Abstract
Purpose of Review
Mechanisms leading to anterior cruciate ligament (ACL) injury have been identified, yet re-injury or a secondary injury persists in the athletic population. The purpose of this review is to identify risk factors associated with ACL injury and investigate programs to prevent injury.
Recent Findings
Faulty mechanics during dynamic movement that cause excessive valgus force at the knee increases the risk of ACL injury. Faulty mechanics may be a result of lateral displacement of the trunk, unequal limb loading, and lack of control to avoid the valgus knee position. Altered movements that place the ACL at risk are best identified in a fatigued state; however, could be recognized in a standard dynamic assessment. The faulty movement patterns are modifiable and should be addressed in an injury prevention program. Prevention programs include various modes of exercise such as plyometrics, neuromuscular training, and strength training.
Summary
This review concludes that those programs which utilize neuromuscular training and strength training at a young age show the most promise in reducing ACL injuries. An ongoing thorough dynamic examination is necessary for all athletes while adjusting the intervention program in order to decrease the risk of ACL injury.
Keywords: Knee injury, Anterior cruciate ligament (ACL), Prevention program, Neuromuscular training, Plyometrics, Strength training
Introduction
Although the incidence of anterior cruciate ligament (ACL) injury is unknown [1], it is estimated that 350,000 ACL reconstructions (ACLRs) are performed annually in the USA [2]. Despite surgical repair, approximately 79% of those individuals develop knee osteoarthritis (OA) and 20% suffer re-injury within 2 years [3]. The risk of re-injury and developing arthritis has become an economic burden and overall concern in the athletic arena [4]. Athletic ACL injury rates are increasing [5] in both D1 career athletes [6] and youth athletes [7]. One in four youths who suffer an ACL injury will suffer a second ACL injury in their athletic career [7]. Athletes who suffer a knee injury prior to participation in D1 career have an eightfold increased risk of suffering another knee injury during their D1 career and spend 50% more time on the disabled list (DL) [6]. Despite the ongoing research to identify contributing factors to potential knee injury in athletes, injury continues to occur and intervention and prevention models fail. As a result, knee injury (specifically ACL) has a large impact on future athletic performance. An accurate functional assessment tool and intervention are needed to curb this injury trend and identify factors that predispose athletes to injury.
Functional Anatomy and Biomechanics of the Knee
The ACL, extending from the lateral femoral condyle to the crest of the anterior medial aspect of the tibia, contributes to knee stability via passive restraint. The orientation and direction of the bands of the ACL act as a biomechanical restraint for rotation as well as limiting anterior translation of the tibia on the femur [8]. The combination of active muscle contraction with precise neuromuscular timing assists with knee stability during running, jumping, and cutting or pivoting maneuvers. Any alteration in the biomechanics or muscular control of the knee increases the risk of ACL injury.
Structural features of the knee that increase risk of injury to the ACL include intercondylar notch size as well as the integrity of the menisci. These factors, although only modifiable via surgery, should be recognized as potential causes of ACL injury. The intercondylar notch of the femur, especially in females, can be a structural risk if too narrow, resulting in compromised space for the ACL during rotation. The depth and integrity of the menisci assist condylar motion as the femur maintains contact during loaded motions such as flexion and rotation. A meniscus tear can alter the translation of the femoral condyles on the tibia and place added stress to the ACL during cutting or jumping maneuvers [9]. Other passive restraints such as joint capsule and ligamentous structures (i.e., collateral ligaments) control dynamic motion and assist with knee stability. Injury to any passive restraint in the knee may compromise the biomechanical function of the knee and increase injury risk to the ACL. It should be noted that tibial slope has been identified as a potential structural risk factor in ACL injury as well.
Dynamic and modifiable biomechanics of the knee such as hyperextension, excessive valgus, or abduction moments attribute to ACL stress. Stress on the ACL is the greatest with internal tibial torsion near full knee extension [9]. Cadaveric studies assist in further understanding the biomechanics of the knee by providing positions of the knee where the ACL is under stress. The ACL resists rotational forces at 10 and 30° knee flexion in cadaveric specimens and less at greater degrees of flexion such as 50–90° [10, 11]. However, dynamic muscular influences such as quadriceps dominance during sustained flexion activities causes anterior translation of the femur on the tibia and could predispose the ACL to stress [12,13,14•]. Effective co-contraction of the hamstrings and quadriceps has been postulated to assist in preventing the magnitude of anterior displacement that may occur with flexion activities such as cutting and landing from a jump [12, 15]. Double-limb or single-limb landing with an extended knee combined with abduction moments provides the greatest force to the ACL [14•,15•,16] (Fig. 1). As the knee accelerates into a valgus position, stress increases on the ACL. Additionally, poor muscular control results in improper knee alignment and increased anterior-posterior translation or rotary shear forces. This shear force and excessive rotary laxity can result in meniscus tears and injury to the ACL.
Fig. 1.
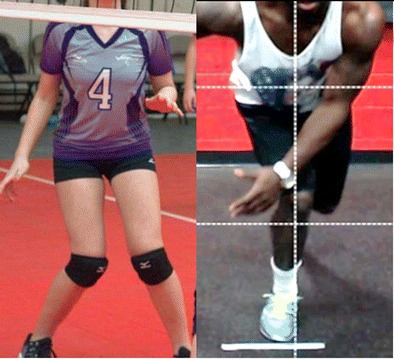
Landing with knee extended and adduction moment causing stress to the ACL
Injury Prevalence
Injury to the ACL occurs during dynamic activities that primarily involve cutting and pivoting and can occur during landing after a jump. Competitive and recreational athletes between the ages of 15 and 25 are at the greatest risk of injury. The majority (80%) of the injuries are non-contact, and therefore, the mechanisms are modifiable [3, 17–19]. Female athletes are at risk four to six times greater than their male counterparts [20–22]. Female high school athletes had a ninefold increase injury risk and fivefold in collegiate sports [23] and those that competed at a higher level of play had a five times higher risk than their male counterpart [24]. Sports that require high dynamic loading of the knee and report a high incidence of injury include soccer, volleyball, handball, and basketball.
