Abstract
Sexual assault (SA) is a common and deleterious form of trauma. Over 40 years of research on its impact has suggested that SA has particularly severe effects on a variety of forms of psychopathology, and has highlighted unique aspects of SA as a form of trauma that contribute to these outcomes. The goal of this meta-analytic review was to synthesize the empirical literature from 1970–2014 (reflecting 497 effect sizes) to understand the degree to which (a) SA confers general risk for psychological dysfunction rather than specific risk for posttraumatic stress, and (b) differences in studies and samples account for variation in observed effects. Results indicate that people who have been sexually assaulted report significantly worse psychopathology than unassaulted comparisons (average Hedges’ g=0.61). SA was associated with increased risk for all forms of psychopathology assessed, and stronger associations were observed for posttraumatic stress and suicidality. Effects endured across differences in sample demographics. Broader SA operationalizations (e.g., including incapacitated, coerced, or nonpenetrative SA) were not associated with differences in effects, although including attempted SA in operationalizations resulted in lower effects. Larger effects were observed in samples with more assaults involving stranger perpetrators, weapons, or physical injury. In the context of the broader literature, our findings provide evidence that experiencing SA is major risk factor for multiple forms of psychological dysfunction across populations and assault types.
Keywords: sexual violence, rape, trauma, mental disorders, mental health, meta-regression
Sexual assault (SA) is a common form of trauma: 17–25% of women and 1–3% of men will be sexually assaulted in their lifetime (Black et al., 2011; Fisher, Cullen, & Turner, 2000; Koss, Gidycz, & Wisniewski, 1987; Tjaden & Thoennes, 2000, 2006). The high prevalence of SA is particularly concerning in light of its significant psychological consequences for survivors (e.g., Campbell, Dworkin, & Cabral, 2009). Indeed, SA appears to have a more significant impact on mental health than other forms of trauma (Kelley, Weathers, McDevitt-Murphy, Eakin, & Flood, 2009; Kessler et al., 1995). As a result, SA is an issue of major public health concern.
Research on the Role of Sexual Assault in the Development of Psychopathology: A Brief History
The past forty years have represented a period of significant growth and evolution in both public and research attention to SA. Beginning as early as the 1970s, increasing attention to SA as a feminist issue as well as growing interest in the impact of traumatic life experiences manifested in several seminal academic works on the psychological impact of SA. Sutherland and Scherl (1970) interviewed 13 women who had been sexually assaulted, and described a condition involving an early period of anxiety and fear, followed by a depressive phase. Burgess and Holstrom (1974) interviewed 146 women admitted to a hospital with a presenting complaint of SA. “Rape trauma syndrome,” as they called the condition they observed, was described as involving a spectrum of acute symptoms including somatic reactions like muscle tension and stomach pain, as well as emotional reactions like fear and self-blame. Over time, survivors were said to enter a “reorganization” phase that included nightmares, phobic reactions to trauma reminders, and increases in motor activity. These articles set the groundwork for an explosion of research on the impact of SA (Koss, 2005).
By 1980, the set of symptoms described by these early studies was recognized to be highly similar to descriptions of other trauma-related syndromes (e.g., “combat fatigue”), and a new condition, called posttraumatic stress disorder (PTSD), was introduced to the Diagnostic and Statistical Manual of Mental Disorders (DSM; APA, 1980). Although the framing of SA’s impact through the lens of a single form of psychopathology was critiqued by feminist scholars (see Wasco, 2003), a benefit of this new construct was a substantial increase in research attention to both trauma generally and SA specifically. This increased attention was reflected in several early longitudinal studies assessing the impact of SA. For example, Kilpatrick and colleagues (1981) followed 20 recent SA survivors and 20 controls over a year, and identified elevations in fear and anxiety within the SA group across this period. Atkeson and colleagues (1982) assessed 115 recent SA survivors and 87 controls for a year, and found that group differences in depression had resolved by four months post-assault. Epidemiological research also began to assess the impact of SA during this time. In the earliest epidemiological assessment of trauma-related psychopathology to assess SA, the Detroit Area Survey of Trauma (N = 1007) found that the prevalence of PTSD in survivors of non-SA traumas ranged from 12% to 24%, but the prevalence of PTSD in survivors of SA was 80% (Breslau, Davis, Andreski, & Peterson, 1991). Similarly, the National Comorbidity Survey (N = 5877) found that rape was the most common cause of PTSD in women, and nearly half of men and women exposed to SA met criteria for lifetime PTSD (Kessler et al., 1999).
As the field evolved, epidemiological studies began to examine the relationship between traumas like SA and conditions beyond PTSD alone. For example, results from the National Epidemiological Survey on Alcohol and Related Conditions—a large, representative US sample (N = 31,875)—indicated that experiencing adult SA was associated with significantly increased risk for new onset of several forms of psychopathology, including substance use disorder, bipolar disorder, and PTSD (Xu et al., 2013). In addition, the National Women’s Study Replication—a nationally-representative sample of women (N = 3001)—found that forcible rape was associated with risk for a major depressive episode (Zinzow et al., 2010), and both forcible and drug/alcohol facilitated rape were associated with risk for PTSD.
Over the following decades, research accumulated to demonstrate that SA is associated with many forms of psychological dysfunction. A qualitative review of the prevalence of various mental disorders in survivors of adult SA found that 17%–65% of people with a history of SA develop PTSD, 13%–51% meet diagnostic criteria for depression, 12–40% experience symptoms of anxiety, 13–49% develop alcohol use disorders, 28–61% develop drug use disorders, 23–44% experience suicidal ideation, and 2–19% attempt suicide (Campbell et al., 2009). Although other psychological conditions have received less frequent attention in relation to SA, there is some evidence that SA is associated with conditions such as obsessive-compulsive disorder (Arata, 1999; Boudreaux, Kilpatrick, Resnick, Best, & Saunders, 1998; Burnam et al., 1988; Frazier & Schauben, 1994; Kilpatrick, Resick, & Veronen, 1981; Walker, Gefland, Gefland, Koss, & Katon, 1995; Winfield, George, Swartz, & Blazer, 1990) and bipolar disorder (Arata, 1999; Burnam et al., 1988; Xu, Olfson, Villegas, Okuda, Wang, Liu, & Blanco, 2013).
It is evident from this work that, although SA is a life-altering experience for many survivors, not all who are assaulted develop psychological problems. Thus, many studies have attempted to understand who is most at risk for developing post-trauma psychopathology. Much of this work has focused on characteristics of individuals (e.g., demographics, prior assault history) or assaults (e.g., assailant type, peritraumatic dissociation) as correlates of post-assault distress, as reflected in early reviews in this area (e.g., Goodman, Koss, & Russo, 1993). In a past meta-analysis of 50 studies assessing the association between interpersonal violence and psychopathology, however, the only demographic characteristics related to distress were the percent of women in the sample and age at the time of victimization (Weaver & Clum, 1993). Characteristics of traumas experienced, such as the amount of force used and survivors’ subjective appraisals of the trauma (e.g., self blame), were also associated with recovery in this analysis.
In contrast to this search for correlates of recovery at the level of individuals or assaults, researchers have increasingly applied an ecological lens to identifying correlates of SA recovery (see Carter-Snell & Jakubec, 2013, Campbell et al., 2009, and Neville & Hepner, 1999 for ecologically-based reviews). This perspective emphasizes that SA recovery occurs in a multilevel social context, in which the unique aspects of SA as a form of trauma interface with aspects of the environment to affect recovery. From this work, it is clear that SA remains a highly stigmatized experience (Kennedy & Prock, 2016) that is associated with societal “rape myths,” such as the idea that survivors are to blame for assault (Edwards, Turchick, Dardis, Reynolds, & Gidycz, 2011). There is evidence that survivors internalize this stigma, leading to self-blame, shame, and unwillingness to seek help (Kennedy & Prock, 2016). In addition, survivors who choose to disclose their assault to friends, relatives, and professionals often experience negative social reactions, such as victim blame, that have been found to increase risk for PTSD in longitudinal research (Ullman & Peter-Hagene, 2014). Reflecting both the increased public attention to the importance of improving community responses SA and the unique nature of SA as a form of trauma, a variety of dedicated services are now available to survivors of SA that may affect their recovery processes (e.g., Sexual Assault Nurse Examiners, rape crisis centers, SA medical and legal advocates) (Campbell et al., 1999). However, the impact of these specialized services on survivors’ mental health has been largely unexplored.
Unresolved Questions in Research on Sexual Assault’s Psychological Impact
Four decades of research on the psychological impact of SA offer a rich body of work that can be examined to identify patterns in findings across studies. Although the bulk of the research on this topic has identified associations between SA and various forms of psychopathology, exceptions exist, and studies differ with regard to the strength of the association that they identify. Clarifying the conditions under which associations between SA and psychopathology are observed has the potential to inform theoretical understandings of the development of mental disorders after trauma, which in turn, could inform the development of efficacious interventions and prevention strategies. Next, we outline unresolved questions in research on SA’s psychological impact—those that have received limited research attention or yielded mixed findings across studies—that can be explored by examining this body of literature as a whole.
Is sexual assault a risk factor for PTSD or psychological dysfunction broadly?
In understanding the mechanisms by which traumas like SA produce psychopathology, it is important to understand whether SA is a specific risk factor for certain conditions or a more general risk factor for psychological dysfunction. The psychological literature on trauma has primarily focused on posttraumatic stress disorder, although other conditions often observed in traumatized populations (e.g., depression, anxiety, substance use disorders) have received relatively less attention (aside from their co-occurrence with PTSD). This focus on PTSD is based in a theoretical understanding of PTSD as a unique phenotype arising from trauma that is conceptually different from other disorders that often are seen in trauma survivors (e.g., depression, anxiety disorders) in that its etiology necessarily involves an external trauma event (APA, 2013). These other disorders are thought to be associated with or exacerbated by a trauma, but are not dependent on an experience of trauma in most cases (Friedman, Resick, Bryant, & Brewin., 2011). Indeed, in the DSM-5, PTSD was moved out of the anxiety disorders into a new diagnostic category, called “trauma and stressor-related disorders” (APA, 2013). The extent to which this focus on PTSD as a primary, distinct, and unique outcome of traumas like SA is justified remains unclear, given the wide variation in prevalence estimates of disorders other than PTSD in trauma survivors described previously. Clarifying whether traumas like SA are specifically associated with PTSD or broadly associated with multiple forms of psychopathology could expand the understanding of the nature of the impact of SA, which may have implications for theory development as well as the assessment and treatment of psychopathology following assault.
How do differences in study methods and samples alter observed relationships?
In understanding inconsistencies in observed relationships between SA and psychopathology across studies, it also is important to account for unique aspects of SA as a form of trauma and corresponding variation in research on this topic. SA is a particularly common, deleterious, and stigmatized trauma that is the focus of much public discourse regarding issues such as the degree to which various forms of SA are expected to produce psychological harm. Because of these characteristics, SA has received significant focused research attention—with unique methodological characteristics—independent from other traumas, and numerous debates have arisen regarding best-practice approaches to researching SA. We next review how these differences in study methods and samples might account for differences in study results.
Operationalization of constructs and assessment quality
There is significant variation in the field regarding the assessment of SA. Some studies use the Sexual Experiences Survey (Koss et al., 2007), which includes a variety of types of SA (e.g., coerced, incapacitated, and forced; attempted and completed; fondling and penetrative SA) and, given its specificity, is considered to be a gold standard self-report measure for assessing SA victimization. However, researchers using the Sexual Experiences Survey vary in terms of the items they use to operationalize SA for analytic purposes. Other researchers create their own measures that include varying operational definitions across these dimensions. Still, other studies use single-item measures of SA that refer broadly to “sexual assault” or “rape” and leave the operational definition of these terms to study participants. This raises two major issues. First, it is not known whether the breadth of operational definitions of SA (e.g., including coerced SA in operational definitions) used in research is associated with the observed strength of the SA-psychopathology relationship. Indeed, an ongoing debate over the appropriate operational definition of SA (Cook, Gidycz, Koss, & Murphy, 2011; Koss, 2011) has centered on concerns that broad definitions of SA may obscure its connection with psychopathology. If survivors of assaults that fall under broader operationalizations truly are less affected by their experiences, then broadening operational definitions should result in smaller observed differences from unassaulted samples. Second, these differences in assessment also represent differences in quality. Best-practice approaches to assessing SA include the use of multi-item validated instruments that explicitly define both behaviors considered assaultive (e.g., vaginal penetration), as well as the tactics through which these behaviors are achieved (e.g., force, coercion). If high-quality assessments capture a wider range of experiences of SA (e.g., less severe forms of SA), and low-quality assessments might fail to capture actual survivors of SA (i.e., false negatives), higher assessment quality would likely reduce observed group differences in psychopathology. Clarifying the impact of assessment quality on observed relationships between SA and psychopathology could help to guide methodological decisions in this research area.
Similar quality issues are present in assessments of psychopathology. The quality of assessment measures range from single-item self-report instruments that are not directly connected to DSM symptom criteria, to standardized, validated diagnostic interviews. Although a past meta-analysis on the relationship between interpersonal violence and distress did not find evidence that indicators of validity were associated with the magnitude of observed effects (Weaver & Clum, 1995), it is not clear whether this relationship has changed in the past 20 years of methodological development in this area. If higher-quality assessments capture more “true” psychopathology, and differences in psychopathology exist between SA and no-SA groups, low quality assessment methods would be expected to reduce these observed differences. Because using the highest-quality assessment measures is resource-intensive, understanding the extent to which they minimize bias could help to inform methodological decisions.
Comparison group
It is unclear in comparison to whom sexually assaulted people evidence greater psychopathology. Some studies use comparison groups that are selected for their lack of trauma experience, others use comparison groups that have not experienced SA, and others use comparison groups that have experienced another form of trauma (e.g., motor vehicle accidents). Experiencing any trauma is an environmental stressor that is likely to increase risk for psychopathology, therefore, sexually assaulted people should evidence high levels of psychopathology relative to people who have never experienced trauma. In addition, there is some evidence to suggest that SA is a particularly harmful form of trauma (Kessler et al., 1995; Kelley et al., 2009). An earlier meta-analysis on psychological distress related to interpersonal violence found no difference between SA and other interpersonal trauma types in terms of their level of distress (Weaver & Clum, 1995), but did not compare SA to non-interpersonal traumas. Such comparisons would be needed to clarify the unique impact of SA relative to other traumas.
Lifetime vs. adult/adolescent SA
Unlike the broader trauma literature, which generally assesses lifetime exposure to a number of forms of trauma (including SA), the SA literature has been largely siloed into research on childhood SA and adolescent/adult SA (i.e., at or after age 12–15, depending on study definitions). The degree to which these bodies of literature are comparable is unclear, and correspondingly, existing systematic quantitative and qualitative reviews of the impact of SA have limited their scope to childhood SA (Chen et al., 2010; Smolak & Murnen, 2002) or adult SA (Campbell et al., 2009). Indeed, evidence from meta-analyses that younger age at trauma exposure is associated with increased risk for PTSD (Brewin, Andrews, & Valentine, 2000; Ozer et al., 2003) suggests that studies of lifetime SA might not be directly comparable to studies of adolescent/adult SA. However, the lifetime SA literature offers an rich potential source of information, and thus, the comparability of lifetime SA studies to adolescent/adult SA studies is an important empirical question to inform further reviews and theory development.
Differences in samples
Interpersonal violence does not inevitably lead to psychopathology (Weaver & Clum, 1995), and it remains unclear how its effects differ across people. Thus, it is important to explore how the relationship between SA and psychopathology differs as a function of sample characteristics (e.g., types of assaults experienced, average time since assault, sample demographics).
Assaults vary in terms of characteristics that could affect psychopathology, such as the presence of physical injury, weapon use by the perpetrator, or the relationship of the victim to the offender. In a past qualitative review of the relationship of these SA assault characteristics to psychopathology, only physical injury was associated with psychopathology (Campbell et al., 2009). This may be because injury increases perceived life threat, which a past meta-analysis has found to predict PTSD across types of trauma (Ozer, Best, Lipsey, & Weiss, 2003). Similarly, a meta-analysis of psychopathology related to child sexual abuse did not find differences based on victim-offender relationship (Paolucci & Genuis, 2001), although child sexual abuse tends to involve different perpetrator types (e.g., family members) than adult SA (Tjaden & Thoennes, 2006). Further examination of how assault characteristics predict psychopathology in relation to SA specifically is needed to clarify the unique aspects of SA experiences that contribute to psychopathology.
Time since assault may alter observed relationships with psychopathology. In a meta-analysis of the association between distress and interpersonal violence, time since stressor was negatively associated with effect sizes (Weaver & Clum, 1995), and a review of the impact of intimate partner violence on psychopathology found that rates of depression decline over time (Golding, 1999). Because SA is thought to have a stronger relationship with psychopathology than other interpersonal forms of trauma (Kessler et al., 1995), it is possible that its effect is more persistent over time. However, this has not been tested.
SA may have a different impact on survivors depending on their demographic characteristics, such as age, gender, and race/ethnicity. A qualitative review of associations between SA specifically and multiple forms of trauma identified mixed findings regarding the importance of current age in post-SA psychopathology: most studies identified no relationship between age and distress, and several identified either positive or negative associations between age and specific forms of psychopathology (Campbell et al., 2009). In terms of gender, results also are mixed. One meta-analysis found that the percentage of women in the sample was positively associated with the magnitude of the relationship between interpersonal victimization and psychological distress (Weaver & Clum, 1995), but this analysis included few samples of men and combined types of interpersonal victimization, which potentially underestimated the impact of SA on men. In contrast, one meta-analysis suggested that the association between interpersonal violence and PTSD is not stronger for women than men (Tolin & Foa, 2006), and a second also did not identify gender differences in the association between child sexual abuse and psychopathology (Paolucci & Genuis, 2001). Results for racial/ethnic differences appear more clear: most studies have not identified an association between race/ethnicity and SA-related psychopathology (Campbell et al., 2009), but no meta-analysis has tested this relationship. Generally, because SA is— unlike many other forms of trauma—disproportionately experienced by women and young people, and there is some evidence to suggest that racial differences exist in SA victimization (Acierno, Resnick, & Kilpatrick, 1998), it is important to clarify whether demographic differences exist in the impact of SA specifically. Understanding who is most affected by SA has the potential to inform targeted efforts to prevent psychopathology.
Finally, increasing attention has been paid to the specific impact of SA on populations such as college students and veterans/military personnel. It is unclear whether different relationships between SA and psychopathology are observed depending on which population is sampled. There is evidence that a lack of a college education is associated with higher likelihood of suicide attempts among SA survivors (Ullman & Brecklin, 2002b), and less-educated SA survivors evidence more self blame compared to college-educated survivors (Long, Ullman, Starzynski, Long, and Mason, 2007). However, when considering population-level differences in psychopathology, it is likely that SA survivors who are able to maintain college enrollment or some other professional role despite trauma exposure are likely to reflect a somewhat higher-functioning subset of survivors relative to the general population (i.e., those most affected by SA may be more likely to withdraw from employment or college enrollment and thus not be reflected in group comparisons). Addressing how study population affects study results is important to inform methodological decisions and the interpretation of results.
The Current Study
In sum, given the relevance to theory and practice of understanding the SA-psychopathology relationship, as well as the multiple unresolved questions that exist in this literature, a systematic summary of this relationship is needed. Specifically, summarizing the literature could clarify (a) the breadth versus specificity of the impact of SA on psychopathology and (b) how this relationship might differ as a function of differences in studies’ methods and samples. Qualitative reviews on this topic tend to be unsystematic, and as such, do not offer a rigorous, thorough picture of the state of the science in this area. Although meta-analyses on related topics exist, they have several major limitations that this work aims to address. First, the most thematically similar quantitative analysis (Weaver & Clum, 1995) assessed dysfunction broadly (e.g., including problems in living) rather than psychopathology specifically. To inform theory and practice regarding the development of mental disorders after trauma, a targeted analysis is needed. Second, several assessed only a single form of psychopathology (e.g., Brewin et al., 2000; Ozer et al., 2003; Smolak & Murnen, 2002), and those that assessed multiple domains of psychopathology did not conduct statistical comparisons across domains (e.g., Chen et al., 2010; Golding, 1999; Paolucci & Genuis, 2001). Attention to multiple specific manifestations of psychopathology raises the possibility of cross-condition comparisons, which could clarify the relative strength of their association with a highly common form of trauma, and thus advance the field’s understanding of how various forms of psychopathology relate to trauma. In particular, forms of psychopathology that have been often been discussed as correlates of SA—like depression1, anxiety, trauma and stressor-related conditions, substance abuse/dependence, suicidality, and disordered eating —as well as certain conditions common in traumatized populations (e.g., bipolar conditions, obsessive-compulsive conditions)—warrant focused attention. Finally, although the amount of research on the association between SA and psychopathology has been increasing, the most recent similar meta-analysis—assessing associations between trauma exposure broadly and PTSD—was conducted in 2003 (Ozer et al., 2003). By quantitatively reviewing the literature from 1970 to 2014, we hoped to update earlier qualitative reviews and reflect the state of the science on this topic.
