Abstract
In this article we explore the value of using visual data in a study on medical expert judgment to better understand medical experts’ conceptualizations of complex, challenging situations. We use examples from a larger study on medical expertise in which rich pictures and interviews were used. The three stories presented in this article belong to experts in the domain of surgery. The stories are used to show the ways in which rich pictures can capture and elucidate potentially hidden aspects of the influence of the context in surgical experts’ judgment during challenging operations. We suggest that incorporating visual representations such as rich pictures as research data can aid in understanding previously unarticulated constructions of medical expertise. We conclude that when the researcher strives for capturing complexity, visual methods have the potential to help medical experts deflect from their tendency to simplify descriptions of accounts and to meaningfully engage these individuals in the research process.
Keywords: complexity; qualitative analysis; research, qualitative; surgery; visual methods
The study of expert judgment has a robust tradition in medical education research. Researchers, relying mostly on experimental methods, have successfully deconstructed a multitude of cognitive skills that expert clinicians exhibit when making decisions (Bornstein & Emler, 2001; Dawson, 1987; Detmer, Fryback, & Gassner, 1978; Klein, 2005; Mylopoulos & Regehr, 2011; Tversky & Kahneman, 1985). However, the increasingly complex nature of medical practice has alerted us to the need to explore the use of these skills in specific situations. We therefore require studies that investigate the contextually embedded nature of medical expertise. In following this rationale and by using a qualitative approach, we set out to investigate what social, organizational, and personal factors influence experts’ clinical judgment during complex and challenging situations. Given the unique use of visual methods in our research, this article is intended to be an exploration in which we focus on discussing the use of drawings to complement interviews, rather than relying on elaborate accounts of the research results.
Qualitative methodologies are now being used to explore these contextual factors of medical expertise, primarily through the use of interviews. Although interviews are a well-established method for gathering complex and heterogeneous accounts of expert judgment (Crandall, Klein, & Hoffman, 2006; Ericsson, 2006a, 2006b; Klein, 1997; Klein, 1995; Klein, Orasanu, Calderwood, & Zsambok, 1993), these might be unable to fully capture experts’ experiences of coping with complexity. A number of issues might limit the interview method, including the difficulty of making the tacit explicit, the insufficiency of words, or the status of the interviewer. For instance, when the interviewer is not an expert in the participant’s area of specialization, experts might resort to simplifying their descriptions to help the interviewer understand their perspectives. Conversely, when the interviewer is an expert, then the participant might forego describing important dimensions of the situation that he or she assumes are well understood by the peer interviewer.
Our research used visual methods from the field of systems engineering (SE) such as rich pictures, systemigrams, causal loop diagrams, system maps, and influence diagrams (Boardman & Sauser, 2008). We sought to understand the influence of the context of challenging and complex situations on expert judgment. Using examples from our dataset, we demonstrate the benefits of using visual methods for elucidating tacit dimensions associated with the ways in which medical experts perceive, negotiate, and act in the context of a challenging situation. There are three issues that commonly surface in interview research with experts: the tendency to simplify descriptions of complex situations, the tendency to focus on the procedural dimension of a situation, and verbalization barriers (Hoffman, Shadbolt, Burton, & Klein, 1995). These issues can be addressed through the inclusion of visual methods.
Researching Expert Judgment in Medicine
The construct of expert judgment in medicine has been built on the assumption that as experience is extended, physicians develop a particular set of skills that allow them to gain a deeper understanding of their practice (Ericsson, 2006a; Norman, Eva, Brooks, & Hamstra, 2006). Researchers have now begun to recognize that in addition to better understanding the nature of those individual skills, we also need to explore how the context influences and determines the ways in which physicians use those skills (Durning, Artino, Pangaro, van der Vleuten, & Schuwirth, 2010; Koens, Mann, Custers, & Ten Cate, 2005; Mylopoulos & Regehr, 2007, 2011). Consequently, an emerging school of researchers is attending to the context dependency of expert clinical judgment as a complex social phenomenon.
These researchers are showing how an expert’s thinking and ability to solve problems is complemented by and often dependent on the cognition that is shared with other people or objects present in the situation (Durning, Artino, Pangaro, van der Vleuten, & Schuwirth, 2011; Durning et al., 2012; Pimmer, Pachler, & Genewein, 2013). Expert judgment therefore emerges as a result of an intentionally driven (goal-driven) participant interacting with a very information-rich environment (Durning & Artino, 2011). This new focus on interactions between the expert and the environment has allowed researchers to identify which particular contextual factors seem to impact to a greater or lesser extent a clinician’s performance during diagnostic reasoning tasks (Durning et al., 2011; Durning et al., 2012). Therefore, expert judgment involves more than applying a set of skills; it can also be understood as an interaction between the expert and multiple dimensions such as the procedural, emotional, or political aspects of a situation.