Associated consequences for both athletes and military personnel who suffer an ACL injury include time on disabled list or loss of duty time, increased risk of another injury, and development of OA [25–27]. Unique to the military, females were not more susceptible to primary ACL injury when compared to male personnel. Overall, prior knee injury in all military personnel contributed to risk of another knee injury and prior hip injury increased risk of specific ACL injury [28]. Re-injury in the athletic population occurs in one of four youths, and ACL graft rupture was higher in male athletes following repair when compared to female athletes who had ACLR [7, 29]. A 12-year follow-up study was conducted on 221 individuals post-ACLR and detected chondral defects (64%) and patellofemoral OA (26%) indicating continued degeneration of the knee joint and adjunct joints [30]. Holm et al. (2012) [3] conducted a 10-year follow-up on 57 patients who had ACLR, and 79% had developed OA. Despite surgical intervention, individuals who suffered ACL injury developed OA and reduced function [30].
Movement and Factors Impacting Performance
Frontal Plane Motion
Excessive adduction moment at the knee in the frontal plane increases injury risk to the ACL [31, 32]. Landing from a drop jump and cutting maneuvers in sports are correlated with increased adduction moment at the knee. The drop jump may be performed with single leg or double leg while the cutting involves a single limb. Therefore, the kinematics and kinetics are different for each of these activities [33]. A single-leg technique, such as the sidestep cutting maneuver, those with poor mechanics demonstrate six times the amount of frontal plane adduction moment when compared to the drop jump [34]. The amount of frontal plane adduction moment can be reduced or controlled to decrease the risk of injury to the ACL [35•], and analysis of single-leg motion should be included as an assessment in sports injury prevention.
Fatigue and Single Limb Testing
Fatigue has been related to increase risk of injury in the athletic population [36]. Athletes demonstrate increased motion in both the sagittal plane and frontal plane accompanied by greater ground reaction forces when fatigued [37]. The hip and knee internal rotation increased with fatigue creating a valgus force at the knee [38] and ground reaction forces increased with a single-limb hop [39]. The combined increased ground reaction force and valgus at the knee predisposes the ACL to injury.
Trunk Stability
Trunk position and hip motion strongly influence knee control during single limb and cutting motions [40•]. Decreases in trunk and hip strength and endurance result in larger center of mass (COM) displacement in athletics [41]. Increased control of trunk and hip sagittal and frontal motions reduces COM displacement and frontal plane motion at the knee [41, 42]. This improvement in COM has been directly correlated to improvements in pitching mechanics [41] and decreased injury rates in major league baseball players [43]. Targeted training to the hip and trunk has been shown to improve frontal plane motion at the knee and improvements in athletic performance measures [44].
Limb Symmetry Index
The standard of practice for assessing an athlete’s ability to return to play is to assess their affected limb in comparison to their unaffected limb or to assess their limb symmetry index (LSI). LSI is a percentile measurement comparing the limb symmetry of the affected side to the unaffected side. Figure 2 shows the calculation for LSI [45].The LSI has been utilized as a quantitative measure to determine the strength and performance of an athlete prior to return to sport [46–48]. Non-injured athletes have a LSI of 90–95% [49], while individuals who suffer an ACL injury rarely reach greater than 90% LSI post reconstruction [50]. Although this has been primarily tested in an open kinetic chain, closed kinetic chain testing has been shown to be a better predictor of true limb symmetry [51–55].
Fig. 2.
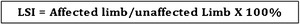
Equation for calculation of limb symmetry index
Lateral Displacement of the Pelvis During Squatting Motion
The squatting motion is an essential movement for the development of lower extremity strength, endurance, and the explosive power associated with sports. Variations in weight distribution during this motion will impact joint and ligamentous loading, soft tissue and ligamentous strain [56], and influence asymmetry in strength development. Lateral displacement of the pelvis occurs during a squatting motion results in altered force distribution and joint forces [57•]. Peak ground reaction force has been calculated up to 3–6 times body weight during sporting activities [58]. A lateral shift of the pelvis with the increased ground reaction force alters distribution of loads through the lower limb, ligamentous structures, and lumbar spine and increases the likelihood of ligamentous and soft tissue injury, such as ACL injuries [58]. The altered length tension relationship of the musculature during training with poor mechanics leads to decreased force production. However, with proper education and rehabilitation, correction of lateral displacement of the pelvis is correlated with improved vertical jump height and sprint speed [59].
Prevention Programs
Many different programs have been developed with the goal of decreasing the risk and/or preventing ACL injuries [14, 22, 60, 61] (Table 1). There is a strong evidence in support of ACL injury prevention programs demonstrated by a risk reduction of 52% in the female athletes and 85% in the male athletes [22, 60, 71, 72]. Grimm et al. (2014) [61] reports a reduction in risk for knee injuries in soccer players and effectiveness of the use of intervention programs. Moreover, ACL injury prevention occurred when female athletes participated in a prevention program using specific training components [73].
Table 1.