The first goal of the current meta-analysis is to quantitatively synthesize the degree of association between SA and various mental disorders to clarify whether traumas like SA are specifically associated with PTSD or broadly associated with multiple forms of psychopathology. We hypothesized that SA would have a significant positive relationship with each form of psychopathology (Hypothesis 1). Given the lack of research regarding the differential impact of SA on various forms of psychopathology, we chose to approach this analysis in an exploratory manner rather than making non-empirically supported hypotheses about the relative magnitude of each average effect size.
A secondary goal of this work is to understand how differences in studies and samples might alter observed relationships between SA and psychopathology. We hypothesized that broadening operational definitions of SA would be associated with smaller effect sizes (Hypotheses 2a–c), lower-quality SA assessment methods would be associated with higher observed effect sizes (Hypothesis 3), lower-quality psychopathology assessment methods would be associated with smaller observed effect sizes (Hypothesis 4), and studies using a no/low-trauma comparison group would result in significantly larger effect sizes than studies using no-SA comparison groups but no difference in effect sizes would be observed for studies using an other-trauma comparison group (Hypotheses 5a–b), and samples assessing lifetime SA would evidence larger effect sizes than those assessing adult SA only (Hypothesis 6), Finally, related to sample characteristic differences, we hypothesized that higher percentages of each assault characteristic (i.e., stranger perpetrators, weapon use, physical injury) would be positively related to observed effect sizes (Hypothesis 7a–c), time elapsed since assault would be negatively related to observed effect sizes (Hypothesis 8), no differences in effect sizes would be observed as a function of age, gender, or race (Hypotheses 9a–c), and samples reflecting college students would evidence smaller effect sizes than other samples (Hypothesis 10).
Method
Literature Search and Study Retrieval
We followed several steps to identify relevant studies for inclusion.
Searching databases
We searched PsychINFO, ProQuest Digital Dissertations & Theses, and Academic Search Premier for the following combinations of search terms anywhere in the article, using Boolean operators: (rape* OR “sexual assault” OR “sexual victimization”) AND (“mental health” OR depression* OR anxiety* OR bipolar* OR mania* OR anxiety* OR phobia* OR distress* OR PTSD OR “post-traumatic” OR “substance dependence” OR “substance abuse” OR suicide* OR “eating disorder” OR “disordered eating”). We limited searches to results published between 1970 and 2014 in English, resulting in 125,780 search results that received title review. Given the large number of results obtained and the targeted efforts to obtain relevant studies described next, these search terms and databases were deemed sufficiently comprehensive. All articles (m = 2813) judged to be potentially eligible based on their titles received full-text review. Finally, we examined a database of articles collected by the first author for a previous review of the mental health effects of SA (Campbell, Dworkin, & Cabral, 2009).
Examining citations
We examined the citations of every eligible article, every article that would have been eligible had it not omitted relevant data, and every article that would have been eligible had it included a comparison group. We also examined reference sections of literature reviews and meta-analyses on similar topics (Brewin et al., 2000; Campbell et al., 2009; Carter-Snell & Jakubec, 2013; Goodman, Koss, & Russo, 1993; Jewkes, 2000; Jordan, Campbell, & Follingstad, 2010; Koss, Heise, & Russo, 1994; Neville & Heppner, 1999; Ozer et al., 2003; Resick, 1987; Resick, 1993; Sarkar & Sarkar, 2005; Steketee & Foa, 1987; Tolin & Foa, 2006; Weaver & Clum, 1995).
Identifying unpublished data
The file drawer effect is a perennial problem in the academic literature (Rosenthal, 1979), which makes it particularly important to attempt to minimize publication bias in meta-analyses (Lipsey & Wilson, 2001). To accomplish this, we took several steps. First, we searched for eligible dissertations and theses. Second, we posted a notice on the APA Division 56 (Traumatic Stress) listserv requesting unpublished data. Third, we developed an initial list of eligible studies and contacted all authors with three or more eligible studies from this list to request unpublished data. Fourth, for studies conducted between 2004–2014, when we believed that it was possible that researchers had collected eligible data that was not presented, or when eligible data was not presented in a format from which we could obtain effect size estimates, we asked study authors for data. In all, we sent 124 requests for additional data, 48 (38.71%) of which yielded usable data, with a total of 108 effects coded from these requests. Fifth, when we made these requests for data, we also requested unpublished data. Ultimately, 35% of the effect sizes that we coded (175/497) used unpublished data obtained through these methods.
Reviewing journals
We reviewed 2010–2014 issues of journals from which we had obtained three or more articles from our tentative list of eligible studies (i.e., Journal of Consulting and Clinical Psychology, Journal of Interpersonal Violence, Violence and Victims, Violence Against Women, Psychology of Women Quarterly, Journal of Traumatic Stress, and Addictive Behaviors).
Determining eligibility
Our inclusion criteria were as follows (see Figure 1 for the percent of articles excluded based on each criterion).
Figure 1.
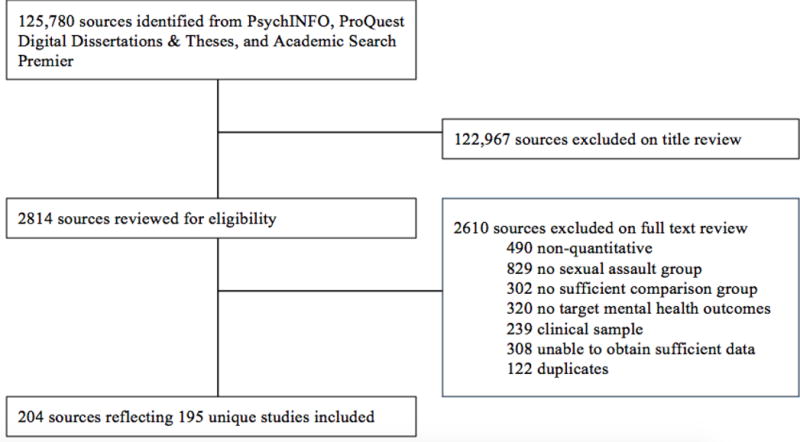
Study Selection
The study must have been quantitative in nature with a sample size of N > 10.
We must have been able to create a sexually assaulted group comprised of survivors of either adolescent/adult or lifetime SA. We defined SA as unwanted sexual contact, which must have been operationalized through terms like “rape,” “sexual violence,” or “sexual assault” and/or behavioral descriptions including (but not necessarily limited to) forced penetration. Because there have been several meta-analyses conducted on associations between child sexual abuse and psychopathology (e.g., Chen et al., 2010; Smolak & Murnen, 2002), in an effort to present a nonduplicative analysis, the SA group must not have been exclusively comprised of children or child sexual abuse survivors. However, because many studies assessed SA across the lifespan (i.e., combined child and adolescent/adult), we coded lifetime effects when no separate data for adolescent/adult SA was available to ensure that the population of studies was not overly restricted, consistent with a similar meta-analysis (Brewin et al., 2000). Thus, adolescent/adult-only and mixed adolescent/adult and child samples were eligible.
Data for a comparison/no-SA group comprised of people who did not experience SA during the focal time period (e.g., adulthood, past 4 weeks) must have been available, either in the article or by request from authors. A comparison group was needed to compute an effect size representing risk for psychopathology associated with experiencing SA; comparisons between people who experienced SA were outside of the scope of the analysis. The construct of SA must not have been operationalized in such a manner that people who had experienced SA were likely to be included in the no-SA group. For example, studies that compared people who had experienced military SA to those who had not were likely to have included survivors of non-military SA in the no-SA group, and were excluded.
The study must have reported data on a construct within at least one of the following domains in both the SA and no-SA group: bipolar conditions (e.g., diagnosis of bipolar I, manic symptoms), depression (e.g., depressed mood, diagnoses of major depressive disorder), anxiety (e.g., fear, anxiety sensitivity, worry, generalized anxiety disorder), obsessive-compulsive conditions (e.g., diagnosis of obsessive-compulsive disorder, presence of obsessions and compulsions), trauma and stressor-related conditions (e.g., diagnosis of acute stress disorder, posttraumatic stress symptoms), substance abuse/dependence (e.g., alcohol use disorder, presence of drug dependence symptoms), suicidality (e.g., attempts, ideation), and disordered eating (e.g., diagnosis of anorexia nervosa, presence of bulimic symptoms). We included only those effects that provided coverage of the domain itself (e.g., depressed mood) or a specific diagnosis within the domain (e.g., major depressive disorder) through an interview or self-report measure, and excluded effects that represented single symptoms of a disorder within the broader domain (e.g., purging, insomnia). We excluded effects that were based on chart diagnoses or self-reports of past diagnoses made by a clinician, as these captured help-seeking behavior for mental health rather than the existence of the condition itself. We excluded studies that, by design, assessed SA risk prospectively after onset of a mental disorder. We included only baseline data for repeated-measures studies (m = 23, 12% of studies), consistent with similar meta-analyses (Ozer et al., 2003), to avoid underestimating the effect size by averaging across assessment periods.
The study population or SA group must not have, by design, only consisted of people who were seeking psychological treatment or people who had an existing mental illness. The study must also not have intentionally oversampled such individuals (i.e., in cases where recruitment was targeted to clinical settings, when the study recruited set numbers of participants with and without particular disorders). We excluded these studies to avoid clinical selection bias (du Fort, Newman, & Bland, 1993), consistent with meta-analyses on related topics (Brewin et al., 2000; Tolin & Foa, 2006). In addition, because we were interested in the degree to which experiencing SA affords risk for psychopathology and these samples were usually entirely comprised of people with psychopathology, we would have been unable to calculate estimates of group differences in such samples.
The study must have presented adequate data in English to calculate the selected effect size (i.e., Hedges’ g) or we must have been able to obtain these data from the authors.
The study must not have been fully duplicative of another eligible study.
Identifying effects from shared samples
We examined articles that shared an author to determine whether effects were based on the same sample. When authors noted that they used a particular dataset or had published results from the same study elsewhere, we recorded this information to ensure that we retained only one effect for each form of psychopathology per sample and assigned a shared identification number across effects representing different forms of psychopathology from a single sample.
Study Moderators
Domain of psychopathology
We coded each effect size as reflecting one of the eight domains defined in our eligibility criteria that were within the scope of the current study.
Operationalization of SA
We coded three dichotomous moderators to reflect how the study operationalized SA. First, we indicated whether the operational definition of SA in each study included both attempted and completed SA or only completed SA. Second, we coded whether each study explicitly included the following tactics through which SA was achieved: coercion (e.g., due to pressure, arguments, or misuse of authority), incapacitation (i.e., victim was unconscious or incapacitated by drugs and/or alcohol), and/or force (i.e., achieved through force or threats of harm). We then created a four-level composite variable to represent a 2×2 interaction of the presence of incapacitation and/or coercion. All studies that specified at least one tactic included force, and studies that did not specify at least one tactic were coded as missing. Third, we coded whether participants could have been included in the SA group on the basis of experiencing nonpenetrative SA (e.g., kissing, touching, fondling), or whether experiencing penetrative SA was necessary to be included in the SA group. Studies that did not specify at least one assaultive sex act that comprised SA were coded as missing. For studies that specifically recruited survivors of SA, we coded these variables based on study recruitment materials and/or inclusion criteria. For all other studies, we obtained this information from SA assessment measures. We recorded missing values for studies that did not provide enough information to determine the operational definition through which the SA group was formed. For example, in studies that used a multi-item measure of SA such as the Sexual Experiences Survey, when authors specified which items were used to determine membership in the SA group, we recorded values for these moderators based on the wording of the specified items; however, when authors did not specify which items were used to determine membership and codes would differ based on items included, we coded these values as missing.
Assessment quality
Psychopathology assessment quality was operationalized as the proportion of the following criteria met: the measure (a) was administered via interview, (b) was previously published, (c) included multiple items, and (d) was explicitly stated to be based on and/or validated against DSM criteria (suicide measures were coded as not applicable for this criterion). Drawing from methodological recommendations (Cook et al., 2011), SA assessment quality was operationalized as the proportion of the following criteria met: the measure (a) was previously published, (b) included multiple items, (c) described at least one sex act behaviorally, and (d) specified at least one tactic (e.g., force or coercion), through which the sex act occurred. For both variables, a proportion of the total criteria for which information was available was calculated if at least three criteria were available.
Comparison group type
We created a categorical variable to represent comparison group type— comparison groups that were selected for their lack of trauma experience (i.e., no/low-trauma groups), comparison groups that had not experienced SA (i.e., no-assault groups), and comparison groups that had experienced another form of trauma (i.e., other-trauma groups)—for each effect.
Lifetime vs. adolescent/adult SA
A dichotomous variable indicated whether the SA group was comprised of participants who experienced lifetime SA or SA in adolescence/adulthood. A study was considered to assess adolescent/adult SA if the minimum age at which SA could have occurred was 12 years old or greater. All other studies, including cross-sectional studies that did not specify an age at which SA could have occurred, were considered to represent lifetime SA.
Features of assaults experienced by participants
We coded three continuous study-level moderators to capture characteristics of the actual assaults experienced by participants. Specifically, we coded the percent of assaults that involved a stranger perpetrator, the percent that involved weapon use, and the percent that involved physical injury to the survivor.
Time since SA
A continuous variable represented the mean number of years elapsed since the focal SA on which participants reported, or if this was not available, the most recent SA.
Sample demographics
We coded the percent of women in the sample, the mean age in the sample, and, for US samples2, the majority (>60%) racial group represented by the sample.
Sample type
A categorical variable indicated the majority (>60%) type of participants that comprised the overall sample (i.e., including both the SA and no-SA group). Categories were college students, general population (i.e., unselected for any particular characteristic), people seeking medical treatment, military personnel or veterans, and people seeking support for crime-related needs. An “other” category included sample types represented in two or fewer samples (e.g., people with a cognitive disability). Mixed samples represented 2–3 of the aforementioned categories; typically, these samples represented either combined college and community recruitment efforts or samples of a help-seeking SA group compared to a college or community no-SA group.
Coding Procedures
The coding team consisted of the first, second, and third authors (i.e., the primary coders) and 10 trained research assistants (i.e., the secondary coders). Every effect was coded by at least two coders (i.e., a primary and secondary coder), but review by three coders was common, and the first author reviewed every effect. In addition, every coding discrepancy was tracked and received review by the primary coder and/or at least one other team member; discrepancies were resolved in group meetings. Additional information about this coding process is available in Appendix A.
To assess coding accuracy, several moderators that were judged to be the most difficult to code were reserved for coding by the primary coders. The primary coders recorded their codes independently and inter-rater reliability was calculated. The variable “operational definition includes both forced and coerced SA or forced SA only” had substantial agreement (κ = 0.77 for first vs. second author and κ = 0.77 for first vs. third author), “operational definition includes both forced and incapacitated SA or forced SA only” had substantial to near-perfect agreement (κ = 0.70 for first vs. second author and κ = 0.94 for first vs. third author), “operational definition includes both penetrative and nonpenetrative SA or penetrative SA only” had near-perfect agreement (κ = 0.80 for the first vs. second author and κ = 0.80 for the first vs. third author), and “operational definition includes both attempted and completed SA or only completed SA” had substantial agreement (κ = 0.61 for first vs. second author and κ = 0.76 for first vs. third author). All discrepancies were resolved by discussion.
Hedges’ g and its variance were calculated using Comprehensive Meta Analysis (Borenstein, Hedges, Higgins, & Rothstein, 2005). We selected g as a conservative alternative to d that represents group differences on both dichotomous and continuous variables and corrects for sample size. In this study, g represents the magnitude of the difference in psychopathology between people who had been sexually assaulted and people who had not been sexually assaulted.
Analyses
Because multiple effects were commonly presented in a single study (i.e., when researchers operationalized the same form of psychopathology in multiple ways or studied multiple forms of psychopathology), we used a multilevel structural equation modeling procedure using the metaSEM package (Cheung, 2012) in R 3.3.1 (R Development Core Team, 2008) to account for nonindependence of effect sizes. We created 3-level models, in which level 1 represented the individual effect sizes, level 2 represented differences in effect sizes within a study, and level 3 represented differences between studies. Additional information about the analytic approach is available in Appendix B.
Results
We begin our presentation of the meta-analysis results by discussing the identification and management of outliers and our examination of publication bias. Then, we characterize the sample and present summary effects. Finally, we describe tests of moderation.
Outliers
We ran influential case diagnostics using the metafor package in R (Viechtbauer, 2010). In an effort to be conservative in calculating summary effect sizes, we identified and excluded outliers specific to each domain of psychopathology as well as the overall sample. Effects with studentized deleted residuals ≥ 2 were considered to be outliers (Viechtbauer & Cheung, 2010). Following Gnambs (2013), these outliers were truncated to the upper bound of the 95% confidence interval of the true effect for the applicable domain of psychopathology, which was calculated by computing unconditional models using a dataset from which the outliers had been removed. Thirteen effects were identified as outliers, which is in the expected range for a meta-analysis of this size (Viechtbauer & Cheung, 2010). Comparing these outliers to nonoutliers on study characteristics (e.g., country of data collection) using bivariate analyses revealed no significant differences. All further results describe the sample including truncated outliers.
Publication Bias
Publication bias is a pervasive problem in the empirical literature (Rosenthal, 1979). Despite our extensive efforts to include unpublished work and the significant number of unpublished effects in our sample (175/500 effects), it is likely that there was still more that we were unable to identify.
We used three strategies to assess publication bias. We first compared published (M = 0.64, SD = .41, k = 322) to unpublished (M = 0.50, SD = .31, k = 175) effect sizes, and concluded that published effect sizes were significantly larger, t(443.74) = 4.30, p < .0001. We then calculated Rosenthal’s fail-safe N (Rosenthal, 1979), and determined that 2,153,789 effects evidencing no relationship between SA and psychopathology (g = 0) would be needed to reduce the significance level of the summary effect size to .05. This suggests that substantial publication bias would need to be present to nullify the observed effect. We next constructed a funnel plot (Figure 2) of the relationship between published effect sizes and their corresponding inverse standard errors (an index of study precision) to visually and statistically assess the presence of publication bias. Funnel plots display the spread of effect sizes around the “true” effect size as a function of study precision; lower-precision studies produce wider variation in observed effect sizes (i.e., the mouth of the funnel), and higher-precision studies cluster closely around the true effect size (i.e., the neck of the funnel). Funnel plot asymmetry indicates that effects that are larger or smaller than the true effect are systematically underpublished. We used the trim and fill method to identify the number of effects missing from each side of the funnel plot, impute these missing values, and re-estimate the overall effect including these values (Duval & Tweedie, 2000a, 2000b). Because methods for assessing publication bias in multilevel meta-analysis have not yet been developed and so this test treats effect sizes as independent observations, we randomly selected one effect size from every study in our sample to include in this test to avoid unduly weighting studies that contributed more effects. Eighteen effects were missing from the right side of the funnel and no effects were missing from the left side. Including the 18 imputed missing values, the summary effect was 0.63 (SE = 0.03), as compared to a summary effect of 0.56 (SE = 0.03) without these effects using a fixed-effects meta-analysis using the randomly selected published data. Using Egger’s regression test for funnel plot asymmetry in a model with standard error as a predictor (Egger, Davey Smith, Schneider, & Minder, 1997), we found that this asymmetry was not statistically significant, z = 1.69, p = 0.09. Thus, there is no evidence for publication bias based on the funnel plot.
Figure 2.
