Abstract
Background
Nasopharyngeal carcinoma (NPC) is endemic in China and patient self-management is poor. Minorities may suffer from psychological problems during treatments for NPC. This study aimed to implement an intervention to promote self-efficacy of minority patients (Zhuang tribe, Guangxi, China) with NPC to improve their quality of life (QOL).
Material/Methods
This was a prospective study of 120 patients with NPC treated at the First Affiliated Hospital of Guangxi Medical University (Guangxi, China), randomized to conventional care (n=60, controls) or conventional care plus self-efficacy interventions based on health education, behavior therapy, and psychological intervention (n=60, self-efficacy group). Self-efficacy was evaluated using the general self-efficacy scale, and QOL using the EORTC QLQ-C30. The questionnaires were completed at discharge, at 6 months, and at 1 and 2 years. The primary outcome was QOL.
Results
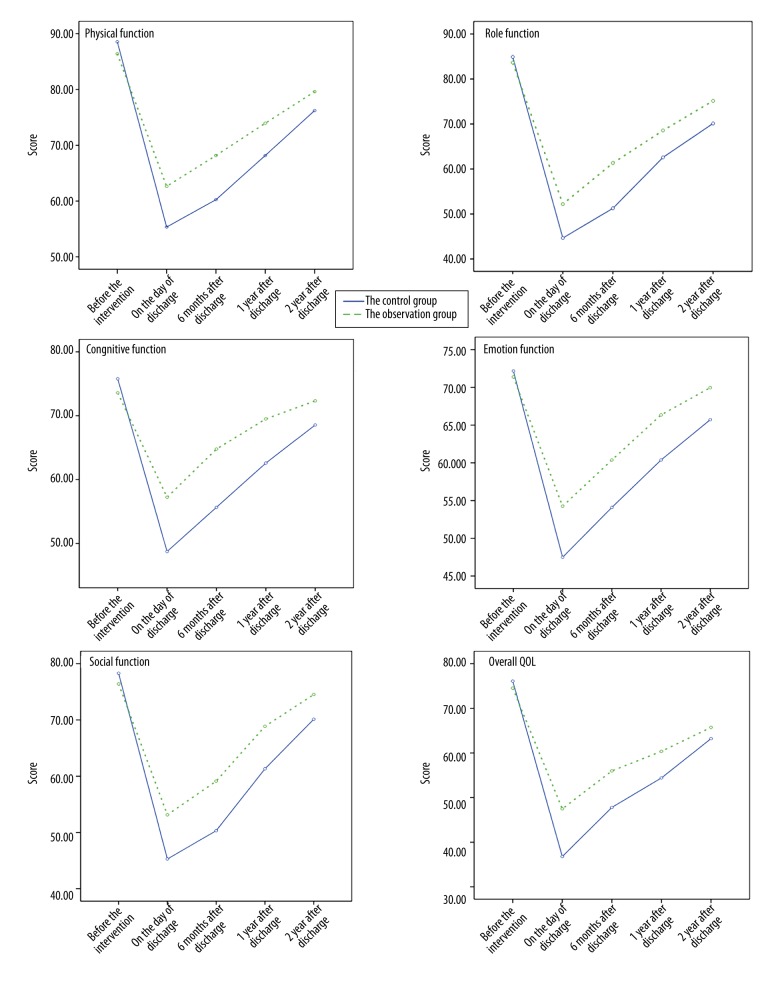
There was no difference in QOL at baseline. From study start to hospital discharge, overall QOL scores decreased in both groups, but this decrease was more important in the control group (controls: −39.31 vs. self-efficacy: −27.04, P<0.05). After discharge, each functional field QOL scores and overall QOL increased with time in the 2 groups, and they were significantly higher in the self-efficacy group.
Conclusions
This intervention promoting self-efficacy could increase patients’ own potential and initiative, enhance their confidence and ability to solve health problems, improve their coping with adverse effects of treatments, and have positive effects on their QOL. Self-efficacy theory-based interventions could be worth popularization during the treatment and recovery of minority patients with NPC.
MeSH Keywords: Nasopharyngeal Diseases, Quality of Health Care, Self Efficacy
Background
Nasopharyngeal carcinoma (NPC) represents the majority of epithelial malignancies of the head and neck [1]. In the United States, the incidence of the disease is 16.6 per 100,000 non-Hispanic Caucasian men and 6.3 per 100,000 non-Hispanic Caucasian women [2]. NPC is particularly endemic in southern China, with Guangdong being the province with the highest prevalence, followed by Guangxi (annual incidence of 15–25 cases per 100,000 people) [3].
Because of the anatomic location and high radio-sensitivity of the disease, radiotherapy is the recommended treatment for NPC [4], achieving high curative rates for patients with early stage cancer. Nevertheless, because of socio-economical characteristics (low income, low education, lack of health-related knowledge) and because symptoms are not always obvious, many patients with NPC are diagnosed at the locally advanced stage, and these patients are rarely treated with radiotherapy alone [4,5]. In these patients, radiotherapy combined with chemotherapy is considered the optimal treatment [4,6,7]. Chemoradiation treatment is associated with significant toxicity and acute radiation reactions, leading to psychological mood changes and adverse effects such as nausea and vomiting, fatigue, oral mucositis, and radio-dermatitis [4,7,8]. These reactions may reduce the patients’ self-efficacy and seriously affect their physical and mental health, treatment compliance, and quality of life (QOL) [9,10].