Commonly cited injury prevention program articles
| Study | Journal | Year | Subjects | No. of subjects | Sport | Program type | Duration | Frequency | Incidence of ACL injury per 1000 occurrences |
|---|---|---|---|---|---|---|---|---|---|
| Ghilchrist et al. [62] | AJSM | 2008 | Female | 583 trained 852 control |
Soccer | M-F approacha | 20 min/session | 3 days/week, entire season | 0.057 trained group 0.189 control group |
| Caraffa et al. [63] | KSSTA | 1996 | Male | 300 trained 300 control |
Soccer | N-M approacha | 20 min/session | Entire season | Not reported |
| Heidt et al. [64] | AJSM | 2000 | Female | 42 trained 258 control |
Soccer | M-F approacha | 2 days/week 7 weeks |
0.25 trained group 0.33 control group |
|
| Hewett et al. [65] | AJSM | 1999 | Female/male | 366 trained 463 control |
Soccer Volleyball Basketball | M-F approacha | 60–90 min/session | 3 days/week, 6 weeks | 0.12 trained group 0.22 control group |
| Mandelbaum et al. [66] | AJSM | 2005 | Female | 1885 trained 3818 control |
Soccer | M-F approacha | 20 min/session | 3 days/week, 12 weeks | 0.09 trained group 0.49 control group |
| Peterson et al. [67] | AOTS | 2005 | Female | 134 trained 142 control |
Handball | N-M approachb | 3 days/week, 8 weeks | 0.08 trained group 0.49 control group |
|
| Pfeiffer et al. [68] | JBJS | 2006 | Female | 577 trained 862 control |
Soccer Volleyball Basketball |
Plyo approachc | 20 min/session | 2 days/week, entire season | 0.078 trained group 0.167 control group |
| Kiani et al. [69] | AIM | 2010 | Female | 1506 | Soccer | M-F approacha | 2 days/week pre-season, 1 day/week in-season | 0.04 trained troup 0.20 control group |
|
| Soligard et al. [70] | BJSM | 2008 | Female | 1055 trained 837 control |
Soccer | M-F approacha | 20 min/session | entire season | Not reported |
AJSM American Journal Sports Medicine, KSSTA Knee Surgery, Sports Traumatology, Arthroscopy, AOTS Archives of Orthopedic and Trauma Surgery, JBJS Journal of Bone and Joint Surgery, AIM Archives of Internal Medicine, BJSM British Journal of Sports Medicine
aM-F approach: multi-faceted approach included a warm-up, strengthening, plyometrics, and agility activities
bN-M approach: neuromuscular approach included proprioceptive, balance, and stability activities
cPlyo approach: plyometric-based approach included jumping and cutting activities
Sugimoto et al. (2015) [74] has proposed six critical principles to follow when developing an ACL injury prevention program. These principles include age, biomechanics, compliance, dosage, feedback, and exercise.
Six Principles of a Prevention Program
Age
It is recommended that ACL prevention programs be implemented at an early age. Fewer ACL injuries were documented in younger athletes who performed a neuromuscular training program compared to older athletes who performed the same program [66, 75•, 76].
Biomechanics
Faulty biomechanics correlated with increased strain on the ACL during different movement patterns and sporting activities with increased knee valgus being one of the strongest indicators of increased ACL injury risk [73, 77•, 78, 79].
Compliance
Compliance of performance of an ACL prevention program is vital to the ability of the program to be successful at reducing injury rates. Compliance greater than 66% resulted in an ACL injury reduction rate of 82%. However, when compliance rate dropped to less than 66%, ACL injury reduction rate dropped to 44% [80]. Currently, compliance is subject to a large degree of heterogeneity in literature and the need to have a uniform definition is needed [81].
Dosage
Frequent participation in an ACL prevention program decreases risk for ACL injury. Most studies agree that each session should be between 20 and 30 min and should be performed several times per week. Optimally, they should be initiated in the pre-season and continued throughout the season to attain the full effectiveness of the program [60, 82].
Feedback
Many studies included some type of feedback, and whether verbal or visual, a decrease in ACL injuries has been shown. Feedback can be in the form of verbal cueing from a coach or a training partner, but can also be visual as in a training video. Feedback should also come in the form of an external focus versus internal focus. External focus is directed toward the outcome or effects of the movement, assists the automation of movements, and accelerates the learning process. When teaching proper landing mechanics, an external focus command would be, “Try to bring your knees as close to the outside walls as possible when you land” [83]. Internal focus is directed toward specific movements, such as “keep your knees out,” and this constant focus on correct movement can lead to a reduction in athlete’s motivation. Thus, it is recommended that a feedback system be implemented in an ACL prevention program with an external focus [62, 76, 83–85].
Exercise Variety
ACL injury prevention programs that included a variety of different exercises have a greater incidence of decreasing injury risk versus programs that include only one type of exercise or component (plyometric, balance, strengthening). These exercises can be mainly classified into three different components: plyometrics, neuromuscular training, and strength training. All three have been utilized as stand-alone programs or have been combined to create comprehensive prevention programs [21, 61, 86•].
Three Components of Exercise in a Prevention Program
Plyometrics
Plyometrics focusing on proper technique and body mechanics can help to reduce serious ligamentous injuries, specifically ACL injuries [65, 68].
