Abstract
Hospitalization is a major source of morbidity among patients with ESRD undergoing maintenance hemodialysis and is a significant contributor to health care costs. To identify subgroups at the highest risk of hospitalization, we analyzed by sex, age, and race, adjusting for demographic and clinical characteristics, the hospitalization rates, and 30-day readmissions for 333,756 hospitalizations among 111,653 patients undergoing maintenance hemodialysis in facilities operated by a large dialysis organization in the United States (2007–2011). The overall hospitalization rate was 1.85 hospitalizations per person-year and was much higher among women than among men (2.08 versus 1.68 hospitalizations per year for women versus men, P<0.001). Age group–specific hospitalization rates were consistently higher for women than for men of the same race, and the differences were greatest in younger age groups (for example, women aged 18–34 years and ≥75 years had 54% [95% confidence interval, 42% to 67%] and 14% [95% confidence interval, 11% to 18%] higher hospitalization rates, respectively, than did men of respective ages). Women also had substantially higher risk for 30-day readmission, with the largest differences at younger ages. Women had a significantly lower serum albumin level than men, and stratification by serum albumin level attenuated sex differences in the age group–specific hospitalization and 30-day readmission rates. These findings suggest that women undergoing maintenance hemodialysis have substantially higher risks for hospitalization and 30-day readmission than men. In this cohort, the sex differences were greatest in the younger age groups and were attenuated by accounting for differences in health status reflected by serum albumin level.
Keywords: end stage kidney disease, hemodialysis, hospitalization
Over 450,000 Americans have ESRD treated with maintenance dialysis; the overwhelming majority of these individuals are Medicare beneficiaries. In 2013, the Medicare program spent $31 billion for the health care of patients with ESRD and even though these patients comprise <1% of the covered population, they accounted for >7% of costs for the fee-for-service Medicare program.1 Hospitalizations are a significant driver of these expenses because patients undergoing maintenance dialysis have a high burden of coexisting illnesses. As such, patients undergoing maintenance dialysis are hospitalized on average 1.9 times per year, spend 12 days in the hospital, and this accounts for almost one-third of annual Medicare expenditure for every patient.1 Furthermore, over one-third of hospitalizations are followed by readmissions within 30 days of discharge, adding further to the burden for patients during these care transitions.1
Recognizing the burden imposed by hospitalizations and 30-day readmissions on both patients and the Medicare program, the Center for Medicare and Medicaid Services has incorporated relevant quality measures in its value-based purchasing program. For example, standardized hospitalization ratio is one of the metrics for the Five Star rating system introduced by the Centers for Medicare and Medicaid Services in 2014.2 Similarly, standardized 30-day readmission ratio is now a measure to judge the quality of care delivered by dialysis facilities.2 These changes in public policy are meant to serve as financial incentives for dialysis facilities to improve care, including care coordination, to reduce hospitalizations and 30-day readmissions.
Identification of populations of patients with ESRD most at risk is a critical step in focusing and refining clinical and policy efforts to reduce these high costs and potentially avoidable hospitalizations and 30-day readmissions. In this study, we compared patterns of hospitalization and readmission between men and women in a large cohort of patients undergoing maintenance dialysis in facilities operated by a large dialysis provider in the United States to identify subgroups, if any, at the highest risk for such events.
Results
The derivation of the study cohort, index hospitalizations, and readmissions are summarized in Supplemental Figure 1. Of 111,653 patients, 57% were men and the median age was 64 years (interquartile range, 53–74 years). White (47%) and black (31%) were the most common races, a majority of patients were insured by Medicare, and 80% had a Charlson comorbidity index of ≥4 (Table 1).
Table 1.
