Abstract
Objectives
To assess the opinion of intensive care unit (ICU) personnel and the impact of their personality and religious beliefs on decisions to forego life-sustaining treatments (DFLSTs).
Setting
Cross-sectional, observational, national study in 18 multidisciplinary Greek ICUs, with >6 beds, between June and December 2015.
Participants
149 doctors and 320 nurses who voluntarily and anonymously answered the End-of-Life (EoL) attitudes, Personality (EPQ) and Religion (SpREUK) questionnaires. Multivariate analysis was used to detect the impact of personality and religious beliefs on the DFLSTs.
Results
The participation rate was 65.7%. Significant differences in DFLSTs between doctors and nurses were identified. 71.4% of doctors and 59.8% of nurses stated that the family was not properly informed about DFLST and the main reason was the family’s inability to understand medical details. 51% of doctors expressed fear of litigation and 47% of them declared that this concern influenced the information given to family and nursing staff. 7.5% of the nurses considered DFLSTs dangerous, criminal or illegal. Multivariate logistic regression identified that to be a nurse and to have a high neuroticism score were independent predictors for preferring the term ‘passive euthanasia’ over ‘futile care’ (OR 4.41, 95% CI 2.21 to 8.82, p<0.001, and OR 1.59, 95% CI 1.03 to 2.72, p<0.05, respectively). Furthermore, to be a nurse and to have a high-trust religious profile were related to unwillingness to withdraw mechanical ventilation. Fear of litigation and non-disclosure of the information to the family in case of DFLST were associated with a psychoticism personality trait (OR 2.45, 95% CI 1.25 to 4.80, p<0.05).
Conclusion
We demonstrate that fear of litigation is a major barrier to properly informing a patient’s relatives and nursing staff. Furthermore, aspects of personality and religious beliefs influence the attitudes of ICU personnel when making decisions to forego life-sustaining treatments.
Keywords: Decisions to foregolife sustaining treatment (DFLST), End-of-Life (EoL), personality, religiousness
Strengths and limitations of this study.
This is one of the few studies that probes the influence of personality and religious beliefs on the decisions to forego life sustaining treatments (DFLSTs) in the intensive care unit (ICU).
The study reports the opinions of ICU professionals on DFLSTs from a culturally and religiously homogenous group, thus eliminating multicultural and religious confounders.
The study confirms that fear of litigation is a major barrier to properly informing the patients’ relatives and nursing staff about end-of-life decisions.
The main weakness is that the study does not take into consideration the opinion of the 34.3% who declined to participate in the survey, thus leading to a representation bias.
Introduction
Modern medicine, especially intensive care with all the technological advances in life support, has “brought the epoch of natural death to an end”.1 Intensive care unit (ICU) patients may be caught up in a medical logic that is less focused on human suffering and dignity than on a struggle to maintain vital functions with the use of ventilators, inotropes, renal replacement, surgery and transplantations.2 Numerous studies recognise the necessity of limiting life support in ICUs and the implementation of a palliative care strategy.2–5 However, withholding or withdrawing medical therapy, thus hastening death, may induce suffering, trauma, compassion fatigue and even post-traumatic stress disorder (PTSD) in ICU healthcare professionals.5–8 This moral distress is accentuated by the ethical ambivalence around end-of-life (EoL).9 ICU doctors and nurses are trapped between the autonomy of the patient or his/her relatives to continue futile treatment, and the benevolence and non-maleficence that may mean withdrawing or never withdrawing futile treatment. Another moral burden to the ICU staff is that our society and even our medical colleagues do not necessarily understand what can be and cannot be achieved in the ICU, frequently insisting to continue active treatment.9
Healthcare professionals involved in EoL decisions may be influenced by cultural, geographical, legal, financial, religious and personal characteristics.3 10–12 There are few studies, using different questionnaires, exploring the influence of religious orientation and personality on the decisions to forego life-sustaining treatments (DFLST).13 However, in these studies the participants were non-ICU professionals. We conducted a multicentre cross-sectional study with a primary endpoint to investigate the attitudes of the ICU personnel towards EoL decisions, and a secondary end point to probe if aspects of personality and religious beliefs may influence DFLSTs.
Participants and methods
Participants
According to the national legislature all ICUs in Greece are multidisciplinary. All level 3 ICUs in the university and general hospitals in Greece with no less than six beds—totalling 21—were invited to participate, and 18 of them took part in the study. ICUs with fewer than six beds were excluded because they are primarily located in small hospitals and often serve as step-down units. Figure 1 provides the flow chart of the participating ICUs and the number of participants. The medical director and the senior head nurse of each ICU were informed beforehand about the study, and gave detailed information about the number of their staff (number of doctors and nurses working full time in their ICU). Questionnaires were delivered by the primary investigator after presenting in detail the study to the medical and nursing staff in all ICUs, except for four, in which the medical directors and head nurses undertook this responsibility. In all ICUs, a staff member was designated to voluntarily collect the completed questionnaires and send them back to the primary investigator centre. Participation in the study was not compulsory, and all ICU staff working for at least 6 months in the ICU were invited to participate in the study. Anonymity was particularly emphasised to all participants.
Figure 1.
