Abstract
IMPORTANCE
Both the overuse of unnecessary medical procedures and poor continuity of care are thought to contribute to high health care spending and poor patient outcomes.
OBJECTIVE
To investigate the association between care continuity and use of potentially unnecessary procedures.
DESIGN, SETTING, AND PARTICIPANTS
Observational retrospective cohort (n = 1 208 250 patients > 65 years) using 5% Medicare fee-for-service claims from 2008.
MAIN OUTCOMES AND MEASURES
We evaluated continuity using the Bice-Boxerman continuity of care index. We measured overuse using a previously validated set of 19 potentially overused procedures.
RESULTS
Altogether, 14.7% of patients received at least 1 potentially overused procedure during the calendar year. For each 0.1 increase in the continuity score (0.4 SDs), patients had 0.93 times the odds of receiving overused procedures than those with lower scores (95% CI, 0.93–0.94). Higher continuity was significantly associated with lower odds of 9 procedures (Holm-Bonferroni corrected P < .02 was significant: 6 of 13 diagnostic tests [with ORs, 0.84–0.99; P < .001] and 3 therapeutic procedures [with ORs 0.81–0.87; P <.001]). Conversely, higher continuity was significantly associated with increased overuse for 3 procedures (1 diagnostic test [OR, 1.06; P < .001], 1 of 2 screening tests [OR, 1.05; P < .001], and the single monitoring test [OR, 1.03; P < .01]).
CONCLUSIONS AND RELEVANCE
Increased continuity was associated with an overall decrease in overuse, suggesting a potential benefit of high-continuity care; however, the strength and direction of the association varied according to the specific procedure.
Currently, too many patients in the United States receive health care that is characterized by poor continuity and high fragmentation.1,2 The average Medicare patient sees 2 primary care physicians and 5 specialists in 4 different practices each year.3 Previous studies4,5 have demonstrated that higher continuity and reduced fragmentation is associated with lower-cost and higher-quality health care; however, to our knowledge, no study has specifically described continuity’s association with patterns of procedural overuse. Multiple health care reforms, such as the establishment of Patient Centered Medical Homes (PCMHs), implementation of accountable care organizations, and use of bundled payments, strive to reduce costs and increase quality by improving care coordination and reducing fragmentation across health care providers (herein, health care providers are defined as medical clinicians including physicians, nurse practitioners, and physicians assistants).6,7
At the same time, an important driver of high cost and low quality in the US health care system is the overuse of health care services and products.8–10 Overuse is defined as the use of a service in the absence of a clear medical basis for its use, when the risk of harm exceeds its likely benefit.11 Multiple efforts, such as the American Board of Internal Medicine’s Choosing Wisely initiative, seek to reign in overuse and reduce health care spending.12
Continuity is known to significantly influence various aspects of the patient-provider relationship, including patient-provider trust,13,14 patient satisfaction,15,16 and communication,17 that may be linked with overuse. First, providers who have greater continuity with their patients may be more confident that their patients will return for follow-up visits, leading to more conservative diagnostic and treatment activities. Second, continuity may give health care providers a deeper understanding of their patients’ symptoms and medical histories, leading to more accurate assessments with less overuse. Last, continuity may give health care providers a comprehensive overview of the care their patients receive across multiple specialists, which could lead to more coordinated and efficient care with less redundant testing.
Despite these plausible mechanisms, to our knowledge, no study has previously examined the association between interpersonal medical care continuity and systematic overuse. Saultz18(p138) described interpersonal continuity as a multifaceted concept that encompasses an “ongoing relationship” wherein “the patient uses this physician for basic health services and depends on the physician to assume personal responsibility for the patient’s overall health care.” Interpersonal continuity is distinct from informational continuity, geographic continuity, and chronologic continuity, which describe the ongoing availability of information, the geographic consistency of care, and the duration of a care episode, respectively. Interpersonal continuity has been operationalized using claims-based metrics of visit dispersion among a patient’s health care providers, which attempt to model the ability of a health care system to support ongoing relationships between individual health care providers and patients. The overall objective of our study was to investigate the association between interpersonal continuity and the overuse of medical procedures using Medicare claims data.