Selected patient characteristics, hospitalizations, and unadjusted hospitalization rates by sex, 2007–2011
| Characteristic | Men | Women | ||||
|---|---|---|---|---|---|---|
| Patients | Admissions | Rate (yr−1) | Patients | Admissions | Rate (yr−1) | |
| Number | 63,133 | 170,556 | 1.68 | 48,520 | 163,200 | 2.08 |
| Age, yra | ||||||
| 18–34 | 5% | 5% | 1.71 | 5% | 6% | 2.63 |
| 35–44 | 8% | 9% | 1.56 | 7% | 8% | 2.38 |
| 45–54 | 17% | 18% | 1.64 | 14% | 15% | 2.06 |
| 55–64 | 24% | 24% | 1.63 | 24% | 24% | 1.98 |
| 65–74 | 23% | 22% | 1.69 | 25% | 24% | 2.00 |
| ≥75 | 23% | 21% | 1.80 | 26% | 22% | 2.08 |
| Race/ethnicity | ||||||
| Asian | 3% | 3% | 1.24 | 3% | 3% | 1.54 |
| Black | 29% | 33% | 1.68 | 34% | 39% | 2.17 |
| White | 49% | 47% | 1.81 | 44% | 42% | 2.18 |
| Hispanic | 15% | 15% | 1.47 | 14% | 14% | 1.80 |
| Other | 4% | 3% | 1.42 | 4% | 3% | 1.76 |
| Primary insurancea | ||||||
| Medicare | 52% | 54% | 1.80 | 56% | 57% | 2.17 |
| Medicaid | 7% | 8% | 1.84 | 7% | 9% | 2.36 |
| Other | 41% | 37% | 1.49 | 37% | 34% | 1.89 |
| Charlson comorbidity index | ||||||
| <4 | 22% | 20% | 1.45 | 18% | 17% | 2.00 |
| 4–5 | 36% | 36% | 1.63 | 36% | 35% | 2.00 |
| 6–7 | 31% | 32% | 1.76 | 34% | 34% | 2.11 |
| ≥8 | 11% | 13% | 2.07 | 13% | 14% | 2.34 |
| Congestive heart failure | ||||||
| No | 64% | 50% | 1.49 | 63% | 49% | 1.86 |
| Yes | 36% | 50% | 1.91 | 37% | 51% | 2.34 |
| Diabetes mellitus | ||||||
| No | 44% | 33% | 1.50 | 40% | 29% | 1.90 |
| Yes | 56% | 67% | 1.78 | 60% | 71% | 2.16 |
| Myocardial infarction | ||||||
| No | 85% | 80% | 1.62 | 86% | 81% | 2.02 |
| Yes | 15% | 20% | 1.93 | 14% | 19% | 2.37 |
| Other cardiovascular comorbidity | ||||||
| No | 85% | 79% | 1.60 | 85% | 81% | 2.00 |
| Yes | 15% | 21% | 2.02 | 15% | 19% | 2.46 |
| Geographic regiona | ||||||
| Northeast | 13% | 14% | 1.80 | 12% | 13% | 2.14 |
| Midwest | 17% | 18% | 1.94 | 17% | 18% | 2.46 |
| South | 43% | 44% | 1.70 | 45% | 46% | 2.11 |
| West | 27% | 23% | 1.43 | 26% | 23% | 1.77 |
| Year of incidence | ||||||
| 2007 | 20% | 28% | 1.58 | 20% | 28% | 1.95 |
| 2008 | 20% | 27% | 1.64 | 20% | 26% | 2.05 |
| 2009 | 21% | 22% | 1.66 | 21% | 22% | 2.08 |
| 2010 | 21% | 16% | 1.79 | 21% | 16% | 2.21 |
| 2011 | 18% | 7% | 2.04 | 18% | 7% | 2.53 |
At time of dialysis initiation.
Hospitalizations
During the entire period of observation, 73% of all patients were hospitalized at least once. The overall unadjusted hospitalization rate was 1.85 per person-year (95% confidence interval [95% CI], 1.84 to 1.86), with 1.68 (95% CI, 1.67 to 1.68) per year among men and 2.08 (95% CI, 2.07 to 2.09) per year among women (Table 1). Unadjusted hospitalization rates were highest among younger (age 18–34 years and 35–44 years) or elderly (age≥75 years) patients, and whites and blacks compared with Asians or Hispanics.
