Abstract
Introduction
Since just after the year 2000 in Quebec, the management of metastatic castration-resistant prostate cancer (mcrpc) has evolved considerably, with the inclusion of docetaxel-based chemotherapy, bone-targeted therapies (zoledronic acid and denosumab), and more recently, abiraterone, enzalutamide, and cabazitaxel for docetaxel-refractory patients. In the present study, we aimed to analyze contemporary mcrpc management patterns and therapy utilization trends in Quebec.
Methods
The study cohort consisted of patients dying of prostate cancer (pca) between January 2001 and December 2013, selected from Quebec public health care insurance databases. Patient selection was based on death from a pca-related cause or therapy used according to the Canadian Urological Association guidelines on mcrpc management. Treatments included chemotherapy (mitoxantrone before 2005 and docetaxel after 2005), abiraterone, bone-targeted therapy (zoledronic acid or denosumab, or both), and palliative radiation therapy (rt). During the study period, neither enzalutamide nor cabazitaxel was publicly reimbursed in Quebec, and as a result, no capture of their use was possible for this study. Multivariate logistic regression was used to identify factors associated with the probability of receiving chemotherapy, bone-targeted therapies, and palliative rt before death from pca.
Results
Overall, the database search identified 3106 patients who died of pca between January 2001 and December 2013. Median age of death was 78 years. Of those 3106 patients, just 2568 (83%) received mcrpc-specific treatments: chemotherapy, abiraterone, palliative rt, or bone-targeted therapy; the other 17% of the patients were managed solely with maximum androgen blockade (androgen deprivation therapy plus anti-androgens) despite a record of pca-related death. Logistic regression analyses indicate that patients dying after 2005 were more likely to have received chemotherapy [odds ratio (or): 1.51; 95% ci: 1.22 to 1.85] and bone-targeted therapy (or: 1.97; 95% ci: 1.64 to 2.37). Age was a significant predictor for the use of chemotherapy, bone-targeted therapy, and palliative rt (ors in the range 0.96–0.98, p < 0.05).
Conclusions
Patient age seems to be a strong determinant in the of selection mcrpc therapy, affecting the probability of the use of chemotherapy, bone-targeted therapy, or palliative rt. Although chemotherapy is still used only in a small percentage of patients, the introduction of new therapies—such as bone-targeted therapy, docetaxel, and abiraterone—affected treatment selection over time. The availability of enzalutamide since February 2014 will likely produce additional changes in mcrpc management.
Keywords: Metastatic castration-resistant prostate cancer, treatments for advanced prostate cancer, health care resource utilization, management of metastatic castration-resistant prostate cancer in Quebec, treatment patterns and trends
INTRODUCTION
Continuous androgen deprivation therapy (adt) is the standard of care for metastatic prostate cancer (pca)1. Androgen deprivation therapy has evolved from being mainly surgical2 to being mostly medically induced by luteinizing hormone–releasing hormone agonists3,4 or antagonists2,5–9. Androgen deprivation therapy successfully reduces tumour burden and improves symptoms, and it can delay disease progression for several years10,11. However, although disease remission is observed in most patients12, most will unfortunately progress to the lethal phase of pca, called metastatic castration-resistant pca (mcrpc). After disease progression to the mcrpc stage, the common practice is to introduce anti-androgens (aas) such as bicalutamide to continuous adt, which produces modest responses13,14. Median overall survival duration in mcrpc is reported in diverse studies to range between 9 and 32 months15–20.
In 2004, docetaxel-based chemotherapy became the standard of care for patients with mcrpc, replacing mitoxantrone21,22. Chemotherapy with docetaxel in the first line for mcrpc has remained the only therapeutic alternative to offer a survival benefit for mcrpc since shortly after the year 2000. Still, use of docetaxel is limited to a small percentage of mcrpc patients17,23,24—mostly those who are younger25,26—and is generally reserved for those with symptomatic mcrpc27. Additionally, because of the high frequency of bone metastasis, the management of mcrpc often requires the use of palliative radiotherapy (rt) and bone-targeted therapies to reduce the disease burden and bone-related morbidity28–31.
Until recently, no clear alternative had emerged for patients with mcrpc progressing after docetaxel chemotherapy. That situation changed after randomized controlled trials showed survival benefits for several new treatments. The therapeutic arsenal now includes four systemic non-chemotherapeutic agents—abiraterone32, enzalutamide19, sipuleucel-T33, and radium-22334—and a new chemotherapeutic drug, cabazitaxel35. Canadian clinical guidelines have since evolved accordingly36.
In 2012, abiraterone was the first drug approved and publicly covered in Quebec for patients having previously received docetaxel, and in 2014, it also became available for patients in the pre-docetaxel setting. Enzalutamide was approved in Quebec in 2014 in the post-docetaxel setting and in 2016 for patients in the pre-docetaxel setting. Radium-223 was approved in 2015; sipuleucel-T was not approved in Canada.
To optimize the use and benefits of the available mcrpc therapies, a better understanding of the management of mcrpc in real life is needed. We therefore used public health care insurance databases in Quebec to undertake a large retrospective population-based study of patients dying from pca during 2001–2013. Our objective was to analyze the contemporary management patterns in this stage of the disease and the therapy utilization trends across the entire province.
METHODS
Study Design
Our observational retrospective cohort study used data from the Régie de l’Assurance Maladie du Québec (ramq) and med-echo databases, both of which are used to administer the public health care insurance programs in Quebec. The med-echo database contains information about acute-care hospitalizations [date of admission, length of stay, and diagnoses (a primary and up to 15 secondary)]. The ramq has four database types:
■ The beneficiary database, containing age, sex, social assistance status, and date of death for all registered people
■ The medical services dataset, containing claims for all inpatient and ambulatory services (date, nature and location of the medical services; diagnoses and procedure codes, plus associated costs)37; all surgical procedure codes in the database are compliant with the Canadian classification of diagnostic, therapeutic, and surgical procedures38
■ The admissibility database, which lists the periods of eligibility for the ramq’s Public Insurance Plan
■ The pharmaceutical database, which provides data about medications dispensed in community drug-stores, including date, drug name, dose, quantity, dosage form, duration of therapy, and drug costs (insured and paid by patients)
All databases contain a unique identifier (the individual’s health insurance number), which serves as a link between them. Approval for our study was obtained from the McGill University Health Centre ethics board and the Comission d’accès à l’information du Québec before data were obtained from the ramq.
