Abstract
Purpose
Intensive therapies in pediatric malignancies increased survival rates but also occurrence of treatment-related morbidities. Therefore, supportive care fulfills an increasingly important role. In planning development of guidelines with incorporation of shared decision making, we noticed that little is known about the needs and preferences of patients and their parents. Our goals were therefore to investigate (1) which supportive care topics patients and parents regard as most important and (2) the preferred role they wish to fulfill in decision making.
Methods
This qualitative study consisted of three focus groups (two traditional, one online) with patients and parents of two Dutch pediatric oncology centers. Data were transcribed as simple verbatim and analyzed using thematic analysis.
Results
Eleven adolescent patients and 18 parents shared detailed views on various aspects of supportive care. Themes of major importance were communication between patient and physician (commitment, accessibility, proactive attitude of physicians), well-timed provision of information, and the suitability and accessibility of psychosocial care. In contrast to prioritized supportive care topics by medical professionals, somatic issues (e.g., febrile neutropenia) were infrequently addressed. Patients and parents preferred to be actively involved in decision making in selected topics, such as choice of analgesics and anti-emetics, but not in, e.g., choice of antibiotics.
Conclusions
Children with cancer and parents were provided a valuable insight into their views regarding supportive care and shared decision making. These results have important implications towards improving supportive care, both in selecting topics for guideline development and incorporating preferences of patients and parents herein.
Electronic supplementary material
The online version of this article (doi:10.1007/s00520-017-3723-7) contains supplementary material, which is available to authorized users.
Keywords: Supportive care, Pediatric oncology, Focus group, Shared decision making, Evidence-based guidelines, Patient involvement
Introduction
During the previous five decades, the five-year survival rates for children with cancer in Europe and the USA have risen to more than 80% for all childhood cancer types combined [1–4]. However, these improvements have led to a growing population of patients (and survivors) experiencing short- and long-term treatment-related diseases and side effects [5–7]. These morbidities may even lead to delays, lowering or premature termination of treatment, consequently reducing individual survival chances, and hence increasing mortality [8–10].
Supportive care (SC), which comprises management of both physical and psychological side effects of treatment, fulfills an important role in reducing morbidity and mortality and increasing quality of life, and should thus be optimized [11, 12]. To provide optimal SC, clinical practice should be based upon the best evidence available. To achieve this transition of evidence to practice, development of clinical practice guidelines (CPG) is needed. A CPG is defined as “a statement that includes recommendations intended to optimize patient care that are informed by a systematic review of evidence and an assessment of the benefits and harms of alternative care options” [13]. Currently, most guidelines in SC in childhood cancer are not evidence-based, contradictory, or outdated [14–16]. Well-developed, evidence-based guidelines in this area are limited to febrile neutropenia and nausea/vomiting [17–19].
In order to prioritize SC topics for the development of CPGs, the opinion of medical professionals has previously been determined [20]. Following this, we aimed to explore views of patients and parents using focus groups to determine which SC topics they regard as most important, as we consider it essential to incorporate this in our CPG development project. The decision for a qualitative research (QR) method (e.g., in-depth interviews, focus groups (FGs)) instead of quantitative research was based on the more explanatory and flexible nature of QR to generate subjective and profound information from poorly explored areas [21–24]. Within QR, FGs are often used in healthcare research and considered most suitable to elicit information about the norms and experiences of a group and are thus applicable to generate a broad overview of topics of interest [23, 25, 26].
Over the last two decades, a global trend has grown towards shared decision making (SDM) and acknowledging children’s right to participate in matters that affect them [27]. Since pediatric oncology treatment has become increasingly complex, patients and their families are more frequently faced with complicated treatment decisions [28]. Studies on parents of children with cancer showed that autonomy-based health care is preferred over a paternalistic approach [29, 30]. However, it was shown that currently adolescent patients fulfilled a minimal role in SDM but desired information on treatment decisions [31]. To facilitate SDM, knowledge of patients’ and parents’ preferred involvement in decision making should be incorporated within CPGs.
Therefore, the aim of this study was bipartite:
To determine which topics within SC pediatric cancer patients and their parents regard as important
To investigate the role pediatric cancer patients and their parents wish to fulfill in SC decision making
Methods
Study population
This study was conducted in the University Medical Center Groningen (UMCG) and the Academic Medical Center (AMC) Amsterdam between April 2015 and December 2015. The pediatric oncology departments in both hospitals each have approximately 90 new patients per year. The psychosocial care team (psychologists, social workers, and child life specialists) covers five full time equivalents (FTEs) in the AMC, compared to three FTEs in the UMCG.
We conducted separate FG meetings among patients and parents since we expected that in these groups different topics and priorities would be discussed. During the study, recruitment of adolescent patients for a live meeting proved to be problematic for personal and organizational reasons (e.g., patients prioritized other activities on the day of the FG meetings). Hence, we conducted two traditional focus groups (TFGs) with parents and one more adolescent-appropriate online focus group (OFG) with adolescent patients [25].
Parents in the TFG were eligible to participate if their child was 0–18 years at the time of diagnosis of childhood cancer; patients in the OFG were eligible if they were aged 12–18 years at time of diagnosis. All patients and children of the parents had to be on treatment for a minimum of 2 months at the time of selection or within 6 months after termination of treatment. To create FGs as diverse as possible, purposeful sampling based on diagnosis, age, and duration of treatment was performed by oncologists from the participating centers and via the patient organization ‘Dutch Cancer Association for Children and Parents’ (VOKK) [32]. As a token of appreciation, all participants (both parents and patients) received a gift card.
This study was approved by the Medical Ethical Committee of the UMCG.