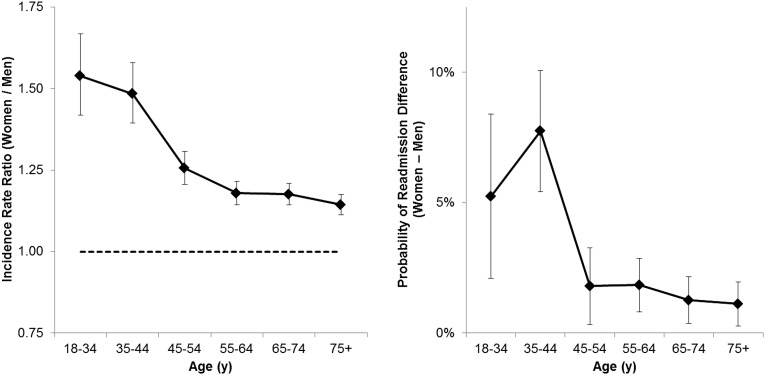
Women had higher adjusted hospitalization rates than men of the same race and age, and, in particular, at younger ages (Figure 1, Supplemental Table 1). Notably, women aged 18–34 years or 35–40 years had 54% (95% CI, 42%–67%) or 48% (95% CI, 40%–58%) higher hospitalization rates than men of the same age and race. This pattern of higher hospitalization rates among women than men was consistent across races when analysis was further stratified by race (Supplemental Figure 2; P=0.1 for additional interaction term). Sensitivity analyses (1) with adjustment of data for coexisting illness at baseline (instead of at any time during follow-up), or (2) without adjustment for Charlson comorbidity index, or (3) with the use of multilevel models accounting for clustering over time and in individual patients within facilities, yielded almost identical results. Similar results were obtained when the analyses were limited to hospitalizations within the first year of dialysis or within the first 90 days of start of dialysis (Supplemental Table 2).
Figure 1.
Sex differences in hospitalization and 30-day readmissions vary by age in patients undergoing thrice-weekly hemodialysis. Adjusted incidence rate ratios (IRRs) of hospitalization (left) and difference in adjusted probability of readmission within 30 days of discharge (right), comparing women to men by age. Error bars represent 95% CIs. Hospitalization IRRs and readmission probability adjusted for race, geographic region, calendar year of dialysis initiation, time since initiation of dialysis, insurance, Charlson comorbidity index, diabetes, and cardiovascular comorbidities, and the interaction of age and race.
30-Day Readmission
Of 314,157 index discharges included in analysis of subsequent readmission (Supplemental Figure 1), 35% and 3% were followed by readmission or death, respectively, within the subsequent 30 days. The unadjusted probability of 30-day readmission was 34% in men and 37% in women, and was higher for younger than for older patients, for patients with more prior hospitalizations, and for blacks and whites compared with Asians and Hispanics (Table 2).
Table 2.
Unadjusted probability of readmission or death within 30 days after hospital discharge by patient characteristic, stratified by sex
| Characteristic | Men | Women | ||
|---|---|---|---|---|
| Readmission, % | Death, % | Readmission, % | Death, % | |
| Probability | 33.0 | 2.9 | 35.3 | 2.5 |
| Age, yra | ||||
| 18–34 | 42.0 | 0.7 | 47.6 | 0.7 |
| 35–44 | 35.0 | 1.2 | 43.2 | 1.1 |
| 45–54 | 35.0 | 1.4 | 37.2 | 1.4 |
| 55–64 | 32.6 | 2.1 | 34.7 | 1.9 |
| 65–74 | 31.6 | 3.3 | 33.1 | 2.7 |
| ≥75 | 30.5 | 5.6 | 31.8 | 4.4 |
| Race/ethnicity | ||||
| Asian | 28.8 | 2.5 | 30.5 | 2.0 |
| Black | 34.1 | 1.9 | 37.2 | 1.8 |
| White | 33.2 | 3.9 | 34.9 | 3.4 |
| Hispanic | 31.3 | 2.0 | 33.0 | 1.8 |
| Other | 30.2 | 2.2 | 32.2 | 1.9 |
| Prior hospitalizations | ||||
| 0 | 25.1 | 1.7 | 26.7 | 1.5 |
| 1–3 | 30.6 | 3.1 | 32.3 | 2.7 |
| 4–8 | 38.4 | 3.7 | 38.8 | 3.1 |
