Abstract
Background
The integrity of a mother-infant dyad is essential for the proper development of maternal behavior and infant growth/ development. At present, there is a lack of objective approaches to monitor mother-infant behavioral exchanges.
Objectives
This is an exploratory prospective study designed to evaluate the Mother-Infant Mutualistic Screening Scale (MIMSS), a novel observational tool focused on monitoring the mutual/ reciprocal sensitivity and responsiveness that mother and infant express toward one another's behaviors/ actions during the obligatory setting of daily meal times.
Methods
Mother-infant interactions were assessed from videotaped feeding sessions conducted under recurrent naturalistic observations. Data were collected from 27 mother-preterm infant singleton dyads at 6 and 12 month corrected age (CA). Four levels of MIMSS are defined: Level I - both mother and infant are not responsive (NR) to one another's actions; Level II - mother is not responsive (NR) to infant, but infant is responsive (R) to mother; Level III - mother is responsive (R) to infant, but infant is not responsive (NR) to mother; Level IV - both mother and infant are responsive (R) to one another.
Results
Inter- and intra-rater reliability between two raters was 93% and ≥ 85%, respectively. At 6 and 12 month CA, 78% and 81% of the dyads were at a MIMSS Level IV, respectively. A change in mother-infant reciprocal behavioral responses or MIMSS levels was observed in 9 of the dyads between these two ages. No association was observed between MIMSS levels and infant growth/ development as monitored by percentile Weight, Length, and Weight by Length at both corrected ages.
Conclusions
The MIMSS is easy to use with high inter- and intra-rater reliabilities. With the ability to differentiate between mother and infant reciprocal behavioral responses toward one another's actions, MIMSS can help health professionals assess the quality of mother-infant interactions and identify the partner(s) who may benefit from individualized assistance. Although MIMSS uses mealtime as a recurrent setting, it offers a conceptual frame work for evaluating co-regulatory processes under different contexts.
Keywords: Mother-Infant Interactive Behaviors, Preterm Infants, Oral feeding
Introduction
Supportive care giving involves sensitive and attuned dyadic interactions between mother and infant and is associated with maternal well being, caregivers' confidence, and beneficial infant developmental outcomes [1–4]. However, it is evident that such interactions are not always consistently harmonious or synchronized [5].
The task of feeding an infant does not only pertain to nutrition. It is also an opportunity for comforting, nurturing, and bonding between mother and infant. As such, the act of feeding plays an inherently important role in determining the collaborative and interactive processes of a mother-infant dyad [6,7]. As infants transition to solid food during their first year of life, mother and infant need to develop a continually changing mealtime “dialogue” to ensure stable interactive feeding sessions [7]. This is not only based on the introduction of new food (e.g., new tastes, textures), but is also essential for the infant's budding autonomy. Consequently, as feeding is a repetitive and mandatory task, the quality of mother-infant interactions is continually challenged [8].
Through our research and practice, we have observed that feeding problems often result from a mismatch between infants' cues and caregivers' subjective interpretations of these cues. The development of such relationships has been shown to impact infant nutrition and subsequent neurodevelopment, which has been particularly evident in the preterm infant cohort [9–11]. They also have less efficient self-regulatory strategies, increased difficulty soothing and regulating negative arousal, and demonstrate greater reactivity and sensitivity to distress [12–14]. Thus, mother-preterm infant dyads are at greater risk of developing suboptimal relationships when compared to mother-term infant counterparts. Such asynchronous exchanges may lead to long-term maternal stress, infant oral feeding disorders, and poor growth/development in addition to increased medical costs [15–20]. It is clear that infants, particularly those born prematurely, may not have attained the degree of neurophysiologic organization that would allow them “to partake in a temporally matched social dialogue” with their mother [21]. As such, the ‘day in-day out’ exchanges taking place during feeding sessions can engender a series of behavioral patterns that may become congenial/ fluid or erratic as mother and infant fall into the familiarity of routine exchanges. Forcada-Guex and colleagues distinguish the effects of two patterns of interactions on the developmental and behavioral outcomes of mother-infant dyads: a cooperative pattern, whereby mothers display a protective role, and a controlling pattern, whereby mothers display a risk-precipitating role. The former is commonly observed in mother-term infant dyads, while the latter is more prominent among mother-preterm infant dyads [22].
