Abstract
Purpose of Review
Because of the epidemiological incidence of anterior cruciate ligament (ACL) injuries, the high reinjury rates that occur when returning back to sports, the actual number of patients that return to the same premorbid level of competition, the high incidence of osteoarthritis at 5–10-year follow-ups, and the effects on the long-term health of the knee and the quality of life for the patient, individualizing the return to sports after ACL reconstruction (ACL-R) is critical. However, one of the challenging but unsolved dilemmas is what criteria and clinical decision making should be used to return an athlete back to sports following an ACL-R. This article describes an example of a functional testing algorithm (FTA) as one method for clinical decision making based on quantitative and qualitative testing and assessment utilized to make informed decisions to return an athlete to their sports safely and without compromised performance. The methods were a review of the best current evidence to support a FTA.
Recent Findings
In order to evaluate all the complicated domains of the clinical decision making for individualizing the return to sports after ACL-R, numerous assessments need to be performed including the biopsychosocial concepts, impairment testing, strength and power testing, functional testing, and patient-reported outcomes (PROs).
Summary
The optimum criteria to use for individualizing the return to sports after ACL-R remain elusive. However, since this decision needs to be made on a regular basis with the safety and performance factors of the patient involved, this FTA provides one method of quantitatively and qualitatively making the decisions. Admittedly, there is no predictive validity of this system, but it does provide practical guidelines to facilitate the clinical decision making process for return to sports. The clinical decision to return an athlete back into competition has significant implications ranging from the safety of the athlete, to performance factors and actual litigation issues. By using a multifactorial FTA, such as the one described, provides quantitative and qualitatively criteria to make an informed decision in the best interests of the athlete.
Electronic supplementary material
The online version of this article (doi:10.1007/s12178-017-9420-9) contains supplementary material, which is available to authorized users.
Keywords: ACL injury, ACL reconstruction, Return to sport, Functional testing, Testing algorithm, Criterion-based progression
Introduction
Anterior cruciate ligament (ACL) knee injuries are common with an estimated prevalence of approximately 350,000 ACL reconstructions performed in the USA annually [1] with roughly one million completed worldwide each year. Following an ACL reconstruction, there are various short-term [2] and long-term [3•] implications that will ultimately affect the health of the knee as well as the overall quality of life for the patient.
Unfortunately, even with appropriate surgery and rehabilitation, there is a high risk of reinjury [4]. This risk for reinjury is multifactorial and made up of not just one isolated source, but various sources working in combination. Nevertheless, a thorough evaluation of the testable and trainable modifiable risk factors associated with reinjury is essential. Certainly one question that has been raised in the literature is: “What are the criteria used for clinical reasoning and decision-making for return to sports (RTS)”? Barber-Westin and Noyes [5] performed a systematic review and found the following criteria from 264 studies: 105 (40%) failed to provide any criteria for RTS, 84 (32%) provided only post-operative time as the sole criteria, 40 (15%) detailed time and subjective criteria, and 35 (13%) focused RTS on objective criteria. Out of the 35 studies, the following objective criteria were used: 9% used muscle strength criteria of 80–90% of quadriceps and hamstrings, 6% use effusion and range of motion, 4% used a single leg hop test, 1 study used stability, and 1 study used validated questionnaires only. Ultimately, many different criteria, both based on time and objective and subjective benchmarks, were shown [5] for assessment to allow for a successful RTS.
Furthermore, Ardern et al. [6•] demonstrated only approximately 55% of patients following an ACL injury returned to their same premorbid level of activity in 314 participants at a mean 39.6 months following surgery. Ardern et al. [6•] listed three non-modifiable criteria as part of the total five that influenced the patient’s ability for RTS including age, male gender, and a positive psychological response. Consequently, when designing a functional testing algorithm (FTA) for RTS, the evaluation criteria should focus on modifiable, instead non-modifiable, risk factors during testing given that treatment interventions can influence them.