| 9+ | 51.6 | 3.0 | 52.6 | 2.3 |
| Primary insurance | ||||
| Medicare | 33.1 | 3.3 | 35.2 | 2.8 |
| Medicaid | 36.3 | 1.8 | 39.1 | 1.8 |
| Other | 32.0 | 2.5 | 34.6 | 2.0 |
| Charlson comorbidity index | ||||
| <4 | 35.2 | 1.3 | 39.0 | 1.2 |
| 4–5 | 32.4 | 2.4 | 35.2 | 2.2 |
| 6–7 | 32.2 | 3.8 | 33.6 | 3.0 |
| >7 | 33.2 | 4.7 | 34.9 | 3.8 |
| Congestive heart failure | ||||
| No | 31.4 | 3.4 | 33.7 | 3.0 |
| Yes | 34.5 | 2.3 | 36.8 | 2.0 |
| Diabetes mellitus | ||||
| No | 31.6 | 3.2 | 34.1 | 2.9 |
| Yes | 33.6 | 2.7 | 35.8 | 2.3 |
| Myocardial infarction | ||||
| No | 32.5 | 2.9 | 34.8 | 2.5 |
| Yes | 34.7 | 2.7 | 37.4 | 2.2 |
| Other cardiovascular comorbidity | ||||
| No | 32.5 | 2.9 | 34.8 | 2.5 |
| Yes | 34.7 | 2.9 | 37.4 | 2.5 |
| Geographic region | ||||
| Northeast | 33.4 | 2.9 | 34.9 | 2.5 |
| Midwest | 35.0 | 2.9 | 37.6 | 2.5 |
| South | 32.8 | 2.8 | 35.6 | 2.3 |
| West | 31.1 | 2.8 | 32.6 | 2.4 |
| Year of incidence | ||||
| 2007 | 32.6 | 3.0 | 34.7 | 2.4 |
| 2008 | 33.2 | 2.9 | 35.4 | 2.5 |
| 2009 | 33.0 | 2.9 | 36.0 | 2.5 |
| 2010 | 33.5 | 2.9 | 35.7 | 2.5 |
| 2011 | 32.6 | 2.1 | 34.7 | 2.1 |
At discharge.
Comparing men and women of the same race and age category, and adjusting for baseline characteristics, women consistently had higher probabilities of 30-day readmission (Figure 1). The largest difference in adjusted readmission probability was between women and men aged 35–44 years (difference in readmission rates between women and men of 7.9% [5.6%–10%]). Further stratification by race showed that the overall pattern of higher adjusted probability of readmission among women than men was consistent across races (Supplemental Figure 2, Supplemental Table 3; P=0.5 for interaction term).
Stratification by Laboratory and Clinical Parameters
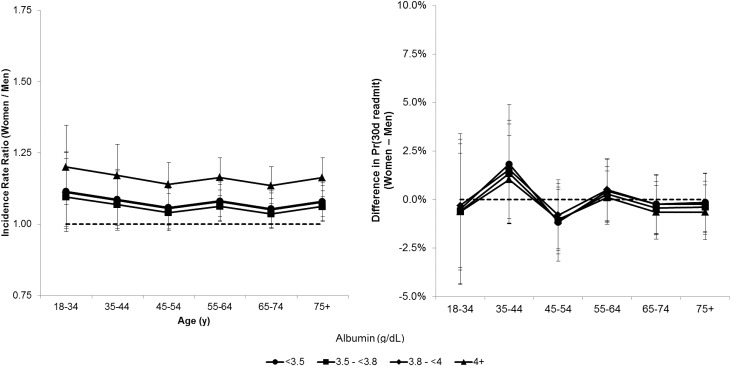
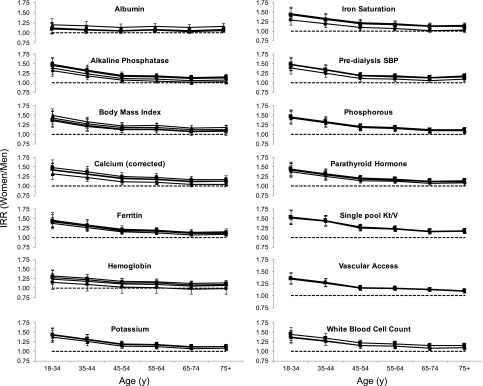
Stratification by serum albumin category (<3.50, 3.50–3.79, 3.80–3.99, ≥4.0 g/dl) showed that hospitalization rates were similar between men and women within the same category of albumin and, thus, stratification by albumin attenuated the hospitalization incidence rate ratio (IRR) comparing women to men (Figure 2). In addition, the IRR comparing women to men stratified by serum albumin was largely independent of age (Figure 2, Supplemental Table 4). Stratification by vascular access showed that the IRR comparing women to men was independent of vascular access method and although the IRR was slightly attenuated across ages, it remained largest among younger patients (Figure 3, Supplemental Table 4). In contrast, stratification by quartiles of other laboratory or clinical parameters did not substantially change the age-specific hospitalization IRRs comparing women to men (Figure 4, Supplemental Table 4). Differences in the adjusted probability of 30-day readmission between women and men were also attenuated when stratified by albumin (Figure 2). However, stratification by any other clinical parameter also generally reduced the difference in 30-day readmission probability between women and men.