Study Population
The study cohort consisted of men 40 years of age and older, who had received adt (medical or surgical castration, or both) and who died between January 2001 and December 2013. Additionally, all patients were required to have a record of pca-related death or at least 1 of the treatments specific to mcrpc in the study period (or both). Per the Canadian guidelines of the time concerning castration-resistant pca (crpc)27 and the availability of treatments through ramq reimbursement, treatments included chemotherapy (mitoxantrone before 2005, docetaxel after 2005), abiraterone, bone-targeted therapy (zoledronic acid or denosumab, or both), and palliative rt. In the available dataset, identification of the chemotherapy drug was not possible, and therefore chemotherapy administered before 2005 was assumed to be mitoxantrone; after 2005, it was assumed to be docetaxel. During the study period, neither enzalutamide nor cabazitaxel was publicly reimbursed in Quebec, and no capture of their utilization was therefore possible in the study. The date of death was defined as the index date. Patient data were collected from first evidence of pca (surgery date, rt date, adt initiation, or diagnosis of pca, back to January 1996) to date of death. Two cohorts were defined based on the year (2005) when docetaxel was integrated into the management of crpc patients in Quebec:
■ Cohort of patients dying from pca before 2005
■ Cohort of patients dying from pca in 2005 onward (that is, patients dying between 2005 and 2013)
Statistical Analysis
Demographics (age of death, residence area), health care resource use, and comorbidities are presented as percentages, means with 95% confidence intervals (cis), or medians with interquartile range (iqr), as applicable. The use of aas (bicalutamide, nilutamide, flutamide, and cyproterone) in the last 2 years of life and the use of mcrpc-specific therapies (chemotherapy, palliative rt, bone-targeted therapy, and abiraterone) were evaluated overall, by year of death (2001 to 2013), by age at death, and by date of death (2001–2005 or 2005–2013).
Multivariate logistic regression models were used to identify factors associated with the probability of receiving chemotherapy, bone-targeted therapy, and palliative rt before death. The models were adjusted for several covariables, as described in the next subsection.
Analyses were performed using the SAS software application (version 9: SAS Institute, Cary, NC, U.S.A.). All tests were 2-sided, with a significance threshold of 5%.
Covariables
Age at death, residence area (rural or urban provincial administrative region), and proximity to a radiation oncology centre were identified at the index date based on data from the beneficiary file. Year of death was considered dichotomous (2001–2005 vs. 2005–2013); each year was also treated individually compared with a year of death of 2013. The presence of comorbidities was identified in the medical, pharmaceutical, and med-echo databases using specific diagnosis codes, procedures, and common drug codes during the 3rd-last to the 2nd-last year of life (mcrpc phase), including cardiovascular disease and chronic diseases such as diabetes, hypertension, and dyslipidemia, which are factors known to be associated with an increased risk for cardiovascular disease and associated mortality39.
RESULTS
Study Population
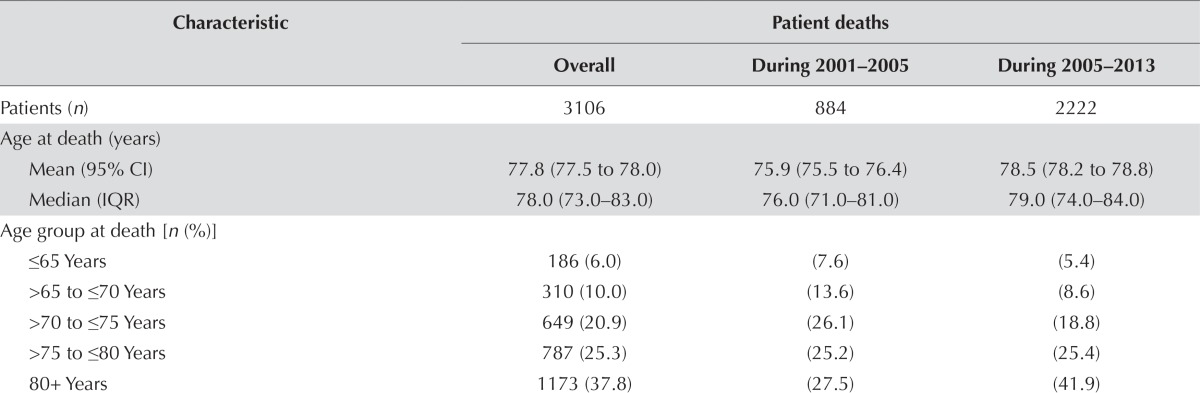
Overall, 3106 patients who died of pca between January 2001 and December 2013 were identified (Table i), with 884 deaths occurring during 2001–2005 and 2222 deaths occurring during 2005–2013. Median age of death was 78 years (iqr: 73–83 years), with the age of death being lower in the 2001–2005 group. Of every 10 patients, almost 8 were living in an urban area (78.0%), and three quarters were living in a region close to a radiation oncology facility (74.7%).
TABLE I.
Characteristics of patients dying of prostate cancer in Quebec during 2001–2013
| Characteristic | Patient deaths | ||
|---|---|---|---|
|
| |||
| Overall | During 2001–2005 | During 2005–2013 | |
| Patients (n) | 3106 | 884 | 2222 |
| Age at death (years) | |||
| Mean (95% CI) | 77.8 (77.5 to 78.0) | 75.9 (75.5 to 76.4) | 78.5 (78.2 to 78.8) |
| Median (IQR) | 78.0 (73.0–83.0) | 76.0 (71.0–81.0) | 79.0 (74.0–84.0) |
| Age group at death [n (%)] | |||
| ≤65 Years | 186 (6.0) | (7.6) | (5.4) |
| >65 to ≤70 Years | 310 (10.0) | (13.6) | (8.6) |
| >70 to ≤75 Years | 649 (20.9) | (26.1) | (18.8) |
| >75 to ≤80 Years | 787 (25.3) | (25.2) | (25.4) |
| 80+ Years | 1173 (37.8) | (27.5) | (41.9) |
| Year of death [n (%)] | |||
| 2001 | 180 (5.8) | (20.4) | |
| 2002 | 257 (8.3) | (29.1) | |
| 2003 | 222 (7.2) | (25.1) | |
| 2004 | 225 (7.2) | (25.5) | |
| 2005 | 223 (7.2) | (10.0) | |
| 2006 | 220 (7.1) | (9.9) | |
| 2007 | 211 (6.8) | (9.5) | |
| 2008 | 234 (7.5) | (10.5) | |
| 2009 | 236 (7.6) | (10.6) | |
| 2010 | 271 (8.7) | (12.2) | |
| 2011 | 276 (8.9) | (12.4) | |
| 2012 | 280 (9.0) | (12.6) | |
| 2013 | 271 (8.7) | (12.2) | |
| Rural residence [n (%)] | 682 (22.0) | (21.7) | (22.1) |
| Proximity to radiation oncology centre [n (%)] | 2319 (74.7) | (74.6) | (74.7) |
| Androgen deprivation therapy [n (%)] | |||
| Surgical | 253 (8.2) | (15.3) | (5.3) |
| Medical castration | 2968 (95.6) | (91.0) | (97.4) |
| Antiandrogens | |||
| Overall | 3029 (97.5%) | (97.2) | (97.7) |
| During last 3 years of life | 2669 (85.9) | (96.2) | (81.9) |
| During last 2 years of life | 2363 (76.1) | (89.1) | (70.9) |
| Tx given any time before death date [n (%)] | |||
| Chemotherapya | 757 (24.4) | (19.5) | (26.3) |
| Palliative radiation therapy | 1261 (40.6) | (44.8) | (38.9) |
| Abiraterone | 210 (6.8) | (0) | (9.5) |
| Bone-targeted therapy | 1129 (36.4) | (25.1) | (40.8) |
| None of the above | 538 (17.3) | (20.7) | (15.9) |
| Comorbiditiesb [n (%)] | |||
| Diabetes | 592 (19.1) | (15.2) | (20.6) |
| Dyslipidemia | 1195 (38.5) | (20.8) | (45.5) |
| Hypertension | 2040 (65.7) | (57.6) | (68.9) |
| Coronary artery disease | 830 (26.7) | (25.2) | (27.3) |
| Chronic heart failure | 335 (10.8) | (10.5) | (10.9) |
| Cerebrovascular disease | 140 (4.5) | (5.8) | (4.0) |
| Arrhythmia | 499 (16.1) | (15.2) | (16.4) |
Per the standard of care (mitoxantrone before 2005; docetaxel after 2005).