Approving a return to sport following an ACL reconstruction is one of the most challenging, complex, and difficult decisions that may be made by a sports medicine team. Therefore, the team including the physician, physical therapist, athletic trainer, strength and conditioning specialist, sport psychologist, and coach need to discuss the decision and arrive at a consensus regarding the ideal time for the patient to return to full activity. In all, several factors must be taken into consideration for a safe return. This ultimately warrants a thorough and honest discussion between all team members.
The topic of return to sports following an ACL injury has seen a recent explosion in the literature. As an example, performing a MedLine Search for “ACL AND return to sports” on January 15, 2017 produced 840 references, including approximately 300 within the last 3 years alone. The majority of the original literature for RTS following ACL reconstruction was temporally focused instead of centered on objective measures. The more current literature, however, focuses RTS around milestone-based progression with examination via objective and functional testing. One of the major trends in the most recent literature is to assess the biopsychosocial aspects of RTS instead of just the physical/physiological parameters. Although all of the biopsychosocial aspects are certainly important to consider for RTS, the focus of this article will be on a quantitative and qualitative FTA criterion-based impairments, strength and power testing, and functional testing.
There are specific categories that have been identified as being important for RTS. The majority of the literature [7–12, 13•, 14•, 15–22] indicates a battery of tests is necessary to assess various outcome parameters and establish criterion-based clinical reasoning for RTS. This review acknowledges multiple tests that should be done aside from medical approval and clearance by the physician to verify a successful RTS such as follows: range of motion, KT1000/KT2000, Lachman’s test, Pivot shift test, isotonic strength tests, isokinetic strength tests, maximum force/peak torque, angle-specific torque testing, rate of force development, hop tests, jump landing tasks (LESS), knee proprioception/kinesthesia/joint position sense testing, quality of movement tests, kinematic analysis, psychological factors/tests based on the anterior cruciate ligament-return to sport after injury (ACL-RSI) scale, PROs: anterior cruciate ligament-return to sport after injury (ACL-RSI) scale, IKDCs, KOOSs, ADL scales, Sport scales, knee self efficacy scale, Quality of Scales, ACL-RSI, Tegner Activity Scale (TAS), Lysholm Scale, and Tampa Kinesiophobia Index.
Despite significant advances concerning ACL injury recognition, surgery, and rehabilitation over the past 40 years, substantial challenges persist for the specific criteria for RTS at the pre-injury level of performance with the ultimate goal of reinjury prevention. Therefore, the purpose of this article is to discuss current literature in selected areas of emphasis for criteria for RTS. Although multiple parameters for RTS have been described, our focus will be on the criteria authors consider most important for a successful RTS. One assessment method based on the use of a FTA, which has been used by the senior author for 37 years, will be described in detail and forms the foundation of this article [23] (Table 1).
Table 1.
Return to sport testing considerations
| Physician approval |
| MRI-based graft maturity |
| Basic measurements |
| Personality type |
| Level of sports activity |
| Patient-reported outcome measures |
| Anterior cruciate ligament—return to spots after injury (ACL-RSI) scale |
| International Knee Documentation Scale (IKDC) |
| Knee orthopedic outcome scales (KOOS) |
| Tegner activity scale |
