Abstract
Study Design
Retrospective cohort
Objective
To investigate the cervical alignment necessary for the maintenance of horizontal gaze depends on underlying thoracolumbar alignment
Summary of Background Data
Cervical curvature (CC) is affected by thoracic and global alignment. Recent studies suggest large variability in normative CC ranging from lordotic to kyphotic alignment. No previous studies have assessed the effect of global spinal alignment on CC in maintenance of horizontal gaze.
Methods
Patients without previous history of spinal surgery and were able to maintain their horizontal gaze while undergoing full body imaging were included. Patients were stratified based on thoracic kyphosis (TK) into (<30, 30–40, 40–50 and >50) then by SRS-Schwab sagittal vertical axis (SVA) modifier into (posterior alignment SVA<0, aligned 0–50 and malaligned >50mm). Cervical alignment was assessed among SVA grade in TK groups. Stepwise linear regression analysis was applied on random selection of 60% of the population. A simplified formula was developed and validated on the remaining 40%.
Results
In each TK group (n=118, 137, 125, 197), lower cervical curvature (C2-C7) was significantly more lordotic by increased Schwab SVA grade. T1 slope and cervical SVA significantly increased with increased thoracolumbar (C7-S1) SVA. Upper cervical curvature (C0-C2) and mismatch between T1 slope and cervical curvature (T1-CL) were similar. Regression analysis revealed LL minus TK (LL-TK) as an independent predictor (r=0.640, r2=0.410) with formula: CC = 10 - (LL-TK)/2. Validation revealed that the absolute difference between the predicted CC and the actual CC was 8.5°. Moreover, 64.2% of patients had their predicted C2-C7 values were within 10° of the actual CC.
Conclusions
Cervical kyphosis may represent normal alignment in a significant number of patients. However, in patients with SVA > 50 and greater thoracic curvatures, cervical lordosis is needed to maintain the gaze. Cervical alignment can be predicted from underlying TK and lumbar lordosis, which may be clinically relevant when considering correction for thoracolumbar or cervical deformity
Keywords: Cervical alignment, Horizontal gaze, Global Spinal Alignment
Introduction
For millennia, the human body has evolved in respect to two major goals: the maintenance of both bipedal standing position and horizontal gaze. Exclusive bipedal standing posture freed the upper limbs, allowed humans greater interaction with the environment. However, this adjustment was complicated by the need to support the cranium while maintaining a functional gaze.1–4 The relationship between alignment and the gaze necessitates a thorough understanding of the Cranio-spino-pelvic alignment as one component of Balance. Specific sagittal cranial and spino-pelvic parameters correlating to HRQOL scores have been described and published in numerous studies5–13.
Horizontal gaze is necessary for neurosensorial interactions with the surrounding environment, because it allows humans to avoid obstacles14 and helps regulate dynamic stability15–17. However, the cranium is intricately linked to its foundation, the cervical spine. In turn, the cervical spine must remain in harmony with the adjacent thoracic curvature and is significantly affected by the correction of thoracolumbar deformities in sagittally malaligned patients21,24,25.
Multiple aspects of the cervical spine have been well-described in the literature. Hardacker et al reported a normal range of cervical lordosis of 40° +/− 9.7°, with the majority of the lordosis occurring at the C1-C2 level26. Other authors have demonstrated that kyphotic alignment may occur in up to thirty percent of the normal population27,28. However, the cervical spine receives several inputs that influence its posture, and isolated investigations of this curvature may not adequately address its proper alignment.
Therefore, the purpose of the current study was to investigate the effect of thoracic and global alignment on the upper and lower cervical sagittal curves in their mission of maintaining a horizontal gaze.
Methods
Study design
This single-center study retrospectively reviewed full-body radiographs of primary patients who presented to a spine surgeon’s office with a diverse range of thoracolumbar pathologies. Inclusion criteria were patients older than 18 years who were able to maintain horizontal gaze without presenting with cervical complaints; maintenance of horizontal gaze as measured by CBVA between −5° and 17°, McGregor’s slope between −6° and 14° or slope of light of sight (SLS) between −5.1° and 18.5°29,30. Exclusion criteria included diagnosis of any cervical pathology, malignancies, infection, neuromuscular scoliosis, ankylosing spondylitis, fractures, and diffuse idiopathic skeletal hyperostosis.
