Abstract
Purpose
It is generally accepted that using a video laryngoscope is associated with an improved visualization of the glottis. However, correctly placing the endotracheal tube might be challenging. Channeled video laryngoscopic blades have an endotracheal tube already pre-loaded, allowing to advance the tube once the glottis is visualized. We hypothesized that use of a channel blade with pre-loaded endotracheal tube results in a faster intubation, compared to a curved Macintosh blade video laryngoscope.
Methods
After ethical approval and informed consent, patients were randomized to receive endotracheal Intubation with either the King Vision® video laryngoscope with curved blade (control) or channeled blade (channeled). Success rate, evaluation of the glottis view (percentage of glottic opening (POGO), Cormack&Lehane (C&L)) and intubating time were evaluated.
Results
Over a two-month period, a total of 46 patients (control n = 23; channeled n = 23) were examined. The first attempt success rates were comparable between groups (control 100% (23/23) vs. channeled 96% (22/23); p = 0.31). Overall intubation time was significantly shorter with control (median 40 sec; IQR [24–58]), compared to channeled (59 sec [40–74]; p = 0.03). There were no differences in glottis visualization between groups.
Conclusion
Compared with the King Vision channeled blade, time for tracheal intubation was shorter with the control group using a non-channeled blade. First attempt success and visualization of the glottis were comparable. These data do not support the hypothesis that a channeled blade is superior to a curved video laryngoscopic blade without tube guidance.
Trial registration
ClinicalTrials.gov NCT02344030
Introduction
It is generally accepted that direct laryngoscopy using a Macintosh blade is a difficult skill to master [1]. The limitations of direct laryngoscopy are well known. A minimum number of 50 intubations is necessary to achieve a first pass Intubation success rate of >85% using direct laryngoscopy [2–4]. To obtain optimal visualisation of the glottis, direct laryngoscopy requires alignment of the oropharyngeal-laryngeal axes. However, duration of intubation and the success rate for securing the airway by tracheal intubation might have a significant impact on undesirable events like hypoxia or regurgitation.
Recently, the use of video laryngoscopy has become a widely accepted method in both emergency medicine and clinical anesthesia. It facilitates easy visualization of the glottis without a direct line of sight [5–6]. Ease of handling, high success rate in patients with normal and with difficult airways, high success rate in difficult airway situations and a steep learning curve makes these devices very popular among physicians [7–8].
It can sometimes be challenging to place an endotracheal tube (ETT) in front of the glottis and advance it despite good visualization on the monitor, especially when a video laryngoscope (VL) with a hyper-angulated blade is used [9]. This phenomena (great view but unable to intubate) is linked to VL blades that are, unlike the traditional Macintosh blade, hyper-angulated. Because of the unique profile that follows the anatomical shape of the human airway, alignment of the oropharyngeal-laryngeal axes becomes unnecessary to visualize the glottis. The new challenge is now to also bring the tip of the ETT to the level of the glottis, pass the glottis and advance the tube inside the trachea. Several techniques have been proposed to meet this challenge; many authors proposed using a stylet to give the tube the shape of a “hockey stick” to follow the curvature of the video blade [10]. However, ETT placement is often associated with a prolonged time for intubation [11]. Additionally, stylet use for video laryngoscopy has been linked to an increased risk of soft tissue injury of the upper airway [12]. VLs with an embedded tube-guiding channel might resolve this issue, because the tube is already loaded on the curved blade allowing the tube to be advanced once the glottis is visualized. This technique removes the need for a stylet and additional manipulations to steer the tube through the upper airway.
We hypothesized that the use of a VL with a curved, channeled blade allows faster intubation compared to a similar-shaped video blade without a guide channel (Fig 1). The King Vision VL was used for this trial because both blade types with a similar shape are available for this device. The only difference between these single-use blades is the presence of tube guidance in the channeled blade. The term “tube-guiding” is representative for the King Vision channeled blade in this manuscript.
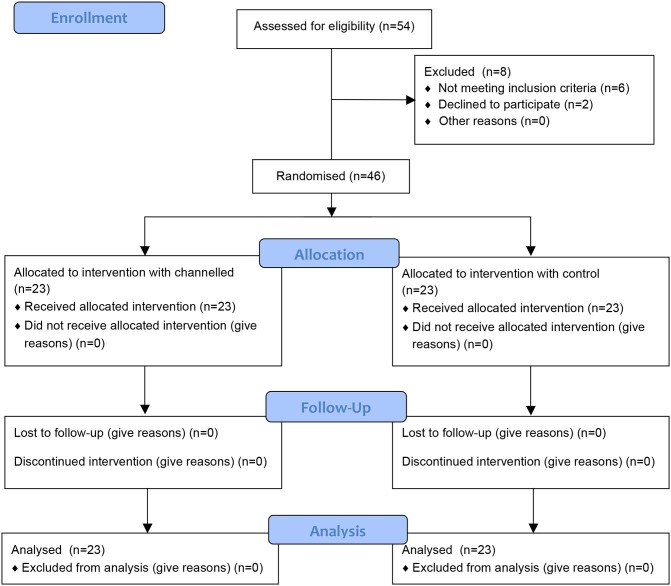
Fig 1. CONSORT flow diagram.