Psychologist Albert Bandura first defined self-efficacy as one’s belief in one’s ability to succeed in specific situations or accomplish a task [11,12]. One’s sense of self-efficacy can play a major role in how one approaches goals, tasks, and challenges. The theory central to Bandura’s definition of self-efficacy is social cognitive theory, which emphasizes the role of observation learning and social experience in the development of personality. Self-efficacy is an individual’s judgment of his/her capabilities to organize and execute courses of action required to attain designated types of performance [13]. Self-efficacy is a cognitive process that is concerned with an individual’s beliefs that his/her actions can produce the outcomes that he/she desires. Self-efficacy values provide the foundation for many individual behaviors such as motivation, well-being, and personal accomplishment [11–13]. It has been suggested that self-efficacy interventions could make patients better cope with the disease and the side effects of the treatments, leading to improved treatment compliance, physical and mental health, and QOL [10,14], but no study has specifically evaluated the effect of self-efficacy interventions (such as a combination of health education, behavior therapy, and psychological intervention) on QOL in patients with NPC. Previous studies showed that the self-efficacy level is low in patients with NPC [15,16]. The analysis of the factors influencing self-efficacy in different settings shows that self-efficacy levels are highly correlated with coping styles, depression, economic conditions, educational level, knowledge, and skills [17–21].
Guangxi, also named Guangxi Zhuang Autonomous Region, contains 11 ethnic minorities. Among them, the Zhuang people is the largest group, with about 15 million, accounting for 32.9% of the total population in Guangxi. They have their own language and about 42% of the Zhuang people are monolingual in Zhuang. Compared with the other provinces in China, Guangxi has a higher proportion of farmers, a low educational level, poor awareness of seeking medical help, inability of understanding certain diseases, and lack of health care common knowledge. Since the Zhuang people shows a high prevalence of depression, poor economic conditions, and low educational level [22], specific interventions might be needed for this population [23]. Self-efficacy is the most influential factor of an individual’s potential; it is not stable with personality characteristics, but variable according to the psychological characteristics that are closely related to specific situations. It can be improved by learning and interventions. Studies have shown that self-efficacy can be well established and developed using psychological factors, knowledge and skills, social and family support, and improvement of health status [13].
Therefore, the aim of this study was to design and implement an intervention promoting self-efficacy for patients with NPC from the Zhuang people in Guangxi (China) and to observe the changes in QOL in these patients.
Material and Methods
Study design
This was a prospective randomized open-label study carried out in 120 patients with NPC treated with radiotherapy at the First Affiliated Hospital of Guangxi Medical University between October 2012 and August 2013. This study was approved by the ethical committee of the First Affiliated Hospital of Guangxi Medical University. The patients were told of the study after they were diagnosed with NPC, during treatment planning. The patient was orally described the study and the intervention and the investigators answered all questions. All patients provided a written informed consent.
Patients
Inclusion criteria were: 1) Zhuang tribe; 2) NPC confirmed by histopathological examination based on standard criteria [24]; 3) no history of chemoradiation therapy; 4) 18–75 years of age; 5) Karnofsky Performance Status (KPS) ≥70; 6) no history of mental disorders and conscious disturbance; and 7) understood the study, willing to participate, and signed the informed consent form. Exclusion criteria were: 1) patients treated for recurrent disease at study screening; or 2) received radiotherapy only.
Randomization
Patients were randomized 1: 1 to the control or intervention group, 60 patients per group. Sealed envelopes were prepared by an independent statistician. Envelopes were opened sequentially upon recruitment. Patients from the 2 groups were housed on 2 different floors of the radiotherapy ward to avoid interference and biases. There was no blinding.
Cancer treatments
All patients received concurrent chemoradiation therapy. Irradiation was mainly performed using 6–10 MV photons and electrons from linear accelerators. Intensity-modulated radiation therapy (IMRT) was given according to the details presented in Table 1. All patients received concurrent chemotherapy during radiotherapy or neoadjuvant chemotherapy followed by concurrent chemotherapy during radiotherapy. All patients were hospitalized during their treatments. Details are presented in Table 1. Because cancer therapy affects QOL, all treatment parameters were controlled in order to avoid a bias introduced by different treatments.
Table 1.
Radiotherapy and chemotherapy given to the patients with NPC.
| Treatment | Details |
|---|---|
| Radiotherapy |
|
| Neoadjuvant chemotherapy | Cisplatin–based concurrent chemotherapy, mainly with 80–100 mg/m2 on days 1–2 every 3 weeks, for 2–3 cycles |
| Concurrent chemotherapy | Two cycles of DF (cisplatin [25 mg/m2 on days 1–3] and 5–fluorouracil [750 mg/m2 on days 1–5]) |
Defined as the gross tumor volume of the nasopharynx +5–10 mm margin, and the range depended on the adjacent texture characteristic, including pharyngonasal cavity mucosa and submucosal 5 mm;
defined as the area that the NPC might extend to, including skull base, the posterior ethmoid sinus, sphenoid sinus bottom, the posterior third of the nasal cavity, pterygoid process, pterygopalatine fossa, parapharyngeal space, retropharyngeal space, and the size of the negative regional lymph nodes.