In this cohort, 55.2% of patients had 2 or more comorbidities. Comorbidities were registered in the 3rd year preceding death using diagnostics or treatment for chronic diseases [diabetes: ICD-9 code 250 or use of insulin or hypoglycemic agents; dyslipidemia: ICD-9 code 272 or use of lipid-lowering drugs; hypertension: ICD-9 codes 401–404 or use of thiazides or angiotensin converting-enzyme inhibitors (without furosemide, calcium channel blockers, or beta blockers), and without other markers of coronary artery disease], cardiovascular events [coronary artery disease: ICD-9 codes 410–414, ICD-10 codes 122–125, a medical procedure (coronary artery bypass grafting, angiography, or angioplasty) or use of oral nitrate; cerebrovascular disease: ICD-9 codes 430–438 or medical procedures; chronic heart failure: ICD-9 codes 398.91, 402, and 428, or a prescription for furosemide with digoxin, angiotensin converting-enzyme inhibitor, spironolactone, or beta blockers; arrhythmia: diagnosis (ICD-9 codes 426–427), a medical procedure using a pacemaker, and the use of drugs for cardiac arrhythmias (amiodarone, digoxin, quinidine, disopyramide, flecainide, mexiletine, procainamide, propafenone, or sotalol)]39.
CI = confidence interval; IQR = interquartile range; Tx = treatment; ICD = International Classification of Diseases (version 9 or 10).
All patients received adt as either medical (95.6%) or surgical (8.2%) castration. Surgical castration was performed more often in patients dying during 2001–2005 (15.3% vs. 5.3% for patients dying during 2005–2013). Most patients (82.7%) received at least one of the treatments associated with crpc, and aas were given to 97.5% of all patients. Therapy with an aa was initiated concurrently with adt in 62% of the patients, and during the last 3 and 2 years of life respectively, 76.1% and 85.9% of patients received aas. The overall use of therapies for crpc was 24.4% for chemotherapy, 40.6% for palliative rt, 6.8% for abiraterone, and 36.4% for bone-targeted therapy. However, greater use of those treatments was observed in patients dying during 2005–2013.
The most common comorbidities in this cohort were hypertension (65.7%), dyslipidemia (38.5%), coronary artery disease (26.7%), diabetes (19.1%), and arrhythmia (16.1%). More than half the patients in both groups had 2 or more comorbidities (52.0%). A greater use of statins (identified as dyslipidemia) was seen in patients who died during 2005–2013 (45.5%) than in those who died during 2001–2005 (20.8%).
Use of CRPC Treatments
Median duration of systemic therapies was 45 months (iqr: 20–77 months) for adt (n = 2968), 35 months (iqr: 13–66 months) for aas (n = 3029), 6 cycles (iqr: 2–11 cycles) for chemotherapy (n = 757), and 4 months (iqr: 2–7 months) for abiraterone (n = 210). Bone-targeted therapy (n = 1129) continued for a median duration of 8 months (iqr: 3–17 months). Palliative rt was administered in 1 or 2 weeks (n = 1256), with most patients receiving 1 course of palliative rt (59.4%), 31.3% receiving 2 courses, and 10.3% receiving 3 courses during the crpc period.
Overall Use of CRPC Treatments by Age and Year of Death
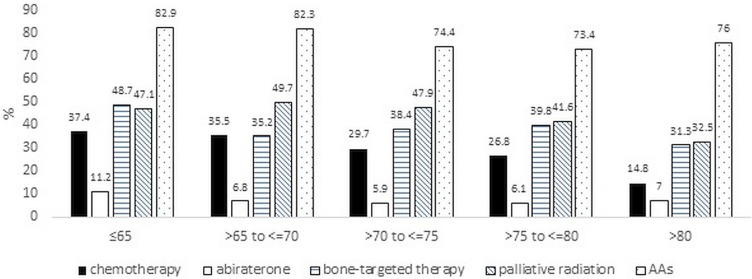
Figure 1 shows the distribution of mcrpc therapies by age-at-death group. Per the overall use of mcrpc treatments, some patterns were observed. In general, the proportion of patients receiving chemotherapy was lower for those 80 years of age and older than for those in other age groups. Use of chemotherapy decreased from 37.4% in patients less than 65 years of age to just 14.8% in patients 80 years of age and older. Small variations in the use of abiraterone, palliative rt, and bone-targeted therapy were evident across age groups, but the lowest rates of use were observed in patients 80 years of age and older.
FIGURE 1.
Percentage of patients receiving treatment for metastatic castration-resistant prostate cancer, by age at death. Overall utilization of chemotherapy, abiraterone, palliative radiation therapy, and bone-targeted therapy. AAs = antiandrogens.
