Abstract
Studies have estimated the average risk of postdonation ESRD for living kidney donors in the United States, but personalized estimation on the basis of donor characteristics remains unavailable. We studied 133,824 living kidney donors from 1987 to 2015, as reported to the Organ Procurement and Transplantation Network, with ESRD ascertainment via Centers for Medicare and Medicaid Services linkage, using Cox regression with late entries. Black race (hazard ratio [HR], 2.96; 95% confidence interval [95% CI], 2.25 to 3.89; P<0.001) and male sex (HR, 1.88; 95% CI, 1.50 to 2.35; P<0.001) was associated with higher risk of ESRD in donors. Among nonblack donors, older age was associated with greater risk (HR per 10 years, 1.40; 95% CI, 1.23 to 1.59; P<0.001). Among black donors, older age was not significantly associated with risk (HR, 0.88; 95% CI, 0.72 to 1.09; P=0.3). Greater body mass index was associated with higher risk (HR per 5 kg/m2, 1.61; 95% CI, 1.29 to 2.00; P<0.001). Donors who had a first-degree biological relationship to the recipient had increased risk (HR, 1.70; 95% CI, 1.24 to 2.34; P<0.01). C-statistic of the model was 0.71. Predicted 20-year risk of ESRD for the median donor was only 34 cases per 10,000 donors, but 1% of donors had predicted risk exceeding 256 cases per 10,000 donors. Risk estimation is critical for appropriate informed consent and varies substantially across living kidney donors. Greater permissiveness may be warranted in older black candidate donors; young black candidates should be evaluated carefully.
Keywords: kidney donation, ESRD, risk factors

Long-term studies of living kidney donors have reported low rates of mortality and ESRD1–5; in a national study of living kidney donors in the United States, we previously estimated overall ESRD risk to donors at 31 ESRD cases per 10,000 living kidney donors in the first 15 years postdonation.2 Recent draft guidelines on the evaluation of living kidney donors from Kidney Disease Improving Global Outcomes (KDIGO) recommend that transplant centers develop and communicate a threshold of “acceptable risk” for living kidney donor candidates.6 Under this paradigm, centers would estimate patient-specific risk for each donor candidate, on the basis of a composite profile of risk factors, and potentially decline candidates whose estimated risk exceeds the acceptable risk threshold. However, although centers have developed ad hoc donor selection heuristics on the basis of a single risk factor (e.g., a maximum body mass index [BMI] cutoff) or a simple combination of risk factors (e.g., declining donors with hypertension if their age falls below a minimum value), the KDIGO guidelines wisely point out that such heuristics fall short of a comprehensive estimate of patient-specific risk.
To support an empirical approach to donor selection, Grams et al. developed a calculator to estimate baseline long-term ESRD risk from patient-specific characteristics in healthy individuals, on the basis of a meta-analysis of multiple population cohorts.7 However, these estimates are on the basis of nondonor populations, and estimate baseline ESRD risk, i.e., long-term risk of ESRD if the individual does not donate. Two large cohort studies of individuals who did donate recently reported higher risk of ESRD in living kidney donors compared with healthy nondonors, consistent across two different populations using two different methods of comparison.2,3 Because donation likely increases the risk of ESRD, postdonation ESRD risk in living kidney donors would be higher than baseline risk estimated from the Grams calculator by an unknown amount. Consequently, true risk prediction for living kidney donors must include not only baseline risk (if the individual does not donate) but absolute risk (if the individual does donate) as well. No tool currently exists to estimate personalized ESRD risk after kidney donation.
To address this knowledge gap, we constructed a prediction model of ESRD after living kidney donation using national registry data. The goals of our study were to characterize risk factors for ESRD in living kidney donors using a multivariable framework, and to produce estimates of 5-, 10-, 15-, and 20-year risk of ESRD for individual donors on the basis of baseline health and demographics. Additionally, we sought to incorporate these estimates into an easy-to-use web-based risk calculator, where a user could provide characteristics of a potential donor and receive estimates of ESRD risk over time.
Results
Study Population
There were 133,824 living kidney donors between 1987 and 2015 in the study population (Table 1). Median (interquartile range [IQR]) age at donation was 40 (31–48) years; 40.8% of donors were men, 12.5% were black, and 59.4% had a first-degree biologic relationship to their recipient (parent, child, or sibling). Median (IQR) BMI at donation was 26.6 (23.7–29.7). BMI was missing for 31.0% of donors. We identified 331 cases of incident ESRD, of which 148 (44.7%) occurred in donors who donated before April of 1994. Donors who experienced incident ESRD were more likely to be men (60.4% versus 40.7%; chi-square P<0.001), black (34.4% versus 12.5%; P<0.001), and first-degree biologically related to the recipient (85.6% versus 59.4%; P<0.001).
