ABSTRACT
Introduction
Dyspepsia is a common symptom with an extensive differential diagnosis. Endoscopy alone may miss serious mucosal lesions in about 15 to 30% of cases. The aim was to determine histopathological features of gastric and duodenal mucosal biopsies in patients with dyspepsia and normal looking upper gastrointestinal (GI) endoscopy.
Materials and methods
One hundred and five adult patients presenting with dyspepsia with no endoscopic mucosal lesions in the upper GI tract were included. Gastric biopsy specimens according to Sydney–Houston system for grading gastritis and biopsy from duodenum were taken. The histopathological features were graded according to the Sydney–Houston system classification for grading gastritis.
Results
The histological lesions were found in 65.7% (69 out of 105 endoscopy free dyspeptic patients). Chronic inflammation was the commonest finding. Neutrophilic activity, glandular atrophy, and mild degree of intestinal metaplasia were present in 27, 45, and 6 patients (22.8, 42.8, and 5.7% respectively). Helicobacter pylori was present in 54 patients with histopathological lesions and in 6 patients without histopathological lesions, and the difference was significant (p = 0.045).
Conclusion
The endoscopic diagnosis of dyspepsia correlated poorly with histopathological findings. The histopathological examination allowed detection and grading of gastric pathology in dyspepsia with normal endoscopy and the commonest finding was the moderate chronic gastritis.
How to cite this article
Dawod HM, Emara MW. Histopathological Assessment of Dyspepsia in the Absence of Endoscopic Mucosal Lesions. Euroasian J Hepato-Gastroenterol 2016;6(2):97-102.
Keywords: Biopsy, Chronic gastritis, Dyspepsia, Endoscopy.
INTRODUCTION
Dyspepsia is a term used for acute, chronic, or recurrent pain or discomfort centered in the upper abdomen. It may be associated with upper abdominal fullness, early satiety, and bloating, burning, belching, nausea, retching, and vomiting.1 Dyspepsia occurs in 25% of adult population and accounts for 5% of general clinics visits.2 Approximately 25% of patients with dyspepsia have an organic cause and up to 75% have functional dyspepsia.3
Patients with symptoms of dyspepsia who have not investigated are defined as having uninvestigated dyspepsia.4 In patients with dyspepsia who are investigated, major causes include medications, functional dyspepsia, chronic peptic ulcer disease, and malignancy.2 Other minor causes include pancreatic and hepatobiliary tract disease, motility disorders, infiltrative diseases of the stomach, celiac disease, metabolic disturbances, diabetic neuropathy, and hernia.5
The alarm signs, age, and the local prevalence of Helicobacter pylori infection determine the diagnostic approach of a case of dyspepsia.6 In patient with an age of ≤55 years, the American Gastroenterological Association (AGA) identifies unintended weight loss, progressive dysphagia, persistent vomiting, evidence of gastrointestinal (GI) bleeding, and family history of cancer as alarm signs. The AGA recommends endoscopy to be done first in patients with alarm signs and in patients >55 years.1 Patients ≤55 years of age without alarm features should be tested and treated for H. pylori if the local prevalence of H. pylori is high (>20%).7 Empiric acid suppressive treatments without H. pylori testing/treatment are recommended in areas of low prevalence for H. pylori (<20%).2
Once a patient has failed a 4 to 8 weeks trial of empiric treatment or failed to respond to eradication of H. pylori, upper endoscopy is indicated.4 Endoscopy alone is insufficient because it may miss serious mucosal lesions in about 15 to 30% of cases that can be picked up later on by histological examination.8 Biopsy is convenient procedure for accurate assessment and diagnosis of premalignant gastric lesions.9 Moreover, the biopsy is important for identifying and grading various mucosal pathologic lesions.10,11 The sites for biopsy taking from stomach according to the Sydney–Houston system are from the antrum, the angulus, and the corpus.12,13 The aim of this study was to determine histopathological features of gastric and duodenal mucosal biopsies in dyspepsia with normal looking upper GI endoscopy.