| Lysholm scale |
| Tampa Kinesiophobia Index |
| Activities of daily living (ADL) scales |
| Sports-specific scales |
| Adequate range of motion |
| Stable KT1000/KT2000 measurements |
| Balance testing/knee proprioceptive tests/kinesthesia/joint position sense testing Quality of movement tests |
| Stable manual ligament stability tests (Lachman’s and Pivot shift) |
| Manual muscle testing/hand held dynamometry—entire lower extremity |
| Isotonic strength tests |
| Isokinetic strength tests |
| Maximum force/peak torque |
| Angle-specific torque |
| Rate of force development |
| Kinematic analysis/gait analysis/running analysis |
| Functional tests |
| Jump tests |
| Hop tests |
| Lower Extremity Functional Test (LEFT) |
| Sport-specific testing |
| Prevention programs |
Methods
A quantitative and qualitative FTA (Fig. 1) has been used for 37 years as the clinical decision making model for criteria for return to sport in the setting of an ACL reconstruction by the senior author. General guidelines about the FTA will be presented first, followed by the specific criterion-based stages. Initially, the patients are stratified into various activity levels including general orthopedic patients, recreational athletes, and competitive athletes. These patients will only be tested to a certain level in the FTA, which represents their activity levels. The FTA is an objective, quantitative, and qualitative method to safely and effectively assesses a patient’s progress from immediate post injury/post-op to return to complete resolution of injury and RTS. Moreover, the purpose of the FTA is to identify a patient’s particular deficits so that they can be addressed through the rehabilitation program. The FTA is divided between strength and power testing and functional tests to evaluate the functional limitations and residual disability, respectively. Each test, and its associated training regimen, successively increases stress on the patient. In all, if the patient demonstrates a deficit in the testing parameter, then the rehabilitation program will focus on rectifying the deficiency. Once a deficit is detected, the patient is retested after an appropriate time frame and allowed to move to the next level of performance if the test is passed. By incrementally testing patients, we found very fast rehabilitation time with a protocol that focuses on interventions specific to the patient’s particular condition and functional status [24].
Fig. 1.
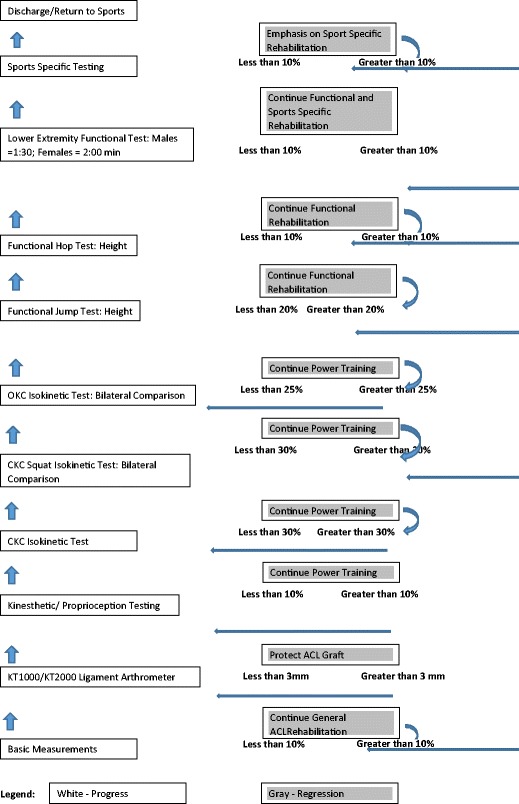
Functional testing algorithm (FTA)
Basic Measurements
Basic measurements include all fundamental tests and measurements involving any examination of a patient. First, these include subjective information including history, and mechanism of injury. Then, from the objective physical examination, it includes observation and posture, gait evaluation, palpation, leg length measurements, anthropometric measurements, referral/related joints, neurological examination, goniometric active range of motion (ROM), passive ROM, manual muscle testing (Resisted ROM), isokinetic testing, flexibility tests, passive mobility testing, patient-reported outcomes (IKDC, Lysholm, etc.), Tampa Kinesiophobia Index, ACL-RSI, and others. Lastly, a thorough understanding of all medications, laboratory tests, and imaging results involving the patient is critical for a relevant examination.
KT 1000/2000 Ligament Stability Testing
Although there is some controversy regarding the use of static ligament stability testing, if equipment is available to objectively document the ligamentous stability, then it should certainly be used. In all, this examination provides a more accurate, more objective assessment of the static restraints compared to manual tests, such as a Lachman’s or pivot shift test, which are subject to possible misinterpretation.