Figure 2.
The sex differences in hospitalization and 30-day readmission are attenuated and do not vary by age when stratified by serum albumin. Adjusted incidence rate ratio (IRR) of hospitalization (left) and difference in adjusted probability of readmission within 30 days of discharge (right) comparing women to men by age, stratified by serum albumin. Error bars represent 95% CIs. Hospitalization IRRs and readmission probability adjusted for race, geographic region, calendar year of dialysis initiation, time since initiation of dialysis, insurance, Charlson index, diabetes, and cardiovascular comorbidities, and the interaction of age and race. Pr(30d readmit), Probability of readmission within 30 days of discharge.
Figure 3.
Sex differences in hospitalization persist and vary by age when stratified by the type of vascular access. Adjusted incidence rate ratio (IRR) of hospitalization comparing women to men by age, stratified by vascular access (CVC, central venous catheter; AV, arteriovenous access). There was no difference in the IRR, comparing women to men by age, in individuals with different vascular access types.
Figure 4.
Adjusted IRR of hospitalization comparing women to men by age, stratified by quartiles of clinical variables. To facilitate comparison, stratification by albumin (as in Figure 2) and vascular access (Figure 3) are included. Laboratory variables were categorized into quartiles except albumin (<3.50, 3.50–3.79, 3.80–3.99, ≥4 mg/dl), body mass index (<18, 18–24.9, 25–29.9, 30–39.9, ≥40 kg/m2), hemoglobin (<9, 9–9.9, 10–10.9, ≥11 g/dl), calcium (<8.5, 8.5–8.9, 9.0–9.4, 9.5–10.1, ≥10.2 mg/dl), and phosphorous (<4.5, 4.6–5.3, 5.4–6.3, ≥6.4 mg/dl). Vascular access was central venous catheter (squares) or any arteriovenous method (circles).
Mean serum albumin tended to increase with time on dialysis in both men and women of all ages. However, averaged over the first 182 days or all of follow-up, mean serum albumin was lower in women compared with men of the same age (Supplemental Figure 3). Thus, the prevalence of serum albumin <3.8 g/dl was higher in women than in men of similar age (Supplemental Figure 3).
Discussion
The results of our study showed that among patients with ESRD undergoing maintenance hemodialysis in the United States, women have higher hospitalization rates than men, and that this difference is especially pronounced among younger patients. Consistent with a higher rate of hospitalization, younger female patients were more often readmitted to the hospital within 30 days of discharge than were male patients. These relationships were similar across categories of race, even as hospitalization and readmission rates varied by race as in earlier studies.3 The sex differences in health outcomes among patients undergoing maintenance dialysis are not well recognized or studied and, in our study, were much greater than racial differences in hospitalizations and 30-day readmissions. Identification of interventions to effectively reduce these differences in hospitalizations by sex for patients undergoing maintenance dialysis could have a substantial effect on public health and health care costs. For example, if women experienced the same hospitalization rate as men of the same age and race, >30,000 hospitalizations (approximately 10% of all hospitalizations observed) would have been averted over 5 years.
The United States Renal Data System provides annual estimates for trends in outcomes for all patients undergoing maintenance dialysis in the United States and has reported higher hospitalization rates for women than men (1.98 and 1.68 per patient-year, respectively) and for younger compared with older patients (1.96 and 1.87 per patient-year for patients 22–44 years and ≥75 years, respectively).1 These data from the United States Renal Data System show that even though our data were derived from a single dialysis provider, our findings are externally valid and likely generalizable to the dialysis patient population in the United States. However, our study describes for the first time the complex interplay between sex and age by race and further effect modification by serum albumin. Hence, our study demonstrates that the sex differences in hospitalization risk are greatest in the youngest age groups, are evident from the time when patients start maintenance dialysis, and extend to the risk for 30-day readmissions.