MATERIALS AND METHODS
Patient Selection
This study was conducted at the Department of Tropical Medicine, Faculty of Medicine, Zagazig University Hospitals in Egypt from July 2014 to August 2015, and 105 consecutive adult patients who were presented with dyspepsia and no mucosal lesions by the upper endoscopy were selected.
Exclusion criteria: Recent history of nonsteroidal anti-inflammatory drugs (NSAIDs), proton pump inhibitors, antibiotic intake within 1 month, peptic ulcer disease, gastroesophageal (GE) reflux disease, choledocholithiasis, pancreatitis, uncontrolled diabetes mellitus, hypercalcemia, coagulopathy, alcohol intake, celiac disease, chronic disease, end organ failure, immunocompromised, abdominal malignancy, or gastrostomy. This study was carried out in accordance with the World Medical Association Code of Ethics (Declaration of Helsinki) and a written informed consent for endoscopy, biopsy, and for taking blood sample was obtained from all patients. The protocol was approved by a review board of Tropical Medicine Department of Zagazig University.
Study Design
A cross-sectional study was conducted on 105 patients presenting with dyspepsia, with no mucosal lesions were found in the upper GI tract by endoscopy. Patients were further evaluated by obtaining gastric biopsy specimens from the following sites according to Sydney–Houston system for grading gastritis: (1) Greater and lesser curvature of the distal antrum, (2) greater and lesser curvature of the proximal corpus, and (3) lesser curvature at the incisor angularis.14 One biopsy from the duodenum was also taken by standard biopsy forceps. The specimens were properly labeled, fixed in 10% buffered formalin, processed using paraffin embedding technique, sectioned at 4 μm perpendicular to the mucosal surface and stained with hematoxylin and eosin (H&E) and with Giemsa. The same pathologist examined all the materials. The histopathological features were graded.
All patients in this study were subjected to history taking, clinical examination, complete blood picture, fasting blood sugar, random blood sugar, blood urea and serum creatinine, liver function tests, H. pylori antigen in stool testing, and abdominal ultrasonography. Upper GI endoscopy was done after overnight fast for 6 hours using Pentax EPM-3500; Tokyo, Japan. The endoscopic examination was done by the same endoscopist.
Statistical Analysis
Data were coded and analyzed using Statistical Package for the Social Sciences (SPSS) version 16. Data were expressed as mean ± standard deviation (SD) for quantitative variables, number, and percentage for qualitative ones. Chi-squared and McNemar tests were used when appropriate, with p < 0.05 considered as statistically significant. The sample size was calculated using Epi-Info version 6 at power of study, 80 and 95% confidence interval, and the level of significance < 0.05.
RESULTS
A total of 105 patients (51 males and 54 females; mean age 45.54 ± 9.5, range: 22–60 years) who presented with dyspepsia and no mucosal lesions found in the upper GI tract by endoscopy were enrolled in the study (Table 1).
Table 1: Demographic characteristics of the patients
| Data | n = 105 patients | ||
| Gender (%) | |||
| Male | 51 (48. 6%) | ||
| Female | 54 (51.4%) | ||
| Age (years) | |||
| Mean ± SD | 45.54 ± 9.50 | ||
| Range | 22–60 | ||
| Frequency of histopathological lesions in dyspeptic patients | 69 (65.7%) |
The laboratory parameters of the patients were within normal values (Table 2). Epigastric pain and epigastric burning were the most common presentation of the studied patients (45 and 27 patients) (42 and 25.7%) respectively, while dysphagia and nausea in 6 and 3 patients (5.7 and 2.9% respectively) were the least common presentations (Table 3).