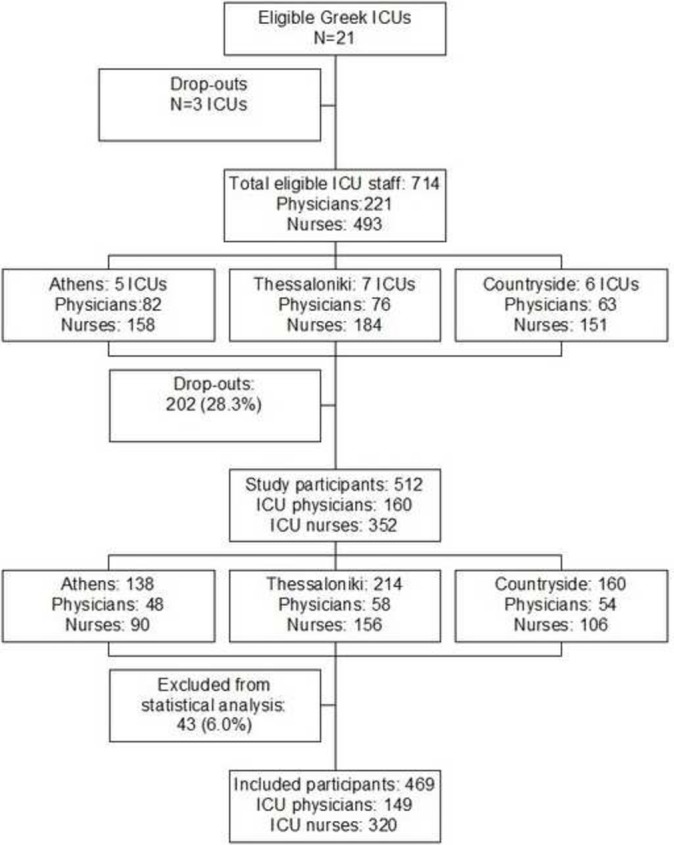
Flow chart demonstrating the participating intensive care units (ICUs) and the number of participants.
Methods
Three questionnaires were used for this study:
The survey questionnaire
This questionnaire was first developed by Ferrand and colleagues in a similar French multicentre study.13 It was preferred among other alternatives, primarily because it was considered efficient for extracting detailed information on the subject of our study. The questionnaire was translated by two Greek intensivists who had worked in France for many years and were equally proficient in both languages. The questionnaire was translated from French to Greek and from Greek to French according to the Brislin model for instrument translation, which is a well-known method for cross-cultural research.14 15 The back translation was done by blinding the second translator to the original document. Both versions (the original and the back translated document) were compared for accuracy. The final form of the Greek version, after being checked for accuracy, maintained the structure of the original questionnaire. The topics investigated were: (1) attitude towards EoL including information about the current EoL decision-making process; (2) the criteria used for DFLST; (3) caregivers' satisfaction of this process; (4) ICU commitment on high ethical standards; (5) communication with the family; (6) legal responsibility and fear of litigation; (7) the satisfaction of the ICU staff with the current practices and future aspects. The pre-test of the questionnaire was conducted with the aid of semi-structured interviews taken from ICU physicians and nurses, in order to ensure that the questions were comprehensible and that all potential answers were provided. Because the special terminology (‘withdrawing’, ‘withholding’, ‘high ethical standards’, ‘high quality decision making process’) included in the questionnaire might be ambiguous or open to a variety of personal interpretations, the definitions were incorporated into the questionnaires.
The Eysenck Personality Questionnaire (EPQ 84 items)
This questionnaire, developed by Eysenck16 and validated in the Greek language by Dimitriou,17 consists of 84 entries evaluated by the participant with a yes or no answer. The questionnaire mainly explores three dimensions of personality: neuroticism (N), psychoticism (P), and extraversion (E). A typical high N scorer is an anxious, worrying individual who is moody and frequently depressed. He may be overly emotional, reacts too strongly to all sorts of stimuli, and finds it difficult to return to a calmer state after each emotionally arousing experience. On the other hand, the high P scorer is defined as a personality type that is prone to take risks, and might engage in antisocial or non-conformist behaviour. A typical P scorer displays recklessness and impulsiveness, has a disregard for common sense, and has inappropriate emotional expression. Finally, an extrovert is defined as being sociable, optimistic, impulsive and carefree. A typical E scorer is outgoing, talkative, energetic, assertive and gregarious.
The Spiritual and Religious Questionnaire (SpREUK 15 items)
This questionnaire deals with the spiritual and religious attitude of the participants. As it avoids exclusive religious terminology, it is suitable for use in both secular and religious societies. Although it was developed to investigate patients with chronic diseases, it is suitable for use in healthcare research.6 It consists of 15 items and differentiates three religiousness dimensions:
Trust: is a measure of intrinsic religiosity dealing with the subjects’ conviction to be connected with a higher source which carries through, and to be sheltered and guided by this sourceirrespective of the consequences.
Reflection:reflects on what is essential in life; hint to change life; chance for development; illness has meaning; death leads to personal growth etc.
The items of the SpREUK are scored on a 5-point scale (0-4) from disagreement to agreement, and the scores can be referred to a 100% level (transformed scale score). Scores >50% indicate a positive attitude, while scores <50% indicate a negative one. Trust scale (religious) is strongly correlated with the engagement in conventional religious practices;Search scale is strongly associated with engagement in spiritual practices; and Reflection scale is moderately associated with engagement in existential practices. Search and trust are separate scales although strongly inter-correlated.
Ethical approval
The study protocol was approved by the ethics committee of the primary investigating hospital (protocol no. 202/05/05/2014) and the national health authority (protocol no. Δ3β/23441/26/09/2014). The above is in accordance with the procedure conducted for national studies. The study was non-compulsory and anonymous for the participants; therefore, no informed consent was obtained. The study was conducted between June and December 2015.
Statistical analysis
Statistical analysis was performed using the SPSS version 11.5 (SPSS Inc, Chicago). All values of p<0.05 were considered significant. Table entries represent numbers with related percentages (%) or medians with 25th–75th IQR, as appropriate. Sample comparisons between ICU physicians and nurses were performed with the Χ2 test of independence for categorical variables, and Mann-Whitney U test for non-parametrical continuous variables with two degrees of freedom. Because our study was cross-sectional, we were limited in our ability to assess causal factors of DFLST attitudes; however, univariate and multivariate logistic regression analysis was performed to identify participant or ICU-related variables, and aspects of personality and religious beliefs as independent predicting factors for specific attitudes towards EoL. In the case of all EPQ and SpREUK variables, cut-off limits could not be applied as there was no literature to support it. However, we used the medians of our sample of participant scores as indicative of splitting each score into two groups (high vs low).
