A 74-year-old female presented with one year history of gradually progressive fatigue, hyperleucocytosis (WBC of 200 K/uL), hemoglobin of 9.7 g/dl, and platelets of 23 K/uL. Physical examination showed generalized petechiae without lymphadenopathy or hepatosplenomegaly. Peripheral smear showed marked leukocytosis with 86% large atypical lymphocytes with prominent small nucleoli. Bone marrow (BM) revealed a hypercellular (80–90%) BM with sheets of atypical lymphocytes (Fig. 1A,B). The atypical neoplastic infiltrate was composed of B-cells with an activated B-cell like immunophenotype (CD5, CD10, BCL-6 negative, and MUM-1 positive) with a Ki-67 proliferation rate of approximately 70–80%. In situ hybridization for EBV – Epstein Barr Virus was negative. Conventional cytogenetic studies showed a complex female karyotype with t(8;14)(q24q32). FISH – fluorescent in situ hybridization study showed 76.5% of cells with a rearrangement of chromosome 8 within the MYC gene breakpoint. Molecular studies showed rearrangements of the IgH heavy chain and TCRγ genes. Initial chest X-ray, spinal fluid examination, and PET-CT –Positron emission tomography with computerised tomography Scan were normal. LDH – lactate dehydrogenase was 2,172 IU/L (normal range 313–618 IU/L). She was treated with a modified hyper CVAD – cyclophosphamide, vincris-tine, adriamycin and dexamethasone protocol. Her BM post three cycles was in complete remission and she had remarkable clinical improvement after completion of eight cycles.
Figure 1.
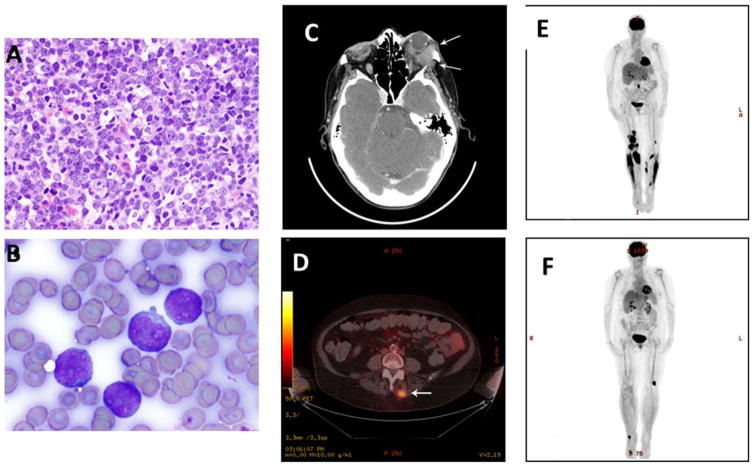
(A–F). Bone marrow biopsy and aspirate findings in leukemic phase of high grade diffuse large B cell lymphoma (DLBCL) with t(8;14). (A) The normal hematopoietic elements in the bone marrow biopsy were almost completely replaced by sheets of atypical lymphocytes (Hematoxylin and Eosin, ×400). (B) Aspirate smears showed numerous large atypical lymphocytes with round and irregular nuclei, dispersed nuclear chromatin, prominent small nucleoli, and moderate to abundant agranular basophilic cytoplasm (Wright Giemsa, × 1000). (C) CT scan of orbits showing orbital recurrence of DLBCL. Recurrence is seen beneath the left lateral rectus muscle (see white arrows). There was also destruction of the posterior wall of the orbit and evidence of left orbital proptosis. (D) PET scan showing multiple hyper metabolic masses involving right and left leg musculature. In the right mid-thigh, whereas in the left leg just above the knee. A mass in medial right gastrocnemius muscle had a SUV of 10.7. (E) Focal hyper metabolism in left posterior paraspinal musculature, with a 2.3 cm nodule and SUV 7.4 at the L4 vertebral level was noted (see arrow). (F). Good response was demonstrated by PET scan, after local radiotherapy except for one area on left lower thigh. [Color figure can be viewed in the online issue, which is available at wileyonlinelibrary.com.]
She then presented with proptosis of her left eye. A CT scan showed a 2.6 cm mass within the left orbit. There was no definitive intracranial extension and bony structures were otherwise intact (Fig. 1C). Her blood counts and BM reports were normal at this time. She was treated with local radiotherapy along with high dose steroids achieving a complete resolution. She was started on a dose attenuated version of Rituximab-hyper-CVAD regime and after 2 months she presented with pain and swelling in both legs. PET scan showed multiple hyper metabolic masses involving right and left leg musculature. Focal hyper metabolism in left posterior paraspinal musculature, with a 2.3 cm nodule and SUV – Standardised uptake value 7.4 at the L4 vertebral level was also noted (Fig. 1D,E). A repeat BM was again normal. Core needle biopsy of right thigh mass showed extra medullary re-recurrence of high grade diffuse large B-cell lymphoma (DLBCL). Local radiotherapy was given to affected areas with disappearance of the lesions (Fig. 1F). She received salvage chemotherapy with ofatu-mumab with ifosfamide, carboplatin, and etoposide (O-ICE), along with supportive multidisciplinary care but ultimately progressed and was referred to hospice care. Patient had DLBCL in the bone marrow with t(8;14) without evidence of a double hit NHL – Non Hodgkin’s Lymphoma, i.e. (myc with Bcl2 gene rearrangement). Patient had multiple extramedullary relapses involving the orbit, muscles of both lower limbs. She did not achieve durable remissions to multiple types of therapies. Our case presented several dilemmas regarding diagnosis and clinical management of leukemic phase of DLBCL [1,2]. The clinical picture mimicked with acute leukemia. The best diagnosis was leukemic phase of recurrent high grade DLBCL with t(8;14). Very few cases of leukemic phase of DLBCL have been described [3].
Acknowledgments
PJ, RS, SK and HK, TK gathered data and organized the figures. PJ, RS, TK, OB collected pictures and evaluated the pathology. All Authors have reviewed the manuscript and checked the literature and took care of the patient.
Footnotes
Conflict of interest: Nothing to report
References
- 1.Muringampurath-John D, Jaye DL, Flowers CR, et al. Characteristics and outcomes of diffuse large B-cell lymphoma presenting in leukaemic phase. Br J Haematol. 2012;158:608–614. doi: 10.1111/j.1365-2141.2012.09209.x. [DOI] [PubMed] [Google Scholar]
- 2.Park S, Moon SH, Park LC, et al. The impact of baseline and interim PET/CT parameters on clinical outcome in patients with diffuse large B cell lymphoma. Am J Hematol. 2012;87:937–940. doi: 10.1002/ajh.23267. [DOI] [PubMed] [Google Scholar]
- 3.Morra E, Lazzarino M, Castello A, et al. Bone marrow and blood involvement by non-Hodgkin’s lymphoma: A study of clinicopathologic correlations and prognostic significance in relationship to the Working Formulation. Eur J Haematol. 1989;42:445–453. doi: 10.1111/j.1600-0609.1989.tb01469.x. [DOI] [PubMed] [Google Scholar]