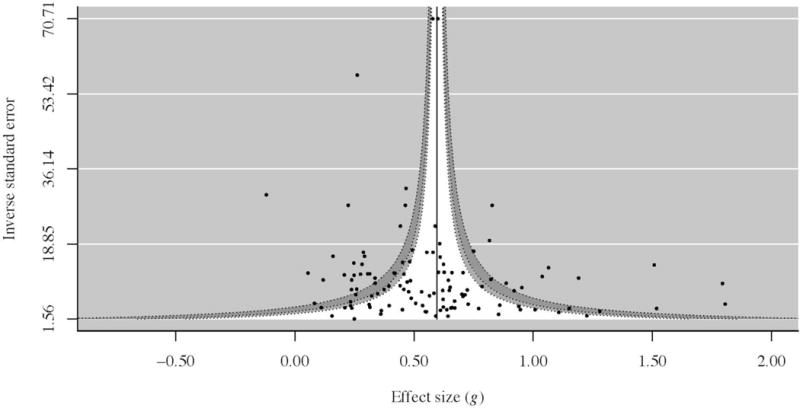
Publication Bias
Sample
See Table 1 for a summary of included studies, Appendix C for the full dataset (Dworkin, Menon, Bystrynski, & Allen, 2017), and Appendix D for corresponding references. The full dataset included k = 497 estimates of effect from 204 sources and m = 195 studies (i.e., independent samples). Results from some samples were published in multiple sources and some sources contained multiple samples. Aggregating sample sizes across studies (using the minimum N used to calculate effect sizes in a given study), this meta-analysis represents N = 238,623 individuals (study range: 27 to 32,075). Among the m = 153 studies where the comparison group was not selectively sampled and the prevalence of SA was an estimate of the prevalence in the population studied, the average SA prevalence was 24.12% (SD = 17.56%, range: 1.59% to 92.57%). Most studies were conducted in the US (77%) and were published journal articles (76%) or dissertations/theses (20%)
Table 1.
Study Characteristics
| Variable | m (studies) | % of studies* |
|---|---|---|
| Publication/data collection year | ||
| 1970s | 0 | 0 |
| 1980s | 14 | 6.90 |
| 1990s | 44 | 21.67 |
| 2000s | 82 | 40.39 |
| 2010s | 63 | 31.03 |
| Continent of data collection | ||
| Africa | 5 | 2.56 |
| Asia | 6 | 3.08 |
| Europe | 18 | 9.23 |
| North America | 158 | 81.02 |
| United States | 151 | 77.44 |
| Canada | 7 | 3.59 |
| Oceania | 4 | 2.05 |
| South America | 2 | 1.03 |
| Multiple | 2 | 1.03 |
| Study type | ||
| Journal article | 155 | 76.35 |
| Dissertation/thesis | 39 | 19.21 |
| Unpublished dataset | 6 | 2.96 |
| Report | 2 | 0.99 |
| Book chapter | 1 | 0.49 |
Percentages do not all sum to 100% because some studies were published in multiple sources
Is Sexual Assault Associated with Psychopathology?
The average effect size across types of psychopathology was g = 0.61 (SE = 0.02), suggesting a moderate association between SA and psychopathology. In this unconditional model, the heterogeneity within studies (due to differences in domains/measures of psychopathology) was τ22 = 0.04 (SE = 0), and the heterogeneity between studies (controlling for differences in domains/measures of psychopathology), or was τ23 = 0.06 (SE = 0.01). Both were significant at p < .001, indicating that significant heterogeneity existed which could be potentially accounted for by moderators.
Moderator Analyses: What Accounts for Differences in Observed Effects?
A summary of moderation analysis results can be found in Table 2.
Table 2.
Moderation Results
| Variable | g | SE(g) | 95% CI | R2 (L2) | R2 (L3) | k | m |
|---|---|---|---|---|---|---|---|
| Psychopathology domain | 0.42 | 0.00 | |||||
| Suicidality | 0.74 | 0.05 | 0.65, 0.83 | 38 | 26 | ||
| Obsessive-compulsive conditions | 0.71 | 0.12 | 0.48, 0.94 | 10 | 9 | ||
| Trauma and stressor-related conditions+ | 0.71 | 0.03 | 0.66, 0.77 | 121 | 103 | ||
| Bipolar conditions | 0.66 | 0.11 | 0.44, 0.87 | 6 | 4 | ||
| Depression** | 0.60 | 0.03 | 0.55, 0.66 | 129 | 102 | ||
| Anxiety** | 0.53 | 0.03 | 0.46, 0.59 | 113 | 62 | ||
| Disordered eating** | 0.39 | 0.07 | 0.24, 0.53 | 21 | 14 | ||
| Substance abuse/dependence** | 0.37 | 0.04 | 0.29, 0.45 | 59 | 33 | ||
| Methodological differences | |||||||
| Operationalizations | |||||||
| Attempted SA included? | 0.00 | 0.06 | |||||
| Completed only+ | 0.64 | 0.03 | 0.59, 0.69 | 350 | 137 | ||
| Attempted and completed* | 0.54 | 0.04 | 0.46, 0.62 | 135 | 54 | ||
| Nonpenetrative SA included? | 0.00 | 0.04 | |||||
| Penetrative only+ | 0.61 | 0.03 | 0.54, 0.68 | 180 | 69 | ||
| Nonpenetrative and penetrative | 0.54 | 0.04 | 0.46, 0.61 | 149 | 55 | ||
| Tactics included | 0.00 | 0.03 | |||||
| Forced only+ | 0.61 | 0.03 | 0.54, 0.67 | 142 | 70 | ||
| Forced and incapacitated | 0.57 | 0.06 | 0.45, 0.69 | 45 | 18 | ||
| Forced and coerced | 0.57 | 0.07 | 0.44, 0.71 | 43 | 13 | ||
| Forced, incapacitated, and coerced | 0.52 | 0.05 | 0.43, 0.61 | 96 | 32 | ||
| Assessment quality | |||||||
| Assessment of SA | 0.01 | 0.04 | |||||
| < quality median (0.75)+a | 0.66 | 0.04 | 0.58, 0.74 | 150 | 61 | ||
| ≥ quality median (0.75)* | 0.54 | 0.03 | 0.48, 0.60 | 238 | 91 | ||
| Assessment of psychopathology | 0.02 | 0.02 | |||||
| < quality median (0.63)+ | 0.57 | 0.03 | 0.51, 0.62 | 198 | 111 | ||
| ≥ quality median (0.63)* | 0.65 | 0.03 | 0.60, 0.71 | 287 | 116 | ||
| Comparison group | 0.00 | 0.08 | |||||
| Type | |||||||
| No SA+ | 0.61 | 0.02 | 0.56, 0.65 | 405 | 152 | ||
| Trauma | 0.59 | 0.05 | 0.50, 0.69 | 85 | 42 | ||
| No trauma** | 1.24 | 0.20 | 0.85, 1.63 | 7 | 3 | ||
| Sample characteristics | |||||||
| Types of assaults experienced | |||||||
| % stranger assaults | 0.01 | 0.18 | |||||
| < stranger median % (16.82)+ | 0.51 | 0.07 | 0.37, 0.64 | 46 | 16 | ||
| ≥ stranger median % (16.82)* | 0.74 | 0.07 | 0.60, 0.88 | 44 | 17 | ||
| Types of assaults experienced, ctd. | |||||||
| % weapon use | 0.00 | 0.71 | |||||
| < weapon median % (10.42)+ | 0.33 | 0.10 | 0.13, 0.53 | 13 | 5 | ||
| ≥ weapon median % (10.42)** | 0.84 | 0.10 | 0.63, 1.04 | 14 | 6 | ||
| % physically injured | 0.00 | 0.93 | |||||
| < injured median % (24.47)+ | 0.32 | 0.07 | 0.18, 0.46 | 13 | 4 | ||
| ≥ injured median % (24.47)** | 0.65 | 0.09 | 0.48, 0.82 | 17 | 4 | ||
| Time since SA | 0.00 | 0.08 | |||||
| < years median (0.63) | 0.73 | 0.07 | 0.60, 0.86 | 50 | 23 | ||
| ≥ years median (0.63) | 0.61 | 0.07 | 0.48, 0.74 | 44 | 24 | ||
| Demographics | |||||||
| Gender | 0.01 | 0.00 | |||||
| ≥ gender median % (100)+ | 0.60 | 0.03 | 0.54, 0.65 | 162 | 70 | ||
| < gender median % (100) | 0.65 | 0.04 | 0.57, 0.72 | 330 | 122 | ||
| Age | 0.00 | 0.00 | |||||
| < sample median age (26.0)+ | 0.61 | 0.04 | 0.54, 0.68 | 138 | 70 | ||
| ≥ sample median age (26.0) | 0.59 | 0.04 | 0.52, 0.66 | 148 | 71 | ||
| Race | 0.00 | 0.03 | |||||
| > 60% White/Caucasian+ | 0.57 | 0.03 | 0.52, 0.62 | 286 | 97 | ||
| > 60% Black/African American | 0.49 | 0.09 | 0.32, 0.66 | 20 | 10 | ||
| > 60% Latino/a | 0.53 | 0.15 | 0.25, 0.82 | 5 | 3 | ||
| > 60% Native American | 1.04 | 0.31 | 0.44, 1.64 | 2 | 1 | ||
| No majority | 0.58 | 0.05 | 0.49, 0.68 | 72 | 30 | ||
| Sample type | 0.00 | 0.14 | |||||
| College students+ | 0.54 | 0.03 | 0.47, 0.60 | 169 | 68 | ||
| General population/unselected* | 0.66 | 0.04 | 0.58, 0.73 | 141 | 52 | ||
| People seeking medical treatment | 0.67 | 0.11 | 0.46, 0.89 | 19 | 7 | ||
| Military personnel or veterans | 0.67 | 0.10 | 0.49, 0.86 | 22 | 10 | ||
| People seeking support for crime-related needs | 0.63 | 0.07 | 0.49, 0.76 | 48 | 22 | ||
| Prison inmates | 0.60 | 0.15 | 0.30, 0.89 | 9 | 3 | ||
| Other | 0.49 | 0.07 | 0.35, 0.63 | 34 | 15 | ||
| Combination of above sample types* | 0.74 | 0.08 | 0.59, 0.89 | 45 | 16 | ||
| Adult/adolescent SA vs. lifetime SA | 0.00 | 0.00 | |||||
| Lifetime SA+ | 0.63 | 0.03 | 0.56, 0.69 | 227 | 95 | ||
| Adult/adolescent SA only | 0.60 | 0.03 | 0.54, 0.66 | 260 | 93 |
Referent group for comparisons
Each continuous moderator was dichotomized via a median split for presentation in this table.
Significantly different from referent group at p < .05
Significantly different from referent group at p < .01
R2 (L2) is the proportion of explained variance within studies
R2 (L3) is the proportion of explained variance between studies
Note. All values of g differed significantly from 0 at p < .01
k = number of effect sizes used in specific analysis
m = number of studies used in specific analysis
What types of psychopathology are associated with sexual assault?
In our sample, depression was the most common domain studied, k = 129, m = 102, followed by trauma and stressor-related conditions, k = 121, m = 103. The most infrequently-studied domain was bipolar conditions, k = 6, m = 4. Average effects were largest for suicidality, g = 0.74, SE = 0.05, k = 38, m = 26, and smallest for substance abuse/dependence, g = 0.37, SE = 0.04, k = 59, m = 33. All domain-level average effect sizes were significantly different from zero (p < .001). All effect sizes were in the moderate range (Cohen, 1988), except for disordered eating and substance abuse/dependence, which were in the small range.
To compare the magnitude of these effect sizes, we selected trauma and stressor-related conditions as the referent group. Compared to effects representing trauma and stressor-related conditions, g = 0.71, SE = 0.03, effect sizes were significantly smaller for depression, Δg = −0.11, SE = 0.03, p < .001, anxiety, Δg = −0.19, SE = 0.03, p < .001, disordered eating, Δg = −0.33, SE = 0.07, p < .001, and substance abuse/dependence, Δg = −0.35, SE = 0.04, p < .001. In contrast, the following effects were not significantly different than trauma and stressor-related conditions: obsessive-compulsive conditions, Δg = 0.00, SE = 0.12, p = .98, suicidality, Δg = −0.03, SE = 0.05, p = .54, and bipolar conditions, Δg = −0.06, SE = 0.11, p = .60. Importantly, though, the effects for obsessive-compulsive conditions and bipolar conditions were based on a small number of studies and effects and had large confidence intervals. These results suggest that SA is associated with all domains of psychopathology studied, and is more strongly related to suicidality and trauma and stressor-related conditions (and, tentatively, obsessive-compulsive and bipolar conditions) than depression, anxiety, disordered eating, and substance abuse/dependence.
Methodological differences
We next tested hypotheses related to study methods.
Operational definition of sexual assault
In this sample of studies, most operationalized SA narrowly—28% included attempted SA, 44% included fondling/nonpenetrative SA, 34% included coerced SA, and 37% included incapacitated SA. We hypothesized that broadening operational definitions of SA would result in smaller effect sizes. Hypothesis 2a was supported: operational definitions that included attempted SA evidenced significantly smaller effect sizes, Δg = −0.10, SE = 0.05, p = .02, as compared to those that included completed SA only. Against Hypothesis 2b, including fondling and other nonpenetrative SA in definitions was not associated with decreased effect sizes as compared to penetrative assault only, Δg = −0.07, SE = 0.05, p = .14. Hypothesis 2b was not supported for operational definitions that included coercion, Δg = −0.04, SE = 0.07, p = .63, incapacitation, Δg = −0.04, SE = 0.07, p = .59, or both coercion and incapacitation, Δg = −0.09, SE = 0.06, p = .12, as compared to those that included forced SA only. This suggests that, with the exception of the inclusion of attempted SA, more evidence would be needed to conclude that changing operationalizations of SA is associated with changes in observed differences between assaulted and nonassaulted samples on psychopathology.
Assessment quality
SA assessment quality varied across effects. Most included multiple items (68% of effects), described at least one sex act behaviorally (70% of effects), and specified at least one tactic through which the sex act occurred (68% of effects), but fewer were previously published (46% of effects). Mean percent quality was 0.68 (SD = 0.35). Hypothesis 3, that lower-quality assessments would be associated with higher effects, was supported, β = −0.07, SE = .03, p < .01, indicating that studies using lower-quality assessments of SA evidenced larger differences between the SA and no-SA groups.
Studies also varied in the quality of their assessments of psychopathology. For most effects, the measure was previously published (88% of effects) and included multiple items (91% of effects), but fewer were administered via interview (47% of effects) or were explicitly stated to be based on and/or validated against DSM criteria (53% of effects). Hypothesis 4, predicting that higher-quality assessments would be associated with higher observed effects, was supported: average quality score was 0.71 (SD = 0.26), and this value was significantly associated with the magnitude of effect sizes, β = 0.04, SE = .02, p = .04. This indicates that indicating that studies using higher-quality assessments of psychopathology evidenced larger differences between the SA and no-SA groups.
Comparison group type
Most studies (81%) used comparison groups that had not experienced SA (i.e., no-assault groups), fewer (17%) used comparison groups that had experienced another form of trauma (i.e., other-trauma groups), and very few (1%) used comparison groups that were selected for their lack of trauma experience (i.e., no/low-trauma groups). Other-trauma groups were most often comprised of people who had experienced physical assault (8%) or any non-SA trauma (11%). Consistent with Hypothesis 5a, compared to studies using a no-SA comparison group, other trauma groups did not differ, Δg = −0.01, SE = 0.05, p = .82 and consistent with Hypothesis 5b, no trauma groups had significantly higher effect sizes, Δg = 0.64, SE = 0.20, p < .01. This indicates that SA survivors evidence significantly greater psychopathology when compared to people who have not experienced trauma, relative to comparisons to people who have experienced a different trauma or who have not experienced SA.
Adult/adolescent or lifetime assault.3
Most samples limited the SA group to those who experienced SA in adolescence and/or adulthood, k = 260, m = 93. Against Hypothesis 6, here was no observed difference in effects as a function of limiting SA to adolescence/adulthood, Δg = −0.02, SE = .04, p = .61, suggesting that there is not enough evidence to indicate that the strength of the association between SA and past-year psychopathology differs when examining lifetime versus adolescent/adult assault.
Sample differences
Our final set of hypotheses addressed differences in samples.
Features of actual assaults experienced by sample
On average, 24% of assaults involved a stranger perpetrator (SD = 23%, range: 0–90%, k = 90, m = 33), 26% involved physical injury (SD = 13%, range: 11–49%, k = 30, m = 8), and 21% involved the use of a weapon (SD = 23%, range: 2–66%, k = 27, m = 11). We hypothesized that higher percentages of each characteristic in the SA group would be positively related to observed effect sizes (i.e., the SA group would be more different from the no-SA group when more members of the SA group experienced assaults with these characteristics). Hypothesis 7a was supported: the percent of survivors who were injured was positively related to the magnitude of difference between groups, β = 0.18, SE = .04, p < .001. Hypothesis 7b was also supported: the percent of assaults that involved a weapon was positively related to the magnitude of difference between groups, β = 0.21, SE = .09, p = .02. Hypothesis 7c was not supported: the percent of stranger perpetrators was unrelated to group differences, β = 0.10, SE = .06, p = .07. Together, this provides evidence that some indices of assault severity are associated with greater severity or frequency of psychopathology.
Time since assault
We limited the sample to those effects that represented past-year psychopathology and reported time since assault (k = 94, m = 47). The mean time elapsed since SA in this subsample was 4.55 years (SD = 9.51, median = 0.63, range: 0.004 to 49.70). Hypothesis 8 was not supported: effects did not differ as a function of years since assault, β = −0.02, SE = .06, p = .70, suggesting that there is not enough evidence to indicate that the strength of the association between SA and past-year psychopathology differs by time since assault. To account for within-study variation in time since assault, we limited the sample to studies assessing past-year SA, and found no differences in effect sizes, β = −0.01, SE = .05, p = .78 (k = 50, m = 23).
Demographic differences
We next tested demographic moderators.
Age
The average of participants’ mean age across studies was 29.84 (SD = 11.13, range: 18.03 to 81.90). We limited the sample to past-year psychopathology because older participants would have a larger range of time in which lifetime psychopathology could have occurred. Hypothesis 9a was supported: effects did not differ as a function of sample mean age, β = 0.00, SE = .02, p = .99. We then limited the sample to studies assessing both past-year SA and past-year psychopathology in order to assess the impact of age at assault on psychopathology. Effect sizes did not differ as a function of sample mean age, β = −1.11, SE = .06, p = .86 (k = 37, m = 19). Finally, to account for within-study variation in participant age, we limited the sample to studies in which most participants had an age within 5 years of the mean (i.e., those studies with SD < 5), and again found no difference in past-year psychopathology, β = 0.01, SE = .03, p = .76 (k = 140, m = 72). These results suggest that there is not enough evidence to suggest that the strength of the association between SA and psychopathology differs by age.
Gender
In the studies included in this analysis, an average of 81.66% of study participants were women (SD = 28.62%). In support of Hypothesis 9b, that effect sizes would not differ as a function of the women in the sample, we found that the percentage of women in the sample was not associated with effect size magnitude, β = −0.03, SE = .02, p = .17. However, because women are significantly more likely to be sexually assaulted, in mixed-gender samples, women may be better-represented in the SA group than men, which could bias the results. Thus, we restricted the dataset to single-gender effect sizes (women-only samples: k = 330, m = 122; men-only samples: k = 14, m = 8). Again, effect sizes did not differ as a function of sample gender, β = −0.02, SE = .06, p = .30. These results suggest that there is not enough evidence to suggest that the association between SA and psychopathology differs by gender.
Race
Most US samples were majority-White/Caucasian (69%). In support of Hypothesis 9c, compared to primarily-White samples, the following groups were not significantly different: majority Black/African American samples, Δg = −0.08, SE = 0.09, p = .40, majority Latino/a samples, Δg = −0.04, SE = 0.15, p = .80, majority Native American samples, Δg = 0.47, SE = 0.31, p = .13, and no-majority samples, Δg = 0.02, SE = 0.05, p = .76. Thus, there was not enough evidence to conclude that racial differences exist in the effect of SA on psychopathology.
Type of sample
Most samples examined college students, k = 169, m = 68, or unselected general population samples, k = 141, m = 52. In partial support of Hypothesis 10, compared to college samples, only general population samples, Δg = 0.12, SE = .05, p = .01, and mixed samples, Δg = 0.20, SE = .08, p = .02, had significantly higher effect sizes. No other differences were observed.
Discussion
As research on SA’s psychological impact has evolved, it has become increasingly clear that SA can have major implications for psychopathology in survivors. In the current meta-analysis, which included 497 estimates of the relationship between SA and psychopathology representing 238,623 individual participants, people who experienced SA evidenced significantly more psychopathology across diagnostic categories than people who have not experienced SA. Further, the effect of SA on psychopathology appears to be stronger than previously estimated. The only prior meta-analysis to examine the association between adult SA and distress (broadly defined to include both psychopathology and distress across domains of life functioning) across 38 studies estimated an average effect size of r = .21 (Weaver & Clum, 1995), which is roughly equivalent to g = .43. The overall effect size of g = 0.61 observed in the current analysis indicates that an experience of SA is associated with more than half a standard deviation increase in psychopathology, and provides evidence that many survivors of SA experience increased frequency or severity of psychopathology.
What Forms of Psychopathology are Associated with Sexual Assault?