Self-efficacy evaluation
The general self-efficacy scale was used to measure patients’ self-efficacy levels [25]. A Chinese version was developed and validated [26,27]. Cronbach’s α is 0.87, test-retest reliability is 0.83 after 10 days, and split-half reliability is 0.90. There are 10 items in the scale, scored 1–4, for total scores of 10–40. Higher scores indicate better self-efficacy.
Conventional care
Both groups received conventional treatment care according to the standards of the radiotherapy department. It consisted of education given at irregular intervals and that included knowledge about health, nutrition, and psychology, and explanations provided at any time while the patients or their families had any questions. The health education was given orally, not following any specific pattern. The patients did not receive any special educating handbooks, no multimedia teaching, and no psychological evaluation. For the behavior intervention, the patients were only told to do mouth exercises, nasal cleaning, and oral gargle. There was no surveillance or outcome evaluation. Psychological guidance was given by nurses, but there was no psychological evaluation, lecturing, or counseling with psychologists.
Intervention promoting self-efficacy
In addition to conventional treatment care, the self-efficacy group received an intervention promoting self-efficacy. This intervention was designed to play on all 4 of the major sources of one’s efficacy: performance accomplishments, vicarious learning, verbal encouragement, and physiological and affective states [11–13,28]. An oncology nurse led the multidisciplinary team, which included 3 oncology experts, 4 nurses, and one psychologist. According to previous results of factors influencing self-efficacy [28], this team designed and implemented an intervention promoting self-efficacy, which included a set of health education, behavior therapy, and psychological therapy focusing on disease knowledge, treatment knowledge, care, and self-efficacy. The specific contents of the study intervention were:
Health education: By distributing a self-made health education handbook (developed by 2 of the authors based on 2 books in Chinese, “Nasopharyngeal carcinoma” by Li Gao and “Radiation oncology” by Weibo Yin; the other authors reviewed the content of this handbook), the patients were given individual one-to-one education using a health education pathway (Figure 1) and collective multimedia teaching on a regular basis (once every 2 weeks). They were educated on the following knowledge: concept of disease, etiology, clinical manifestation, focal inspection items before treatment and matters needing attention, treatment plan, common adverse reactions and coping strategies, diet guidance, and discharge guidance. All of the above were to improve patients’ awareness of disease, treatment, and rehabilitation nursing knowledge, allow their potential and initiative, and improve their treatment compliance, ensuring the smooth implementation of the treatment.
-
Behavior therapy: The behavioral goals included: a) oral hygiene: upon rising, upon going to sleep, and every time after eating, the patients were asked to brush their teeth with a soft toothbrush or to rinse their mouth (gargling for 2–3 min) with warm boiled water or brackish water; the aim was to remove any food particles between the teeth, to clean the teeth, to maintain a good oral hygiene, and to prevent any secondary infection of the oral cavity; b) nasopharyngeal cleaning care: 3 times a day (morning, before radiotherapy, and before sleep), the patients were asked to wash the nasal cavity first with warm boiled water and then with weak brine, eliminating secretions of the mucosal surface; the aim was to reduce radiations reactions, to improve comfort, and to prevent or relieve the occurrence of sinusitis; and c) mouth exercises: the patients were asked to slowly open their mouth to the maximum, maintain it for 5 sec, and then to close it, for 2–3 min each time, 3–4 times per day; the aim was to prevent the occurrence of mouth movement difficulties.
According to these pre-set targets, a behavior contract was signed between the nurses and patients. All objectives were made clear between the patients and the nurses and were implemented in accordance with the requirements. Meanwhile, the completion status was recorded every day to reach the goals of self-monitoring and reinforcement in behavior. At the same time, researchers checked daily the completeness status of the targets, and gave confirmation and encouragements to the patients who completed their targets. Goal achievement was noted in the signed contract as a mean of further empowerment. To the ones not reaching the goals, the researchers analyzed the reasons with the patients, communicated with them every day and tried to find practical tips to overcome difficulties and to complete their behavior targets. In addition, the rehabilitation nursing skills needed to be mastered and exercised persistently by the patients were divided into several small and easy goals. The goal was that the patients had a constant successful experience while completing the targets in order to enhance self-efficacy.
Psychological intervention: The nurses established a good relationship with the patients, won the trust of the patients and their family, assessed the timely psychological status of the patients using validated Chinese versions of the self-rating depression scale (SDS) [29], guided the patients to express their opinion and requirements about diagnosis, treatment, nursing, and prognosis, and answered patients’ questions with patience, making the patients face their disease with the right and best attitude. Patients were evaluated by psychologists every 2 weeks. For patients with serious depressive symptoms, psychologists were asked to provide counseling and treatment.
Figure 1.
