Abstract
Phagocytes clear dying cells within an organism to prevent damaging inflammation and autoimmunity. In this issue of Immunity, Luo et al. (2016) describe how “find-me” signals from apoptotic cells induce erythropoietin signaling within macrophages to prime them for efferocytosis.
Billions of cells die each day within a human as part of normal homeostasis, yet it is relatively rare to find these cells within the host. Specialized immune cells called phagocytes have evolved efficient ways in which to track down dying cells and dispose of them quietly, without eliciting unwanted immune responses (Ravichandran, 2010). This process, termed efferocytosis, is not merely a single course, as the dying cells actively advertise their presence through the release of chemoattractants or “find-me” signals and the exposure of distinct molecular signatures called “eat-me” signals (Martinez, 2015). Whereas much has been uncovered in the recognition and engulfment of dying cells, the nuances of “find-me” signals released by dying cells are relatively undefined. Luo et al. (2016) have uncovered that “find-me” signals function to promote clearance, suggesting that “find-me” signals are more than the tantalizing aromas that draw in the phagocyte (Luo et al. (2016).
The most physiologically common cell death pathway is apoptosis, or programmed cell death. During apoptosis, cellular components are broken down and neatly packaged within membrane blebs, without exposing potentially inflammatory contents to the extracellular environment where they could ultimately act as autoantigens (Green et al., 2009). In addition to its ability to stimulate phagocyte chemotaxis, Luo et al. (2016) have discovered that the “find-me” signal, sphingosine 1-phosphate (S1P), can trigger the activity of a secondary signaling protein, erythropoietin (EPO), which plays a role in priming macrophages for apoptotic cell engulfment. EPO is primarily known for its role in red blood cell development by binding the cognate EPO receptor (EPOR) on erythroid progenitor cells, but has also been shown to exert effects on a variety of non-erythroid tissues (Nairz et al., 2012).
Several pieces of evidence pointed to EPO’s role in macrophage clearance of apoptotic cells. First, EPOR is expressed on macrophages and treatment of macrophages with EPO suppresses inflammatory gene expression, an outcome associated with apoptotic cell engulfment (Lifshitz et al., 2010). Second, the “find-me” signal S1P is known to induce hypoxia-inducible factor 1α (HIF1α), a key regulator of EPO expression. Third, EPO has been shown to ameliorate models of autoimmune diseases linked to defective dead cell clearance (Luo et al., 2013). Despite these published observations, how a hormone critical for erythropoiesis functions in the clearance of dying cells remained a mystery. Here, Luo et al. (2016) bridge that gap by demonstrating that EPO can prime phagocytes for effective efferocytosis (Figure 1).
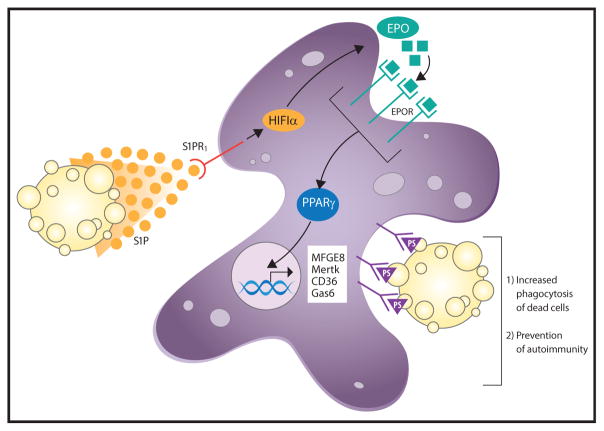
Figure 1. The “Find-Me” Signal S1P Activates the EPO-EPOR Axis to Prime Macrophages for Efferocytosis.
Release of the “find-me” signal, S1P, by dying cells upregulates EPO expression in phagocytic cells, such as macrophages. Signaling via the EPO-EPOR axis activates the PPARγ pathway, which increases levels of phagocytic receptors, such as MFGE8, MerTK, CD36, and Gas6. Mice in which EPO-EPOR signaling is disrupted display decreased clearance of dying cells and increased incidence of autoimmunity.