An unresolved question in this body of literature is whether SA has a narrow psychological impact (i.e., on PTSD) or a broad impact on a range of mental disorders. PTSD has been reconceptualized in DSM-5 as a condition distinct from the anxiety disorders given that trauma exposure is seen as a necessary condition for its onset (APA, 2013). Although other disorders (e.g., depression) may follow trauma, they may also emerge in the absence of trauma. In this analysis, although trauma and stressor-related conditions evidenced one of the strongest associations with a history of SA, SA was significantly positively related to all forms of psychopathology studied, suggesting that SA is broadly associated with psychopathology. The relatively high effect size for trauma and stressor-related disorders is unsurprising, because trauma exposure is a necessary precondition to receive a diagnosis of PTSD, and effect sizes compared groups that had experienced one such trauma (i.e., SA) to groups that had not necessarily been exposed to trauma. Thus, SA groups would be expected to, by definition, evidence more PTSD than no-SA groups. As a result, although SA was associated with greater risk for PTSD than depression, anxiety, disordered eating, and substance abuse/dependence, it is important to be cautious about interpreting the relative magnitude of these effects as evidence to support the idea that PTSD is necessarily a distinct psychological phenomenon. It also is possible that the higher prevalence of non-PTSD disorders in SA populations reflects the high comorbidity of these disorders with PTSD or overlapping symptoms between PTSD and conditions like depression and anxiety (Kessler et al., 1995). Patterns of comorbidity with PTSD in SA populations should be investigated in future research to understand whether these conditions arise directly from SA or are secondary to PTSD.
Survivors of SA appear to be at substantially increased risk for suicidal ideation and attempts; indeed, relative to other conditions, SA was associated with the highest increases in risk for suicidality. This is consistent with past epidemiological studies that have controlled for other risk factors (Ullman & Brecklin, 2002; Stein et al., 2010). Of the disorders assessed in this analysis, suicidality is explicitly included as part of the diagnostic criteria in DSM-5 for depression only, which evidenced a significantly smaller effect size relative to suicidality (APA, 2013). Thus, although explicitly shared symptoms with other disorders are likely an insufficient explanation for the strong association between SA and suicidality, all types of psychopathology included in this analysis have been associated with elevated risk for suicidality (Harris & Barraclough, 1997; Panagioti et al., 2012; Preti et al., 2011), including in SA-specific samples (Ullman & Brecklin, 2002). It is possible, then, that survivors of SA are at high risk for suicidality because its risk is elevated across forms of psychopathology associated with SA, and may be even more highly elevated when disorders co-occur (Panagioti et al., 2012). However, evidence from cross-national epidemiological studies indicates that SA is more strongly associated with suicidality than other forms of trauma, and this effect appears to be independent of co-occurring disorders (Stein et al., 2010). It is also possible that this is due to the high degree of stigma and shame associated with SA victimization (Rudd, 2006). This evidence highlights the importance of screening for lethality risk and safety planning among SA survivors, and suggests that future research clarifying the mechanism of the relationship between SA and suicidality would be useful.
SA also appears to be associated with substantially increased risk for bipolar conditions and obsessive-compulsive conditions. Although these conditions are typically thought to be highly genetically-based (Etain et al., 2008; Hettema, Neale, & Kendler, 2001), emerging empirical evidence suggests that trauma may play a bigger role in their development than previously thought (Cromer, Schmidt, & Murphy, 2007; Etain et al., 2008). These results must be interpreted with caution, given the relatively small number of studies on which they were based coupled with their large confidence intervals, but it is still important to consider associations between SA and both conditions. One potential explanation is that experiencing SA could trigger symptom expression in these disorders (e.g., mania, checking rituals) to a greater degree than other conditions (Cromer et al., 2007). Comorbid PTSD may also explain this relationship. For example, there is some evidence that PTSD can be misdiagnosed as bipolar disorder (Hernandez et al., 2013), and intrusive thoughts related to trauma could instead be miscategorized as a symptom of obsessive-compulsive disorder. In addition, having PTSD related to SA could interfere with obsessive-compulsive disorder treatment (Gershuny et al., 2002).
Although the association between substance use disorders and PTSD after SA (e.g., Kilpatrick et al., 1997) has been well-documented, survivors of SA appear to be at relatively lower risk of substance use disorders than other conditions. Prospective studies have found no effect for SA on problem substance use when controlling for pre-assault drinking (Testa & Livingston, 2000; Testa, Livingston, & Hoffman, 2007). It is possible that substance use, rather than abuse/dependence per se, is associated with assault, given that much of the literature in this area has identified associations for substance use. Because substance use after SA has been conceptualized as a strategy to reduce negative affect (Kilpatrick et al., 1997), it would seem to be more likely to be present either in the subset of survivors with other disorders (e.g., PTSD; Chilcoat & Breslau, 1998; Stewart & Conrad, 2003) or in the early aftermath of assault only, when distress is more typical (e.g., Rothbaum, Foa, Riggs, Murdock, & Walsh, 1992). Survivors in the latter group might not have significantly higher substance use than nonsurvivors who use substances to cope with other life stresses, and any negative affect driving substance use would be likely to dissipate relatively quickly. This possibility should be tested empirically.
Although it is difficult to discern whether SA necessarily has an etiological role in psychopathology, the greater prevalence and severity of a range of mental disorders in survivors of SA suggests that trauma exposure should be considered when treating mental disorders. Trauma exposure generally, and SA exposure specifically, should be assessed to inform case conceptualization. If SA plays an etiological role in the development of non-PTSD conditions, trauma-informed interventions may be more effective than disorder-specific treatments for survivors of SA with these conditions. Additionally, if SA is considered to be a broad risk factor for distress rather than a specific etiological risk factor for certain disorders, transdiagnostic approaches, such as the Unified Protocol (Ellard, Fairholme, Boisseau, Farchione, & Barlow, 2010), could have added success in treating distress arising from SA. This possibility, as well as the possible etiological role of SA in a range of mental disorders beyond PTSD, should be investigated in future research.
How do Differences in Study Methods and Samples Alter Observed Effects?
To guide future research on SA and psychopathology, it is important to understand how methodological choices—such as the measures used and population sampled—might affect study results. Next, we review these methodological choices in light of the current results.
Critics have raised questions about the appropriate breadth of operational definitions of SA (e.g., Gilbert, 1993). These critics argue that the only people who should be considered victims in a research context are those who experienced forms of SA that match narrow societal stereotypes regarding the types of sexual acts involved and tactic used to compel them (e.g., forcible rape) (Cook et al., 2011; Koss, 2011). In light of these controversies, it is important to understand whether broadening operational definitions has an effect on differences in psychopathology between assaulted and unassaulted groups. In the current analysis, we found that including coerced, and incapacitated SA in operational definitions did not significantly alter observed group differences in psychopathology. Although including attempted SA reduced group differences, it is important to note that studies that included both attempted and completed assaults still evidenced moderate-sided effects. This indicates that broadening operational definitions to include attempted SA may reduce effect sizes somewhat, but they are not lowered to the point of inconsequentiality. An important limitation of these findings is that they only reflect the operational definition of SA, and not the actual inclusion of assaults that fall under these broader operational definitions in the SA group. For example, it is possible that a study considered people who experienced either attempted or completed SA to fall in the SA group, but all members of the SA group experienced completed SA. It is likely, though, that broadening these operational definitions added a substantial number of participants to the SA group who would otherwise have been in the comparison group. Indeed, past studies have found that including attempted rape increased the size of the SA group by 65–79% (Fisher et al., 2000; Koss et al., 1987), including coerced SA increased the size of the SA group by 77–164% (Koss et al., 1987), and including nonpenetrative SA increased the size by 94–232% (Koss et al., 1987). Further, a meta-analysis failed to find differences in psychopathology between penetrative and nonpenetrative child sexual abuse (Paolucci & Genuis, 2001), providing support for the current findings. Thus, in spite of these limitations, our results provide evidence that narrowing operational definitions in terms of the acts and tactics included does not significantly obscure group differences.
The quality of measures used to assess SA and psychopathology may also affect study results. Lower-quality SA assessment methods—which we defined as those using measures that contained a single item only, were unpublished, did not behaviorally define SA, and/or did not specify a tactic through which SA could have occurred—tended to overestimate group differences. It is possible that societal disagreement about what “counts” as SA necessitates more assessment specificity. SA survivors who have not experienced assaults that are consistent with societal SA schemas (e.g., acquaintance rape) might be less likely to endorse questions like, “have you ever been raped?,” and their inclusion in the no-SA group would thus lessen observed group differences. It is notable that the population of studies included in this analysis varied widely in the quality of SA assessments. The same was not true for the psychopathology assessment quality: lower-quality assessment methods appeared to underestimate group differences. While a past meta-analysis on the relationship between interpersonal violence and distress did not find evidence that indicators of validity were associated with effects, this prior analysis was not limited to diagnostic constructs (Weaver & Clum, 1995). Although rigorous assessment methods tend to be more time-intensive for participants, these results suggest that researchers may introduce bias to their estimates of the impact of psychopathology on SA by using lower-quality assessments.
The selection of the group against which sexually assaulted people are compared may also alter study results. As expected, effect sizes were significantly higher for studies using no-trauma comparison groups than for studies using no-assault or other-trauma comparison groups. It is likely that no-assault comparison groups are comprised mostly of people who experienced some other form of trauma, even though they were not selected for this quality, so it is not surprising that intentionally selecting a comparison group comprised of no/low trauma resulted in large differences from a SA group. These results also suggest that SA has a stronger association with psychopathology than other forms of trauma, consistent with past work (Kelley et al., 2009; Kessler et al., 1995). SA’s uniquely strong impact on psychopathology could occur for several reasons. First, SA commonly co-occurs with other forms of trauma like intimate partner violence and child sexual abuse (Campbell, Greeson, Bybee, & Raja, 2008). The increased risk of psychopathology observed in SA might be associated with cumulative trauma exposure rather than SA specifically (Green et al., 2000). Indeed, although having a past trauma generally increased the risk for PTSD in a different meta-analysis, this effect was strongest when the current trauma was interpersonal violence (Ozer et al., 2003). Second, it is possible that survivors of SA receive less social support following trauma than survivors of other traumas, given the stigma associated with rape, and social support has been identified as a correlate of PTSD (Brewin et al., 2000; Ozer et al., 2003). Third, it is possible that pre-trauma psychological problems might be more common in SA than in other traumas, which would increase risk for post-trauma psychopathology (Ozer et al., 2003). Fourth, experiencing an interpersonal trauma of such a personal nature could be uniquely violating (Green et al., 2000). These possibilities should be explored in future meta-analyses.
Given the large number of studies from the general trauma literature that do not specify at what age SA must have occurred, as well as the division of the SA literature into adult/adolescent SA research and child SA research, it is important to understand whether lifetime SA studies can be integrated into reviews and theoretical development regarding adolescent/adult SA. Although prior meta-analyses found that age at trauma exposure was associated with PTSD (Brewin et al., 2000; Ozer et al., 2003), we did not find that including lifetime SA studies—which likely included survivors of child SA in their SA groups—reduced effects. In light of the high rates of adolescent/adult victimization after childhood SA (Classen, Palesh, & Aggarwal, 2005), it is possible that few survivors of child SA who had not also experienced adolescent/adult SA were included in the SA group in lifetime studies. Nevertheless, these findings do not suggest that studies of lifetime SA and adolescent/adult SA are so distinct as to be incomparable.
Understanding how assault features might be associated with psychopathology can clarify the development of psychopathology and inform targeted interventions to mitigate the harm of assault. It appears that assault characteristics like stranger perpetrators, weapon use, and resulting physical injury, are associated with higher risk for psychopathology. It is possible that these assault characteristics make the assault itself more distressing or increase perceived life threat, which then increases risk for the development of later psychopathology (Ozer, Best, Lipsey, & Weiss, 2003). These results help to contextualize the findings of a past review on gender differences in PTSD by trauma type: adult SA was one of the only traumas that did not appear to have a higher frequency or severity of PTSD in women as compared to men, and the authors hypothesized that this might be explained by the greater likelihood of physical injury and other markers of severity or life threat not addressed in this meta-analysis (e.g., multiple perpetrators) (Tolin & Foa, 2006). Early intervention efforts could be targeted to survivors of these types of assaults in order to reduce their impact.
The effect of SA on psychopathology appears to be relatively durable over time. In one of the earliest prospective longitudinal studies of the impact of SA on PTSD, results suggest that symptoms decrease rapidly over the first month post-SA for survivors who do not ultimately develop PTSD, but are relatively durable over time for survivors with PTSD (Rothbaum et al., 1992). In contrast, past reviews suggest that the impact of interpersonal violence broadly on distress appears to decrease over time (Weaver & Clum, 1995), as does the impact of intimate partner violence on depression (Golding, 1999). It is possible that SA has a more durable effect on psychopathology than other types of interpersonal violence. This emphasizes the critical importance of increasing access to the multiple highly-effective short-term treatments for PTSD (e.g., Cognitive Processing Therapy, Prolonged Exposure Therapy) and other conditions (e.g., cognitive behavioral therapy for depression, exposure and response prevention for OCD) among SA survivors. Because these treatments are designed to resolve symptoms within months, their use can reduce the long-term impact of SA while making efficient use of provider time and minimizing survivors’ financial costs and time investment. Rape crisis center counselors can be trained to offer these treatments, or can maintain community referral lists to connect survivors with these services.
Understanding which demographic groups are most affected by SA can help to target outreach and prevention efforts. However, it does not appear that any particular demographic group evidences relatively higher post-assault psychopathology. Although race/ethnicity and age had little support from past meta-analyses in relation to observed effects, there had been some prior support for the role of gender. A meta-analysis identified gender differences in the impact of interpersonal violence on distress (Weaver & Clum, 1995), but this previous analysis’s study population lacked representation from men and contained no men-only samples, which could have underestimated the impact of SA on men. Men, people who identify as transgender, and sexual minorities are significantly understudied populations with regard to the impact of SA, and more research is needed to understand their post-assault experiences.
Across populations like college students, people seeking healthcare, military/veterans, prison inmates, and people seeking support for crime-related needs, the impact of SA appears to be similarly substantial. People in most of these populations may be more likely to have characteristics that could represent better psychological functioning (e.g., employment, student status, help-seeking behavior), but regardless, people exposed to SA still evidence higher levels psychopathology relative to those unexposed to SA. In the general population, though, there are likely to be SA survivors who have withdrawn from the workforce voluntarily or involuntarily, dropped out of educational opportunities, or ceased help-seeking due to the severity of the impact of SA. As a result, research on general population samples appears to evidence the greatest differences in psychopathology between assaulted and unassaulted groups.
Causal Associations Between Sexual Assault and Psychopathology
It is clear that SA and psychopathology have a robust association, but a causal relationship between SA and psychopathology cannot be inferred from this body of work. Indeed, there are multiple mechanisms through which the observed relationship could occur.
The first set of mechanisms explaining the relationship between SA and psychopathology involve increases in vulnerability to psychopathology as a result of SA. Generally, in these mechanisms, SA and its aftermath would be expected to produce the distorted cognitions (e.g., overestimation of dangerousness of situations), alterations to mood (e.g., sadness, fear), and changes to behavior (e.g., increased substance use, behavioral avoidance, social withdrawal, compulsions) seen across all disorders studied. First, distress could arise directly from the assault or its aftermath. SA is experienced as a trauma by some survivors, and this experience of violation or life threat could cause psychopathology; indeed, in the current analysis, studies with larger proportions of survivors of assaults that likely involved more life threat (e.g., weapon use) evidenced larger effect sizes. In addition, negative experiences at multiple levels of the social ecology (e.g., negative experiences with community responders, lack of social support) could intensify distress (Campbell et al., 2009). Survivors’ pre-existing coping strategies could also affect the degree to which this distress becomes problematic or long-lasting (Ullman et al., 2007). Second, SA could worsen existing disorders. In support of this idea, a meta-analysis of risk factors for PTSD found that past difficulties with psychological adjustment were particularly strongly related to post-trauma psychopathology for survivors of SA relative to other traumas (Ozer et al., 2003) and a literature review on associations between SA and psychopathology identified pre-assault mental health difficulties as a predictor of post-assault psychopathology (Campbell et al., 2009). Because people who have experienced SA are particularly likely to have also experienced past traumas, like CSA, distress from these multiple traumatic experiences may be cumulative (Arata, 1999). Third, SA could trigger the expression of a genetic liability. Indeed, the broader field of developmental psychopathology has moved away from diathesis-stress models towards gene-by-environment interplay models, in which environments have an interactive, rather than an additive effect on psychopathology (Kendler et al., 1997; Kendler et al., 2003).
Another possibility, consistent with stress generation theory (Conway, Hammen, & Brennan, 2012), is that psychopathology could increase risk for SA, perhaps through impairment to attentional, concentration, and motivational systems that result in reduced capacity to identify and avoid threats (Orcutt, Erikson, & Wolfe, 2002; Pineles, Shipherd, Welch, & Yovel, 2007). Indeed, there is some evidence from the SA revictimization literature, albeit mixed, that the psychosocial consequences of childhood SA increase risk for adolescent/adult SA via increased contact with potential perpetrators (e.g., as a result of using alcohol) and/or an increased likelihood that perpetrators will target the individual (e.g., due to impaired risk recognition) (Classen et al., 2005; Messman-Moore & Long, 2003). There is a relative dearth of prospective studies that assess the causal direction of the relationship between psychopathology and SA, but meta-analyzing these studies could clarify this issue.
Strengths and Limitations
This meta-analysis had a number of strengths. First, our exhaustive study retrieval strategy led to the identification of a large number of effects, many of which were unpublished, which minimizes publication bias while also increasing confidence in effects. Second, because we used both continuous and categorical measures of psychopathology to calculate effect sizes, our findings reflect both syndromal and subsyndromal psychopathology, and thus provide a more accurate representation of the range of effects on survivors than a study including only categorical data. Because trauma survivors may drop below a diagnostic threshold as they recover but continue to evidence chronic distress, capturing only syndromal psychopathology is likely to underestimate group differences (Ozer et al., 2003). Third, our sophisticated analytic strategy involving attention to publication bias and dependency in effects increases our confidence in the study findings. Although investigating between versus within study variance was not a central research question, our approach meant that we did not violate assumptions of independence of observations because we drew multiple effect sizes from many studies.
There also are several limitations to this work. First, because the focus of this study was primarily on study-level differences in effect sizes, we did not assess a number of characteristics of survivors that could explain observed heterogeneity, including pre-trauma factors (e.g., past history of victimization), peri-traumatic factors (e.g., peri-traumatic dissociation, perceptions of life threat), and post-traumatic factors (e.g., self-blame, social support). It is also unclear whether the study-level moderators (e.g., percent of women in the sample, percent of assaults involving weapons) tested would evidence similar effects in relation to psychopathology when directly comparing survivors with these characteristics. These questions would be better answered in a meta-analysis focused on differences between survivors on these characteristics, instead of between survivors and nonsurvivors, as in the current work. Such a meta-analysis should include studies without comparison groups, which the current study did not (302 studies were excluded for this reason). Second, we are not able to make causal inferences because we coded cross-sectional data only; although few prospective longitudinal studies exist that could parse out these effects (e.g., Calhoun, Atkeson, & Resick, 1982; Kilpatrick et al., 1981; Zweig, Crockett, Sayer, & Vicary, 1999), future meta-analyses should address this question. Third, as in any meta-analysis, the findings are only as strong as the studies that contribute to it. A limitation of this body of work identified through this review is the use of single-item, unpublished assessments of SA without behaviorally-based descriptions, which fail to capture a large minority of SA survivors (Cook et al., 2011) and appear to overestimate effects. Future meta-analyses could limit their samples to only rigorously-conducted studies to determine whether findings persist. Fourth, we are not able to rule out biased reporting as an explanation for effects. People are more likely to remember events that match their mood at the time of recall (Bower, 1981), suggesting that people who are in distress due to psychopathology might be more likely to endorse SA, or people experiencing negative affect might be more likely to endorse both SA and psychopathology. Finally, we did not assess every outcome of SA. Several forms of psychopathology (e.g., personality disorders), externalizing behaviors (e.g., substance use), and problems in living (e.g., health problems), as well as co-occurring problems within and across these domains, were not within the scope of this analysis and should be investigated in future reviews.
Conclusion
There is strong evidence that SA victimization is associated with increased risk for multiple forms of psychopathology across most populations, assault types, and methodological differences in studies. This indicates that conditions beyond PTSD alone should be considered in relation to histories of trauma exposure in research and practice, and that increased dissemination of evidence-based practices for trauma-related conditions to SA survivors is critically needed.