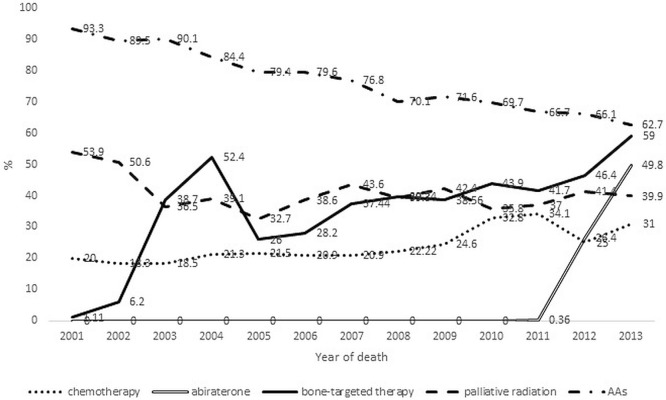
Figure 2 shows time trends for the use of mcrpc therapy in Quebec during 2002–2013. With the exception of aas, palliative rt was the therapy most used in the first 2 years of the study (53.9% and 50.6%), declining to 36.5% in 2003—a proportion that was roughly maintained during the rest of the study period. Use of chemotherapy did not vary much during 2001–2009, but an upward trend was seen in the subsequent years, reaching a peak in 2011 (34.1%), followed by a drop and a rise in the last 2 years of the study. Average chemotherapy use in the period before docetaxel (2001–2004) and in the docetaxel period (2005–2013) was 19.5% and 26.3% respectively. The introduction of bone-targeted therapy in 2002 was followed by a sharp increase in the use of that therapy, which reached its highest level (52.4%) in 2004, with a subsequent decline in 2005 and 2006, followed by another rise to a maximum of 59.0%, reached in 2013. Abiraterone was made available in Quebec only in 2012, when it was used in 26.4% of patients. Abiraterone use almost doubled in the subsequent year, being used in 49.8% of patients in the cohort. Finally, an important decline over time was observed for aas received in the last 2 years of life, ranging from 93.3% in 2001 to 62.7% in 2013.
FIGURE 2.
Time trends of the use, in Quebec, of contemporary treatments in the management of metastatic castration-resistant prostate cancer, by age at death. AAs = antiandrogens.
Factors Associated with the Use of CRPC Treatment
The logistic regression analyses (Table ii) revealed a 51% increase in the use of chemotherapy in patients who died during 2005–2013 (or: 1.51; 95% ci: 1.22 to 1.85), with lesser use in older patients (or: 0.94; 95% ci: 0.93 to –0.95). An increased odds of chemotherapy use was also observed for patients receiving bone-targeted therapy (or: 1.94; 95% ci: 1.63 to 2.31) and for those living near a radiation oncology centre (or: 1.56; 95% ci: 1.26 to 1.93). Moreover, a lesser use of chemotherapy was observed for patients receiving palliative rt (or: 0.64; 95% ci: 0.54 to 0.77).
TABLE II.
Factors associated with the probability of chemotherapy use
| Covariable | Analysis | |||
|---|---|---|---|---|
|
| ||||
| Univariate | Multivariate | |||
|
|
|
|||
| OR | 95% CI | OR | 95% CI | |
| Age at death | 0.94 | 0.93 to 0.95 | 0.94 | 0.93 to 0.95 |
| Death after 2005 | 1.48 | 1.22 to 1.79 | 1.51 | 1.22 to 1.85 |
| Bone-targeted therapy | 2.22 | 1.88 to 2.62 | 1.94 | 1.63 to 2.31 |
| Palliative radiation therapy | 0.74 | 0.63 to 0.88 | 0.64 | 0.54 to 0.77 |
| Rural residence | 1.11 | 0.92 to 1.35 | 1.13 | 0.99 to 1.40 |
| Proximity to radiation oncology centre | 1.35 | 1.11 to 1.64 | 1.56 | 1.26 to 1.93 |
| Comorbiditiesa | ||||
| Diabetes | 1.08 | 0.88 to 1.33 | 0.97 | 0.78 to 1.21 |
| Dyslipidemia | 1.28 | 1.08 to 1.51 | 1.13 | 0.93 to 1.38 |
| Hypertension | 1.05 | 0.88 to 1.24 | 1.18 | 0.96 to 1.45 |
| Coronary artery disease | 0.90 | 0.75 to 1.09 | 1.00 | 0.80 to 1.26 |
| Chronic heart failure | 0.66 | 0.50 to 0.89 | 0.79 | 0.56 to 1.10 |
| Cerebrovascular disease | 0.96 | 0.64 to 1.42 | 1.16 | 0.76 to 1.77 |
| Arrhythmia | 0.71 | 0.56 to 0.90 | 0.87 | 0.67 to 1.14 |
Comorbidities were registered in the 3rd year preceding death using diagnostics or treatment for chronic diseases [diabetes: ICD-9 code 250 or use of insulin or hypoglycemic agents; dyslipidemia: ICD-9 code 272 or use of lipid-lowering drugs; hypertension: ICD-9 codes 401–404 or use of thiazides or angiotensin converting-enzyme inhibitors (without furosemide, calcium channel blockers, or beta blockers), and without other markers of coronary artery disease], cardiovascular events [coronary artery disease: ICD-9 codes 410–414, ICD-10 codes 122–125, a medical procedure (coronary artery bypass grafting, angiography, or angioplasty) or use of oral nitrate; cerebrovascular disease: ICD-9 codes 430–438 or medical procedures; chronic heart failure: ICD-9 codes 398.91, 402, and 428, or a prescription for furosemide with digoxin, angiotensin converting-enzyme inhibitor, spironolactone, or beta blockers; arrhythmia: diagnosis (ICD-9 codes 426–427), a medical procedure using a pacemaker, and the use of drugs for cardiac arrhythmias (amiodarone, digoxin, quinidine, disopyramide, flecainide, mexiletine, procainamide, propafenone, or sotalol)]39.
OR = odds ratio; CI = confidence interval; ICD = International Classification of Diseases (version 9 or 10).
Similar results were observed when evaluating the probability of the use of bone-targeted therapy (Table iii): the probability of receiving that therapy increased for patients who died during 2005–2013 (or: 1.97; 95% ci: 1.64 to 2.37) and for patients who received chemotherapy (or: 1.93; 95% ci: 1.62 to 2.29), and decreased for older patients (or: 0.98; 95% ci: 0.97 to 0.99) and for those who received palliative rt (or: 0.84; 95% ci: 0.71 to 0.98).
TABLE III.