We found that this difference between men and women was sharply attenuated when patients’ serum albumin was taken into account. This is perhaps unsurprising because hypoalbuminemia is an indicator of protein-energy wasting and inflammation and is a marker of health of patients undergoing maintenance dialysis.4 Hypoalbuminemia was more common among female patients, and the average difference in serum albumin between men and women was largest at younger ages, the age range with the largest sex differences in hospitalization rates. Because we assessed serum albumin measurements taken before the hospitalizations—and only included albumin measured in 3-month intervals in which a patient was not hospitalized—our findings are not influenced by likely decrease in serum albumin after hospitalization. Instead, taken together, these results suggest that the disparity in hospitalization between men and women, and especially younger men and women, treated with maintenance hemodialysis results from real differences in health that can be detected by measurement of serum albumin.
Hospital admission and readmission rates are sources of significant morbidity and suffering for patients and have important policy and financial implications. The large expense associated with hospital stays among patients receiving dialysis is primarily borne by public health insurance and has been well documented. Recent quality measures introduced by the United States Centers for Medicare and Medicaid Services aim to create incentives for dialysis facilities to reduce hospitalizations and 30-day readmission.2 The implementation of these quality measures and resulting financial consequences for dialysis providers has been controversial, in particular with respect to the risk adjustment employed to estimate excess hospitalization and readmissions. Our results show that hospital admissions and readmissions depend in a complex manner on patient age, race, and sex that may not be fully accounted for by risk-adjustment models that do not include interactions between these variables.
Limitations to our study include the use of data collected as a part of routine delivery of care and hence lacking information on patient psychosocial factors that bear on hospitalization risk, such as presence and degree of social support. These data also do not include information on the cause of hospitalization. The laboratory and clinical parameters we evaluated may be influenced by the time a patient spends in the hospital. To minimize this “reverse causality” we limited analysis of laboratory and clinical measurements to 91-day periods in which a patient was not hospitalized. Nonetheless, if hospitalizations have a long-term effect on later laboratory and clinical parameters, some bias may have been introduced. In addition, because our data did not include laboratory measurements from periods of hospitalization, we were unable to examine how readmission probability may have been affected by these parameters.
Despite these limitations, our study also has important strengths, beginning with the size and diversity of the patient population. Detailed records of dialysis treatment sessions including laboratory and clinical measurements were available for analysis. That the vast majority of dates of hospitalization admission and discharge were consistent with dates of outpatient dialysis sessions supports the validity of the hospitalization data. Finally, the follow-up of patients receiving care through the dialysis provider in our study is highly complete, with a small proportion of patients discharged to another provider or otherwise lost to follow-up.
In summary, our results highlight a large difference in hospitalization rates and 30-day readmission between men and women on hemodialysis and the differences are largest in the youngest age groups. Efforts to further understand the reasons that underlie the sex differences in hospitalization and 30-day readmission, particularly for younger age groups, may help identify targeted interventions to improve the health and wellbeing of patients undergoing maintenance dialysis.
Concise Methods
Study Population and Data Source
The source population comprised all patients age≥18 years who initiated maintenance dialysis in calendar years 2007 through 2011 and received treatment at a facility operated by a large dialysis organization for at least 60 days (DaVita Inc. [n=162,664]).5 All data were obtained from facility electronic medical records. For these analyses the following groups of patients were excluded: (1) those treated at any time with peritoneal dialysis, home hemodialysis, or in-center hemodialysis with a frequency other than three times weekly; (2) patients with >91 days between initiation of dialysis and first recorded treatment at a participating dialysis facility; and (3) those with missing information on race. Hence, the final population included 111,653 individuals (Supplemental Figure 1).
Patients were followed through December 31, 2011 until the earliest of death, kidney transplant, transfer of care to a facility operated by another dialysis provider, discontinuation of dialysis, or administrative end of follow-up. All laboratory values were measured using standardized automated methods in a central laboratory (Deland, FL) within 24 hours of blood collection. Coexisting illnesses were coded as prevalent for all of follow-up if they were recorded at any time during follow-up, and the Charlson comorbidity index was calculated as previously described.6,7
To capture time-varying laboratory and clinical measurements, follow-up time for each patient was divided into 91-day periods from the initiation of dialysis; follow-up was available for up to 20 such periods. Vascular access was dichotomized as either central venous catheter or any arteriovenous access (fistula, graft, or unspecified). The most frequently recorded vascular access and dialysis facility were assigned to each 91-day period, and each 91-day period was assigned the mean of recorded laboratory and clinical measurements and parenteral drugs received during the period.
