngeal temperature and a bispectral index (BIS, Covidien LLC, Mansfield, MA USA) monitor. The depth of anaesthesia was controlled in range 45–60 of BIS for the entire surgery. CPB was provided by a roller-pump (MAQUET HL 20, MAQUET GmbH & Co. KG, Rastatt, Germany) and membrane oxygenator (MAQUET Quadrox, MAQUET GmbH & Co. KG, Rastatt, Germany). The components of CPB prime were 1200 mL of Ringer lactate, 100 mL of mannitol, and 60 mL of sodium bicarbonate 8.4%. The non-pulsatile flow rate of CPB was maintained in the range of 2.2–2.4 L/min/m2. The mean arterial blood pressure (MAP) was controlled with noradrenaline or glyceryl trinitrate to retain the target MAP of 60–80 mmHg during CPB. Clinical management of anaesthesia and CPB was based on institutional standards, including the temperature, metabolic targets (α-stat acid-base management) and transfusion triggers.
Continuous propofol IV infusion was administered as postoperative sedation during the mechanical ventilation period in the intensive care unit (ICU). Postoperative analgesia consisted of morphine sulphate IV boluses adjusted to the patients’ requirements and 1 g of paracetamol IV infusion (every 6 h as needed). The treatment of study patients in the ICU and cardiothoracic surgical ward did not involve benzodiazepine.
Neuropsychological assessment
The assessment of neurocognitive functions was performed on the day before surgery and the seventh postoperative day in the cardiac surgery group by the following test battery: Mini Mental State Examination (MMSE; dementia screening); Trail Making Tests A and B (TMA and TMB, respectively; executive functions: organized visual search, planning, attention, set shifting, cognitive flexibility, and divided attention); Digit Symbol Test (DS; attention, psychomotor speed, coding task, and visual short-term memory); Stroop Colour and Word Test (cognitive flexibility and control, as well as resistance to interference). The Beck Depression Inventory (BDI; validated in native language [27]) and State-Trait Anxiety Inventory (STAI; validated in native language [28]) were used to examine mood states and anxiety levels at the same time points as the neurocognitive assessment. BDI was only performed preoperatively. Subjects in the normative control group were examined and retested after a time interval of 7 days with the same test battery and protocol. All tests were performed in a specified room separated from the cardiothoracic surgical ward and evaluated by one clinical psychologist who was blinded to the inflammatory status of the patients.
After the collection of test-retest data for each individual, the within-subject change in the performance on neurocognitive tests was measured using the Reliable Change Index modified for practice (RCIp) [29]:
| 1 |
| 2 |
| 3 |
where r xx is test-retest reliability coefficient, SD1 is the standard deviation of the baseline score (normative controls), SEm is the standard error of measurement (normative controls), SEdiff is the standard error of the difference (normative controls) [29], X2 is the postoperative test score and X1 is the preoperative test score (cardiac surgery patients). The practice effect was computed by changes in the mean scores over the test-retest time interval (normative controls). A significant change was considered for an RCIp Z score ≥ ± 1.96 (α = 0.05) in all neurocognitive tests, including the MMSE. POCD was defined by a significant decline in ≥ two neurocognitive tests [10]. The criterion of ≥ 2 scores difference in the MMSE was used to specify the threshold of significance in the comparison of baseline cognitions in the three groups [30, 31]. MMSE scores between 28 and 30 were considered normal cognition, and the range of 24–27 was considered mild cognitive impairment [32].
Measurement of inflammatory markers
Venous blood was collected to measure the PCT and CRP levels at the following six pre-specified time points: before the operation and then every 24 h during the first five postoperative days. Blood samples were analysed using the electrochemiluminescence immunoassay (Elecsys BRAHMS PCT, Roche Diagnostics GmbH, Mannheim, Germany) and particle enhanced turbidimetric assay (COBAS INTEGRA C-Reactive Protein Latex, Roche Diagnostics GmbH, Mannheim, Germany) techniques to quantify the PCT and CRP levels, respectively. Concentrations greater than 0.5 μg/L PCT and 5.0 mg/L CRP were considered elevated levels according to their normal values. The inflammatory response was defined as “low” for PCT ≤ 0.5 μg/L or “high” for PCT > 0.5 μg/L measured on the first postoperative day (POD).
Statistical analysis
Continuous variables were analysed with the Shapiro-Wilk test for normality. Descriptive statistics are presented as the mean ± standard deviation for normally distributed data and the median (interquartile range) for non-normally distributed data. The unpaired t test and Mann-Whitney U test were used for comparisons of group means or medians. The differences in observed frequencies were determined by the χ2 test and Fischer’s exact test. Relationships between variables were assessed using the Spearman correlation test. To justify the sample size of this study, we calculated the statistical power of the difference between the two inflammatory responses post hoc, which was 0.7. Statistical significance was defined at p < 0.05 by all tests. Analysis was performed with IBM® SPSS Statistics version 23.0 (IBM® Armonk, NY, USA).
Results
Seventy-four elderly patients with a mean age of 68 ± 6 years were recruited in the study. The details of patient characteristics and perioperative parameters can be seen in Table 1 and Table 2. The normative controls (n = 32) and patients in the cardiac surgery group (n = 42) were similar in baseline characteristics, including the age, gender and education (Table 1). Test-retest data of the normative controls used to calculate the RCIp Z scores are summarized in Table 3. We found strong test-retest reliability with reliability coefficients between 0.60 and 0.84. One of five cognitive tests (i.e., TMB) was not sensitive to practice.
Table 1.
Baseline neurocognitive and social characteristics of the study population and normative control group
| Normative controls (n = 32) | Study subjects (n = 42) | |
|---|---|---|
| Age (year)a | 68 ± 7 | 69 ± 6 |
| Gender (n) F / Mb | 18 / 14 | 20 / 22 |
| Education (year)c | 14 (9–16) | 12 (11–12) |
| MMSE (score)d | 29 (28–30) | 28 (27–28) |
Data are presented as the mean ± standard deviation, median (interquartile range) and number of patients
aunpaired t test
bχ2 test and Fischer’s exact test
cMann-Whitney U test. F female, M male, and MMSE Mini Mental State Examination. There is no significant difference between normative controls and study subjects regarding age, gender and education
dBased on the a priori criterion of a significant difference in MMSE scores (i.e., ≥ 2 scores [30, 31]), the median MMSE scores do not differ in the normative controls and study subjects. Additionally, there is no difference in the baseline cognition between the two groups
Table 2.