Data collection and radiographic measurements
Demographic data including age, gender, BMI and history of previous surgery were collected. Full-body lateral radiographs were analyzed using a dedicated and validated software31. The following sagittal radiographic parameters were evaluated.
Cervical Parameters:
Lower cervical sagittal curve (CC): the angle between the lower endplate of C2 and the lower endplate of C7. Negative value denotes lordosis.
Upper cervical sagittal curve (C0–C2): the angle between McGregor line and lower endplate of C2. Negative value denotes lordosis.
C1 axis: the angle formed by the line passing through the center of the anterior and posterior tubercule of the atlas and the horizontal
C2-C7 sagittal vertical axis (cSVA): the horizontal offset of a plumb line dropped from the center of C2 vertebral body to the postero-superior corner of C7 vertebra
T1 slope minus cervical lordosis (TS-CL)
Thoracolumbar Parameters:
Thoracic kyphosis (TK): the angle between the upper endplate of T1 and the lower endplate of T12
Lumbar lordosis (LL): the angle between the upperendplate of L1 and the upper endplate of S1 vertebra
Sacral slope (SS): the angle between upper endplate of S1 and the horizontal
Sagittal vertical axis (SVA): the horizontal offset from a plumb line dropped from the center of C7 vertebral body to the postero-superior corner of S1 vertebra
Horizontal Gaze Parameters:
Chin brow vertical angle (CBVA): angle subtended between a line between the brow to the chin and the vertical
McGregor slope (McGS: angle between the line from the postero-superior aspect of the hard palate to the caudal aspect of the opisthion and the horizontal)
Slope of line of sight (SLS): angle between Frankfurt line and the horizontal (Figure 1)
Figure 1.
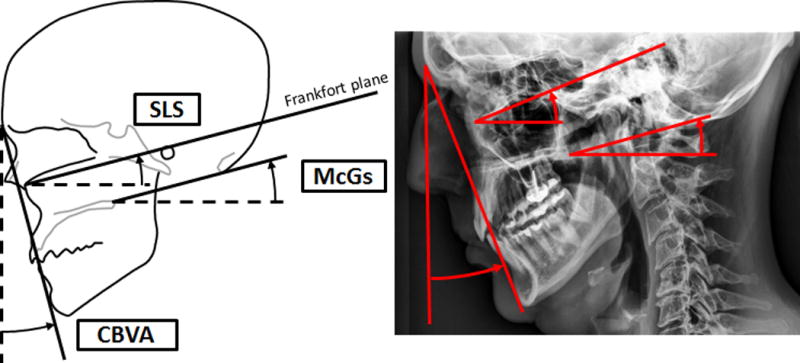
Horizontal Gaze Parameters. McGS is McGregor slope; angle between the line from the postero-superior aspect of the hard palate to the caudal aspect of the opisthion and the horizontal. SLS is Slope of line of sight; angle between Frankfurt line and the horizontal. CBVA is Chin brow vertical angle which is subtended between a line between the brow to the chin and the vertical.
Statistical Analysis
The study population was described using descriptive analysis. Patients were stratified based on thoracic kyphosis (TK) (<30°, 30°−40°, 40°–50°, and >50°), then based on Scoliosis Research Society-Schwab SVA grade (posterior alignment SVA<0 mm, neutral alignment 0–50mm, and anterior positive malalignment >50mm). Cervical parameters were analyzed by comparison between SVA groups inside each TK group using analysis of variance (ANOVA). Pearson correlation was used to investigate relationships between cervical and thoracolumbar parameters.
Formula Development and Validation
A random selection of 60% of the study population was used to develop the formula, and the remaining 40% was used for formula validation. Stepwise linear regression analysis was performed to predict lower cervical sagittal curve based on thoracic kyphosis and lumbar lordosis along with global spinal alignment (SVA), controlling for patient age, gender, pelvic morphology. A simplified formula was derived from this analysis. For validation, the percentage of patients with predicted CC within 10° of their actual CC was investigated. ISO (International Organization of Standardization) reproducibility of lower CC used in this software was 5.87°31. Level of significance was set at p < 0.05.