Neuromuscular Training
The term neuromuscular training is utilized throughout the literature and is included in most injury prevention programs [62, 65, 87] (Table 1). The objective of neuromuscular training is to improve the ability to generate optimal muscle firing patterns, increase dynamic joint stability, and to perform movement patterns and skills necessary during activities of daily living and sports activities. This may include balance exercises, proprioceptive activities on balance and wobble boards [63, 87], single-leg stability activities [66, 73], dynamic joint stability exercises, jump training, plyometric exercises, agility drills, and sport-specific exercises [88, 89]. These types of proprioceptive and balance training can improve postural control and side-to-side imbalances in lower extremity measures [90].
Strength Training
The programs that incorporated strength training were among the most effective at decreasing ACL injury rates; however, strength training alone may not be efficacious for prevention. Programs have been shown to be effective in decreasing ACL injures without the usage of strength training [67, 68, 91]. Resistance training may aid in the reduction of ACL injuries when combined with other training components; however, the efficacy of a single-faceted resistance training protocol on ACL injury prevention has yet to be determined [14].
Conclusion/Summary
Injury to the ACL is the leading knee complication in sports and the primary cause of time on the disabled list.
Modifiable factors such as excessive frontal plane motion leading to dynamic valgus forces at the knee and improper landing or cutting techniques directly stress the ACL and contribute to the risk of injury. The authors recognize that valgus stress at the knee associated with poor neuromuscular control and trunk position predisposes the athlete to injury especially in a fatigued state. However, terminology in the literature varies how this position is described. Abduction moment of the knee and adduction moment were both utilized to describe a valgus force depending on the reference of orientation of tibia on femur (distal to proximal) or femur on tibia (proximal to distal). Despite the discrepancy, the resultant valgus stress at the knee with limited neuromuscular control is the largest risk for ACL injury and is a modifiable mechanism utilized in prevention programs.
A dynamic assessment is recommended for evaluating athletes at risk for ACL injury. Faulty mechanics especially in a fatigued state can assist in identifying alterations in the trunk, pelvis, and lower kinetic chain during functional movements that may predispose the athlete to injury. Herein, the development of specific interventions can be established and incorporated into a prevention program that is specific to the athlete.
Some prevention programs utilize a multi-faceted approach or neuromuscular approach while others utilize strengthening and plyometrics. Programs that integrated strengthening with neuromuscular training were the most effective, and incorporating this method at a younger age was beneficial for injury prevention. Time spent in the prevention program has yet to be standardized for the most effective outcomes, though currently, most studies agree that 20–30min sessions several times weekly are needed. Further work is needed to establish the ideal approach for ACL injury prevention programs.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on ACL Rehab
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Meisterling SW, Schoderbek RJ, Andrews JR. Anterior cruciate ligament reconstruction. Oper Tech Sports Med. 2009;17:2–10. doi: 10.1053/j.otsm.2009.02.003. [DOI] [Google Scholar]
- 2.Allografts in Sports Medicine: What do we know, need to know, and need to do? Round table discussion: American Orthopedic Society for Sports Medicine; 2006. Park City, UT
- 3.Holm I, Oiestad B, Risberg M, et al. No difference in prevalence of osteoarthritis or function after open versus endoscopic technique for anterior cruciate ligament reconstruction: 12-year follow-up report of randomized controlled trial. Am J Sports Med. 2012;40:2492–2498. doi: 10.1177/0363546512458766. [DOI] [PubMed] [Google Scholar]
- 4.Flynn RK, Pedersen CL, Birmingham TB, et al. The familial predisposition toward tearing the anterior cruciate ligament: a case control study. Am J Sports Med. 2005;33:23–28. doi: 10.1177/0363546504265678. [DOI] [PubMed] [Google Scholar]
- 5.Dodwell E, LaMont L, Green D, et al. 20years of pediatric anterior cruciate ligament reconstruction in New York state. 2014;42:675–680. [DOI] [PubMed]
- 6.Rugg C, Wang D, Sulzicki P, et al. Effects of prior knee surgery on subsequent injury, imaging and surgery in NCAA collegiate athletes. Am J Sport Med. 2014;42:959–964. doi: 10.1177/0363546513519951. [DOI] [PubMed] [Google Scholar]
- 7.Wiggins A, Granhi R, Schneider D, et al. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sport Med. 2016;44:1861–1876. doi: 10.1177/0363546515621554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Amis AA. The functions of the fibre bundles of the anterior cruciate ligament in anterior drawer, rotational laxity and the pivot shift. Knee Surg Sports Traumatol Arthrosc. 2012;20:613–620. doi: 10.1007/s00167-011-1864-7. [DOI] [PubMed] [Google Scholar]