Methods
The ethics committee of the Medical Association of the state of Rhineland Palatine (Germany) approved this trial (Registration Nr.: 837.403.14 (9642)). This study is registered with ClinicalTrial.gov register number NCT 02344030. Written informed consent was obtained from all patients at least 18 hours before randomization.
After sample size calculation, a prospective, randomized, controlled trial (S1 File) in patients undergoing general anesthesia at a tertiary university hospital (Anesthesia Division of the Departments of Ear-nose-throat Surgery and Ophthalmic Surgery) was designed to examine the hypothesis that a video laryngoscope with a guide channel is more superior (S2 File).
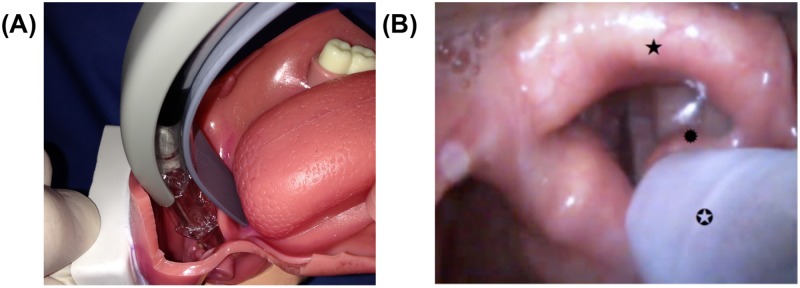
The King Vision™ aBlade VL (KV; Ambu GmbH, Bad Nauheim, Germany) was used for this study. For the KV, two types of blades are available: one with an integrated tube guiding channel (channeled) and a non-channeled version (control; Fig 2). Both models have high blade angulation (blade angle 90 degrees) with a similar shape; the only difference is the presence of a tube guide channel. The KV device consists of a 2.4-inch reusable OLED-Display (organic light emitting diode) and a disposable rigid blade that also includes a CMOS (Complementary metal-oxide-semiconductor) video camera (Fig 2). The KV is a wireless and fully portable VL with a high blade angulation, making direct visualization of the glottis unlikely. The blade size #3 is provided for adult use (tube sizes 6.0 to 8.0 mm). In total, 25 anesthesiologists participated in this trial; all were previously trained with video laryngoscopes and had sufficient clinical experiences using the device (Table 1). Each physician was given a standardized demonstration of the King Vision by one of the investigators: after an introduction which included handling as well the specifics of the device an intubation procedure was demonstrated.
Fig 2. King Vision with non-channeled and channeled blades.
Table 1. Data collection.
| Patient characteristics | Control (n = 23) | Channeled (n = 23) | p-value |
|---|---|---|---|
| Age (years) | 44 (23–89 [31–64]) | 48 (20–72 [32–58]) | 0.79 |
| Gender (female/male) | 12/11 | 11/12 | 0.76 |
| BMI kg.m2 | 25.3 (21–32 [23.8–26.8]) | 26 (20–34 [24.1–30.5]) | 0.32 |
| ASA class | 2 (1–3 [1–3]) | 2 (1–3 [1–3]) | 0.54 |
| Provider (n = 25) | < 0.001 | ||
| Residents (n = 18) | 16/23 (69%) | 18/23 (78%) | 0.37 |
| Specialists (n = 7) | 7/23 (31%) | 5/23 (22%) | 1.0 |
| Anesthesia experience (months) | 15 (5–200 [6–96]) | 23 (2–180 [12–72]) | 0.82 |
| VL experience (n = 25) (applications) | 0.87 | ||
| <10 | 1 | 0 | |
| >10 | 6 | 6 | |
| >25 | 6 | 7 | |
| >50 | 10 | 10 |
Data are given as Median (range [IQR]) or absolute numbers (%).
Patient selection
Patients undergoing elective, routine anesthesia were asked to participate in this trial. Exclusion criteria were: age under 18 years, potential risk of regurgitation, pregnancy, ASA classification > III and patients with an anticipated difficult airway.