The authors begin by demonstrating a link between apoptotic cell-derived S1P and macrophage EPO signaling. S1P and apoptotic cell-conditioned media containing S1P were able to induce both EPO production by and EPOR surface expression on mouse macrophages in vitro. This effect was dependent upon signaling via S1P receptor 1 (S1PR1), as antagonism of this receptor blocked S1P effects. As predicted, S1P controlled EPO expression through activation of HIF1α, but EPOR was shown to be upregulated by EPO itself as part of a positive feedback loop. This mechanism might help to explain amplification of EPO signaling by macrophages residing in tissues where the EPO concentration is normally low. The authors also elegantly demonstrated that the S1P-EPO-EPOR signaling axis is at play in vivo. Apoptotic cells or apoptotic cells in which S1P expression had been inhibited by siRNA to sphingosine kinase-1 (SphK1) were injected into mice. Untreated apoptotic cells induced EPO expression in the spleen and EPOR expression by splenic macrophages—responses that were drastically reduced by SphK1 inhibition. In addition, chemically induced thymocyte apoptosis caused a spike in S1P, EPO, and EPOR, while chemical inhibition of apoptosis downregulated these players.
But what effect does EPO-EPOR signaling have on macrophage phagocytosis of apoptotic cells? To answer this question, Luo et al. (2016) labeled apoptotic cells with a pH-sensitive probe able to distinguish extracellular cells from those that have been engulfed, and tracked them in wild-type mice or those missing EPOR only in cells of myeloid lineage, by way of Lyz2-cre. Although phagocytosis was enhanced by treatment of wild-type mice with recombinant EPO, this treatment had no effect on the EPOR-deficient mice, which were clearly defective in dead cell uptake. Despite equivalent numbers of macrophages, EPOR-deficient mice showed a greater accumulation of apoptotic cells in vivo compared to wild-type after dexamethasone treatment or with age, which clearly suggests a role for EPO signaling in the regulation of macrophage apoptotic cell clearance. Importantly, EPOR-deficiency also skewed the macrophage cytokine profile to a more pro-inflammatory phenotype, consistent with other models of defective dead cell clearance (Poon et al., 2014).
Luo et al. (2016) also tackled the question of how EPO stimulates efferocytosis, and begin by examining regulators of phagocytic receptors or bridging molecules that link phagocytic receptors with “eat-me” signals on dying cells. One group of transcription factors called peroxisome proliferator activated receptors (PPARs) have been previously shown to regulate phagocytic receptors in response to engulfed cargo (Mukundan et al., 2009). The authors demonstrated that EPO induced expression of PPARγ, and that a PPARγ agonist was able to enhance apoptotic cell phagocytosis in EPOR-deficient macrophages. The authors then connect these results to S1P release by apoptotic cells by showing that apoptotic cell-conditioned media enhanced macrophage phagocytosis, but that this response could be inhibited S1PR1 antagonism. Additionally, they demonstrated that S1P alone could induce upregulation of PPARγ-mediated phagocytic receptors, such Mfge8, Mertk, and Cd36, in an EPO-EPOR-dependent manner.
The sheer importance of effective efferocytosis is highlighted by the fact that defects in dead cell clearance mechanisms are associated with autoimmune diseases, such as systemic lupus erythematosus (SLE) and rheumatoid arthritis (Liu and Davidson, 2012; Martinez, 2015). Indeed, uncleared dead cells can be found in tissue from SLE patients (Liu and Davidson, 2012). The authors ultimately asked whether the EPO-EPOR axis plays a role in the prevention of systemic autoimmune disease by ridding the host of unwanted cellular corpses that could stimulate an autoantigen-specific immune response. Strikingly, mice with EPOR-deficient macrophages developed higher concentrations of autoantigen-specific antibodies, including anti-dsDNA and anti-nuclear antibodies, over time when compared to wild-type controls. Antibody deposition in kidney glomeruli and subsequent kidney damage was more pronounced in EPOR-deficient mice as well. Serum concentration of pro-inflammatory cytokines, such as interleukin-6 (IL-6), in EPOR-deficient mice was also increased, along with a concomitant decrease in anti-inflammatory TGF-β. Importantly, Luo et al. (2016) demonstrate that recombinant EPO administration in a model of pristane-induced SLE-like disease caused decreased disease severity, as well as heightened dead cell clearance by macrophages in vivo. Finally, the importance of PPARγ was addressed, as pharmacological agonism of PPARγ ameliorates signs of autoimmunity even in the absence of EPOR. Collectively, the authors elegantly demonstrate a role for the “find-me” signal S1P outside of its chemoattractive capacity and clearly establish the EPO-EPOR signaling axis as a critical node in efferocytosis and the prevention of the autoimmune phenotype.
