Abstract
Purpose of Review
The purpose of this paper is to identify strategies for a successful transition to sports in patients following rehabilitation for ACL reconstruction surgery (ACLR).
Recent Findings
Recent research continues to demonstrate a relatively low rate of return to previous level of play among athletes following ACLR combined with a significant risk of injury to either the ipsi or the contralateral ACL. Recent research also demonstrates a growing use of a varied battery of assessments to determine readiness to return to sport as well as a lack of consensus on the ideal rehabilitation program, the criteria for clearance for return to play (both in time from surgery and functional milestones), and the nature of a conditioning program designed specifically for transitioning the cleared athlete back to competition.
Summary
Due to the lack of consensus and consistency regarding rehabilitation protocols and criteria for clearance to play after ACLR, deficits in strength, neuromuscular control, and psychological readiness may exist in “cleared” athletes. These deficits may not only negatively impact sports performance but also raise the risk of re-injury. Programs designed to successfully return an athlete to previous level of play should include not only strength and conditioning aimed at restoring fitness that was compromised as a result of the injury but also include attention to psychological readiness and address deficits in neuromuscular control. Problems that exist following ACLR cannot be solved by one professional; successful rehabilitation and return to play require a coordinated effort among the surgeon, physical therapist, athletic trainer, and fitness professional. Future research is needed to determine the optimal strategy to restore the neuromuscular control, functional strength, and psychological readiness necessary for a successful return to competition following ACLR.
Electronic supplementary material
The online version of this article (doi:10.1007/s12178-017-9419-2) contains supplementary material, which is available to authorized users.
Keywords: ACL, ACLR, Return-to-sport, Sports performance, Injury prevention, Re-injury
Introduction
Approximately 200,000 ACL injuries occur annually in the USA, and evidence indicates that the incidence of this devastating injury is increasing, particularly in the adolescent age group [1, 2]. The majority of ACL injuries are non-contact, and athletes who participate in cutting and pivoting sports are at the greatest risk [3, 4]. The primary aim of ACL reconstruction surgery is to restore normal function of the knee and allow the athlete to return to the previous level of play. Recent research suggests that achieving this goal remains elusive; the rate of return to play remains relatively low while the risk of re-injury remains unacceptably high.
Ardern’s 2010 review reported a 66% rate of return to pre-injury level of sports participation and less than half returning to competitive sport at the previous level of play [5]. The updated review in 2014 showed that little had changed; 65% of the athletes reported returning to pre-injury level of sport following ACLR and 55% reported returning to a competitive level of play [6•] with similar numbers reported following revision surgery [7•, 8]. This overall rate of return is consistent with data reported for professional athletes [9, 10] as well as college and high school level athletes [11]. One might expect significantly greater success among professional and collegiate athletes; these are presumably athletes with access to the best in rehabilitation and strength and conditioning resources, adequate time to devote to rehabilitation, and the inherent athleticism and baseline fitness to create the best odds for a successful return to pre-injury level of play.
Among professional athletes, the evidence is mixed regarding athletic performance among those who return to competition following ACLR. A drop in performance has been reported in NBA players and professional soccer players who return to competition after ACLR [4, 9, 12] while performance consistent with pre-injury statistics has been reported in professional hockey players, skiers, and snowboarders [13, 14]. Data from the MOON (Multicenter Orthopedic Outcomes Network) group demonstrates negative outcomes for high school and college athletes with only 43% reporting returning to play at their previous level [11]. Data from recreational athletes shows similar results with roughly half reporting returning to their previous level of play following ACLR [15].
The risk of incurring a second injury—either to the ipsi or the contralateral knee—also remains significant. A recent meta-analysis of risk of secondary injury reported an overall re-injury rate of 15% with roughly equal risk to the ipsi and contralateral knee. Patients under age 25 faced a 20% risk of secondary injury as did athletes of any age who returned to playing sports (21% risk). The combination of young age and return to sport resulted in a 23% risk of secondary injury [16]. Female gender further elevates this risk with a reported 30% risk of secondary injury in this group [17].
Considering this relatively low rate of return to pre-injury level of play, this alarmingly high risk of secondary injury, and the reports of long-term detrimental effects on joint health and quality of life [18], there is clearly a need to improve our ability to guide athletes to a successful transition back to their previous level of activity.
Lack of Consensus Regarding Rehab Protocols Following ACLR
Despite the growing incidence of ACL injuries [1] and the resulting experience with rehabilitating this injury, there remains a lack of consensus regarding optimal rehabilitation protocols and criteria for return to play. The variability in clinical opinions among AAOS orthopedic surgeons who perform ACLR reported in 2003 [19] seems to persist today. A recent review of Physical Therapy Protocols for ACLR from US academic orthopedic surgery programs revealed wide variation in the composition and recommended length of rehabilitation programs [20]. Less than a third of these protocols recommended a pre-habilitation program despite evidence of better functional outcomes and higher rates of return to pre-injury activity in patients who received physical therapy prior to surgery [21•]. Fewer than 20% recommended achieving specific strength and activity criteria prior to returning to sport despite the well-documented high risk of secondary injury and relatively low rate of successful return to play. Return to sport was not even mentioned as a goal of rehabilitation in 12% of the protocols.
Despite awareness of the need for better outcomes for athletes returning to play following ACLR, there remains significant inconsistency in the criteria used for return to sport clearance and no clear guidelines on the transition from being “cleared” to being ready for full competition.