Setting and intervention
All intubations were performed using either a size 3 curved blade (“control”) or a size 3 curved blade with a tube-guiding channel (“channeled”), respectively. The size of the ETT was predefined by the standard operating procedure of the study center. ETT size 7.0 internal diameter (ID) was used for female patients and 7.5 ID for male patients (Mallinckrodt Medical, Athlone, Ireland). For intubation in the control group a malleable stylet was inserted in the ETT in a hockey-stick shape (distal end of ETT angulated of 90°). When applying the channeled blade, the ETT was preloaded in the tube-guiding channel before insertion of the channeled into the mouth of the patient. After three minutes of pre-oxygenation with a facemask, anesthesia was induced with sufentanil (0.2–0.5 μg.kg-1) and propofol (2–3 mg.kg-1). Mivacurium (0.2 mg.kg-1) or atracurium (0.5 mg.kg-1) was used for neuromuscular blockade. The intubation attempt was performed three minutes after injection of the neuromuscular blocking agent.
Outcome measurements
Our primary study objective was to determine whether there is a difference in intubation time (seconds) for the control compared to the channeled blade. The intubation time defined when the blade tip passed the incisors to the point until confirmation of the first wave of CO2 of the capnometer (Primus, Dräger, Lübeck, Germany). Additionally, two time points before final tracheal placement were evaluated: time to “glottic view” and time to “tube placement” after introducing the device into the oral cavity. “Glottic view” was defined from blade insertion until the best view on the glottis was achieved. “Tube placement” was defined as time from inserting the ETT until the tip of the tube disappeared between the vocal cords. Time was measured using the built-in stopwatch of the monitoring system (Philips® MX500, Philips GmbH, Hamburg, Germany).
Secondary outcomes were: first attempt and overall intubation success rates, visualization of the glottis using Cormack & Lehane grade (C&L; [13]) and percentage of glottic opening score in percent (POGO; [14]). External laryngeal manipulations like the BURP manoeuvre (backwards, upwards and rightwards pressure) were allowed to improve glottis view. Failed intubation was defined as: a) an elapsed intubation time of more than 120 s; b) failed tracheal placement of the tube; and c) removal of the device / repositioning from the oral cavity without advancing the tube. After each intubation, the anesthetist was asked to rate the degree of difficulty of intubation using a 5-point Likert scale (1 = very easy until 5 = very difficult; [15]) for each blade. Patient data (age, gender and BMI) were also documented.
Sample size and statistics
Sample size calculation was performed based on results from a previously published manikin study [16]. In this publication, participants needed an average time of 60 s (median) (range [11–60]) to ventilate using the control, compared to 20.5 s with the channeled blade (range [7.2–60]). Using these data for sample size calculation, a total of 46 patients were considered necessary to prove a local 5% level with power >90%. Data were tested using a Log-rank test. All recorded data were documented using a controlled evaluation sheet. Patients were randomized to treatment group using GraphPad QuickCalcs Web site: http://www.graphpad.com/quickcalcs/randmenu (accessed January 2015).
For statistical analysis, GraphPad Prism (Vers. 6.0 for MAC; GraphPad Software, San Diego, CA, USA) was used. Data were expressed as the median (range; interquartile range [IQR]) for non-Gaussian variables. A chi-squared test was used to compare the success rate. Comparisons the view of the glottis and the Likert-scale were analyzed by the Mann-Whitney U test. The differences were considered statistically significant if the p-value was less than 0.05.
Results
From February to March 2015, a total of 46 (control n = 23; channeled n = 23) adult patients eligible to participate in this study were included (Fig 1 and S3 File). No statistically relevant differences in patient demographics were found (Table 1; p>0.05). More residents with fewer than four years of clinical experience than anesthesia specialists participated in this study (p<0.001). The provider experience in anesthesia practice was comparable between the two groups. (p = 0.82).
Success rate and intubation time
All intubation attempts were successful with a maximum of two attempts and were completed within the time limit of 120 s. Correct endotracheal placement of the control blade was successful at the first attempt in 23/23 (100%) patients, compared to 22/23 patients with the channeled blade (96%; p = 0.31).
The overall time needed for first ventilation was shorter with the control 40 s [24–58], compared to the channeled 59 s [40–74] (p = 0.03).
Time to view with 9 s [6–11] was significantly shorter with control (p<0.001). However, there were no differences between time to place with control 26 s [13–49], compared with channeled 44 s [21–54] (p = 0.21). Fig 3 shows the chronological sequence of the time points evaluated.
Fig 3. Time sequnce of intubation.