Focus group design, data collection, and analysis
In a TFG, six to ten persons are led through an open discussion by an experienced and neutral moderator to examine a specific topic or set of issues [33–35]. In an OFG, for instance, a secured online forum, participants anonymously respond to posted topics and to the comments of the moderator and fellow participants [25]. In this study, we conducted two 2 hours TFGs that were moderated by a social psychologist with extensive TFG-moderator experience. The moderator was fully informed by the researchers about the topic and the study aims. Two researchers attended the TFGs to take notes and assist the moderator if necessary. The moderator and researchers were unacquainted with the parents. Questions were composed by the researchers and checked and revised by the social psychologist to ensure that all questions were open, broadly formulated, applicable to the target group, and in line with the research objectives (Table 1). While we did complete a prior SC prioritization effort among medical professionals, these outcomes were not taken into account when composing the FG questions [20]. This approach was chosen as we believed it was essential to get a clear and an unbiased overview of insights and to explore differences in preferred SC topics among patients and parents versus medical professionals. Before the TFGs, all parents completed a short socio-demographic questionnaire. A local childhood oncologist attended the first 15 min of the TFGs to inform parents about SC and the aims of the study. Thereafter, the moderator introduced the FG procedure in general and the ground rules (e.g., speaking one by one).
Table 1.
Semi-structured discussion guide used in the traditional focus group sessions (TFG)
| Opening question |
| - Could you introduce yourself and share your child’s diagnosis with us? |
| Key questions |
| Objective 1. To determine which topics within supportive care patients and parents regard as important |
| - How did you experience supportive care? |
| - What went well in the current supportive care, what went wrong? And why did this go well/wrong? |
| - What do you miss in the current supportive care? |
| - What topics often caused confusion between different doctors/nurses or different hospitals? |
| - What would you like to change in these topics in the supportive care? |
| Objective 2. To investigate the role pediatric cancer patients and their parents wish to fulfill in supportive care decision making |
| - Which role have you played in making decisions in supportive care? |
| - Which role would you like to play in making decisions about treatment? |
| - With which topics would you like to think along with doctors/nurses and with which topics would you not? |
| - Would you appreciate it to talk separately from your child with the doctor regarding some topics and if so, which topics? |
| Final questions |
| - Do you have any other comments? |
| - Are there any topics you would like to address, which we have not talked about? |
The OFG was performed using a specifically designed, secured online forum. To ensure anonymity during the OFG, all 11 patients received a personal, anonymous login name and password and were asked not to mention names or share private information. The questions asked in the OFG were derived from overarching principal themes identified from the TFGs to ensure continuity of topics and to be able to compare the outcomes (Table 2). We posted an opening question to inform patients about SC, the aims of the study, and the procedure. During a 2-week period, each weekday at 10:00 a.m., we posted a new question with a short explanation. A moderator actively participated in the OFG to ask for clarification in case of ambiguous comments and to encourage non-responding patients.
Table 2.
Topics with explanation as posted on the forum at the OFG
| Day 1 Care in the hospital |
| Explanation A lot happens at the hospital in the area of supportive care: You receive medication for pain or nausea, you talk with psychosocial staff (such as a teaching assistant, or perhaps a psychologist), you get your food at the pediatric oncology ward, you have to get to the operation center in isolation, and so on. Would you like to share your experience in the hospital? This should of course be both positive and negative. You can talk about anything, about the hospital, both the clinic and the department(s), the emergency department, the operations center, the pharmacy, and so on. Question In the hospital, a lot happens in addition to the main treatment (giving chemotherapy, radiation therapy). What do you experience? And how do you feel about it? |
| Day 2 Care at home* |
| How do you manage things at home on the area of supportive care? |
| Day 3 Communication* |
| What do you think of the way people communicate with you? |
| Day 4 Provision of information* |
| Are you satisfied with the information you get and questions people ask you? And what do you think of the ways you get this information? |
| Day 5 Psychosocial care* |
| Psychosocial care is all about how you feel, emotionally and socially. How do you experience this type of care? |
| Day 6 Physical care* |
| How do you experience the physical medical care? |
| Day 7 Shared decision making* |
| Which role do you prefer to play in making decisions about supportive care during your treatment? |
| Day 8 Remaining topics* |
| Are there any other things related to the care for your illness that you would like to share? |
*Each question was posted along with an explanation. Above, only the explanation of day 1 is showed
Both TFG meetings were audio recorded using a digital Tascam DR-100 MKII audio recorder and the record function on a mobile phone as backup. These audio recordings were transferred to a secured computer and deleted from both devices after the meetings ended in order to guarantee privacy. Subsequently, the audio files were loaded into the application ATLAS.ti version 7.5.6 (Cleverbridge AG, Berlin, Germany) to be transcribed as simple verbatim. After transcription, transcripts were proofread by one researcher (LT) to eliminate major typographical errors. Qualitative data from the OFG were copied from the secured forum and incorporated in ATLAS.ti.
Thereafter, all transcripts were thoroughly read, and thematic analysis was performed to identify recurring topics and to create meaningful themes within the data [36, 37]. Themes were converted into codes and then organized into larger clusters. Subsequently, each quote was coded by using this coding scheme and on its overall assessment of care (positive, negative, or neutral) by two researchers (LT, EL) independently. A quote could be labeled with one or more codes since a quote could fit within more than one category. Corresponding codes were retained in the combined document while dissimilar codes were discussed until consensus was reached (third party arbitration was not necessary). Regarding ranked importance of topics, we decided to compose a quantitative ranking list using the numerical frequency of occurrence of the codes.