Supplementary Material
Highlights.
Associations between sexual assault and psychopathology are meta-analyzed
Sexual assault was associated with increased risk for and severity of all disorders
Effects were largest and most robust for PTSD and suicidality
Samples reporting more severe assaults evidenced more psychopathology
Sexual assault history should be considered when treating common mental disorders
Acknowledgments
The authors would like to thank Konrad Bresin, Yara Mekawi, and Xiaolu Zhu, who provided methodological consultation, Debra Kaysen and Yara Mekawi, who provided feedback on a draft manuscript, the researchers who provided unpublished data, and the undergraduate research assistants who assisted with this study: Amanda Abraham, Alexis Thorstenson, Allison Schartman, Ashton Fields, Christina Mantas, Kulsumjehan Siddiqui, Laura Seimetz, Mary Kennedy, Namrata Nanavaty, and Thane Fowler assisted with study retrieval and coding, and Courtney Marin, Cynthia Blocker, Daniel Szoke, Kimber Schmitt, and Lauren Knight assisted with study retrieval.
Funding
Manuscript preparation was supported in part by a grant from NIAAA [grant number T32AA007455, PI: Larimer]. NIAAA had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Appendix A: Coding Procedure
The primary coders developed a detailed codebook and trained the secondary coders by collaboratively coding articles each week with them for a semester (18–24 articles, depending on training semester) and meeting weekly to discuss each code. After the successful completion of this training process, secondary coders independently coded articles that were then checked by a primary coder, or checked the work of the primary coders. Secondary coders independently coded k = 213 effects (43% of the effects), all of which were checked by the first author, and 46% of which were double-checked by the second author. The first author independently coded k = 263 (53%) of the effects. Of these, 58% were checked by the second author, 9% were checked by the third author, and 33% were checked by a member of the secondary coding team. The remainder of the effects were coded by the second author and checked by either the first author or both the first author and a secondary coder.
Overall SA and no-SA group sample sizes presented by authors did not always reflect the sample sizes used in specific bivariate analyses (i.e., authors sometimes did not report missing data). We coded outcome-specific sample sizes and took steps to ensure that we recorded sample sizes that reflected missing data. For dichotomous outcomes, when authors presented the number of people positive for an outcome in each group along with a percentage that that number reflected, we computed the outcome-specific sample size by dividing the number presented by the percentage (e.g., if there were 10 people with depression in the SA group and the authors stated that this was 10% of the SA group, we divided 10/.01 = 100). We also examined degrees of freedom presented for bivariate analyses to check the accuracy of sample sizes. If this information led us to believe that sample sizes were smaller than what the authors presented, and we were able to compute effect sizes by other information provided that was not dependent on sample size (e.g., t-tests), we coded these values instead of means and standard deviations. If we were not able to compute effect sizes without sample sizes, we reduced the sample size proportionally in each group to match the overall reduction in sample size (e.g., if there were 20 missing cases in a study in which 25% of the sample had been sexually assaulted, we removed 5 from the SA group and 15 from the no-SA group). These strategies allowed us to determine an accurate effect size that was unbiased by inflated sample sizes. Nevertheless, it is possible that sample sizes do not reflect missing data in cases in which the authors did not provide adequate information to allow us to make this determination.
To code effect sizes for dichotomous outcomes, we constructed a 2×2 contingency table based on data presented regarding the frequency of experiencing and not experiencing the outcome in each group. We added .5 to all cells when one or more was zero (Lipsey & Wilson, 2001). To code effect sizes for continuous outcomes, we recorded means and standard deviations for both groups and the sample size specific to that outcome. If these univariate statistics were not available, we coded bivariate t, F, or point-biserial r statistics. When a study reported both a continuous and a categorical effect for the same data (e.g., mean score on a scale and the percent scoring above a specified cutoff), we coded the continuous effect.
- Lipsey MW, Wilson DB. Practical meta-analysis. Thousand Oaks, CA: Sage Publications, Inc; 2001. [Google Scholar]
Appendix B: Analyses
Increasingly, researchers conducting meta-analyses have attended to the issue of dependence in effect sizes. When multiple effects are presented in a single study–in the current study, this occurred when researchers operationalized the same form of psychopathology in multiple ways or studied multiple forms of psychopathology–it is desirable to code each effect. However, these effects are not independent from each other, because they are nested within the same sample and the same research methodology. There are multiple approaches to manage this problem. One approach is to treat these effects as independent. Some researchers attempt to partially account for nonindependence by weighting effect sizes by some study-level characteristic (e.g., inverse variance of effect sizes). Both approaches, though, artificially inflate study power by treating each study as contributing multiple degrees of freedom, and thus increase type I error. Another approach is to code only a single effect per study. One could achieve this by significantly limiting the scope of eligible effects, which would limit the scope of the meta-analysis, or randomly selecting a single effect size to code. Another approach is to average effects within studies (e.g., Weaver & Clum, 1995). However, many effect-level moderators (e.g., type of psychopathology) would then be masked, which would preclude a full examination of heterogeneity in effects through the testing of moderators.
In research beyond meta-analyses, the issue of nonindependent observations in research is typically addressed through multilevel modeling, which partials variance into within-group and between-group components. Increasingly, researchers have used variations on this approach to address this problem when it arises in meta-analyses. We selected one such variation, multilevel structural equation modeling, which we conducted using the metaSEM package (Cheung, 2012) in R 3.3.1 (R Development Core Team, 2008). We created a three-level model, in which level 1 represents the individual effect sizes, level 2 represents differences in effect sizes within a study, and level 3 represents differences between studies. R code used for this study is available on request from the authors.
Although a three-level meta-analysis was warranted given the data structure, we nevertheless tested the null hypothesis that heterogeneity in effect sizes exists at level 3 (τ2(3) = 0), which would indicate that this variance should be accounted for statistically (Cheung, 2014). The likelihood ratio test was 77.53 (df = 1), p < .0001, suggesting that the 3-level model is statistically superior to the 2-level model. We then tested whether significantly more heterogeneity exists at level 3 (controlling for differences in domains/measures of psychopathology) than level 2 (due to differences in domains/measures of psychopathology) (H0: τ2(3) = τ2(2)) by conducting a likelihood ratio test in which level 2 and level 3 random effects heterogeneity variances were both constrained to 0.1. The likelihood ratio test was 3.30 (df = 1), p = .07, suggesting that there is insufficient evidence to reject the null hypothesis that level 2 heterogeneity is equivalent to level 3 heterogeneity. These findings indicate that a 3-level meta-analysis is warranted and suggest the presence of significant heterogeneity at both level 2 and level 3 that could be accounted for by moderators.
We first tested an unconditional 3-level model (i.e., without independent variables) to examine the overall effect size and assess the amount of heterogeneity across levels. We then tested models with independent variables to examine moderation hypotheses. For each categorical moderator, all categories were entered simultaneously into the model and the intercept was constrained to zero to estimate the average effect size for each. We then compared the relative magnitude of effects by dummy coding variables and selecting one as the referent group, which was left out of the model. Continuous moderators were directly entered into the model.
Appendix D: Studies Included in Analysis
- Cheung MWL. metaSEM: An R package for meta-analysis using structural equation modeling. Frontiers in Psychology. 2012;5:1–7. doi: 10.3389/fpsyg.2014.01521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung MWL. Modeling dependent effect sizes with three-level meta-analyses: A structural equation modeling approach. Psychological Methods. 2014;19(2):211–229. doi: 10.1037/a0032968. [DOI] [PubMed] [Google Scholar]
- R Development Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing; Vienna, Austria: 2008. URL http://www.R-project.org. [Google Scholar]
- Weaver TL, Clum GA. Psychological distress associated with interpersonal violence: A meta-analysis. Clinical Psychology Review. 1995;15(2):115–140. [Google Scholar]
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
ERD designed the study and conducted statistical analyses in consultation with NEA, SVM, and JB. ERD and SVM developed the protocol, reviewed study eligibility, and coordinated data extraction. ERD, SM, and JB were primarily responsible for extracting data. ERD drafted the manuscript with contributions from SVM, JB, and NEA. All authors contributed to and have approved the final manuscript.
Conflict of Interest
All authors report that they have no conflicts of interest.
These conditions are referred to in nondiagnostic terms to indicate that this review includes a range of forms of psychopathology in each of these domains, from subthreshhold symptoms assessed with self-report measures to diagnoses assessed with diagnostic interviews.
No non-US country was represented with sufficient frequency to test within-country racial differences. Cross-country tests of racial differences would have limited utility under the assumption that race is a context-dependent social construct.
We also tested this moderator in two-way interactions with each other moderator. No significant interactions were identified, which provides further evidence that including studies that do not limit sexual victimization to adolescence/adulthood does not appear to impact observed effects.
References
- Abrams MP. Human tonic immobility: An exploration of three trauma contexts. 2008 (Unpublished master’s thesis) [Google Scholar]
- Acierno R, Lawyer SR, Rheingold AA, Kilpatrick DG, Resnick HS, Saunders BE. Current psychopathology in previously assaulted older adults. Journal of Interpersonal Violence. 2007;22(2):250–258. doi: 10.1177/0886260506295369. [DOI] [PubMed] [Google Scholar]
- Amir M, Sol O. Psychological impact and prevalence of traumatic events in a student sample in Israel: The effect of multiple traumatic events and physical injury. Journal of Traumatic Stress. 1999;12(1):139–154. doi: 10.1023/A:1024754618063. [DOI] [PubMed] [Google Scholar]
- Aosved AC, Long PJ, Voller EK. Sexual revictimization and adjustment in college men. Psychology of Men & Masculinity. 2011;12(3):285–296. doi: 10.1037/a0020828. [DOI] [Google Scholar]
- Arata CM. Repeated sexual victimization and mental disorders in women. Journal of Child Sexual Abuse. 1999;7(3):1–17. doi: 10.1300/J070v07n03. [DOI] [Google Scholar]
- Arata CM, Burkhart BR. Post-traumatic stress disorder among college student victims of acquaintance assault. Journal of Psychology and Human Sexuality. 1996;8(1–2):79–92. [Google Scholar]
- Badour CL. An empirical investigation of emotional reactivity and elevated mental contamination: A comparison of sexual and physical assault. 2011 (Unpublished master’s thesis) [Google Scholar]
- Bailey CA, Gibbons SG. Physical victimization and bulimic‐like symptoms: Is there a relationship? Deviant Behavior. 1989;10(4):335–352. doi: 10.1080/01639625.1989.9967821. [DOI] [Google Scholar]
- Balsam KF, Lehavot K, Beadnell B. Sexual revictimization and mental health: A comparison of lesbians, gay men, and heterosexual women. Journal of Interpersonal Violence. 2011;26(9):1798–1814. doi: 10.1177/0886260510372946. [DOI] [PubMed] [Google Scholar]
- Becker JV, Skinner LJ, Abel GG, Axelrod R, Treacy EC, Ma ECT. Depressive symptoms associated with sexual assault. Journal of Sex and Marital Therapy. 1984;10:185–192. doi: 10.1080/00926238408405944. [DOI] [PubMed] [Google Scholar]
- Belik SL, Stein MB, Asmundson GJG, Sareen J. Relation between traumatic events and suicide attempts in Canadian military personnel. Canadian Journal of Psychiatry. 2009;54(2):93–104. doi: 10.1177/070674370905400207. [DOI] [PubMed] [Google Scholar]
- Ben-Ezra M, Palgi Y, Sternberg D, Berkley D, Eldar H, Glidai Y, Shrira A. Losing my religion: A preliminary study of changes in belief pattern after sexual assault. Traumatology. 2010;16(2):7–13. http://dx.doi.org/10.1177/1534765609358465. [Google Scholar]
- Betts KS, Williams GM, Najman JM, Alati R. Exploring the female specific risk to partial and full PTSD following physical assault. Journal of Traumatic Stress. 2013;26:86–93. doi: 10.1002/jts. [DOI] [PubMed] [Google Scholar]
- Binder-Brynes KL. The prevalence of fear and depression in sexually abused women: An analysis of archival data. 1991 (Unpublished doctoral dissertation) [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL) Behaviour Research and Therapy. 1996;34(8):669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Blix I, Brennen T. Mental time travel after trauma: The specificity and temporal distribution of autobiographical memories and future-directed thoughts. Memory. 2011;19(8):956–967. doi: 10.1080/09658211.2011.618500. [DOI] [PubMed] [Google Scholar]
- Blix I, Brennen T. Retrieval-induced forgetting after trauma: A study with victims of sexual assault. Cognition and Emotion. 2012;26(2):321–331. doi: 10.1080/02699931.2011.570312. [DOI] [PubMed] [Google Scholar]
- Bolton EE, Litz BT, Britt TW, Adler A. Reports of prior exposure to potentially traumatic events and PTSD in troops poised for deployment. Journal of Traumatic Stress. 2001;14(1):249–256. [Google Scholar]
- Borja SE, Callahan JL, Rambo PL. Understanding negative outcomes following traumatic exposure: The roles of neuroticism and social support. Psychological Trauma: Theory, Research, Practice, and Policy. 2009;1(2):118–129. doi: 10.1037/a0016011. [DOI] [Google Scholar]
- Boudreaux E, Kilpatrick DG, Resnick HS, Best CL, Saunders BE. Criminal victimization, posttraumatic stress disorder, and comorbid psychopathology among a community sample of women. Journal of Traumatic Stress. 1998;11(4):665–678. doi: 10.1023/A:1024437215004. [DOI] [PubMed] [Google Scholar]
- Brener ND, McMahon PM, Warren CW, Douglas KA. Forced sexual intercourse and associated health-risk behaviors among female college students in the United States. Journal of Consulting and Clinical Psychology. 1999;67(2):252–259. doi: 10.1037/0022-006X.67.2.252. [DOI] [PubMed] [Google Scholar]
- Breslau N, Davis GC, Andreski P, Peterson E. Traumatic events and posttraumatic stress disorder in an urban population of young adults lifetime prevalence of exposure to traumatic events. Archives of General Psychiatry. 1991;48:216–222. doi: 10.1001/archpsyc.1991.01810270028003. [DOI] [PubMed] [Google Scholar]
- Brooks CW. Forgiveness and empathy in victims of sexual aggression and their relationship with mental and physical health. 2007 (Unpublished doctoral dissertation) [Google Scholar]
- Brown EJ. Self-discourse, social anxiety, and symptomatology in rape victim-survivors: The effects of cognitive and emotional processing. 1996 (Unpublished doctoral dissertation) [Google Scholar]
- Brown NL, Wilson SR, Kao Y, Luna V, Kuo ES, Rodriguez C, Lavori PW. Correlates of sexual abuse and subsequent risk taking. Hispanic Journal of Behavioral Sciences. 2003;25(3):331–351. http://dx.doi.org/10.1177/0739986303257147. [Google Scholar]
- Brownlie EB, Jabbar A, Beitchman J, Vida R, Atkinson L. Language impairment and sexual assault of girls and women: Findings from a community sample. Journal of Abnormal Child Psychology. 2007;35(4):618–626. doi: 10.1007/s10802-007-9117-4. [DOI] [PubMed] [Google Scholar]
- Bryan CJ, McNaugton-Cassill M, Osman A, Hernandez AM. The associations of physical and sexual assault with suicide risk in nonclinical military and undergraduate samples. Suicide & Life-Threatening Behavior. 2013;43(2):223–234. doi: 10.1111/sltb.12011. [DOI] [PubMed] [Google Scholar]
- Burnam MA, Stein JA, Golding JM, Siegel JM, Sorenson SB, Forsythe AB, Telles CA. Sexual assault and mental disorders in a community population. Journal of Consulting and Clinical Psychology. 1988;56(6):843–850. doi: 10.1037//0022-006x.56.6.843. [DOI] [PubMed] [Google Scholar]
- Calhoun KS, Atkeson BM, Resick PA. A longitudinal examination of fear reactions in victims of rape. Journal of Counseling Psychology. 1982;29(6):655–661. doi: 10.1037//0022-0167.29.6.655. [DOI] [Google Scholar]
- Capitaine M, Rodgers RF, Chabrol H. Unwanted sexual experiences, depressive symptoms and disordered eating among college students. Eating Behaviors. 2011;12:86–9. doi: 10.1016/j.eatbeh.2010.11.003. [DOI] [PubMed] [Google Scholar]
- Chang B, Skinner KM, Zhou C, Kazis LE. The relationship between sexual assault, religiosity and mental health among male veterans. The International Journal of Psychiatry in Medicine. 2003;33(3):223–239. doi: 10.2190/NM3D-EWYR-4B59-DFM8. [DOI] [PubMed] [Google Scholar]
- Chang EC, Hirsch JK. Social problem solving under assault: Understanding the impact of sexual assault on the relation between social problem solving and suicidal risk in female college students. Cognitive Therapy and Research. 2014:1–11. doi: 10.1007/s10608-014-9664-2. [DOI] [Google Scholar]
- Cheasty M, Clare AW, Collins C. Child sexual abuse: A predictor of persistent depression in adult rape and sexual assault victims. Journal of Mental Health. 2002;11(1):79–84. doi: 10.1080/096382301200041489. [DOI] [Google Scholar]
- Clark CB, Perkins A, McCullumsmith CB, Islam MA, Hanover EE, Cropsey KL. Characteristics of victims of sexual abuse by gender and race in a community corrections population. Journal of Interpersonal Violence. 2012;27(9):1844–1861. doi: 10.1177/0886260511430390. [DOI] [PubMed] [Google Scholar]
- Clements CM, Ogle RL. Does acknowledgment as an assault victim impact postassault psychological symptoms and coping? Journal of Interpersonal Violence. 2009;24(10):1595–1614. doi: 10.1177/0886260509331486. [DOI] [PubMed] [Google Scholar]
- Cohen MH, Fabri M, Cai X, Shi Q, Hoover DR, Binagwaho A, Anastos K. Prevalence and predictors of posttraumatic stress disorder and depression in HIV-infected and at-risk Rwandan women. Journal of Women’s Health. 2009;18(11):1783–1791. doi: 10.1089/jwh.2009.1367. http://dx.doi.org/10.1089/jwh.2009.1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins B, Fischer S, Stojek M, Becker K. The relationship of thought suppression and recent rape to disordered eating in emerging adulthood. Journal of Adolescence. 2014;37:113–121. doi: 10.1016/j.adolescence.2013.11.002. [DOI] [PubMed] [Google Scholar]
- Conley TD, Garza MR. Gender and sequelae of child versus adult onset of sexual victimization: Body mass, binge eating, and promiscuity. Journal of Applied Social Psychology. 2011;41(11):2551–2572. doi: 10.1111/j.1559-1816.2011.00828.x. [DOI] [Google Scholar]