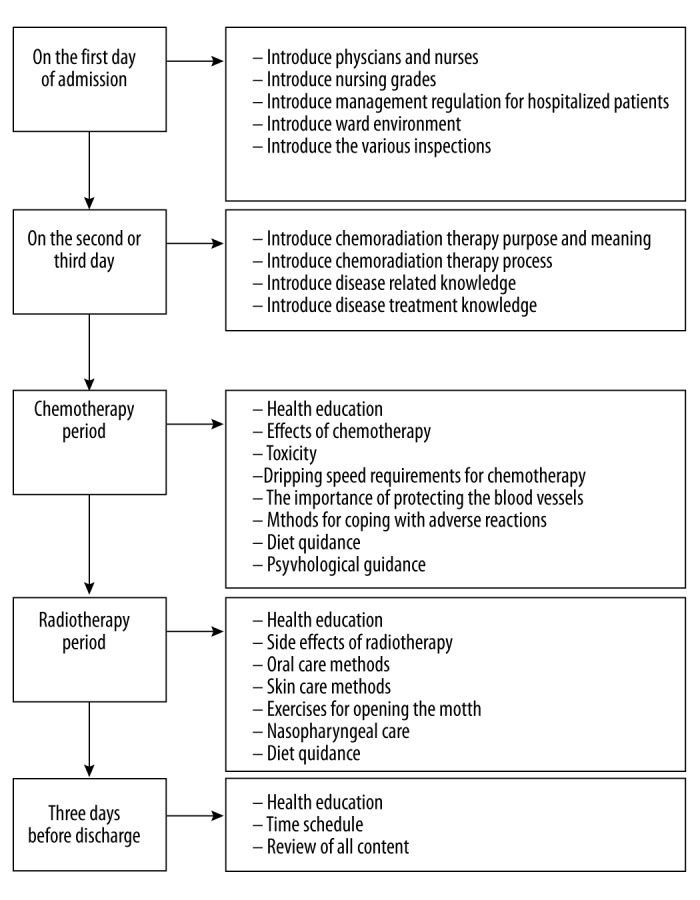
Health education pathway for NPC in the self-efficacy group.
Evaluation indicators
European organization for research and treatment of cancer QOL questionnaire (EORTC QLQ-C30) [30]: A Chinese version of the EORTC QLQ-C30 was used to assess the QOL [31], which showed good reliability, validity, and sensitivity. It includes 30 items encompassing 15 areas, 5 functional fields (physical, role, cognitive, emotion, and social function), 3 symptom domains (fatigue, pain, and nausea and vomiting), and one overall health condition (QOL) field. The overall health condition (QOL) field includes 7 grades that can be scored 1 to 7 points. The other items are divided into 4 grades (none, less, more, and many), scored 1 to 4 points. Higher scores indicate better functional condition and QOL.
Follow-up
The patients were recruited when they received their NPC treatments, i.e. between October 2012 and August 2013. They were subsequently followed up for 2 years, i.e. at discharge, 6 months, 1 year, and 2 years. The last follow-up for the last patient was in August 2015.
Data collection
All study staff were required to be trained and to fully understand the study scheme. All patients filled the questionnaires with unified guidance language, or their families could help to answer if they had difficulties. All patients also completed the questionnaires at discharge, and 6 months, 1 year, and 2 years after discharge. All questionnaires were checked item-by-item immediately after completion and the patients were asked immediately to correct mistakes or unanswered questions. Baseline data were collected after signing the informed consent and prior to any study intervention. Data was entered into the database by one researcher. All data were validated by a second independent researcher.
Outcomes
The primary outcome was the change in QOL over time. The secondary outcome was the change in self-efficacy over time.
Statistical analysis
Data was analyzed as in a per protocol fashion. SPSS 13.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. Continuous data was presented as mean ± standard deviation and analyzed using the Student t test, repeated measure ANOVA or Friedman M test, as appropriate. Categorical data was presented as frequencies and analyzed using the Fisher exact test. Two-sided P-values <0.05 were considered statistically significant.
Results
Characteristics of the patients
Fifty-three patients from the control group and 53 from the self-efficacy group completed the 2-year study. Thirty-two patients (15 from the control group and 17 from the self-efficacy group) received radiotherapy and concurrent chemotherapy. Seventy-four patients (38 from the control group and 36 from the self-efficacy group) first received 2 cycles of neoadjuvant chemotherapy, then received radiotherapy with concurrent chemotherapy. Over the first year after discharge, 3 patients were lost to follow-up and 2 patients had a recurrence in the control group; 3 patients had a recurrence in the self-efficacy group. Over the second year after discharged, 2 patients had a recurrence in the control group and 4 patients had a recurrence in the self-efficacy group.
Table 2 presents the characteristics of the patients. There were no significant differences in age, sex, income, pathological type, clinical stage, or treatment plan between the 2 groups (all P>0.05).
Table 2.