Results
There were 577 patient visits included, with the patients’ mean age 54.8 ± 19.5 years; mean BMI 27.0 ± 6.1 kg/m2 (mean weight: 74.3kg, mean height: 1.66 m), and 65.7% females. Diagnoses included were: 99 degenerative disc disease, 58 degenerative spondylolisthesis, and 420 adult spinal deformity patients. Overall, 168 visits out of 577 (29.1%) maintained a horizontal gaze with kyphotic cervical alignment. These patients were significantly younger (42.2 vs. 59.9 years old, p=0.001) than patients with lordotic cervical alignment, and had less BMI (25.7 vs. 27.4, p=0.016), and a similar proportion of females 66.7% vs. 65.3%.
Group Analysis
The number of visits in each SVA group was as follows: (SVA < 0 mm: 211, SVA 0–50 mm: 249, SVA > 50 mm: 117). The number of visits in each TK groups was as follows: (TK <30° – 118), (TK 30–40° – 137), (TK 40°–50° – 125), and (TK > 50° – 197). The distribution of SVA visits in each TK groups was not significantly different (p=0.155).
Cervical alignment analysis
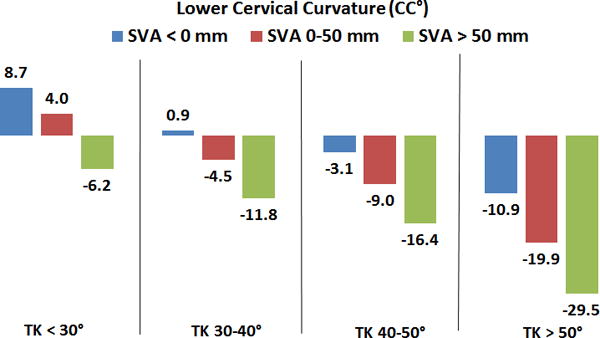
Within each TK group, the lower cervical sagittal curve became significantly more lordotic with increasing SVA (Figure 2). All patients with SVA > 50 mm or TK > 40° had lordotic CC. Patients who were posteriorly aligned (SVA < 0 mm) had kyphotic alignment when TK < 40° but neutral alignment when TK was 40–50°. Patients with TK > 50° had lordotic CC, regardless of SVA. All p < 0.05.
Figure 2.
Comparison of lower cervical sagittal curve (C2-C7) in SRS-Schwab SVA groups in every group of Thoracic Kyphosis. Negative values denote cervical kyphosis. P=0.001 for all comparisons.
cSVA significantly increased with increased SVA groups (Table 1). Upper cervical sagittal curve (C0-C2) and C1 axis were similar between all SVA groups. C0-C2 ranged between −28.8°– −31.4° (p > 0.6 in all TK groups), whereas C1 axis ranged between 10.0° – 14.1° (p > 0.18 in all TK groups). TS-CL was also similar between SVA groups and ranged between 17.5°- 22.2° (p > 0.24 in all TK groups). However, T1 slope significantly increased with increase SVA in each TK group (Table 2). Correlation analysis revealed that upper cervical sagittal curve (C0-C2) correlated with cSVA (r=−0.270, p=0.001), but did not correlate with SVA (r=−0.054, p=0.196). However, Lower CC (C2-C7) was correlated with SVA (r=−0.431, p=0.001) and cSVA (r=−0.248, p=0.001).
Table 1.
Comparison between cervical sagittal vertical axis (cSVA) between SVA groups in each TK group.
| cSVA mm | ||||
|---|---|---|---|---|
| TK < 30 | TK 30–40 | TK 40–50 | TK > 50 | |
| SVA < 0 | 18.3 | 19.7* | 23.2* | 31.9* |
| SVA 0–50 | 19.5 | 25.3* | 24.5ǂ | 33.9 |
| SVA > 50 | 22.5 | 28.8 | 33.8 *ǂ | 41.0* |
| P value | 0.28 | 0.001 | 0.001 | 0.001 |
denote significant difference P=0.001 for all comparisons.
Table 2.
Comparison between T1 Slope between SVA groups in each TK group.
| T1 Slope (°) | ||||
|---|---|---|---|---|
| TK < 30 | TK 30–40 | TK 40–50 | TK > 50 | |
| SVA < 0 | 11.6 | 18.2 | 22.8 | 32.9 |
| SVA 0–50 | 15.7 | 23.5 | 28.4 | 39.7 |
| SVA > 50 | 23.8 | 32.4 | 37.4 | 51.7 |
| P value | 0.28 | 0.001 | 0.001 | 0.001 |
P=0.001 for any comparison between SVA groups.