- 9.Senter C, Hame S. Biomechanicial analysis of tibial torque and knee flexion angle. Sports Med. 2006;36(8):635–641. doi: 10.2165/00007256-200636080-00001. [DOI] [PubMed] [Google Scholar]
- 10.Wunschel M, Muller O, Lo J, et al. The anterior cruciate ligament provides resistance to externally applied anterior tibial force but not to internal rotational torque during simulated weight-bearing flexion. Arthroscopy JArthrosc Relat Surg. 2010;26(11):1520–1527. doi: 10.1016/j.arthro.2010.04.069. [DOI] [PubMed] [Google Scholar]
- 11.Andersen HN, Dyhre-Poulsen P. The anterior cruciate ligament does play a role in controlling axial rotation in the knee. Knee Surg Sports Traumatol Arthrosc. 1997;5(3):145–149. doi: 10.1007/s001670050042. [DOI] [PubMed] [Google Scholar]
- 12.Baratta R, Solomonow M, Zhou BH, et al. Muscular coactivation: the role of the antagonist musculature in maintaining knee stability. Am J Sport Med. 1988;16(2):113–122. doi: 10.1177/036354658801600205. [DOI] [PubMed] [Google Scholar]
- 13.Withrow TJ, Huston LJ, Wojtys EM, et al. The relationship between quadriceps muscle force, knee flexion, and anterior cruciate ligament strain in an in vitro simulated jump landing. Am J Sport Med. 2006;34(2):269–274. doi: 10.1177/0363546505280906. [DOI] [PubMed] [Google Scholar]
- 14.Hewett TE, Ford KR, Hoogenboom BJ, et al. Understanding and preventing ACL injuries: current biomechanical and epidemiologic considerations—update 2010. North American J Sports Phys Ther. 2010;5(4):234–250. [PMC free article] [PubMed] [Google Scholar]
- 15.Myer GD, Ford KR, Di Stasi SL, et al. High knee abduction moments are common risk factors for patellofemoral pain (PFP) and anterior cruciate ligament (ACL) injury in girls: is PFP itself a predictor for subsequent ACL injury? Br J Sports Med. 2015;49:118–122. doi: 10.1136/bjsports-2013-092536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huston LJ, Vibert B, Ashton-Miller JA, et al. Gender differences in knee angle when landing from a drop-jump. Am J knee Surg. 2001;14:215–220. [PubMed] [Google Scholar]
- 17.Myer GD, Ford KR, Brent JL, et al. Differential neuromuscular training effects on ACL injury risk factors in “high-risk” versus “low-risk” athletes. BMC Musculoskel Dis. 2007;8(39). [DOI] [PMC free article] [PubMed]
- 18.Sell TC, Ferris CM, Abt JP, et al. Predictors of proximal tibia anterior shear force during a vertical stop-jump. J Orthop Res. 2007;25(12):1589–1597. doi: 10.1002/jor.20459. [DOI] [PubMed] [Google Scholar]
- 19.Dowling AV, Favre J, Andriacchi TP. Inertial sensor-based feedback can reduce key risk metrics for anterior cruciate ligament injury during jump landings. Am J Sport Med. 2012;40(5):1075–1083. doi: 10.1177/0363546512437529. [DOI] [PubMed] [Google Scholar]
- 20.Griffin L, Albohm M, Arendt E, et al. Understanding and preventing noncontact anterior cruciate ligament injuries: a review of the Hunt Valley II meeting, January 2005. Am J Sports Med. 2006;34:1512–1532. doi: 10.1177/0363546506286866. [DOI] [PubMed] [Google Scholar]
- 21.Hewett TE, Ford KR, Myer GD, et al. Anterior cruciate ligament injuries in female athletes. Part 2, a meta-analysis of neuromuscular interventions aimed at injury prevention. Am J Sport Med. 2006;34(3):490–498. doi: 10.1177/0363546505282619. [DOI] [PubMed] [Google Scholar]
- 22.Yoo JH, Lim BO, Ha M, et al. A meta-analysis of the effect of neuromuscular training on the prevention of the anterior cruciate ligament injury in female athletes. Knee Surg Sports Traumatol Arthrosc. 2010;18(6):824–830. doi: 10.1007/s00167-009-0901-2. [DOI] [PubMed] [Google Scholar]
- 23.National Collegiate Athletic Association . NCAA injury surveillance system summary. Indianapolis: National Collegiate Athletic Association; 2002. [Google Scholar]
- 24.Johnsen M, Guddal M, Smastuen M, et al. Sport participation and the risk of anterior cruciate ligament reconstruction in adolescents: a population-based prospective cohort study (The Young-HUNT Study) Am J Sport Med. 2016;44:2917–2924. doi: 10.1177/0363546516643807. [DOI] [PubMed] [Google Scholar]
- 25.Ford KR, Myer GD, Toms HE, et al. Gender differences in the kinematics of unanticipated cutting in young athletes. Med Sci Sports Exerc. 2005;37:124–129. doi: 10.1249/01.MSS.0000150087.95953.C3. [DOI] [PubMed] [Google Scholar]
- 26.Lohmander LS, Englund PM, Dahl LL, et al. The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med. 2007;35:1756–1769. doi: 10.1177/0363546507307396. [DOI] [PubMed] [Google Scholar]
- 27.Hill OT, Bulathsinhala L, Scofield DE, et al. Risk factors for soft tissue knee injuries in active duty US Army soldiers, 2000–2005. Mil Med. 2013;178(6):676–682. doi: 10.7205/MILMED-D-13-00049. [DOI] [PubMed] [Google Scholar]
- 28.Owens BD, Mountcastle SB, Dunn WR, et al. Incidence of anterior cruciate ligament injury among active duty US military servicemen and servicewomen. Mil Med. 2007;172(1):90–91. doi: 10.7205/MILMED.172.1.90. [DOI] [PubMed] [Google Scholar]
- 29.Webster K, Feller J. Exploring the high reinjury rate in younger patients undergoing anterior cruciate ligament reconstruction. Am J Sport Med. 2016;44:2827–2832. doi: 10.1177/0363546516651845. [DOI] [PubMed] [Google Scholar]