Results
Participants
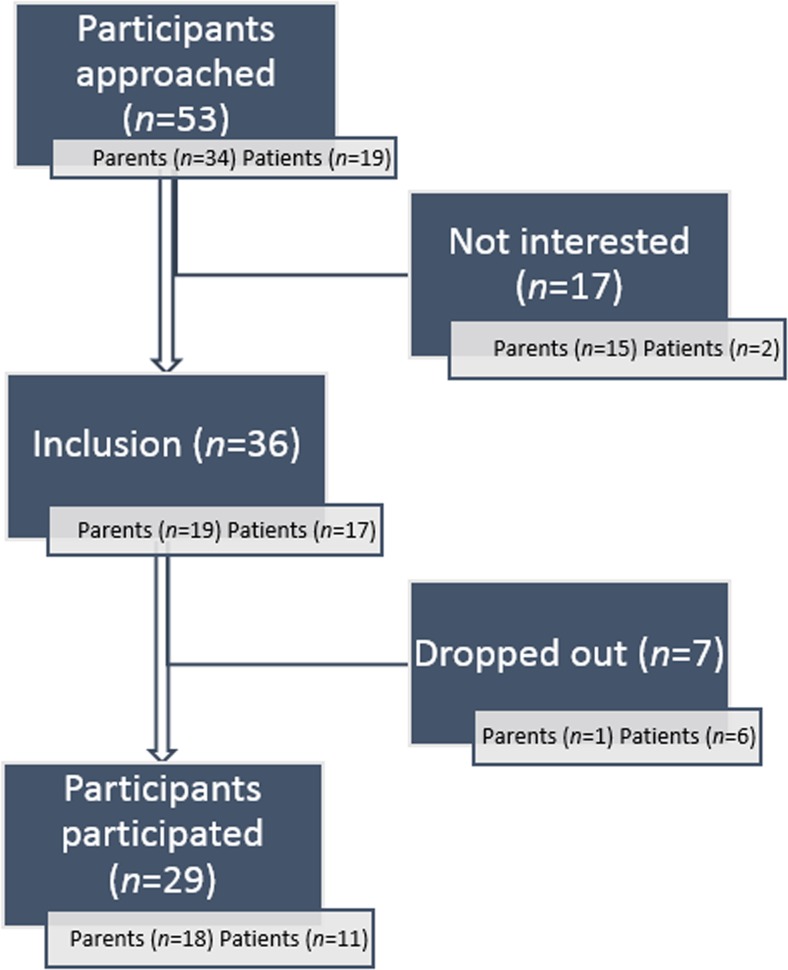
In total, 53 parents and patients were approached of which 29 (54.7%) eventually participated (Fig. 1). Nine fathers and nine mothers with a median age of 44 years (range 29 to 56 years) attended the TFGs (Table 3). Most of them were parents of a child diagnosed with acute lymphoblastic leukemia (ALL, n = 9, 50.0%). The median period of treatment was 13 months (range 3 to 66 months). Five girls and six boys with a median age of 15 years (range 12 to 18 years and a median period of treatment of 23.5 months, range 2 to 27) participated in the OFG. Most of them (n = 6, 54.5%) suffered from ALL.
Fig. 1.
Flow chart shows the results of participant selection
Table 3.
Demographics of participants
| Traditional focus groups (parents) |
Online focus group (patients) |
|
|---|---|---|
| Gender | ||
| Male | 9 (50.0%) | 6 (54.5%) |
| Female | 9 (50.0%) | 5 (45.5%) |
| Age (years) | ||
| Median, range | 44 (29.0–56.0)a | 15 (12.0–18.0)b |
| Age child (in years) | ||
| Mean, range | 11.5 (3–18) | |
| Diagnosis (child) | ||
| ALL | 9 (50.0%) | 6 (54.5%) |
| Bone tumor | 2 (11.1%) | 1 (9.1%) |
| GCT | 1 (5.5%) | 0 (0.0%) |
| Brain tumor | 2 (11.0%) | 1 (9.1%) |
| STT | 4 (22.0%) | 3 (27.3%) |
| Period of treatment (months) | ||
| Mean + range | 17.2 (3–66) | 18.9 (2–27) |
| Highest level of educationc | ||
| Low | 5 (27.8%) | 10 (90.9%) |
| Intermediate | 6 (33.3%) | 1 (9.1%) |
| High | 7 (38.8%) | 0 (0.0%) |
| Place of residenced | ||
| Village | 10 (55.6%) | 6 (54.5%) |
| City | 8 (44.4%) | 5 (45.5%) |
| Total number of children | ||
| 1 | 4 (22.2%) | |
| 2 | 7 (38.9%) | |
| 3 | 3 (16.7%) | |
| 4 | 4 (22.2%) | |
| Marital status (parents) | ||
| Married | 17 (94.4%) | |
| Cohabiting | 1 (5.5%) | |
Within the sample of 18 parents, three parent-parent couples and three child-parent couples were included leading to the characteristics being included in the descriptive statistics twice. These data have been included in the descriptive statistics since this analysis concerns participants’ backgrounds, and their judgments are correlated with this
SD standard deviation, ALL acute lymphatic leukemia, GCT germ cell tumor, STT soft tissue tumor
aAge at 1 April 2015
bAge at 1 December 2015
cHighest education is reported. Low = primary education, general secondary education; Intermediate = secondary vocational education; High = higher vocational education and university
dA place of residence with a population >50,000 inhabitants is labeled as a city
Determination of important topics
Characteristics of the responses are shown in Table 4. Fifty-six codes were described and organized in five larger clusters: care in the hospital (q = 247, q = number of quotations), communication (q = 214), psychosocial care (q = 175), care at home (q = 104), and somatic care (q = 80). Thereafter, 826 quotations were coded by the coding scheme as showed in Table 5. The assessment of care was quoted as negative (q = 453), positive (q = 332), or neutral (q = 52). The topic concerning communication between physician and patients was quoted as both most negative (q = 34) and most positive (q = 35). In general, parents’ quotes were more often labeled as negative than patients’ quotes (64.1 and 23.4%, respectively). Topics at which there was clear and quick consensus among the participants were “exchange tips among parents” (negative; currently few facilities to do so), “communication between different departments” (negative; currently miscommunication on treatment agreements), and “communication on nutritional advice” (negative; currently lack of nutritional guidelines). For practical reasons, the ten most quoted codes are represented below; the full and detailed description of all codes is available in the supplemental data.
Table 4.