Age analysis
Older age independently correlated with increased values of both TK and SVA (P<0.05). Of the cases with kyphotic cervical alignment, patients with TK < 30° and negative SVA (<0mm) were younger (mean age 38.2 years) than patients with TK 30–40° and SVA <0mm (mean age 43.7 years). Following this trend, the patients with kyphotic cervical alignment, TK<30°, and SVA 0–50mm had mean age 52.1 years. (Table 3)
Table 3.
Comparison of age between SVA groups in each TK group. Lower cervical curvature measures are in between parentheses.
| Patients’ Age (Cervical curvature measure) | |||||
|---|---|---|---|---|---|
| TK < 30 | TK 30–40 | TK 40–50 | TK > 50 | P value | |
| SVA < 0 | 38.2 (+8.7°) | 43.7 (+0.9°) | 43.8 (−3.1°) | 49.9 (−10.9°) | 0.002 |
| SVA 0–50 | 52.1 (+4.0°) | 53.5 (−4.5°) | 56.0 (−9.0°) | 62.3 (−19.9°) | 0.002 |
| SVA > 50 | 68.2 (−6.2°) | 65.9 (−11.8°) | 65.1 (−16.4°) | 73.0 (−29.5°) | 0.041 |
| P value | 0.28 | 0.001 | 0.001 | 0.001 | 0.001 |
Formula development
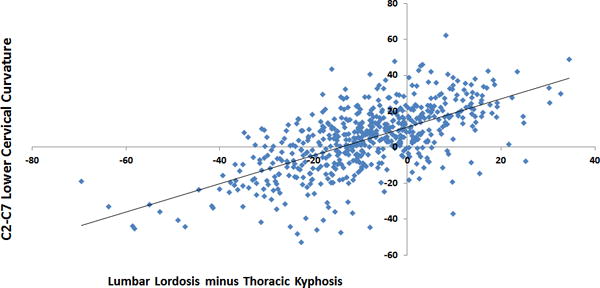
345 (57.88%) visits were included. Regression analysis demonstrated that LL minus TK (LL-TK: both with absolute value) was an independent predictor of CC (R=0.640, R2=0.410, p<0.05) (Figure 3). Addition of SS to the model improved the CC prediction capability to R= 0.799. The simplified version of LL-TK model was denoted by the following: CC = 10 - (LL-TK)/2.
Figure 3.
Scatter plot between cervical sagittal curve (C2-C7) and lumbar lordosis minus thoracic kyphosis
Formula validation
For validation of this formula, 232 visits were included. The absolute difference between the predicted CC and the actual CC was 8.5°. 64.2% of predicted CC values were within 10° of the actual CC values.
Discussion
Cervical kyphosis is a prevalent phenomenon and is often interpreted to indicate cervical deformity. However, studies have shown that in up to 30% of patients, cervical kyphosis may simply be a component of normal sagittal spinal alignment.27,28,32 Thus, it is clear that in some patients, the presence of a kyphotic cervical alignment may indicate substantial deformity and be linked to poor clinical outcomes, while in others, a kyphotic cervical alignment may be appropriate given the patient’s global and thoracic sagittal alignment. There is therefore an obvious need to more accurately define cervical deformity and distinguish it from cervical compensation for thoracolumbar alignment. This study sought to investigate the relationship between cervical alignment, thoracic kyphosis, and the global sagittal alignment.
In the present study, of all patients who presented to the spine surgeon’s office without cervical complaints, 29% were able to maintain horizontal gaze with kyphotic cervical alignment, which is consistent with rates in previous literature27,28,32. These patients were younger with lower BMI, though they were otherwise similar in gender.
The current results demonstrate that in patients with normal horizontal gaze, thoracolumbar alignment and thoracic kyphosis independently impacted cervical alignment. As thoracic kyphosis increased, the amount of lower cervical lordosis increased. Similarly, as the global alignment (assessed by SVA) progressed (greater than 0mm), cervical lordosis increased as well. Conversely, posterior global alignment and flattening of the thoracic spine led to progressive cervical kyphosis. These findings were echoed by Yu et al, who studied both symptomatic and asymptomatic patients and found that larger curvatures in the thoracic and lumbar spines were associated with greater cervical lordosis.33
Based on these findings, kyphotic alignment of the cervical spine cannot alone define cervical deformity. Correspondingly, cervical lordosis should not be synonymous with harmonious alignment. In patients with severe thoracic kyphosis or large global malalignment, increased cervical lordosis may actually be functioning as a compensatory mechanism to maintain horizontal gaze.34 In general, this data showed that patients were able to maintain the horizontal gaze with mean C2-C7 values that ranged from 8.7 of kyphosis to −29.5 degrees of lordosis.