Characteristics of the patients.
| Controls | Self-efficacy | P | |
|---|---|---|---|
| N | 53 | 53 | |
|
| |||
| Sex | 0.824 | ||
| Female | 13 | 14 | |
| Male | 40 | 39 | |
|
| |||
| Age (years) | 51.5 (20–68) | 52.1 (21–70) | 0.631 |
|
| |||
| Family monthly income | 0.993 | ||
| <¥ 800 | 18 | 18 | |
| ¥ 800–1500 | 15 | 16 | |
| ¥ 1500–3000 | 9 | 9 | |
| ¥ 3000–5000 | 7 | 6 | |
| >¥ 5000 | 4 | 3 | |
|
| |||
| Tumor differentiation | 0.978 | ||
| Moderate | 7 | 7 | |
| Poor | 18 | 19 | |
| Undifferentiated | 28 | 27 | |
|
| |||
| Clinical stage | 0.821 | ||
| I | 6 | 4 | |
| II | 9 | 10 | |
| III | 28 | 26 | |
| IV | 10 | 13 | |
|
| |||
| Treatment approach | |||
| Chemotherapy | 0.672 | ||
| Neoadjuvant + concurrent chemotherapy | 38 | 36 | |
| Concurrent chemotherapy | 15 | ||
| Radiotherapy | 17 | 1.000 | |
| Intensity-modulated radiation therapy | 53 | 53 | |
Self-efficacy
Table 3 presents the self-efficacy results. There was no difference in self-efficacy at baseline (P=0.814), but self-efficacy was significantly higher in the self-efficacy group compared with controls at all time points during the intervention (all P<0.001). In addition, self-efficacy decreased over time in controls (P<0.001), while self-efficacy increased in the self-efficacy group compared with baseline (P<0.001).
Table 3.
Comparison of self-efficacy and depression symptoms between the two groups before and during radiotherapy.
| Group | Before | During radiotherapy | ||
|---|---|---|---|---|
| Days 1 to 10 | Days 11 to 20 | Days >21 | ||
| Self-Efficacy | ||||
| Controls (n=53) | 27.6±4.3 | 27.0±3.2 | 25.2±3.6 | 24.3±3.3 |
| Self-efficacy (n=53) | 27.4±4.6 | 29.6±3.2 | 28.7±2.7 | 29.3±2.7 |
| P | 0.814 | <0.001 | <0.001 | <0.001 |
| SDS | ||||
| Controls (n=53) | 46.3±5.5 | 50.5±4.9 | 58.3±4.5 | 63.2±6.9 |
| Self-efficacy (n=53) | 46.8±5.2 | 48.1±4.8 | 53.9±4.8 | 58.9±4.4 |
| P | 0.444 | <0.001 | <0.001 | <0.001 |
Depression
There was no difference in depression between the 2 groups at baseline (P=0.444) (Table 3). During the intervention, the SDS score gradually increased in both groups (P<0.001), indicating increasing depression symptoms, but the self-efficacy group had lower scores at all time points (all P<0.001).
Improvement of quality of life over time
Figure 2 presents the longitudinal QOL results. There was no difference in QOL at baseline (all P>0.05) (Figure 2). During the 2-year study, the QOL improvement became significantly different between the 2 groups. From the start of study to hospital discharge, QOL scores decreased in both groups, but this decrease was more important in the control group (overall QOL: controls: −39.31 vs. self-efficacy: −27.04, P<0.05). After discharge, each functional field QOL scores and overall QOL increased with time in the 2 groups (Figure 2). The QOL in the self-efficacy group remained significantly higher over time than in the control group (all P<0.05).
Figure 2.
Changes in time in indicators of QOL between the 2 groups.
Compared with controls, the intervention promoting self-efficacy improved physical function (P=0.004), role function (P=0.03), cognitive function (P=0.03), emotion function (P=0.048), social function (P=0.04), and overall QOL (P=0.04) (Table 4). Compared with controls, the intervention promoting self-efficacy had time and interaction effects on physical function (both P<0.001), role function (P<0.001 and P=0.01, respectively), cognitive function (P<0.001 and P=0.003, respectively), emotion function (P<0.001 and P=0.03, respectively), social function (P<0.001 and P=0.045, respectively), and overall QOL (both P<0.001).
Discussion
Nasopharyngeal carcinoma is endemic in Guangxi (China) and patients’ self-management is poor. Minorities such as the Zhuang people may suffer more deeply from psychological problems during treatments for NPC [22,23]. Therefore, this study aimed to design and implement an intervention promoting self-efficacy for Zhuang patients with NPC to improve their QOL. There was no difference in QOL at baseline between the 2 groups, but during the 2-year study, the QOL improvement became significantly different between the 2 groups. From the start of study to hospital discharge, QOL scores decreased in both groups, but the magnitude of this decrease was more important in the control group, probably because controls did not receive the intervention promoting self-efficacy. After discharge, each functional field QOL scores and overall QOL increased over time in the 2 groups, but the QOL in the self-efficacy group remained significantly better at each time point.
With the transformation of the medical model and the development of medical technologies, the curative rate and survival of NPC is continuously improving, but acute and chronic toxicities caused by radiations and chemotherapy seriously affect the QOL of the patients [32,33]. This study showed that during treatments, each functional field and overall QOL of the 2 groups decreased, but the decrease of the self-efficacy group was less important than the decrease of the control group. This decrease could be due to the side effects of chemotherapy and radiotherapy. Indeed, both treatment modalities are known to deeply affect the QOL of the patients [34–36], supporting the decrease in QOL observed at discharge. The decrease could have been less severe in the self-efficacy group because of better empowerment and better cooperation with the treatments.