Sensorimotor System Testing: Balance/Proprioceptive Testing
Given that most functional activity in sports occurs in a weight bearing position, we recommend sensorimotor system testing be performed in a weight bearing position. There are a variety of devices that can be used to assess balance, such as a Biodex Balance Stabilometer. Moreover, weight bearing or non-weight bearing angular joint replication testing can also be performed to measure proprioception of the knee. As a result of the report loss of proprioception following an ACL injury, angular joint replication testing is absolutely key [25]. Several recent studies [26–29] have also discussed and stressed the importance of knee proprioception following an ACL injury for the long-term health of the knee.
Closed Kinetic Chain Testing
Controlled closed kinetic chain testing of muscle strength and power should be examined. This can be performed with Linea Isokinetic testing [30], progressive resistive exercise (PRE) testing, wall slide tests, a Vail Sport Cord test, or plyometric-type power tests. When performing closed kinetic chain (CKC) testing, multiple lower extremity muscle groups are being tested simultaneously. Consequently, if there is a deficit, the question remains as to where the specific deficit is located.
Open Kinetic Chain Testing
Open kinetic chain (OKC) or isolated muscle test performance can be performed by manual muscle testing (MMT), hand held dynamometry (HHD), dynamic PRE testing, or dynamic isokinetic testing. There are numerous reasons for performing isolated testing, which include examination of possible interdependency between muscles proximal or distal to the knee to determine any weakness or compensation [31, 32], identification of muscles which may be compensating for a potential weakness within the kinematic chain, and lastly, determination of isolated muscle performance to assess whether or not a muscle may be dependent on other muscles of the kinetic chain.
For many years, clinicians have complained that isokinetic testing is not functionally based. Although this is true, function is made up of individual links, which together construct a kinematic chain. Consequently, if each link in the kinematic chain is not tested, then the presence of a deficit cannot be confirmed. Therefore, we suggest to “test, don’t guess.” Interestingly, several studies demonstrate a correlation between OKC isolated testing and functional performance testing [33–35]. Moreover, although peak torque is the most commonly assessed value in over 3000 articles (PubMed Search, January 15, 2017) dealing with isokinetic testing of the knee, we continue to recommend [36–38] that angle-specific torque, total work, average power, and rate of force development be examined as part of a full patient muscle performance evaluation. This is based on previous findings, which show that quadriceps force development deficits are one of the primary limiting factors in RTS [39–42]. Ultimately, the ability to generate force quickly is a key factor in muscular performance and a successful RTS. As part of a full examination, bilateral comparisons, unilateral ratios, and comparison to sport-specific/position-specific [36] data is necessary.
Functional Jump Tests
When starting to perform functional testing, we begin with a double leg jump test to develop confidence in the patient that they can jump off BOTH legs with the controlled propulsive force [43–45]. However, more importantly, it is a “psychological apprehension” for the patient to have to control the eccentric deceleration landing, particularly for the involved knee. We think it is important for the patient to experience the eccentric deceleration landing response with both legs before they transition to the hop test which is with a single leg. Since one cannot perform a bilateral comparison with the jump test, we calculate the performance based on allometric scaling to the patient’s height (see Table 2).
Table 2.
Allometric scaling and descriptive normative data for functional jump and functional hop tests
| Test | Men | Women |
|---|---|---|
| Jump test (bilaterally) | 90–100%/height | 80–90%/height |
| Hop tests (uninvolved) | 80–90%/height | 70–80%/height |
| Hop tests (involved) | 80–90%/height | 70–80%/height |
Functional Hop Tests
The functional hop test is the recommended IKDC functional test. Ultimately, we believe it is one of the most important psychological readiness tests for the patient. We calculate the performance of this test by performing a bilateral comparison (within 10%) as well as allometric scaling to the patient’s height (see Table 2).
Lower Extremity Functional Tests
The final structured test in the FTA is the Lower Extremity Functional test (LEFT). The LEFT test was developed to create an in-clinic test that could incorporate the following factors: (1) progressively stress the patient, (2) incorporate acceleration and deceleration maneuvers, (3) perform multiple stresses to the lower extremity, (4) simulate varied movement patterns often encountered in reactive sporting activities, and (5) induce a fatigue factor during the test [24]. The LEFT test effectively identifies deficits during screening to identify potential injuries in athletes [46–49]. Consequently, it may have also have value in identifying residual deficits following ACL reconstruction which will guide the implementation of a successful rehabilitation program. The test area, 30 ft long and 10 ft wide completed in a diamond shape, does not take too large of any area to perform and may be finished in a couple of minutes [24].