Patient characteristics and perioperative clinical data in the low and high inflammatory response groups
| LIR group n = 20 | HIR group n = 22 | |
|---|---|---|
| Preoperative parameters | ||
| Age (year)a | 68 ± 6 | 69 ± 7 |
| Gender (n) F / Mb | 9 / 11 | 11 / 11 |
| Body mass index (kg/m2)c | 29.4 (24.7–33.0) | 27.2 (25.4–28.8) |
| Education (year)c | 11 (11–12) | 12 (11–12) |
| BDI (score)c | 9 (5.3–14.3) | 8.0 (5.0–10.0) |
| STAI-state (score)a | 41.9 ± 10.3 | 41.2 ± 11.4 |
| EuroSCORE (%)c | 3.9 (2.8–5.7) | 4.3 (2.7–7.6) |
| HTN (n)b | 15 | 14 |
| DM (n)b | 5 | 6 |
| CAD (n)b | 8 | 9 |
| PVD (n)b | 3 | 2 |
| COPD (n)b | 3 | 4 |
| Left ventricle EF (%)c | 55 (55–67) | 55 (50–60) |
| Creatinine (μmol/L)a | 74.3 ± 12.6 | 84.0 ± 21.9 |
| Antihypertensives (n)b | 15 | 14 |
| Statin use (n)b | 11 | 5 |
| Antiplatelet drug (n)b | 11 | 6 |
| Type of surgery | ||
| CABG (n)b | 6 | 5 |
| Single valve (n)b | 11 | 13 |
| Combined (n)b | 3 | 4 |
| Intraoperative parameters | ||
| Aorta cross-clamp time (minute)a | 67 ± 22 | 64 ± 20 |
| CPB time (minute)a | 92 ± 23 | 91 ± 22 |
| Rewarming time (minute)c | 18 (14–22) | 17 (10–21) |
| CPB temperature (°C)c | 35.0 (34.7–35.4) | 35.2 (34.7–35.5) |
| Operation time (minute)a | 193 ± 27 | 181 ± 41 |
| Bispectral indexa | 44.3 ± 6.0 | 43.1 ± 5.6 |
| Propofol (mg/kg/h)a | 4.1 ± 1.5 | 4.3 ± 1.3 |
| Sufentanyl (μg/kg/h)c | 0.27 (0.2–0.35) | 0.28 (0.21–0.3) |
The results are presented as the mean ± standard deviation, median (interquartile range) and number of patients
aunpaired t test
bχ2 test and Fischer’s exact test
cMann-Whitney U test. LIR low inflammatory response, HIR high inflammatory response, F female, M male, BDI Beck Depression Inventory, STAI State-Trait Anxiety Inventory, HTN hypertension, DM diabetes mellitus, CAD coronary artery disease, PVD peripheral vascular disease, COPD chronic obstructive pulmonary disease, EF ejection fraction, CABG coronary artery bypass graft, and CPB cardiopulmonary bypass. There are no significant differences between the two groups regarding all parameters listed in this table
Table 3.
Statistical parameters of the Reliable Change Index modified for practice measured in normative controls
| Cognitive test | r xx | PE | SEdiff |
|---|---|---|---|
| MMSE | 0.66 | 0.5*** | 0.9 |
| TMA | 0.71 | −7.6** | 14.0 |
| TMB | 0.60 | −9.0 | 29.1 |
| DS | 0.81 | 2.5* | 6.1 |
| Stroop W | 0.66 | 1.6*** | 5.7 |
| Stroop C | 0.84 | 3.0*** | 4.8 |
| Stroop CW | 0.80 | 5.1*** | 5.2 |
r xx test-retest reliability coefficient, PE practice effect, and SE diff standard error of the difference. The significance of PE was tested using paired t test. * p < 0.05; ** p < 0.01, and *** p < 0.001; MMSE Mini Mental State Examination, TMA Trail Making Test A, TMB Trail Making Test B, DS Digit Symbol test, Stroop W Stroop word task, Stroop C Stroop colour task and Stroop CW Stroop colour-word task
Based on the a priori definition, cardiac surgery patients were separated into the low inflammatory response (LIR, n = 20) and high inflammatory response (HIR, n = 22) groups. While the PCT peaked at a level of 7.71 (3.90–21.52) μg/L on POD1 and then returned to 0.87 (0.48–2.50) μg/L by POD5 in the HIR group, it remained within the normal range (PCT ≤ 0.5 μg/L) with a maximum value of 0.18 (0.11–0.26) μg/L in the LIR group throughout the postoperative period (Fig. 1a). CRP reached its highest serum levels between POD2 and POD3 in both the LIR and HIR groups (166.5 (154.6–210.7) mg/L vs 138.1 (115.5–187.6) mg/L, p = 0.05, respectively) and did not show significant differences between the two groups during the first five postoperative days (Fig. 1b). The white blood cell (WBC) count had a significantly higher peak value on POD1 in the HIR group compared to the LIR group: 15.0 (11.9–19.5) G/L vs 12.8 (10.8–14.5) G/L, p = 0.012, respectively (Fig. 1c), and it showed a strong correlation with the PCT level on the first postoperative day in the HIR group (r = 0.67, p = 0.001). We did not find a correlation between the peak PCT and peak CRP values in either the HIR or LIR group (r = 0.10, p = 0.67 and r = − 0.42, p = 0.06, respectively). There were no differences between the LIR and HIR groups in the preoperative statin use, complexity of cardiac surgery, aorta cross-clamp time and CPB time (Table 2).
Fig. 1.