Return to Sport Criteria
Time from surgery is commonly cited in return to sport decision-making [19, 22]. In a 2011 review of studies of return to sports participation, one third reported time from surgery as the sole criterion in determining readiness to play [22]. Recent research suggests outcomes may be achieved by delaying clearance to play. A 51% reduction in re-injury rate has recently been reported for each month that return to sport was delayed until 9 months after surgery [23••]. Evidence from a 2016 prospective study by Capin supports the value of prolonging return to sports beyond 6 months post-surgery [24]. Young female athletes who sustained a second injury reached criterion-based return-to-sport standards sooner and were cleared for return sooner than those that did not sustain a second injury (6.8 ± 1.5 vs 9.5 ± 1.9 months) despite exhibiting a more normal gait pattern than those that did not re-injure. Extending the return to sport for 2 years following surgery has been proposed based on evidence of time required to re-establish biological joint health and function [25••]. Despite this evidence, 6 months remain a common expectation among surgeons, therapists, and coaches for both professional and recreational athletes [19, 26].
Recent research indicates that it is the rare patient who is without functional deficits 6 months after ACLR. In studies of return to sport testing protocols that include a variety of combinations of hop tests, isokinetic strength testing, LESS scores, IKDC, and ACL-RSI scores, the percentage of patients who met passing criteria was 0–7% at 6 months [27•, 28, 29].
In addition to qualitative evaluations (hop tests, isokinetic strength testing, KT1000) performed at 6 months post-surgery, our institution incorporates a Quality of Movement Assessment (QMA®). The QMA consists of 10 tasks progressing from double to single limb vertical and horizontal movements (squat, single leg stance, forward step down, single leg squat, single leg bridge, jump in place, side-to-side jump, broad jump, hop to opposite leg, single leg hop). Tasks are videotaped as well as evaluated live from the frontal and sagittal plane by a physical therapist and strength and conditioning specialist. The patient’s movements are evaluated for strategy, depth, control, symmetry, and alignment with the focus on identifying movements associated with risk of ACL injury [30–32]. A musculoskeletal evaluation is also performed to determine joint range of motion of the lower extremities (hips, knees, ankles). In 136 patients who underwent a Quality of Movement Assessment at 5–7 months post-ACLR, 60% demonstrated movement patterns associated with risk of ACL injury in more than 50% of the tasks. No significant difference was noted between males and females. This prevalence of faulty movement patterns is consistent with the previously cited data demonstrating significant functional deficits in the majority of patients at 6 months post-ACLR [33].
A varied battery of tests has recently been proposed to determine readiness to return to play including various measures of Limb Symmetry Index (LSI) from hop tests, strength tests, as well as measures of quality of movement, psychological readiness, and Patient Reported Outcome Measures (PROMs) [27•, 34•, 35••, 36••, 37•, 38–40, 41•]. This recent call for a comprehensive battery of tests to determine readiness to return to play has not yet been answered, and a widely accepted and implemented gold standard for determining readiness to return to play does not currently exist leaving a wide gap between completion of traditional physical therapy and true readiness for play.
From Rehabilitation to Performance
Lack of consensus regarding optimal rehabilitation protocols, lack of a gold standard of return to sport criteria, as well as insurance and financial constraints may all contribute to patients being cleared to discontinue rehabilitation and return to play. Pressure from coaches or family or the athlete’s own desire to return may also result in a decision to return to play regardless of readiness. Coaches, athletic trainers, strength and conditioning specialists, and personal trainers are all faced with athletes returning to sports participation following ACLR who may need far more than a simple resumption of sport-specific training. Rehabilitation does not end with the transition from physical therapy back to sport-specific training and requires a coordinated effort between the physical therapist and the fitness professional, as well as the athletic trainer when involved—teamwork that seems to be the exception rather than the rule in current practice. The cleared athlete may range from a recreational athlete 6 months post-surgery with significant strength deficits to a professional athlete who has progressed through extensive rehabilitation. Regardless, regaining and enhancing sports performance will require ongoing attention to a range of factors specific to this population. As would apply to any athlete, the fitness professional must ensure that the athlete has adequate mobility, strength, fatigue resistance, and motor skill to meet the demands of the sport. In addition, the sensorimotor deficits, neuromuscular control, and psychological impact of this injury must be addressed if successful sports performance is to be achieved.
Bridging the Gap from Rehabilitation to Performance
The transition back to unrestricted play should be a gradual process with a focus on functional deficits. The “gap” results when an athlete is cleared after completing a course of physical therapy and shifts to solely sport-specific training while deficits related to the injury persist. Many patients are ready to begin transitioning to sports-specific activity after 6 months of rehabilitation, but the focus on developing functional strength and neuromuscular control should continue. A well-rounded strength and conditioning program with a primary focus on proper movement patterns, single limb alignment, strength, endurance, and motor control should be the foundation to build higher level sports-specific training and conditioning. A gradual, periodized return to the workloads associated with competition is critical to building sport-specific fatigue resistance and successfully transitioning the athlete back to the field.
Understanding the Common Deficits
Since the main focus during rehabilitation is restoring strength and motion to the affected limb, it is unlikely that the athlete will maintain the previous level of cardiovascular fitness and overall conditioning. Many patients will lack either the time, the motivation, or the resources to supplement their physical therapy sessions with attention to overall fitness. Deficits in alignment, symmetry, control, balance, eccentric quadriceps strength, and cardiovascular fitness are common and must be addressed in the transition period from physical therapy to sports performance. Bridging the gap between these deficits and safely returning the athlete back to their chosen sport should be the main focus of fitness professional.