Methods
Study Population
We used a random 5% sample of fee-for-service patients insured by Medicare in 2008. Medicare is a federal insurance program for senior citizens and people with disabilities, and insurance claims data are available in the MedPar, Carrier, and Outpatient data files, which contain Part A hospital claims, Part B professional health care provider claims, and institutional outpatient health care provider claims, respectively. We required that patients had 12 months of complete enrollment in Medicare Parts A and B during 2008, were older than 65 years, and were not enrolled in a Medicare health maintenance organization (N = 1 451 542 patients). We excluded patients who died during the study year; we were unable to calculate comparable continuity indices for patients with different durations of observation (73 567 patients). Patients who had fewer than 2 outpatient medical visit in 2008 were excluded (169 425 patients). All remaining patients were eligible for an overused procedure (1 208 150 patients; see eFigure 1 in the Supplement for flowchart). The study protocol was approved by the institutional review board from the Johns Hopkins Bloomberg School of Public Health.
Continuity Measurement
We used the Bice-Boxerman continuity of care (COC) index to calculate continuity. The COC index represents the concentration of visits among a patient’s health care providers (see eFigure 2 in the Supplement for formula).19,20 If a patient sees exclusively 1 health care provider with multiple encounters during the study period, the patient’s COC index would be 1.0, and if a patient sees many different health care providers with 1 encounter each, the patient’s COC index would be closer to 0. To calculate the COC index, we included only evaluation and management visits that occurred in the outpatient setting defined by Berenson-Eggers Type of Service and Healthcare Common Procedure Coding System codes regardless of provider specialty. Only a single evaluation and management visit per day for each patient-provider pair was counted. We defined “providers” according to the National Provider Indices for attending physicians in the Outpatient file and performing physician in the Carrier file. The COC index was chosen from among many continuity metrics for our primary analysis based on its ability to characterize the overall dispersion of care for patients with multiple health care providers and medical problems, which was appropriate for the patients in this data set with multiple medical visits with different health care providers and complex conditions. We conducted sensitivity analyses using the Usual Provider of Care (UPC) index21 and the SEquential CONtinuity (SECON) index,22 2 additional metrics of continuity that show the concentration of care among one’s main health care provider and the number of health care provider transitions across visits, respectively (see eFigure 2 in the Supplement for formulas). The UPC index is the most-cited continuity metric in the medical literature and is widely measured for PCMH accreditation; however, by focusing exclusively on the concentration of a patient’s care with the “usual” health care provider, it may not capture important care patterns with a patient’s other health care providers.23
Overuse Measurement
The goal of overuse measurement is not to define procedures that should never be done but rather to identify procedures that are often overused and serve as indicators of broader overuse in health care systems with specific practice patterns and resources.24 We operationalized overuse using items from a previously studied set of 19 potentially overused procedures, including 13 diagnostic, 3 therapeutic, 2 screening, and 1 monitoring procedures.25 These measures were derived from publications of national professional societies and consumer groups with interests in quality improvement or cost-containment and were selected if they were obtainable from claims data and relevant for patients older than 65 years.26 These measures have been previously linked with considerable variability between and within hospital referral regions. Each overuse indicator is defined by a denominator of eligible patients and a numerator of patients receiving the potentially overused procedures (see eTable 1 in the Supplement). We excluded 1 indicator from the validated set because it was based on patient death during the survey year.
Covariates
Covariates included age, sex, self-reported race (white, black, or unknown/other), comorbidity, and zip code median income. Comorbidity was calculated using Aggregated Diagnostic Group (ADG) count, a case-mix adjustment derived from the Adjusted Clinical Groups software that takes into consideration all diagnoses found in the claims file.27 Patients are assigned to ADGs based on clinically similar diagnosis codes with similar morbidity and resource consumption over a given year. We used the count of total ADGs as a summative measure of comorbidity for patients in this sample, many of whom have multiple acute and chronic health care needs demonstrated by ADG inclusion. Zip code median house hold income was calculated based on the 2006–2010 American Community Survey and was included as a continuous variable.28
Statistical Analysis
We compared characteristics of the patients who received potentially overused procedures with those who did not receive those procedures using t test for continuous variables and χ2 analysis for categorical variables. We then performed multiple logistic regression analyses, adjusting for age, sex, race, comorbidity, and income to examine the association between COC index and the receipt of any potentially overused procedure. In the primary analysis, COC index was included as a continuous variable where odds ratios (ORs) represent the odds of receiving a procedure for a 0.1-U difference in continuity. We ran separate multiple logistic regression analyses for each overused procedure and used the Holm-Bonferroni correction for multiple comparisons (based on 19 overuse measures) for an overall α = .05.