Table 2: Laboratory data of studied patients
| Variable | Mean ± SD | Range | |||
| WBC (×103/mL) | 7.29 ± 4.62 | 4.5–11 | |||
| Hemoglobin (mg/dL) | 13.05 ± 1.60 | 8–15 | |||
| Platelet (×103/mL) | 274.11 ± 82.27 | 156–411 | |||
| ALT (IU/mL) | 17.6 ± 4.50 | 12–24 | |||
| AST (IU/mL) | 19.00 ± 4.62 | 12–30 | |||
| Bilirubin (mg/dL) | 0.74 ± 0.17 | 0.5–1.2 | |||
| Albumin (mg/dL) | 4.19 ± 0.27 | 3.8–5 | |||
| INR | 1.15 ± 0.061 | 1.1–1.3 | |||
| Creatinine (mg/dL) | 0.7 ± 0.12 | 0.8–1.1 |
ALT: Alanine aminotransferase; AST: Aspartate aminotransferase; INR: International normalized ratio
Table 3: Clinical presentation of studied patients
| Symptom | Number | Percentage | |||
| Epigastric pain | 45 | 42.8 | |||
| Epigastric burning | 27 | 25.7 | |||
| Unexplained weight loss | 15 | 14.3 | |||
| Persistent vomiting | 9 | 8.6 | |||
| Dysphagia | 6 | 5.7 | |||
| Nausea | 3 | 2.8 | |||
| Total | 105 | 100 |
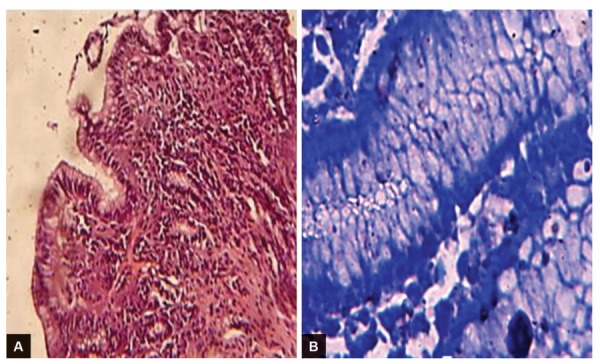
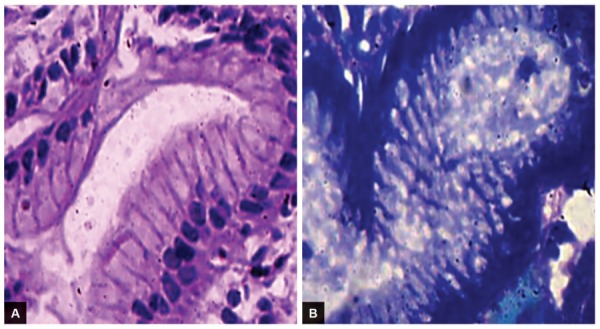
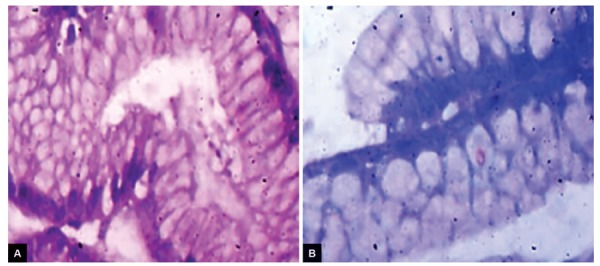
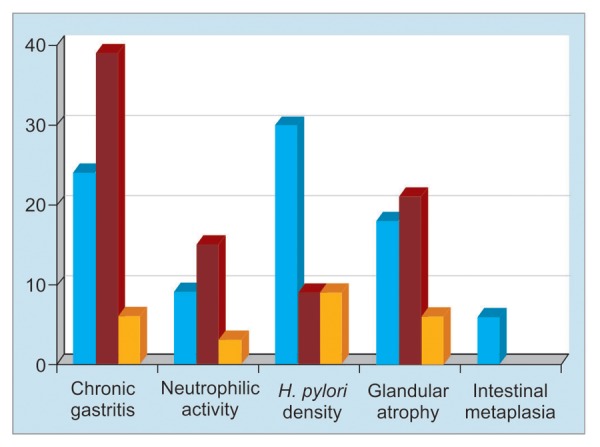
The frequency of histological lesions among dyspeptic patients was 65.7% (69 out of 105 patients), while no lesions in the other 36 (34.3%) patients were observed by endoscopy and biopsy (Table 2). The commonest lesion was the chronic inflammation of gastric mucosa (65.7%) (Table 4, Graph 1). The grading of the chronic inflammation was as follows: 24 patients with mild chronic inflammation, 39 patients with moderate chronic inflammation (Figs 1A and B), and 6 patients with marked chronic inflammation. Neutrophilic activity was present in 27 patients with only 3 patients with marked neutrophilic activity (Figs 2A and B). Helicobacter pylori density was present in 54 patients and 30 of them showed mild degree of H. pylori density. Glandular atrophy was present in 45 patients with only 6 patients with marked degree of glandular atrophy. Mild degree of intestinal metaplasia was only present in 6 female patients (Figs 3A and B).