Though it appeared that global alignment of the spine was closely linked to the lower cervical sagittal curve (CC), the upper lordosis (C0-C2) consistently remained around −30°. Though this value is somewhat higher than the means of 14–16° reported by Le Huec et al27 and Park et al,35 both other studies and the present study found consistent values of the C0-C2 in patients without cervical complaints, despite variations in other thoracolumbar parameters. Importantly, however, these studies only established the consistency of the C0-C2 angle in asymptomatic individuals, and presumably, those able to maintain horizontal gaze. If the C2-C7 region is capable of providing the adequate regional cervical alignment necessary for maintenance of the horizontal gaze, the C0-C2 angle will remain constant across ages and thoracolumbar alignment parameters. Yet in patients with true cervical deformity, such as those with severely malaligned cSVA, the C0-C2 region may be recruited as an additional compensatory mechanism to maintain horizontal gaze. This hypothesis was supported by Protopsaltis et al23, who found that the C0-C2 varied in patients with thoracolumbar deformity and concomitant cervical malalignment. Therefore, this value of approximately 30° for the C0-C2 may serve as potential threshold for classifying cervical deformity. If larger than 30°, this angle may represent increased compensation from the upper cervical region for a regional lower cervical deformity.
In addition, this study investigated the cervical SVA (cSVA) across the patient groups. Among all of the alignment subgroups, the highest cSVA was observed in the group with SVA > 50mm and TK > 50°. This value of 41mm for cSVA thus represented the maximum amount of cSVA tolerated by patients while still remaining asymptomatic and able to maintain horizontal gaze. Importantly, this value is nearly identical to the threshold of cSVA=40mm that corresponds to poor health-related quality of life scores as described by Tang et al.36
From these findings, a different understanding of cervical deformity arises: the inability (or, the painful/symptomatic ability) to maintain horizontal gaze. Recent work from Blondel et al25 and Barrey et al37 suggested that because patients with lordotic CC have significantly greater values for SRS-Schwab sagittal parameters (SVA, PT, and PI-LL), increasing cervical lordosis is required as a compensatory mechanism to maintain horizontal gaze. In this study, patients with SVA > 50 mm were more likely to adapt lordotic cervical alignment, regardless of their thoracic kyphosis. These patients were also significantly older than patients with less drastic values for thoracic kyphosis and global alignment. Related work from Schwab et al proposed age-adjusted alignment targets based on health-related quality of life scores; for example, for patients > 65 years old, SVA between 50–65 mm is actually ideal.38 For these older patients or other individuals with an element of positive global malalignment (SVA > 50 mm), a kyphotic cervical alignment is less likely to be adequate to keep an horizontal gaze. Thus, a thorough evaluation of thoracolumbar alignment is necessary for the evaluation of potential cervical realignment patients.
Finally, the present study proposed a preliminary formula to predict the cervical alignment necessary for horizontal gaze. The mismatch between lumbar lordosis and thoracic kyphosis (LL-TK) was an independent predictor of C2-C7 sagittal curve. The following simplified formula was developed using this parameter: CC = 10 - (LL-TK)/2. Understood in a clinical context, several scenarios may lead to the need for increased cervical lordosis following the reverse pendulum concept of Dubousset39. The first possibility is isolated thoracic hyperkyphosis, which would warrant increased cervical lordosis. However, increased cervical lordosis would also be needed for a patient with pathologic loss of lordosis, and lack of compensatory thoracic hypokyphosis. Future work investigating additional clinical applications for this formula will undoubtedly be valuable.