Table 1.
Characteristics of living donors in the United States, 1987–2014
| Characteristic | No ESRD | ESRD |
|---|---|---|
| N | 133,493 | 331 |
| Median (IQR) yr of donation | 2004 (1999–2010) | 1995 (1991–2000) |
| Median (IQR) age at donation | 40 (31–48) | 38 (30–48) |
| Median (IQR) BMI at donation, kg/m2a | 26.6 (23.7–29.7) | 28.9 (24.4–31.4) |
| Men, % | 40.7 | 60.4 |
| Black, % | 12.5 | 34.4 |
| First-degree biologically related to recipient, % | 59.4 | 85.6 |
| Sibling of recipient | 29.9 | 46.8 |
| Child of recipient | 16.0 | 18.2 |
| Parent of recipient | 13.5 | 20.9 |
BMI at donation and relationship to recipient were missing for 31.0% of donors and 0.7% of donors, respectively. Missingness of BMI was primarily due to incomplete reporting before 1999. In regression analyses, multiple imputation was used to account for missing data.
Risk Factors for ESRD: Univariable
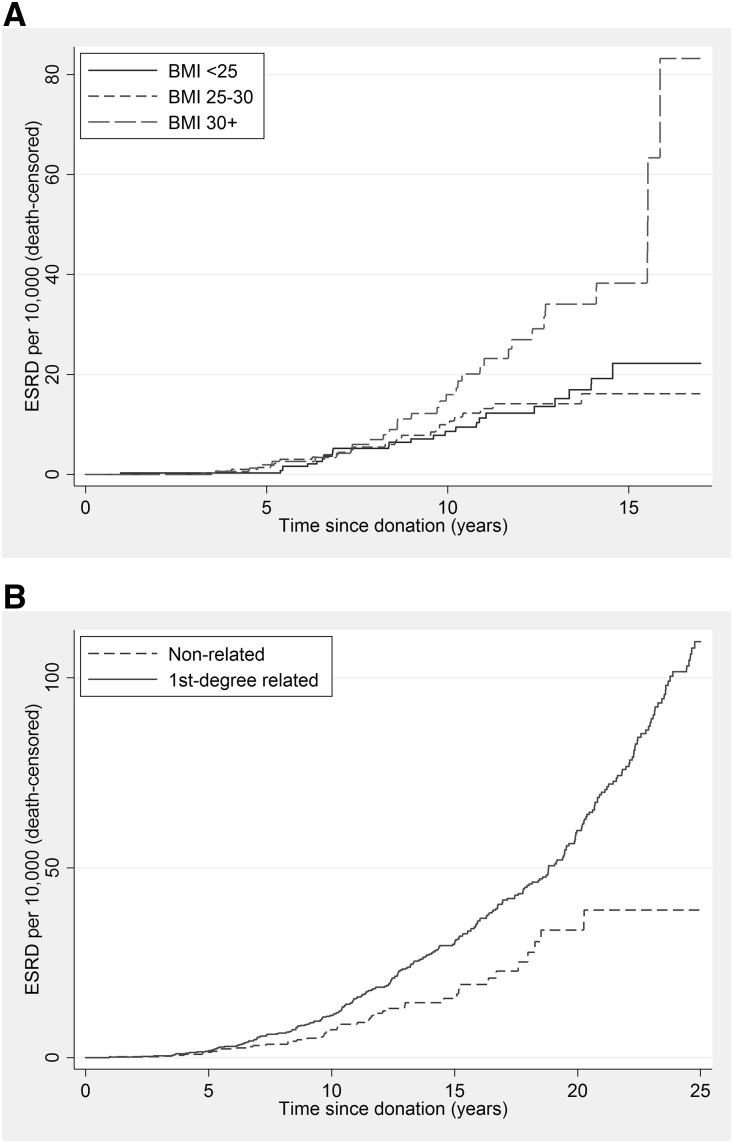
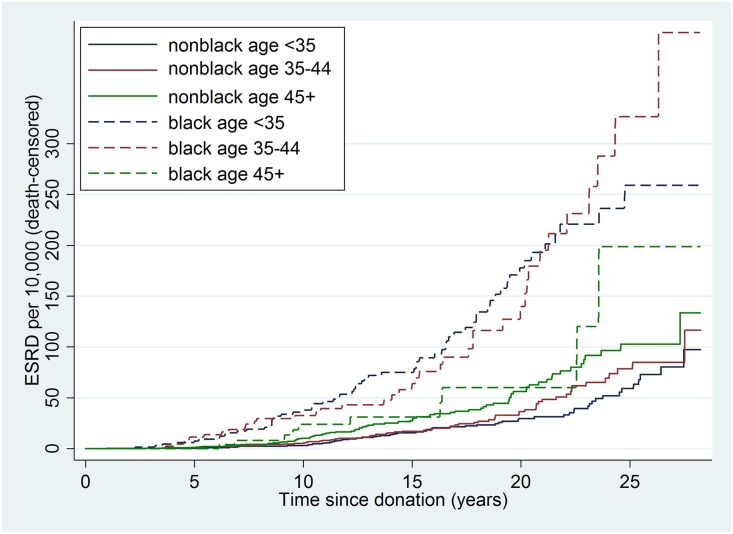
In unadjusted analysis, cumulative incidence of ESRD was lowest among donors with BMI<25 and highest among donors with BMI>30 (Figure 1A) (P<0.01). Cumulative incidence of ESRD was higher among donors who were first-degree biologically related to their recipient (Figure 1B) (P<0.001). Among nonblack donors, older age groups had higher cumulative incidence of ESRD; among black donors, older age groups had lower risk of ESRD (Figure 2). Among donors age<45, blacks had higher cumulative incidence of ESRD; among donors age≥45, incidence was roughly equivalent in black and nonblack donors (Figure 2).
Figure 1.
Cumulative incidence of ESRD was lowest among living donors with BMI <25 and highest among donors with BMI>30 and it was higher among donors who were first-degree biologically related to their recipient. Incidence of ESRD is stratified separately by BMI category (A) and relatedness to recipient (B).
Figure 2.
Among nonblack donors, older age groups had higher cumulative incidence of ESRD, whereas among black donors, older age groups had lower risk of ESRD.
Risk Factors for ESRD: Multivariable