The repetitive and obligatory task of having to feed an infant daily offers an optimal setting to study the development of mother-infant relationships that eventually form within the mother-preterm infant dyad. The present study is based on the theoretical construct that the sustained and obligatory interchanges recurring during daily feeding sessions between mother and infant create a double feedback circuit that offers a unique opportunity to study the development of mother-infant interactions. It is hypothesized that for balanced exchanges of mutual benefit, such feedback would compel partners to continually “re-adjust” their actions towards one another as illustrated in the schematic in Figure 1.
Figure 1.
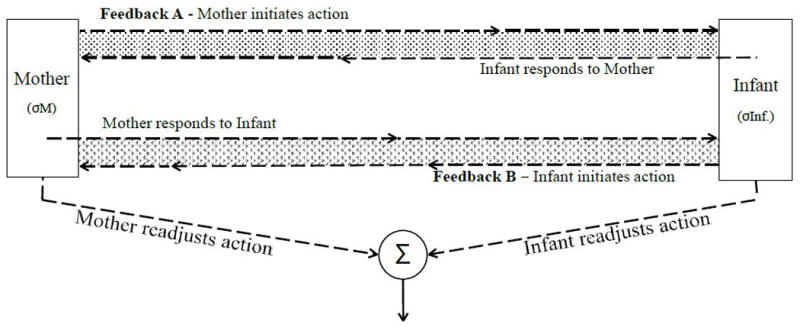
Schematic of a mother-infant double feedback circuit (Feedback A, B) representing mother- infant interactions with respective “error detectors” σ M and σ Inf. when co-exchanges are unbalanced. Error detectors (σ M and σ Inf.) will annul when the partners of the dyad re-adjust their behaviors/actions, thereby leading to a balanced and stable exchange (Σ).
Two possible feedback circuits may occur depending upon whether the partner initiating the action is the mother (Figure 1, Feedback A) or the infant (Figure 1, Feedback B). We further advance that the learning of such mutual responsiveness/ sensitivity early on in the relationship will safeguard the integrity of the mother-infant dyad. It is based on this working premise that the Mother-Infant Mutualistic Screening Scale (MIMSS) was developed to monitor the presence or absence of any response expressed by one partner (responder) towards the action/ behavioral changes of the other partner (initiator), irrespective of the quality of such responses. It is further hypothesized that such real-time monitoring in a routine meal time setting will help identify the fluidity of mother-infant interactions and may assist health professionals in identifying the partner(s) who may benefit from assistance in optimizing such co-exchanges.
Methods
MIMSS Scale
The MIMSS scale is an observational tool based on two working premises: 1) the degree of synchronicity between mother and infant interactions is a function of their respective immediate responsiveness to one another's actions. 2) Mothers, due to their maturity, are the active partners, i.e., the decision-makers who control the feeding, while infants, due to their immaturity, are the passive partners who cannot initiate volitional choices. However, depending upon the maturity level of their neuro-physiologic and/ or –motor development, infants will provide feedback when overwhelmed through “reflexive“ behaviors, e.g., arching, spitting, choking, “shutting down,” and/or physiologic adverse events, e.g., oxygen desaturation, apnea, bradycardia. With maturation, infants will demonstrate increasing volitional feedback or autonomy, e.g., fussing, pushing away.
The MIMSS considers four levels of interactions between partners, characterized simply by whether mother or infant are immediately responsive (R), i.e., within ≤ 5 sec, or not responsive (NR) to one another's positive or negative behavioral changes during a feeding session (Figure 2): Level I - both mother and infant are not responsive (NR) to one another's action/ behavior; Level II - mother is not responsive (NR) to infant, but infant is responsive (R) to mother; Level III - mother is responsive (R) to infant, but infant is not responsive (NR) to mother; Level IV – both mother and infant are responsive (R) to one another. As such, with MIMSS Levels I through III, mother-infant interactions would be deemed imbalanced, as opposed to Level IV where mother and infant mutually contribute to a balanced co-exchange (Figure 2).