The proportion of missing information for laboratory and clinical variables was <10% for all variables. Missing values were imputed using multiple imputation with chained equations and five repetitions; the imputation model included a wide variety of case-mix variables, clinical and laboratory variables, prescriptions, and hospitalizations (details in Supplemental Material). The Institutional Review Boards at the University of Washington and Los Angeles Biomedical Research Institute approved the study as exempt from informed consent.
Hospitalization Records
The data on hospitalizations were obtained from the dialysis provider. Hospitalization records with a recorded date of admission as before the first recorded dialysis treatment, after the censoring date, with the same admission and discharge date as another record, or with admission and discharge on the same date were excluded (Supplemental Figure 1). Hospitalizations likely related to kidney transplant were also excluded, defined as any hospitalization with a discharge on or after the date of a kidney transplant, or an admission date the same date as for the transplant. Hospitalization dates were reconciled with dates of outpatient dialysis treatment. For patients with a recorded outpatient dialysis treatment before the recorded discharge date, discharge date was replaced with the date of the first outpatient treatment after hospitalization and before the discharge date (<1% of hospitalizations affected). Overlapping hospitalizations were combined into a single stay, resulting in the deletion of 0.4% of hospitalization records. Admissions that occurred on the same date as the discharge of the previous hospitalization were considered as two distinct hospitalizations and neither was altered. The final dataset included 333,756 hospitalizations.
For analysis of readmission within 30 days of discharge (30-day readmission), patients with no hospitalizations were excluded (n=30,370). Hospitalizations with a discharge date on or after the patient’s date of censoring were excluded (8076 hospitalizations); for n=1176 patients this was the only recorded hospitalization. Patient records were examined for hospitalization, death, or censoring on the date of discharge or during the subsequent 30 days. We excluded index discharges that were followed by fewer than 30 days before transplant, transfer to another provider, dialysis discontinuation, or end of study period (11,523 hospitalizations and 1942 patients). Hence, analysis of 30-day outcomes included 78,167 patients with 314,157 index discharges.
Statistical Analyses
Hospitalization Rate
For each patient, time at risk of hospitalization began on the date of the first recorded dialysis session, did not include the days of hospitalization, and ended at the earliest of death, kidney transplant, transfer to another dialysis provider, discontinuation of dialysis, or administrative end of follow-up. Crude hospitalization rates were calculated for the entire cohort and by sex, age category (18–34, 35–44, 45–54, 55–64, 65–74, and ≥75 years), race, insurance, Charlson comorbidity index category (<4, 4–5, 6–7, ≥8), diabetes, cardiovascular comorbidities, year of incidence, and geographic region (Northeast, Midwest, South, West), as the total number of hospitalizations divided by the total person-years at risk. Exact Poisson 95% CIs were computed for crude hospitalization rates.
To estimate associations of sex or other patient characteristics with hospitalization rates, negative binomial regression was used to model the number of admissions for each patient in each 91-day period. Generalized estimating equations with an exchangeable working correlation structure and robust standard errors were used to account for repeated longitudinal observations of patients.
To examine differences in hospitalization rates between sexes, hospitalization events were first modeled separately by sex to yield IRRs and 95% CIs comparing each age group to 45–54 years olds of the same race, adjusted for primary insurance, geographic region, calendar year of dialysis incidence, time since dialysis initiation in 91-day increments, Charlson comorbidity index, and presence of diabetes, congestive heart failure, myocardial infarction, and other cardiovascular comorbidity. Next, hospitalization rates were modeled in men and women together with the same covariates, and interaction terms of age with race, age with sex, and sex with race. The interaction of sex and race was not significant (P=0.1) and was dropped from the final combined model. Results from this model are presented as IRRs and 95% CIs comparing women to men of the same race within age categories.