In multivariable analysis, risk of ESRD was higher in male donors (adjusted hazard ratio [aHR], 1.88; 95% confidence interval [CI], 1.50 to 2.35; P<0.001), black donors (aHR at age 40, 2.96; 95% CI, 2.25 to 3.89; P<0.001), and donors who were first-degree biologic relatives of their recipient (aHR, 1.70; 95% CI, 1.24 to 2.34; P<0.01) (Table 2). Among nonblack donors, older age at donation was associated with higher risk (aHR per 10 years of age, 1.40; 95% CI, 1.23 to 1.59; P<0.001). However, among black donors, older age at donation was nonsignificantly associated with lower risk (aHR per 10 years, 0.88; 95% CI, 0.72 to 1.09; P=0.3; age/race interaction P<0.001). Higher BMI was associated with increased ESRD risk (aHR per 5 kg/m2, 1.61; 95% CI, 1.29 to 2.00; P<0.001). In exploratory models, there was no evidence of change in risk associated with Hispanic ethnicity (aHR, 1.16; 95% CI, 0.75 to 1.80; P=0.5), eGFR (aHR per 10 U, 0.97; 95% CI, 0.85 to 1.10; P=0.6), right kidney donation versus left kidney donation (aHR, 0.97; 95% CI, 0.74 to 1.29; P=0.9), secular trend in year of donation (aHR per year, 0.98; 95% CI, 0.95 to 1.01; P=0.1), or systolic BP (aHR per 5 mmHg, 1.05; 95% CI, 0.95 to 1.16; P=0.3).
Table 2.
Risk factors for ESRD in living kidney donors
| Characteristic | aHRa | P Value |
|---|---|---|
| Men (at age 40) | 1.88 (95% CI, 1.50 to 2.35) | <0.001 |
| black race (at age 40) | 2.96 (95% CI, 2.25 to 3.89) | <0.001 |
| Age per 10 yr: nonblack | 1.40 (95% CI, 1.23 to 1.59) | <0.001 |
| Age per 10 yr: black | 0.88 (95% CI, 0.72 to 1.09) | 0.3 |
| BMI per 5 kg/m2 | 1.61 (95% CI, 1.29 to 2.00) | <0.001 |
| First-degree biologically related to recipient | 1.70 (95% CI, 1.24 to 2.34) | <0.01 |
Male sex and greater BMI were associated with higher risk of ESRD (both P<0.001). Older age was associated with higher risk of ESRD in nonblack male donors (P<0.001), but the association between age and risk was not statistically significant in black donors (P=0.1). Donors who were closely related to their recipient had higher risk of ESRD (P<0.01).