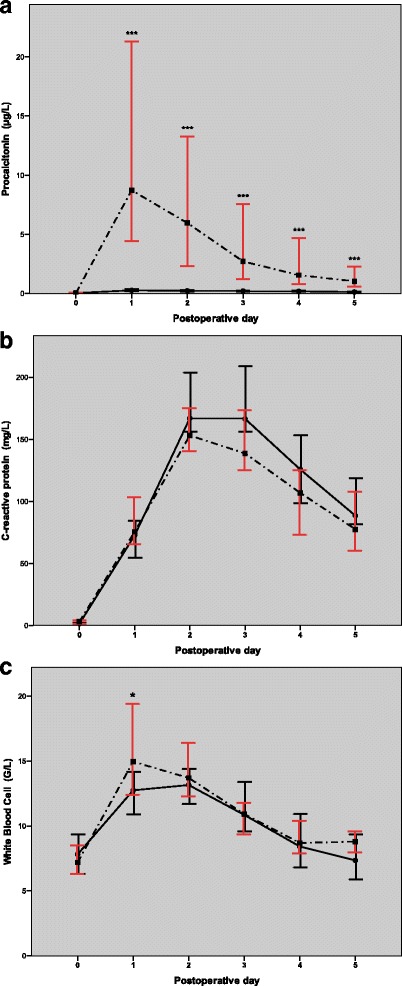
Changes in the procalcitonin (a), C-reactive protein (b) and white blood cell count (c) levels during the postoperative period. A continuous line demonstrates low inflammatory response (LIR) and a dotted line shows the high inflammatory response (HIR) group. Spots and error bars represent the medians and 95% confidence intervals. Significant differences between the LIR and HIR groups are demonstrated with asterisks: *** p < 0.001, Mann-Whitney U test
Seventy-four percent of cardiac surgical patients (n = 31) had a significantly decreased performance in at least one cognitive test according to their RCIp Z scores 1 week after surgery. Cognitive flexibility and control were the most vulnerable tasks to cardiac surgery, as demonstrated by the Stroop word-colour task results. Additionally, 38.1% of patients (n = 16) had a significant decline in this test. Based on the a priori definition of the POCD (i.e., a significant decline at least in two neurocognitive tests), 15 of 42 patients (35.7%) met the criteria of POCD. The RCIp Z scores of each neurocognitive test were similar in the two inflammatory response groups (Fig. 2). Hence, the frequencies of POCD in the LIR group did not vary from that in the HIR group observed at the first postoperative week (7 cases vs 8 cases, respectively). We did not find differences between the LIR and HIR groups in the preoperative BDI scores; pre- and postoperative levels of anxiety; and intraoperative parameters, including the CPB time, body temperature on-CPB, rewarming time on-CPB, operation time, BIS values, propofol and sufentanyl requirements (Table 2). We registered similar postoperative ventilation times in the two inflammatory response groups, LIR: 5.3 (4.4–8.3) hour vs HIR: 5.7 (3.3–7.9) hour, p = 0.60 and the morphine requirement during the first 24 h were also comparable, LIR: 0.11 (0–0.2) mg/kg vs HIR: 0.11 (0–0.3) mg/kg, p = 0.38. Infection or sepsis and delirium did not develop among cardiac surgical patients in the postoperative period. Details of the postoperative outcome are summarized in Table 4.
Fig. 2.
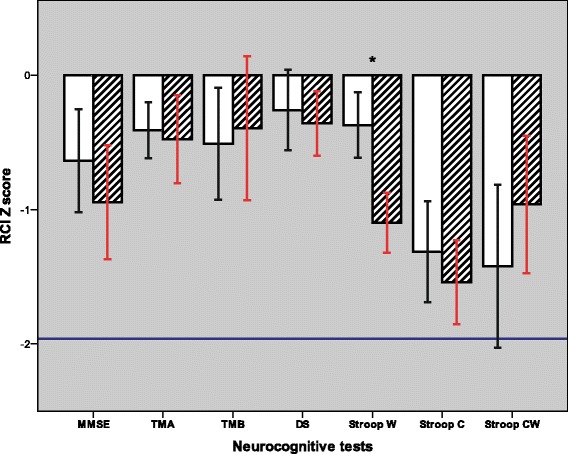
RCIp Z scores of neurocognitive tests. Z score means are demonstrated with a blank bar in the low inflammatory response group and striped bar in the high inflammatory response group. Error bars represent the standard error of the mean. The limit of the significant decline in performance is indicated by a continuous line at RCIp Z score of −1.96. None of the neurocognitive tests showed a significant decline at the group level. The RCIp Z scores were similar in the two inflammatory response groups, except the Stroop word task, based on the Mann-Whitney U test. Significant differences between the LIR and HIR groups are demonstrated with asterisks: * p < 0.05. MMSE = Mini Mental State Examination; TMA = Trail Making Test A; TMB = Trail Making Test B; DS = Digit Symbol test; Stroop W = Stroop word task; Stroop C = Stroop colour task; and Stroop CW = Stroop colour-word task
Table 4.
Postoperative outcome parameters in the low and high inflammatory response groups
| LIR group (n = 20) | HIR group (n = 22) | |
|---|---|---|
| Ventilation time (hour)a | 5.3 (4.4–8.3) | 5.7 (3.3–7.9) |
| Transfused patients (n)b | 6 | 6 |
| PRC (unit)a | 0 (0) | 0 (0–1) |
| Respiratory failure (n)b | 3 | 2 |
| New onset AF(n)b | 5 | 4 |
| Acute kidney injury (n)b | 2 | 5 |
| STAI-state (score)c | 36.7 ± 8.8 | 38.2 ± 8.1 |
| POCD (n)b | 7 | 8 |
| Length-of-ICU-stay (hour)a | 24 (24–46) | 23 (22–60) |
| Length-of-hospital-stay (day)a | 10 (8–17) | 11 (9–13) |
| In-hospital death (n) | 0 | 0 |
Data are presented as the median (interquartile range), number of patients and mean ± standard deviation
aMann-Whitney U test
bχ2 test and Fischer’s exact test
cunpaired t test; LIR low inflammatory response, HIR high inflammatory response, PRC packed red cells, AF atrial fibrillation, STAI State-Trait Anxiety Inventory, POCD postoperative cognitive dysfunction, and ICU intensive care unit. There are no significant differences between the two groups regarding all parameters listed in this table
Discussion
This study was designed to explore whether the grade of postoperative non-infective inflammatory response generated by CPB surgery directly affects the development of POCD. We distinguished between two different inflammatory response levels (i.e., LIR and HIR) of our elderly patients and applied a strict definition of POCD based on statistical change criteria. With the exclusion of confounding factors, our study did not find a direct relationship between the magnitude of non-infective inflammatory response and incidence of POCD.