Sport-Specific/Position-Specific Testing
The final portion of examination, prior to a full RTS, is a simulated, sport-specific testing in the clinical setting through guidance of a sports medicine professional. Given that the majority of sport activity is a reactive response to an opponent, it is difficult to replicate in a clinical setting. Therefore, the actual sport-specific testing oftentimes needs to be performed as the patient is transitioning back to sport.
Conclusions
Although there are many recent publications indicating criteria for return to sports following ACL reconstruction, there is no predictive validity of any of the studies at the present time [50]. Therefore, based on the present literature and clinical experiences of the authors, we recommend the following:
A battery of varying tests examining different psychometric properties
A battery of tests based on the measurement of impairment in addition to the examination of strength and power
Specific quantitative and qualitative criteria for assessment of performance and function
Examination via proactive and reactive activity to simulate a real-case sport activity scenario
A fatigue factor in the terminal phases of clinic testing
Psychological testing to evaluate for potential kinesiophobia
Patient-reported outcomes
Electronic Supplementary Material
(DOCX 19 kb)
Compliance with Ethical Standards
Conflict of Interest
George J. Davies and Matthew Provencher declare that they have no conflict of interest.
Eric McCarty reports consultancy fees from Zimmer and Biomet, Royalties from Elsevier, and institutional and educational support from Arthrex, Smith Nephew, and Depuy Mitey, outside of the submitted work.
Robert Manske reports royalties from Elsevier Science and Human Kinetics, and an honorarium from Rehab Champions, outside of the submitted work.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on ACL Rehab
Electronic supplementary material
The online version of this article (doi:10.1007/s12178-017-9420-9) contains supplementary material, which is available to authorized users.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Sugimoto D, LeBlanc JC, Wooley SE, et al. The effectiveness of a functional knee brace on joint-position sense in anterior cruciate ligament-reconstructed individuals. J Sport Rehabil. 2016;25(2):190–194. doi: 10.1123/jsr.2014-0226. [DOI] [PubMed] [Google Scholar]
- 2.Heard BJ, Solbak NM, Achari Y, et al. Changes of early post-traumatic osteoarthritis in an ovine model of simulated ACL reconstruction are associated with transient acute post-injury synovial inflammation and tissue catabolism. Osteoarthr Cartil. 2013;21(12):1942–1949. doi: 10.1016/j.joca.2013.08.019. [DOI] [PubMed] [Google Scholar]
- 3.Risberg MA, Oiestad BE, Gunderson R, et al. Changes in knee osteoarthritis, symptoms, and function after anterior cruciate ligament reconstruction: a 20-year prospective follow-up study. Am J Sports Med. 2016;44(5):1215–1224. doi: 10.1177/0363546515626539. [DOI] [PubMed] [Google Scholar]
- 4.Kamath GV, Murphy T, Creighton RA, et al. Anterior cruciate ligament injury, return to play, and reinjury in the elite collegiate athlete: analysis of an NCAA Division I cohort. Am J Sports Med. 2014;42(7):1638–1643. doi: 10.1177/0363546514524164. [DOI] [PubMed] [Google Scholar]
- 5.Ardern CL, Taylor NF, Feller JA, et al. Return-to-sport outcomes at 2 to 7 years after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2012;40(1):41–48. doi: 10.1177/0363546511422999. [DOI] [PubMed] [Google Scholar]
- 6.Barber-Westin SD, Noyes FR. Factors used to determine return to unrestricted sports activities after anterior cruciate ligament reconstruction. Arthroscopy. 2011;27(12):1697–1705. doi: 10.1016/j.arthro.2011.09.009. [DOI] [PubMed] [Google Scholar]