Previous studies found that the self-efficacy level is low in patients with NPC [15,16]. The intervention promoting self-efficacy (health education, psychological intervention, signing behavior agreement, etc.) showed better improvement in QOL compared with the conventional interventions, which is supported by previous studies in cancer and other problems. Indeed, a previous study showed that teaching specific nose irrigation techniques improved QOL of patients after NPC treatments [37]. A study of breastfeeding women showed that an intervention aiming at improving self-efficacy had a significant impact on breastfeeding self-efficacy and related outcomes [38]. Nevertheless, a study of cancer patients before/after radiotherapy showed that general self-efficacy is associated with anxiety, symptom distress, and QOL [39]. The course of the cancer treatments cannot always be changed to fit the patients, but it may be possible to change the patient’s perception of his illness [40]. Indeed, if cancer patients feel that they are in control of some mundane problems, it may protect them from being overwhelmed by strong emotions and negative events [41], and it could help them adjust to the situations [42]. People who are interested in information that will improve their well-being will be better armed to understand their immediate problems and anticipate the future [43]. A Chinese study showed that not all types of self-efficacy were associated with QOL of cancer survivors and that coping self-efficacy showed the best association [16]. Indeed, among cancer survivors in general, some previous studies showed that coping self-efficacy was positively associated with QOL [10,44–46]. Future studies could explore the different types of self-efficacy in order to refine the intervention program proposed in the present study.
Specifically, since minorities such as the Zhuang people often have characteristics that are associated with low self-efficacy [17–22], specific interventions are required in these patients. The intervention proposed in the present study seemed to be efficient in the Zhuang people, but it was not tested in a control group made of non-minorities. In addition, different approaches should be tested in order to optimize the intervention.
Of course, this study is not without limitations. Despite its prospective design, the sample size was small and the results are mostly preliminary. Additional multicenter studies are necessary to determine the effectiveness of this intervention in patients with NPC. Secondly, the study was performed in selected patients, introducing a selection bias. Thirdly, because of the nature of the intervention, blinding was not possible. It was partially overcome by separating the patients on 2 different floors to prevent patients from discussing of their interventions. Future studies should have, at least, blinded assessors. Fourthly, the control group did not receive any psychological counseling, which could have introduced a bias because eventual psychological problems affecting QOL were not necessarily detected. Fifthly, 7 patients dropped out in each group, probably introducing a bias since these patients were no longer in a set of mind that was favorable to study participation. Sixthly, a time-related bias cannot be excluded because of the improvements in patient care over time. Finally, we cannot exclude the possibility that the improvements in QOL were due, at least in part, by the natural improvements in adverse effects and symptoms after the end of treatments. Additional studies are needed to address this issue.
Conclusions
The intervention promoting self-efficacy could promote the patients’ own potential and initiative, enhance their confidence and ability to solve healthy problems, improve their coping with adverse effects of treatments, and have positive effects on their QOL. Interventions promoting self-efficacy could warrant wider use during the treatment and recovery of minority Zhuang patients with NPC.
Acknowledgements
None.
Footnotes
Source of support: This study was supported by the Medical and Health Appropriate Technology Research and Development Project of Guangxi, China (Key No: S201413-02)
References
- 1.Argiris A, Karamouzis MV, Raben D, Ferris RL. Head and neck cancer. Lancet. 2008;371:1695–709. doi: 10.1016/S0140-6736(08)60728-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kohler BA, Ward E, McCarthy BJ, et al. Annual report to the nation on the status of cancer, 1975–2007, featuring tumors of the brain and other nervous system. J Natl Cancer Inst. 2011;103:714–36. doi: 10.1093/jnci/djr077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tao Q, Chan AT. Nasopharyngeal carcinoma: Molecular pathogenesis and therapeutic developments. Expert Rev Mol Med. 2007;9:1–24. doi: 10.1017/S1462399407000312. [DOI] [PubMed] [Google Scholar]