Defining the inflammatory response related to cardiac surgery
Cardiac surgery is frequently accompanied by non-infective systemic inflammatory response syndrome (SIRS) induced by surgical trauma, CPB, organ ischaemia-reperfusion injuries, a change in the body temperature and endotoxin release [33, 34]. This genetically influenced, complex inflammatory process – depending on its magnitude – can result in multi-organ dysfunction, increasing the risk of mortality in the postoperative period [33, 35, 36]. Numerous inflammatory mediators have been investigated to characterize the inflammatory responses related to cardiac surgery with the purpose of using them as prognostic markers of the complications and outcome [37]. PCT is one of the accepted and widely used inflammatory markers, and it is also applied for follow-up in the cardiac surgery setting [24, 25]. Its use is based on the assumption that proinflammatory cytokines can contribute to PCT induction after surgery [24, 26]. In the case of non-infective SIRS, the PCT concentration increases in the first 24–48 h after cardiac surgery up to its maximum level and returns to the baseline range in the subsequent days [24, 26]. The peak level of PCT seems to be associated with the extent of surgical procedure, duration of aortic cross-clamp and CPB, and the length of operation [24]. Constantly elevated PCT levels in the postoperative period suggest ongoing inflammation due to a possible septic process [20, 24, 38].
In our study, we followed up PCT as a primary and CRP as a secondary inflammatory marker to distinguish the grade of the inflammatory response in the perioperative period. We observed significant differences in the magnitudes of PCT changes in the individuals who were clearly isolated to the LIR and HIR groups. While the main characteristics of the PCT time course in the HIR group were consistent with previous reports as it reached a peak value at 7.71 μg/L on POD1 [35, 38–40], PCT did not exceed the cut-off value of 0.5 μg/L at any time-point in the LIR group (Fig. 1a). Despite the markedly divergent PCT kinetics in the LIR and HIR groups, they did not differ in the perioperative parameters that are supposed to influence the inflammatory response and course, such as the preoperative statin use, duration of aortic cross-clamp and CPB, length of operation, propofol requirements, number of transfusions and postoperative infection [33, 41–44] (Table 2). We also investigated the possible factors of immune priming. Coexisting chronic diseases, such as diabetes mellitus (DM) or peripheral vascular disease (PVD), are frequently accompanied by a pro-inflammatory state, which possibly amplifies the inflammatory response in the postoperative period [2]. However, our comparative analysis did not show differences in DM and PVD between the LIR and HIR groups. These results are similar to the findings of previous studies [36, 45], supporting that an evolving complex inflammatory response to stimuli of CPB surgery is primarily determined by the individual reactivity of cytokines and the proinflammatory-anti-inflammatory balance. In the present study, we found a completely different behaviour of the CRP level compared to PCT. The results published elsewhere show that CRP increases after cardiac surgery irrespective of the extent of the surgery or presence of SIRS [24, 26, 39]. This fact makes the interpretation of the CRP time course uncertain. Our results agree with these findings because the peak CRP did not correlate with peak PCT, and it was markedly elevated in all subjects of the cohort and did not vary between the LIR and HIR groups during the postoperative period. Interestingly, the WBC count did correlate with PCT rather than with CRP in the HIR group. Hence, our data confirm that PCT follow-up is appropriate to discriminate the grade of the non-infective inflammatory response related to cardiac surgery.
Role of the inflammatory response in the development of POCD after cardiac surgery
The occurrence of POCD was 35.7% in this study based on RCIp analysis [29] of neurocognitive tests and the definition of decline in at least two tests. Instead of frequently used fixed cut-off methods (i.e., 20% or 1–2 SD change) [8, 29], we applied RCIp involving the age-matched healthy non-surgical control group to determine the incidence of POCD. RCIp employs statistical change criteria –corrected for measurement error and mean practice effect– to estimate the valid change of performance on a neurocognitive test [8, 29, 46]. There are only a few comparable publications in the literature that apply statistical change criteria methods in a cardiac surgery setting [29, 47–49]. The observed POCD incidence in our elderly group of patients is in line with their findings (36 vs 33–43%, respectively), which supports the conclusion of a recent investigation of Raymond et al. [29] Analyses that use statistical change criteria can considerably contribute to valid estimation of POCD as they minimize the risk of both overestimation and underestimation of decline in the test performance [8, 29].
The main result of this study was that a direct relationship has not been revealed between the degree of PCT elevation and decline in any neurocognitive test or early POCD. The secondary analysis of our data validated this result as perioperative mood states, and predisposing factors of POCD [2, 6, 47, 50] were similar in the two inflammatory response groups defined by the PCT levels (Tables 2 and 4). Furthermore, we did not observe postoperative complications that affect cognitive function. Numerous investigations have focused on the link between proinflammatory cytokines and cognitive dysfunction related to cardiac surgery in the last two decades [2, 17]. Using animal models, Cibelli et al. [51] and Terrando et al. [52] described a potential link between systemic and hippocampal inflammation through the TNF-α, IL-1β and NF-κB pathways, and the impairment of memory as a consequence of the former processes. Jungwirth et al. also confirmed significant cerebral expression of NF-κB in the hippocampus after CPB surgery in a high-quality randomized controlled animal study; however, it was not associated with the neurocognitive outcome [53]. Clinical trials applying arbitrary cut-off criteria for POCD definition in either the cardiac or non-cardiac surgery setting concluded conflicting results on the relationship between pro-inflammatory cytokines and POCD [54–56]. In a recent investigation of elective coronary artery bypass patients, Hudetz et al. demonstrated that short- and medium-term cognitive dysfunction was related to elevated postoperative IL-6 and CRP levels [57]. Their results were based on the POCD definition involving data from the normative population and Z score [57]. By contrast, most recently published large randomized clinical trials have conflicting results on the incidence of POCD or postoperative delirium when they used pharmacological anti-inflammatory treatment (i.e., dexamethasone or methylprednisolone) during non-cardiac and cardiac surgery [19, 58, 59]. This result might strengthen earlier assumptions that factors other than the grade of the inflammatory response play key role in the pathogenesis of POCD [53, 56]. Our results support this concept because we could clearly demonstrate that the incidence of POCD measured in this study does not depend on the magnitude of the inflammatory response.