Factors associated with the probability of bone-targeted therapy utilization
| Covariable | Analysis | |||
|---|---|---|---|---|
|
| ||||
| Univariate | Multivariate | |||
|
|
|
|||
| OR | 95% CI | OR | 95% CI | |
| Age at death | 0.98 | 0.97 to 0.98 | 0.98 | 0.97 to 0.99 |
| Death after 2005 | 2.06 | 1.73 to 2.25 | 1.97 | 1.64 to 2.37 |
| Chemotherapy | 2.22 | 1.88 to 2.62 | 1.93 | 1.62 to 2.29 |
| Palliative radiation therapy | 0.84 | 0.73 to 0.98 | 0.84 | 0.71 to 0.98 |
| Rural residence | 1.03 | 0.86 to 1.22 | 0.94 | 0.78 to 1.13 |
| Proximity to radiation oncology centre | 0.92 | 0.78 to 1.08 | 0.88 | 0.74 to 1.06 |
| Comorbiditiesa | ||||
| Diabetes | 1.18 | 0.98 to 1.42 | 1.07 | 0.88 to 1.31 |
| Dyslipidemia | 1.45 | 1.25 to 1.68 | 1.33 | 1.12 to 1.59 |
| Hypertension | 1.07 | 0.91 to 1.25 | 1.03 | 0.96 to 1.23 |
| Coronary artery disease | 0.86 | 0.73 to 1.02 | 0.83 | 0.68 to 1.01 |
| Chronic heart failure | 0.79 | 0.62 to 1.01 | 0.94 | 0.71 to 1.24 |
| Cerebrovascular disease | 0.72 | 0.49 to 1.04 | 0.77 | 0.52 to 1.14 |
| Arrhythmia | 0.77 | 0.63 to 0.95 | 0.87 | 0.69 to 1.09 |
Comorbidities were registered in the 3rd year preceding death using diagnostics or treatment for chronic diseases [diabetes: ICD-9 code 250 or use of insulin or hypoglycemic agents; dyslipidemia: ICD-9 code 272 or use of lipid-lowering drugs; hypertension: ICD-9 codes 401–404 or use of thiazides or angiotensin converting-enzyme inhibitors (without furosemide, calcium channel blockers, or beta blockers), and without other markers of coronary artery disease], cardiovascular events [coronary artery disease: ICD-9 codes 410–414, ICD-10 codes 122–125, a medical procedure (coronary artery bypass grafting, angiography, or angioplasty) or use of oral nitrate; cerebrovascular disease: ICD-9 codes 430–438 or medical procedures; chronic heart failure: ICD-9 codes 398.91, 402, and 428, or a prescription for furosemide with digoxin, angiotensin converting-enzyme inhibitor, spironolactone, or beta blockers; arrhythmia: diagnosis (ICD-9 codes 426–427), a medical procedure using a pacemaker, and the use of drugs for cardiac arrhythmias (amiodarone, digoxin, quinidine, disopyramide, flecainide, mexiletine, procainamide, propafenone, or sotalol)]39.
OR = odds ratio; CI = confidence interval; ICD = International Classification of Diseases (version 9 or 10).
Table iv presents the results for factors associated with the probability of the use of palliative rt. Older age (or: 0.96; 95% ci: 0.95 to 0.97) was again a factor associated with a decreased probability of receiving palliative rt. Furthermore, patients who received chemotherapy (or: 0.64; 95% ci: 0.53 to 0.77) or bone-targeted therapy (or: 0.83; 95% ci: 0.71 to 0.98) had a lesser probability of receiving palliative rt. Proximity to a radiation oncology centre was associated with an increased probability of receiving palliative rt (or: 1.19; 95% ci: 1.00 to 1.41).
TABLE IV.
Factors associated with the probability of the use of palliative radiation therapy
| Covariable | Analysis | |||
|---|---|---|---|---|
|
| ||||
| Univariate | Multivariate | |||
|
|
|
|||
| OR | 95% CI | OR | 95% CI | |
| Age at death | 0.96 | 0.95 to 0.97 | 0.96 | 0.95 to 0.97 |
| Death after 2005 | 0.79 | 0.67 to 0.92 | 0.88 | 0.74 to 1.04 |
| Bone-targeted therapy | 0.84 | 0.73 to 0.98 | 0.83 | 0.71 to 0.98 |
| Chemotherapy | 0.74 | 0.63 to 0.88 | 0.64 | 0.53 to 0.77 |
| Rural residence | 1.06 | 0.89 to 1.26 | 1.05 | 0.87 to 1.25 |
| Proximity to radiation oncology centre | 1.10 | 0.93 to 1.30 | 1.19 | 1.00 to 1.41 |
| Comorbiditiesa | ||||
| Diabetes | 1.07 | 0.89 to 1.28 | 1.03 | 0.85 to 1.24 |
| Dyslipidemia | 1.11 | 0.96 to 1.28 | 1.17 | 0.98 to 1.39 |
| Hypertension | 1.02 | 0.88 to 1.19 | 1.14 | 0.96 to 1.36 |
| Coronary artery disease | 0.95 | 0.81 to 1.11 | 0.96 | 0.79 to 1.17 |
| Chronic heart failure | 0.86 | 0.68 to 1.08 | 0.96 | 0.74 to 1.26 |
| Cerebrovascular disease | 0.78 | 0.55 to 1.11 | 0.82 | 0.57 to 1.18 |
| Arrhythmia | 0.76 | 0.63 to 0.93 | 0.83 | 0.66 to 1.03 |
Comorbidities were registered in the 3rd year preceding death using diagnostics or treatment for chronic diseases [diabetes: ICD-9 code 250 or use of insulin or hypoglycemic agents; dyslipidemia: ICD-9 code 272 or use of lipid-lowering drugs; hypertension: ICD-9 codes 401–404 or use of thiazides or angiotensin converting-enzyme inhibitors (without furosemide, calcium channel blockers, or beta blockers), and without other markers of coronary artery disease], cardiovascular events [coronary artery disease: ICD-9 codes 410–414, ICD-10 codes 122–125, a medical procedure (coronary artery bypass grafting, angiography, or angioplasty) or use of oral nitrate; cerebrovascular disease: ICD-9 codes 430–438 or medical procedures; chronic heart failure: ICD-9 codes 398.91, 402, and 428, or a prescription for furosemide with digoxin, angiotensin converting-enzyme inhibitor, spironolactone, or beta blockers; arrhythmia: diagnosis (ICD-9 codes 426–427), a medical procedure using a pacemaker, and the use of drugs for cardiac arrhythmias (amiodarone, digoxin, quinidine, disopyramide, flecainide, mexiletine, procainamide, propafenone, or sotalol)]39.
OR = odds ratio; CI = confidence interval; ICD = International Classification of Diseases (version 9 or 10).
In addition, a tendency of a lesser probability of receiving chemotherapy, bone-targeted therapy, or palliative rt was associated with some cardiovascular risk factors, although those probabilities were not statistically significant. Moreover, when year of death was considered, comparing each year individually (2001–2012) with a year of death of 2013, the calculated ors confirmed the trends observed in univariate analysis (Figure 2, data not shown).