We performed multiple sensitivity analyses. First, although claims-based measures of continuity have been shown to be highly correlated with one another, we examined the associations between alternative continuity measures—the UPC and SECON indices—and overuse.19 Second, we classified the COC index as a categorical variable, dividing patients into tertiles to examine potential nonlinear associations between continuity and overuse. Third, we investigated the potential temporal relationship between continuity and overuse by constructing the COC index only during the first 6 months of 2008 and examining overuse during the last 6 months of the year. Fourth, we tested the contribution of primary care providers by including whether the patient had a visit with a primary care provider (defined as an outpatient claim with a general practitioner, family physician, geriatrician, or internal medicine physician without subspecialty training) as a covariate in the logistic regressions. Data were analyzed using SAS statistical software (version 9.3; SAS Institute Inc).
Results
A total of 1 208 150 Medicare patients were eligible for at least 1 potentially overused procedure in 2008 and met other inclusion criteria (see eFigure 1 in the Supplement). Patient characteristics of both recipients and nonrecipients of potentially overused procedures are shown in Table 1. On average, patients were 77 years old, 88.6% were white, and over half (63.7%) were female. Recipients of any potentially overused procedures were sicker than those who did not experience overuse (12.5 vs 9.7 ADG count; P < .01). Continuity was lower on average among patients with any overused procedure than among patients who did not have an overused procedure (COC index: 0.24 vs 0.33; P < .01).
Table 1.
Patient Characteristicsa
| Characteristic | Patients | ||
|---|---|---|---|
| All | With Overused Procedures | Without Overused Procedures | |
| Sex, No. (%) | |||
| Female | 769 714 (63.7) | 113 024 (63.7) | 656 690 (63.7) |
| Male | 438 436 (36.3) | 64 516 (36.3) | 373 920 (36.3) |
| Race/ethnicity, No. (%) | |||
| White | 1 070 230 (88.6) | 158 326 (89.2) | 911 904 (88.5) |
| Black | 83 576 (6.92) | 10 839 (6.11) | 72 737 (7.06) |
| Other/unknown | 54 344 (4.50) | 8375 (4.72) | 45 969 (4.46) |
| Age, mean (SD), y | 76.9 (7.62) | 76.5 (7.18) | 77.0 (7.70) |
| ADGs, mean (SD), No. | 10.1 (4.90) | 12.5 (3.95) | 9.68 (4.17) |
| Zip code median income, mean (SD), $ | 56 401 (22 551) | 57 246 (23 401) | 56 256 (22 398) |
| Continuity, mean (SD) | |||
| COC | 0.31 (0.26) | 0.24 (0.19) | 0.33 (0.27) |
| UPC | 0.51 (0.22) | 0.43 (0.19) | 0.53 (0.22) |
| SECON | 0.32 (0.29) | 0.26 (0.22) | 0.33 (0.30) |
Abbreviations: ADG, adjusted diagnostic group; COC, Bice-Boxerman continuity of care index; SECON, SEquential CONtinuity index; UPC, usual provider of care index.
P< .001 for all comparisons except sex (P= .64).
Table 2 details the differences in continuity between individuals with and without each indicator of overuse. For 15 of the 19 procedures, continuity was lower on average for patients who experienced potential overuse compared with those who did not. In unadjusted analysis, the 3 procedures for which continuity was higher among patients who experienced overuse included 1 monitoring test (routine monitoring of digoxin) and 2 diagnostic procedures (magnetic resonance imaging [MRI] of the lumbar spine for low back pain prior to conservative therapy and thorax computed tomographic[CT] scans with and without contrast).
Table 2.