Table 4: Pathological variability in patients with dyspepsia
| Grade | |||||||||||
| Variability | None | Mild | Moderate | Marked | Total n (%) | ||||||
| Chronic gastritis | 36 | 24 | 39 | 6 | 69 (65.7) | ||||||
| Neutrophilic activity | 78 | 9 | 15 | 3 | 27 (22.8) | ||||||
| H. pylori density | 51 | 30 | 12 | 12 | 54 (51.4) | ||||||
| Glandular atrophy | 60 | 18 | 21 | 6 | 45 (42.8) | ||||||
| Intestinal metaplasia | 99 | 6 | – | – | 6 (5.7) | ||||||
Graph 1:
Pathological variability in patients with functional dyspepsia
Figs 1A and B:
Chronic gastritis and positive H. pylori infection: (A) H&E stain; and (B) geimsa stain
Figs 2A and B:
Chronic gastritis and positive H. pylori infection: The lamina propria is moderately infiltrated by chronic inflammatory cells, mainly plasma cells and lymphocytes with few neutrophils: (A) H&E stain; and (B) geimsa stain
Figs 3A and B:
Chronic gastritis, positive H. pylori infection, and intestinal metaplasia: (A) H&E stain; and (B) geimsa stain
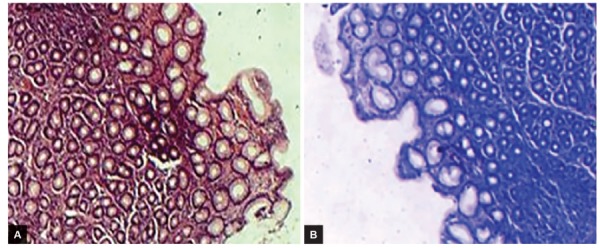
Table 5 shows that the H. pylori infection was present in 6 patients without histopathological lesion (16.67%) (Figs 4A and B), while it was present in 54 patients with histopathological lesion (78.2%) and the difference was statistically significant (p = 0.04). Helicobacter pylori infection was present in 24 patients (53.33%) out of 45 patients with glandular atrophy. All the patients tolerated endoscopy and biopsy with no complications.