- 4.NCCN Clinical Practice Guildeines in Oncology (NCCN Guidelines) Head and Neck Cancers. Fort Washington: National Comprehensive Cancer Network; 2015. [Google Scholar]
- 5.Lee AW, Lin JC, Ng WT. Current management of nasopharyngeal cancer. Semin Radiat Oncol. 2012;22:233–44. doi: 10.1016/j.semradonc.2012.03.008. [DOI] [PubMed] [Google Scholar]
- 6.Zhang L, Chen QY, Liu H, et al. Emerging treatment options for nasopharyngeal carcinoma. Drug Des Devel Ther. 2013;7:37–52. doi: 10.2147/DDDT.S30753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Furness S, Glenny AM, Worthington HV, et al. Interventions for the treatment of oral cavity and oropharyngeal cancer: Chemotherapy. Cochrane Database Syst Rev. 2011;(4):CD006386. doi: 10.1002/14651858.CD006386.pub3. [DOI] [PubMed] [Google Scholar]
- 8.Lee AW, Lau WH, Tung SY, et al. Preliminary results of a randomized study on therapeutic gain by concurrent chemotherapy for regionally-advanced nasopharyngeal carcinoma: NPC-9901 Trial by the Hong Kong Nasopharyngeal Cancer Study Group. J Clin Oncol. 2005;23:6966–75. doi: 10.1200/JCO.2004.00.7542. [DOI] [PubMed] [Google Scholar]
- 9.Yeh SA, Tang Y, Lui CC, et al. Treatment outcomes and late complications of 849 patients with nasopharyngeal carcinoma treated with radiotherapy alone. Int J Radiat Oncol Biol Phys. 2005;62:672–79. doi: 10.1016/j.ijrobp.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 10.Porter LS, Keefe FJ, Garst J, et al. Self-efficacy for managing pain, symptoms, and function in patients with lung cancer and their informal caregivers: Associations with symptoms and distress. Pain. 2008;137:306–15. doi: 10.1016/j.pain.2007.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 12.Bandura A, Adams NE, Beyer J. Cognitive processes mediating behavioral change. J Pers Soc Psychol. 1977;35:125–39. doi: 10.1037//0022-3514.35.3.125. [DOI] [PubMed] [Google Scholar]
- 13.Tsang SK, Hui EK, Law BC. Self-efficacy as a positive youth development construct: A conceptual review. ScientificWorldJournal. 2012;2012:452327. doi: 10.1100/2012/452327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tsang SK, Hui EK. Self-efficacy as a positive youth development construct: Conceptual bases and implications for curriculum development. Int J Adolesc Med Health. 2006;18:441–49. [PubMed] [Google Scholar]
- 15.Fang FM, Tsai WL, Chien CY, et al. Pretreatment quality of life as a predictor of distant metastasis and survival for patients with nasopharyngeal carcinoma. J Clin Oncol. 2010;28:4384–89. doi: 10.1200/JCO.2010.28.8324. [DOI] [PubMed] [Google Scholar]
- 16.Yeung NC, Lu Q, Lin W. Specificity may count: Not every aspect of coping self-efficacy is beneficial to quality of life among Chinese cancer survivors in China. Int J Behav Med. 2014;21:629–37. doi: 10.1007/s12529-014-9394-6. [DOI] [PubMed] [Google Scholar]
- 17.Blackman IR. Factors influencing Australian agricultural workers’ self-efficacy using chemicals in the workplace. Workplace Health Saf. 2012;60:489–96. doi: 10.1177/216507991206001104. [DOI] [PubMed] [Google Scholar]
- 18.Liang SY, Yates P, Edwards H, Tsay SL. Factors influencing opioid-taking self-efficacy and analgesic adherence in Taiwanese outpatients with cancer. Psychooncology. 2008;17:1100–7. doi: 10.1002/pon.1326. [DOI] [PubMed] [Google Scholar]
- 19.Raynor PA. An exploration of the factors influencing parental self-efficacy for parents recovering from substance use disorders using the social ecological framework. J Addict Nurs. 2013;24:91–99. doi: 10.1097/JAN.0b013e3182922069. quiz 100–1. [DOI] [PubMed] [Google Scholar]
- 20.Reynolds NR, Testa MA, Marc LG, et al. Factors influencing medication adherence beliefs and self-efficacy in persons naive to antiretroviral therapy: A multicenter, cross-sectional study. AIDS Behav. 2004;8:141–50. doi: 10.1023/B:AIBE.0000030245.52406.bb. [DOI] [PubMed] [Google Scholar]
- 21.Takahashi LM, Magalong MG, Debell P, Fasudhani A. HIV and AIDS in suburban Asian and Pacific Islander communities: Factors influencing self-efficacy in HIV risk reduction. AIDS Educ Prev. 2006;18:529–45. doi: 10.1521/aeap.2006.18.6.529. [DOI] [PubMed] [Google Scholar]
- 22.Santee RG. An integrative approach to counseling - bridging chinese thought, evolutionary theory, and stress management. Thousand Oaks: Sage Publications, Inc; 2007. [Google Scholar]
- 23.Brewster ME, Moradi B, Deblaere C, Velez BL. Navigating the borderlands: the roles of minority stressors, bicultural self-efficacy, and cognitive flexibility in the mental health of bisexual individuals. J Couns Psychol. 2013;60:543–56. doi: 10.1037/a0033224. [DOI] [PubMed] [Google Scholar]
- 24.Brady LW, Heilmann HP, Molls M, Nieder C. Nasopharyngeal cancer – multidisciplinary management. Berlin: Spinger-Verlag; 2010. [Google Scholar]