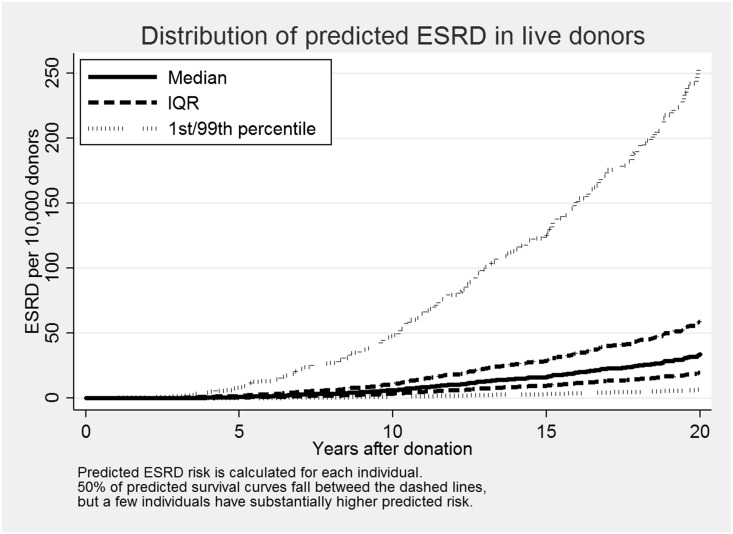
Estimates of 5-, 10-, 15-, and 20-Year ESRD Risk
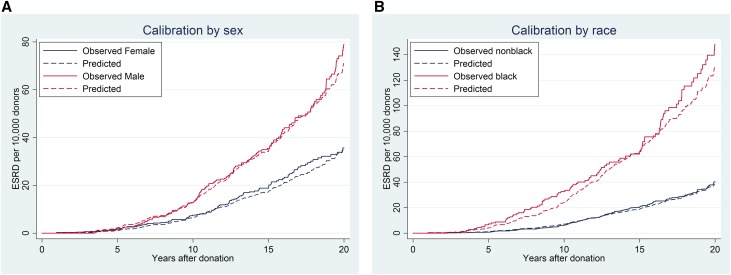
The C-statistic of the model was 0.71. For comparison, the C-statistic in this population of a risk calculator previously published by Ibrahim et al. was 0.57; the C-statistic of that risk calculator among white donors in this population was 0.64. Among all donors in the study, median (IQR) predicted risk of ESRD was 1 (1–2) cases per 10,000 donors at 5 years postdonation; 6 (4–11) per 10,000 at 10 years postdonation; 16 (10–29) per 10,000 at 15 years postdonation; and 34 (20–59) per 10,000 at 20 years postdonation (Figure 3). However, the full range of risk was wide: the 1% of donors with lowest predicted risk had predicted risk below 0.2 cases per 10,000 donors at 5 years postdonation; 1.2 per 10,000 at 10 years postdonation; three per 10,000 at 15 years postdonation; and seven per 10,000 at 20 years postdonation (Figure 3). In contrast, the 1% of donors with highest predicted risk had predicted risk exceeding eight cases per 10,000 donors at 5 years postdonation; 48 per 10,000 at 10 years postdonation; 125 per 10,000 at 15 years postdonation; and 256 per 10,000 at 20 years postdonation (Figure 3). Plots of predicted and observed cumulative incidence of ESRD stratified by race and sex showed good model calibration (Figure 4). A risk calculator can be found at http://www.transplantmodels.com/donesrd/.
Figure 3.
Among all donors in the study, the full range of predicted risk of ESRD was wide, with median (IQR) range of 1 (1–2) cases per 10,000 donors at 5 years postdonation; 6 (4–11) per 10,000 at 10 years postdonation; 16 (10–29) per 10,000 at 15 years postdonation; and 34 (20–59) per 10,000 at 20 years postdonation. Predicted risk of postdonation ESRD for each donor was calculated on the basis of donor characteristics. The median donor had 34 per 10,000 predicted risk of ESRD at 20 years postdonation. Half of all donors have predicted risk between the two dashed lines, but 1% of donors had predicted 20-year ESRD risk exceeding 256 per 10,000.
Figure 4.