Table 5: Distribution of H. pylori infection in dyspeptic patients with and without histopathological lesion
| H. pylori | Without HPL | With HPL | Total | p-value | |||||
| +ve | 6 (16.67%) | 54 (78.2%) | 60 | ||||||
| –ve | 30 (83.33%) | 15 (20.8%) | 45 | ||||||
| Total | 36 | 69 | 105 | 0.04* |
*p & 0.05: Significant; HPL: Histopathological lesion
Figs 4A and B:
Chronic gastritis and negative H. pylori infection: (A) H&E stain; and (B) geimsa stain
DISCUSSION
Dyspepsia is a common symptom and represents a great health care problem.15 Around 60% of patients with dyspepsia still have no explanation for their symptoms.16 The aim of this study was to determine histopathological features of gastric and duodenal mucosal biopsies in dyspeptic patients with free endoscopy. In this study, the histopathological examination of the gastric biopsies showed normal findings in around 34.3% and a high degree of inflammation which occurred in 65.7%. This result was in agreement with observations by Nwokediuko and Okafor,17 who found that only 29.3% of patients with functional dyspepsia had normal histology of gastric biopsies by histological examination. This result is also in accordance with which was reported by Arruda et al,18 who studied 40 dyspeptic patients (28 women and 12 men) with endoscopically normal stomach and found 72.5% of patients with gastritis by histological examination. This emphasizes the role of biopsy in examining a case of dyspepsia as the normal endoscopy does not rule out underlying pathology. Garg et al19 and Khan et al20 reported in their studies a lower rate of inflammation in the gastric biopsies (20 and 32% respectively) of dyspeptic cases with a normal endoscopy. This difference may be attributed to high prevalence of H. pylori infection among Egyptian patients.
Chronic inflammation was present in 65.7% of patients with dyspepsia and was higher than that of H. pylori infections (51.4%). This could be explained by the presence of other causes of inflammation than H. pylori or previous ingestion of antibiotics which are known to suppress the H. pylori infection with a slow disappearance of chronic inflammatory cells.21
In the present study, the prevalence of H. pylori was 51.4%. Nwokediuko and Okafor17 and Calabrese et al22 reported lower rates of the prevalence of H. pylori (37.3 and 30.9% respectively) in patients with normal looking mucosa, while Shrivastava et al23 observed a higher incidence rate of H. pylori infection among functional dyspeptic patients (65%). This could be explained by variations in the prevalence of H. pylori according to geographic area, age, and socioeconomic status.24 Moreover, there is a variation in diagnostic methods which may further contribute to different rates of detection.
A highlight on the relation between H. pylori infection and chronic gastritis was noted in our study, as H. pylori was present only in 6 patients without histopathological lesions, while it was present in 54 patients with histopathological lesions and the difference was statistically significant (p = 0.04), which is matching with the fact that the main cause of chronic gastritis is H. pylori infection.25
Intestinal metaplasia and glandular atrophy were present in 5.7 and 42.8% respectively, of patients with dyspepsia. However, these results were less than those reported by Leodolter et al26 and Anatoliy et al27 (24.1 and 64.0% respectively), and this difference may be due to including patients with functional dyspepsia and positive H. pylori infection in their studies.
Biopsy was not taken from the lower esophagus as patients with history or symptoms of reflux disease were not included and this is in accordance with the recent recommendation of AGA28 that routine biopsy of normal esophagus or GE junction in patients with dyspepsia alone would have very low probability of diagnosing esophageal abnormalities or have little impact on clinical management. Piatek et al11 advised biopsy taking from stomach and duodenum only in either organic or functional dyspepsia. They reported in their study nonspecific inflammation of all normal looking duodenums independent of H. pylori state, unlike in our study where the duodenal biopsy showed nonspecific inflammation in 3 patients only. Our results clarify the need to obtain gastric biopsies during upper GI endoscopy even if the endoscopic appearance is normal or without any gross pathology which is matching with recent recommendations from AGA.28
CONCLUSION
The conventional endoscopic diagnosis of dyspepsia correlated poorly with histopathological findings. The histopathological examination allowed detection and grading of gastric pathology in dyspepsia with normal endoscopy and it showed that the moderate chronic gastritis was the most common finding in this study.