DISCUSSION
In the present study, we evaluated real-life crpc management patterns and trends in a population-based cohort of patients dying from pca during 2001–2013 in Quebec. More than 8 in 10 patients (82.7%) received at least 1 of the crpc-specific treatments, with almost all of them receiving an aa in the last 2–3 years of life.
Chemotherapy was the least-prescribed crpc treatment and was limited to a small percentage of men even in the docetaxel era. Other real-world studies have shown similar patterns, with secondary hormonal therapy being largely used as the only therapeutic intervention during the mcrpc period40–42. Chemotherapy was prescribed more frequently in younger patients; all other crpc treatments showed a smaller variation with age.
Overall, abiraterone use was modest, given that it was available only in the last 2 years of the study. However, once abiraterone became available, its use increased quickly and significantly. The greater use of abiraterone in patients less than 65 years of age might be explained by the fact that, during the study period, the drug was approved for use only after docetaxel.
As with chemotherapy, bone-targeted therapy and palliative rt were least used in patients 80 years of age and older. That finding accords with results from other studies suggesting a lesser use of palliative rt in older patients43,44.
The use of chemotherapy also varied considerably according to age at death in our cohort: patients less than 65 years of age, compared with those 80 years of age and older, were 2–3 times more likely to receive chemotherapy. The American and Canadian Urological Association guidelines recommend docetaxel chemotherapy only for mcrpc patients with a good performance status20,27. Despite the fact that aging is known to increase the risk of comorbidities that could influence a patient’s performance status, chronologic age seems to have played a role in decision-making and therapy selection in our cohort, more so than the presence of comorbidities. Likewise, Lissbrant et al.25 recently reported that, compared with their younger counterparts, elderly patients were less likely to receive chemotherapy when reaching crpc. Another study revealed a chemotherapy rate of 45.4% in patients with bone metastasis secondary to pca during the 2003–2011 period in the United States45.
In Canada in 2004, after a randomized controlled trial22,46 had demonstrated a 2.4-month survival increment and reduced disease-related burden, docetaxel-based chemotherapy was approved to replace the standard cytotoxic therapy with mitoxantrone. Use of chemotherapy showed an upward trend after 2005, with a peak in 2009, which could be explained by a slow uptake of docetaxel. On average, chemotherapy use remained low in our cohort, with an overall penetrance of less than 25%, similar to usage rates reported in other observational studies24,25,42. The high proportion of patients more than 75 years of age in our population could partly explain the low rate of chemotherapy use overall.
After publication of the results of the cou-aa-301 study32, abiraterone was approved for use in the post-docetaxel setting in 2012. The introduction of abiraterone immediately affected treatment patterns in mcrpc, with a high uptake after reimbursement approval. In 2012, abiraterone use had already surpassed the use of chemotherapy, the only other therapy offering a survival benefit during the study period. Abiraterone use is expected to continue to rise, given that it was later approved (in 2014) for docetaxel-naïve patients progressing after adt. Moreover, compared with chemotherapy agents, abiraterone is associated with fewer high-grade adverse events36. The availability of newer therapies such as enzalutamide and radium-223, which offer a similar overall survival benefit and a moderate toxicity profile, could change that trend.
The multivariate analyses confirmed that the probability of chemotherapy use was associated with age at death, period of death (2001–2005 vs. 2005–2013), proximity to a radiation oncology centre, and use of bone-targeted therapy and palliative rt. Similarly, the probability of receiving bone-targeted therapy was associated with age at death, period of death (2001–2005 vs. 2005–2013), and use of chemotherapy and palliative rt. The probability of palliative rt use was associated with age at death and with use of chemotherapy and bone-targeted therapy.
Our population-based study possesses some limitations inherent in analyses of administrative databases. First, our databases do not provide detailed clinical and pathologic information. Therefore, the use of crpc-specific treatments was used to identify patients with advanced pca who ultimately reached crpc and died of pca. Consequently, some patients not treated with those specific treatments might have been omitted from the cohort. To account for that possibility, cause of death was used to select additional patients with a record of pca-related death. Given that a diagnostic code is not mandatory in the databases, the number of patients dying of pca might be underestimated because some patients might not have received crpc-specific treatments, and for some of them, cause of death might have been missing or inaccurately specified. If patients were missed, crpc treatment use in our cohort could have been overestimated, and the actual use of such treatments might be even smaller than estimated. Additionally, patients not having received crpc-specific treatments might have died from pca without reaching the crpc phase (and thus being ineligible for some crpc therapies such as chemotherapy or abiraterone). Second, some patients selected into the cohort, albeit quite a small number, might have died from other causes. Third, the pharmaceutical database does not include information about hospital-administered drugs, and therefore no analysis for the type of chemotherapeutic drug administered was possible. In our analyses, we assumed that a chemotherapy administration code in the period after 2005 indicated the use of docetaxel; conversely, a chemotherapy code before 2005 was assumed to indicate use of mitoxantrone. Additionally, patients could have participated in clinical trials or received treatments through special access programs before those treatments became publicly approved or available. Access to treatments in such settings is not captured in the ramq administrative databases. The result might be an underestimate of their use in the period before public reimbursement, and consequently, their overall use. Finally, enzalutamide was publically funded in 2014, and it likely contributed to additional changes in mcrpc management that were not captured in the present study.
CONCLUSIONS
Patient age seems to be a strong determinant for the use of mcrpc therapy, with elderly patients being less likely to be given such therapy. The time period was also an important factor for mcrpc treatment use—with the introduction of bone-targeted therapy, post-docetaxel abiraterone, and to a lesser extent, docetaxel—affecting treatment use. The availability of post-docetaxel enzalutamide since February 2014 will likely cause additional changes in mcrpc management. Surprisingly, the use of life-prolonging chemotherapy is still limited to a small proportion of patients, showing only a modest increase after the introduction of docetaxel, despite universal availability throughout the province. The availability of abiraterone (since 2014) and enzalutamide (since 2016) for chemotherapy-naïve patients is very significant, because it will likely increase the overall use of cancer therapies in men dying of pca, and particularly in older patients or those ineligible for chemotherapy. An important area of research will be to examine the effectiveness and cost-effectiveness of the new treatments in routine clinical practice.
CONFLICT OF INTEREST DISCLOSURES
We have read and understood Current Oncology’s policy on disclosing conflicts of interest, and we declare that we have none.