Mobility
Restoring normal knee joint ROM is one of the standard components of rehabilitation protocols following ACLR [20, 35••, 42–44] Ensuring adequate mobility in the hip and ankle is also critical to provide the best chance for optimal movement patterns. In a 2015 update on ACL reconstruction and rehabilitation, Nyland suggests that inhibition of the quadriceps and upregulation of the hip abductor/external rotators and ankle plantar flexors may result in compromised tissue extensibility in these regions which would affect movement patterns [41•]. Valgus in the knee may result from limitations in dorsiflexion. Ongoing attention to adequate mobility is essential to maximize the ability of the athlete to maintain alignment of the knee during functional movements.
Using foam rollers and other soft tissue tools can help address tissue restriction and allow for reciprocal muscle groups to work more efficiently. Table 1 describes a mobility strategy involving self-myofascial release, stretching, and activating the reciprocal muscle groups. For example, foam rolling the anterior thigh is followed by statically stretching the hip flexor quad complex, then patterning the glute to fire by performing a glute bridge with a band above the knees for added abduction strengthening.
Motor Learning
ACL injuries are not simply musculoskeletal injuries but also have central nervous system implications. Local mechanoreceptors and sensory nerves are disrupted leading to changes in sensorimotor cortical areas and subsequent changes in motor patterns [45–49]. The timeline for resolution of proprioceptive deficits appears to extend beyond the usual course of physical therapy and return to sports [25••, 50]. It is incumbent on the fitness professional to include an ongoing focus on neuromuscular control and patterning optimal movement patterns. Developing and retaining changes in movement patterns require long-term repetition [51] and therefore should be a standard component of the conditioning program in the athlete cleared to play following ACLR. Developing reliable neuromuscular control even in a fatigued state is critical to prevent secondary injury as well as to maximize sports performance.
Establishing proper squat mechanics is essential to develop optimal mechanics in any sport. Many athletes will present with valgus patterns at the knee, asymmetrical shifting, and knee-dominant movement patterns. Figure 1 demonstrates an athlete hyperextending the lower back while performing a knee-dominant squat. When looking at the squat pattern from the front (Fig. 2), the same athlete is presenting with internal rotation of the femur, valgus at the knee, and a collapsed foot. When viewing the squat pattern from behind (Fig. 3), the athlete presents with a lateral shift of the hips toward the unaffected side.
Fig. 1.

Poor squat form, side view. Athlete presents with hyperextension of lumbar spine and knees traveling past toes
Fig. 2.
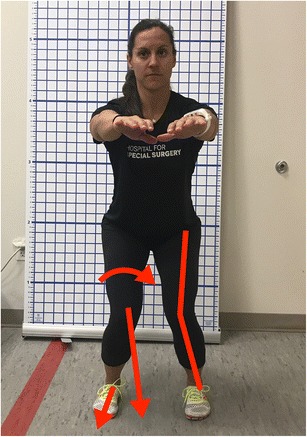
Poor squat form, front view. Athlete presents with internal femoral rotation, knee abduction, and collapsed foot
Fig. 3.
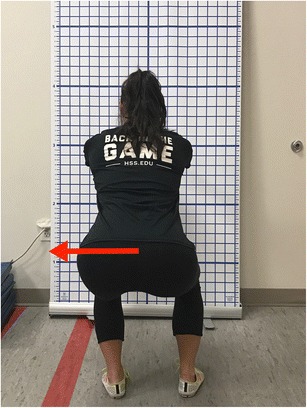
Poor squat form, back view. Athlete presents with a lateral shift of hips to the left
There are several strategies to correct squat deficits. For example, with the athlete in front of a bench or chair, have the athlete reach the hips back toward chair while allowing the chest to fall slightly forward. The goal of this exercise is for the athlete to understand how to sit back into the hips and create a hip hinge correctly. Once in this position, have the athlete perform anterior (Fig. 4a) and posterior (Fig. 4b) tilts. A basic pelvic tilt will allow the athlete to have a better understanding of core control and femoral rotation. Once the athlete demonstrates good control and a proper hip hinge, the next step is to address the valgus alignment and squat symmetry. Add a resistance band above the knee and have the athlete return back into a quarter squat position with a neutral pelvis and spine. Cue the athlete to separate the band slightly, so the lower limbs are vertical while ensuring the foot remains straight. Have the athlete slowly lower one knee toward the midline while maintaining good alignment at the pelvis, spine, and opposite knee. This exercise will help develop eccentric control of the external rotators of the hip. Having control over this pelvic and femoral separation will promote proper motor control and alignment.
Fig. 4.
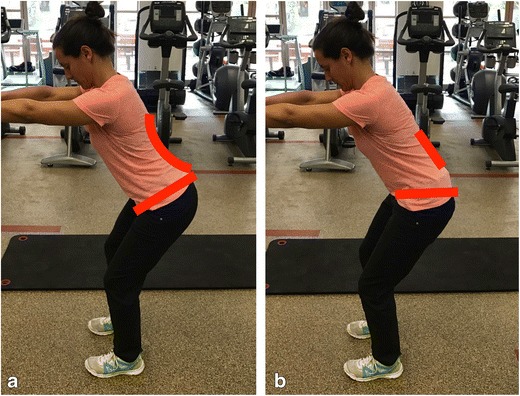
a Anterior pelvic tilt. Athlete moves pelvis through anterior tilt by arching lower back and tipping pelvis forward. b Posterior pelvic tilt. Athlete moves pelvis through posterior tilt by flattening lower back and tipping pelvis backward
Single limb motor control should start by addressing simple single limb stance. Look for posture, and overall alignment and control. Figure 5a demonstrates a common single leg stance for an athlete recovering from ACLR. Note the contralateral pelvic drop and rotation and femoral internal rotation. Figure 5b shows proper alignment and control while standing on one limb. Notice that the pelvis is now level and square, allowing for the knee to point toward the toe line. Getting the athlete set in the correct position prior to moving will help further educate what proper form and control feels and looks like.