This study also investigated the role of the T1 slope across the different TK and SVA subgroups. T1 slope significantly increased with increases in both thoracic kyphosis and global alignment, with a minimum of 11.6 in when TK was <30° and SVA was <0mm, and a maximum of 51.7° when TK was >50° and SVA was >50mm. These targets for each specific thoracic kyphosis and global alignment may be useful in surgical planning for patients undergoing correction of major sagittal deformity. By taking these ideal T1 slope values into account, surgeons may respect the ideal cervical alignment necessary to maintain horizontal gaze while still performing the adequate thoracolumbar reconstruction. For example: Fifty five year old patient is undergoing cervical realignment surgery with SVA of 40 mm, TK of 35° and LL of 50°. Based on patients of this study (Table 3), the cervical alignment necessary to maintain the horizontal gaze was slightly lordotic and measured about 4.5°. CC can also be calculated using the formula: CC = 10 – (50–35)/2 = 2.5°. On the other hand, if this patient is undergoing thoracolumbar fusion to the upper thoracic region, T1 slope is recommended to be about 23.5° (Table 2).
Several limitations in this study are recognized. The first is the heterogeneity of the cohort; the patients used in this study represented a wide variety of visits to the spine surgeon’s office for any matters not pertaining to the cervical spine. In addition, the alignment ideals set forth in this study are closely linked to maintenance of horizontal gaze, though future studies should consider additional variables in the role of the cervical spine, including head positioning, chest and face morphologies, and soft tissue/muscular involvement. This study addressed a small part of the entire understanding of postural alignment and horizontal gaze. It remains important for an ambulating person to have enough flexion in the Cranio-thoracic area to allow vision of his or her feet to avoid stumbling while ambulating. If this is not present, leaning on a walker or two canes is necessary for safety. Of course, additional validation with health-related quality of life outcomes would be critical.
Conclusion
Despite the traditional thought that cervical kyphosis is indicative of cervical deformity, it may actually represent normal alignment in a significant number of well-aligned or posteriorly aligned patients. However, in patients with SVA > 50mm and greater thoracic kyphosis, cervical lordosis is needed to maintain the gaze. Cervical alignment can be predicted from underlying TK and lumbar lordosis, or suggested values of T1 slope, which may be clinically relevant when considering correction for thoracolumbar or cervical deformity.
Acknowledgments
The manuscript submitted does not contain information about medical device(s)/drug(s).
No funds were received in support of this work.
Relevant financial activities outside the submitted work: board membership, payment for lectures, grants, stocks.
Footnotes
Level of Evidence: 3
References
- 1.Lovejoy CO. The origin of man. Science. 1981;211:341–50. doi: 10.1126/science.211.4480.341. [DOI] [PubMed] [Google Scholar]
- 2.Lovejoy CO. The natural history of human gait and posture Part 1. Spine and pelvis Gait Posture. 2005;21:95–112. doi: 10.1016/j.gaitpost.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 3.Lovejoy CO, Suwa G, Spurlock L, et al. The Pelvis and Femur of Ardipithecus ramidus: The Emergence of Upright Walking. Science (80-) 2009;326:71–71. 71e1–71e6. [PubMed] [Google Scholar]
- 4.Friedman MJ. The Evolution of Hominid Bipedalism. 2006 [Google Scholar]
- 5.Schwab FJ, Lafage V, Boyce R, et al. Gravity line analysis in adult volunteers: age-related correlation with spinal parameters, pelvic parameters, and foot position. Spine (Phila Pa 1976) 2006;31:E959–67. doi: 10.1097/01.brs.0000248126.96737.0f. [DOI] [PubMed] [Google Scholar]