Multivariate Logistic Regression Results
| Procedure | Total Patients Eligible, No. | Cumulative Incidence (Events per 1000 Eligible Patients) | COC Continuity, Mean (SD) | P Value for Adjusted Difference in COC Continuity | |
|---|---|---|---|---|---|
| With Procedure | Without Procedurea | ||||
| Diagnostic tests | |||||
| Laryngoscopy for sinusitis | 117897 | 11 | 0.20 (0.14) | 0.29 (0.23) | <.001b |
| Nasal endoscopy for sinusitis | 117897 | 44 | 0.20 (0.14) | 0.29 (0.23) | <.001b |
| Electroencephalogram in syncope | 74097 | 56 | 0.21 (0.16) | 0.27 (0.21) | <.001b |
| Stress echocardiography for acute chest pain | 30 288 | 43 | 0.21 (0.15) | 0.23 (0.18) | .002b |
| MRI in mild traumatic brain injury | 36104 | 25 | 0.24 (0.19) | 0.27 (0.21) | .003b |
| Sinus CT or antibiotics for rhinosinusitis | 84126 | 15 | 0.24 (0.18) | 0.29 (0.23) | .03 |
| Unproven allergy tests | 171268 | 13 | 0.25 (0.19) | 0.29 (0.23) | .02 |
| Tumor marker studies in asymptomatic breast cancer | 42 288 | 338 | 0.21 (0.16) | 0.22 (0.18) | .02 |
| Abdomen CT with and without contrast | 139338 | 255 | 0.24 (0.18) | 0.24 (0.19)a | .006b |
| MRI lumbar spine for low back pain | 33209 | 398 | 0.24 (0.19) | 0.22 (0.16) | .52 |
| Advanced imaging in low-risk prostate cancer | 55 208 | 179 | 0.21 (0.15) | 0.24 (0.19) | .83 |
| Preoperative chest radiograph | 147011 | 250 | 0.22 (0.16) | 0.23 (0.17) | .18 |
| Thorax CT with and without contrast | 97698 | 77 | 0.26 (0.20) | 0.24 (0.18) | <.001b |
| Therapeutic procedures | |||||
| Laminectomy and/or spinal fusion | 1118224 | 2 | 0.19 (0.13) | 0.32 (0.27) | <.001b |
| Hysterectomy for benign disease | 761178 | 2 | 0.21 (0.16) | 0.32 (0.26) | <.001b |
| Traction for low back pain | 325381 | 96 | 0.21 (0.17) | 0.27 (0.22) | <.001b |
| Screening tests | |||||
| Carotid artery stenosis screening | 974572 | 14 | 0.27 (0.21) | 0.33 (0.27) | .03 |
| Serological tests for Helicobacter pylori | 1208 150 | 10 | 0.29 (0.23) | 0.31 (0.26) | <.001b |
| Monitoring test | |||||
| Routine monitoring of digoxin | 256403 | 41 | 0.36 (0.26) | 0.29 (0.22) | <.001b |
| Any overused procedure | 1208150 | 147 | 0.24 (0.19) | 0.33 (0.27) | <.001b |
Abbreviations: COC, Bice-Boxerman continuity of care index; CT, computed tomography; MRI, magnetic resonance imaging.
All unadjusted differences in mean COC between patients receiving and those not receiving overused procedures are statistically different than 0 based on a Holm-Bonferroni with an overall α = .05 except abdomen CT with and without contrast, for which there is no statistically significant difference.
P < .02 is significant based on Holm-Bonferroni correction for 19 comparisons with overall α = .05.
The multivariate model showed an association between higher continuity of care and decreased overuse OR for a 0.1-U increase in COC index of 0.93 (95% CI, 0.93–0.94). For patients with 13 total annual visits—the median in our sample— moving from 4 to 3 health care providers or increasing the number of visits with their main health care provider from 3 to 5 visits may increase the COC index by 0.1, which corresponds to a 0.4 standard deviation change (see eTable 2 in the Supplement for an example of COC index calculations). The Figure shows associations between higher continuity and significantly lower odds of 9 procedures (6 of 13 diagnostic tests and 3 of 3 therapeutic procedures). Regression models also showed an association between higher continuity and increased overuse for 3 procedures (1 diagnostic, 1 of 2 screening, and 1 of 1 monitoring test). There was no statistically significant association between continuity and the overuse of 7 procedures examined (6 diagnostic tests and 1 screening test: positron emission tomography/computed tomography/bone scan in prostate cancer, P = .83; coronary artery stenosis screening, P = .03; preoperative chest radiograph, P = .17; tumor marker studies in asymptomatic breast cancer, P =.02; unproven allergy tests, P = .02; and magnetic resonance imaging of the lumbar spine for low back pain, P = .52) (Figure).