Characteristics of response in both focus groups
| TFG | OFG | |||
| Total number of quotes/postings | 643 | 76 | ||
| Quotes/postings per topica | 11.5 (1–28) | 9.5 (2–14) | ||
| Total participants | 18 | 17 | ||
| Active participants | 18 | 11 | ||
| Quotes/postings per participanta | 35.7 | 4.5 (1–11) | ||
| Average time spent on the foruma | 39.6 min (0.6 min–78 min) | |||
| Total views | 284 | |||
| Views per topica | 38.5 (4–66) | |||
| Day | Topic | Quotes | Views | |
| Day 1 | Care in the hospital | 10 | 66 | |
| Day 2 | Care at home | 14 | 58 | |
| Day 3 | Communication | 9 | 42 | |
| Day 4 | Provision of information | 8 | 35 | |
| Day 5 | Psychosocial care | 8 | 36 | |
| Day 6 | Physical care | 7 | 34 | |
| Day 7 | Shared decision making | 7 | 36 | |
| Day 8 | Remaining topics | 2 | 11 | |
Data includes the topic on “remaining comments,” does not include the topic “questions,” and includes non-reacting participants. As one quote was classified by several codes, the number of coded quotes is not equal to the total number of quotes
aReported are means and ranges
Table 5.
Number of quotes per code
| Code | BFGs | TFG | OFG | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Total | Value assessment | Total | Value assessment | Total | Value assessment | ||||
| + | − | + | − | + | − | ||||
| 1. Care in the hospital | |||||||||
| Care at the departments | |||||||||
| Pediatric oncology ward | 36 | 12 | 11 | 27 | 5 | 9 | 9 | 7 | 2 |
| Outpatient clinic of pediatric oncology | 23 | 16 | 2 | 15 | 9 | 1 | 8 | 7 | 1 |
| Emergency department | 17 | 5 | 14 | 13 | 0 | 14 | 4 | 5 | 0 |
| Operation center | 10 | 0 | 7 | 10 | 0 | 7 | 0 | 0 | 0 |
| Single day admission | 4 | 2 | 2 | 4 | 2 | 2 | 0 | 0 | 0 |
| Facilities at the hospital | |||||||||
| Comfort for parents | 21 | 5 | 14 | 21 | 5 | 14 | 0 | 0 | 0 |
| Privacy (e.g., room layout) | 20 | 2 | 16 | 19 | 2 | 15 | 1 | 0 | 1 |
| Hygiene | 11 | 1 | 11 | 11 | 1 | 11 | 0 | 0 | 0 |
| Parking | 6 | 0 | 6 | 6 | 0 | 6 | 0 | 0 | 0 |
| Comfort for the patient | 5 | 2 | 2 | 5 | 2 | 2 | 0 | 0 | 0 |
| Making decisions at the hospital | |||||||||
| Management of medication | 23 | 16 | 6 | 22 | 9 | 6 | 1 | 7 | 0 |
| Management of nutrition | 6 | 0 | 6 | 6 | 0 | 6 | 0 | 0 | 0 |
| Waiting time at the hospital | 21 | 6 | 14 | 20 | 5 | 13 | 1 | 1 | 1 |
| Intervene in treatment | 16 | 1 | 8 | 16 | 1 | 8 | 0 | 0 | 0 |
| Movement and activation | 11 | 2 | 7 | 10 | 2 | 7 | 1 | 0 | 0 |
| Exchange tips among parents | 10 | 0 | 7 | 10 | 0 | 7 | 0 | 0 | 0 |
| Patient record management | 7 | 0 | 7 | 7 | 0 | 7 | 0 | 0 | 0 |
| Total care in the hospital | 247 | 70 (33.3%) | 140 (66.7%) | 222 | 43 (24.1%) | 135 (75.8%) | 25 | 27 (84.3%) | 5 (15.6%) |
| 2. Communication | |||||||||
| Within the hospital, between: | |||||||||
| physician and patient | 42 | 34 | 35 | 28 | 13 | 28 | 14 | 21 | 7 |
| nurse and patient | 17 | 16 | 17 | 8 | 8 | 14 | 9 | 8 | 3 |
| physician and physician | 11 | 1 | 10 | 11 | 1 | 10 | 0 | 0 | 0 |
| different departments | 10 | 0 | 7 | 10 | 0 | 7 | 0 | 0 | 0 |
| patient and other staff | 9 | 1 | 4 | 9 | 1 | 4 | 0 | 0 | 0 |
| physician and nurse | 5 | 1 | 6 | 5 | 1 | 6 | 0 | 0 | 0 |
| Provision of information | 41 | 11 | 21 | 26 | 3 | 18 | 15 | 8 | 3 |
| Shared decision making | 22 | 19 | 5 | 14 | 11 | 4 | 8 | 8 | 1 |
| Separate consultation (child/parent) | 19 | 13 | 3 | 16 | 11 | 3 | 3 | 2 | 0 |
| Communication between hospitals | 14 | 3 | 7 | 14 | 3 | 7 | 0 | 0 | 0 |
| Case-manager | 11 | 1 | 10 | 11 | 1 | 10 | 0 | 0 | 0 |
| Nutritional advice | 10 | 0 | 8 | 10 | 0 | 8 | 0 | 0 | 0 |
| Between GP and oncologist | 3 | 1 | 1 | 3 | 1 | 1 | 0 | 0 | 0 |
| Total communication | 214 | 101 (43.0%) | 134 (57.0%) | 165 | 54 (31.0%) | 120 (69.0%) | 49 | 47 (77.0%) | 14 (23.0%) |
| 3. Psychosocial care | |||||||||
| Psychosocial support | |||||||||
| For patient | 30 | 22 | 13 | 20 | 10 | 8 | 10 | 12 | 5 |
| By specialized psychosocial care | 25 | 21 | 15 | 17 | 11 | 10 | 8 | 10 | 5 |
| For parents | 17 | 6 | 10 | 17 | 6 | 10 | 0 | 0 | 0 |
| By social workers | 17 | 4 | 14 | 15 | 3 | 13 | 2 | 1 | 1 |
| By child life specialists | 12 | 6 | 7 | 6 | 5 | 5 | 6 | 1 | 2 |
| For siblings | 10 | 6 | 1 | 10 | 6 | 1 | 0 | 0 | 0 |
| Difference between child and adolescent | 4 | 0 | 4 | 4 | 0 | 4 | 0 | 0 | 0 |
| Empathy | |||||||||
| Of nurses | 20 | 3 | 11 | 18 | 2 | 10 | 2 | 1 | 1 |
| Of physicians | 15 | 4 | 9 | 10 | 3 | 7 | 5 | 1 | 2 |
| Of the environment | 13 | 10 | 3 | 4 | 3 | 1 | 9 | 7 | 2 |
| Of other professionals | 12 | 4 | 3 | 9 | 3 | 3 | 3 | 1 | 0 |
| Total psychosocial care | 175 | 86 (48.9%) | 90 (51.1%) | 130 | 52 (41.9%) | 72 (58.1%) | 45 | 34 (65.4%) | 18 (34.6%) |
| 4. Care at home | |||||||||
| School | 23 | 15 | 5 | 11 | 6 | 3 | 12 | 9 | 2 |
| Movement and activation | 23 | 13 | 5 | 13 | 7 | 3 | 10 | 6 | 2 |
| Nutrition at home | 17 | 1 | 7 | 17 | 1 | 7 | 0 | 0 | 0 |
| Treatment options at home | 17 | 11 | 8 | 13 | 7 | 6 | 4 | 4 | 2 |
| Role of GP | 15 | 11 | 2 | 15 | 11 | 2 | 0 | 0 | 0 |