- Cotton DJ. The male victim of sexual assault: Patterns of occurrence, trauma reactions and adaptive reactions. 1980 (Unpublished doctoral dissertation) [Google Scholar]
- Coxell A, King M, Mezey G, Gordon D. Lifetime prevalence, characteristics, and associated problems of non-consensual sex in men: Cross sectional survey. BMJ: British Medical Journal. 1999;318:846–850. doi: 10.1136/bmj.318.7187.846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cramer RJ, McNiel DE, Holley SR, Shumway M, Boccellari A. Mental health in violent crime victims: Does sexual orientation matter? Law and Human Behavior. 2012;36(2):87–95. doi: 10.1037/h0093954. [DOI] [PubMed] [Google Scholar]
- Creamer M, Burgess P, McFarlane AC. Post-traumatic stress disorder: Findings from the Australian National Survey of Mental Health and Well-being. Psychological Medicine. 2001;31(7):1237–1247. doi: 10.1017/s0033291701004287. [DOI] [PubMed] [Google Scholar]
- Cuevas CA, Sabina C, Picard EH. Interpersonal victimization patterns and psychopathology among Latino women: Results from the SALAS study. Psychological Trauma: Theory, Research, Practice, and Policy. 2010;2(4):296–306. doi: 10.1037/a0020099. [DOI] [Google Scholar]
- Danielson CK, Amstadter AB, Dangelmaier RE, Resnick HS, Saunders BE, Kilpatrick DG. Trauma-related risk factors for substance abuse among male versus female young adults. Addictive Behaviors. 2009;34:395–399. doi: 10.1016/j.addbeh.2008.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dansky BS, Brewerton TD, Kilpatrick DG, O’Neil PM. The National Women’s Study: Relationship of victimization and posttraumatic stress disorder to bulimia nervosa. The International Journal of Eating Disorders. 1997;21(3):213–228. doi: 10.1002/(sici)1098-108x(199704)21:3<213::aid-eat2>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- Davidson JR, Hughes DC, George LK, Blazer DG. The association of sexual assault and attempted suicide within the community. Archives of General Psychiatry. 1996;53:550–555. doi: 10.1001/archpsyc.1996.01830060096013. [DOI] [PubMed] [Google Scholar]
- Deliramich AN, Gray MJ. Changes in women’s sexual behavior following sexual assault. Behavior Modification. 2008;32(5):611–621. doi: 10.1177/0145445508314642. http://dx.doi.org/10.1177/0145445508314642. [DOI] [PubMed] [Google Scholar]
- DiVasto P. Measuring the aftermath of rape. Journal of Psychosocial Nursing and Mental Health Services. 1985;23(2):33–35. doi: 10.3928/0279-3695-19850201-08. [DOI] [PubMed] [Google Scholar]
- Dorsett EM. Primary and secondary trauma in a non-clinical population. 1995 (Unpublished doctoral dissertation) [Google Scholar]
- Dubosc A, Capitaine M, Franko DL, Bui E, Brunet A, Chabrol H, Rodgers RF. Early adult sexual assault and disordered eating: The mediating role of posttraumatic stress symptoms. Journal of Traumatic Stress. 2012;25(1):50–56. doi: 10.1002/jts.21664. [DOI] [PubMed] [Google Scholar]
- Duke LA, Allen DN, Rozee PD, Bommaritto M. The sensitivity and specificity of flashbacks and nightmares to trauma. Journal of Anxiety Disorders. 2008;22:319–327. doi: 10.1016/j.janxdis.2007.03.002. [DOI] [PubMed] [Google Scholar]
- Dworkin ER, Allen NE. [Campus violence study] Unpublished raw data 2014 [Google Scholar]
- Dworkin ER, Pittenger SL, Allen NE. Disclosing sexual assault within social networks: A mixed-method investigation. American Journal of Community Psychology. 2016;57:216–228. doi: 10.1002/ajcp.12033. [DOI] [PubMed] [Google Scholar]
- Dyck KG. The relationship between attributional dimensions and symptomatology in women reporting sexual assault. 1995 (Unpublished doctoral dissertation) [Google Scholar]
- Eap S. Predictors of risky sexual behavior in emerging adulthood: An examination of sexual trauma and depression trajectories. 2008 (Unpublished doctoral dissertation) [Google Scholar]
- Edwards VJ. The risk of sexual assault and mental health problems in adult daughters of battered women. 1998 (Unpublished doctoral dissertation) [Google Scholar]
- Eggers LW. Attitudes toward rape and recovery from sexual assault. 1985 (Unpublished doctoral dissertation) [Google Scholar]
- Ehring T, Quack D. Emotion regulation difficulties in trauma survivors: The role of trauma type and PTSD symptom severity. Behavior Therapy. 2010;41:587–598. doi: 10.1016/j.beth.2010.04.004. [DOI] [PubMed] [Google Scholar]
- Elklit A, Hyland P, Shevlin M. Evidence of symptom profiles consistent with posttraumatic stress disorder and complex posttraumatic stress disorder in different trauma samples. European Journal of Psychotraumatology. 2014;5:1–10. doi: 10.3402/ejpt.v5.24221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott DM, Mok DS, Briere J. Adult sexual assault: Prevalence, symptomatology, and sex differences in the general population. Journal of Traumatic Stress. 2004;17(3):203–211. doi: 10.1023/B:JOTS.0000029263.11104.23. [DOI] [PubMed] [Google Scholar]
- Ellis EM, Atkeson BM, Calhoun KS. An assessment of long-term reaction to rape. Journal of Abnormal Psychology. 1981;90(3):263–266. doi: 10.1037//0021-843x.90.3.263. [DOI] [PubMed] [Google Scholar]
- Elwood LS. The role of cognitive vulnerabilities in the maintenance of posttraumatic stress symptoms: A prospective examination of a diathesis-stress model. 2008 doi: 10.1016/j.jbtep.2009.07.005. (Unpublished doctoral dissertation) [DOI] [PubMed] [Google Scholar]
- Evans-Campbell T, Lindhorst T, Huang B, Walters KL. Interpersonal violence in the lives of urban American Indian and Alaska Native women: Implications for health, mental health, and help-seeking. American Journal of Public Health. 2006;96(8):1416–1422. doi: 10.2105/AJPH.2004.054213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fanslow J, Robinson E. Violence against women in New Zealand: Prevalence and health consequences. The New Zealand Medical Journal. 2004;117(1206):1–12. [PubMed] [Google Scholar]
- Faravelli C, Giugni A, Salvatori S, Ricca V. Psychopathology after rape. The American Journal of Psychiatry. 2004;161(8):1483–1485. doi: 10.1176/appi.ajp.161.8.1483. [DOI] [PubMed] [Google Scholar]
- Filipas HH, Ullman SE. Child sexual abuse, coping responses, self-blame, posttraumatic stress disorder, and adult sexual revictimization. Journal of Interpersonal Violence. 2006;21(5):652–672. doi: 10.1177/0886260506286879. [DOI] [PubMed] [Google Scholar]
- Forman-Hoffman VL, Mengeling M, Booth BM, Torner J, Sadler AG. Eating disorders, post-traumatic stress, and sexual trauma in women veterans. Military Medicine. 2012;177(10):1161–1168. doi: 10.7205/milmed-d-12-00041. [DOI] [PubMed] [Google Scholar]
- Frank E, Anderson BP. Psychiatric disorders in rape victims: Past history and current symptomatology. Comprehensive Psychiatry. 1987;28(1):77–82. doi: 10.1016/0010-440x(87)90047-2. [DOI] [PubMed] [Google Scholar]
- Frazier PA, Schauben LJ. Stressful life events and psychological adjustment among female college students. Measurement and Evaluation in Counseling and Development. 1994;27(1):280–292. [Google Scholar]
- Frazier PA, Anders S, Perera S, Tomich P, Tennen H, Park C, Tashiro T. Traumatic events among undergraduate students: Prevalence and associated symptoms. Journal of Counseling Psychology. 2009;56(3):450–460. doi: 10.1037/a0016412. [DOI] [Google Scholar]
- Frazier PA, Steward J, Mortensen H. Perceived control and adjustment to trauma: A comparison across events. Journal of Social and Clinical Psychology. 2004;23(3):303–324. [Google Scholar]
- Freedy JR, Magruder KM, Mainous AG, Frueh BC, Geesey ME, Carnemolla M. Gender differences in traumatic event exposure and mental health among veteran primary care patients. Military Medicine. 2010;175(10):750–758. doi: 10.7205/milmed-d-10-00123. [DOI] [PubMed] [Google Scholar]
- Freedy JR, Magruder KM, Zoller JS, Hueston WJ, Carek PJ, Brock CD. Traumatic events and mental health in civilian primary care: Implications for training and practice. Family Medicine. 2010;42(3):185–192. [PubMed] [Google Scholar]
- Fusé T. Psychophysiological responses to sexual assault related imagery in sexual assault survivors with and without a history of tonic immobility. 2007 (Unpublished doctoral dissertation) [Google Scholar]
- Gidycz CA, Koss MP. Predictors of long-term sexual assault trauma among a national sample of victimized college women. Violence and Victims. 1991;6(3):175–190. [PubMed] [Google Scholar]
- Gidycz CA, Coble CN, Latham L, Layman MJ. Sexual assault experience in adulthood and prior victimization experiences: A prospective analysis. Psychology of Women Quarterly. 1993;17:151–168. [Google Scholar]
- Gidycz CA, Orchowski LM, King CR, Rich CL. Sexual victimization and health-risk behaviors: A prospective analysis of college women. Journal of Interpersonal Violence. 2008;23(6):744–763. doi: 10.1177/0886260507313944. [DOI] [PubMed] [Google Scholar]
- Gilboa-Schechtman E, Foa EB. Patterns of recovery from trauma: The use of intraindividual analysis. Journal of Abnormal Psychology. 2001;110(3):392–400. doi: 10.1037//0021-843X.110.3.392. [DOI] [PubMed] [Google Scholar]
- Goldmann E, Aiello A, Uddin M, Delva J, Koenen K, Gant LM, Galea S. Pervasive exposure to violence and posttraumatic stress disorder in a predominantly African American urban community: The Detroit neighborhood health study. Journal of Traumatic Stress. 2011;24(6):747–751. doi: 10.1002/jts. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutner CA, Rizvi SL, Monson CM, Resick PA. Changes in coping strategies, relationship to the perpetrator, and posttraumatic distress in female crime victims. Journal of Traumatic Stress. 2006;19(6):813–823. doi: 10.1002/jts. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagen KL. The impact of childhood maltreatment experiences, adult revictimization, history of traumatization symptoms, and racism on the psychological well-being of African-American women. 1998 (Unpublished doctoral dissertation) [Google Scholar]
- Halligan SL, Michael T, Clark DM, Ehlers A. Posttraumatic stress disorder following assault: The role of cognitive processing, trauma memory, and appraisals. Journal of Consulting and Clinical Psychology. 2003;71(3):419–431. doi: 10.1037/0022-006X.71.3.419. [DOI] [PubMed] [Google Scholar]
- Hapke U, Schumann A, Rumpf HJ, John U, Meyer C. Post-traumatic stress disorder: The role of trauma, pre-existing psychiatric disorders, and gender. European Archives of Psychiatry and Clinical Neuroscience. 2006;256:299–306. doi: 10.1007/s00406-006-0654-6. [DOI] [PubMed] [Google Scholar]
- Harris HN, Valentiner DP. World assumptions, sexual assault, depression, and fearful attitudes toward relationships. Journal of Interpersonal Violence. 2002;17(3):286–305. doi: 10.1177/0886260502017003004. [DOI] [Google Scholar]
- Heidt JM, Marx BP, Gold SD. Sexual revictimization among sexual minorities: A preliminary study. Journal of Traumatic Stress. 2005;18(5):533–540. doi: 10.1002/jts.20061. [DOI] [PubMed] [Google Scholar]
- Hidaka Y, Operario D, Tsuji H, Takenaka M, Kimura H, Kamakura M, Ichikawa S. Prevalence of sexual victimization and correlates of forced sex in Japanese men who have sex with men. PLoS ONE. 2014;9(5):1–6. doi: 10.1371/journal.pone.0095675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hossain M, Zimmerman C, Abas M, Light M, Watts C. The relationship of trauma to mental disorders among trafficked and sexually exploited girls and women. American Journal of Public Health. 2010;100(12):2442–2449. doi: 10.2105/AJPH.2009.173229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson K, Scott J, Rughita B, Kisielewski M, Asher J, Ong R, Lawry L. Association of sexual violence and human rights violations with physical and mental health in territories of the Eastern Democratic Republic of the Congo. JAMA: The Journal of the American Medical Association. 2010;304(5):553–562. doi: 10.1001/jama.2010.1086. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Benotsch E, Rompa D, Gore-Felton C, Austin J, Luke W, Simpson D. Unwanted sexual experiences and sexual risks in gay and bisexual men: Associations among revictimization, substance use, and psychiatric symptoms. Journal of Sex Research. 2001;38(1):1–9. [Google Scholar]
- Kaltman S, Krupnick J, Stockton P, Hooper L, Green BL. Psychological impact of types of sexual trauma among college women. Journal of Traumatic Stress. 2005;18(5):547–555. doi: 10.1002/jts.20063. [DOI] [PubMed] [Google Scholar]
- Kaminer D, Grimsrud A, Myer L, Stein DJ, Williams DR. Risk for post-traumatic stress disorder associated with different forms of interpersonal violence in South Africa. Social Science & Medicine (1982) 2008;67(10):1589–1595. doi: 10.1016/j.socscimed.2008.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaysen D, Atkins DC, Moore SA, Lindgren KP, Dillworth T, Simpson T. Alcohol use, problems, and the course of posttraumatic stress disorder: A prospective study of female crime victims. Journal of Dual Diagnosis. 2011;7(4):262–279. doi: 10.1080/15504263.2011.620449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keller A, Lhewa D, Rosenfeld B, Sachs E, Aladjem A, Cohen L, Porterfield K. Traumatic experiences and psychological distress in an urban refugee population seeking treatment services. The Journal of Nervous and Mental Disease. 2006;194(3):188–194. doi: 10.1097/01.nmd.0000202494.75723.83. [DOI] [PubMed] [Google Scholar]
- Kelley EL. Women’s conceptualization of their unwanted sexual experiences: A focus on labeling, time since assault, psychological functioning and risky sexual behavior. 2009 (Unpublished bachelor’s thesis) [Google Scholar]
- Kelley LP, Weathers FW, McDevitt-Murphy ME, Eakin DE, Flood AM. A comparison of PTSD symptom patterns in three types of civilian trauma. Journal of Traumatic Stress. 2009;22(3):227–235. doi: 10.1002/jts. [DOI] [PubMed] [Google Scholar]
- Kendall-Tackett K, Cong Z, Hale TW. Depression, sleep quality, and maternal well-being in postpartum women with a history of sexual assault: A comparison of breastfeeding, mixed-feeding, and formula-feeding mothers. Breastfeeding Medicine. 2013;8(1):16–22. doi: 10.1089/bfm.2012.0024. [DOI] [PubMed] [Google Scholar]
- Kennedy AC, Bybee D, Greeson MR. Examining cumulative victimization, community violence exposure, and stigma as contributors to PTSD symptoms among high-risk young women. The American Journal of Orthopsychiatry. 2014;84(3):284–294. doi: 10.1037/ort0000001. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB, Breslau N. Epidemiological risk factors for trauma and PTSD. In: Yehuda R, editor. Risk factors for posttraumatic stress disorder. Washington, D C: American Psychiatric Association; 1999. pp. 23–59. [Google Scholar]
- Kievit LW. Coping with rape: The relationship between context, resources, and outcome. 1999 (Unpublished doctoral dissertation) [Google Scholar]
- Kilpatrick DG, Edmunds CN, Seymour AK. Rape in America: A report to the nation. Charleston, SC: Crime Victims Research and Treatment Center; 1992. [Google Scholar]
- Kilpatrick DG, Resick PA, Veronen LJ. Effects of a rape experience: A longitudinal study. Journal of Social Issues. 1981;37(4):105–122. http://dx.doi.org/10.1111/j.1540-4560.1981.tb01073.x. [Google Scholar]
- Kilpatrick DG, Resnick HS, Ruggiero KJ, Conoscenti LM, McCauley J. Drug-facilitated, incapacitated, and forcible rape: A national study. Charleston, S C: 2007. [Google Scholar]
- Kimerling R, Alvarez J, Pavao J, Kaminski A, Baumrind N. Epidemiology and consequences of women’s revictimization. Women’s Health Issues. 2007;17:101–106. doi: 10.1016/j.whi.2006.12.002. [DOI] [PubMed] [Google Scholar]
- King C. The relationship between health risk behaviors and sexual assault: A prospective analysis. 2003 (Unpublished doctoral dissertation) [Google Scholar]
- Kunst MJJ, Winkel FW, Bogaerts S. Posttraumatic anger, recalled peritraumatic emotions, and PTSD in victims of violent crime. Journal of Interpersonal Violence. 2011;26(17):3561–3579. doi: 10.1177/0886260511403753. [DOI] [PubMed] [Google Scholar]
- Lancaster SL, Melka SE, Rodriguez BF, Bryant AR. PTSD symptom patterns following traumatic and nontraumatic events. Journal of Aggression, Maltreatment & Trauma. 2014;23:414–429. [Google Scholar]
- Lang AJ, Rodgers CS, Laffaye C, Satz LE, Dresselhaus TR, Stein MB. Sexual trauma, posttraumatic stress disorder, and health behavior. Behavioral Medicine. 2003;28:150–158. doi: 10.1080/08964280309596053. [DOI] [PubMed] [Google Scholar]
- Larimer ME, Lydum AR, Anderson BK, Turner AP. Male and female recipients of unwanted sexual contact in a college student sample: Prevalence rates, alcohol use, and depression symptoms. Sex Roles. 1999;40(3):295–308. [Google Scholar]
- Laura RK. Response to sexual trauma in relation to event centrality and objectified view of self. 2012 (Unpublished doctoral dissertation) [Google Scholar]
- Laws A, Golding JM. Sexual assault history and eating disorder symptoms among white, Hispanic, and African-American women and men. American Journal of Public Health. 1996;86(4):579–582. doi: 10.2105/ajph.86.4.579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Layman MJ, Gidycz Ca, Lynn SJ. Unacknowledged versus acknowledged rape victims: Situational factors and posttraumatic stress. Journal of Abnormal Psychology. 1996;105(1):124–131. doi: 10.1037//0021-843x.105.1.124. [DOI] [PubMed] [Google Scholar]
- Lexington JM. An examination of the relationship between tonic immobility and the psychophysiology, behaviors, and perceptions in response to a hypothetical date rape scenario. 2006 (Unpublished doctoral dissertation) [Google Scholar]
- Lindquist CH, Barrick K, Krebs C, Crosby CM, Lockard AJ, Sanders-Phillips K. The context and consequences of sexual assault among undergraduate women at Historically Black Colleges and Universities (HBCUs) Journal of Interpersonal Violence. 2013;28(12):2437–2461. doi: 10.1177/0886260513479032. [DOI] [PubMed] [Google Scholar]
- Littleton HL, Grills-Taquechel AE, Buck KS, Rosman L, Dodd JC. Health risk behavior and sexual assault among ethnically diverse women. Psychology of Women Quarterly. 2012;37(1):7–21. doi: 10.1177/0361684312451842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Littleton HL, Grills AE, Drum KB. Predicting risky sexual behavior in emerging adulthood: Examination of a moderated mediation model among child sexual abuse and adult sexual assault victims. Violence and Victims. 2014;29(6):981–998. doi: 10.1891/0886-6708.vv-d-13-00067. [DOI] [PubMed] [Google Scholar]
- Logie CH, Alaggia R, Rwigema MJ. A social ecological approach to understanding correlates of lifetime sexual assault among sexual minority women in Toronto, Canada: Results from a cross-sectional internet-based survey. Health Education Research. 2014;29(4):671–682. doi: 10.1093/her/cyt119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loshek EA. Predictors of sexual assertiveness in women: A comparative study of women during different life-stages. 2014 (Unpublished doctoral dissertation) [Google Scholar]
- Lown EA, Vega WA. Alcohol abuse or dependence among Mexican American women who report violence. Alcoholism: Clinical and Experimental Research. 2001;25(10) [PubMed] [Google Scholar]
- Lueger-Schuster B, Glück TM, Tran US, Zeilinger EL. Sexual violence by occupational forces during and after World War II: Influence of experiencing and witnessing of sexual violence on current mental health in a sample of elderly Austrians. International Psychogeriatrics. 2012;24(8):1354–1358. doi: 10.1017/S104161021200021X. [DOI] [PubMed] [Google Scholar]
- Martin SL, Rentz ED, Chan RL, Givens J, Sanford CP, Kupper LL, Macy RJ. Physical and sexual violence among North Carolina women: Associations with physical health, mental health, and functional impairment. Women’s Health Issues. 2008;18:130–140. doi: 10.1016/j.whi.2007.12.008. [DOI] [PubMed] [Google Scholar]
- Martinson AA. The impact of sexual trauma and posttraumatic stress disorder symptom severity on psychological and physiological reactivity to an intimacy induction task. 2013 (Unpublished doctoral dissertation) [Google Scholar]
- Masho SW, Ahmed G. Age at sexual assault and posttraumatic stress disorder among women: prevalence, correlates, and implications for prevention. Journal of Women’s Health. 2007;16(2):262–271. doi: 10.1089/jwh.2006.M076. [DOI] [PubMed] [Google Scholar]