- 30.Oiestad BE, Holm I, Engebretsen L, et al. The prevalence of patellofemoral osteoarthritis 12 years after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2013;21:942–949. doi: 10.1007/s00167-012-2161-9. [DOI] [PubMed] [Google Scholar]
- 31.Sigward S, Powers C. Loading characteristics of females exhibiting excessive valgus moments during cutting. Clin Biomech. 2007;22:827–833. doi: 10.1016/j.clinbiomech.2007.04.003. [DOI] [PubMed] [Google Scholar]
- 32.Pollard C, Stearns K, Hayes A, et al. Altered lower extremity movement variability in female soccer players during side-step cutting after anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43:460–465. doi: 10.1177/0363546514560153. [DOI] [PubMed] [Google Scholar]
- 33.Kristinaslund E, Krosshaug T. Comparison of drop jumps and sport-specific sidestep cutting: implications for anterior cruciate ligament injury risk screening. Am J Sports Med. 2013;41:684–688. doi: 10.1177/0363546512472043. [DOI] [PubMed] [Google Scholar]
- 34.Cortes N, Onate J, Van Lunen B. Pivot tasks increases frontal plane loading compared with sidestep and drop-jump. J Sports Sci. 2011;29:83–92. doi: 10.1080/02640414.2010.523087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stearns K, Powers C. Improvements in hip muscle performance result in increased use of the hip extensors and abductors during a landing task. Am J Sports Med. 2014;42:602–609. doi: 10.1177/0363546513518410. [DOI] [PubMed] [Google Scholar]
- 36.Moore I, Ranson C, Mathema P. Injury risk in international rugby union: three-year injury surveillance of the welsh national team. Orth J Sports Med. 2015;3:1–9. doi: 10.1177/2325967115596194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brazen D, Todd K, Ambegaonkar J, et al. The effect of fatigue on landing biomechanics in single-leg drop landings. Clin J Sport Med. 2010;20:286–282. doi: 10.1097/JSM.0b013e3181e8f7dc. [DOI] [PubMed] [Google Scholar]
- 38.Borotikar B, Newcomer R, Koppes R, et al. Combined effects of fatigue and decision making on female lower limb landing postures: central and peripheral contributions to ACL risk. Clin Biomech. 2008;23:81–92. doi: 10.1016/j.clinbiomech.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 39.Orishimo K, Kremenic I. Effect of fatigue on single leg hop landing biomechanics. J App Biomech. 2006;10:1–10. doi: 10.1123/jab.22.4.245. [DOI] [PubMed] [Google Scholar]
- 40.Frank B, Bell D, Norcross M, et al. Trunk and hip biomechanics influence anterior cruciate loading mechanisms in physically active participants. Am J Sports Med. 2013;41:2676–2686. doi: 10.1177/0363546513496625. [DOI] [PubMed] [Google Scholar]
- 41.Chaudhari A, McKenzie C, Pan X, et al. Lumbopelvic control and days missed because of injury in professional baseball pitchers. Am J Sports Med. 2014;42:2734–2741. doi: 10.1177/0363546514545861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Baldon R, Piva S, Silva R, et al. Evaluating eccentric hip torque and trunk endurance as mediators of changes in lower limb and trunk kinematics in response to functional stabilization training in women with patellofemoral pain. Am J Sport Med. 2015;43:1485–1493. doi: 10.1177/0363546515574690. [DOI] [PubMed] [Google Scholar]
- 43.Chaudhari AM, McKenzie C, Borchers J, et al. Lumbopelvic control and pitching performance of professional baseball players. J Strength Con Res. 2011;25:2127–2132. doi: 10.1519/JSC.0b013e31820f5075. [DOI] [PubMed] [Google Scholar]
- 44.Hoshikawa Y, Iida T, Muramatsu M, et al. Effects of stabilization training on trunk muscularity and physical performance in youth soccer players. J Strength Con Research. 2013;27:3142–3149. doi: 10.1519/JSC.0b013e31828bed36. [DOI] [PubMed] [Google Scholar]
- 45.Gaunt B, Curd D. Anthropometric and demographic factors affecting distance hopped and limb symmetry index for the crossover hop-for-distance test in high school athletes. J Orth Sport Phy Ther. 2001;31:145–151. doi: 10.2519/jospt.2001.31.3.145. [DOI] [PubMed] [Google Scholar]
- 46.Noyes F, Barber S, Magine R. Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Am J Sports Med. 1991;19:513–518. doi: 10.1177/036354659101900518. [DOI] [PubMed] [Google Scholar]
- 47.Ardern CL, Taylor NF, Feller JA, et al. Return-to-sport outcomes at 2 to 7 years after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2012;40(1):41–48. doi: 10.1177/0363546511422999. [DOI] [PubMed] [Google Scholar]
- 48.Thomee R, Neeter C, Gustavsson A, et al. Variability in leg muscle power and hop performance after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2012;20:1143–1151. doi: 10.1007/s00167-012-1912-y. [DOI] [PubMed] [Google Scholar]
- 49.Rohman E, Steubs T, Tompkins M. Changes in involved and uninvolved limb function during rehabilitation after anterior cruciate ligament reconstruction: implications for limb symmetry index measures. Am J Sport Med. 2015;43:1391–1399. doi: 10.1177/0363546515576127. [DOI] [PubMed] [Google Scholar]
- 50.Zwolski C, Schmitt L, Thomas S, et al. The utility of limb symmetry indices in return to sport assessment in patients with bilateral anterior cruciate ligament reconstruction. Am J Sport Med. 2016;44:2030–2038. doi: 10.1177/0363546516645084. [DOI] [PubMed] [Google Scholar]