Results
Detailed information for all questions and answers of all participants for the survey questionnaire are provided in the supplementary material (see online supplementary table 1, table 2, table 3). A sampling of information from the survey questionnaire and detailed information of the other questionnaires are provided below.
bmjopen-2016-013916supp001.pdf (258.5KB, pdf)
bmjopen-2016-013916supp002.pdf (247.7KB, pdf)
bmjopen-2016-013916supp003.pdf (207.7KB, pdf)
Participation rate
The total number of ICU staff in the 18 ICUs was 714. Therefore, 714 three-leaflet questionnaires were delivered (221 to physicians, 493 to nurses), and 469 of them were completed and collected back (149 by physicians and 320 by nurses). The response rate was 67.4% for the medical staff and 64.9% for the nursing staff.
Sociodemographic characteristics and job description
Table 1 summarises the sociodemographic and job characteristics of both medical and nursing staff members participating in the study. According to our data the majority of the nursing staff was female and significantly younger than the medical staff. Interestingly, 60.4% of the doctors and 55.1% of the nurses declared that they had an experience of losing a close family member. The majority of ICU staff (67.2%) had a working experience of >5 years. The nursing staff was less satisfied with their job compared with the medical staff; however, >60% of both groups was highly satisfied with their job.
Table 1.
Baseline participant characteristics*
| Variables | Physicians n=149 | Nurses n=320 | p Value† |
| Male gender | 63 (44.4%) | 58 (19.2%) | <0.001 |
| Age (years) | <0.001 | ||
| 20–30 | 2 (1.3%) | 47 (14.8%) | |
| 30–40 | 46 (30.9%) | 152 (47.8%) | |
| 40–50 | 71 (47.7%) | 113 (35.5%) | |
| >50 | 30 (20.1%) | 6 (1.9%) | |
| Personal experience of losing a close family member | 90 (60.4%) | 172 (55.1%) | NS |
| Working experience (years) | <0.001 | ||
| <2 | 42 (28.2%) | 39 (12.4%) | |
| 2–5 | 13 (8.7%) | 58 (18.4) | |
| 5–10 | 28 (18.8%) | 89 (28.3%) | |
| 10–15 | 32 (21.5%) | 77 (24.4%) | |
| >15 | 34 (22.8%) | 52 (16.5%) | |
| Job title | NA | ||
| ICU medical director | 23 (15.4%) | NA*** | |
| Senior ICU physician | 45 (30.2%) | NA | |
| Fellow physician | 26 (17.4%) | NA | |
| Resident | 44 (29.5%) | NA | |
| Head nurse | NA | 34 (10.6%) | |
| Nurse | NA | 227 (70.9%) | |
| Assistant nurse | NA | 48 (15.0%) | |
| Physiotherapist | NA | 9 (2.8%) | |
| Hospital type | 0.031 | ||
| University | 82 (55.0%) | 142 (44.4%) | |
| General | 67 (45.0%) | 178 (55.6%) | |
| Job satisfaction | 0.001 | ||
| Low | 3 (2.1%) | 22 (6.9%) | |
| Moderate | 25 (17.1%) | 95 (29.7%) | |
| High | 118 (80.8%) | 203 (63.4%) |
*Table entries represent numbers with related percentages (n, %).
†Statistical comparisons were performed with Χ2 test of independence between two categorical variables (one dichotomous ‘physician/nurse’ and the second with two or more groups, respectively).
ICU, intensive care unit; NA, not applicable; NS, non-significant.
Opinions and common practices about EoL
Table 2 summarises the set of specific questions regarding the opinion of ICU staff about EoL decisions and their application in clinical practice. Interestingly, 93.9% of the doctors and 83.7% of the nurses declared that they had a former experience in EoL decision-making during their professional career and that prior experience with dying patients had influenced their attitude towards EoL (67.1% and 47.3%, respectively); 48.6% of the medical staff and 37.2% of the nursing staff stated that EoL discussion was useful, and 84.9% of the doctors and 65.0% of the nurses said it was indispensable, although a small percentage (7.5%) of nurses considered EoL discussions and decisions dangerous, criminal or illegal. In addition, 89 doctors and 205 nurses agreed with the application of a progressive scale of withholding life-sustaining treatment, starting from the more invasive and expensive therapies (table 2). Finally, >75% in both groups suggested that all discussions about ethical issues taking place in the ICU should be performed with greater caution or in a different way. Concerning the ICU commitment to high ethical standards, 75.7% of ICU physicians and 57.1% of the nursing staff (p<0.001) stated that their ICU was committed to high ethical standards and both declared that this commitment implicated the nursing staff as well.
Table 2.
Physician and nurse attitudes towards specific end-of-life questions
| Regarding end-of-life questions, participants stated: | Physicians (n=149) |
Nurses (n=320) |
p Values* |
| Satisfaction with current DFLST | 79 (53.4%) | 109 (34.6%) | 0.011 |
| ICU commitment to high ethical standards | 112 (75.7%) | 180 (57.1%) | 0.001 |
| This commitment involves the nursing staff | 89 (80.2%) | 134 (74.9%) | NS |
| The decision to limit treatment is: (more than one answer) |
|||
| indispensable | 124 (84.9%) | 208 (65.0%) | <0.001 |
| useful | 71 (48.6%) | 119 (37.2%) | 0.020 |
| dangerous, criminal or illegal | 2 (1.4%) | 24 (7.5%) | 0.047 |
| DFLSTs are taken by all the physicians as a group without the nursing staff | 113 (75.8%) | 257 (80.3%) | NS |
| DFLSTs should ideally be taken collaboratively by the nursing staff and physicians | 96 (64.4%) | 176 (55.5%) | NS |
| The family should be informed about DFLST | 99 (66.9%) | 257 (81.1%) | <0.001 |
| The family should not be properly informed because of its inability to understand the medical details | 77 (77.8%) | 118 (73.8%) | NS |
| The family is actually informed about DFLST | 26 (17.7%) | 62 (19.9%) | NS |
| The main reason that the families are not fully informed is fear of litigation | 25 (17.4%) | 46 (14.9%) | NS |
| When you make a DFLST, you worry that this might lead to litigation | 80 (54.4%) | NA | NA |
| Withholding tracheal intubation can be considered if the patient will not benefit from intubation | 112 (75.2%) | 214 (67.5%) | NS |
| Extubation can be considered because intubation prolongs the dying process unnecessarily | 42 (28.4%) | 74 (23.2%) | NS |
| Decreasing the FiO2 is different from extubating | 113 (75.8%) | 229 (71.6%) | NS |
| Withdrawal of artificial ventilation represents a different approach from withdrawing other treatments (breath=life) | 76 (51.4%) | 198 (63.5%) | 0.004 |
| Withholding or withdrawal of inotropic medications can be considered because inotropic medications prolong the dying process unnecessarily | 122 (81.9%) | 209 (65.3%) | <0.001 |
| In favour of using a scale for gradual treatment limitation, recorded clearly in the patient’s medical record† | 89 (68.5%) | 205 (84.4%) | <0.001 |
| Increasing sedation is limited because it can hasten death | 14 (9.5%) | 66 (20.8%) | <0.001 |
| The appropriate term is ‘refusal of futile care’ instead of ‘passive euthanasia’ | 104 (71.7%) | 140 (44.7%) | <0.001 |
| Personal experience with dying patients has influenced your approach | 100 (67.1%) | 149 (47.3%) | 0.002 |
| Discussions about ethics in the ICU should be given more attention or should be approached in a different way | 110 (74.8%) | 254 (80.4%) | NS |
*Statistical comparisons were performed with χ2 test for categorical variables.