Close calibration of observed and predicted cumulative incidence of ESRD. The calibration is stratified by sex in (A) and by race in (B). The plots show good agreement between observed and predicted values.
Discussion
In this national study of ESRD in living kidney donors, risk of ESRD for the median donor in the first 20 years postdonation was estimated at 34 cases per 10,000 donors. However, estimated risk varied widely according to donor characteristics, from fewer than seven cases per 10,000 donors (for the 1% of donors at the lowest estimated risk) to at least 256 cases per 10,000 donors (for the 1% of donors at highest estimated risk). In general, male donors, black donors, donors with higher BMI, and donors biologically related to their recipient had greater risk of ESRD. However, the association between age at donation and ESRD risk was modified by donor race. In other words, among nonblack donors, older age was associated with increased risk; however, among black donors, this association did not hold. The absence of increased risk for older black donors may be partly due to a selection effect; among older blacks, individuals predisposed to CKD may manifest decreased eGFR before donor evaluation and thus be screened out before donation.
This study estimated cumulative incidence for the median donor as 16 cases per 10,000 donors at 15 years postdonation, and 34 cases per 10,000 donors at 20 years postdonation. A recent meta-analysis reported pooled cumulative incidence of ESRD at 1.1% (110 per 10,000) among studies that followed donors for at least 10 years postdonation.8 However, this estimate draws on studies with varying follow-up times and of heterogeneous populations of donors from many different countries including South Africa,9 Sweden,10 South Korea,11 Pakistan,12 Singapore,13 and Egypt14 and, as such, may not apply to any specific patient population.
Our findings that male sex and black race are associated with ESRD risk are consistent with a 2008 study by Gibney et al. of 126 living kidney donors who subsequently joined the deceased donor kidney waitlist. This study reported that black donors, male donors, and donors who were under age 35 at the time of donation made up a larger proportion of waitlist registrants than would be expected on the basis of these groups’ proportion in the general population of donors.15 In contrast with our study, the Gibney study suggested that younger age was a risk factor for ESRD. Because the Gibney study ascertained ESRD based only on waitlist registration, inference may have been affected by listing practices and perceived suitability of donors with ESRD for kidney transplantation. Furthermore, the authors did not test the interaction between age and race, and as such their inference about the effect of age was limited to an average, overall effect.
Our findings are broadly consistent with a recently published ESRD risk calculator for white kidney donors from Ibrahim et al.,16 but extended to donors of all races and using a substantially larger population (133,824 versus 3956). The Ibrahim calculator estimates ESRD risk in white donors on the basis of age, BMI, and systolic BP, all measured at time of donation. Both calculators estimate higher risk for older donors (among nonblack donors) and higher risk for donors with greater BMI. The Ibrahim calculator did not include donor sex or relationship to recipient, and was on the basis of a cohort of white kidney donors. Our calculator did not include systolic BP, on the basis of exploratory models showing no statistically significant association between systolic BP and ESRD risk in the national donor cohort. Although our cohort was substantially larger than the cohort used for the Ibrahim calculator, their dataset has longer follow-up for donors with measured systolic BP, whereas our dataset relied on imputation to ascertain BP for donors who donated before 1998. It may be that added risk associated with elevated systolic BP emerges only gradually for living donors. However, predictive discrimination among the national kidney donor population was substantially higher for our model (0.710) than for the Ibrahim calculator (0.567).
Our identification of BMI and donor sex as risk factors for ESRD in living kidney donors was in contrast with a recent national study of ESRD in Norwegian donors and healthy nondonor controls, which reported no association between these characteristics and ESRD risk.3 There are several potential explanations for the discrepancy. Notably, donors made up only 5.5% of the Norwegian cohort; the investigators compared donors to healthy nondonors but did not investigate interaction between donor status and ESRD risk, so associations in this study were likely driven by the much larger nondonor cohort. Also, the Norwegian study had only 34,522 participants (31 ESRD events), whereas our study has 133,824 participants (331 events), allowing for more precise estimation of the association. Differences in risk between Norwegians and Americans (or differences between donor selection in Norway and America) may have affected results. Our study was also able to explore potential risk factors not included in the Norwegian study, including donor race and biologic relationship to the recipient.