- 51.Myer G, Schmitt L, Brent J, et al. Utilization of modified NFL combine testing to identify functional deficits in athletes following ACL reconstruction. J Orth Sport Phy Ther. 2011;41:377–391. doi: 10.2519/jospt.2011.3547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Myer G, Paterno M, Ford K, et al. Rehabilitation after anterior cruciate ligament reconstruction: criteria-based progression through the return-to-sport phase. J Orth Sport Phy Ther. 2006;36:385–408. doi: 10.2519/jospt.2006.2222. [DOI] [PubMed] [Google Scholar]
- 53.Weir A, Darby J, Inklaar H, et al. Core stability: inter- and intraobserver reliability of 6 clinical tests. Clin J Sport Med. 2010;20:34–38. doi: 10.1097/JSM.0b013e3181cae924. [DOI] [PubMed] [Google Scholar]
- 54.Ekstrom R, Donatelli R, Carp K. Electromyographic analysis of core, trunk, hip, thigh muscles during 9 rehabilitation exericses. J Orth Sport Phy Ther. 2007;37:754–762. doi: 10.2519/jospt.2007.2471. [DOI] [PubMed] [Google Scholar]
- 55.Cleather D, Goodwin J, Bull A. Hip and knee joint loading during vertical jumping and push jerking. Clin Biomech. 2013;28:98–103. doi: 10.1016/j.clinbiomech.2012.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Nordin M, Frankel VH. Basic biomechanics of the musculoskeletal system. J of Biomech. 2002;35(6):871–872. doi: 10.1016/S0021-9290(02)00015-5. [DOI] [Google Scholar]
- 57.Atkins S, Hesketh C, Sinclair J. The presence of bilateral imbalance of the lower limbs in elite youth soccer players of different ages. J Strength Cond Res. 2016;30:1007–1013. doi: 10.1519/JSC.0b013e3182987044. [DOI] [PubMed] [Google Scholar]
- 58.Nessler T. Using movement assessment to improve performance and reduce injury risk. J Athl Ther Train. 2013;18:8–12. doi: 10.1123/ijatt.18.2.8. [DOI] [Google Scholar]
- 59.Wisloff U, Castagna C, Helgerud J, et al. Strong correlation of maximal squat strength with sprint performance and vertical jump height in elite soccer players. Br. J Sports Med. 2004;38:285–288. doi: 10.1136/bjsm.2002.002071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sadoghi P, von Keudell A, Vavken P. Effectiveness of anterior cruciate ligament injury prevention training programs. J Bone Joint Surg Am. 2012;94:769–776. doi: 10.2106/JBJS.K.00467. [DOI] [PubMed] [Google Scholar]
- 61.Grimm N, Jacobs J, Jr, Kim J, et al. Anterior cruciate ligament and knee injury prevention programs for soccer players: a systematic review and meta-analysis. Am J Sports Med. 2014;43(8):2049–2056. doi: 10.1177/0363546514556737. [DOI] [PubMed] [Google Scholar]
- 62.Gilchrist J, Mandelbaum BR, Melancon H, et al. A randomized controlled trial to prevent noncontact anterior cruciate ligament injury in female collegiate soccer players. Am J Sports Med. 2008;36:1476–1483. doi: 10.1177/0363546508318188. [DOI] [PubMed] [Google Scholar]
- 63.Soderman K, Werner S, Pietila T, et al. Balance board training: prevention of traumatic injuries of the lower extremities in female soccer players? Knee Surg Sports Traumatol Arthrosc. 2000;8:356–363. doi: 10.1007/s001670000147. [DOI] [PubMed] [Google Scholar]
- 64.Heidt RS, Jr, Sweeterman LM, Carlonas RL, et al. Avoidance of soccer injuries with preseason conditioning. Am J Sports Med. 2000;28:659–662. doi: 10.1177/03635465000280050601. [DOI] [PubMed] [Google Scholar]
- 65.Hewett TE, Lindenfeld TN, Riccobene JV, et al. The effect of neuromuscular training on the incidence of knee injury in female athletes: a prospective study. Am J Sports Med. 1999;27:699–706. doi: 10.1177/03635465990270060301. [DOI] [PubMed] [Google Scholar]
- 66.Mandelbaum BR, Silvers HJ, Watanabe D, et al. Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: two-year follow-up. Am J Sports Med. 2005;33:1003–1010. doi: 10.1177/0363546504272261. [DOI] [PubMed] [Google Scholar]
- 67.Petersen W, Braun C, Bock W, et al. A controlled prospective case control study of a prevention training program in female team handball players: the German experience. Arch Orthop Trauma Surg. 2005;125:614–616. doi: 10.1007/s00402-005-0793-7. [DOI] [PubMed] [Google Scholar]
- 68.Pfeiffer RP, Shea KG, Roberts D, et al. Lack of effect of a knee ligament injury prevention program on the incidence of noncontact anterior cruciate ligament injury. J Bone Joint Surg Am. 2006;88:1769–1774. doi: 10.2106/JBJS.E.00616. [DOI] [PubMed] [Google Scholar]
- 69.Kiani A, Hellquist E, Ahlqvist K, et al. Prevention of soccer-related knee injuries in teenaged girls. Arch Intern Med. 2010;170(1):43–49. doi: 10.1001/archinternmed.2009.289. [DOI] [PubMed] [Google Scholar]
- 70.Soligard T, Myklebust G, Steffen K, et al. Comprehensive warm-up programme to prevent injuries in young female footballers: cluster randomised controlled trial. BMJ. 2008;337 [DOI] [PMC free article] [PubMed]
- 71.Soomro N, Sanders R, Hackett D, et al. The efficacy of injury prevention programs in adolescent team sports: a meta-analysis. Am J Sport Med. 2015;44(9):2415–2424. doi: 10.1177/0363546515618372. [DOI] [PubMed] [Google Scholar]