Limitations
Our investigation has several limitations. First, the study was conducted in a single centre, which influenced the sample size over the study period. The description of the postoperative inflammatory response was based on the PCT, CRP and WBC count measurements, and we did not involve pro-inflammatory cytokines in the analysis for further specifications. Our study did not strictly adhere to the Statement of Consensus on Assessment of Neurobehavioral Outcomes after Cardiac Surgery [60] in terms of the applied neurocognitive tests. This study was designed for the short interval outcome measure that aimed to assess the early changes in cognitive function after cardiac surgery, which restricts the interpretation of our results. Considering the post hoc statistical power of this observational study, our presented results are preliminary results, while these data are not confirmed by further investigations.
Conclusions
Despite the significant difference in the magnitude of the non-infective inflammatory response induced by CPB surgery, the incidence of POCD was similar in the LIR and HIR groups of our elderly patients when POCD was measured in a strict methodological framework. The role of the inflammatory response in the pathogenesis of POCD needs to be cleared by further investigations.
Acknowledgements
None.
Funding
None.
Availability of data and materials
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BBB
Blood-brain barrier
- BDI
Beck Depression Inventory
- CPB
Cardiopulmonary bypass
- CRP
C-reactive protein
- DM
Diabetes mellitus
- DS
Digit Symbol Test
- HIR
High inflammatory response
- ICU
Intensive Care Unit
- IL-6
Interleukin-6
- IV
Intravenously
- LIR
Low inflammatory response
- MAP
Mean arterial pressure
- MMSE
Mini Mental State Examination
- PCT
Procalcitonin
- POCD
Postoperative cognitive dysfunction
- POD
Postoperative day
- PVD
Peripheral vascular disease
- RCIp
Reliable Change Index modified for practice
- rxx
Test-retest reliability coefficient
- SD
Standard deviation
- SEdiff
Standard error of the difference
- SEm
Standard error of measurement
- SIRS
Systemic inflammatory response syndrome
- STAI
State-trait anxiety inventory
- TMA
Trail-Making A
- TMB
Trail-Making B
- WBC
White blood cell
Authors’ contributions
All authors have made substantial contributions to the conception and design of the study. EN, KV, KR, KBK, KIR, FPH, CB and AE participated in the acquisition, analysis and interpretation of data. All authors have been involved in the drafting and review of the manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki and approved by the Regional and Institutional Committee of Science and Research Ethics, Semmelweis University, Budapest, Hungary. Number of ethical approval: No: 99/2012. Date of approval: 13.09.2012. Written informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Endre Nemeth, Email: nemeth.endre@med.semmelweis-univ.hu.
Katalin Vig, Email: vigkata.pszicho@gmail.com.
Kristof Racz, Email: krisracz@yahoo.de.
Kinga B. Koritsanszky, Email: kinga.koritsanszky@gmail.com
Klara I. Ronkay, Email: ronkayk@gmail.com
Fumiko P. Hamvas, Email: hamvas.fumiko.panna@gmail.com
Csaba Borbély, Email: csborbely@gmail.com.
Ajandek Eory, Email: ajandekeory@gmail.com.
Bela Merkely, Email: merkely.bela@kardio.sote.hu.
Janos Gal, Email: gal.janos@med.semmelweis-univ.hu.
References
- 1.Newman MF, Mathew JP, Grocott HP, Mackensen GB, Monk T, Welsh-Bohmer KA, Blumenthal JA, Laskowitz DT, Mark DB. Central nervous system injury associated with cardiac surgery. Lancet. 2006;368(9536):694–703. doi: 10.1016/S0140-6736(06)69254-4. [DOI] [PubMed] [Google Scholar]
- 2.van Harten AE, Scheeren TWL, Absalom AR. A review of postoperative cognitive dysfunction and neuroinflammation associated with cardiac surgery and anaesthesia. Anaesthesia. 2012;67(3):280–293. doi: 10.1111/j.1365-2044.2011.07008.x. [DOI] [PubMed] [Google Scholar]
- 3.Mashour GA, Woodrum DT, Avidan MS. Neurological complications of surgery and anaesthesia. Br J Anaesth. 2015;114(2):194–203. doi: 10.1093/bja/aeu296. [DOI] [PubMed] [Google Scholar]
- 4.Kastaun S, Gerriets T, Schwarz NP, Yeniguen M, Schoenburg M, Tanislav C, Juenemann M. The relevance of postoperative cognitive decline in daily living: results of a 1-year follow-up. J Cardiothorac Vasc Anesth. 2016;30(2):297–303. doi: 10.1053/j.jvca.2015.12.008. [DOI] [PubMed] [Google Scholar]
- 5.Krenk L, Rasmussen LS, Kehlet H. New insights into the pathophysiology of postoperative cognitive dysfunction. Acta Anaesthesiol Scand. 2010;54(8):951–956. doi: 10.1111/j.1399-6576.2010.02268.x. [DOI] [PubMed] [Google Scholar]
- 6.Monk TG, Weldon BC, Garvan CW, Dede DE, Van Der Aa MT, Heilman KM, Gravenstein JS. Predictors of cognitive dysfunction after major noncardiac surgery. Anesthesiology. 2008;108(1):18–30. doi: 10.1097/01.anes.0000296071.19434.1e. [DOI] [PubMed] [Google Scholar]