- 25.Schwarzer R, Jerusalem M. Generalized Self-Efficacy scale. In: Weinmann J, Wright S, Johnston M, editors. Measures in health psychology: A user’s portfolio Causal and control beliefs. Windsor: NFER-NELSON; 1995. [Google Scholar]
- 26.Luszczynska A, Scholz U, Schwarzer R. The general self-efficacy scale: Multicultural validation studies. J Psychol. 2005;139:439–57. doi: 10.3200/JRLP.139.5.439-457. [DOI] [PubMed] [Google Scholar]
- 27.Zhang JX, Schwarzer R. Measuring optimistic self-beliefs: A Chinese adaptation of the General Self-Efficacy Scale. Psychologia. 1995;38:174–81. [Google Scholar]
- 28.Yang L, Lu JM, Zheng XF. [Analysis on self-efficacy level of patients nasopharyngeal carcinoma (NPC) and their related factors]. Chinese Journal of Modern Nursing. 2010;16:4352–55. [in Chinese] [Google Scholar]
- 29.Lee HC, Chiu HF, Wing YK, et al. The Zung Self-rating Depression Scale: Screening for depression among the Hong Kong Chinese elderly. J Geriatr Psychiatry Neurol. 1994;7:216–20. doi: 10.1177/089198879400700404. [DOI] [PubMed] [Google Scholar]
- 30.Aaronson NK, Ahmedzai S, Bergman B, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85:365–76. doi: 10.1093/jnci/85.5.365. [DOI] [PubMed] [Google Scholar]
- 31.Zhao H, Kanda K. Translation and validation of the standard Chinese version of the EORTC QLQ-C30. Qual Life Res. 2000;9:129–37. doi: 10.1023/a:1008981520920. [DOI] [PubMed] [Google Scholar]
- 32.Xiao WW, Lu TX, Li JX. [Study on changing trend of survival quality of nasopharyngeal carcinoma patients with conventional radiotherapy]. Chinese Journal of Radiation Oncology. 2010;12:87–91. [in Chinese] [Google Scholar]
- 33.Deng ZX, Yang HY, Zhou FL. [The impact that concurrent healthy education of patients with nasopharyngeal carcinoma and their families have on quality of life in patients]. Journal of Nursing Science. 2007;22:62–64. [in Chinese] [Google Scholar]
- 34.Yucel B, Akkas EA, Okur Y, et al. The impact of radiotherapy on quality of life for cancer patients: A longitudinal study. Support Care Cancer. 2014;22:2479–87. doi: 10.1007/s00520-014-2235-y. [DOI] [PubMed] [Google Scholar]
- 35.Dehkordi A, Heydarnejad MS, Fatehi D. Quality of life in cancer patients undergoing chemotherapy. Oman Med J. 2009;24:204–7. doi: 10.5001/omj.2009.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gunnars B, Nygren P, Glimelius B SBU-group. Swedish Council of Technology Assessment in Health Care: Assessment of quality of life during chemotherapy. Acta Oncol. 2001;40:175–84. doi: 10.1080/02841860151116222. [DOI] [PubMed] [Google Scholar]
- 37.Luo HH, Fu ZC, Cheng HH, et al. Clinical observation and quality of life in terms of nasal sinusitis after radiotherapy for nasopharyngeal carcinoma: Long-term results from different nasal irrigation techniques. Br J Radiol. 2014;87:20140043. doi: 10.1259/bjr.20140043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wu DS, Hu J, McCoy TP, Efird JT. The effects of a breastfeeding self-efficacy intervention on short-term breastfeeding outcomes among primiparous mothers in Wuhan, China. J Adv Nurs. 2014;70:1867–79. doi: 10.1111/jan.12349. [DOI] [PubMed] [Google Scholar]
- 39.Mystakidou K, Tsilika E, Parpa E, et al. Relationship of general self-efficacy with anxiety, symptom severity and quality of life in cancer patients before and after radiotherapy treatment. Psychooncology. 2013;22:1089–95. doi: 10.1002/pon.3106. [DOI] [PubMed] [Google Scholar]
- 40.Takaki J, Nishi T, Shimoyama H, et al. Interactions among a stressor, self-efficacy, coping with stress, depression, and anxiety in maintenance hemodialysis patients. Behav Med. 2003;29:107–12. doi: 10.1080/08964280309596063. [DOI] [PubMed] [Google Scholar]
- 41.Monroe B, Oliviere D. Resilience in palliative care. Eur J Palliat Care. 2006;13:22–25. [Google Scholar]
- 42.Thompson SC, Sobolew-Shubin A, Galbraith ME, et al. Maintaining perceptions of control: Finding perceived control in low-control circumstances. J Pers Soc Psychol. 1993;64:293–304. doi: 10.1037//0022-3514.64.2.293. [DOI] [PubMed] [Google Scholar]
- 43.Rankin SH, Stallings KD. Patient Education Principles & Practuce. 4th ed. Philadelphia: Lippincott; 2001. [Google Scholar]
- 44.Hochhausen N, Altmaier EM, McQuellon R, et al. Social support, optimism, and self-efficacy predict physical and emotional well-being after bone marrow transplantation. J Psychosoc Oncol. 2007;25:87–101. doi: 10.1300/J077v25n01_05. [DOI] [PubMed] [Google Scholar]
- 45.Howsepian BA, Merluzzi TV. Religious beliefs, social support, self-efficacy and adjustment to cancer. Psychooncology. 2009;18:1069–79. doi: 10.1002/pon.1442. [DOI] [PubMed] [Google Scholar]
- 46.Mosher CE, Duhamel KN, Egert J, Smith MY. Self-efficacy for coping with cancer in a multiethnic sample of breast cancer patients: Associations with barriers to pain management and distress. Clin J Pain. 2010;26:227–34. doi: 10.1097/AJP.0b013e3181bed0e3. [DOI] [PMC free article] [PubMed] [Google Scholar]