Fig. 5.
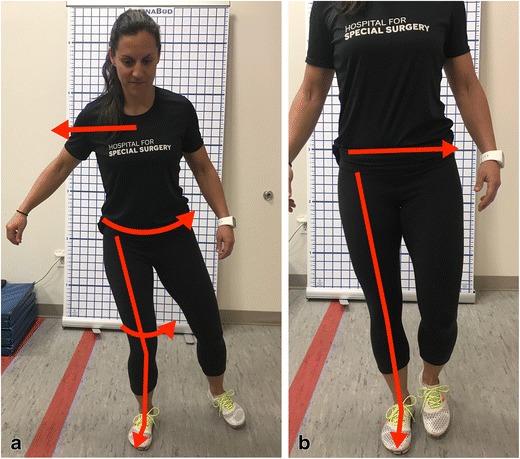
a Poor single leg stance. Athlete presents with a lateral shift of trunk, pelvis rotating backward, femoral internal rotation, knee abduction, and a collapsed foot. b Proper single leg stance. Athlete presents with level pelvis and proper hip, knee, and foot alignment
Similar to the squat, many of these athletes present with pelvic obliquity, valgus at the knee, and poor foot control in a single leg squat. Figure 6 demonstrates lack of alignment at the hip, knee, and foot. Table 2 illustrates a clock exercise with an emphasis on alignment and control. The athlete begins by setting up in a quarter squat position with proper hip, knee, and ankle positioning. Have the athlete shift 90% of the body weight to one side, keeping the weight in the mid foot, all without losing proper alignment. The opposite heel should be elevated so that the athlete is light on the forefoot and securely planted on the stance leg. Next, have the athlete tap the foot forward, lateral, and backward, all without losing alignment and control. To progress this exercise, an elastic band, foam surface, or both can be added.
Fig. 6.

Poor single leg squat form. Athlete presents when single leg squatting with pelvis rotated backward and dropped, knee abduction, and collapsed foot
Strength
Limb Symmetry Index is one criterion used to determine readiness to return to play; patients must demonstrate 85–90% symmetry on isokinetic testing or hop tests to be cleared. However, isokinetic testing involves relatively few repetitions of an open-chain, concentric movement and hop tests similarly require just a few repetitions of a planned and uncontested movement. It is unclear whether a 10–15% deficit in strength poses a significant risk to an athlete who then returns to the sustained efforts and unpredictable demands involved in sports participation. Strength deficits have been reported to persist for up to 3 years following ACLR [52–55]. In addition, strength measured by isokinetic testing and hop tests have not been validated as reliable predictors of successful return to sports [40].
Restoring and maintaining symmetrical strength should be an ongoing component of the athlete’s training program following ACL injury. The fitness professional should pay close attention to symmetry in double limb strength training exercises (squats, dead lifts) and incorporate single limb strengthening exercises (single leg squats, single leg dead lifts, lunges). Single limb strength and endurance should be the foundation of the training program and should consistently be worked on throughout the return to play process as seen in Table 3. Once proper alignment and limb control are demonstrated, the fitness professional can progress to loading patterns and building absolute strength, endurance, and, finally, explosiveness and power. When transitioning from therapy to performance training, many athletes still present a deficit in quadriceps strength and control and use compensatory movement patterns to navigate around weakness. Figure 7a demonstrates an athlete reaching toward the floor with the opposite limb when performing a step down to compensate for poor eccentric quadriceps strength. Bridging the strength gap between each leg and building adequate eccentric strength and control is key, and the eccentric leg press is a good place to start when compensatory movement patterns are present. The athlete should press up with two legs and slowly lower with the affected limb (Fig. 7b). The weight should be challenging and the pace very slow. The athlete should focus on good alignment and control and count slowly to 10 before completely lowering. Take note of any weak links in the entire range of motion and focus on holding any weak positions for 3–5 s to build strength and endurance. Have the athlete perform five repetitions and gradually increase weight when good control is observed.
Fig. 7.
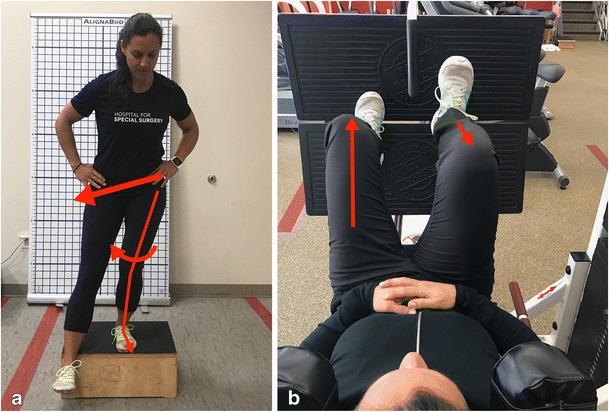
a Poor forward step down form. Athlete presents with dropped pelvis, femoral internal rotation, and collapsed foot. b Single leg eccentric leg press. Athlete slowly controls eccentric movement with correct knee alignment
Building single leg squat strength will help build motor control as well as overall strength and the athlete’s confidence in loading the limb. The single leg squat can be a very challenging exercise to master and should be gradually progressed throughout the strength and conditioning program. Starting the athlete with the opposite foot elevated on a small yoga block will allow for proper form when first building strength. This also tends to slightly hike the contralateral hip in the air, allowing for the athlete to feel the gluteals work more efficiently. When the athlete masters this movement and builds symmetrical strength, substitute the block with a small medicine ball. Now, the athlete must focus on balance and control while maintaining proper alignment. Advancing the movement further, remove the ball and have the athlete single leg squat freely to a bench. To challenge proprioception and motor control, have the athlete stand on a foam pad or bosu ball and slowly perform single leg squats while maintaining proper alignment. When performing this movement, some repetitions may not be ideal but will allow the athlete to build both strength and control.