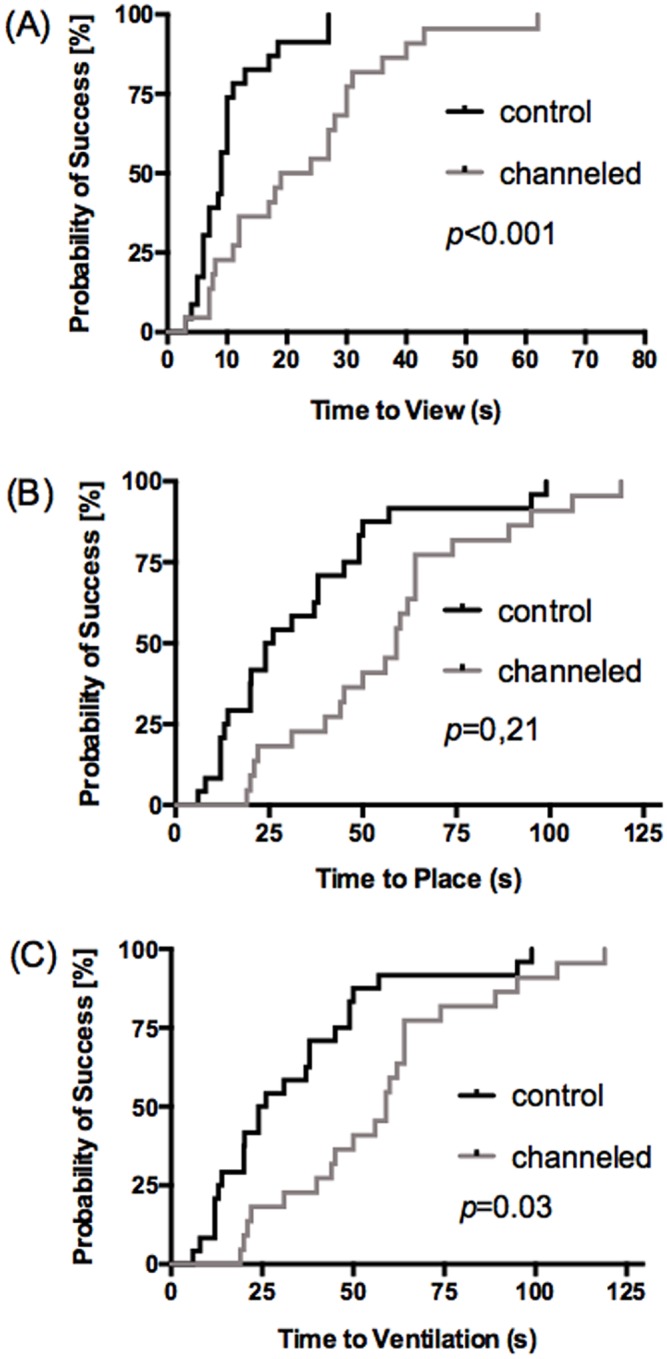
Time steps of (A) differences in Time to view (B) differences in Time for place the TT (C) differences in overall intubation time; Data are given in Kaplan-Meier curve and median.
Visualization of the glottis
Glottic view was excellent in both groups: control C&L I [I], POGO 100% [100] and channeled C&L I [I] (p = 0.48), POGO 100% [100] (p = 0.55).
Subjective assessment of blades
Using the 5-point Likert-Scale, no differences between groups were observed. The degree of difficult intubation was evaluated with the control as 2 (easy) and with the channeled as 3 (moderate) (p = 0.05).
Discussion
In the present study, a faster intubation time using a curved video laryngoscopic blade was found in a group of 46 patients. Using a similar shaped laryngoscope blade with a tube-guiding channel did not have any advantages compared to a similar blade without the channel. In this trial, intubation success rate, visualization of the glottis and subjective assessment were in this trial comparable between groups. So far, most studies have compared the King Vision with other makes of VL or the traditional Macintosh laryngoscope [16–22].
Patient demographics and provider data were comparable to other studies investigating the King Vision [16,19–21,23]. The success rate in this trial was higher than in two other studies comparing control with channeled blades or with other video laryngoscopes, but still lay within the range of the published data [14,18–20,23]. In this one failed case the performer had an anesthesia experience of 13 months and 15 video laryngoscopic intubations prior to the study. The examination of the patient showed no predictors for a difficult airway (Mallampati class I, thyromental distance > 6.5 cm). The laryngeal view was rated C&L grade II and with a POGO of 20%. Using the channeled-blade the ETT moved towards the right part of the larynx and could not be steered towards the vocal cords. After the intubation time limit of 120 seconds was reached the intubation attempt was stopped.