Figure. Odds Ratios for Overuse Associated With a0.1-U Change in Continuity of Care (COC) Index.
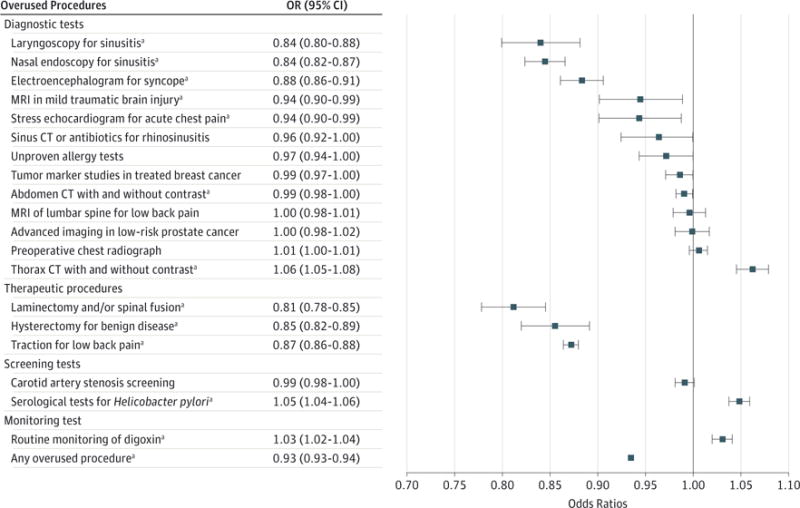
Forest plot of adjusted association between 0.1-U change in COC index and the extent of overused procedures with Holm-Bonferroni-corrected 95% CIs for an overall α = .05. Points to the left of 1.00 represent decreased overuse with increased continuity, whereas points to the right of 1.00 represent increased overuse with increased continuity. CT indicates computed tomography; MRI, magnetic resonance imaging; OR, odds ratio.
aStatistically significant.
In sensitivity analyses, we found qualitatively similar results when using SECON and UPC indices as measures of continuity (eTable 3 in the Supplement).Modeling the COC index as a categorical variable also yielded similar results, with the only exceptions being a loss of statistical significance for the associations between continuity and 3 overused diagnostic tests (stress echocardiograms for acute coronary syndrome, MRI in traumatic brain injury, and abdominal CT scans with and without contrast). When we analyzed the data longitudinally by calculating the COC index using the first6 months of claims and overuse based on the following 6 months of claims, we continued to observe a significant association between increased continuity and decreased overuse, although with a smaller effect size (OR, 0.993; 95% CI, 0.990–0.995; P < .001) (see eTable 3 in the Supplement). Of the 9 procedures that had been significantly associated with lower continuity in the main analyses, 4 remained statistically significant in these analyses (2 diagnostic and 2 therapeutic [Holm-Bonferroni corrected P < .008 was significant]: laminectomy and/or spinal fusion, P < .001; laryngoscopy for sinusitis, P = .004; nasal endoscopy for sinusitis, P < .001; and traction for low-back pain, P < .001). All 3 procedures that were significantly associated with higher continuity in the main analysis remained significant (Holm-Bonferroni correction with overall α = .05, P < .008 was significant: routine monitoring of digoxin, P < .001; serological tests for Helicobacter pylori, P < .001; thorax CT with and without contrast, P < .001), and another 3 became significantly associated (2 diagnostic procedure and 1 screening procedure) (Holm-Bonferroni corrected, P < .008 was significant: PET/CT/bone scan in prostate cancer, P < .001; preoperative chest radiograph, P < .001; coronary artery stenosis screening, P = .004). Including whether the patient had a visit with a primary care provider as a covariate in the multivariate model did not alter the association between continuity and overuse of any of the tested procedures.
Discussion
We found that increased interpersonal care continuity was associated with lower overall overuse among fee-for-service Medicare patients older than 65 years in a cross-sectional analysis. The baseline incidence of any overused procedure in the study population was 147 events per 1000 patients per year, and an increase in 0.1 U of continuity was associated with 9 fewer events per 1000 patients per year. Higher continuity was associated with a lower likelihood of overuse for 9 procedures, with a more consistent relationship found for diagnostic tests and therapeutic procedures. Conversely, higher continuity was associated with higher overuse of 3 procedures. The study is important because both continuity and overuse are key components of efforts to improve health care delivery, and the potential links between the 2 concepts had not, to our knowledge, been previously described. Even relatively small differences in the odds of overuse associated with continuity may have large impacts on population health and spending owing to the observed high prevalence of overuse in the Medicare population.