†A substantial percentage of participants (19.6%) declined to express an opinion in this question. Statistical analysis was performed between participants who gave a ‘yes’ or ‘no’ answer.
DFLST, decisions to forego life sustaining treatments; FiO2, fraction of inspired oxygen; ICU, intensive care unit; NS, non-significant.
Communication with the family and fear of litigation
A statistically higher percentage of nurses compared with the doctors (81.1% vs 66.9%, respectively, p<0.001) believed that the family should be informed about DFLST. However, if they were opposed to disclosing such information, the main reason would be that the family was unable to understand and manage all the EoL medical details (stated by 77.8% of the doctors and 73.8% of the nurses who believed that the family should not be properly informed about DFLST). Additionally, 17.4% of the doctors acknowledged the fear of legal consequences as a reason for non-disclosure of such information to the family; 47.5% of the physicians who worried about legal consequences stated that this concern influenced the information given to the patient, 81.3% stated this concern influenced the information given to the family, 38.8% stated this concern influenced the information given to the nursing staff, and 60% stated this concern influenced the information recorded in medical files. Finally, 54.4% of ICU physicians expressed concerns about possible litigation induced by EoL decision-making, while 4.8% was unwilling to answer or expressed no opinion. Both doctors (52.3%) and nurses (56.1%) denied the nursing staff’s involvement in a case of litigation for DFLSTs.
EPQ and SpREUK questionnaires and their relationship with participant baseline characteristics and attitudes towards DFLSTs
Table 3 summarises the results of the participants’ aspects of personality and religous beliefs (‘religiousness’) scores. Female gender and nursing job were found to be positively and independently associated with neuroticism, religiousness and trust. All other baseline variables did not reach statistical significance.
Table 3.
Personality and religiousness participant scores*
| Aspects/dimensions | Total (n=469) |
Physicians (n=149) |
Nurses (n=320) |
p Values | Males (n=121) |
Females (n=323) |
p Values |
| Personality | |||||||
| Neuroticism | 10 (7–13) | 9 (6–12) | 10 (7–14) | 0.039 | 9 (5–12) | 10 (7–14) | <0.001 |
| Psychoticism | 3 (2–5) | 3 (2–4) | 3 (2–5) | NS† | 4 (2–6) | 3 (2–5) | 0.009 |
| Extraversion | 15 (12–17) | 15 (11–17) | 15 (12–17) | NS | 15 (11–17) | 15 (12–17) | NS |
| Religiousness/spirituality | |||||||
| Total score | 39 (30–48) | 37 (25.5–46.5) | 39 (32–48) | 0.023 | 34.5 (25–42) | 40 (33–48) | <0.001 |
| Search for support | 11 (8–16) | 11 (7–16) | 11 (8–15) | NS | 10.5 (7–16) | 11 (8–16) | 0.029 |
| Trust in higher guidance | 13 (10–16) | 12 (7–15.5) | 13 (11–16) | 0.004 | 11 (7–15) | 13 (11–16) | <0.001 |
| Reflection | 15 (11–18) | 14 (9–17) | 15 (11–18) | 0.023 | 12 (9–16) | 15 (12–18) | <0.001 |
*Table entries represent medians with 25th–75th interquartile ranges, along with their p values of statistical comparisons between groups performed with Mann-Whitney U test for non-parametrical continuous variables.
NS, non-significant.
Table 4 summarises the relationship between aspects of personality and religiousness with specific DFLSTs. Specifically, a total of 84 ICU staff members preferred the term ‘passive euthanasia’ over 244 who opted for ‘futile care’. Multivariate logistic regression analysis demonstrated that the two independent predicting factors for using the term passive euthanasia was to be a nurse (OR 4.41, p<0.001) and to have high scores of neuroticism (OR 1.59, p=0.048). Concerning the question of whether withdrawal of artificial ventilation is a different approach from withdrawing other treatments, being a nurse and having a high score of intrinsic religiousness (trust) were the independent predicting factors for positive answers. Finally, we found that the factors associated with fear of legal consequences as a reason for not informing the family properly about DFLSTs were: work experience in the ICU for <10 years, working in a university hospital, and having a high score on psychotisicm.
Table 4.