Sport-Specific Skill
The transition from sport-specific drills performed deliberately in an uncontested situation to full competition should be gradual and dictated by the athlete’s progress in gaining the strength and control necessary to perform well on the field. As strength, power, and neuromuscular control improves, so does the intensity and duration of sport-specific skill training. Blanch and Gabbett have proposed a system of quantifying an acute/chronic workload ratio to identify a safe progression for an athlete returning to full competition after an injury [56]. This model provides a useful tool for developing an individualized and safe training plan. See Table 4 for later stage progressions aimed at developing strength, power, coordination, and, most importantly, confidence in performing unanticipated, multi-directional movement patterns.
Psychological Factors
Besides restoring physical strength and sport-specific skill, the performance specialist must be sensitive to the psychological impact of this injury. Psychological factors such as fear of re-injury have been increasingly recognized in the literature as key determinants of a successful return to sport after ACLR. [8, 36••, 37•, 38, 39, 57, 58, 59•, 60]. Following a gradual and systematic approach to return to sport while monitoring milestones in strength, fatigue resistance, motor control, and sport-specific skill should contribute to building psychological readiness for a full return to pre-injury activity.
Conclusion
The traditional trajectory for an athlete after ACLR is a course of physical therapy followed by clearance from the surgeon to return to sport. Based on the low rates of successful return to sport and high incidence or re-injury, this model does not seem to be serving these athletes well. Recent research has focused on identifying the battery of tests that will best indicate readiness to return to play as well as broadening the return to play decision-making process to include input from a multi-disciplinary team and consideration of factors beyond time from surgery [25••, 36••, 41•, 44, 61–63]. Perhaps it is time to move away from a binary decision regarding return to sports made after several months of traditional physical therapy and re-frame the trajectory after ACLR as a journey with a series of milestones along the way. Dingenen and Gokeler have recently described this “optimized return to sport approach” [36••] which involves shared decision-making and careful supervision of the athlete far beyond 6 months after surgery. Ongoing communication between all members of the return to sport team (surgeon, physical therapist, fitness professional, athletic trainer, sport psychologist, coach) is critical for this model to succeed. By recognizing, understanding, and addressing the lingering effects of this injury in a systematic manner, the fitness professional has the potential to provide the missing link in the transition from physical therapy to successful return to sports performance.
Electronic supplementary material
(DOCX 677 kb)
(DOCX 394 kb)
(DOCX 690 kb)
(DOCX 1560 kb)
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors. Additional informed consent was obtained from all individual participants for whom identifying information is included in this article.
Footnotes
This article is part of the Topical Collection on ACL Rehab
Electronic supplementary material
The online version of this article (doi:10.1007/s12178-017-9419-2) contains supplementary material, which is available to authorized users.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Dodwell ER, Lamont LE, Green DW, Pan TJ, Marx RG, Lyman S. 20 years of pediatric anterior cruciate ligament reconstruction in New York State. Am J Sports Med. 2014;42:675–680. doi: 10.1177/0363546513518412. [DOI] [PubMed] [Google Scholar]
- 2.Kim S, Bosque J, Meehan JP, Jamali A, Marder R. Increase in outpatient knee arthroscopy in the United States: a comparison of National Surveys of Ambulatory Surgery, 1996 and 2006. J Bone Joint Surg Am. 2011;93:994–1000. doi: 10.2106/JBJS.I.01618. [DOI] [PubMed] [Google Scholar]
- 3.Andernord D, Desai N, Björnsson H, Ylander M, Karlsson J, Samuelsson K. Patient predictors of early revision surgery after anterior cruciate ligament reconstruction: a cohort study of 16,930 patients with 2-year follow-up. Am J Sports Med. 2015;43:121–127. doi: 10.1177/0363546514552788. [DOI] [PubMed] [Google Scholar]
- 4.Brophy RH, Stepan JG, Silvers HJ, Mandelbaum BR. Defending puts the anterior cruciate ligament at risk during soccer: a gender-based analysis. Sports Health. 2015;7:244–249. doi: 10.1177/1941738114535184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ardern CL, Webster KE, Taylor NF, Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med. 2011;45:596–606. doi: 10.1136/bjsm.2010.076364. [DOI] [PubMed] [Google Scholar]
- 6.Ardern CL, Taylor NF, Feller JA, Webster KE. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48:1543–1552. doi: 10.1136/bjsports-2013-093398. [DOI] [PubMed] [Google Scholar]
- 7.Grassi A, Zaffagnini S, Marcheggiani Muccioli GM, Neri MP, Della Villa S, Marcacci M. After revision anterior cruciate ligament reconstruction, who returns to sport? A systematic review and meta-analysis. Br J Sports Med. 2015;49:1295–1304. doi: 10.1136/bjsports-2014-094089. [DOI] [PubMed] [Google Scholar]