The variation among our findings raises several key concerns about the relationship between continuity and overuse. Overused procedures represent a broad array of therapeutic, diagnostic, screening, and monitoring tests. We found the most consistent associations between higher continuity and lower use of procedures in the therapeutic category. These procedures were also the most invasive ones among the 19 studied (eg, hysterectomy, laminectomy, spinal fusion). Although we are unable to determine any causal mechanisms from the data, it is possible that in settings with high continuity, patients and health care providers are more willing to conservatively treat symptoms and defer potentially unnecessary procedures until clinically indicated. Alternatively, use of these invasive unnecessary procedures might lead patients to require care from more health care providers, which may lower continuity scores. It is plausible that procedures that were overused more among high-continuity patients may be attributable to less specialist consultation and resulting health care provider uncertainty about the appropriate choice of screening and monitoring procedures.
Continuity is a multifaceted concept that includes informational, longitudinal, and interpersonal components.18 Claims-based measures examine patterns of care but are unable to capture multiple aspects of continuity that may be particularly important for some of the overused procedures. Despite our sensitivity analyses using the UPC and SECON indices, other metrics of continuity, such as information sharing or duration of patient-provider relationships, might show different associations. Furthermore, various aspects of continuity may be differently associated with the various types of potentially overused procedures.
We observed several differences when we examined the data cross-sectionally vs longitudinally. The longitudinal data used a smaller sample (owing to the inability to calculate the COC index on a large portion of patients with no visits or 1 visit ina 6-month period),which may have mitigated our ability to see significant associations. The smaller time periods for measuring the exposure and outcome may have led to less stable estimates of each. In particular, the COC is highly dependent on the total number of visits, and decreasing the observational period for calculating continuity from 12 to 6 months may significantly affect the assessment of continuity. As noted herein, reverse causation may be another potential explanation for the results in which increased overuse leads to changes in continuity.
Study Strengths
This study contains multiple methodological strengths. Our sample population is large and representative of Medicare patients older than 65 years nationwide. Our research topic is novel, investigating an association between 2 important but previously unlinked factors in American health care. We used sensitivity analyses to correlate our findings using other metrics of continuity and to examine a temporal relationship between measures.
Study Limitations
This study has several key limitations. First, overuse measures do not define procedures that should never be done but rather identify procedures that are often overused and serve as indicators of broader overuse in health care systems with specific practice patterns and resources.24 Second, administrative-based measures of care continuity are commonly used but may not reflect multiple aspects of care coordination.19,24 The measured mean COC index in this study is slightly lower than other continuity indices published for Medicare patients by ourselves and others (0.31 in this study vs 0.35–0.3629 and 0.50–0.605 published elsewhere); however, other sources define study periods, episodes of care, and minimum numbers of patient visits differently, limiting the appropriateness of interstudy comparisons. Third, claims-based measures lack clinical detail for complex clinical risk adjustment. The large difference in ADG counts between recipients and nonrecipients of overused procedures suggests the possibility of unmeasured confounding. Other patient and health care provider factors may potentially confound the relationship between continuity and overuse. For example, skeptical patients might pursue second and third medical opinions and insist on excessive diagnostic tests, which could decrease continuity and increase overuse. Fourth, our data are cross-sectional in nature, and we were unable to determine causation. Our sensitivity analysis measuring continuity and overuse using claims from different time periods begins to address the temporal relationship between these variables. Measuring continuity of care and overuse over a longer time course in future analyses may demonstrate different associations. Future studies may also seek to link specific overused procedures to the ordering health care providers to further clarify the relationship between continuity and overuse. Fifth, though we used ADGs for risk adjustment, claims data lack important clinical detail that may confound the relationship between continuity and overuse. Finally, the data reflect older adults in fee-for-service Medicare and may not be generalizable to younger populations or those in managed care.
Conclusions
This study provides evidence of a relationship between interpersonal continuity of care and overuse of potentially unnecessary procedures. Our research suggests that higher levels of continuity are associated with lower use of certain commonly overused therapeutic procedures and increased use of other indicators of overuse. It will be critical to monitor the link between continuity and overuse over time as health care reforms seek to modify the 2. It is possible that efforts to improve continuity—for example, through PCMHs and accountable care organizations—may reduce some forms of waste in our health care system while increasing others.