Logistic regression analysis of factors predicting specific end-of-life attitudes
|
Variables* |
Univariate analysis | Multivariate analysis | |||||
| OR | 95% CI | p Values | OR | 95% CI | p Values | ||
| Preference of term ‘passive euthanasia’ over ‘refusal of futile care’ | Gender: female | 1.24 | 0.70 to 2.22 | NS | |||
| Age <40 years | 1.60 | 0.97 to 2.64 | NS | ||||
| Nurses | 4.93 | 2.49 to 9.76 | <0.001 | 4.41 | 2.21 to 8.82 | <0.001 | |
| Working <10 years | 1.07 | 0.65 to 1.77 | NS | ||||
| University hospital | 0.67 | 0.41 to 1.10 | NS | ||||
| Personal loss | 1.10 | 0.66 to 1.82 | NS | ||||
| Job satisfaction | 0.49 | 0.29 to 0.83 | 0.008 | 0.65 | 0.38 to 1.13 | NS | |
| Neuroticism | 1.74 | 1.04 to 2.89 | 0.033 | 1.59 | 1.03 to 2.72 | 0.048 | |
| Psychoticism | 1.65 | 0.94 to 2.91 | NS | ||||
| Extraversion | 0.62 | 0.38 to 1.03 | NS | ||||
| Spirituality | 1.11 | 0.67 to 1.84 | NS | ||||
| Support | 1.11 | 0.67 to 1.85 | NS | ||||
| Trust | 1.15 | 0.70 to 1.92 | NS | ||||
| Reflection | 1.46 | 0.88 to 2.42 | NS | ||||
| Positive attitude towards withdrawal of artificial ventilation when EoL decision is made versus denial to withdraw | Gender: female | 1.43 | 0.92 to 2.24 | NS | |||
| Age <40 years | 1.69 | 1.14 to 2.50 | 0.009 | ||||
| Nurses | 1.83 | 1.21 to 2.76 | 0.004 | 1.78 | 1.17 to 2.71 | 0.007 | |
| Working < 10 years | 0.94 | 0.63 to 1.40 | NS | ||||
| University hospital | 1.46 | 0.99 to 2.17 | NS | ||||
| Personal loss | 0.92 | 0.62 to 1.37 | NS | ||||
| Job satisfaction | 0.71 | 0.46 to 1.11 | NS | ||||
| Neuroticism | 0.87 | 0.59 to 1.29 | NS | ||||
| Psychoticism | 0.88 | 0.58 to 1.34 | NS | ||||
| Extraversion | 0.93 | 0.63 to 1.38 | NS | ||||
| Spirituality | 1.37 | 0.92 to 2.05 | NS | ||||
| Support | 1.18 | 0.79 to 1.76 | NS | ||||
| Trust | 1.69 | 1.14 to 2.52 | 0.010 | 1.60 | 1.07 to 2.39 | 0.023 | |
| Reflection | 1.24 | 0.84 to 1.84 | NS | ||||
| Fear of legal consequences when withholding DFLST information from the family versus all other reasons |
Gender: female | 0.64 | 0.37 to 1.11 | NS | |||
| Age <40 years | 1.06 | 0.63 to 1.76 | NS | ||||
| Nurses | 0.85 | 0.50 to 1.45 | NS | ||||
| Working <10 years | 1.81 | 1.05 to 3.12 | 0.031 | 1.96 | 1.12 to 3.45 | 0.014 | |
| University hospital | 2.41 | 1.42 to 4.10 | 0.001 | 2.41 | 1.38 to 4.20 | 0.002 | |
| Personal loss | 1.24 | 0.75 to 2.07 | NS | ||||
| Job satisfaction | 1.08 | 0.62 to 1.89 | NS | ||||
| Neuroticism | 1.00 | 0.60 to 1.66 | NS | ||||
| Psychoticism | 2.46 | 1.30 to 4.65 | 0.006 | 2.45 | 1.25 to 4.80 | 0.009 | |
| Extraversion | 1.16 | 0.69 to 1.94 | NS | ||||
| Spirituality | 0.71 | 0.43 to 1.19 | NS | ||||
| Support | 0.51 | 0.31 to 0.86 | 0.012 | 0.60 | 0.35 to 1.02 | NS | |
| Trust | 0.72 | 0.43 to 1.20 | NS | ||||
| Reflection | 1.00 | 0.60 to 1.67 | NS | ||||
*Continuous variables of ‘Neuroticism’, ‘Psychoticism’, ‘Extraversion’, ‘Spirituality’, ‘Support’, ‘Trust’ and ‘Reflexion’ were dichotomised using their total medians (table 3) as cut-off limits.
DFLST, decisions to forego life-sustaining treatment; EoL, end-of-life.
Discussion
Our findings show that there are discrepancies between doctors and nurses concerning EoL issues in the ICU. Both groups agreed that the family should be informed about the EoL decisions; however, they do not disclose such information to the families because the latter would not be able to understand the medical details, and because of fear of litigation. Moreover, we found that personality and religious characteristics influence the EoL issues. There are few studies probing the influence of religious orientation and personality on DFLST. Moreover, in these studies the participants were non-ICU professionals.13 Our study on this subject concerns the majority of ICU staff members at a national level with a higher participation rate compared with other studies,14 18 suggesting that our first national survey about DFLSTs was highly expected by the Greek ICU personnel and that they were very interested in the ethical aspects on DFLSTs.