REFERENCES
- 1.National Comprehensive Cancer Network (nccn) NCCN Clinical Practice Guidelines in Oncology: Prostate Cancer. Fort Washington, PA: NCCN; 2011. Ver. 1.2011. [Current version available online at: https://www.nccn.org/professionals/physician_gls/PDF/prostate.pdf (free registration required); cited 19 June 2017] [Google Scholar]
- 2.Moul JW. Prostate cancer: making the switch from lhrh antagonist to lhrh agonist. Nat Rev Urol. 2012;9:125–6. doi: 10.1038/nrurol.2012.5. [DOI] [PubMed] [Google Scholar]
- 3.de Jong IJ, Eaton A, Bladou F. lhrh agonists in prostate cancer: frequency of treatment, serum testosterone measurement and castrate level: consensus opinion from a roundtable discussion. Curr Med Res Opin. 2007;23:1077–80. doi: 10.1185/030079907X187973. [DOI] [PubMed] [Google Scholar]
- 4.Labrie F. Medical castration with lhrh agonists: 25 years later with major benefits achieved on survival in prostate cancer. J Androl. 2004;25:305–13. doi: 10.1002/j.1939-4640.2004.tb02791.x. [DOI] [PubMed] [Google Scholar]
- 5.Cook T, Sheridan WP. Development of gnrh antagonists for prostate cancer: new approaches to treatment. Oncologist. 2000;5:162–8. doi: 10.1634/theoncologist.5-2-162. [DOI] [PubMed] [Google Scholar]
- 6.Keizman D, Eisenberger MA. lhrh antagonists vs lhrh agonists: which is more beneficial in prostate cancer therapy? Oncology (Williston Park) 2009;23:631–2. [PubMed] [Google Scholar]
- 7.Crawford ED, Hou AH. The role of lhrh antagonists in the treatment of prostate cancer. Oncology (Williston Park) 2009;23:626–30. [PubMed] [Google Scholar]
- 8.Weston P, Persson BE. Re: Weckermann D, Harzmann R. Hormone therapy in prostate cancer: lhrh antagonists versus lhrh analogues [Eur Urol 2004;46:279–84] Eur Urol. 2005;47:422. doi: 10.1016/j.eururo.2004.11.015. [DOI] [PubMed] [Google Scholar]
- 9.Schröder F, Crawford ED, Axcrona K, Payne H, Keane TE. Androgen deprivation therapy: past, present and future. BJU Int. 2012;109(suppl 6):1–12. doi: 10.1111/j.1464-410X.2012.11215.x. [DOI] [PubMed] [Google Scholar]
- 10.Huggins C, Hodges CV. Studies on prostatic cancer: I. The effect of castration, of estrogen and of androgen injection on serum phosphatases in metastatic carcinoma of the prostate. 1941. J Urol. 2002;168:9–12. doi: 10.1016/S0022-5347(05)64820-3. [DOI] [PubMed] [Google Scholar]
- 11.Huggins C, Hodges CV. Studies on prostatic cancer. I. The effect of castration, of estrogen and androgen injection on serum phosphatases in metastatic carcinoma of the prostate. CA Cancer J Clin. 1972;22:232–40. doi: 10.3322/canjclin.22.4.232. [DOI] [PubMed] [Google Scholar]
- 12.Harris WP, Mostaghel EA, Nelson PS, Montgomery B. Androgen deprivation therapy: progress in understanding mechanisms of resistance and optimizing androgen depletion. Nat Clin Pract Urol. 2009;6:76–85. doi: 10.1038/ncpuro1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Usami M, Akaza H, Arai Y, et al. Bicalutamide 80 mg combined with a luteinizing hormone–releasing hormone agonist (lhrh-a) versus lhrh-a monotherapy in advanced prostate cancer: findings from a phase iii randomized, double-blind, multicenter trial in Japanese patients. Prostate Cancer Prostatic Dis. 2007;10:194–201. doi: 10.1038/sj.pcan.4500934. [DOI] [PubMed] [Google Scholar]
- 14.Manikandan R, Srirangam SJ, Pearson E, Brown SC, O’Reilly P, Collins GN. Diethylstilboestrol versus bicalutamide in hormone refractory prostate carcinoma: a prospective randomized trial. Urol Int. 2005;75:217–21. doi: 10.1159/000087797. [DOI] [PubMed] [Google Scholar]
- 15.Kirby M, Hirst C, Crawford ED. Characterising the castration-resistant prostate cancer population: a systematic review. Int J Clin Pract. 2011;65:1180–92. doi: 10.1111/j.1742-1241.2011.02799.x. [DOI] [PubMed] [Google Scholar]
- 16.Berthold DR, Pond GR, Soban F, de Wit R, Eisenberger M, Tannock IF. Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer: updated survival in the tax 327 study. J Clin Oncol. 2008;26:242–5. doi: 10.1200/JCO.2007.12.4008. [DOI] [PubMed] [Google Scholar]
- 17.Zielinski RR, Azad AA, Chi KN, Tyldesely S. Population-based impact on overall survival after the introduction of docetaxel as standard therapy for metastatic castration resistant prostate cancer. Can Urol Assoc J. 2014;8:E520–3. doi: 10.5489/cuaj.2076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fizazi K, Scher HI, Molina A, et al. on behalf of the cou-aa-301 investigators Abiraterone acetate for treatment of metastatic castration-resistant prostate cancer: final overall survival analysis of the cou-aa-301 randomised, double-blind, placebo-controlled phase 3 study. Lancet Oncol. 2012;13:983–92. doi: 10.1016/S1470-2045(12)70379-0. [DOI] [PubMed] [Google Scholar]
- 19.Scher HI, Fizazi K, Saad F, et al. on behalf of the affirm investigators Increased survival with enzalutamide in prostate cancer after chemotherapy. N Engl J Med. 2012;367:1187–97. doi: 10.1056/NEJMoa1207506. [DOI] [PubMed] [Google Scholar]
- 20.Beer TM, Armstrong AJ, Rathkopf DE, et al. on behalf of the prevail investigators Enzalutamide in metastatic prostate cancer before chemotherapy. N Engl J Med. 2014;371:424–33. doi: 10.1056/NEJMoa1405095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tannock IF, Osoba D, Stockler MR, et al. Chemotherapy with mitoxantrone plus prednisone or prednisone alone for symptomatic hormone-resistant prostate cancer: a Canadian randomized trial with palliative end points. J Clin Oncol. 1996;14:1756–64. doi: 10.1200/JCO.1996.14.6.1756. [DOI] [PubMed] [Google Scholar]
- 22.Tannock IF, de Wit R, Berry WR, et al. on behalf of the tax 327 investigators Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer. N Engl J Med. 2004;351:1502–12. doi: 10.1056/NEJMoa040720. [DOI] [PubMed] [Google Scholar]
- 23.Nakabayashi M, Hayes J, Taplin ME, et al. Clinical predictors of survival in men with castration-resistant prostate cancer: evidence that Gleason score 6 cancer can evolve to lethal disease. Cancer. 2013;119:2990–8. doi: 10.1002/cncr.28102. [DOI] [PubMed] [Google Scholar]