Supplementary Material
Acknowledgments
Funding/Support: Mr Romano is supported by the Johns Hopkins Institute for Clinical and Translational Research (ICTR), which is funded in part by grant No. TL1 TR001078 from the National Center for Advancing Translational Sciences (NCATS) a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. Dr Pollack is supported by a career development award from the National Cancer Institute (K07CA151910).
Role of the Funder/Sponsor: The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Author Contributions: Mr Romano had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Romano, Pollack.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Romano.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Romano.
Obtained funding: Romano.
Administrative, technical, or material support: All authors.
Study supervision: Segal, Pollack.
Conflict of Interest Disclosures: None reported.
Disclaimer: This article’s contents are solely the responsibility of the authors and do not necessarily represent the official view of the Johns Hopkins ICTR, NCATS, or NIH.
Additional Contributions: Hsien-Yen Chang, PhD, Johns Hopkins Bloomberg School of Public Health, provided statistical analytic support. He was not compensated for his assistance.
Contributor Information
Max J. Romano, Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland; Johns Hopkins University School of Medicine, Baltimore, Maryland.
Jodi B. Segal, Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland; Johns Hopkins University School of Medicine, Baltimore, Maryland.
Craig Evan Pollack, Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland; Johns Hopkins University School of Medicine, Baltimore, Maryland.
References
- 1.Bodenheimer T. Coordinating care: a perilous journey through the health care system. N Engl J Med. 2008;358(10):1064–1071. doi: 10.1056/NEJMhpr0706165. [DOI] [PubMed] [Google Scholar]
- 2.Cebul RD, Rebitzer JB, Taylor LJ, Votruba M. Organizational Fragmentation and Care Quality in the US Health Care System. No. 14212. Cambridge, MA: National Bureau of Economic Research; 2008. [DOI] [PubMed] [Google Scholar]
- 3.Pham HH, Schrag D, O’Malley AS, Wu B, Bach PB. Care patterns in Medicare and their implications for pay for performance. N Engl J Med. 2007;356(11):1130–1139. doi: 10.1056/NEJMsa063979. [DOI] [PubMed] [Google Scholar]
- 4.Saultz JW, Lochner J. Interpersonal continuity of care and care outcomes: a critical review. Ann Fam Med. 2005;3(2):159–166. doi: 10.1370/afm.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hussey PS, Schneider EC, Rudin RS, Fox DS, Lai J, Pollack CE. Continuity and the costs of care for chronic disease. JAMA Intern Med. 2014;174(5):742–748. doi: 10.1001/jamainternmed.2014.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de Brantes F, Rosenthal MB, Painter M. Building a bridge from fragmentation to accountability: the Prometheus Payment model. N Engl J Med. 2009;361(11):1033–1036. doi: 10.1056/NEJMp0906121. [DOI] [PubMed] [Google Scholar]
- 7.Goldsmith J. Accountable care organizations: the case for flexible partnerships between health plans and providers. Health Aff (Millwood) 2011;30(1):32–40. doi: 10.1377/hlthaff.2010.0782. [DOI] [PubMed] [Google Scholar]
- 8.Zuckerman S, Waidmann T, Berenson R, Hadley J. Clarifying sources of geographic differences in Medicare spending. N Engl J Med. 2010;363(1):54–62. doi: 10.1056/NEJMsa0909253. [DOI] [PubMed] [Google Scholar]
- 9.Song Y, Skinner J, Bynum J, Sutherland J, Wennberg JE, Fisher ES. Regional variations in diagnostic practices. N Engl J Med. 2010;363(1):45–53. doi: 10.1056/NEJMsa0910881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Epstein AM. Geographic variation in Medicare spending. N Engl J Med. 2010;363(1):85–86. doi: 10.1056/NEJMe1005212. [DOI] [PubMed] [Google Scholar]
- 11.Chassin MR, Galvin RW, Institute of Medicine National Roundtable on Health Care Quality The urgent need to improve health care quality. JAMA. 1998;280(11):1000–1005. doi: 10.1001/jama.280.11.1000. [DOI] [PubMed] [Google Scholar]