Concerning our results from the survey questionnaire, some differences are notable when compared with previous studies.14 19 20 These differences are expected as the DFLST attitudes in the ICU evolve over time together with the ICU patient population, who, unlike many years ago, are not always admitted with a single condition but have multiple age-related comorbidities.8 In our study, 53.4% of the doctors but only 34.6% of the nurses were satisfied with the way DFLST was practised in their ICU, although they recognised its absolute necessity. The main obstacle to DFLST is uncertainty.8 21 It is extremely difficult to define a patient's prognosis, and prognostic uncertainty is the main reason for perceived inappropriate care among physicians.22 Murray et al observed that physicians modify the ICU monitoring and treatment when they are provided with a prediction of a patient's outcome, thus making DFLST a self-fulfilling prophecy.23 Moreover, DFLSTs are different between private and ICU doctors,24 among ICU doctors in the same ICU,11 between the referring physician and senior ICU doctors,22 even among physicians with the same ethnic origin but practising in different countries.25 Not all patients to whom DFLST is applied actually die. In the recent study by Lautrette et al 21 involving 1290 ICU patients for whom DFLST was decided, 56% were afforded no escalation of treatment, 19% had treatment withheld and, disturbingly, 4% who had treatment withdrawn were discharged alive from the hospital. Additionally, in previous studies, survival rates after DFLST were reported to range from 0–31%.20 26 27
A clear paternalistic pattern is noticed in our study concerning the participation of the family in DFLST; 71.5% of the doctors and 68.6% of the nurses declared that the family was not properly informed or involved in DFLST because they were not able to understand the medical details. The above results are in contrast with data on family participation in DFLST reported in French,14 Spanish,19 and English and South African studies.20 In these studies, the family participation in DFLST was 61%, 72% and almost 100%, respectively. On the other hand, Azoulay and colleagues in a multicentre study identified that only 47% of the family members of ICU patients want to participate in the decision-making process.28 Another study questions the capacity of the family to take part in decision-making as they suffered from anxiety and depression.29 Concerning the attitude of the nurses against specific DFLST questions, multivariate analysis revealed that nurses are more prone to use the term passive euthanasia over futile care (OR 4.41, 95% CI 2.21 to 8.82) and to deny withdrawal of artificial ventilation (OR 1.78, 95% CI 1.17 to 2.71). These findings make sense, together with the high score of neuroticism and intrinsic religiousness–trust recorded in this group of participants, and indicate that DFLSTs are badly perceived by ICU staff in the sense that breath = life, thus they are performing passive euthanasia in their patients.
Fear of legal consequences was expressed by 54.4% of the doctors; in 47% of them, this fear led to non-disclosure of information to the family (81.3%), non-disclosure of information to the nurses (38.8%), and not recording the DFSLT in the medical files (60%). Interestingly multivariate regression analysis demonstrated that being a young doctor and working in a university hospital are independent factors for withholding information about DFLST from the family information for fear of litigation. Fear of litigation is reported by almost 50% of Brazilian doctors,30 23% of French physicians,14 and 19% of US physicians.31 Interestingly, there are data suggesting that the more educated we become on ethical aspects, by attending EoL classes or reading at least four articles per year on EoL, the more likely we are to acquire communication skills and to involve family and nurses in the EoL process.30 Unfortunately, education in medical and nursing schools in Greece, as in many other countries, is focused on curative care and there is no training in palliative care, or teaching on ethics and communication skills.
Personality is defined as distinctive and relatively enduring ways of thinking, feeling and acting. Eysenck developed a very influential model of personality.17 We used this questionnaire—although cumbersome and possibly outdated on personality traits taxonomy—because it is validated in Greek.32 Based on the results of factor analyses of responses on personality questionnaires, Eysenck identified three dimensions of personality: extraversion, neuroticism and psychoticism. According to our results, nurses and females scored higher on neuroticism compared with physicians and males (p<0.05 and <0.001, respectively), while a higher score for psychoticism was found in males. We can postulate that there is a bias concerning these differences in the psychological profile between doctors and nurses because there is a predominance of females in our sample (80% among nurses and 55.6% among physicians). However, these two categorical variables were independently related to neuroticism. Concerning the relationship between the personality profile and the attitude against DFLST, ICU professionals with high scores on neuroticism prefer the term passive euthanasia over futile care, and professionals with psychoticism withhold information from the family for fear of litigation.
Religion is different from spirituality, spirituality being a broader concept in that it is compatible with all forms of religious beliefs and even the rejection of religion.7 As previously stated, although the questionnaire is suitable for healthcare research, it has never been used in ICU staff members who, undoubtedly, share the same questions as their patients about life, the meaning of life, and death. Moreover, ICU staff members are in permanent contact with terminally ill patients and are thus engaging in the search for the meaning of suffering and for motivation that allows them to cope with the necessities of their profession.33 Although we are aware of its limitations, we used this particular questionnaire in the absence of another better option.
Greeks are exclusively Christian Orthodox, as were all the physicians and nurses in our study. We were interested to see if religion or Christian Orthodox spirituality played a role in the EoL decisions. It is already known that people of the Greek Orthodox faith prefer to withhold therapy rather than withdraw it, as compared with the preference of Catholics and Protestants.3 10 In our study, we found that nurses are more religious compared with doctors, females versus males. Interestingly, the more religious we are, the more we are reluctant to withdraw mechanical ventilation. A strong negative attitude between intrinsic religiosity and withdrawal of therapy was also found, using a different religiosity questionnaire, in Iranian students of Muslim faith.13
It is already well reported that DFLST and death in the ICU impose a significant emotional burden on healthcare professionals.18 We found in our study that personality and religious traits may interfere with decision-making in regard to specific DFLSTs, leading to collaborative issues between persons with different personality and religious traits—which may obstruct the teamwork in the ICU and increase the emotional burden and burnout among ICU personnel. Unfortunately, we cannot easily change our personality and religious traits; however, by improving the communication between ICU professionals, involving the nursing staff in the DFLSTs, and discussing on a regular basis the ethical dilemmas we face every day in the ICU, we can improve the feeling of good care and reduce job strain.34
Concerning the results of our study, there may be some methodological issues such as representation bias. We believe that if this bias exists in our study it is small because the majority of the Greek ICUs participated in the study and the participation rate was very satisfactory. However, despite this participation rate, we ignored the opinion of the 34.3% who declined to participate in the survey. This percentage may have a positive or a negative opinion in regard to DFLST. The reasons for the non-participation in the survey may be fear relating to the need for anonymity, or fear of legal consequences given the fact that the Greek legislation is not clear on the subject and that there is a complete lack of recommendations and support from the relevant scientific societies and official bodies. Another weakness of our study is that we compared the results of our questionnaire on EoL decisions with data recorded more than 15 years ago.14 19 22 The data from these studies have not so far been actualised by new studies, thus making it impossible to draw safe comparisons between the actual Greek attitudes and what is now happening in other countries. However, our results from the main questionnaire are not so very different from the results already reported by other European countries; we therefore have no reason to believe that major changes have not been undertaken in the healthcare systems of these other countries and that their working conditions have not improved dramatically.