Overall, intubation success rate for the KV VL, varies in several studies and ranges from 51% to 100% [17, 18, 19, 20]. In one study comparing channeled King Vision with non-channeled and Macintosh blade, the overall success rate of intubation was better with the channeled (87%), compared to the non-channeled blade (47%) [16]. In several studies, most of the participants were paramedics or registered nurses with practical video laryngoscopy experience of less than 10 uses [17,19,22,23]. The study setting in these publications was also different in subjects (manikin or human cadaver vs. alive patients) and in the study setting (pre-hospital setting with anticipated difficult airway) [17,22,23]. We speculate that previous experience with laryngoscopy and especially other types of non-channeled video laryngoscopes results in a better success rate. Additionally, stylet use has been reported to increase the success rate with video laryngoscopy.
The primary endpoint of this study was evaluation of the time for first ventilation confirmed by the first CO2-wave on the capnometer. Most studies cannot be compared because the definition of “intubation time” varies. In two studies, the intubation time with the channeled blade was 20.1 s [20] compared to 25 s [17] evaluated in a manikin. The time required in adult patients was in median 38 s when using a channeled blade [20]. In one study comparing both KV blades in a manikin, the time for first ventilation with the non-channeled blade was 60 s [11]. The measurements differ between these two studies from taking hold of the handle of the device until confirmation of adequate lung ventilation [16] and the time stops when the cuff of the ETT is inflated [23]. Both studies used a manikin (Laerdal, Skill Trainer), which is suitable to evaluate and practice with a novel device since the airway is controlled (i.e. mouth already open, spacious mouth cavity, epiglottis fixed in the pharynx). It is likely that the intubation time in human patients undergoing general anesthesia in which anatomy varies is prolonged. Time for first ventilation was prolonged using the channeled blade in this study, presumably because advancing the tube meant that the tip did not follow the line of the blade (Fig 4B). The tube contains the channel and drifted towards the right arytenoid. Because of this deviation, it was necessary to correct the position of the blade multiple times until it was possible to advance the tube through the glottis. Based on the manufacturer`s instructions, the blades allows either a Macintosh blade-like technique (Fig 4A) to position the tip of blade in the vallecula or a Miller blade-like technique (the blade tip passes underneath the laryngeal surface of the epiglottis) to be used successfully. In order to achieve optimal intubation technique, it is recommended to position the KV blades with the tip in the vallecula (Macintosh blade-like technique). In this trial, a Macintosh-approach was also used. However, we observed that inexperienced participants initially positioned the tip of the channeled blade too deep in the airway, which resulted in uploading of the epiglottis (Miller blade-like position). In this position, steering of the tube towards the glottis was nearly impossible because the channel of the blade restricted tube movement.
Fig 4. Insertion technique and view.
(A) typical Macintosh-blade technique: blade tip placed in the vallecula (B) view from the monitor display using the channeled blade (★: epiglottic; ✪: ET leave the channeled; ✹: right arytenoid).
The Miller blade-like technique, with an upload of the epiglottis, results in difficult handling when directing the ETT opposite the glottis. This might influence the longer time taken for intubation with the control or channeled blade compared with other published results.
It is generally thought that the learning curve for video laryngoscopy is steep. A minimum of 10 uses is necessary to improve the success rate or intubation time with the C-MAC™ Macintosh-blade (Karl Storz, Tuttlingen, Germany), McGrath Series 5 (Aircraft Medical, Edinburgh, UK) and GlideScope™ Ranger (Verathon, Bothell, USA) [23–25]. Comparative studies analysed other tube-guiding blades like the Airtraq™ (Prodol Meditec S.A., Vizcaya, Spain) or the Pentax™ AWS® (Hoya Corporation, Tokyo, Japan), presenting different results between 5–50 applications until a success rate >80% is achieved [8,26,27]. This skill level of the operator determines the efficacy of success intubation. Also, training and experience using manikins alone does not enable the optimized use of any device, even when experienced airway specialists considered the training sufficient. Significant clinical experience was proposed before using Airtraq channeled blades in an emergency intubation setting [23]. In a recent study, a significantly higher number of 76 uses were documented for the GlideScope VL to master its use, indicating that the learning curve might be flatter than originally thought [28]. The first-pass success rate using highly curved blades ranges between 74 and 96% [25,27,29,30]. There are two typical difficulties of the ETT placement. One is that the tongue interferes with the advancing of the ETT, while the second is that the high curvature of the blade typically makes it virtually impossible to obtain a direct view of the glottis. To overcome the high curvature of the blade with an ETT, a malleable stylet might be necessary to shape the ETT according to the blade shape for VL with hyper-angulated blades. However, using a stylet bears the risk of causing airway injury, especially to the soft tissue of the pharynx [31,32]. A current method is to shape the ETT at 60 to 90 degrees at the distal curvature and rotate the ETT after passing the vocal cords by about 180 degrees down and forward [33,34]. This feature could prolong the intubation time and reduce the intubation success. Because of potential risk of upper airway injury, it is important to advance the ETT beyond the uvula under direct vision before directing one’s attention to the video monitor [12].