- 8.Lefevre N, Klouche S, Mirouse G, Herman S, Gerometta A, Bohu Y. Return to sport after primary and revision anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45:34–41. doi: 10.1177/0363546516660075. [DOI] [PubMed] [Google Scholar]
- 9.Shah VM, Andrews JR, Fleisig GS, McMichael CS, Lemak LJ. Return to play after anterior cruciate ligament reconstruction in National Football League athletes. Am J Sports Med. 2010;38:2233–2239. doi: 10.1177/0363546510372798. [DOI] [PubMed] [Google Scholar]
- 10.Waldén M, Hägglund M, Magnusson H, Ekstrand J. ACL injuries in men’s professional football: a 15-year prospective study on time trends and return-to-play rates reveals only 65% of players still play at the top level 3 years after ACL rupture. Br J Sports Med. 2016;50:744–750. doi: 10.1136/bjsports-2015-095952. [DOI] [PubMed] [Google Scholar]
- 11.McCullough KA, Phelps KD, Spindler KP, Matava MJ, Dunn WR, Parker RD, Reinke EK. Return to high school- and college-level football after anterior cruciate ligament reconstruction: a Multicenter Orthopaedic Outcomes Network (MOON) cohort study. Am J Sports Med. 2012;40:2523–2529. doi: 10.1177/0363546512456836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Busfield BT, Kharrazi FD, Starkey C, Lombardo SJ, Seegmiller J. Performance outcomes of anterior cruciate ligament reconstruction in the National Basketball Association. Arthroscopy. 2009;25:825–830. doi: 10.1016/j.arthro.2009.02.021. [DOI] [PubMed] [Google Scholar]
- 13.Erickson BJ, Harris JD, Fillingham YA, Cvetanovich GL, Bhatia S, Bach BR, Bush-Joseph CA, Cole BJ. Performance and return to sport after anterior cruciate ligament reconstruction in X-Games skiers and snowboarders. Orthop J Sports Med. 2013;1:2325967113511196. doi: 10.1177/2325967113511196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Erickson BJ, Harris JD, Cole BJ, Frank RM, Fillingham YA, Ellman MB, Verma NN, Bach BR. Performance and return to sport after anterior cruciate ligament reconstruction in National Hockey League players. Orthop J Sports Med. 2014;2:2325967114548831. doi: 10.1177/2325967114548831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rodríguez-Roiz JM, Caballero M, Ares O, Sastre S, Lozano L, Popescu D. Return to recreational sports activity after anterior cruciate ligament reconstruction: a one- to six-year follow-up study. Arch Orthop Trauma Surg. 2015;135:1117–1122. doi: 10.1007/s00402-015-2240-8. [DOI] [PubMed] [Google Scholar]
- 16.Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med. 2016;44:1861–1876. doi: 10.1177/0363546515621554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. Am J Sports Med. 2014;42:1567–1573. doi: 10.1177/0363546514530088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Risberg MA, Oiestad BE, Gunderson R, Aune AK, Engebretsen L, Culvenor A, Holm I. Changes in knee osteoarthritis, symptoms, and function after anterior cruciate ligament reconstruction: a 20-year prospective follow-up study. Am J Sports Med. 2016;44:1215–1224. doi: 10.1177/0363546515626539. [DOI] [PubMed] [Google Scholar]
- 19.Marx RG, Jones EC, Angel M, Wickiewicz TL, Warren RF. Beliefs and attitudes of members of the American Academy of Othopaedic Surgeons regarding the treatment of anterior cruciate ligament injury. Arthroscopy. 2003;19:762–770. doi: 10.1016/S0749-8063(03)00398-0. [DOI] [PubMed] [Google Scholar]
- 20.Makhni EC, Crump EK, Steinhaus ME, Verma NN, Ahmad CS, Cole BJ, Bach BR. Quality and variability of online available physical therapy protocols from academic orthopaedic surgery programs for anterior cruciate ligament reconstruction. Arthroscopy. 2016;32:1612–1621. doi: 10.1016/j.arthro.2016.01.033. [DOI] [PubMed] [Google Scholar]
- 21.Failla MJ, Logerstedt DS, Grindem H, Axe MJ, Risberg MA, Engebretsen L, Huston LJ, Spindler KP, Snyder-Mackler L. Does extended preoperative rehabilitation influence outcomes 2 years after ACL reconstruction? A comparative effectiveness study between the MOON and Delaware-Oslo ACL cohorts. Am J Sports Med. 2016;44:2608–2614. doi: 10.1177/0363546516652594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Barber-Westin SD, Noyes FR. Factors used to determine return to unrestricted sports activities after anterior cruciate ligament reconstruction. Arthroscopy. 2011;27:1697–1705. doi: 10.1016/j.arthro.2011.09.009. [DOI] [PubMed] [Google Scholar]
- 23.Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med. 2016;50:804–808. doi: 10.1136/bjsports-2016-096031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Capin JJ, Khandha A, Zarzycki R, Manal K, Buchanan TS, Snyder-Mackler L. Gait mechanics and second ACL rupture: implications for delaying return-to-sport. J Orthop Res. 2016. doi:10.1002/jor.23476. [DOI] [PMC free article] [PubMed]
- 25.Nagelli CV, Hewett TE. Should return to sport be delayed until 2 years after anterior cruciate ligament reconstruction? Biological and functional considerations. Sports Med. 2017;47:221–232. doi: 10.1007/s40279-016-0584-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Erickson BJ, Harris JD, Fillingham YA, Frank RM, Bush-Joseph CA, Bach BR, Cole BJ, Verma NN. Anterior cruciate ligament reconstruction practice patterns by NFL and NCAA football team physicians. Arthroscopy. 2014;30:731–738. doi: 10.1016/j.arthro.2014.02.034. [DOI] [PubMed] [Google Scholar]