A recent KDIGO-led study estimated risk of ESRD in healthy potential donors in the absence of kidney donation (“healthy nondonors”),7 on the basis of donor candidate characteristics. This study projected higher risk of ESRD in blacks than in whites, and higher risk in men than in women (e.g., baseline 15-year risk of ESRD at age 40 was estimated at 0.24% for black men, 0.15% for black women, 0.06% for white men, and 0.04% for white women). However, among donor candidates age≤60 years, increased age was associated with increased risk of ESRD within 15 years, across categories of race and sex (e.g., baseline risk at age 60 was estimated at 0.32% for black men, 0.18% for black women, 0.13% for white men, and 0.08% for white women). The contrast between results from this study and our findings may result from donor selection practices; for example, older blacks at risk of ESRD but classified as “healthy” in the KDIGO study may be more reluctant to donate, or less likely to be cleared for donation. The Grams study reported a relatively modest association between BMI and ESRD risk (HR, 1.16 [95% CI, 1.04 to 1.29] per 5 kg/m2 among individuals with BMI>30). In contrast, in our population a 5-U increase in BMI was associated with 61% higher risk across the range of BMI, suggesting that the effect of obesity on ESRD risk might be worse when living with only one kidney and the physiologic changes that occur postdonation. The KDIGO model has the advantage of a larger population and more covariates. By contrast, our model is limited to the population of people who have actually undergone living donor nephrectomy, and our covariates are limited to those collected by the Organ Procurement and Transplantation Network (OPTN). However, unlike the KDIGO calculator, our calculator estimates actual postdonation risk rather than baseline risk—a critical question both for candidates considering donation, and for living kidney donors wishing to understand and minimize their future risk.
Our study must be understood in the context of its limitations. By definition, our study population consists of individuals who were cleared for donation. In other words, predicted risk for a given donor candidate reflects risk among individuals with similar characteristics who were cleared to donate; risk to an individual with similar characteristics from the general population might be higher. We were only able to study risk factors captured in the national donor registry, meaning that we cannot draw firm inference with regard to characteristics that were only measured in recent years (e.g., serum creatinine, smoking status) or not at all (e.g., glucose tolerance, albumin-to-creatinine ratio). Our estimate of risk associated with BMI relies on multiple imputation, because BMI was missing for 31% of donors. However, misspecification of the imputation model would likely bias toward the null. Despite these limitations, our estimates of ESRD risk on the basis of donor age, sex, race, and BMI improve dramatically upon prior estimates, and provide a usable calculator to help with shared clinical decision-making and to respond to the new KDIGO-recommended acceptable risk paradigm.
Living kidney donors voluntarily undergo surgery for no direct medical benefit to themselves; it is therefore incumbent upon the transplant community to provide donors with accurate estimates of long-term risk to improve shared decision making and to provide clinical decision support in the donor evaluation process. Our risk prediction model can be of use to individuals considering donation, and to living donors and their care providers in planning long-term follow-up care and health maintenance.
Concise Methods
Study Population
This study used data from the Scientific Registry of Transplant Recipients (SRTR). The SRTR data system includes data on all donors, waitlisted candidates, and transplant recipients in the United States, submitted by the members of the OPTN, and has been described elsewhere.17 The Health Resources and Services Administration, US Department of Health and Human Services provides oversight to the activities of the OPTN and SRTR contractors. The study population consisted of living kidney donors in the United States between October 1, 1987 and December 31, 2015 as ascertained from the SRTR database. Donors with missing race or age at donation (n=77; 0.06% of donors) were excluded from analysis.
Outcome Ascertainment
Donors were followed from date of donation to death, ESRD diagnosis, or end of study on December 31, 2015. Death was ascertained through standard OPTN follow-up and via linkage to the Social Security Death Master File. Incident ESRD was ascertained from the Center for Medicare and Medicaid Services (CMS) Form 2728. Although Form 2728 has been available since 1973, reporting of incident ESRD became mandatory for non-Medicare patients in 1994. Because the study population includes donors since 1986, person-time before April 1, 1994 was treated as immortal. In other words, patients who donated before April of 1994 did not contribute person-time to the study until that date, and entered the study on that date as late entries. Donors with documented ESRD before April 1, 1994 (n=7) were excluded from analysis. Donors who were diagnosed with ESRD within 30 days of donation (n=17) were also excluded from analysis, under the assumption that these patients underwent AKI during nephrectomy rather than CKD as a long-term consequence of living with one kidney.