- 72.Donnell-Fink LA, Klara K, Collins JE, et al. Effectiveness of knee injury and anterior cruciate ligament tear prevention programs: a meta-analysis. PLoS One. 2015;10(12):1–17. doi: 10.1371/journal.pone.0144063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hewett TE, Myer GD. The mechanistic connection between the trunk, knee, and ACL injury. Exerc Sport Sci Rev. 2011;39(4):161–166. doi: 10.1097/JES.0b013e3182297439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sugimoto D, Myer GD, Micheli LJ, et al. ABCs of evidence-based anterior cruciate ligament injury prevention strategies in female athletes. Curr Phys Med Rehabil Rep. 2015;3(1):43–49. doi: 10.1007/s40141-014-0076-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Myer GD, Sugimoto D, Thomas S, et al. The influence of age on the effectiveness of neuromuscular training to reduce anterior cruciate ligament injury in female athletes: a meta-analysis. Am J Sports Med. 2013;41(1):203–215. doi: 10.1177/0363546512460637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Steffen K, Myklebust G, Olsen OE, et al. Preventing injuries in female youth football—a cluster-randomized controlled trial. Scand J Med Sci Sports. 2008;18(5):605–614. doi: 10.1111/j.1600-0838.2007.00703.x. [DOI] [PubMed] [Google Scholar]
- 77.Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33(4):492–501. doi: 10.1177/0363546504269591. [DOI] [PubMed] [Google Scholar]
- 78.Hewett TE, Torg JS, Boden BP. Video analysis of trunk and knee motion during non-contact anterior cruciate ligament injury in female athletes: lateral trunk and knee abduction motion are combined components of the injury mechanism. Br J Sports Med. 2009;43(6):417–422. doi: 10.1136/bjsm.2009.059162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Zazulak BT, Hewett TE, Reeves NP, et al. Deficits in neuromuscular control of the trunk predict knee injury risk: a prospective biomechanical-epidemiologic study. Am J Sports Med. 2007;35(7):1123–1130. doi: 10.1177/0363546507301585. [DOI] [PubMed] [Google Scholar]
- 80.Sugimoto D, Myer GD, Bush HM, et al. Compliance with neuromuscular training and anterior cruciate ligament injury risk reduction in female athletes: a meta-analysis. J Athl Train. 2012;47(6):714–723. doi: 10.4085/1062-6050-47.6.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.van Reijen M, Vriend I, van Mechelen W, et al. Compliance with sport injury prevention interventions in randomised controlled trials: a systematic review. Sports Med. 2016;46:1125–1139. doi: 10.1007/s40279-016-0470-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Joy E, Taylor JR, Novak M, et al. Factors influencing the implementation of ACL injury prevention strategies by girls soccer coaches. J Strength Cond Res. 2013;27(8):2263–2269. doi: 10.1519/JSC.0b013e31827ef12e. [DOI] [PubMed] [Google Scholar]
- 83.Benjaminse A, Gokeler A, Dowling AV, et al. Optimization of the anterior cruciate ligament injury prevention paradigm: novel feedback techniques to enhance motor learning and reduce injury risk. J Orthop Sports Phys Ther. 2015;45(3):170–182. doi: 10.2519/jospt.2015.4986. [DOI] [PubMed] [Google Scholar]
- 84.LaBella CR, Huxford MR, Grissom J, et al. Effect of neuromuscular warm-up on injuries in female soccer and basketball athletes in urban public high schools: cluster randomized controlled trial. Arch Pediatr Adolesc Med. 2011;165(11):1033–1040. doi: 10.1001/archpediatrics.2011.168. [DOI] [PubMed] [Google Scholar]
- 85.Olsen OE, Myklebust G, Engebretsen L, et al. Exercises to prevent lower limb injuries in youth sports: cluster randomised controlled trial. BMJ (Clinical research ed) 2005;330(7489):449. doi: 10.1136/bmj.38330.632801.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Sugimoto D, Myer GD, Foss KD, et al. Dosage effects of neuromuscular training intervention to reduce anterior cruciate ligament injuries in female athletes: meta- and sub-group analyses. Sports Med. 2014;44(4):551–562. doi: 10.1007/s40279-013-0135-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Caraffa A, Cerulli G, Projetti M, et al. Prevention of anterior cruciate ligament injuries in soccer: a prospective controlled study of proprioceptive training. Knee Surg Sports Traumatol Arthrosc. 1996;4:19–21. doi: 10.1007/BF01565992. [DOI] [PubMed] [Google Scholar]
- 88.Risberg MA, Mork M, Jenssen HK, et al. Design and implementation of a neuromuscular training program following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2001;31(11):620–631. doi: 10.2519/jospt.2001.31.11.620. [DOI] [PubMed] [Google Scholar]
- 89.Wilk KE, Macrina LC, Cain EL, et al. Recent advances in the rehabilitation of anterior cruciate ligament injuries. J Orthop Sports Phys Ther. 2012;42(3):153–171. doi: 10.2519/jospt.2012.3741. [DOI] [PubMed] [Google Scholar]
- 90.Heitkamp HC, Horstmann T, Mayer F, et al. Gain in strength and muscular balance after balance training. Int J Sports Med. 2001;22:285–290. doi: 10.1055/s-2001-13819. [DOI] [PubMed] [Google Scholar]
- 91.Myklebust G, Engebretsen L, Braekken IH, et al. Prevention of anterior cruciate ligament injuries in female team handball players: a prospective intervention study over three seasons. Clin J Sport Med. 2003;13(2):71–78. doi: 10.1097/00042752-200303000-00002. [DOI] [PubMed] [Google Scholar]