- 27.Gokeler A, Welling W, Zaffagnini S, Seil R, Padua D. Development of a test battery to enhance safe return to sports after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2017;25:192–199. doi: 10.1007/s00167-016-4246-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Thomeé R, Waldén M, Hägglund M. Return to sports after anterior cruciate ligament injury: neither surgery nor rehabilitation alone guarantees success—it is much more complicated. Br J Sports Med. 2015;49:1422. doi: 10.1136/bjsports-2015-094793. [DOI] [PubMed] [Google Scholar]
- 29.Larsen JB, Farup J, Lind M, Dalgas U. Muscle strength and functional performance is markedly impaired at the recommended time point for sport return after anterior cruciate ligament reconstruction in recreational athletes. Hum Mov Sci. 2015;39:73–87. doi: 10.1016/j.humov.2014.10.008. [DOI] [PubMed] [Google Scholar]
- 30.Paterno MV, Schmitt LC, Ford KR, Rauh MJ, Myer GD, Huang B, Hewett TE. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38:1968–1978. doi: 10.1177/0363546510376053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Burnham JM, Yonz MC, Robertson KE, McKinley R, Wilson BR, Johnson DL, Ireland ML, Noehren B. Relationship of hip and trunk muscle function with single leg step-down performance: implications for return to play screening and rehabilitation. Phys Ther Sport. 2016;22:66–73. doi: 10.1016/j.ptsp.2016.05.007. [DOI] [PubMed] [Google Scholar]
- 32.Hewett TE, Myer GD, Ford KR, Paterno MV, Quatman CE. The 2012 ABJS Nicolas Andry Award: the sequence of prevention: a systematic approach to prevent anterior cruciate ligament injury. Clin Orthop Relat Res. 2012;470:2930–2940. doi: 10.1007/s11999-012-2440-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.de Mille P, Nguyen J, Brown A, Do H, Selvaggio E, Chiaia T. Quality of movement for athletes six months post-ACL reconstruction. Orthop J Sports Med. 2016;4:2325967116S00202. [Google Scholar]
- 34.Kyritsis P, Bahr R, Landreau P, Miladi R, Witvrouw E. Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br J Sports Med. 2016;50:946–951. doi: 10.1136/bjsports-2015-095908. [DOI] [PubMed] [Google Scholar]
- 35.van Melick N, van Cingel REH, Brooijmans F, Neeter C, van Tienen T, Hullegie W, Nijhuis-van der Sanden MWG. Evidence-based clinical practice update: practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. Br J Sports Med. 2016;50:1506–1515. doi: 10.1136/bjsports-2015-095898. [DOI] [PubMed] [Google Scholar]
- 36.•• Dingenen B, Gokeler A. Optimization of the return-to-sport paradigm after anterior cruciate ligament reconstruction: a critical step back to move forward. Sports Med. 2017. doi:10.1007/s40279-017-0674-6. Proposes an optimized, criterion-based, continuous, and multi-factorial return to sport approach within a biopsychosocial framework. [DOI] [PubMed]
- 37.Czuppon S, Racette BA, Klein SE, Harris-Hayes M. Variables associated with return to sport following anterior cruciate ligament reconstruction: a systematic review. Br J Sports Med. 2014;48:356–364. doi: 10.1136/bjsports-2012-091786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Morris RC, Hulstyn MJ, Fleming BC, Owens BD, Fadale PD. Return to play following anterior cruciate ligament reconstruction. Clin Sports Med. 2016;35:655–668. doi: 10.1016/j.csm.2016.05.009. [DOI] [PubMed] [Google Scholar]
- 39.Hamrin Senorski E, Samuelsson K, Thomeé C, Beischer S, Karlsson J, Thomeé R. Return to knee-strenuous sport after anterior cruciate ligament reconstruction: a report from a rehabilitation outcome registry of patient characteristics. Knee Surg Sports Traumatol Arthrosc. 2017;25:1364–1374. [DOI] [PMC free article] [PubMed]
- 40.Undheim MB, Cosgrave C, King E, Strike S, Marshall B, Falvey É, Franklyn-Miller A. Isokinetic muscle strength and readiness to return to sport following anterior cruciate ligament reconstruction: is there an association? A systematic review and a protocol recommendation. Br J Sports Med. 2015;49:1305–1310. doi: 10.1136/bjsports-2014-093962. [DOI] [PubMed] [Google Scholar]
- 41.Nyland J, Mattocks A, Kibbe S, Kalloub A, Greene JW, DNM C. Anterior cruciate ligament reconstruction, rehabilitation, and return to play: 2015 update. Open Access J Sports Med. 2016;7:21. doi: 10.2147/OAJSM.S72332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Adams D, Logerstedt DS, Hunter-Giordano A, Axe MJ, Snyder-Mackler L. Current concepts for anterior cruciate ligament reconstruction: a criterion-based rehabilitation progression. J Orthop Sports Phys Ther. 2012;42:601–614. doi: 10.2519/jospt.2012.3871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wilk KE, Arrigo CA. Rehabilitation principles of the anterior cruciate ligament reconstructed knee: twelve steps for successful progression and return to play. Clin Sports Med. 2017;36:189–232. doi: 10.1016/j.csm.2016.08.012. [DOI] [PubMed] [Google Scholar]
- 44.Joreitz R, Lynch A, Rabuck S, Lynch B, Davin S, Irrgang J. Patient-specific and surgery-specific factors that affect return to sport after acl reconstruction. Int J Sports Phys Ther. 2016;11:264–278. [PMC free article] [PubMed] [Google Scholar]