- 7.Reiman MP, Manske RC. The assessment of function: how is it measured? A clinical perspective. J Man Manip Ther. 2011;19(2):91–99. doi: 10.1179/106698111X12973307659546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reiman MP, Manske RC. The assessment of function. Part II: clinical perspective of a javelin thrower with low back and groin pain. J Man Manip Ther. 2012;20(2):83–90. doi: 10.1179/2042618611Y.0000000018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Manske RC, Reiman M. Functional performance testing for power and return to sports. Sports Health. 2013;5:244–250. doi: 10.1177/1941738113479925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Morris RC, Hulstyn MJ, Fleming BC, et al. Return to play following anterior cruciate ligament reconstruction. Clin Sports Med. 2016;35(4):655–668. doi: 10.1016/j.csm.2016.05.009. [DOI] [PubMed] [Google Scholar]
- 11.van Melick N, van Cingel RE, Brooijmans F, et al. Evidence-based clinical practice update: practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. Br J Sports Med. 2016;24:1506–1515. [DOI] [PubMed]
- 12.Gokeler A, Welling W, Zaffagnini S, et al. Development of a test battery to enhance safe return to sports after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2017;25(1):192–199. [DOI] [PMC free article] [PubMed]
- 13.Kyritsis P, Bahr R, Landreau P, et al. Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br J Sports Med. 2016;50(15):946–951. doi: 10.1136/bjsports-2015-095908. [DOI] [PubMed] [Google Scholar]
- 14.Grindem H, Snyder-Mackler L, Moksnes H, et al. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med. 2016;50(13):804–808. doi: 10.1136/bjsports-2016-096031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Joreitz R, Lynch A, Rabuck S, et al. Patient-specific and surgery specific factors that affect return to sport after ACL reconstruction. Int J Sports Phys Ther. 2016;11(2):264–278. [PMC free article] [PubMed] [Google Scholar]
- 16.Waldén M, Hägglund M, Magnusson H, et al. ACL injuries in men's professional football: a 15-year prospective study on time trends and return-to-play rates reveals only 65% of players still play at the top level 3 years after ACL rupture. Br J Sports Med. 2016;50(12):744–750. doi: 10.1136/bjsports-2015-095952. [DOI] [PubMed] [Google Scholar]
- 17.Dingenen B, Gokeler A. Optimization of the return-to-sport paradigm after anterior cruciate ligament reconstruction: a critical step back to move forward. Sports Med. 2017;11. [DOI] [PubMed]
- 18.McGrath TM, Waddington G, Scarvell JM, et al. An ecological study of anterior cruciate ligament reconstruction, part 1: clinical tests do not correlate with return-to-sport outcomes. Orthop J Sports Med. 2016;4(11):2325967116672208. doi: 10.1177/2325967116672208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lefevre N, Klouche S, Mirouse G, et al. Return to sport after primary and revision anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45(1):34–41. doi: 10.1177/0363546516660075. [DOI] [PubMed] [Google Scholar]
- 20.Grassi A, Vascellari A, Combi A, et al. SIGASCOT Sports Committee. Return to sport after ACL reconstruction: a survey between the Italian Society of Knee, Arthroscopy, Sport, Cartilage and Orthopaedic Technologies (SIGASCOT) members. Eur J Orthop Surg Traumatol. 2016;26(5):509–516. doi: 10.1007/s00590-016-1756-0. [DOI] [PubMed] [Google Scholar]
- 21.Undheim MB, Cosgrave C, King E, et al. Isokinetic muscle strength and readiness to return to sport following anterior cruciate ligament reconstruction: is there an association? A systematic review and a protocol recommendation. Br J Sports Med. 2015;49(20):1305–1310. doi: 10.1136/bjsports-2014-093962. [DOI] [PubMed] [Google Scholar]