| Restrictions in daily life and activities | 9 | 4 | 4 | 8 | 3 | 4 | 1 | 1 | 0 |
| Total care at home | 104 | 55 (64.0%) | 31 (36.0%) | 77 | 35 (58.3%) | 25 (41.7%) | 27 | 20 (77.0%) | 6 (23.0%) |
| 5. Somatic care | |||||||||
| Nutrition at the hospital | 16 | 3 | 16 | 14 | 3 | 15 | 2 | 0 | 1 |
| General somatic care | 15 | 3 | 5 | 9 | 1 | 5 | 6 | 2 | 0 |
| Nutrition | 14 | 3 | 11 | 13 | 2 | 11 | 1 | 1 | 0 |
| Nausea-vomiting | 13 | 5 | 9 | 7 | 0 | 9 | 6 | 5 | 0 |
| Pain | 7 | 6 | 4 | 2 | 2 | 4 | 5 | 4 | 0 |
| Fatigue | 6 | 6 | 1 | 0 | 0 | 0 | 6 | 6 | 1 |
| Muscle weakness and reduction of strength | 5 | 4 | 2 | 0 | 0 | 0 | 5 | 4 | 2 |
| Infection | 3 | 0 | 5 | 3 | 0 | 5 | 0 | 0 | 0 |
| Anemia | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 0 |
| Total somatic care | 80 | 30 (35.7%) | 54 (64.3%) | 49 | 8 (13.8%) | 50 (86.2%) | 31 | 22 (84.6%) | 4 (15.4%) |
| Total | 826 | 332 (42.3%) | 453 (57.7%) | 648 | 175 (30.2%) | 405 (69.8%) | 178 | 157 (76.6%) | 48 (23.4%) |
Number of quotes per code. Note 1: As one quote was classified by several codes, the number of coded quotes is not equal to the total number of quotes. Note 2: The total number of quotations is not necessarily the sum of all positive and negative quotations; quotes are double valued at times. Neutral quotations are not shown
FGs both focus groups, + = positive assessment of care, − = negative assessment of care
Care in the hospital
Regarding the pediatric oncology ward and outpatient clinic, participants (both patients and parents) felt that they were sufficiently cared for. Participants felt at home when they visited the pediatric oncology ward, the outpatient clinic, and the single day admission. In contrast, participants missed a stimulus to be physically active, e.g., dinner was currently often served in bed instead of at the table. Regarding comfort, parents felt that a quiet place to conduct private conversations and a sufficient, clean, and private cooking facilities were important. To reduce waiting time, participants appreciated that several appointments in the hospital were clustered, and that arrangements were made to visit the pediatric oncology ward immediately in case of an emergency.
Communication
Participants were satisfied with the communication they received from physicians. The commitment, accessibility, explaining, and proactive attitude in decisions about treatment and treatment options strengthened their relationship. Participants positively valued that information on diagnosis, and treatment was provided in a phased manner, adapted to the stage they were in. However, practical information, such as available forms of administering medicines, was often provided too late. Participants acknowledged there was great demand for information at the beginning of the process, but little energy and time to search for it.
Psychosocial care
Patients shared that they had to cope with a great deal, especially during the first weeks of treatment. The support provided by physicians, nurses, and social workers through talking about positive things was appreciated. Furthermore, participants expressed that physicians frequently asked how they felt mentally and appreciated that they could always contact the physician. Participants felt physicians would notice it when they did not feel well.
Many patients and some parents reported to have searched for specialized psychological support during various stages of treatment. They were satisfied with the specialized psychological support from both the hospital and the specialized psychological centers. However, making an appointment with a psychologist was often difficult. Participants regretted the absence of a periodic assessment regarding whether the patient, parents, or siblings had psychological needs. Furthermore, since the need for support varied with age and phase of treatment, patients shared that psychosocial care should adapt to these differences.
“Well , I expected some more guidance from the child life specialists with my daughter. We had bad luck with changing psychologists so we had about 6 different people. We receive the beads from her but, well, she doesn’t ask, gosh can we do something for you? I truly expected that they would be more involved.”
41-year-old mother of a nine-year-old son suffering from ALL
Care at home
All participants viewed going to school as very important since at school they did not feel like a patient and could interact with their classmates. Hospitalization and fatigue were the most frequent reasons for them being absent. Proper arrangements on attending school were made, and various solutions were invented to allow classes to be followed from home or the educational provision at the hospital.
“At school, everything is arranged really well. If I have to go to the hospital for chemotherapy or a dose, I can easily go without any problems. All teachers are aware and understand if I want to leave class, for a breath of fresh air for example.”