- 7.Newman MF, Kirchner JL, Phillips-Bute B, Gaver V, Grocott H, Jones RH, Mark DB, Reves JG, Blumenthal JA. Longitudinal assessment of neurocognitive function after coronary-artery bypass surgery. N Engl J Med. 2001;344(6):395–402. doi: 10.1056/NEJM200102083440601. [DOI] [PubMed] [Google Scholar]
- 8.Uysal S, Reich DL. Neurocognitive outcomes of cardiac surgery. J Cardiothorac Vasc Anesth. 2013;27(5):958–971. doi: 10.1053/j.jvca.2012.11.021. [DOI] [PubMed] [Google Scholar]
- 9.Rasmussen LS. Postoperative cognitive dysfunction: incidence and prevention. Best Pract Res Clin Anaesthesiol. 2006;20(2):315–330. doi: 10.1016/j.bpa.2005.10.011. [DOI] [PubMed] [Google Scholar]
- 10.Rudolph JL, Schreiber KA, Culley DJ, McGlinchey RE, Crosby G, Levitsky S, Marcantonio ER. Measurement of post-operative cognitive dysfunction after cardiac surgery: a systematic review. Acta Anaesthesiol Scand. 2010;54(6):663–677. doi: 10.1111/j.1399-6576.2010.02236.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Steinmetz J, Rasmussen LS. Peri-operative cognitive dysfunction and protection. Anaesthesia. 2016;71:58–63. doi: 10.1111/anae.13308. [DOI] [PubMed] [Google Scholar]
- 12.Weaver JD, Huang MH, Albert M, Harris T, Rowe JW, Seeman TE. Interleukin-6 and risk of cognitive decline: Macarthur studies of successful aging. Neurology. 2002;59(3):371–378. doi: 10.1212/WNL.59.3.371. [DOI] [PubMed] [Google Scholar]
- 13.Kuo HK, Yen CJ, Chang CH, Kuo CK, Chen JH, Sorond F. Relation of C-reactive protein to stroke, cognitive disorders, and depression in the general population: systematic review and meta-analysis. Lancet Neurol. 2005;4(6):371–380. doi: 10.1016/S1474-4422(05)70099-5. [DOI] [PubMed] [Google Scholar]
- 14.Tegeler C, O'Sullivan JL, Bucholtz N, Goldeck D, Pawelec G, Steinhagen-Thiessen E, Demuth I. The inflammatory markers CRP, IL-6, and IL-10 are associated with cognitive function-data from the Berlin aging study II. Neurobiol Aging. 2016;38:112–117. doi: 10.1016/j.neurobiolaging.2015.10.039. [DOI] [PubMed] [Google Scholar]
- 15.Simone MJ, Tan ZS. The role of inflammation in the pathogenesis of delirium and dementia in older adults: a review. CNS Neurosci Ther. 2011;17(5):506–513. doi: 10.1111/j.1755-5949.2010.00173.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Merino JG, Latour LL, Tso A, Lee KY, Kang DW, Davis LA, Lazar RM, Horvath KA, Corso PJ, Warach S. Blood-brain barrier disruption after cardiac surgery. Am J Neuroradiol. 2013;34(3):518–523. doi: 10.3174/ajnr.A3251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Peng L, Xu L, Ouyang W. Role of peripheral inflammatory markers in Postoperative Cognitive Dysfunction (POCD): A meta-analysis. PLoS ONE. 2013;8(11) doi: 10.1371/journal.pone.0079624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reinsfelt B, Ricksten SE, Zetterberg H, Blennow K, Fredén-Lindqvist J, Westerlind A. Cerebrospinal fluid markers of brain injury, inflammation, and blood-brain barrier dysfunction in cardiac surgery. Ann Thorac Surg. 2012;94(2):549–555. doi: 10.1016/j.athoracsur.2012.04.044. [DOI] [PubMed] [Google Scholar]
- 19.Ottens TH, Sauër AMC, Peelen LM, De Groot WJ, Buijsrogge MP, Bredée JJ, Buhre WF, Dieleman JM, Van Dijk D, Van Herwerden LA, et al. Effects of dexamethasone on cognitive decline after cardiac surgery a randomized clinical trial. Anesthesiology. 2014;121(3):492–500. doi: 10.1097/ALN.0000000000000336. [DOI] [PubMed] [Google Scholar]
- 20.Wacker C, Prkno A, Brunkhorst FM, Schlattmann P. Procalcitonin as a diagnostic marker for sepsis: a systematic review and meta-analysis. Lancet Infect Dis. 2013;13(5):426–435. doi: 10.1016/S1473-3099(12)70323-7. [DOI] [PubMed] [Google Scholar]
- 21.de Jong E, van Oers JA, Beishuizen A, Vos P, Vermeijden WJ, Haas LE, Loef BG, Dormans T, van Melsen GC, Kluiters YC, et al. Efficacy and safety of procalcitonin guidance in reducing the duration of antibiotic treatment in critically ill patients: a randomised, controlled, open-label trial. Lancet Infect Dis. 2016;16(7):819–827. doi: 10.1016/S1473-3099(16)00053-0. [DOI] [PubMed] [Google Scholar]
- 22.Aouifi A, Piriou V, Blanc P, Bouvier H, Bastien O, Chiari P, Rousson R, Evans R, Lehot JJ. Effect of cardiopulmonary bypass on serum procalcitonin and C-reactive protein concentrations. Br J Anaesth. 1999;83(4):602–607. doi: 10.1093/bja/83.4.602. [DOI] [PubMed] [Google Scholar]
- 23.Kerbaul F, Giorgi R, Oddoze C, Collart F, Guidon C, Lejeune PJ, Villacorta J, Gouin F. High concentrations of N-BNP are related to non-infectious severe SIRS associated with cardiovascular dysfunction occurring after off-pump coronary artery surgery. Br J Anaesth. 2004;93(5):639–644. doi: 10.1093/bja/aeh246. [DOI] [PubMed] [Google Scholar]
- 24.Sponholz C, Sakr Y, Reinhart K, Brunkhorst F. Diagnostic value and prognostic implications of serum procalcitonin after cardiac surgery: A systematic review of the literature. Crit Care. 2006;10(5):R145. [DOI] [PMC free article] [PubMed]
- 25.Dörge H, Schöndube FA, Dörge P, Seipelt R, Voss M, Messmer BJ. Procalcitonin is a valuable prognostic marker in cardiac surgery but not specific for infection. Thorac Cardiovasc Surg. 2003;51(6):322–326. doi: 10.1055/s-2003-45425. [DOI] [PubMed] [Google Scholar]