- 22.Ellman MB, Sherman SL, Forsythe B, et al. Return to play following anterior cruciate ligament reconstruction. J Am Acad Orthop Surg. 2015;23(5):283–296. doi: 10.5435/JAAOS-D-13-00183. [DOI] [PubMed] [Google Scholar]
- 23.Herbst E, Hoser C, Hildebrandt C, et al. Functional assessments for decision-making regarding return to sports following ACL reconstruction. Part II: clinical application of a new test battery. Knee Surg Sports Traumatol Arthrosc. 2015;23(5):1283–1291. doi: 10.1007/s00167-015-3546-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Logerstedt D, Di Stasi S, Grindem H, et al. Self-reported knee function can identify athletes who fail return-to-activity criteria up to 1 year after anterior cruciate ligament reconstruction: a Delaware-Oslo ACL cohort study. J Orthop Sports Phys Ther. 2014;44(12):914–923. doi: 10.2519/jospt.2014.4852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Harris JD, Abrams GD, Bach BR, et al. Return to sport after ACL reconstruction. Orthopedics. 2014;37(2):e103–e108. doi: 10.3928/01477447-20140124-10. [DOI] [PubMed] [Google Scholar]
- 26.Davies GJ, Zillmer DA. Functional progression of a patient through a rehabilitation program. Orthop Phys Therapy Clin North Am. 2000;9:103–118. [Google Scholar]
- 27.Davies, GJ. Individualizing the return to play decision after ACL reconstruction. Oper Tech Orthop. 2017. doi:10.1053/j.oto.2017.01.013. In press.
- 28.Kennedy JC, Weinberg HW, Wilson AS. The anatomy and function of the anterior cruciate ligament. As determined by clinical and morphological studies. J Bone Joint Surg Am. 1974;56(2):223–235. doi: 10.2106/00004623-197456020-00001. [DOI] [PubMed] [Google Scholar]
- 29.Nagelli CV, Hewett TE. Should return to sport be delayed until 2 years after anterior cruciate ligament reconstruction? Biological and functional considerations. Sports Med. 2017;47:221–232. doi: 10.1007/s40279-016-0584-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nagelli CV, Cook JL, Kuroki K, et al. Does anterior cruciate ligament innervation matter for joint function and development of osteoarthritis? J Knee Surg. 2017;30(4):364–371. [DOI] [PubMed]
- 31.Kim HJ, Lee JH, Lee DH. Proprioception in patients with anterior cruciate ligament tears. Am J Sports Med. 2016 Dec 1:363546516682231. doi:10.1177/0363546516682231.
- 32.Suarez T, Laudani L, Giombini A, et al. Comparison in joint-position sense and muscle coactivation between anterior cruciate ligament-deficient and healthy individuals. J Sport Rehabil. 2016;25(1):64–69. doi: 10.1123/jsr.2014-0267. [DOI] [PubMed] [Google Scholar]
- 33.Davies GJ, Heiderscheidt B. Linea reliability of the Lido Linea closed kinetic chain isokinetic dynamometer. J Orthop Sports Phys Ther. 1997;25(2):133–136. doi: 10.2519/jospt.1997.25.2.133. [DOI] [PubMed] [Google Scholar]
- 34.Nicholas JA, Marino M. The relationship of injuries of the leg, foot, and ankle to proximal thigh strength in athletes. Foot Ankle. 1987;7(4):218–228. doi: 10.1177/107110078700700404. [DOI] [PubMed] [Google Scholar]
- 35.Gleim GW, Nicholas JA, Webb JN. Isokinetic evaluation following leg injuries. Phys Sportsmed. 1978;6(8):75–82. doi: 10.1080/00913847.1978.11710743. [DOI] [PubMed] [Google Scholar]
- 36.Greenberger HB, Paterno MV. Relationship of knee extensor strength and hopping test performance in the assessment of lower extremity function. J Orthop Sports Phys Ther. 1995;22(5):202–206. doi: 10.2519/jospt.1995.22.5.202. [DOI] [PubMed] [Google Scholar]
- 37.Pincivero DM, Lephart SM, Karunakara RG. Relation between open and closed kinematic chain assessment of knee strength and functional performance. Clin J Sport Med. 1997;7(1):11–16. doi: 10.1097/00042752-199701000-00003. [DOI] [PubMed] [Google Scholar]