18-year-old patient suffering from ALL
The degree of suffering from side effects such as fatigue and loss of strength varied among patients. All patients agreed that physical therapy helped to restore their strength. They felt that their physical condition was properly taken into account at school and at sport clubs, resulting in participation in sports practice as much as possible. In contrast, parents of adolescent patients experienced difficulties in motivating their child to be more physically active and wished to receive more support.
Somatic care
This topic was scarcely mentioned. Full and detailed descriptions of these codes are available in the supplemental data.
Determination of topics concerning shared decision making
The preferred role in SDM was investigated by analysis of the following five codes: “shared decision making,” “decisions concerning medication,” “decisions concerning nutrition management,” “intervening in treatment,” and “treatment options at home.” In all FGs, participants appreciated autonomy and active involvement in making decisions about their/child’s treatment, particularly regarding decisions about medications to diminish side effects (e.g., analgesics). Participants often consulted the physician to discuss a medical decision and were satisfied with the non-compelling way of receiving information and the options they were offered, such as composing personalized medication schemes. Regarding specific types and doses of medication (e.g., antibiotics in febrile neutropenia), participants relied on and trusted the physicians’ advice, since they felt of lack sufficient knowledge. Participants shared that they preferred to manage the administration of medication and nutrition on their own behalf and desired time without interference of health care professionals, both at home and at the hospital. Regarding care in the hospital (e.g., administration of medication), several parents felt they had to be constantly aware (and to explicitly check) that care was being performed as agreed upon.
Discussion
To our knowledge, this is the first study that explores the experiences, needs, and preferences regarding SC of children with cancer and their parents. Themes of major importance were communication between patient and physician (i.e., the accessibility and proactive attitude of physicians), the well-timed and balanced provision of information, psychosocial care, and facilities to be physically active. A notable finding was the emphasis of parents on practical aspects, such as room layout and privacy, parking facilities, and hygiene. In contrast to prioritized SC topics by medical professionals, somatic issues such as anemia and infections were infrequently addressed, with the exception of nutritional issues [20].
With regard to SDM, patients and parents shared to fulfill an active role in decision making regarding the use of medication to diminish side effects at home and in the hospital and wished this to remain so. This is in accordance with previous research in the field of pediatric palliative care [29]. The provision of well-timed, complete, and accurate information is considered to be a major condition for achieving SDM, which is in line with previously published work on provision of care to parents of children with cancer [38]. As participants felt to have insufficient knowledge on specific types of medication (e.g., antibiotics), they relied on and trusted the physicians’ advice. Some parents did however wish to be involved in checking medication (i.e., agreed type and dose) in the hospital before it was administered to their child.
Interestingly, patients addressed somatic topics, empathy of the social environment, and going to school relatively more often than parents. Furthermore, quotes concerning fatigue, muscle weakness, and reduction of strength were made exclusively by patients, probably because parents can only estimate these from observation.
Notably, with 76.6% of patient’s quotes and only 27.7% of parent’s quotes assessed as positive, patients appeared to be more positive towards the supportive care they received. This might be explained by the more structured and closed nature of OFGs and the fact that various parents made assenting quotes on certain negative topics. Remarkably, communication between physician and patients was quoted both most negative and positive, which could be explained by the large amount of engagement on this topic.
Although these data were collected in the context of guideline development, participant’s insights and suggestions were often practical and easy to implement. Therefore, the feedback including practical improvements was shared with the participating pediatric oncology wards. Organizing discussion groups could thus function as an evaluation of SC in general. In addition, parents mentioned that they liked sharing experiences and tips with parents in the same situation. Conducting support groups could therefore be of great value for this population.
Although this study provides an interesting insight into patients’ and parents’ experiences, needs, and preferences, it naturally has its limitations. The selection of importance of topics on the basis of a number of quotations may affect validity. The most frequently quoted codes were not automatically implied to be the most important since there may be important issues which participants quickly agreed upon (either in a positive or negative way) and which were thus not selected quantitatively as of major importance. Nevertheless, we felt this approach was most appropriate and provided the best insight into the large amount of qualitative data.
Another limitation of this study concerned the possible selection bias that arose by the purposeful selection of participants. This was however necessary to ensure diversity in composition (e.g., in living environment, age) of the relatively small groups. Approximately, half of all participating patients and children of participating parents were diagnosed with ALL, which could have caused bias. On the other hand, since ALL is the most common childhood cancer, this study provides a reflection of daily practice [1]. As patients below 12 years were not included for practical reasons (e.g., difficulties in communicating online) and to ensure unity within the OFG, this study only represented insights of these patients by proxy (their parents). Half of all included parents had a child below the age of 12 years.
Moreover, it should be taken into account that needs are likely to change in the process of treatment, and this study provides a status quo description of needs and preferences. However, by purposefully sampling participants at various stages in this continuum, insight into their needs from various angles was ensured.
Since questions asked in the OFG were set in advance, it is likely that less free association arose than in the TFGs. Also, we did not pilot these questions which might have affected their quality. However, all questions were checked and revised by the social psychologist with broad FG experience to ensure quality and appropriateness. Furthermore, it is important to realize that in the OFG setting, the emotions and benefits of conversation (e.g., fast interaction, non-verbal signs) were missed, which potentially caused an incomplete scope of the content. To overcome this, patients were invited to make any sort of comment since the questions raised at the OFG were broadly formulated, and the moderator frequently asked them to elucidate their comments.
In conclusion, this study provides an important insight into patients’ and parents’ views regarding SC and their preferred role in SDM. Themes of major importance were communication (i.e., commitment, accessibility, explaining, and proactive attitude by physicians) and the well-timed provision of information. To improve SC, a larger range of possibilities for psychosocial care for both patients and parents should be ensured. Furthermore, to save time and diminish frustrations, practical aspects of care should be improved (e.g., hygiene and making an appointment with the child life specialists or psychologist).