- 6.Bess S, Kai-Ming GF, Lafage V, et al. Disease State Correlates for Pain and Disability in Adult Spinal Deformity (ASD); Assessment Guidelines for Health Care Providers. Spine J. 2013;13:109S–110S. [Google Scholar]
- 7.Terran J, Schwab FJ, Shaffrey CI, et al. The SRS-Schwab Adult Spinal Deformity Classification: Assessment and Clinical Correlations Based on a Prospective Operative and Nonoperative Cohort. Neurosurgery. 2013;73:559–68. doi: 10.1227/NEU.0000000000000012. [DOI] [PubMed] [Google Scholar]
- 8.Lafage V, Schwab FJ, Patel A, et al. Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine (Phila Pa 1976) 2009;34:E599–E606. doi: 10.1097/BRS.0b013e3181aad219. [DOI] [PubMed] [Google Scholar]
- 9.Smith JS, Shaffrey CI, Glassman SD, et al. Clinical and radiographic parameters that distinguish between the best and worst outcomes of scoliosis surgery for adults. Eur Spine J. 2013;22:402–10. doi: 10.1007/s00586-012-2547-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schwab F, Ungar B, Blondel B, et al. SRS-Schwab Adult Spinal Deformity Classification: A Validation Study. Spine (Phila Pa 1976) 2012;37:1077–1082. doi: 10.1097/BRS.0b013e31823e15e2. [DOI] [PubMed] [Google Scholar]
- 11.Schwab FJ, Blondel B, Bess S, et al. Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine (Phila Pa 1976) 2013;38:E803–12. doi: 10.1097/BRS.0b013e318292b7b9. [DOI] [PubMed] [Google Scholar]
- 12.Schwab FJ, Bess RS, Blondel B, et al. Combined Assessment of Pelvic Tilt, Lumbar Lordosis/Pelvic Incidence Mismatch and Sagittal Vertical Axis Predicts Disability in Adult Spinal Deformity: A Prospective Analysis. Spine J. 2011;11:S158–S159. [Google Scholar]
- 13.Lafage R, Challier V, Liabaud B, et al. Natural Head Posture in the Setting of Sagittal Spinal Deformity: Validation of Chin-Brow Vertical Angle, Slope of Line of Sight, and McGregor’s Slope With Health-Related Quality of Life. Neurosurgery. 2015 doi: 10.1227/NEU.0000000000001193. [DOI] [PubMed] [Google Scholar]
- 14.Patla AE, Prentice SD, Robinson C, et al. Visual control of locomotion: strategies for changing direction and for going over obstacles. J Exp Psychol Hum Percept Perform. 1991;17:603–34. doi: 10.1037//0096-1523.17.3.603. [DOI] [PubMed] [Google Scholar]
- 15.Patla AE, Vickers JN. How far ahead do we look when required to step on specific locations in the travel path during locomotion? Exp brain Res. 2003;148:133–8. doi: 10.1007/s00221-002-1246-y. [DOI] [PubMed] [Google Scholar]
- 16.Patla AE, Niechwiej E, Racco V, et al. Understanding the contribution of binocular vision to the control of adaptive locomotion. Exp brain Res. 2002;142:551–61. doi: 10.1007/s00221-001-0948-x. [DOI] [PubMed] [Google Scholar]
- 17.Patla AE. Understanding the roles of vision in the control of human locomotion. Gait Posture. 1997;5:54–69. [Google Scholar]
- 18.Min K, Hahn F, Leonardi M. Lumbar spinal osteotomy for kyphosis in ankylosing spondylitis: the significance of the whole body kyphosis angle. J Spinal Disord Tech. 2007;20:149–53. doi: 10.1097/01.bsd.0000211252.67576.d9. [DOI] [PubMed] [Google Scholar]
- 19.Sansur CA, Fu K-MG, Oskouian RJ, et al. Surgical management of global sagittal deformity in ankylosing spondylitis. Neurosurg Focus. 2008;24:E8. doi: 10.3171/FOC/2008/24/1/E8. [DOI] [PubMed] [Google Scholar]
- 20.van Royen BJ, Scheerder FJ, Jansen E, et al. ASKyphoplan: a program for deformity planning in ankylosing spondylitis. Eur Spine J. 2007;16:1445–9. doi: 10.1007/s00586-007-0371-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Scheer JK, Tang JA, Smith JS, et al. Cervical spine alignment, sagittal deformity, and clinical implications. J Neurosurg Spine. 2013;19:141–59. doi: 10.3171/2013.4.SPINE12838. [DOI] [PubMed] [Google Scholar]
- 22.Van Royen BJ, De Gast A, Smit TH. Deformity planning for sagittal plane corrective osteotomies of the spine in ankylosing spondylitis. Eur Spine J. 2000;9:492–8. doi: 10.1007/s005860000183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Protopsaltis TS, Lafage R, Lafage V, et al. Upper cervical compensation and maintenance of horizontal gaze in 150 thoracolumbar deformity patients with and without cervical deformity. Int Meet Adv Spine Tech. 2014 [Google Scholar]