Figure 2.
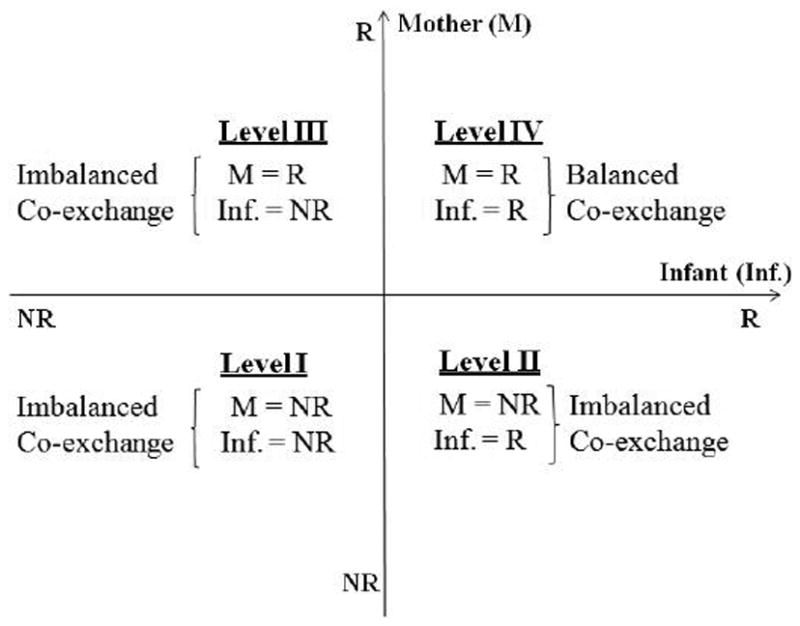
MIMSS is characterized by four levels of interactions between partners: Mother's (M) responsiveness (R) and non-responsiveness (NR) presented on the Y-Axis and infant's (Inf.) R and NR on the X-axis.
Participants
Twenty-seven mother-preterm infant dyads, with singletons born between 25 to 30 weeks gestational age (GA), participated in the study. The subjects were part of a larger long-term follow-up study conducted at Texas Children's Hospital (Houston TX) that monitored maternal stress and infants' growth/development during their stay in the neonatal intensive care unit (NICU) through 24 month corrected age (CA). The Baylor College of Medicine Institutional Review Board for Human Research approved the study, and mothers consented for their infant(s) and themselves prior to the study. Infants' exclusion criteria included gastrointestinal complications, congenital anomalies or chronic medical conditions, periventricular leukomalacia, necrotizing enterocolitis, and bronchopulmonary dysplasia. Inclusion criteria included only “feeders and growers”, defined as clinically stable infants whose hospital discharge were delayed due to their inability to attain independent oral feeding.
Study Design/Methodologies
Following their NICU discharge, mother-infant dyads returned at 6 and 12 month (± 2 weeks) corrected age (CA) to the General Clinical Research Center (GCRC) at the hospital for a videotaped mid-day meal, as this was when parents brought their infant to the GCRC. Parents were instructed to bring their infant's meal as infants were expected to be transitioning to purée and solids, respectively, around these two ages. Videotaping was conducted in a private room at the GCRC with a camera (Panasonic PV-Gs400 3-CCD) placed discreetly behind a door at an angle where both mother and infant's faces were visible while remaining minimally disruptive to the infant's attention. Mothers decided on how infants were fed, i.e., mother's lap or high chair, and determined when a feeding ended. In general, purée/ solids were offered prior to milk (bottle/ cup). Mothers were encouraged to interact with their infant as they would at home, e.g., talking, singing. The primary outcome measure was the MIMSS scoring. Infants' measures of growth/development included their percentile Weight, Length, and Weight by Length using the World Health Organization (WHO) growth curves [23].