With regard to SDM, this study provides a worthy addition to the scarce knowledge regarding SDM in childhood oncology. Patients and parents were generally actively involved in SDM concerning medication management (e.g., anti-emetics) and wished to remain so. It is noteworthy that patients and parents in some specific somatic issues (e.g., febrile neutropenia) relied on the physicians’ choice with regard to the specific type and dose of medication and were not interested to be involved in these decisions. Overall, healthcare professionals should take time to adjust the care as much as possible to the preferences of the child and his/her parents.
Regarding our aims, each described topic yielded important implications for both clinical practice and the development of CPGs. CPGs in SC can now be developed with the prioritization of the professionals in mind and incorporating the preferences of patients and parents. In addition, these results led us to believe that each CPG should incorporate specific sections on SDM, thereby increasing their quality and practical applicability. Summarizing, we believe that this study is a step towards high-quality patient-centered CPG development improves SC in childhood cancer.
Electronic supplementary material
(DOCX 33 kb).
Acknowledgements
We would like to thank all children and parents who participated in the various focus groups. Also, we would like to thank social psychologist P.H.J. van Haaren for his contribution to this study as TFG moderator.
Compliance with ethical standards
Funding source
The project “Towards evidence-based guidelines for supportive care in childhood oncology” is supported by the Alpe d’HuZes foundation/Dutch Cancer Society (RUG 2013–6345).
Conflicts of interest
The authors declare that they have no conflict of interest.
Footnotes
L. J. A. Tenniglo and E. A. H. Loeffen contributed equally to this work
Electronic supplementary material
The online version of this article (doi:10.1007/s00520-017-3723-7) contains supplementary material, which is available to authorized users.
References
- 1.Meulepas JM, Kiemeney LALM (2011) Kanker in Nederland tot 2020 Trends en prognoses. Signaleringscommissie Kanker van KWF Kankerbestrijding ;H28
- 2.Pritchard-Jones K, Kaatsch P, Steliarova-Foucher E, Stiller CA, Coebergh JW. Cancer in children and adolescents in Europe: developments over 20 years and future challenges. Eur J Cancer. 2006;42(13):2183–2190. doi: 10.1016/j.ejca.2006.06.006. [DOI] [PubMed] [Google Scholar]
- 3.Gatta G, Botta L, Rossi S, Aareleid T, Bielska-Lasota M, Clavel J, et al. Childhood cancer survival in Europe 1999-2007: results of EUROCARE-5—a population-based study. Lancet Oncol. 2014;15(1):35–47. doi: 10.1016/S1470-2045(13)70548-5. [DOI] [PubMed] [Google Scholar]
- 4.Ward E, DeSantis C, Robbins A, Kohler B, Jemal A. Childhood and adolescent cancer statistics, 2014. CA Cancer J Clin. 2014;64(2):83–103. doi: 10.3322/caac.21219. [DOI] [PubMed] [Google Scholar]
- 5.Möller TR, Garwicz S, Barlow L, Falck Winther J, Glattre E, Gudridur O, et al. (2001) Decreasing Late Mortality Among Five-Year Survivors of Cancer in Childhood and Adolescence: A Population-Based Study in the Nordic Countries. J Clin Oncol:3173–3181 [DOI] [PubMed]
- 6.Lipshultz SE, Colan SD, Gelber RD, Perez-Atayde AR, Sallan SE, Sanders SP. Late cardiac effects of doxorubicin therapy for acute lymphoblastic leukemia in childhood. N Engl J Med. 1991;324(12):808–815. doi: 10.1056/NEJM199103213241205. [DOI] [PubMed] [Google Scholar]
- 7.Mertens AC, Liu Q, Neglia JP, Wasilewski K, Leisenring W, Armstrong GT, et al. Cause-specific late mortality among 5-year survivors of childhood cancer: the childhood cancer survivor study. J Natl Cancer Inst. 2008;100(19):1368–1379. doi: 10.1093/jnci/djn310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mody R, Li S, Dover DC, Sallan S, Leisenring W, Oeffinger KC, et al. Twenty-five-year follow-up among survivors of childhood acute lymphoblastic leukemia: a report from the childhood cancer survivor study. Blood. 2008;111(12):5515–5523. doi: 10.1182/blood-2007-10-117150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dreizen S, McCredie KB, Bodey GP, Keating MJ. Quantitative analysis of the oral complications of antileukemia chemotherapy. Oral Surg Oral Med Oral Pathol. 1986;62(6):650–653. doi: 10.1016/0030-4220(86)90258-6. [DOI] [PubMed] [Google Scholar]
- 10.Spiegler BJ, Kennedy K, Maze R, Greenberg ML, Weitzman S, Hitzler JK, et al. Comparison of long-term neurocognitive outcomes in young children with acute lymphoblastic leukemia treated with cranial radiation or high-dose or very high-dose intravenous methotrexate. J Clin Oncol. 2006;24(24):3858–3864. doi: 10.1200/JCO.2006.05.9055. [DOI] [PubMed] [Google Scholar]
- 11.Multinational Association of Supportive Care in Cancer (MASCC) (2016) Strategic Plan, Consensus on the Core Ideology of MASCC; Available at: http://www.mascc.org/index.php?option=com_content&view=article&id=493:mascc-strategic-plan&catid=30:navigation. Accessed 8, 2016
- 12.Rittenberg CN, Johnson JL, Kuncio GM An oral history of MASCC, its origin and development from MASCC’s beginnings to 2009. Support Care Cancer 2010 10–03-2010;775–784 [DOI] [PubMed]
- 13.Graham R, Mancher M, Wolman DM. Clinical practice guidelines we can trust. Washington: The National Academies Press; 2011. [PubMed] [Google Scholar]