- 26.Meisner M, Rauschmayer C, Schmidt J, Feyrer R, Cesnjevar R, Bredle D, Tschaikowsky K. Early increase of procalcitonin after cardiovascular surgery in patients with postoperative complications. Intensive Care Med. 2002;28(8):1094–1102. doi: 10.1007/s00134-002-1392-5. [DOI] [PubMed] [Google Scholar]
- 27.Kopp M, Foris N. A szorongás kognitív viselkedésterápiája. Budapest: Végeken Kiadó; 1993. [Google Scholar]
- 28.Sipos K, Sipos M. The development and validation of the Hungarian form of the STAI. In: Spielberger CD, Diaz-Guerrero R, editors. Cross-cultural anxiety. Washington: Hemisphere Publishing Corporation; 1978. pp. 51–61. [Google Scholar]
- 29.Raymond PD, Hinton-Bayre AD, Radel M, Ray MJ, Marsh NA. Assessment of statistical change criteria used to define significant change in neuropsychological test performance following cardiac surgery. Eur J Cardiothorac Surg. 2006;29(1):82–88. doi: 10.1016/j.ejcts.2005.10.016. [DOI] [PubMed] [Google Scholar]
- 30.Stein J, Luppa M, Maier W, Wagner M, Wolfsgruber S, Scherer M, Köhler M, Eisele M, Weyerer S, Werle J, et al. Assessing cognitive changes in the elderly: reliable change indices for the mini-mental state examination. Acta Psychiatr Scand. 2012;126(3):208–218. doi: 10.1111/j.1600-0447.2012.01850.x. [DOI] [PubMed] [Google Scholar]
- 31.Meineke M, Applegate RL, II, Rasmussen T, Anderson D, Azer S, Mehdizadeh A, Kim A, Allard M. Cognitive dysfunction following desflurane versus sevoflurane general anesthesia in elderly patients: A randomized controlled trial 6. Med Gas Res. 2014;4(1):6. doi: 10.1186/2045-9912-4-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chapman KR, Bing-Canar H, Alosco ML, Steinberg EG, Martin B, Chaisson C, Kowall N, Tripodis Y, Stern RA. Mini Mental State Examination and Logical Memory scores for entry into Alzheimer's disease trials. Alzheimers Res Ther. 2016;8(1):9. doi: 10.1186/s13195-016-0176-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Laffey JG, Boylan JF, Cheng DCH. The systemic inflammatory response to cardiac surgery. Anesthesiology. 2002;97(1):215–252. doi: 10.1097/00000542-200207000-00030. [DOI] [PubMed] [Google Scholar]
- 34.Parolari A, Camera M, Alamanni F, Naliato M, Polvani GL, Agrifoglio M, Brambilla M, Biancardi C, Mussoni L, Biglioli P, et al. Systemic inflammation after on-pump and off-pump coronary bypass surgery: a one-month follow-up. Ann Thorac Surg. 2007;84(3):823–828. doi: 10.1016/j.athoracsur.2007.04.048. [DOI] [PubMed] [Google Scholar]
- 35.Kallel S, Jmel W, Jarraya A, Abdenadher M, Frikha I, Karouia A. The role of procalcitonin and N-terminal pro-B-type natriuretic peptide in predicting outcome after cardiac surgery. Perfusion. 2012;27(6):504–511. doi: 10.1177/0267659112454155. [DOI] [PubMed] [Google Scholar]
- 36.Wang JF, Bian JJ, Wan XJ, Zhu KM, Sun ZZ, Lu AD. Association between inflammatory genetic polymorphism and acute lung injury after cardiac surgery with cardiopulmonary bypass. Med Sci Monit. 2010;16(5):CR260–CR265. [PubMed] [Google Scholar]
- 37.Hall R. Identification of inflammatory mediators and their modulation by strategies for the management of the systemic inflammatory response during cardiac surgery. J Cardiothorac Vasc Anesth. 2013;27(5):983–1033. doi: 10.1053/j.jvca.2012.09.013. [DOI] [PubMed] [Google Scholar]
- 38.Meisner M. Pathobiochemistry and clinical use of procalcitonin. Clin Chim Acta. 2002;323(1–2):17–29. doi: 10.1016/S0009-8981(02)00101-8. [DOI] [PubMed] [Google Scholar]
- 39.Delannoy B, Guye ML, Slaiman DH, Lehot JJ, Cannesson M. Effect of cardiopulmonary bypass on activated partial thromboplastin time waveform analysis, serum procalcitonin and C-reactive protein concentrations. Crit Care. 2009;13(6):R180. doi: 10.1186/cc8166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jun KR, Lee JN, Song SA, Oh SH, Lee JY, Shin JH, Kim HR. Serial changes in serum procalcitonin, interleukin 6, and C-reactive protein levels according to non-specific surgical stimulation. Clin Chem Lab Med. 2015;53(4):549–558. doi: 10.1515/cclm-2014-0090. [DOI] [PubMed] [Google Scholar]
- 41.Warren OJ, Smith AJ, Alexiou C, Rogers PLB, Jawad N, Vincent C, Darzi AW, Athanasiou T. The inflammatory response to cardiopulmonary bypass: part 1-mechanisms of pathogenesis. J Cardiothorac Vasc Anesth. 2009;23(2):223–231. doi: 10.1053/j.jvca.2008.08.007. [DOI] [PubMed] [Google Scholar]
- 42.Warren OJ, Watret AL, de Wit KL, Alexiou C, Vincent C, Darzi AW, Athanasiou T. The inflammatory response to cardiopulmonary bypass: part 2-anti-inflammatory therapeutic strategies. J Cardiothorac Vasc Anesth. 2009;23(3):384–393. doi: 10.1053/j.jvca.2008.09.007. [DOI] [PubMed] [Google Scholar]
- 43.Morgan C, Zappitelli M, Gill P. Statin prophylaxis and inflammatory mediators following cardiopulmonary bypass: A systematic review. Crit Care. 2009;13(5):R165. doi: 10.1186/cc8135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sayed S, Idriss NK, Sayyed HG, Ashry AA, Rafatt DM, Mohamed AO, Blann AD. Effects of propofol and isoflurane on haemodynamics and the inflammatory response in cardiopulmonary bypass surgery. Br J Biomed Sci. 2015;72(3):93–101. doi: 10.1080/09674845.2015.11666803. [DOI] [PubMed] [Google Scholar]