When comparing the visualization of the glottis, we found no differences between the control and the channeled blade using the Cormack & Lehane scoring system and POGO-score. These findings are similar to one manikin study, which evaluated a C&L grade I (86%), II (14%) and best view of the glottis entrance from 100% by a rate of 27 [23]. This was an expected result in this trial since both blades examined are curved blades, with the only difference being that the tube is pre-loaded in the channeled blade.
Based on subjective judgement, after completing the study, the participants rated the use of the control as very easy to easy and the channeled blade as easy to moderate. Our findings are contrary to another manikin study, in which the control was rated from difficult to very difficult [11]. In contrast to this study, participants were registered nurses without a high level of expertise in tracheal intubation. A reason for preferring a channeled blade might be that preloading of the ETT makes it easier for more unexperienced providers to guide both the tube and the blade tip towards the glottis. The intraoral space created by laryngoscopy with a curved blade might be limited and additional manipulation with the ETT loaded on a stylet might be more difficult. Thus, this might contribute to a higher Likert Scale score. The reason for this subjective rating in this study might be the high pre-existing experience with video laryngoscopy using curved blades without a guidance channel.
There are several limitations in our study. First, advancing the tip of the channeled blade too far towards the glottis might not leave enough space to allow directing the tip of the ETT through the glottis. Second, this trial might be limited by the heterogeneous experiences of the providers (e.g. experiences in anesthesia practice and in video laryngoscopy technique). Some providers had a high level of expertise, which might have influenced the results of this trial. Most of the participants had a higher experience using the video laryngoscopy with a non-channeled blade and a stylet with angulated hockey stick tip to insert the ETT into the glottis. Third, the standardized tube size of this trial could result in a limited generalizability for the intubation time when a larger tube size is used. Until recently, the use of a nerve stimulator to confirm sufficient neuromuscular blockade was not standardized in the study center. Because of the design of this trial, the protocol did not allow blinding of the operators using the different blades. Finally, only one VL with a hyper-angulated blade was used. The KV is the only device that uses the same type of angulated blade for channeled and non-channeled. Consequently, this device was evaluated to compare channeled vs. non-channeled blades.
Conclusion
Practitioners with experience in clinical practice and the technique of video laryngoscopy facilitated tracheal intubation without any esophageal intubation. We found for the primary endpoint, that a curved video laryngoscopic blade was superior in intubation time compared to a curved blade using a tube-guiding channel. The use of a VL with tube-guiding channels does not optimize the performance of the tracheal intubation of anesthesiologists in a controlled environment.
Supporting information
(DOC)
(DOCX)
(XLS)
Acknowledgments
The authors wish to thank Irene Schmidtman (Institute of Medical Biostatistics, Epidemiology and Informatics, University Medical Center of the Johannes Gutenberg-University, Mainz, Germany). Presented in parts as poster at the German National Congress of Anesthesiologists April 2016, Leipzig, Germany.
Abbreviations
- ASA
American Society of Anesthesiologists
- BMI
Body Mass Index
- BURP
Backward upward rightward pressure
- channeled
King Vision channeled blade
- control
King Vision non-channeled blade
- EMS
Emergency Medical Service
- ENT
Department of Ear, Nose, Throat, Neck & Head surgery
- ETT
Endotracheal tube
- VL
Video laryngoscope
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Cobas MA, De la Pena MA, Manning R, Candiotti K, Varon AJ. Pre-hospital intubations and mortality: a level 1 trauma center perspective. Anesth and Analg. 2009;109:489–93. [DOI] [PubMed] [Google Scholar]