The authors rated 54 videos scoring mothers and infants as responsive (R) or not responsive (NR) as per MIMSS's criteria. In order to attain a more complete perspective of the mealtime interactions, each minute of the first and last three minutes of a feeding session were scored, i.e., a total of six 1-minute scores/ subject. The overall MIMSS level for the entire feeding duration was based on the most frequent 1-minute MIMSS scores observed during these six minutes. Chi-square analysis was used to monitor infants' growth outcomes, i.e., percent (%) Weight, Length, and Weight by Length at 6 and 12 month CA. Regression analysis was used to assess potential correlations between MIMSS levels and infants' corresponding percent growth measures at these two ages. Significance was determined at p ≤ 0.05.
Results
Infants' characteristics at birth, 6 and 12 month corrected age (CA) and their Weight, Length, and Weight by Length percentile according to the WHO growth curves are presented in Tables 1A and 1B, respectively. Table 1B shows that there was a greater percentile of infants falling below 25% in % Weight at 12 month vs. 6 month CA (p < 0.006). However, no such difference was observed in the % Length and Weight by Length between these two ages.
Table 1A.
Infant characteristics (N = 27).
| GA (weeks) [range] | Gender % male (n) | Birth Weight (kg) [range] | 6 Month Weight (kg) [range] | 6 Month Length (cm) [range] | 12 Month Weight (kg) [range] | 12 Month Length (cm) [range] |
|---|---|---|---|---|---|---|
| 27.56 ±1.56* [24.29 – 30.29] |
63 (17) | 1.03 ± 0.22 [0.60 – 1.62] |
7.53 ± 1.26 [4.78 – 10.71] |
65.34 ± 3.35 [56.80 – 72.30] |
9.02 ± 1.37 [6.09 – 12.94] |
73.15 ±4.71 [62.20 – 81.30] |
mean ± SD
Table 1B.
Percentile of infants falling within each % WHO growth curve for Weight Length, and Weight by Length.
| WHO Growth Curve (%) | 6 Month % Weight (n) | 6 Month % Length (n) | 6 Month % W × L (n) | 12 Month % Weight (n) | 12 Month % Length (n) | 12 Month % W × L (n) |
|---|---|---|---|---|---|---|
| <25 | 25.9 (7)* | 44.4 (12) | 14.8 (4) | 66.7 (16)* | 41.7 (10) | 29.2 (7) |
| 25–50 | 40.7 (11) | 25.9 (7) | 22.2 (6) | 25.0 (6) | 29.2 (7) | 41.7 (10) |
| 51–75 | 18.5 (5) | 11.1 (3) | 25.9 (7) | - | 16.7 (4) | 12.5 (3) |
| >75 | 14.8 (4) | 18.5 (5) | 37.0 (10) | 8.3 (2) | 12.5 (3) | 16.7 (4) |
Between symbols χ2 p < 0.006
Maternal characteristics are shown in Table 2. Maternal age at the start of the study was 29.4 ± 6.6 years (mean ± SD), ranging between 15 to 41 years. Mothers identified their ethnicity as Caucasian (25.9%), African-American (25.9%), and Hispanic (48.1%). Of note, the majority (65.4%) of families' annual income were ≤ $50,000 and most mothers received some level of post high school education.
Table 2.
Maternal characteristics.
| Age (Range) | Ethnicity (%) | Annual Income (%) | Education (%) | |||
|---|---|---|---|---|---|---|
| 29.4 ± 6.6 Years | Caucasian | 25.9 | < $10,000 | 23.1 | Grade school | 11.5 |
| (15 – 41) | African-American | 25.9 | $10,000 -- $49,999 | 42.3 | Middle School | 7.7 |
| Hispanic | 48.1 | $50,000 -- $99,999 | 23.1 | High School | 19.2 | |
| > $100,000 | 11.5 | College | 50.0 | |||
| Post-Graduate | 11.5 | |||||
Inter- and intra-rater reliability between two raters was 93% and ≥ 85, respectively. Both observers rated 78% of the dyads (21/27) at a MIMSS Level IV at 6 month CA. Eighty one percent (22/27) attained a MIMSS Level IV at 12 month CA. Eighteen of the dyads demonstrated a MIMSS Level IV at both 6 and 12 month CA (67%). Nine of the 27 dyads (33%) demonstrated changes in MIMSS Levels between 6 and 12 month CA. Table 3 shows the respective partner(s) who changed their responsiveness towards the other between 6 and 12 month CA. The MIMSS levels of three of these nine dyads regressed due to mother and/or infant non-responsiveness to one another; whereas, the others showed improved responsiveness by mother or infant.