- Matich-Maroney J. Sexual exploitation and its aftereffects in developmentally disabled adults. 1996 (Unpublished doctoral dissertation) [Google Scholar]
- McAuslan P. After sexual assault: The relationship between women’s disclosure, the reactions of others, and health. 1998 (Unpublished doctoral dissertation) [Google Scholar]
- McCutcheon VV, Sartor CE, Pommer NE, Bucholz KK, Nelson EC, Madden PAF, Heath AC. Age at trauma exposure and PTSD risk in young adult women. Journal of Traumatic Stress. 2010;23(6):811–814. doi: 10.1002/jts. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messman-Moore TL, Brown AL, Koelsch LE. Posttraumatic symptoms and self-dysfunction as consequences and predictors of sexual revictimization. Journal of Traumatic Stress. 2005;18(3):253–261. doi: 10.1002/jts.20023. [DOI] [PubMed] [Google Scholar]
- Messman-Moore TL, Coates AA, Gaffey KJ, Johnson CF. Sexuality, substance use, and susceptibility to victimization: Risk for rape and sexual coercion in a prospective study of college women. Journal of Interpersonal Violence. 2008;23(12):1730–1746. doi: 10.1177/0886260508314336. [DOI] [PubMed] [Google Scholar]
- Messman-Moore TL, Long PJ, Siegfried NJ. The revictimization of child sexual abuse survivors: An examination of the adjustment of college women with child sexual abuse, adult sexual assault, and adult physical abuse. Child Maltreatment. 2000;5(1):18–27. doi: 10.1177/1077559500005001003. [DOI] [PubMed] [Google Scholar]
- Meyerson LA. A prospective analysis of sexual assault and alcohol use among college women. 2002 (Unpublished doctoral dissertation) [Google Scholar]
- Miller BC, Monson BH, Norton MC. The effects of forced sexual intercourse on white female adolescents. Child Abuse & Neglect. 1995;19(10):1289–1301. doi: 10.1016/0145-2134(95)00081-i. [DOI] [PubMed] [Google Scholar]
- Moss M, Frank E, Anderson BP. The effects of marital status and partner support on rape trauma. American Journal of Orthopsychiatry. 1990;60(3):379–391. doi: 10.1037/h0079179. [DOI] [PubMed] [Google Scholar]
- Nayak MB, Lown EA, Bond JC, Greenfield TK. Lifetime victimization and past year alcohol use in a U.S. population sample of men and women drinkers. Drug and Alcohol Dependence. 2012;123(1):213–219. doi: 10.1016/j.drugalcdep.2011.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norris FH. Epidemiology of trauma: Frequency and impact of different potentially traumatic events on different demographic groups. Journal of Consulting and Clinical Psychology. 1992;60(3):409–418. doi: 10.1037//0022-006x.60.3.409. [DOI] [PubMed] [Google Scholar]
- Nosek MA, Hughes RB, Taylor HB. Disability, psychosocial, and demographic characteristics of abused women with physical disabilities. Violence Against Women. 2006;12(9):838–850. doi: 10.1177/1077801206292671. [DOI] [PubMed] [Google Scholar]
- Orchowski LM. Disclosure of sexual victimization: A prospective study of social reactions and subsequent adjustment. 2009 (Unpublished doctoral dissertation) [Google Scholar]
- Orth U, Maercker A. Do trials of perpetrators retraumatize crime victims? Journal of Interpersonal Violence. 2004;19(2):212–227. doi: 10.1177/0886260503260326. [DOI] [PubMed] [Google Scholar]
- Orth U, Cahill SP, Foa EB, Maercker A. Anger and posttraumatic stress disorder symptoms in crime victims: A longitudinal analysis. Journal of Consulting and Clinical Psychology. 2008;76(2):208–218. doi: 10.1037/0022-006X.76.2.208. [DOI] [PubMed] [Google Scholar]
- Owens GP, Chard KM. PTSD severity and cognitive reactions to trauma among a college sample: An exploratory study. Journal of Aggression, Maltreatment & Trauma. 2006;13(2):23–36. doi: 10.1300/J146v13n02. [DOI] [Google Scholar]
- Palmer M. Evidence for persistent hypervigilance for sexual assault survivors. 2002 (Unpublished doctoral dissertation) [Google Scholar]
- Parks KA, Hsieh Y, Taggart C, Bradizza CM. A longitudinal analysis of drinking and victimization in college women: Is there a reciprocal relationship? Psychology of Addictive Behaviors. 2014;28(4):943–951. doi: 10.1037/a0036283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pepper SE. Self blame in sexual assault survivors and attributions to other sexual assault survivors. 2009 (Unpublished master’s thesis) [Google Scholar]
- Phillips SR. The development of disordered eating among female undergraduates: A test of objectification theory. 2011 (Unpublished doctoral dissertation) [Google Scholar]
- Plichta SB, Falik M. Prevalence of violence and its implications for women’s health. Women’s Health Issues. 2001;11(3):244–258. doi: 10.1016/S1049-3867(01)00085-8. [DOI] [PubMed] [Google Scholar]
- Preti A, Incani E, Camboni MV, Petretto DR, Masala C. Sexual abuse and eating disorder symptoms: The mediator role of bodily dissatisfaction. Comprehensive Psychiatry. 2006;47(6):475–481. doi: 10.1016/j.comppsych.2006.03.004. [DOI] [PubMed] [Google Scholar]
- Price M, Kearns M, Houry D, Rothbaum BO. Emergency department predictors of posttraumatic stress reduction for trauma-exposed individuals with and without an early intervention. Journal of Consulting and Clinical Psychology. 2014;82(2):336–341. doi: 10.1037/a0035537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prosser VL. The impact of sexual assault, sexual abuse, and physical violence on women. 1997 (Unpublished master’s thesis) [Google Scholar]
- Raja S. Secondary victimization among female veterans who have experienced sexual assault. 1999 (Unpublished doctoral dissertation) [Google Scholar]
- Ratner PA, Johnson JL, Shoveller JA, Chan K, Martin SL, Schilder AJ, Hogg RS. Non-consensual sex experienced by men who have sex with men: prevalence and association with mental health. Patient Education and Counseling. 2003;49(1):67–74. doi: 10.1016/s0738-3991(02)00055-1. [DOI] [PubMed] [Google Scholar]
- Read JP, Colder CR, Merrill JE, Ouimette P, White J, Swartout A. Trauma and posttraumatic stress symptoms predict alcohol and other drug consequence trajectories in the first year of college. Journal of Consulting and Clinical Psychology. 2012;80(3):426–439. doi: 10.1037/a0028210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed E, Raj A, Falbo G, Caminha F, Decker MR, Kaliel DC, Silverman JG. The prevalence of violence and relation to depression and illicit drug use among incarcerated women in Recife, Brazil. International Journal of Law and Psychiatry. 2009;32:323–328. doi: 10.1016/j.ijlp.2009.06.006. [DOI] [PubMed] [Google Scholar]
- Resick PA. Reactions of female and male victims of rape or robbery. U.S Department of Justice, National Institute of Justice; 1988. [Google Scholar]
- Resick PA. Cognitive processes in PTSD-Etiology and treatment. 1991 Unpublished raw data. [Google Scholar]
- Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, Best CL. Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. Journal of Consulting and Clinical Psychology. 1993;61(6):984–991. doi: 10.1037//0022-006x.61.6.984. [DOI] [PubMed] [Google Scholar]
- Rice T. Predicting sexually victimized women’s mental health and substance use help-seeking behavior. 2014 (Unpublished doctoral dissertation) [Google Scholar]
- Risser H, Hetzel-Riggin M, Thomsen C, McCanne T. PTSD as a mediator of sexual revictimization: The role of reexperiencing, avoidance, and arousal symptoms. Journal of Traumatic Stress. 2006;19(5):687–698. doi: 10.1002/jts.20156. [DOI] [PubMed] [Google Scholar]
- Rizvi SL, Kaysen D, Gutner CA, Griffin MG, Resick PA. Beyond fear: The role of peritraumatic responses in posttraumatic stress among female crime victims. Journal of Interpersonal Violence. 2008;23(6):853–868. doi: 10.1177/0886260508314851. [DOI] [PubMed] [Google Scholar]
- Roberts B, Ocaka KF, Browne J, Oyok T, Sondorp E. Factors associated with post-traumatic stress disorder and depression amongst internally displaced persons in northern Uganda. BMC Psychiatry. 2008;8:38–47. doi: 10.1186/1471-244X-8-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sachs-Ericsson N, Kendall-Tackett KA, Sheffler J, Arce D, Rushing NC, Corsentino E. The influence of prior rape on the psychological and physical health functioning of older adults. Aging & Mental Health. 2014:1–14. doi: 10.1080/13607863.2014.884538. [DOI] [PubMed] [Google Scholar]
- Sadler AG, Mengeling MA, Fraley SS, Torner JC, Booth BM. Correlates of sexual functioning in women veterans: Mental health, gynecologic health, health status, and sexual assault history. International Journal of Sexual Health. 2012;24(1):60–77. [Google Scholar]
- Sandberg DA, Matorin AI, Lynn SJ. Dissociation, posttraumatic symptomatology, and sexual revictimization: A prospective examination of mediator and moderator effects. Journal of Traumatic Stress. 1999;12(1):127–138. doi: 10.1023/A:1024702501224. [DOI] [PubMed] [Google Scholar]
- Santaularia J, Johnson M, Hart L, Haskett L, Welsh E, Faseru B. Relationships between sexual violence and chronic disease: A cross-sectional study. BMC Public Health. 2014;14(1):868–882. doi: 10.1186/1471-2458-14-1286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawtell CS. The victim-perpetrator relationship in the crime of rape: Victims’ mental well-being. 2008 (Unpublished doctoral dissertation) [Google Scholar]
- Saxon AJ, Davis TM, Sloan KL, McKnight KM, McFall ME, Kivlahan DR. Trauma, symptoms of posttraumatic stress disorder, and associated problems among incarcerated veterans. Psychiatric Services. 2001;52(7):959–964. doi: 10.1176/appi.ps.52.7.959. [DOI] [PubMed] [Google Scholar]
- Schry AR, White SW. Social behaviors and psychological health study. 2013 Unpublished raw data. [Google Scholar]
- Schumm JA, Briggs-Phillips M, Hobfoll SE. Cumulative interpersonal traumas and social support as risk and resiliency factors in predicting PTSD and depression among inner-city women. Journal of Traumatic Stress. 2006;19(6):825–836. doi: 10.1002/jts. [DOI] [PubMed] [Google Scholar]
- Shabalala N, Jasson A. PTSD symptoms in intellectually disabled victims of sexual assault. South African Journal of Psychology. 2011;41(4):424–436. doi: 10.1177/008124631104100403. [DOI] [Google Scholar]
- Shakespeare-Finch J, Armstrong D. Trauma type and posttrauma outcomes: Differences between survivors of motor vehicle accidents, sexual assault, and bereavement. Journal of Loss & Trauma. 2010;15(2):69–82. [Google Scholar]
- Smith CP, Freyd JJ. Dangerous safe havens: Institutional betrayal exacerbates sexual trauma. Journal of Traumatic Stress. 2013;26:119–124. doi: 10.1002/jts. [DOI] [PubMed] [Google Scholar]
- Sorenson SB, Golding JM. Depressive sequelae of recent criminal victimization. Journal of Traumatic Stress. 1990;3(3):337–350. [Google Scholar]
- Stein MB, Walker JR, Forde DR. Gender differences in susceptibility to posttraumatic stress disorder. Behaviour Research and Therapy. 2000;38:619–628. doi: 10.1016/s0005-7967(99)00098-4. [DOI] [PubMed] [Google Scholar]
- Stepakoff S. Effects of sexual victimization on suicidal ideation and behavior in U.S. college women. Suicide and Life-Threatening Behavior. 1998;28(1):107–126. [PubMed] [Google Scholar]
- Temple JR, Weston R, Rodriguez BF, Marshall LL. Differing effects of partner and nonpartner sexual assault on women’s mental health. Violence Against Women. 2007;13(3):285–297. doi: 10.1177/1077801206297437. [DOI] [PubMed] [Google Scholar]
- Testa M, Livingston JA, Hoffman JH. Does sexual victimization predict subsequent alcohol consumption? A prospective study among a community sample of women. Addictive Behaviors. 2007;32(12):2926–2939. doi: 10.1016/j.addbeh.2007.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teutscher JM. Victimization history and its effect on women’s use of rape avoidance behaviors. 2014 (Unpublished master’s thesis) [Google Scholar]
- Thelen MH, Sherman MD, Borst TS. Fear of intimacy and attachment among rape survivors. Behavior Modification. 1998;22(1):108–116. doi: 10.1177/01454455980221007. http://dx.doi.org/10.1177/01454455980221007. [DOI] [PubMed] [Google Scholar]
- Thompson KM, Crosby RD, Wonderlich S, Mitchell JE, Redlin J, Demuth G, Haseltine B. Psychopathology and sexual trauma in childhood and adulthood. Journal of Traumatic Stress. 2003;16(1):35–38. doi: 10.1023/A:1022007327077. [DOI] [PubMed] [Google Scholar]
- Thompson MP, Kingree JB. Sexual victimization, negative cognitions, and adjustment in college women. American Journal of Health Behavior. 2010;34(1):54–59. doi: 10.5993/ajhb.34.1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turchik JA. Sexual victimization among male college students: Assault severity, sexual functioning, and health risk behaviors. Psychology of Men & Masculinity. 2011;13:243–255. doi: 10.1037/a0024605. [DOI] [Google Scholar]
- Turchik JA, Hassija CM. Female sexual victimization among college students: Assault severity, health risk behaviors, and sexual functioning. Journal of Interpersonal Violence. 2014;29(13):2439–2457. doi: 10.1177/0886260513520230. [DOI] [PubMed] [Google Scholar]
- United States Department of Justice. Bureau of Justice Statistics. Survey of Inmates in State and Federal Correctional Facilities, 2004. Ann Arbor, MI: Inter-university Consortium for Political and Social Research; 2004. ICPSR04572-v1. [distributor] [DOI] [Google Scholar]
- Vaile Wright C, Collinsworth LL, Fitzgerald LF. Why did this happen to me? Cognitive schema disruption and posttraumatic stress disorder in victims of sexual trauma. Journal of Interpersonal Violence. 2010;25(10):1801–1814. doi: 10.1177/0886260509354500. [DOI] [PubMed] [Google Scholar]
- Varma D, Chandra PS, Thomas T, Carey MP. Intimate partner violence and sexual coercion among pregnant women in India: Relationship with depression and post-traumatic stress disorder. Journal of Affective Disorders. 2007;102(1–3):227–235. doi: 10.1016/j.jad.2006.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veronen LJ, Kilpatrick DG. Self-reported fears of rape victims: A preliminary investigation. Behavior Modification. 1980;4(3):383–396. doi: 10.1177/014544558043007. [DOI] [Google Scholar]
- Walker EA, Gelfand AN, Gelfand MD, Koss MP, Katon WJ. Medical and psychiatric symptoms in female gastroenterology clinic patients with histories of sexual victimization. General Hospital Psychiatry. 1995;17(2):85–92. doi: 10.1016/0163-8343(94)00058-l. [DOI] [PubMed] [Google Scholar]
- Walker J, Archer J, Davies M. Effects of male rape on psychological functioning. British Journal of Clinical Psychology. 2005;44:445–451. doi: 10.1348/014466505X52750. [DOI] [PubMed] [Google Scholar]
- Wang B, Li X, Stanton B, Fang X, Yang H, Zhao R, Hong Y. Sexual coercion, HIV-related risk, and mental health among female sex workers in China. Health Care for Women International. 2007;28(8):745–762. doi: 10.1080/07399330701465226. [DOI] [PubMed] [Google Scholar]
- Ward JA. Association of traumatic event, chronicity, and developmental level to posttraumatic symptomology. 1998 (Unpublished doctoral dissertation) [Google Scholar]
- Wasco SM. An ecological study of repeated sexual victimization among college women. 2004 (Unpublished doctoral dissertation) [Google Scholar]
- Weaver TL, Griffin MG, Mitchell ER. Symptoms of posttraumatic stress, depression, and body image distress in female victims of physical and sexual assault: Exploring integrated responses. Health Care For Women International. 2014;35:458–475. doi: 10.1080/07399332.2013.858162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb CL. Social support and the psychological outcome of rape. 1981 (Unpublished doctoral dissertation) [Google Scholar]
- Wenzel SL, Leake BD, Gelberg L. Health of homeless women with recent experience of rape. Journal of General Internal Medicine. 2000;15(4):265–268. doi: 10.1111/j.1525-1497.2000.04269.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winfield I, George LK, Swartz M, Blazer DG. Sexual assault and psychiatric disorders among a community sample of women. American Journal of Psychiatry. 1990;147(3):335–341. doi: 10.1176/ajp.147.3.335. [DOI] [PubMed] [Google Scholar]
- Wingood GM, DiClemente RJ. Rape among African American Women: Sexual, psychological, and social correlates predisposing survivors to risk of STD/HIV. Journal of Women’s Health. 1998;7(1):77–84. doi: 10.1089/jwh.1998.7.77. [DOI] [PubMed] [Google Scholar]
- Wirtz PW, Harrell AV. Assaultive versus nonassaultive victimization: A profile analysis of psychological response. Journal of Interpersonal Violence. 1987;2(3):264–277. http://dx.doi.org/10.1177/088626087002003003. [Google Scholar]
- Wolf EJ, Miller MW, Kilpatrick D, Resnick HS, Badour CL, Marx BP, Friedman MJ. ICD-11 complex PTSD in U.S. national and veteran samples: Prevalence and structural associations with PTSD. Clinical Psychological Science. 2014:1–15. doi: 10.1177/2167702614545480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wonderlich SA, Crosby RD. Eating disturbance and sexual trauma in childhood and adulthood. International Journal of Eating Disorders. 2001;30:401–412. doi: 10.1002/eat.1101. [DOI] [PubMed] [Google Scholar]
- Wright LL. Negative sexual experiences and rape: Understanding the relationship between adult and childhood Sexual victimization and somatic complaints, psychological factors, and self-rated health in college women. 2014 (Unpublished doctoral dissertation) [Google Scholar]
- Xu Y, Olfson M, Villegas L, Okuda M, Wang S, Liu S, Blanco C. A characterization of adult victims of sexual violence: Results from the National Epidemiological Survey for Alcohol and Related Conditions. Psychiatry. 2013;76(3):223–240. doi: 10.1521/psyc.2013.76.3.223. [DOI] [PubMed] [Google Scholar]
- Zayed MH. Effects of adult sexual assault types and tactics on cognitive appraisals and mental health symptoms. 2008 (Unpublished doctoral dissertation) [Google Scholar]
- Zinzow HM, Grubaugh AL, Frueh BC, Magruder KM. Sexual assault, mental health, and service use among male and female veterans seen in Veterans Affairs primary care clinics: A multi-site study. Psychiatry Research. 2008;159:226–236. doi: 10.1016/j.psychres.2007.04.008. [DOI] [PubMed] [Google Scholar]
- Zinzow HM, Resnick HS, McCauley JL, Amstadter AB, Ruggiero KJ, Kilpatrick DG. Prevalence and risk of psychiatric disorders as a function of variant rape histories: Results from a National Survey of Women. Social Psychiatry and Psychiatric Epidemiology. 2012;47(6):893–902. doi: 10.1007/s00127-011-0397-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zlotnick C, Johnson J, Kohn R, Vicente B, Rioseco P, Saldivia S. Epidemiology of trauma, post-traumatic stress disorder (PTSD) and co-morbid disorders in Chile. Psychological Medicine. 2006;36:1523–1533. doi: 10.1017/S0033291706008282. [DOI] [PubMed] [Google Scholar]
- Zweig JM, Barber BL, Eccles JS. Sexual coercion and well-being in young adulthood comparisons by gender and college status. Journal of Interpersonal Violence. 1997;12(2):291–308. [Google Scholar]
- Zweig JM, Crockett LJ, Sayer A, Vicary JR. A longitudinal examination of the consequences of sexual victimization for rural young adult women. Journal of Sex Research. 1999;36(4):396–409. [Google Scholar]
- Acierno R, Resnick HS, Kilpatrick DG. Health impact of interpersonal violence 1: Prevalence rates, case identification, and risk factors for sexual assault, physical assault, and domestic violence in men and women. Behavioral Medicine. 1997;23(2):53–64. doi: 10.1080/08964289709596729. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual (DSM-III) Washington, DC: Author; 1980. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th. Washington, DC: Author; 2013. [Google Scholar]
- Arata CM. Repeated sexual victimization and mental disorders in women. Journal of Child Sexual Abuse. 1999;7(3):1–17. doi: 10.1300/J070v07n03. [DOI] [Google Scholar]
- Atkeson BM, Calhoun KS, Resick PA, Ellis EM. Victims of rape: Repeated assessment of depressive symptoms. Journal of Consulting and Clinical Psychology. 1982;50:96–102. doi: 10.1037//0022-006x.50.1.96. [DOI] [PubMed] [Google Scholar]