The study of immunomodulation during phagocytic events is an area of great interest. While “find-me” signals have been described, their mechanisms of action have long been speculatory. Despite displaying a role in the recruitment of phagocytes, the validity of this function in vivo has often been questioned, as serum concentrations of “find-me” signals are often ten times higher than tissue concentrations, indicating a local rather than systemic role, and in vivo evidence supporting a necessary role has not be forthcoming (Martinez, 2015; Ravichandran, 2010). Here, Luo et al. (2016) reveal that the answer might lie in its role in priming phagocytic cells for efferocytosis, rather than recruiting them to sites of cell death.
Thus, it appears that the EPO-EPOR axis can have distinct effects depending on the cell type through which it is signaling. Although it has been known that EPO is required for proliferation, differentiation, and survival of erythroid precursors, it appears to also be a critical regulator of immunosuppression and lipid handling. How does one reconcile two seemingly separate functions? In one sense, EPO-EPOR signaling can be considered a master controller of cell fate, whether that fate be erythrocyte or phagocyte. The differential effects might depend on the machinery each type of cell possesses, with phagocytes, but not erythrocytes, expressing high levels of PPAR family members. Furthermore, erythrocytes, produced at a rate of 1010 per hour, represent one of the most common cleared cell, and thus EPO might be promoting erythrocyte development while simultaneously preparing phagocytes for their future meal.
As more evidence links efferocytosis to autoimmunity, how a phagocyte handles the metabolic burden of engulfing a dying cell, essentially doubling its lipid and protein content, is an area of growing interest. S1P mediates its effect through activation of HIF1α, a known regulator of cell metabolism (Martinez, 2015). Future studies should investigate whether phagocyte priming extends beyond upregulation of phagocytic receptors and immunomodulation to affect metabolism and energy expenditure in preparation of its upcoming meal. In addition, do other known “find-me” signals illicit similar priming factors, and do these factors also have dual physiological functions? Although defects in Mertk, Atg5, and Pparg have been associated with human SLE (Martinez, 2015), it is unclear whether defects in the EPO-EPOR axis also contribute to SLE or other autoimmune diseases linked to defective efferocytosis. EPO could represent a potential therapeutic target for autoimmune pathologies. Taken together, Luo et al. (2016) have described the pairing of a “find-me” signal with an erythropoiesis hormone, sure to arouse the phagocyte’s appetite. Thus, the term “find-me” signal is a misnomer and would be better described as an appetizer.
References
- Green DR, Ferguson T, Zitvogel L, Kroemer G. Nat Rev Immunol. 2009;9:353–363. doi: 10.1038/nri2545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lifshitz L, Tabak G, Gassmann M, Mittelman M, Neumann D. Haematologica. 2010;95:1823–1831. doi: 10.3324/haematol.2010.025015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Z, Davidson A. Nat Med. 2012;18:871–882. doi: 10.1038/nm.2752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo B, Jiang M, Yang X, Zhang Z, Xiong J, Schluesener HJ, Zhang Z, Wu Y. Biochim Biophys Acta. 2013;1832:1260–1270. doi: 10.1016/j.bbadis.2013.04.015. [DOI] [PubMed] [Google Scholar]
- Luo BGW, Liu Z, Zhen A, Wang J, Shi R, Liu Y, Liu Y, Zhang Z, Wu Y. Immunity. 2016;44:287–302. doi: 10.1016/j.immuni.2016.01.002. this issue. [DOI] [PubMed] [Google Scholar]
- Martinez J. Current Topics in Microbiology and Immunology. Springer International Publishing; 2015. pp. 1–36. [Google Scholar]
- Mukundan L, Odegaard JI, Morel CR, Heredia JE, Mwangi JW, Ricardo-Gonzalez RR, Goh YP, Eagle AR, Dunn SE, Awakuni JU, et al. Nat Med. 2009;15:1266–1272. doi: 10.1038/nm.2048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nairz M, Sonnweber T, Schroll A, Theurl I, Weiss G. Microbes Infect. 2012;14:238–246. doi: 10.1016/j.micinf.2011.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poon IK, Lucas CD, Rossi AG, Ravichandran KS. Nat Rev Immunol. 2014;14:166–180. doi: 10.1038/nri3607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ravichandran KS. J Exp Med. 2010;207:1807–1817. doi: 10.1084/jem.20101157. [DOI] [PMC free article] [PubMed] [Google Scholar]