- 12.Cassel CK, Guest JA. Choosing wisely: helping physicians and patients make smart decisions about their care. JAMA. 2012;307(17):1801–1802. doi: 10.1001/jama.2012.476. [DOI] [PubMed] [Google Scholar]
- 13.Mainous AG, III, Baker R, Love MM, Gray DP, Gill JM. Continuity of care and trust in one’s physician: evidence from primary care in the United States and the United Kingdom. Fam Med. 2001;33(1):22–27. [PubMed] [Google Scholar]
- 14.Mainous AG, III, Kern D, Hainer B, Kneuper-Hall R, Stephens J, Geesey ME. The relationship between continuity of care and trust with stage of cancer at diagnosis. Fam Med. 2004;36(1):35–39. [PubMed] [Google Scholar]
- 15.Wasson JH, Sauvigne AE, Mogielnicki RP, et al. Continuity of outpatient medical care in elderly men: a randomized trial. JAMA. 1984;252(17):2413–2417. [PubMed] [Google Scholar]
- 16.Smith CS. The impact of an ambulatory firm system on quality and continuity of care. Med Care. 1995;33(3):221–226. doi: 10.1097/00005650-199503000-00001. [DOI] [PubMed] [Google Scholar]
- 17.Katz DA, McCoy K, Sarrazin MV. Does improved continuity of primary care affect clinician-patient communication in VA? J Gen Intern Med. 2014;29(2(suppl 2)):S682–S688. doi: 10.1007/s11606-013-2633-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saultz JW. Defining and measuring interpersonal continuity of care. Ann Fam Med. 2003;1(3):134–143. doi: 10.1370/afm.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pollack CE, Hussey PS, Rudin RS, Fox DS, Lai J, Schneider EC. Measuring care continuity: a comparison of claims-based methods [published online December 3, 2013] Med Care. 2013 doi: 10.1097/MLR.0000000000000018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bice TW, Boxerman SB. A quantitative measure of continuity of care. Med Care. 1977;15(4):347–349. doi: 10.1097/00005650-197704000-00010. [DOI] [PubMed] [Google Scholar]
- 21.Breslau N, Haug MR. Service delivery structure and continuity of care: a case study of a pediatric practice in process of reorganization. J Health Soc Behav. 1976;17(4):339–352. [PubMed] [Google Scholar]
- 22.Steinwachs DM. Measuring provider continuity in ambulatory care: an assessment of alternative approaches. Med Care. 1979;17(6):551–565. doi: 10.1097/00005650-197906000-00001. [DOI] [PubMed] [Google Scholar]
- 23.Jee SH, Cabana MD. Indices for continuity of care: a systematic review of the literature. Med Care Res Rev. 2006;63(2):158–188. doi: 10.1177/1077558705285294. [DOI] [PubMed] [Google Scholar]
- 24.Nassery N. Systematic overuse of healthcare services: a conceptual model [published online September 6, 2014] Appl Health Econ Health Policy. doi: 10.1007/s40258-014-0126-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Segal JB, Bridges JF, Chang HY, et al. Identifying possible indicators of systematic overuse of health care procedures with claims data. Med Care. 2014;52(2):157–163. doi: 10.1097/MLR.0000000000000052. [DOI] [PubMed] [Google Scholar]
- 26.Chan KS, Chang E, Nassery N, Chang HY, Segal JB. The state of overuse measurement: a critical review. Med Care Res Rev. 2013;70(5):473–496. doi: 10.1177/1077558713492202. [DOI] [PubMed] [Google Scholar]
- 27.Weiner JP, Starfield BH, Steinwachs DM, Mumford LM. Development and application of a population-oriented measure of ambulatory care case-mix. Med Care. 1991;29(5):452–472. doi: 10.1097/00005650-199105000-00006. [DOI] [PubMed] [Google Scholar]
- 28.US Census Bureau. American Community Survey, 2005–2010, Median Household Income Table; generated by University of Michigan Population Studies Center. http://www.psc.isr.umich.edu/dis/census/Features/tract2zip/index.html Accessed March 5, 2014.
- 29.Nyweide DJ, Anthony DL, Bynum JPW, et al. Continuity of care and the risk of preventable hospitalization in older adults. JAMA Intern Med. 2013;173(20):1879–1885. doi: 10.1001/jamainternmed.2013.10059. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