Footnotes
Source of support: Nil
Conflict of interest: None
REFERENCES
- 1.Conoroy RT. Siddiqi. B. Dyspepsia. Prim Care. 2007 Mar;34(1):99–108. doi: 10.1016/j.pop.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 2.Talley NJ, Vakil NB, Moayyedi P. American Gastroenterological Association technical review on the evaluation of dyspepsia. Gastroenterology. 2005 Nov;129(5):1756–1780. doi: 10.1053/j.gastro.2005.09.020. [DOI] [PubMed] [Google Scholar]
- 3.Drossman DA. The functional gastrointestinal disorders and the Rome III process. Gastroenterology. 2006 Apr;130(5):1377–1390. doi: 10.1053/j.gastro.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 4.Lieberman D, Fennerty MB, Morris CD, Holub J, Eisen G, Sonnenberg A. Endoscopic evaluation of patients with dyspepsia: results from the national endoscopic data repository. Gastroenterology. 2004 Oct;127(4):106–775. doi: 10.1053/j.gastro.2004.07.060. [DOI] [PubMed] [Google Scholar]
- 5.Bytzer P. Dyspepsia. Ann Intern Med. 2001 May;134(9 Pt 2):815. doi: 10.7326/0003-4819-134-9_part_2-200105011-00004. [DOI] [PubMed] [Google Scholar]
- 6.World Gastroenterology Organization Global Guideline. Helicobacter pylori in developing countries. J Dig Dis. 2011 Oct;12(5):319–326. doi: 10.1111/j.1751-2980.2011.00529.x. [DOI] [PubMed] [Google Scholar]
- 7.Grad YH, Lipsitch M, Aiello AE. Secular trends in Helicobacter pylori seroprevalence in adults in the United States: evidence for sustained race/ethnic disparities. Am J Epidemiol. 2012;175(1):54–59. doi: 10.1093/aje/kwr288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eisen G, Baron TH, Dominitz J et al. Complications of upper GI endoscopy. Gastrointest Endosc. 2002;55:784–93. doi: 10.1016/s0016-5107(02)70404-5. [DOI] [PubMed] [Google Scholar]
- 9.Redéen S, Petersson F, Jönsson KA, Borch K. Relationship of gastroscopic features to histological findings in gastritis and Helicobacter pylori infection in a general population sample. Endoscopy. 2003 Nov;35(11):946–950. doi: 10.1055/s-2003-43479. [DOI] [PubMed] [Google Scholar]
- 10.Carpenter HA, Talley NJ. Gastroscopy is incomplete without biopsy: clinical relevance of distinguishing gastropathy from gastritis. Gastroenterology. 1995 Mar;108(3):917–924. doi: 10.1016/0016-5085(95)90468-9. [DOI] [PubMed] [Google Scholar]
- 11.Piatek A, Przybylska M, Dynowski W, Zwolińska M, Lickiewicz J, Mach T. Endoscopic and histopathological findings of the upper gastrointestinal tract in patients with functional and organic dyspepsia. Przegl Lek. 2014;71(4):204–209. [PubMed] [Google Scholar]
- 12.Dixon MF, Genta RM, Yardley JH, Correa P. Classification and grading of gastritis. Am J Surg Pathol. 1996 Oct;20(10):1161–1181. doi: 10.1097/00000478-199610000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Sharaf RN, Shergill AK, Odze RD, Krinsky ML, Fukami N, Jain R, Appalaneni V, Anderson MA, Ben-Menachem T, Chandrasekhara V et al. Endoscopic mucosal tissue sampling. Gastrointest Endosc. 2013 Aug;78(2):216–224. doi: 10.1016/j.gie.2013.04.167. [DOI] [PubMed] [Google Scholar]
- 14.Rugge M. Atrophic gastritis: pathology and endoscopy in the reversibility assessment. Gut. 2003 Sep;52(9):1387–1388. doi: 10.1136/gut.52.9.1387-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tack J, Talley NJ, Camilleri M, Holtmann G, Hu P, Malagelada JR, Stanghellini V. Functional gastroduodenal disorders. Gastroenterology. 2006 Apr;130(5):1466–1479. doi: 10.1053/j.gastro.2005.11.059. [DOI] [PubMed] [Google Scholar]