Table 3.
Dyads demonstrating different MIMSS scores at 6 and 12 months corrected age.
| Dyads (n) | MIMSS Level | Mothers | Infants |
|---|---|---|---|
| 4 | II to IV | Improved (NR → R) | No Change (R → R) |
| 2 | IV to II | Regressed (R → NR) | No Change (R → R) |
| 1 | III to IV | No change (R → R) | Improved (NR → R) |
| 1 | IV to I | Regressed (R → NR) | Regressed (R → NR) |
| 1 | I to II | No Change (NR → NR) | Improved (NR → R) |
No association was observed between MIMSS levels and infants' growth/development as monitored by their percent weight, length, or weight by length at 6 and12 month CA (p > 0.05).
Discussion
Symbiosis describes the three intimate associations existing between two dissimilar organisms with: 1) one partner benefiting, while the other is neither harmed or benefiting [commensalism]; 2) one partner benefiting, while the other is harmed [parasitism] and 3) both partners benefiting [mutualism] [24].
Based on the dissimilarity existing between the mature and immature organism represented by the mother and child, respectively, it has been proposed that the “living together” of mother and child can be defined as a symbiotic relationship where by both partners would strive to benefit [2,25]. However, such togetherness may only be productive if there is a “friendly and mutual recognition” of each partner's differences or characteristics [2]. One may speculate that the type of symbiotic relationship that evolves will determine the quality of mother-infant bonding that will ensue. If mother and infant respond in a positive manner to one another's actions, the synchronous bidirectional process would result in effective and beneficial co-exchanges. In turn, such co-exchanges ultimately would lead to both partners readily adapting their own behaviors to meet the other's needs, thereby reducing their respective levels of emotional and behavioral difficulties while strengthening their bond [19,26]. The beneficial nature of such reciprocal responses would encompass social and sensory cues, e.g., vocalization, olfaction (pheromones), and/or touch, whether expressed mutually or in isolation by mother or infant [27–29]. Accordingly, attainment of such fluid exchanges of information would enhance both partners' communication as well as cognitive and emotional development over the long term [30]. Behavioral patterns between mother and infant customarily develop as the dyad enters into routine relationships evolving as a function of mother-infant mutual sensibility towards one another. Unfavorable relationships that are not recognized may threaten the balance of the dyad and negatively impact maternal/infant behavior and infant growth and development, while increasing both partners' stress.
In monitoring mother's and infant's respective ability to continually “re-adjust” their actions towards one another, MIMSS offers a unique opportunity to differentiate between both partners' sensitivity towards one another's actions. Its simplicity is reflected by its high inter- and intra- rater reliability (93% and ≥ 85%, respectively). MIMSS also offers additional advantages: 1) its use over time offers a means to identify the partner(s) who have progressed or regressed; 2) its use is not only relevant to mothers and preterm infants, but also to mothers and their infants of any age, insofar as it is based solely on the presence/absence of partners' responsiveness towards one another's actions, regardless of circumstances and appropriateness of their responses. As such, it is advanced that MIMSS's conceptual framework allows for the longitudinal study of the development of mother-infant co-regulatory processes as their dyadic relationship evolves.