- 45.Kapreli E. Anterior cruciate ligament deficiency causes brain plasticity: a functional MRI study. Am J Sports Med. 2009;37:2419–2426. doi: 10.1177/0363546509343201. [DOI] [PubMed] [Google Scholar]
- 46.Grooms DR, Page SJ, Onate JA. Brain activation for knee movement measured days before second anterior cruciate ligament injury: neuroimaging in musculoskeletal medicine. J Athl Train. 2015;50:1005–1010. doi: 10.4085/1062-6050-50.10.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Goerger BM, Marshall SW, Beutler AI, Blackburn JT, Wilckens JH, Padua DA. Anterior cruciate ligament injury alters preinjury lower extremity biomechanics in the injured and uninjured leg: the JUMP-ACL study. Br J Sports Med. 2015;49:188–195. doi: 10.1136/bjsports-2013-092982. [DOI] [PubMed] [Google Scholar]
- 48.Dingenen B, Janssens L, Claes S, Bellemans J, Staes FF. Lower extremity muscle activation onset times during the transition from double-leg stance to single-leg stance in anterior cruciate ligament reconstructed subjects. Clin Biomech (Bristol, Avon) 2016;35:116–123. doi: 10.1016/j.clinbiomech.2016.04.014. [DOI] [PubMed] [Google Scholar]
- 49.Grooms DR, Myer GD. Upgraded hardware—what about the software? Brain updates for return to play following ACL reconstruction. Br J Sports Med. 2017;51:418–19. [DOI] [PMC free article] [PubMed]
- 50.Iwasa J, Ochi M, Adachi N, Tobita M, Katsube K, Uchio Y. Proprioceptive improvement in knees with anterior cruciate ligament reconstruction. Clin Orthop Relat Res. 2000:381:168–76. [DOI] [PubMed]
- 51.Padua DA, DiStefano LJ, Marshall SW, Beutler AI, de la Motte SJ, DiStefano MJ. Retention of movement pattern changes after a lower extremity injury prevention program is affected by program duration. Am J Sports Med. 2012;40:300–306. doi: 10.1177/0363546511425474. [DOI] [PubMed] [Google Scholar]
- 52.Abourezk MN, Ithurburn MP, McNally MP, Thoma LM, Briggs MS, Hewett TE, Spindler KP, Kaeding CC, Schmitt LC. Hamstring strength asymmetry at 3 years after anterior cruciate ligament reconstruction alters knee mechanics during gait and jogging. Am J Sports Med. 2017;45:97–105. doi: 10.1177/0363546516664705. [DOI] [PubMed] [Google Scholar]
- 53.Myer GD, Martin L, Ford KR, Paterno MV, Schmitt LC, Heidt RS, Colosimo A, Hewett TE. No association of time from surgery with functional deficits in athletes after anterior cruciate ligament reconstruction: evidence for objective return-to-sport criteria. Am J Sports Med. 2012;40:2256–2263. doi: 10.1177/0363546512454656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nawasreh Z, Logerstedt D et al. Do patients failing return-to-activity criteria at 6 months after anterior cruciate ligament reconstruction continue demonstrating deficits at 2 years? Am J Sports Med. 2017;45:1037–48. [DOI] [PMC free article] [PubMed]
- 55.Paterno MV, Ford KR, Myer GD, Heyl R, Hewett TE. Limb asymmetries in landing and jumping 2 years following anterior cruciate ligament reconstruction. Clin J Sport Med. 2007;17:258–262. doi: 10.1097/JSM.0b013e31804c77ea. [DOI] [PubMed] [Google Scholar]
- 56.Blanch P, Gabbett TJ. Has the athlete trained enough to return to play safely? The acute:chronic workload ratio permits clinicians to quantify a player’s risk of subsequent injury. Br J Sports Med. 2016;50:471–475. doi: 10.1136/bjsports-2015-095445. [DOI] [PubMed] [Google Scholar]
- 57.Sonesson S, Kvist J, Ardern C, Österberg A, Silbernagel KG. Psychological factors are important to return to pre-injury sport activity after anterior cruciate ligament reconstruction: expect and motivate to satisfy. Knee Surg Sports Traumatol Arthrosc. 2017;25:1375–84. [DOI] [PMC free article] [PubMed]
- 58.Forsdyke D, Gledhill A, Ardern C. Psychological readiness to return to sport: three key elements to help the practitioner decide whether the athlete is REALLY ready? Br J Sports Med. 2017;51:555–6. [DOI] [PubMed]
- 59.Ardern CL, Österberg A, Tagesson S, Gauffin H, Webster KE, Kvist J. The impact of psychological readiness to return to sport and recreational activities after anterior cruciate ligament reconstruction. Br J Sports Med. 2014;48:1613–1619. doi: 10.1136/bjsports-2014-093842. [DOI] [PubMed] [Google Scholar]
- 60.Wu H, Liu M, Dines JS, Kelly JD, Garcia GH. Depression and psychiatric disease associated with outcomes after anterior cruciate ligament reconstruction. World J Orthop. 2016;7:709–717. doi: 10.5312/wjo.v7.i11.709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Creighton DW, Shrier I, Shultz R, Meeuwisse WH, Matheson GO. Return-to-play in sport: a decision-based model. Clin J Sport Med. 2010;20:379–385. doi: 10.1097/JSM.0b013e3181f3c0fe. [DOI] [PubMed] [Google Scholar]
- 62.Shrier I, Safai P, Charland L. Return to play following injury: whose decision should it be? Br J Sports Med. 2014;48:394–401. doi: 10.1136/bjsports-2013-092492. [DOI] [PubMed] [Google Scholar]
- 63.Myer GD, Paterno MV, Ford KR, Quatman CE, Hewett TE. Rehabilitation after anterior cruciate ligament reconstruction: criteria-based progression through the return-to-sport phase. J Orthop Sports Phys Ther. 2006;36:385–402. doi: 10.2519/jospt.2006.2222. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 677 kb)
(DOCX 394 kb)
(DOCX 690 kb)
(DOCX 1560 kb)