- 2.Konrad C, Schupfer G, Wietlisbach M, Gerber H. Learning manual skills in anaesthesiology: Is there a recommended number of cases for anaesthetic procedures? Anesth Analg. 1998;86:635–39. [DOI] [PubMed] [Google Scholar]
- 3.Sakles JC, Chiu S, Mosier J, Walker C, Stolz U. The importance of first pass success when performing orotracheal intubation in the emergency department. Acad Emerg Med. 2013;20:71–78. doi: 10.1111/acem.12055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Garza AG, Gratton MC, Coontz D, Noble E, Ma OJ. Effect of paramedic experience on orotracheal intubation success rates. J Emerg Med. 2003;25: 251–56. [DOI] [PubMed] [Google Scholar]
- 5.Mulcaster JT, Mills J, Hung OR, MacQuarrie K, Law JA, Pytka S, et al. Laryngoscopic intubation: learning and performance. Anesthesiology. 2003; 98: 23–27. [DOI] [PubMed] [Google Scholar]
- 6.Wang HE P A, Cassidy L, Adelson D, Yealy D. Out-of-hospital endotracheal intubation and outcome after traumatic brain injury. Ann Emerg Med. 2004;44: 439–50. doi: 10.1016/S0196064404004160 [DOI] [PubMed] [Google Scholar]
- 7.Savoldelli GL, Schiffer E, Abegg C, Baeriswyl V, Clergue F, Waeber JL. Learning curves of the Glidescope, the McGrath and the Airtraq laryngoscopes: a manikin study. Eur J Anaesth. 2009;26:554–58. [DOI] [PubMed] [Google Scholar]
- 8.Maharaj CH, Costello JF, Higgins BD, Harte BH, Laffey JG. Learning and performance of tracheal intubation by novice personnel: a comparison of the Airtraq and Macintosh laryngoscope. Anaesthesia. 2006;61:671–77. doi: 10.1111/j.1365-2044.2006.04653.x [DOI] [PubMed] [Google Scholar]
- 9.Cavus E, Bein B, Dörges V. Airwaymanagement: video-assisted airway management. AINS. 2011;46:588–96. doi: 10.1055/s-0031-1286611 [DOI] [PubMed] [Google Scholar]
- 10.Jones PM, Turkstra TP, Armstrong KP, Armstrong PM, Cherry RA, Hoogstra J, Harle CC. Effect of stylet angulation and endotracheal tube camber on time to intubation with the GlideScope. Can J Anaesth. 2007;54:21–7. [DOI] [PubMed] [Google Scholar]
- 11.Cavus E, Neumann T, Doerges V, Moeller T, Scharf E, Wagner K, et al. First clinical evaluation of the C-MAC D-Blade videolaryngoscope during routine and difficult intubation. Anesth Analg. 2011;112:382–85. doi: 10.1213/ANE.0b013e31820553fb [DOI] [PubMed] [Google Scholar]
- 12.van Zundert A, Pieters B, van Zundert T, Gatt S. Avoiding palatopharyngeal trauma during videolaryngoscopy: do not forget the "blind spots". Acta Anesthesiol Scand. 2012;56:532–4. [DOI] [PubMed] [Google Scholar]
- 13.Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia. 1984;39:1105–11. [PubMed] [Google Scholar]
- 14.Levitan RM, Ochroch EA, Kush S, Shofer FS, Hollander JE. Assessment of airway visualization: validation of the percentage of glottic opening (POGO) scale. Acad Emerg Med. 1998;5:919–23. [DOI] [PubMed] [Google Scholar]
- 15.Weiss M, Schwarz U, Gerber AC. Difficult airway management: comparison of the Bullard laryngoscope with the video-optical intubation stylet. Can J Anesth. 2000;47:280–4. doi: 10.1007/BF03018927 [DOI] [PubMed] [Google Scholar]
- 16.Akihisa Y, Maruyama K, Koyama Y, Yamada R, Ogura A, Andoh T. Comparison of intubation performance between the King Vision and Macintosh laryngoscopes in novice personnel: a randomised, crossover manikin study. J Anesth. 2014;28:51–57. doi: 10.1007/s00540-013-1666-9 [DOI] [PubMed] [Google Scholar]
- 17.Murphy LD, Kovacs GJ, Reardon PM, Law JA. Comparison of the king vision video laryngoscope with the Macintosh laryngoscope. J Emerg Med. 2014;47: 239–46. doi: 10.1016/j.jemermed.2014.02.008 [DOI] [PubMed] [Google Scholar]
- 18.Jarvis JL, McClure SF, Johns D. EMS Intubation Improves with King Vision Video Laryngoscopy. Prehosp Emerg Care. 2015;19:482–89. doi: 10.3109/10903127.2015.1005259 [DOI] [PubMed] [Google Scholar]
- 19.Burnett AM, Frascone RJ, Wewerka SS, Kealey SE, Evens ZN, Griffith KR, et al. Comparison of success rates between two video laryngoscope systems used in a pre-hospital clinical trial. Prehosp Emerg Care. 2014;18:231–38. doi: 10.3109/10903127.2013.851309 [DOI] [PubMed] [Google Scholar]