Our observations that the majority of our dyads (67%) maintained a MIMSS Level IV at 6 and 12 month CA, while others did not, is supported by the study of Van Dijk and colleagues. These authors noted that during feeding, “while the interaction behavior of some caretaker-infant dyads remains variable, others stabilize quickly [as a result of] a co-regulation process of consensual frames” [7]. Variability in dyadic interactions measured at any one time point needs to be carefully interpreted because additional maternal, infant, and/or environmental factors may be interfering, e.g., maternal stress, social support, infant's status and/or maturation, home environment. As such, the longitudinal MIMSS monitoring over time is recommended for the identification of an overall sustained pattern of maternal-infant exchanges.
The absence of association between MIMSS levels and infant's percentile weight, length, and weight by length at both ages' supports the view that infants' growth status, although important, is not a prime determinant of the quality of their interactions.
In brief, it is advanced that MIMSS's ability to detect mother and infant immediate responsiveness to one another's behaviors/ actions facilitates the monitoring of mother-infant relationships and bonding, and may help identify the partner(s) who may benefit from external support. Indeed, as we have observed, within each MIMSS level, developmental specialists could identify the initiator and the ability of the responder to re-balance their interactions. Although mothers, as the active partners, may bear more responsibility than their infants in upholding balanced dyadic exchanges, an infant may encounter neuro-physiologic/ motor issues hindering his/her interactions with mother.
Study Limitations
The limitations of this study lie in its small sample size derived from a single NICU site and its limited testing times. To extend MIMMS' potential outreach, its evaluation to a larger cohort across multiple NICUs and examiners would be needed. Additionally, as it was conducted only on infants at 6 and 12 month corrected age, it currently lacks reliability across meals and days for individual dyads. However, as MIMMS can be used at any time, its reliability under the above conditions can be verified by monitoring subjects at closer time intervals. This would have the advantage of further offering a more accurate profile of the evolution of mother-infant interactions during meal times could be obtained. Future studies conducted on mothers with high-risk and healthy infants will also further determine the outreach that MIMSS may have on different population of mother-infant dyads.
In summary, MIMSS is a novel objective and observational scale that can differentiate between the immediate reciprocal behavioral responsiveness of mother and infant during feeding. Its concept is not only relevant to mother and their healthy preterm infants, but germane to a broad spectrum of mother-infant dyads across development. As feeding is an obligatory repetitive task, feeding sessions provide an optimal opportunity to study mother-infant ‘forced’ interactive behaviors during routine tasks. MIMSS yielded high inter- and intra-rater reliability. With its simple ‘yes/no’ approach, it allows for a more unbiased/ objective evaluation of the subjects' interactions. Indeed, the rapid objective real-time assessment of the presence/ absence of any response(s) from mother/ infant eliminate the subjective interpretations that developmental specialists may have as to the quality of the observed responses.
Acknowledgments
The authors wish to thank the families who participated in this study and the support received from the National Institutes of Health (R01- HD 044469; MO1RR000188). The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of the National Institute of Infant Health and Human Development or the National Institutes of Health.
Abbreviations
- CA
Corrected Age
- GA
Gestational Age
- GCRC
General Clinical Research Center
- Inf
Infant
- MIMSS
Mother Infant Mutualistic Screening Scale
- M
Mother
- NICU
Neonatal Intensive Care Unit
- NR
Not Responsive
- R
Responsive
- WHO
World Health Organization
Footnotes
Conflict of Interest: There are no conflicts of interests to disclose.
