A 21-year-old man presented with a painless ulcer on the penis, which had been present for 4 weeks, and diffuse, symmetrical erythematous maculopapules on the trunk, extremities, palms, and soles, which had been present for 1 week. Gram staining of bloody exudate from his chancre revealed very weakly Gram-negative spiral rods (Picture 1; ×1,000). We therefore performed Giemsa staining, which revealed spiral-shaped bacteria (Picture 2; ×1,000; arrows) that were thought to be spirochetes. The rapid plasma regain (titer, 1:128) and Treponema pallidum latex agglutination test results were positive. The patient was treated with antisyphilitic medication. His cutaneous lesions and chancre resolved within 2 weeks after treatment.
Picture 1.

Picture 2.
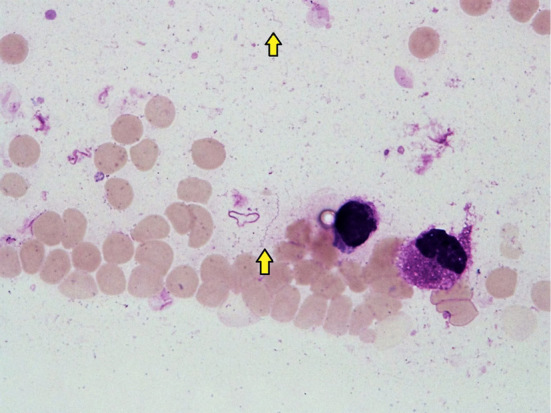
Darkfield microscopy, a representative method for the direct detection of T. pallidum, can detect spirochetes in patients with early-stage syphilis who are nonreactive to serologic tests; however, this is not performed at all facilities (1). If syphilis is suspected, Giemsa staining should be performed in addition to Gram staining; these simple tests might aid in the early diagnosis of syphilis.
The authors state that they have no Conflict of Interest (COI).
References
- 1. Radolf JD, Tramont EC, Salazar JC. Syphilis (Treponema pallidum). In: Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 8th ed Bennett JE, Dolin R, Blaser MJ, Eds. Saunders, Pennsylvania, 2015: 2684-2709. [Google Scholar]