30-Day Outcomes
Outcomes within 30 days after hospital discharge were categorized as readmission, death, or no event. Thirty-day periods after discharge ending due to transplant, end of study period, transfer to a different dialysis provider, or discontinuation of dialysis were excluded from analyses. The crude probability of readmission within 30 days was calculated as the number of discharges followed by an admission within the subsequent 30 days, divided by the total number of discharges.
For analyses of 30-day outcomes, polytomous logistic regression was used to model the probability of each possible 30-day outcome (readmission or death) compared with no event. Standard errors were adjusted for clustering of discharges by patient. Thirty-day outcome probabilities were first modeled separately by sex and subsequently in both men and women as described for hospitalization rates. The interaction of race with sex was not statistically significant (P=0.6) and was not included in final models. The results of these models were then used to estimate least squares adjusted probabilities of readmission within 30 days with 95% CIs.
Time-Varying Laboratory/Clinical Parameters
To investigate modification of associations of sex and age by laboratory and clinical parameters, negative binomial regression modeling was repeated in both sexes together as described above, with the addition of one categorized time-varying laboratory/clinical parameter measured in the preceding 91-day period, as well as the interactions of this variable with age and sex. For readmission analyses, the laboratory/clinical parameter was thus measured during the 91-day period preceding the 91-day period of the initial admission (i.e., the admission before the index discharge). Only 91-day periods preceded by a 91-day period during which the patient was not hospitalized were included in this analysis (63% of all patients). From this model, hospitalization IRRs comparing women to men of the same age, race, and quartile of laboratory/clinical variable were estimated. Variables examined included serum albumin, alkaline phosphatase, body mass index, serum calcium corrected for albumin, ferritin, hemoglobin, iron saturation, phosphorous, potassium, systolic BP before dialysis session, parathyroid hormone, single pool Kt/V, and white blood cell count.
Analyses were performed with Stata 13.0 (Stata Corp, College Station, TX).
Disclosures
None.
Supplementary Material
Acknowledgments
The authors extend their thanks to the many staff members and providers working in DaVita clinics and to DaVita Clinical Research.
Supported by grants from the National Institutes of Health/National Institute of Diabetes and Digestive and Kidney Diseases (R01DK095668 to R.M. and K.K.-Z., and T32DK007467 supporting M.R.).
S.V.A. had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. The funding bodies had no role in designing the study; in collecting, analyzing, or interpreting the data; or in preparing or writing this manuscript.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
This article contains supplemental material online at http://jasn.asnjournals.org/lookup/suppl/doi:10.1681/ASN.2016090986/-/DCSupplemental.
References
- 1.United States Renal Data System : Annual Data Report. US Department of Public Health and Human Services, Public Health Service, Bethesda, National Institutes of Health, 2015 [Google Scholar]
- 2.Kliger AS: Quality measures for dialysis: Time for a balanced scorecard. Clin J Am Soc Nephrol 11: 363–368, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yan G, Norris KC, Greene T, Yu AJ, Ma JZ, Yu W, Cheung AK: Race/ethnicity, age, and risk of hospital admission and length of stay during the first year of maintenance hemodialysis. Clin J Am Soc Nephrol 9: 1402–1409, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fouque D, Kalantar-Zadeh K, Kopple J, Cano N, Chauveau P, Cuppari L, Franch H, Guarnieri G, Ikizler TA, Kaysen G, Lindholm B, Massy Z, Mitch W, Pineda E, Stenvinkel P, Treviño-Becerra A, Wanner C: A proposed nomenclature and diagnostic criteria for protein-energy wasting in acute and chronic kidney disease. Kidney Int 73: 391–398, 2008 [DOI] [PubMed] [Google Scholar]
- 5.Kuttykrishnan S, Kalantar-Zadeh K, Arah OA, Cheung AK, Brunelli S, Heagerty PJ, Katz R, Molnar MZ, Nissenson A, Ravel V, Streja E, Himmelfarb J, Mehrotra R: Predictors of treatment with dialysis modalities in observational studies for comparative effectiveness research. Nephrol Dial Transplant 30: 1208–1217, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Charlson ME, Pompei P, Ales KL, MacKenzie CR: A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis 40: 373–383, 1987 [DOI] [PubMed] [Google Scholar]
- 7.Beddhu S, Bruns FJ, Saul M, Seddon P, Zeidel ML: A simple comorbidity scale predicts clinical outcomes and costs in dialysis patients. Am J Med 108: 609–613, 2000 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.