- 24.Ames CP, Blondel B, Scheer JK, et al. Cervical radiographical alignment: comprehensive assessment techniques and potential importance in cervical myelopathy. Spine (Phila Pa 1976) 2013;38:S149–60. doi: 10.1097/BRS.0b013e3182a7f449. [DOI] [PubMed] [Google Scholar]
- 25.Smith JS, Shaffrey CI, Lafage V, et al. Spontaneous improvement of cervical alignment after correction of global sagittal balance following pedicle subtraction osteotomy. J Neurosurg Spine. 2012;17:300–7. doi: 10.3171/2012.6.SPINE1250. [DOI] [PubMed] [Google Scholar]
- 26.Hardacker JW, Shuford RF, Capicotto PN, et al. Radiographic standing cervical segmental alignment in adult volunteers without neck symptoms. Spine (Phila Pa 1976) 22:1472–1480. doi: 10.1097/00007632-199707010-00009. discussion 1480 (1997) [DOI] [PubMed] [Google Scholar]
- 27.Le Huec JC, Demezon H, Aunoble S. Sagittal parameters of global cervical balance using EOS imaging: normative values from a prospective cohort of asymptomatic volunteers. Eur Spine J. 2014;24:63–71. doi: 10.1007/s00586-014-3632-0. [DOI] [PubMed] [Google Scholar]
- 28.Yukawa Y, Kato F, Suda K, et al. Age-related changes in osseous anatomy, alignment, and range of motion of the cervical spine. Part I: Radiographic data from over 1,200 asymptomatic subjects. Eur Spine J. 2012;21:1492–8. doi: 10.1007/s00586-012-2167-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lafage R, Challier V, Ferrero E, et al. Validation of Correlation between CBVA, SLS and McGregor’s Slope. Scoliosis Res Soc (SRS) Sept. 2014:10–13. [Google Scholar]
- 30.Lafage VC, Ferrero E, Lafage R, et al. Validation of Correlation between Chin Brow Vertical Angle (CBVA), Slope of Line of Sight (SLS), and McGregor’s Slope (McGS) for Cervical Disability. Cerv Spine Res Soc Annu Meet December. 2014:5–7. [Google Scholar]
- 31.Lafage R, Ferrero E, Henry JK, et al. Validation of a new computer-assisted tool to measure spino-pelvic parameters. Spine J. 2015 doi: 10.1016/j.spinee.2015.08.067. [DOI] [PubMed] [Google Scholar]
- 32.Huec JC, Le Demezon H, Aunoble S. L’équilibre sagittal du rachis cervical sur une population asymptomatique : Nouveaux paramètres et valeurs standards Sagittal parameters of cervical global balance Normative values from a prospective cohort of asymptomatic volunteers. e-mémoires l’Académie Natl Chir. 2013;12:18–24. [Google Scholar]
- 33.Yu M, Zhao WK, Li M, et al. Analysis of cervical and global spine alignment under Roussouly sagittal classification in Chinese cervical spondylotic patients and asymptomatic subjects. Eur Spine J. 2015:1265–1273. doi: 10.1007/s00586-015-3832-2. [DOI] [PubMed] [Google Scholar]
- 34.Scheer JK, Tang JA, Smith JS, et al. Cervical spine alignment, sagittal deformity, and clinical implications: a review. J Neurosurg Spine. 2013;19:141–59. doi: 10.3171/2013.4.SPINE12838. [DOI] [PubMed] [Google Scholar]
- 35.Park MS, Moon SH, Lee HM, et al. The effect of age on cervical sagittal alignment: normative data on 100 asymptomatic subjects. Spine (Phila Pa 1976) 2013;38:E458–63. doi: 10.1097/BRS.0b013e31828802c2. [DOI] [PubMed] [Google Scholar]
- 36.Tang JA, Scheer JK, Smith JS, et al. The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery. Neurosurgery. 71:662–9. doi: 10.1227/NEU.0b013e31826100c9. discussion 669 (2012) [DOI] [PubMed] [Google Scholar]
- 37.Barrey CC, Roussouly P, Le Huec JCC, et al. Compensatory mechanisms contributing to keep the sagittal balance of the spine. Eur Spine J. 2013;22(Suppl 6):S834–41. doi: 10.1007/s00586-013-3030-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schwab FJ, Lafage R, Liabaud BB, et al. Does One Size Fit All? Defining Spinopelvic Alignment Thresholds Based on Age. Spine J. 2014;14:S120–S121. [Google Scholar]
- 39.Dubousset J. Pediatr Spine Princ Pract (SL, W) Raven Press; 1994. pp. 479–496. 1994. [Google Scholar]