- 38.Perry MC, Morrissey MC, King JB, et al. Effects of closed versus open kinetic chain knee extensor resistance training on knee laxity and leg function in patients during the 8- to 14-week post-operative period after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2005;13(5):357–369. doi: 10.1007/s00167-004-0568-7. [DOI] [PubMed] [Google Scholar]
- 39.Davies GJ. A compendium of isokinetics in clinical usage and rehabilitation techniques. Fourth. Onalaska: S. & S Publishers; 1992. [Google Scholar]
- 40.Davies GJ, Gould JA, et al. Torque acceleration energy and average power changes in quadriceps and hamstrings through the selected velocity spectrum as determined by computerized Cybex testing. Presented at the ACSM National Conference, 1983. Med Sci Sports Exerc. 1983;15(2):144. doi: 10.1249/00005768-198315020-00262. [DOI] [Google Scholar]
- 41.Gould JA, Davies GJ, et al. Computerized Cybex testing of ACL reconstruction assessing hamstrings peak torque, TAE, total work, and average power. Presented at the ACSM National Conference, 1984. Med Sci Sports Exerc. 1984;16(2):204. doi: 10.1249/00005768-198404000-00443. [DOI] [Google Scholar]
- 42.Mirkov DM, Knezevic OM, Maffiuletti NA, et al. Contralateral limb deficit after ACL-reconstruction: an analysis of early and late phase of rate of force development. J Sports Sci. 2017;35(5):435–440. doi: 10.1080/02640414.2016.1168933. [DOI] [PubMed] [Google Scholar]
- 43.Larsen JB, Farup J, Lind M, et al. Muscle strength and functional performance is markedly impaired at the recommended time point for sport return after anterior cruciate ligament reconstruction in recreational athletes. Hum Mov Sci. 2015;39:73–87. doi: 10.1016/j.humov.2014.10.008. [DOI] [PubMed] [Google Scholar]
- 44.Myer GD, Martin L, Jr, Ford KR, et al. No association of time from surgery with functional deficits in athletes after anterior cruciate ligament reconstruction: evidence for objective return-to-sport criteria. Am J Sports Med. 2012;40(10):2256–2263. doi: 10.1177/0363546512454656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vairo GL, Myers JB, Sell TC, et al. Neuromuscular and biomechanical landing performance subsequent to ipsilateral semitendinosus and gracilis autograft anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2008;16(1):2–14. doi: 10.1007/s00167-007-0427-4. [DOI] [PubMed] [Google Scholar]
- 46.Brumitt J, Engilis A, Isaak D, et al. Preseason jump and hop measures in male collegiate basketball players: an epidemiological report. Int J Sports Phys Ther. 2016;11(6):954–961. [PMC free article] [PubMed] [Google Scholar]
- 47.Brumitt J, Heiderscheit BC, Manske RC, et al. Lower extremity functional tests and risk of injury in Division III collegiate athletes. Int J Sports Phys Ther. 2013;8(3):216–227. [PMC free article] [PubMed] [Google Scholar]
- 48.Brumitt J, Heiderscheit BC, Manske RC, et al. Off-season training habits and preseason functional test measures of Division III collegiate athletes: a descriptive report. Int J Sports Phys Ther. 2014;9(4):447–455. [PMC free article] [PubMed] [Google Scholar]
- 49.Brumitt J, Heiderscheit BC, Manske RC, et al. The lower-extremity functional test and lower-quadrant injury in NCAA Division III athletes: a descriptive and epidemiologic report. J Sport Rehabil. 2016;25(3):219–226. doi: 10.1123/jsr.2014-0316. [DOI] [PubMed] [Google Scholar]
- 50.Narducci E, Waltz A, Gorski K, et al. The clinical utility of functional performance tests within one-year post-ACL reconstruction: a systematic review. Int J Sports Phys Ther. 2011;6(4):333–342. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 19 kb)