Conclusion
According to our study, major differences were found between doctors and nurses in their responses to several questions regarding current practices on DFLST. High levels of fear of litigation, perceived by the ICU doctors, strongly interact with certain DFLST attitudes and impedes the provision of honest information to the families and the medical records. Moreover, it seems that personality and religious characteristics of the ICU personnel influence their attitudes against certain, indeed very critical, DFLSTs. Personality and religious characteristics may affect the collaborative work and may induce dissatisfaction and conflicts between the ICU personnel. There is an urgent need for solid recommendations and support from the relevant scientific societies and official bodies concerning DFLSTs, and the implementation in all ICUs of an ethical course is an absolute necessity. More studies and more specific questionnaires are necessary to confirm our data and to enlighten the relationship between DFLSTs, spirituality and personal characteristics.
Supplementary Material
Acknowledgments
The authors acknowledge Dr Martin Tobin for his editorial assistance and the following medical directors, nurses and head nurses for their invaluable help in this study: Alexandroupolis University Hospital: Pneumatikos I, MD, Gogotsi CH, RN; Kavala General Hospital: Nagi E, MD, Koutsouki S, RN; Ippokratio General Hospital, Thessaloniki: Gerogiani N, MD, Tsokaridou E, RN; Papanikolaou General Hospital, Thessaloniki, ICU A: Bitzani M, MD, Hatzika K, RN; Papanikolaou General Hospital Thessaloniki, ICU B: Kapravelos N, MD, Kiromiti A, RN; ΑHΕPΑ University Hospital Thessaloniki: Skourtis CH, MD, Rizopoulos R, RN; Genimatas General Hospital Thessaloniki: Antoniadou E, MD, Kelesidou S, RN; Ag. Paulos General Hospital Thessaloniki: Dioritou OU, MD, Armeni P, RN; Heraklion University Hospital: Georgopoulos D, MD, Xirouxaki N, MD; Larissa University Hospital: Zakinthinos E, MD, Tzalera V, RN; GenikoKratikoNikaias Athens: Mavromatis A, MD, Pontikaki I, RN; Tzanio General Hospital Athens: Prekates A, MD, Laspiti I, RN; ΑΤΤΙΚΟ University Hospital Athens: Armaganidis A, MD, Politis S, RN; 251 Air Forces General Hospital Athens: Anthopoulos G, MD; Evangelismos University Hospital Athens: Zakinthinos S, MD, Mendi F, RN; Arta General Hospital: Lagos N, MD, Christou E, RN; Ioannina University Hospital: Zylis G, MD, Naoum K, RN; 401 Army Hospital Athens: Sourlas S, MD, Iliopoulou K, RN.
Footnotes
Contributors: VK, DM, AN, MG, MG, GN were responsible for the study design and conception.Data acquisition, analysis and interpretation were performed by AN, SS, KM, DM, VK and MG, DM, SS and AN had full access to all data of the study and take responsibility for the integrity of the data and accuracy of the data analysis. Manuscript writing: DM, SS, AN.
Competing interests: None declared.
Patient consent: The participation in the study was not compulsory but voluntary.
Ethics approval: The study protocol was approved by the national health authority (Protocol No Δ3β/23441) and the ethics committees of all participating hospitals were informed of the study by the national authority.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: All data from the study are available to anyone who may have an interest in the research, by email from the correspondent author.
References
- 1. Illich I. Medical nemesis: the expropriation of health. New York: Pantheon Books Random House, 1976. [Google Scholar]
- 2. Clark D. Between hope and acceptance: the medicalisation of dying. BMJ 2002;324:905–7. 10.1136/bmj.324.7342.905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sprung CL, Cohen SL, Sjokvist P, et al. End-of-life practices in European intensive care units: the Ethicus Study. JAMA 2003;290:790–7. 10.1001/jama.290.6.790 [DOI] [PubMed] [Google Scholar]
- 4. Carlet J, Thijs LG, Antonelli M, et al. Challenges in end-of-life care in the ICU: statement of the 5th International Consensus Conference in Critical care. Intensive Care Med 2004;34:770–84. [DOI] [PubMed] [Google Scholar]
- 5. Cook D, Rocker G. Dying with dignity in the intensive care unit. N Engl J Med 2014;370:2506–14. 10.1056/NEJMra1208795 [DOI] [PubMed] [Google Scholar]
- 6. Büssing A, Ostermann T, Matthiessen PF, et al. Role of religion and spirituality in medical patients: confirmatory results with the SpREUK questionnaire. Health Qual Life Outcomes 2005;3:1–10. 10.1186/1477-7525-3-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sulmasy DP. Spirituality, religion, and clinical care. Chest 2009;135:1634–42. 10.1378/chest.08-2241 [DOI] [PubMed] [Google Scholar]
- 8. STROBE statement: strengthening the Reporting of observational studies in Epidemiology. International Committee of Medical Journal Editors. 2009. http://www.strobe-statement.org (accessed 30 Mar 2016).