- Black MC, Basile KC, Breiding MJ, Smith SG, Walters ML, Merrick MT, Stevens MR. National intimate partner and sexual violence survey(NISVS): 2010 summary report. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; 2011. [Google Scholar]
- Borenstein M, Hedges L, Higgins J, Rothstein H. Comprehensive meta-analysis (Version 2)) [Computer software] Englewood, NJ: Biostat; 2005. [Google Scholar]
- Boudreaux E, Kilpatrick DG, Resnick HS, Best CL, Saunders BE. Criminal victimization, posttraumatic stress disorder, and comorbid psychopathology among a community sample of women. Journal of Traumatic Stress. 1998;11:665–678. doi: 10.1023/A:1024437215004. [DOI] [PubMed] [Google Scholar]
- Bower GH. Mood and memory. American Psychologist. 1981;36(2):129–148. doi: 10.1037//0003-066x.36.2.129. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology. 2000;68:748–766. doi: 10.1037//0022-006x.68.5.748. [DOI] [PubMed] [Google Scholar]
- Burgess AW, Holmstrom LL. Rape trauma syndrome. The American Journal of Psychiatry. 1974;131:981–986. doi: 10.1176/ajp.131.9.981. [DOI] [PubMed] [Google Scholar]
- Burnam MA, Stein JA, Golding JM, Siegel JM, Sorenson SB, Forsythe AB, Telles CA. Sexual assault and mental disorders in a community population. Journal of Consulting and Clinical Psychology. 1988;56:843–850. doi: 10.1037//0022-006x.56.6.843. [DOI] [PubMed] [Google Scholar]
- Calhoun KS, Atkeson BM, Resick PA. A longitudinal examination of fear reactions in victims of rape. Journal of Counseling Psychology. 1982;29(6):655–661. [Google Scholar]
- Campbell R, Dworkin ER, Cabral G. An ecological model of the impact of sexual assault on women’s mental health. Trauma, Violence, & Abuse. 2009;10(3):225–246. doi: 10.1177/1524838009334456. [DOI] [PubMed] [Google Scholar]
- Campbell R, Greeson MR, Bybee D, Raja S. The co-occurrence of childhood sexual abuse, adult sexual assault, intimate partner violence, and sexual harassment: A mediational model of posttraumatic stress disorder and physical health outcomes. Journal of Consulting and Clinical Psychology. 2008;76(2):194–207. doi: 10.1037/0022-006X.76.2.194. [DOI] [PubMed] [Google Scholar]
- Campbell R, Sefl T, Barnes HE, Ahrens CE, Wasco SM, Zaragoza-Diesfeld Y. Community services for rape survivors: Enhancing psychological well-being or increasing trauma? Journal of Consulting and Clinical Psychology. 1999;67(6):847–858. doi: 10.1037//0022-006x.67.6.847. [DOI] [PubMed] [Google Scholar]
- Carter-Snell CJ, Jakubec SL. Exploring women’s risks and resilience to mental illness after interpersonal violence. International Journal of Child Youth and Family Studies. 2013;1:72–99. [Google Scholar]
- Chen LP, Murad MH, Paras ML, Colbenson KM, Sattler AL, Goranson EN, Zirakzadeh A. Sexual abuse and lifetime diagnosis of psychiatric disorders: Systematic review and meta-analysis. Mayo Clinic Proceedings. 2010;85(7):618–629. doi: 10.4065/mcp.2009.0583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung MWL. metaSEM: An R package for meta-analysis using structural equation modeling. Frontiers in Psychology. 2012;5:1–7. doi: 10.3389/fpsyg.2014.01521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chilcoat HD, Breslau N. Investigations of causal pathways between PTSD and drug use disorders. Addictive Behaviors. 1998;23(6):827–840. doi: 10.1016/s0306-4603(98)00069-0. [DOI] [PubMed] [Google Scholar]
- Classen CC, Palesh OG, Aggarwal R. Sexual revictimization: A review of the empirical literature. Trauma, Violence, & Abuse. 2005;6:103–129. doi: 10.1177/1524838005275087. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- Conway CC, Hammen C, Brennan PA. Expanding stress generation theory: Test of a transdiagnostic model. Journal of Abnormal Psychology. 2012;121(3):754–766. doi: 10.1037/a0027457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook SL, Gidycz CA, Koss MP, Murphy M. Emerging issues in the measurement of rape victimization. Violence Against Women. 2011;17:201–218. doi: 10.1177/1077801210397741. [DOI] [PubMed] [Google Scholar]
- Cromer KR, Schmidt NB, Murphy DL. An investigation of traumatic life events and obsessive-compulsive disorder. Behaviour Research and Therapy. 2007;45(7):1683–1691. doi: 10.1016/j.brat.2006.08.018. [DOI] [PubMed] [Google Scholar]
- du Fort GG, Newman S, Bland R. Psychiatric comorbidity and treatment seeking: sources of selection bias in the study of clinical populations. Journal of Nervous and Mental Disease. 1993;181:464–474. [PubMed] [Google Scholar]
- Duval S, Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000a;56:455–463. doi: 10.1111/j.0006-341x.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- Duval S, Tweedie R. A nonparametric “trim and fill” method of accounting for publication bias in meta-analysis. Journal of the American Statistical Society. 2000b;95(449):89–98. [Google Scholar]
- [dataset]; Dworkin ER, Menon S, Bystrynski J, Allen NE. Data for: Sexual assault victimization and psychopathology: A review and meta-analysis. Mendeley Data. 2017 doi: 10.1016/j.cpr.2017.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards KM, Turchik JA, Dardis CM, Reynolds N, Gidycz CA. Rape myths: History, individual and institutional-level presence, and implications for change. Sex Roles. 2011;65:761–773. [Google Scholar]
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. British Medical Journal. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellard KK, Fairholme CP, Boisseau CL, Farchione TJ, Barlow DH. Unified Protocol for the Transdiagnostic Treatment of Emotional Disorders: Protocol development and initial outcome data. Cognitive and Behavioral Practice. 2010;17(1):88–101. doi: 10.1016/j.cbpra.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Etain B, Henry C, Bellivier F, Mathieu F, Leboyer M. Beyond genetics: Childhood affective trauma in bipolar disorder. Bipolar Disorders. 2008;10:867–876. doi: 10.1111/j.1399-5618.2008.00635.x. [DOI] [PubMed] [Google Scholar]
- Fisher BS, Cullen FT, Turner MG. The sexual victimization of college women. Washington, D C: National Institute of Justice; 2000. [Google Scholar]
- Frazier PA, Schauben LJ. Stressful life events and psychological adjustment among female college students. Measurement and Evaluation in Counseling and Development. 1994;27(1):280–292. [Google Scholar]
- Friedman MJ, Resick PA, Bryant RA, Brewin CR. Considering PTSD for DSM-5. Depression and Anxiety. 2011;28:750–769. doi: 10.1002/da.20767. [DOI] [PubMed] [Google Scholar]
- Gershuny BS, Baer L, Jenike MA, Minichiello WE, Wilhelm S. Comorbid posttraumatic stress disorder: Impact on treatment outcome for obsessive-compulsive disorder. American Journal of Psychiatry. 2002;159:852–854. doi: 10.1176/appi.ajp.159.5.852. [DOI] [PubMed] [Google Scholar]
- Gilbert N. Examining the facts: Advocacy research overstates the incidence of date and acquaintance rape. In: Gelles RJ, Loseke DR, editors. Current controversies on family violence. Newbury Park, CA: SAGE; 1993. pp. 120–132. [Google Scholar]
- Gnambs T. The elusive general factor of personality: The acquaintance effect. European Journal of Personality. 2013;27:507–520. doi: 10.1002/per.1933. [DOI] [Google Scholar]
- Golding JM. Intimate partner violence as a risk factor for mental disorders: A meta-analysis. Journal of Family Violence. 1999;14(2):99–132. [Google Scholar]
- Goodman LA, Koss MP, Russo NF. Violence against women: Physical and mental health effects. Part I: Research findings. Applied & Preventive Psychology. 1993;2(2):79–89. [Google Scholar]
- Green BL, Goodman LA, Krupnick JL, Corcoran CB, Petty RM, Stockton P, Stern NM. Outcomes of single versus multiple trauma exposure in a screening sample. Journal of Traumatic Stress. 2000;13(2):271–286. doi: 10.1023/A:1007758711939. [DOI] [PubMed] [Google Scholar]
- Harris EC, Barraclough B. Suicide as an outcome for mental disorders: A meta-analysis. British Journal of Psychiatry. 1997;170:205–228. doi: 10.1192/bjp.170.3.205. [DOI] [PubMed] [Google Scholar]
- Hartung CM, Widiger TA. Gender differences in the diagnosis of mental disorders: Conclusions and controversies of the DSM-IV. Psychological Bulletin. 1998;123(3):260–278. doi: 10.1037/0033-2909.123.3.260. [DOI] [PubMed] [Google Scholar]
- Hernandez JM, Cordova MJ, Ruzek J, Reiser R, Gwizdowski IS, Suppes T, Ostacher MJ. Presentation and prevalence of PTSD in a bipolar disorder population: A STEP-BD examination. Journal of Affective Disorders. 2013;150:450–455. doi: 10.1016/j.jad.2013.04.038. [DOI] [PubMed] [Google Scholar]
- Hettema JM, Neale MC, Kendler KS. A review and meta-analysis of the genetic epidemiology of anxiety disorders. The American Journal of Psychiatry. 2001;158:1568–1578. doi: 10.1176/appi.ajp.158.10.1568. [DOI] [PubMed] [Google Scholar]
- Jewkes R. Violence against women: An emerging health problem. International Clinical Psychoparmacology. 2000;15(Supp3):S37–S45. [PubMed] [Google Scholar]
- Jordan CE, Campbell R, Follingstad D. Violence and women’s mental health: The impact of physical, sexual, and psychological aggression. Annual Review of Clinical Psychology. 2010;6:607–628. doi: 10.1146/annurev-clinpsy-090209-151437. [DOI] [PubMed] [Google Scholar]
- Kelley LP, Weathers FW, McDevitt-Murphy ME, Eakin DE, Flood AM. A comparison of PTSD symptom patterns in three types of civilian trauma. Journal of Traumatic Stress. 2009;22(3):227–235. doi: 10.1002/jts. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Davis CG, Kessler RC. The familial aggregation of common psychiatric and substance use disorders in the National Comorbidity Survey: A family history study. The British Journal of Psychiatry. 1997;170:541–548. doi: 10.1192/bjp.170.6.541. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Archives of General Psychiatry. 2003;60:929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- Kennedy AC, Prock KA. “I still feel like I am not normal”: A review of the role of stigma and stigmatization among female survivors of child sexual abuse, sexual assault, and intimate partner violence. Trauma, Violence, & Abuse. 2016 doi: 10.1177/1524838016673601. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB, Sonnega A, Nelson CB. Posttraumatic stress disorder in the National Comorbity Survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB, Breslau N. Epidemiological risk factors for trauma and PTSD. In: Yehuda R, editor. Risk factors for posttraumatic stress disorder. Washington, D C: American Psychiatric Association; 1999. pp. 23–59. [Google Scholar]
- Kilpatrick DG, Acierno R, Resnick HS, Saunders BE, Best CL. A 2-year longitudinal analysis of the relationships between violent assault and substance use in women. Journal of Consulting and Clinical Psychology. 1997;65(5):834–847. doi: 10.1037//0022-006x.65.5.834. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Resick PA, Veronen LJ. Effects of a rape experience: A longitudinal study. Journal of Social Issues. 1981;37(4):105–122. [Google Scholar]
- Koss MP. Hidden, unacknowledged, acquaintance, and date rape: Looking back, looking forward. Psychology of Women Quarterly. 2011;35:348–354. [Google Scholar]
- Koss MP, Abbey A, Campbell R, Cook S, Norris J, Testa M, White J. Revising the SES: A collaborative process to improve assessment of sexual aggression and victimization. Psychology of Women Quarterly. 2007;31:357–370. [Google Scholar]
- Koss MP, Gidycz CA, Wisniewski N. The scope of rape: Incidence and prevalence of sexual aggression and victimization in a national sample of higher education students. Journal of Consulting and Clinical Psychology. 1987;55(2):162–170. doi: 10.1037//0022-006x.55.2.162. [DOI] [PubMed] [Google Scholar]
- Koss MP, Heise L, Russo NF. The global health burden of rape. Psychology of Women Quarterly. 1994;18(4):509–537. [Google Scholar]
- Long LM, Ullman SE, Starzynski LL, Long SM, Mason GE. Age and educational differences in African American women’s sexual assault experiences. Feminist Criminology. 2007;2:117–136. [Google Scholar]
- Messman-Moore TL, Long PJ. The role of childhood sexual abuse sequelae in the sexual revictimization of women: An empirical review and theoretical reformulation. Clinical Psychology Review. 2003;23:537–571. doi: 10.1016/s0272-7358(02)00203-9. [DOI] [PubMed] [Google Scholar]
- Neville HA, Heppner MJ. Contextualizing rape: Reviewing sequelae and proposing a culturally inclusive ecological model of sexual assault recovery. Applied & Preventive Psychology. 1999;8:41–62. [Google Scholar]
- Orcutt HK, Erickson DJ, Wolfe J. A prospective analysis of trauma exposure: The mediating role of PTSD symptomatology. Journal of Traumatic Stress. 2002;15:259–266. doi: 10.1023/A:1015215630493. [DOI] [PubMed] [Google Scholar]
- Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychological Bulletin. 2003;129(1):52–73. doi: 10.1037/0033-2909.129.1.52. [DOI] [PubMed] [Google Scholar]
- Panagioti M, Gooding PA, Tarrier N. A meta-analysis of the association between posttraumatic stress disorder and suicidality: The role of comorbid depression. Comprehensive Psychiatry. 2012;53(7):915–930. doi: 10.1016/j.comppsych.2012.02.009. [DOI] [PubMed] [Google Scholar]
- Paolucci EO, Genuis ML. A meta-analysis of the published research on the effects of child sexual abuse. The Journal of Psychology. 2001;135(1):17–36. doi: 10.1080/00223980109603677. [DOI] [PubMed] [Google Scholar]
- Pineles SL, Shipherd JC, Welch LP, Yovel I. The role of attentional biases in PTSD: Is it interference or facilitation? Behaviour Research and Therapy. 2007;45:1903–1913. doi: 10.1016/j.brat.2006.08.021. [DOI] [PubMed] [Google Scholar]
- Preti A, Rocchi MBL, Sisti D, Camboni MV, Miotto P. A comprehensive meta-analysis of the risk of suicide in eating disorders. Acta Psychiatrica Scandinavica. 2011;124(1):6–17. doi: 10.1111/j.1600-0447.2010.01641.x. [DOI] [PubMed] [Google Scholar]
- R Development Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing; Vienna, Austria: 2008. URL http://www.R-project.org. [Google Scholar]
- Resick PA. Psychological effects of victimization: Implications for the criminal justice system. Crime & Delinquency. 1987;33:468–478. doi: 10.1177/0011128787033004004. [DOI] [Google Scholar]
- Resick PA. The psychological impact of rape. Journal of Interpersonal Violence. 1993;8:223–255. [Google Scholar]
- Rosenthal R. The file drawer problem and tolerance for null results. Psychological Bulletin. 1979;86(3):638–641. doi: 10.1037/0033-2909.86.3.638. [DOI] [Google Scholar]
- Rothbaum BO, Foa EB, Riggs DS, Murdock T, Walsh W. A prospective examination of post-traumatic stress disorder in rape victims. Journal of Traumatic Stress. 1992;5(3):455–475. [Google Scholar]
- Rudd MD. Fluid vulnerability theory: a cognitive approach to understanding the process of acute and chronic suicide risk. In: Ellis TE, editor. Cognition and suicide: Theory, research, and therapy. Washington, DC: American Psychological Association; 2006. [Google Scholar]
- Sarkar NN, Sarkar R. Sexual assault on woman: Its impact on her life and living in society. Sexual and Relationship Therapy. 2005;20(4):407–419. [Google Scholar]
- Smolak L, Murnen SK. A meta-analytic examination of the relationship between child sexual abuse and eating disorders. International Journal of Eating Disorders. 2002;31(2):136–150. doi: 10.1002/eat.10008. [DOI] [PubMed] [Google Scholar]
- Stein DJ, Chiu WT, Hwang I, Kessler RC, Sampson N, Alonso J, Nock MK. Cross-national analysis of the associations between traumatic events and suicidal behavior: Findings from the WHO World Mental Health Surveys. PloS ONE. 2010;5(5):e10574. doi: 10.1371/journal.pone.0010574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steketee G, Foa EB. Rape victims: Post-traumatic stress responses and their treatment: A review of the literature. Journal of Anxiety Disorders. 1987;1:69–86. [Google Scholar]
- Stewart SH, Conrod PJ. Psychosocial models of functional associations between posttraumatic stress disorder and substance use disorder. In: Ouimette P, Brown PJ, editors. Trauma and substance abuse: Causes, consequences, and treatment of comorbid disorders. Washington, DC: American Psychological Association; 2003. pp. 29–55. [Google Scholar]
- Sutherland S, Scherl DJ. Patterns of response among victims of rape. American Journal of Orthopsychiatry. 1970;40(3):503–511. doi: 10.1111/j.1939-0025.1970.tb00708.x. [DOI] [PubMed] [Google Scholar]
- Testa M, Livingston JA. Alcohol and sexual aggression: Reciprocal relationships over time in a sample of high-risk women. Journal of Interpersonal Violence. 2000;15(4):413–427. [Google Scholar]
- Testa M, Livingston JA, Hoffman JH. Does sexual victimization predict subsequent alcohol consumption? A prospective study among a community sample of women. Addictive Behaviors. 2007;32(12):2926–2939. doi: 10.1016/j.addbeh.2007.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tjaden P, Thoennes N. Prevalence and consequences of male-to-female and female-to-male intimate partner violence as measured by the National Violence Against Women Survey. Violence Against Women. 2000;6(2):142–161. doi: 10.1177/10778010022181769. [DOI] [Google Scholar]
- Tjaden P, Thoennes N. Extent, nature, and consequences of rape victimization: Findings from the National Violence Against Women Survey. Washington, D C: 2006. [Google Scholar]
- Tolin DF, Foa EB. Sex differences in trauma and posttraumatic stress disorder: A quantitative review of 25 years of research. Psychological Bulletin. 2006;132(6):959–992. doi: 10.1037/0033-2909.132.6.959. [DOI] [PubMed] [Google Scholar]
- Ullman SE, Brecklin LR. Sexual assault history and suicidal behavior in a national sample of women. Suicide and Life-Threatening Behavior. 2002;32:117–130. doi: 10.1521/suli.32.2.117.24398. [DOI] [PubMed] [Google Scholar]
- Ullman SE, Peter-Hagene LC. Longitudinal relationships of social reactions, PTSD, and revictimization in sexual assault survivors. Journal of Interpersonal Violence. 2014;29:1–21. doi: 10.1177/0886260514564069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ullman SE, Townsend SM, Filipas HH, Starzynski LL. Structural models of the relations of assault severity, social support, avoidance coping, self-blame, and PTSD among sexual assault survivors. Psychology of Women Quarterly. 2007;31(1):23–37. [Google Scholar]
- Viechtbauer W. Conducting meta-analyses in R with the metafor package. Journal of Statistical Software. 2010;36(3):1–48. URL: http://www.jstatsoft.org/v36/i03/ [Google Scholar]
- Viechtbauer W, Cheung MWL. Outlier and influence diagnostics for meta-analysis. Research Synthesis Methods. 2010;1:112–125. doi: 10.1002/jrsm.11. [DOI] [PubMed] [Google Scholar]
- Walker EA, Gelfand AN, Gelfand MD, Koss MP, Katon WJ. Medical and psychiatric symptoms in female gastroenterology clinic patients with histories of sexual victimization. General Hospital Psychiatry. 1995;17(2):85–92. doi: 10.1016/0163-8343(94)00058-l. [DOI] [PubMed] [Google Scholar]
- Weaver TL, Clum GA. Psychological distress associated with interpersonal violence: A meta-analysis. Clinical Psychology Review. 1995;15(2):115–140. [Google Scholar]
- Winfield I, George LK, Swartz M, Blazer DG. Sexual assault and psychiatric disorders among a community sample of women. American Journal of Psychiatry. 1990;147(3):335–341. doi: 10.1176/ajp.147.3.335. [DOI] [PubMed] [Google Scholar]
- Xu Y, Olfson M, Villegas L, Okuda M, Wang S, Liu S, Blanco C. A characterization of adult victims of sexual violence: Results from the National Epidemiological Survey for Alcohol and Related Conditions. Psychiatry. 2013;76(3):223–240. doi: 10.1521/psyc.2013.76.3.223. [DOI] [PubMed] [Google Scholar]
- Zinzow HM, Resnick HS, Amstadter AB, McCauley JL, Ruggiero KJ, Kilpatrick DG. Drug- or alcohol-facilitated, incapacitated, and forcible rape in relationship to mental health among a national sample of women. Journal of Interpersonal Violence. 2010;25:2217–2236. doi: 10.1177/0886260509354887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zweig JM, Crockett LJ, Sayer A, Vicary JR. A longitudinal examination of the consequences of sexual victimization for rural young adult women. Journal of Sex Research. 1999;36:396–409. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