- 45.Roth-Isigkeit A, Hasselbach L, Ocklitz E, Brückner S, Ros A, Gehring H, Schmucker P, Rink L, Seyfarth M. Inter-individual differences in cytokine release in patients undergoing cardiac surgery with cardiopulmonary bypass. Clin Exp Immunol. 2001;125(1):80–88. doi: 10.1046/j.1365-2249.2001.01521.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kneebone AC, Andrew MJ, Baker RA, Knight JL. Neuropsychologic changes after coronary artery bypass grafting: use of reliable change indices. Ann Thorac Surg. 1998;65(5):1320–1325. doi: 10.1016/S0003-4975(98)00158-1. [DOI] [PubMed] [Google Scholar]
- 47.Bruce KM, Yelland GW, Smith JA, Robinson SR. Recovery of cognitive function after coronary artery bypass graft operations. Ann Thorac Surg. 2013;95(4):1306–1313. doi: 10.1016/j.athoracsur.2012.11.021. [DOI] [PubMed] [Google Scholar]
- 48.Evered L, Scott DA, Silbert B, Maruff P. Postoperative cognitive dysfunction is independent of type of surgery and anesthetic. Anesth analg. 2011;112(5):1179–85. doi: 10.1213/ANE.0b013e318215217e. [DOI] [PubMed] [Google Scholar]
- 49.Raymond PD, Radel M, Ray MJ, Hinton-Bayre AD, Marsh N. Investigation of factors relating to neuropsychological change following cardiac surgery. Perfusion. 2007;22(1):27–33. doi: 10.1177/0267659107077952. [DOI] [PubMed] [Google Scholar]
- 50.Stroobant N, Vingerhoets G. Depression, anxiety, and neuropsychological performance in coronary artery bypass graft patients: a follow-up study. Psychosomatics. 2008;49(4):326–331. doi: 10.1176/appi.psy.49.4.326. [DOI] [PubMed] [Google Scholar]
- 51.Cibelli M, Fidalgo AR, Terrando N, Ma D, Monaco C, Feldmann M, Takata M, Lever IJ, Nanchahal J, Fanselow MS, et al. Role of interleukin-1β in postoperative cognitive dysfunction. Ann Neurol. 2010;68(3):360–368. doi: 10.1002/ana.22082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Terrando N, Eriksson LI, Kyu Ryu J, Yang T, Monaco C, Feldmann M, Jonsson Fagerlund M, Charo IF, Akassoglou K, Maze M. Resolving postoperative neuroinflammation and cognitive decline. Ann Neurol. 2011;70(6):986–995. doi: 10.1002/ana.22664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jungwirth B, Eckel B, Blobner M, Kellermann K, Kochs EF, Mackensen GB. The impact of cardiopulmonary bypass on systemic interleukin-6 release, cerebral nuclear factor-kappa B expression, and neurocognitive outcome in rats. Anesth Analg. 2010;110(2):312–320. doi: 10.1213/ANE.0b013e3181bbc42e. [DOI] [PubMed] [Google Scholar]
- 54.Li YC, Xi CH, An YF, Dong WH, Zhou M. Perioperative inflammatory response and protein S-100β concentrations ? Relationship with post-operative cognitive dysfunction in elderly patients. Acta Anaesthesiol Scand. 2012;56(5):595–600. doi: 10.1111/j.1399-6576.2011.02616.x. [DOI] [PubMed] [Google Scholar]
- 55.Ramlawi B, Rudolph JL, Mieno S, Feng J, Boodhwani M, Khabbaz K, Levkoff SE, Marcantonio ER, Bianchi C, Sellke FW. C-reactive protein and inflammatory response associated to neurocognitive decline following cardiac surgery. Surgery. 2006;140(2):221–226. doi: 10.1016/j.surg.2006.03.007. [DOI] [PubMed] [Google Scholar]
- 56.Westaby S, Saatvedt K, White S, Katsumata T, Van Oeveren W, Halligan PW. Is there a relationship between cognitive dysfunction and systemic inflammatory response after cardiopulmonary bypass? Ann Thorac Surg. 2001;71(2):667–672. doi: 10.1016/S0003-4975(00)02405-X. [DOI] [PubMed] [Google Scholar]
- 57.Hudetz JA, Gandhi SD, Iqbal Z, Patterson KM, Pagel PS. Elevated postoperative inflammatory biomarkers are associated with short- and medium-term cognitive dysfunction after coronary artery surgery. J Anesth. 2011;25(1):1–9. doi: 10.1007/s00540-010-1042-y. [DOI] [PubMed] [Google Scholar]
- 58.Whitlock RP, Devereaux PJ, Teoh KH, Lamy A, Vincent J, Pogue J, Paparella D, Sessler DI, Karthikeyan G, Villar JC, et al. Methylprednisolone in patients undergoing cardiopulmonary bypass (SIRS): a randomised, double-blind, placebo-controlled trial. Lancet. 2015;386(10000):1243–1253. doi: 10.1016/S0140-6736(15)00273-1. [DOI] [PubMed] [Google Scholar]
- 59.Valentin LSS, Pereira VFA, Pietrobon RS, Schmidt AP, Oses JP, Portela LV, Souza DO, Vissoci JRN, Da Luz VF, De Souza TLMDA, et al. Effects of single low dose of dexamethasone before noncardiac and nonneurologic surgery and general anesthesia on postoperative cognitive dysfunction - A phase III double blind, randomized clinical trial. PLoS ONE. 2016;11(5) doi: 10.1371/journal.pone.0152308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Murkin JM, Newman SP, Stump DA, Blumenthal JA. Statement of consensus on assessment of neurobehavioral outcomes after cardiac surgery. Ann Thorac Surg. 1995;59(5):1289–1295. doi: 10.1016/0003-4975(95)00106-U. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request.