- 9. Hillman KM, Cardona-Morrell M. The ten barriers to appropriate management of patients at the end of their life. Intensive Care Med 2015;41:1700–2. 10.1007/s00134-015-3712-6 [DOI] [PubMed] [Google Scholar]
- 10. Sprung CL, Maia P, Bulow HH, et al. The importance of religious affiliation and culture on end-of-life decisions in European intensive care units. Intensive Care Med 2007;33:1732–9. 10.1007/s00134-007-0693-0 [DOI] [PubMed] [Google Scholar]
- 11. Cook DJ, Guyatt GH, Jaeschke R, et al. Determinants in Canadian health care workers of the decision to withdraw life support from the critically ill. Canadian Critical Care Trials Group. JAMA 1995;273:703–7. 10.1001/jama.1995.03520330033033 [DOI] [PubMed] [Google Scholar]
- 12. Mebane EW, Oman RF, Kroonen LT, et al. The influence of physician race, age, and gender on physician attitudes toward advance care directives and preferences for end-of-life decision-making. J Am Geriatr Soc 1999;47:579–91. 10.1111/j.1532-5415.1999.tb02573.x [DOI] [PubMed] [Google Scholar]
- 13. Aghababaei N, wasserman JA. Attitude toward euthanasia scale: psychometric properties and relations with religious orientation, personality and life satisfaction. Am J Hospice Palliative Med 2013;30:781–5. [DOI] [PubMed] [Google Scholar]
- 14. Ferrand E, Lemaire F, Regnier B, et al. Discrepancies between perceptions by physicians and nursing staff of intensive care unit end-of-life decisions. Am J Respir Crit Care Med 2003;167:1310–5. 10.1164/rccm.200207-752OC [DOI] [PubMed] [Google Scholar]
- 15. Brislin RW. Back-translation for cross-cultural research. J Cross Cult Psychol 1970;1:185–216. 10.1177/135910457000100301 [DOI] [Google Scholar]
- 16. McDermott MA, Palchanes K. A literature review of the critical elements in translation theory. Image J Nurs Sch 1994;26:113–8. 10.1111/j.1547-5069.1994.tb00928.x [DOI] [PubMed] [Google Scholar]
- 17. Eysenck H, Eysenck SBG. Manual of the Eysenck personality questionnaire (EPQ). London, UK: Hodder and Stoughton Educational, 1975. [Google Scholar]
- 18. Mealer ML, Shelton A, Berg B, et al. Increased prevalence of post-traumatic stress disorder symptoms in critical care nurses. Am J Respir Crit Care Med 2007;175:693–7. 10.1164/rccm.200606-735OC [DOI] [PubMed] [Google Scholar]
- 19. Esteban A, Gordo F, Solsona JF, et al. Withdrawing and withholding life support in the intensive care unit: a Spanish prospective multi-centre observational study. Intensive Care Med 2001;27:1744–9. 10.1007/s00134-001-1111-7 [DOI] [PubMed] [Google Scholar]
- 20. Turner JS, Michell WL, Morgan CJ, et al. Limitation of life support: frequency and practice in a London and a Cape Town intensive care unit. Intensive Care Med 1996;22:1020–5. 10.1007/BF01699222 [DOI] [PubMed] [Google Scholar]
- 21. Lautrette A, Garrouste-Orgeas M, Bertrand PM, et al. Respective impact of no escalation of treatment, withholding and withdrawal of life-sustaining treatment on ICU patients' prognosis: a multicenter study of the Outcomerea Research Group. Intensive Care Med 2015;41:1763–72. 10.1007/s00134-015-3944-5 [DOI] [PubMed] [Google Scholar]
- 22. Piers RD, Azoulay E, Ricou B, et al. Inapropriate care in European ICUs: confronting views from nurses and junior and senior physicians. Chest 2014;146:267–75. 10.1378/chest.14-0256 [DOI] [PubMed] [Google Scholar]
- 23. Murray LS, Teasdale GM, Murray GD, et al. Does prediction of outcome alter patient management? Lancet 1993;341:1487–91. 10.1016/0140-6736(93)90631-P [DOI] [PubMed] [Google Scholar]
- 24. Kollef MH. Private attending physician status and the withdrawal of life-sustaining interventions in a medical intensive care unit population. Crit Care Med 1996;24:968–75. 10.1097/00003246-199606000-00016 [DOI] [PubMed] [Google Scholar]
- 25. Asai A, Fukuhara S, Lo B. Attitudes of Japanese and Japanese-American physicians towards life-sustaining treatment. Lancet 1995;346:356–9. 10.1016/S0140-6736(95)92230-X [DOI] [PubMed] [Google Scholar]
- 26. Melltorp G, Nilstun T. Decisions to forego life-sustaining treatment and the duty of documentation. Intensive Care Med 1996;22:1015–9. 10.1007/BF01699221 [DOI] [PubMed] [Google Scholar]
- 27. Wood GG, Martin E. Withholding and withdrawing life-sustaining therapy in a Canadian intensive care unit. Can J Anaesth 1995;42:186–91. 10.1007/BF03010673 [DOI] [PubMed] [Google Scholar]
- 28. Azoulay E, Pochard F, Chevret S, et al. Half the family members of intensive care unit patients do not want to share in the decision-making process: a study in 78 French intensive care units. Crit Care Med 2004;32:1832–8. 10.1097/01.CCM.0000139693.88931.59 [DOI] [PubMed] [Google Scholar]
- 29. Pochard F, Azoulay E, Chevret S, et al. Symptoms of anxiety and depression in family members of intensive care unit patients: ethical hypothesis regarding decision-making capacity. Crit Care Med 2001;29:1893–7. 10.1097/00003246-200110000-00007 [DOI] [PubMed] [Google Scholar]
- 30. Forte D, Vincent JL, Velasco I, et al. Association between education in EOL care and variability in EOL practice: a survey of ICU physicians. Intensive Care Med 2012;38:404–12. [DOI] [PubMed] [Google Scholar]
- 31. Asch AA, Hansen-Flaschen J, Lanken PN. Decisions to limit or continue life-sustaining treatment by critical care physicians in the United States: conflicts between physicians’ practices and patient wishes. Am J RespirCrit care Med 1995;151:288–92. [DOI] [PubMed] [Google Scholar]
- 32. Dimitriou E. EPQ Personality questionnaire. Greek validation in the Greek population. Engefalos 1986;23:41–54. [Google Scholar]
- 33. Gualdani S, Fegoli M. Spirituality in health care: the role of needs in critical care. Trends AnaestCrit Care 2014;4:175–7. [Google Scholar]
- 34. Jensen HI, Ammentrop J, Ording H. Withholding or withdrawing therapy in intensive care units: an analysis of collaboration among health care professionals. Intensive Care Med 2011;37:1696–705. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2016-013916supp001.pdf (258.5KB, pdf)
bmjopen-2016-013916supp002.pdf (247.7KB, pdf)
bmjopen-2016-013916supp003.pdf (207.7KB, pdf)