Risk Factors for ESRD
We used Kaplan–Meier curves and logrank tests to compare ESRD incidence across donor subgroups (univariable analysis), and Cox regression to model risk of ESRD in living kidney donors as a function of sex, age, race (classified as black versus nonblack), interaction between age and race, first-degree biologic relationship to recipient, and BMI (multivariable analysis). Because of substantial missingness in BMI (which was not widely collected before 1999), we used multiple imputation with chained equations (20 burn-in iterations and 50 imputations) to account for missing data, accounting for exposure time as per the methods of White and Royston.18
Estimates of 5-, 10-, 15-, and 20-Year ESRD Risk
We calculated predictive discrimination of the model by calculating the Harrell C statistic, using a custom implementation of the Harrell C as previously described.19 For comparison, we also calculated the Harrell C statistic on the ESRD risk calculator for white kidney donors previously published by Ibrahim et al., among the 79,389 donors in our study population with recorded BMI and systolic BP.16 We used baseline hazard curves and HRs obtained from the Cox models described above to calculate estimated cumulative incidence of ESRD at 5, 10, 15, and 20 years as a function of donor characteristics. In other words, given baseline cumulative hazard function H0(t), and coefficient vector β, the cumulative hazard function for a donor with covariate vector X was calculated by H(t) = H0×eβX. Cumulative incidence I at time t was calculated by I(t) = 1−e−H(t). We checked the validity of our models by producing graphs of observed and predicted ESRD, stratified by sex, race, and BMI (in categories of <25, 25–30, and 30–35 kg/m2).
Sensitivity Analyses for Handling of Immortal Person-Time
Because ESRD outcome ascertainment was not comprehensive before start-of-study on April 1, 1994, we treated person-time between date of donation and April 1, 1994 as immortal, as described above. It is likely that a few donors experienced incident ESRD before start-of-study, and did not have their ESRD reported to CMS. Our analysis mistakenly classifies these donors as ESRD-free until death or end-of-study. Therefore, our estimates of ESRD incidence would be biased downward, although the bias was probably very slight because ESRD in the first few years postdonation is a rare outcome. In order to quantify the bias introduced by our methods, we used our Cox models to estimate cumulative incidence of ESRD during immortal person-time for all donors who donated before the beginning of the study period, as a function of donor age, race, and sex. For example, for a donor who donated on April 1, 1990, we calculated estimated cumulative incidence of ESRD 4 years after donation. The sum of these cumulative incidence figures gives an estimate of the number of ESRD cases in donors before start-of-study. We repeated this procedure on 100 bootstrapped samples to obtain a 95% confidence interval for number of missed ESRD cases before April 1, 1994. Among 14,681 donors who donated before that date, the estimated number of unobserved ESRD cases was 1.2. A bootstrap with 100 repetitions gave a 95% confidence interval of 0.7 to 1.7 missed cases. In other words, an estimated 0.01% of our late entries (0.002% of all study participants) may be false negatives (missed ESRD cases); this number is too small to meaningfully affect our estimates of cumulative ESRD incidence.
As an additional sensitivity analysis, we repeated our main analyses using only donors who donated on or after April 1, 1994; inference was consistent with our main findings.
Statistical Analyses
All analyses were performed using Stata 14.1/MP for Windows (College Station, TX).
Disclosures
None.
Acknowledgments
This work was supported by grant numbers K01DK101677, R01DK096008, and K24DK101828 from the National Institute of Diabetes and Digestive and Kidney Diseases.
Versions of this work were previously presented at American Society of Nephrology Kidney Week, November 6, 2015 (San Diego, California); and at the American Transplant Congress, June 12, 2016 (Boston, Massachusetts).
The analyses described here are the responsibility of the authors alone and do not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the United States government. The data reported here have been supplied by the Minneapolis Medical Research Foundation as the contractor for the Scientific Registry of Transplant Recipients. The interpretation and reporting of these data are the responsibility of the author(s) and in no way should be seen as an official policy of or interpretation by the Scientific Registry of Transplant Recipients or the United States government.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
See related editorial, “Synthesizing Absolute and Relative Risks and the Many Unknowns to Inform Living Kidney Donors,” on pages 2559–2561.