References
- 1.Ainsworth MDS, Blehar MC, Waters E, Wall SN. Patterns of attachment: A psychological study of the Strange Situation. Classic Edition. New York & London: Psychology Press; 2015. [Google Scholar]
- 2.Dunbar F. Symbiosis of parent and child. Am J Orthopsychiatry. 1952;22(4):809–24. doi: 10.1111/j.1939-0025.1952.tb01984.x. [DOI] [PubMed] [Google Scholar]
- 3.Leavitt LA. Mothers' sensitivity to infant signals. Pediatrics. 1998;102(5 Suppl E):1247–9. [PubMed] [Google Scholar]
- 4.Evans T, Whittingham K, Boyd R. What helps the mother of a preterm infant become securely attached, responsive and well-adjusted? Infant Behav Dev. 2012;35(1):1–11. doi: 10.1016/j.infbeh.2011.10.002. [DOI] [PubMed] [Google Scholar]
- 5.Tronick EZ, Cohn JF. Infant-mother face-to-face interaction: age and gender differences in coordination and the occurrence of miscoordination. Child Dev. 1989;60(1):85–92. [PubMed] [Google Scholar]
- 6.Bergmeier H, Aksan N, McPhie S, Fuller-Tyszkiewicz M, Baur L, Milgrom J, et al. Mutually Responsive Orientation: A novel observational assessment of mother-child mealtime interactions. Appetite. 2016;105:400–9. doi: 10.1016/j.appet.2016.06.019. [DOI] [PubMed] [Google Scholar]
- 7.van Dijk M, Hunnius S, van Geert P. The dynamics of feeding during the introduction to solid food. Infant Behav Dev. 2012;35(2):226–39. doi: 10.1016/j.infbeh.2012.01.001. [DOI] [PubMed] [Google Scholar]
- 8.Biringen Z, Emde RN, Pipp-Siegel S. Dyssynchrony, conflict, and resolution: positive contributions to infant development. Am J Orthopsychiatry. 1997;67(1):4–19. doi: 10.1037/h0080207. [DOI] [PubMed] [Google Scholar]
- 9.De Witt SJ, Sparks JW, Swank PB, Smith K, Denson SE, Landry SH. Physical growth of low birthweight infants in the first year of life: impact of maternal behaviors. Early Hum Dev. 1997;47(1):19–34. doi: 10.1016/s0378-3782(96)01757-4. [DOI] [PubMed] [Google Scholar]
- 10.Cioni G, Inguaggiato E, Sgandurra G. Early intervention in neurodevelopmental disorders: underlying neural mechanisms. Dev Med Child Neurol. 2016;58(Suppl 4):61–6. doi: 10.1111/dmcn.13050. [DOI] [PubMed] [Google Scholar]
- 11.Jarjour IT. Neurodevelopmental outcome after extreme prematurity: a review of the literature. Pediatr Neurol. 2015;52(2):143–52. doi: 10.1016/j.pediatrneurol.2014.10.027. [DOI] [PubMed] [Google Scholar]
- 12.Feldman R. The development of regulatory functions from birth to 5 years: insights from premature infants. Child Dev. 2009;80(2):544–61. doi: 10.1111/j.1467-8624.2009.01278.x. [DOI] [PubMed] [Google Scholar]
- 13.Korja R, Maunu J, Kirjavainen J, Savonlahti E, Haataja L, Lapinleimu H, et al. Mother-infant interaction is influenced by the amount of holding in preterm infants. Early Hum Dev. 2008;84(4):257–67. doi: 10.1016/j.earlhumdev.2007.06.006. [DOI] [PubMed] [Google Scholar]
- 14.Lester BM, Boukydis CF, LaGasse L. Cardiorespiratory reactivity during the Brazelton Scale in term and preterm infants. J Pediatr Psychol. 1996;21(6):771–83. doi: 10.1093/jpepsy/21.6.771. [DOI] [PubMed] [Google Scholar]
- 15.Lau C, Hurst N. Oral feeding in infants. Curr Probl Pediatr. 1999;29:105–24. doi: 10.1016/s0045-9380(99)80052-8. [DOI] [PubMed] [Google Scholar]
- 16.Mantymaa M, Puura K, Luoma I, Salmelin RK, Tamminen T. Mother's early perception of her infant's difficult temperament, parenting stress and early mother-infant interaction. Nord J Psychiatry. 2006;60:379–86. doi: 10.1080/08039480600937280. [DOI] [PubMed] [Google Scholar]