- 14.Lehrnbecher T, Ethier MC, Zaoutis T, Creutzig U, Gamis A, Reinhardt D, et al. International variations in infection supportive care practices for paediatric patients with acute myeloid leukaemia. Br J Haematol. 2009;147(1):125–128. doi: 10.1111/j.1365-2141.2009.07844.x. [DOI] [PubMed] [Google Scholar]
- 15.van de Wetering MD, Abbink F, Ball L, Michiels E, Loeffen J, Segers H, et al. Werkboek supportive care 2015; Available at: https://www.skion.nl/workspace/uploads/inhouds-opgave.pdf. Accessed 10 Jul 2016
- 16.Kamps WA, Naafs-Wilstra MC, Schouten-van Meeteren AYN, Tissing WJE. Werkboek Ondersteunende behandeling in de Kinderoncologie. Amsterdam: VU University Press; 2005. [Google Scholar]
- 17.Lehrnbecher T, Phillips R, Alexander S, Alvaro F, Carlesse F, Fisher B, et al. Guideline for the management of fever and neutropenia in children with cancer and/or undergoing hematopoietic stem-cell transplantation. J Clin Oncol. 2012;30(35):4427–4438. doi: 10.1200/JCO.2012.42.7161. [DOI] [PubMed] [Google Scholar]
- 18.Dupuis LL, Boodhan S, Holdsworth M, Robinson PD, Hain R, Portwine C, et al. Guideline for the prevention of acute nausea and vomiting due to antineoplastic medication in pediatric cancer patients. Pediatr Blood Cancer. 2013;60(7):1073–1082. doi: 10.1002/pbc.24508. [DOI] [PubMed] [Google Scholar]
- 19.Wiener L, Viola A, Koretski J, Perper ED, Patenaude AF. Pediatric psycho-oncology care: standards, guidelines, and consensus reports. Psycho-Oncology. 2015;24(2):204–211. doi: 10.1002/pon.3589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Loeffen EA, Mulder RL, Kremer LC, Michiels EM, Abbink FC, Ball LM, et al. Development of clinical practice guidelines for supportive care in childhood cancer-prioritization of topics using a Delphi approach. Support Care Cancer. 2015;23(7):1987–1995. doi: 10.1007/s00520-014-2559-7. [DOI] [PubMed] [Google Scholar]
- 21.Sofaer S. Qualitative research methods. Int J Qual Health Care. 2002;14:329–336. doi: 10.1093/intqhc/14.4.329. [DOI] [PubMed] [Google Scholar]
- 22.Mays N, Pope C. Qualitative research in health care. Assessing quality in qualitative research. BMJ. 2000;320:50–52. doi: 10.1136/bmj.320.7226.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mack N, Woodsong C, MacQueen KM, Guest G, Namey E (2005) Module 1, Qualitative Research Methods Overview. Qualitative research methods: a data collector’s field guide North Carolina: Research Triangle Park. p. 4–8
- 24.Pope C, Ziebland S, Mays N. Qualitative research in health care. Analysing qualitative data. BMJ. 2000;320:114–116. doi: 10.1136/bmj.320.7227.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tates K, Zwaanswijk M, Otten R, van Dulmen S, Hoogerbrugge PM, Kamps WA, et al. (2009) Online focus groups as a tool to collect data in hard-to-include populations: examples from paediatric oncology. BMC Med Res Methodol 9:15–2288–9-15 [DOI] [PMC free article] [PubMed]
- 26.Jefford M, Karahalios E, Pollard A, Baravelli C, Carey M, Franklin J, et al. Survivorship issues following treatment completion—results from focus groups with Australian cancer survivors and health professionals. J Cancer Surviv. 2008;2(1):20–32. doi: 10.1007/s11764-008-0043-4. [DOI] [PubMed] [Google Scholar]
- 27.Kane HL, Halpern MT, Squiers LB, Treiman KA, McCormack LA. Implementing and evaluating shared decision making in oncology practice. CA Cancer J Clin. 2014;64(6):377–388. doi: 10.3322/caac.21245. [DOI] [PubMed] [Google Scholar]
- 28.Lipstein EA, Brinkman WB, Britto MT. What is known about parents’ treatment decisions? A narrative review of pediatric decision making. Med Decis Mak. 2012;32(2):246–258. doi: 10.1177/0272989X11421528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Contro N, Larson J, Scofield S, Sourkes B, Cohen H. Family perspectives on the quality of pediatric palliative care. Arch Pediatr Adolesc Med. 2002;156(1):14–19. doi: 10.1001/archpedi.156.1.14. [DOI] [PubMed] [Google Scholar]
- 30.Kilicarslan-Toruner E, Akgun-Citak E. Information-seeking behaviours and decision-making process of parents of children with cancer. Eur J Oncol Nurs. 2013;17(2):176–183. doi: 10.1016/j.ejon.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 31.Coyne I, Amory A, Kiernan G, Gibson F. Children’s participation in shared decision-making: children, adolescents, parents and healthcare professionals’ perspectives and experiences. Eur J Oncol Nurs. 2014;18(3):273–280. doi: 10.1016/j.ejon.2014.01.006. [DOI] [PubMed] [Google Scholar]
- 32.VOKK. Vereniging Ouders, Kinderen en Kanker (2016) Available at: http://vokk.nl. Accessed 7/21 2016
- 33.Sim J, Snell J. Focus groups in physiotherapy evaluation and research. Physiotherapy. 1996;82(3):189–198. doi: 10.1016/S0031-9406(05)66923-4. [DOI] [Google Scholar]
- 34.Krueger RA, Casey MA (2009) Focus groups: A practical guide for applied research. Sage Publications
- 35.Kitzinger J. The methodology of focus groups: the importance of interaction between research participants. Sociology of Health & Illness. 1994;16(1):103–121. doi: 10.1111/1467-9566.ep11347023. [DOI] [Google Scholar]
- 36.Saldana J. The coding manual for qualitative researchers. Thousand Oaks: Sage Publications; 2009. p. 157. [Google Scholar]
- 37.Harding Jamie (2013) Qualitative Data Analysis from Start to Finish London, SAGE Publishers. p.452
- 38.James K, Keegan-Wells D, Hinds PS, Kelly KP, Bond D, Hall B, et al. The care of my child with cancer: parents’ perceptions of caregiving demands. J Pediatr Oncol Nurs. 2002;19(6):218–228. doi: 10.1053/jpon.2002.128777. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 33 kb).