References
- 1.Segev DL, Muzaale AD, Caffo BS, Mehta SH, Singer AL, Taranto SE, McBride MA, Montgomery RA: Perioperative mortality and long-term survival following live kidney donation. JAMA 303: 959–966, 2010 [DOI] [PubMed] [Google Scholar]
- 2.Muzaale AD, Massie AB, Wang MC, Montgomery RA, McBride MA, Wainright JL, Segev DL: Risk of end-stage renal disease following live kidney donation. JAMA 311: 579–586, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mjøen G, Hallan S, Hartmann A, Foss A, Midtvedt K, Øyen O, Reisaeter A, Pfeffer P, Jenssen T, Leivestad T, Line PD, Øvrehus M, Dale DO, Pihlstrøm H, Holme I, Dekker FW, Holdaas H: Long-term risks for kidney donors. Kidney Int 86: 162–167, 2014 [DOI] [PubMed] [Google Scholar]
- 4.Ibrahim HN, Foley R, Tan L, Rogers T, Bailey RF, Guo H, Gross CR, Matas AJ: Long-term consequences of kidney donation. N Engl J Med 360: 459–469, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Locke JE, Reed RD, Massie A, MacLennan PA, Sawinski D, Kumar V, Mehta S, Mannon RB, Gaston R, Lewis CE, Segev DL: Obesity increases the risk of end-stage renal disease among living kidney donors. Kidney Int 91: 699–703, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kidney Disease Improving Global Outcomes (KDIGO) Living Kidney Donor Work Group : KDIGO Draft Clinical Practice Guideline on the Evaluation and Follow-up Care of Living Kidney Donors, 2015. Available at http://kdigo.org/home/guidelines/livingdonor. Accessed March 25, 2017 [DOI] [PMC free article] [PubMed]
- 7.Grams ME, Sang Y, Levey AS, Matsushita K, Ballew S, Chang AR, Chow EK, Kasiske BL, Kovesdy CP, Nadkarni GN, Shalev V, Segev DL, Coresh J, Lentine KL, Garg AX; Chronic Kidney Disease Prognosis Consortium : Kidney-failure risk projection for the living kidney-donor candidate. N Engl J Med 374: 411–421, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li SS, Huang YM, Wang M, Shen J, Lin BJ, Sui Y, Zhao HL: A meta-analysis of renal outcomes in living kidney donors. Medicine (Baltimore) 95: e3847, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abdu A, Morolo N, Meyers A, Wadee S, Britz R, Naicker S: Living kidney donor transplants over a 16-year period in South Africa: A single center experience. Ann Afr Med 10: 127–131, 2011 [DOI] [PubMed] [Google Scholar]
- 10.Fehrman-Ekholm I: Living donor kidney transplantation. Transplant Proc 38: 2637–2641, 2006 [DOI] [PubMed] [Google Scholar]
- 11.Kim SH, Hwang HS, Yoon HE, Kim YK, Choi BS, Moon IS, Kim JC, Hwang TK, Kim YS, Yang CW: Long-term risk of hypertension and chronic kidney disease in living kidney donors. Transplant Proc 44: 632–634, 2012 [DOI] [PubMed] [Google Scholar]
- 12.Rizvi SA, Naqvi SA, Jawad F, Ahmed E, Asghar A, Zafar MN, Akhtar F: Living kidney donor follow-up in a dedicated clinic. Transplantation 79: 1247–1251, 2005 [DOI] [PubMed] [Google Scholar]
- 13.Tan L, Tai BC, Wu F, Raman L, Consigliere D, Tiong HY: Impact of kidney disease outcomes quality initiative guidelines on the prevalence of chronic kidney disease after living donor nephrectomy. J Urol 185: 1820–1825, 2011 [DOI] [PubMed] [Google Scholar]
- 14.Wafa EW, Refaie AF, Abbas TM, Fouda MA, Sheashaa HA, Mostafa A, Abo El Ghar MI, Ghoneim MA: End-stage renal disease among living-kidney donors: Single-center experience. Exp Clin Transplant 9: 14–19, 2011 [PubMed] [Google Scholar]
- 15.Gibney EM, Parikh CR, Garg AX: Age, gender, race, and associations with kidney failure following living kidney donation. Transplant Proc 40: 1337–1340, 2008 [DOI] [PubMed] [Google Scholar]
- 16.Ibrahim HN, Foley RN, Reule SA, Spong R, Kukla A, Issa N, Berglund DM, Sieger GK, Matas AJ: Renal function profile in white kidney donors: The first 4 decades. J Am Soc Nephrol 27: 2885–2893, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Massie AB, Kucirka LM, Segev DL: Big data in organ transplantation: Registries and administrative claims. Am J Transplant 14: 1723–1730, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.White IR, Royston P: Imputing missing covariate values for the Cox model. Stat Med 28: 1982–1998, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Massie AB, Leanza J, Fahmy LM, Chow EK, Desai NM, Luo X, King EA, Bowring MG, Segev DL: A risk index for living donor kidney transplantation. Am J Transplant 16: 2077–2084, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]