- 24.Harris V, Lloyd K, Forsey S, Rogers P, Roche M, Parker C. A population-based study of prostate cancer chemotherapy. Clin Oncol (R Coll Radiol) 2011;23:706–8. doi: 10.1016/j.clon.2011.04.014. [DOI] [PubMed] [Google Scholar]
- 25.Lissbrant IF, Garmo H, Widmark A, Stattin P. Population-based study on use of chemotherapy in men with castration resistant prostate cancer. Acta Oncol. 2013;52:1593–601. doi: 10.3109/0284186X.2013.770164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Humphreys MR, Fernandes KA, Sridhar SS. Impact of age at diagnosis on outcomes in men with castrate-resistant prostate cancer (crpc) J Cancer. 2013;4:304–14. doi: 10.7150/jca.4192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Saad F, Hotte S, Catton C, et al. cua-cuog guidelines for the management of castration-resistant prostate cancer (crpc): 2013 update. Can Urol Assoc J. 2013;7:231–7. doi: 10.5489/cuaj.1542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fizazi K, Carducci M, Smith M, et al. Denosumab versus zoledronic acid for treatment of bone metastases in men with castration-resistant prostate cancer: a randomised, double-blind study. Lancet. 2011;377:813–22. doi: 10.1016/S0140-6736(10)62344-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Smith MR, Saad F, Coleman R, et al. Denosumab and bone-metastasis-free survival in men with castration-resistant prostate cancer: results of a phase 3, randomised, placebo-controlled trial. Lancet. 2012;379:39–46. doi: 10.1016/S0140-6736(11)61226-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Carter JA, Botteman MF. Health-economic review of zoledronic acid for the management of skeletal-related events in bone-metastatic prostate cancer. Expert Rev Pharmacoecon Outcomes Res. 2012;12:425–37. doi: 10.1586/erp.12.31. [DOI] [PubMed] [Google Scholar]
- 31.Konski A. Radiotherapy is a cost-effective palliative treatment for patients with bone metastasis from prostate cancer. Int J Radiat Oncol Biol Phys. 2004;60:1373–8. doi: 10.1016/j.ijrobp.2004.05.053. [DOI] [PubMed] [Google Scholar]
- 32.de Bono JS, Logothetis CJ, Molina A, et al. on behalf of the couaa-301 investigators Abiraterone and increased survival in metastatic prostate cancer. N Engl J Med. 2011;364:1995–2005. doi: 10.1056/NEJMoa1014618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kantoff PW, Higano CS, Shore ND, et al. on behalf of the impact study investigators Sipuleucel-T immunotherapy for castration-resistant prostate cancer. N Engl J Med. 2010;363:411–22. doi: 10.1056/NEJMoa1001294. [DOI] [PubMed] [Google Scholar]
- 34.Parker C, Nilsson S, Heinrich D, et al. on behalf of the Royal Marsden nhs Foundation Trust Updated analysis of the phase iii, double-blind, randomized, multinational study of radium-223 chloride in castration-resistant prostate cancer (crpc) patients with bone metastases (alsympca) J Clin Oncol. 2012;30 [Available online at: http://meetinglibrary.asco.org/record/74842/abstract; cited 24 June 2017] [Google Scholar]
- 35.de Bono JS, Oudard S, Ozguroglu M, et al. on behalf of the tropic investigators Prednisone plus cabazitaxel or mitoxantrone for metastatic castration-resistant prostate cancer progressing after docetaxel treatment: a randomised open-label trial. Lancet. 2010;376:1147–54. doi: 10.1016/S0140-6736(10)61389-X. [DOI] [PubMed] [Google Scholar]
- 36.Saad F, Chi KN, Finelli A, et al. The 2015 cua-cuog guidelines for the management of castration-resistant prostate cancer (crpc) Can Urol Assoc J. 2015;9:90–6. doi: 10.5489/cuaj.2526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.World Health Organization (who) Manual of the International Statistical Classification of Diseases, Injuries, and Causes of Deaths, Based on Recommendations of the Ninth Revision Conference, 1975. Geneva, Switzerland: WHO; 1977. [Google Scholar]
- 38.Statistics Canada . Canadian Classification of Diagnostic, Therapeutic, and Surgical Procedures. 2nd ed. Ottawa, ON: Statistics Canada, Health Division; 1986. [Google Scholar]
- 39.Dragomir A, Côté R, Roy L, et al. Impact of adherence to anti-hypertensive agents on clinical outcomes and hospitalization costs. Med Care. 2010;48:418–25. doi: 10.1097/MLR.0b013e3181d567bd. [DOI] [PubMed] [Google Scholar]
- 40.Lafeuille MH, Gravel J, Grittner A, Lefebvre P, Ellis L, McKenzie RS. Real-world corticosteroid utilization patterns in patients with metastatic castration-resistant prostate cancer in 2 large US administrative claims databases. Am Health Drug Benefits. 2013;6:307–16. [PMC free article] [PubMed] [Google Scholar]
- 41.Engel-Nitz NM, Alemayehu B, Parry D, Nathan F. Differences in treatment patterns among patients with castration-resistant prostate cancer treated by oncologists versus urologists in a US managed care population. Cancer Manag Res. 2011;3:233–45. doi: 10.2147/CMR.S21033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ribal MJ, Martínez-Salamanca JI, García Freire C. Current patterns of management of advanced prostate cancer in routine clinical practice in Spain. Prostate Cancer. 2015;2015:186740. doi: 10.1155/2015/186740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Heidenreich A, Bellmunt J, Bolla M, et al. on behalf of the European Association of Urology eau guidelines on prostate cancer. Part 1: screening, diagnosis, and treatment of clinically localised disease. Eur Urol. 2011;59:61–71. doi: 10.1016/j.eururo.2010.10.039. [DOI] [PubMed] [Google Scholar]
- 44.Mottet N, Bellmunt J, Bolla M, et al. eau guidelines on prostate cancer. Part ii: treatment of advanced, relapsing, and castration-resistant prostate cancer. Eur Urol. 2011;59:572–83. doi: 10.1016/j.eururo.2011.01.025. [DOI] [PubMed] [Google Scholar]
- 45.Hagiwara M, Delea TE, Cong Z, Chung K. Utilization of intravenous bisphosphonates in patients with bone metastases secondary to breast, lung, or prostate cancer. Support Care Cancer. 2014;22:103–13. doi: 10.1007/s00520-013-1951-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Petrylak DP, Tangen CM, Hussain MH, et al. Docetaxel and estramustine compared with mitoxantrone and prednisone for advanced refractory prostate cancer. N Engl J Med. 2004;351:1513–20. doi: 10.1056/NEJMoa041318. [DOI] [PubMed] [Google Scholar]