- 17.Coppola G, Cassibba R, Costantini A. What can make the difference? Premature birth and maternal sensitivity at 3 months of age: the role of attachment organization, traumatic reaction and baby's medical risk. Infant Behav Dev. 2007;30:679–84. doi: 10.1016/j.infbeh.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 18.DeWitt SJ, Sparks JW, Swank PB, Smith K, Denson SE, Landry SH. Physical growth of low birth weight infants in the first year of life: impact of maternal behaviors. Early Hum Dev. 1997;47:19–34. doi: 10.1016/s0378-3782(96)01757-4. [DOI] [PubMed] [Google Scholar]
- 19.Reyna BA, Pickler RH. Mother-infant synchrony. J Obstet Gynecol Neonatal Nurs. 2009;38(4):470–7. doi: 10.1111/j.1552-6909.2009.01044.x. [DOI] [PubMed] [Google Scholar]
- 20.Leclère C, Viaux S, Avril M, Achard C, Chetouani M, Missonnier S, et al. Why synchrony matters during mother-child interactions: a systematic review. PLoS One. 2014;9(12):e113571. doi: 10.1371/journal.pone.0113571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Feldman R. From biological rhythms to social rhythms: Physiological precursors of mother-infant synchrony. Dev Psychol. 2006;42(1):175–88. doi: 10.1037/0012-1649.42.1.175. [DOI] [PubMed] [Google Scholar]
- 22.Forcada-Guex M, Pierrehumbert B, Borghini A, Moessinger A, Muller-Nix C. Early dyadic patterns of mother-infant interactions and outcomes of prematurity at 18 months. Pediatrics. 2006;118(1):e107–14. doi: 10.1542/peds.2005-1145. [DOI] [PubMed] [Google Scholar]
- 23.Grummer-Strawn LM, Reinold C, Krebs NF Centers for Disease Control and Prevention (CDC) Use of World Health Organization and CDC growth charts for children aged 0-59 months in the United States. MMWR Recomm Rep. 2010;59(RR-9):1–15. [PubMed] [Google Scholar]
- 24.Lau C, Henning SJ. Mutualism in mother-offspring interaction: its importance in the regulation of milk release. In: Meisami E, Timiras PS, editors. Handbook of human growth and developmental biology, Part 2. Boca Raton: CRC-Press, Inc.; 1990. pp. 195–216. [Google Scholar]
- 25.Alberts jr, Gubernick DJ. Reciprocity and resource Exchange. A symbiotic model of parent-offspring relations. In: Rosenblum LA, Moltz H, editors. Symbiosis in Parent-Offspring Interactions. New York: Plenum Press; 1983. pp. 7–44. [Google Scholar]
- 26.Mantymaa M, Puura K, Luoma I, Latva R, Salmelin RK, Tamminen T. Shared pleasure in early mother-infant interaction: predicting lower levels of emotional and behavioral problems in the child and protecting against the influence of parental psychopathology. Infant Ment Health J. 2015;36(2):223–37. doi: 10.1002/imhj.21505. [DOI] [PubMed] [Google Scholar]
- 27.Schaal B, Coureaud G, Doucet S, Delaunay-El Allam M, Moncomble AS, Montigny D, et al. Mammary olfactory signalisation in females and odor processing in neonates: ways evolved by rabbits and humans. Behav Brain Res. 2009;200(2):346–58. doi: 10.1016/j.bbr.2009.02.008. [DOI] [PubMed] [Google Scholar]
- 28.Soussignan R, Schaal B, Boulanger V, Garcia S, Jiang T. Emotional communication in the context of joint attention for food stimuli: effects on attentional and affective processing. Biol Psychol. 2015;104:173–83. doi: 10.1016/j.biopsycho.2014.12.006. [DOI] [PubMed] [Google Scholar]
- 29.Mantis I, Stack DM, Ng L, Serbin LA, Schwartzman AE. Mutual touch during mother-infant face-to-face still-face interactions: influences of interaction period and infant birth status. Infant Behav Dev. 2014;37(3):258–67. doi: 10.1016/j.infbeh.2014.04.005. [DOI] [PubMed] [Google Scholar]
- 30.Feldman R. Parent-infant synchrony and the construction of shared timing; physiological precursors, developmental outcomes, and risk conditions. J Child Psychol Psychiatry. 2007;48(3-4):329–54. doi: 10.1111/j.1469-7610.2006.01701.x. [DOI] [PubMed] [Google Scholar]