- 20.Alvis BD, Hester D, Watson D, Higgins M, St Jacques P. Randomized controlled trial comparing the McGrath MAC video laryngoscope with the King Vision video laryngoscope in adult patients. Minerva anestesiol. 2016;82:30–35. [PubMed] [Google Scholar]
- 21.Ali QE, Amir SH, Jamil S, Ahmad S. A comparative evaluation of the Airtraq and King Vision video laryngoscope as an intubating aid in adult patients. Acta anaesthesiol Belg. 2015;66:81–85. [PubMed] [Google Scholar]
- 22.Yun BJ, Brown CA 3rd, Grazioso CJ, Pozner CN, Raja AS. Comparison of video, optical, and direct laryngoscopy by experienced tactical paramedics. Prehosp emerg care. 2014;18:442–445. doi: 10.3109/10903127.2013.864356 [DOI] [PubMed] [Google Scholar]
- 23.Ruetzler K, Imach S, Weiss M, Haas T, Schmidt AR. Comparison of five video laryngoscopes and conventional direct laryngoscopy: Investigations on simple and simulated difficult airways on the intubation trainer. Anaesthesist. 2015; 64:513–19. doi: 10.1007/s00101-015-0051-5 [DOI] [PubMed] [Google Scholar]
- 24.Kaplan MB, Hagberg CA, Ward DS, Brambrink A, Chhibber AK, Heidegger T, et al. Comparison of direct and video-assisted views of the larynx during routine intubation. J Clin Anesth. 2006;18:357–62. doi: 10.1016/j.jclinane.2006.01.002 [DOI] [PubMed] [Google Scholar]
- 25.Piepho T, Weinert K, Heid FM, Werner C, Noppens RR. Comparison of the McGrath® Series 5 and GlideScope® Ranger with the Macintosh laryngos-scope by paramedics. Scand J Trauma Resusc Emerg Med. 2011;19:4 doi: 10.1186/1757-7241-19-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Trimmel H, Kreutziger J, Fertsak G, Fitzka R, Dittrich M, Voelckel WG. Use of the Airtraq laryngoscope for emergency intubation in the pre-hospital setting: a randomized control trial. Crit Care Med. 2011;39:489–93. doi: 10.1097/CCM.0b013e318206b69b [DOI] [PubMed] [Google Scholar]
- 27.Malik MA, Subramaniam R, Maharaj CH, Harte BH, Laffey JG. Randomised controlled trial of the Pentax AWS, Glidescope, and Macintosh laryngoscopes in predicted difficult intubation. Br J Anaesth. 2009;103:761–68. doi: 10.1093/bja/aep266 [DOI] [PubMed] [Google Scholar]
- 28.Cortellazzi P, Caldiroli D, Byrne A, Sommariva A, Orena EF, Tramacere I. Defining and developing expertise in tracheal intubation using a GlideScope® for anaesthetists with expertise in Macintosh direct laryngoscopy: an in-vivo longitudinal study. Anaesthesia. 2015;70:290–95. doi: 10.1111/anae.12878 [DOI] [PubMed] [Google Scholar]
- 29.Silverberg MJ, Li N, Acquah SO, Kory PD. Comparison of video laryngoscopy versus direct laryngoscopy during urgent endotracheal intubation: a randomised controlled trial. Crit Care Med. 2015;43:636–41. doi: 10.1097/CCM.0000000000000751 [DOI] [PubMed] [Google Scholar]
- 30.Piepho T, Fortmueller K, Heid FM, Schmidtmann I, Werner C, Noppens RR. Performance of the C-MAC video laryngoscope in patients after a limited glottic view using Macintosh laryngoscopy. Anaesthesia. 2011;66:1101–05. doi: 10.1111/j.1365-2044.2011.06872.x [DOI] [PubMed] [Google Scholar]
- 31.van Zundert A, Maassen R, Lee R, Willems R, Timmerman M, Siemonsma M, et al. A Macintosh laryngoscope blade for videolaryngoscopy reduces stylet use in patients with normal airways. Anesth Analg. 2009;109:825–31. doi: 10.1213/ane.0b013e3181ae39db [DOI] [PubMed] [Google Scholar]
- 32.Maassen R, Lee R, Hermans B, Marcus M, van Zundert A. A comparison of three videolaryngoscopes: the Macintosh laryngoscope blade reduces, but does not replace, routine stylet use for intubation in morbidly obese patients. Anesth Analg. 2009;109:1560–65. doi: 10.1213/ANE.0b013e3181b7303a [DOI] [PubMed] [Google Scholar]
- 33.Cooper RM, Pacey JA, Bishop MJ, McCluskey SA. Early clinical experience with a new videolaryngoscope (GlideScope) in 728 patients. Can J Anaesth. 2005;52:191–98. [DOI] [PubMed] [Google Scholar]
- 34.Noppens RR, Werner C, Piepho T. Indirect laryngoscopy: Alternatives to securing the airway. Anaesthesist. 2010;59:149–61. doi: 10.1007/s00101-009-1656-3 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(DOCX)
(XLS)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.