- 16.Fraser A, Delaney B, Moayyedi P. Symptom-based outcome measures for dyspepsia and GERD trials: a systematic review. Am J Gastroenterol. 2005 Feb;100(2):442–452. doi: 10.1111/j.1572-0241.2005.40122.x. [DOI] [PubMed] [Google Scholar]
- 17.Nwokediuko SC, Okafor OC. Gastric mucosa in nonulcer dyspepsia: a histopathological study of Nigerian patients. I J Gastroenterol. 2007;5(2) [Google Scholar]
- 18.Arruda SMB de, Forones NM, Jucá NT, Barros KSC de. Could gastric histology be a useful marker for making decision on Helicobacter pylori eradication therapy in patients with dyspepsia? Arq Gastroenterol. 2009 Jul-Sep;46(3):209–213. doi: 10.1590/s0004-28032009000300013. [DOI] [PubMed] [Google Scholar]
- 19.Garg B, Sandhu V, Sood N, Sood A, Malhotra V. Histopathological analysis of chronic gastritis and correlation of pathological features with each other and with endoscopic findings. Pol J Pathol. 2012;3:172–178. doi: 10.5114/pjp.2012.31501. [DOI] [PubMed] [Google Scholar]
- 20.Khan MQ, Alhomsi Z, Al-Momen S, Ahmad M. Endoscopic features of Helicobacter pylori induced gastritis. Saudi J Gastroenterol. 1999 Jan;5(1):9–14. [PubMed] [Google Scholar]
- 21.Witteman EM, Mravunac M, Becx MJ, Hopman WP, Verschoor JS, Tytgat GN, de Koning RW. Improvement of gastric inflammation and resolution of epithelial damage one year after eradication of Helicobacter pylori. J Clin Pathol. 1995 Mar;48(3):250–256. doi: 10.1136/jcp.48.3.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Calabrese C, Di Febo G, Brandi G, Morselli-Labate AM, Areni A, Scialpi C, Biasco G, Miglioli M. Correlation between endoscopic features of gastric antrum, histology and Helicobacter pylori infection in adults. Ital J Gastroenterol Hepatol. 1999 Jun-Jul;31(5):359–365. [PubMed] [Google Scholar]
- 23.Shrivastava UK, Gupta A, Gupta A, Bhatia A. Role of Helicobacter pylori in functional dyspepsia. Indian J Surg. 2004;66:341–346. [Google Scholar]
- 24.Kumar R, Bano G, Kapoor B, Sharma S, Gupta Y. Clinical profile in H. pylori positive patients in Jammu. JK Sci. 2006 Jul-Sep;8(3):148–150. [Google Scholar]
- 25.Sipponen P, Maaroos H-I. Chronic gastritis. Scand J Gastroenterol. 2015 Jun;50(6):657–667. doi: 10.3109/00365521.2015.1019918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Leodolter A, Ebert MP, Peitz U, Wolle K, Kahl S, Vieth M, Malfertheiner P. Prevalence of H. pylori associated “high risk gastritis” for development of gastric cancer in patients with normal endoscopic findings. World J Gastroenterol. 2006 Sep;12(34):5509–5512. doi: 10.3748/wjg.v12.i34.5509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Anatoliy S, Iryna K, Olena K, Solovyova G. The frequency and type of histological gastric changes in patients with functional dyspepsia. 22nd United European Gastroenterology Week. 2014 Oct;:18–22. Vienna, Australia. [Google Scholar]
- 28.Allen JI, Katzka D, Robert M, Leontiadis GI. American Gastroenterological Association institute technical review on the role of upper gastrointestinal biopsy to evaluate dyspepsia in the adult patient in the absence of visible mucosal lesions. Gastroenterology. 2015 Oct;149(4):1088–1118. doi: 10.1053/j.gastro.2015.07.040. [DOI] [PubMed] [Google Scholar]