In the domain of surgery, qualitative methodologies have been particularly instrumental in understanding how experienced surgeons internally negotiate between routine and nonroutine moments of their practice, showing surgical judgment as a continuous process of transforming and reconciling information (Cristancho, Vanstone, et al., 2014; Cristancho et al., 2013; Moulton, Regehr, Lingard, Merritt, & MacRae, 2010a, 2010b). As qualitative research acknowledges and includes subjective experience, these findings are based on the participants’ own understandings of their decision-making and coping strategies through an exploration of the “how” and “why” of their perceptions. Qualitative research is therefore a powerful means to study expertise and expert judgment because it permits the researcher to discover unknown processes or skills, attend to the contextual specificity of a situation, probe deeper into motivations and influencers, and produce a more holistic and integrated view of expertise (Mylopoulos & Regehr, 2007, 2011). In other words, we are able to see situations more clearly through the experts’ eyes.
Nonetheless, designing qualitative research using interviews carries some particular challenges when attempting to study complex situations in surgery from the perspective of experts. As researchers we must take into account issues such as verbalization barriers to elucidate tacit knowledge and simplification of descriptions, and focus on the procedural aspects of the situation. The need to verbalize experiences might limit the depth to which certain topics are described, inadvertently prompting the experts to simplify their accounts of those topics or to focus on only one component or dimension. In surgery, the procedural aspect of the situation is commonly the one that surgeons emphasize. Moreover, verbalizations might disregard nonverbal aspects of how experts’ understanding is communicated, such as building trust.
Visual methods that foster a process of deliberation and articulation potentially offer a solution to the methodological limitations of interviews alone, as described above, especially in studies of expertise in challenging situations. We suggest that visual methods are a promising alternative to better capture the multiple dimensions of a situation that experts navigate when interacting with their professional context.
Using Rich Pictures to Capture the Complexity of Challenging Situations
We followed a systems engineering (SE) approach to research, which is particularly appropriate for describing and solving complex phenomena (Cristancho, Lingard, & Regehr, 2014). Diagramming is the key activity used in SE. System diagrams are visual methods used to visually communicate the complexity of a situation in terms of the multiple forces acting on the components of the situation and the interactions between those forces (Boardman & Sauser, 2008). In our research, we used a particular type of system diagram called a “rich picture.” Rich pictures are pictorial representations that attempt to capture an individual’s perspective of a situation, including objects, ideas, people, character, feelings, conflicts, and prejudices (Armson, 2011). Using roughly sketched symbols such as stick figures, rich pictures can display features of interest and the interactions among those features. Rich pictures allow individuals to tell their story of the relevant conditions affecting a situation at a particular place and time; therefore, these pictures constitute an effective method of understanding how individuals see their world (Guillemin, 2004).
We purposefully sampled 10 faculty surgeons from a variety of surgical specialties (hepatobiliary, colorectal, cardiac, vascular, and neurosurgery) at two academic hospitals in London, Ontario, Canada, who provided consent and were willing to be observed and to reflect on their surgical experiences. The Health Sciences Research Ethics Board of Western University approved the research, in which 40 “snapshots” were collected through a combination of interviews, observations, and rich picture sessions. A snapshot is the state of a system at a particular point in time.
The system of interest was expert judgment, and snapshots allowed us to capture particular moments in which surgeons exercised their judgment and reflected on this skill during their participation. Snapshots consisted of (a) preoperative interviews (Preop snapshot) in which surgeons verbally shared their perspective on the potential challenges that they had anticipated playing a role in the situation; (b) intraoperative observations (OR snapshot), through which researchers documented the evolution of the situation; this encompassed not only the surgeon’s actions but any interactions within the boundaries of the operating room; (c) postoperative interviews (Postop snapshot), in which surgeons verbally described their perspective on how the situation actually played out, including any unanticipated elements; and (d) rich pictures (RP snapshot), through which surgeons visually represented their perspective on the complexity of the situation as it evolved.
Participants were given instructions on how to create rich pictures based on the guidelines offered by Armson (2011). Armson provided an example of the development of a rich picture from a personal story. At the beginning of each drawing session, we used this example to teach participants about the process and to show them what the final product might look like. We also emphasized that rich pictures were meant to be free-form drawings to depict an experience, and that art skills were neither necessary nor assessed.
Our approach to the data analysis revolved around an aesthetic analysis of the rich pictures; that is, the RP snapshots and the use of sensitizing concepts from SE to inform the interpretation of results. The Preop snapshots, the OR snapshots, and the Postop snapshots supported the aesthetic analysis throughout. Two members of the research team with a professional background in design from engineering (Cristancho) and the arts (Bidinosti) led the analysis of the data. The researchers’ academic backgrounds directed our choice of using an aesthetic approach to visual analysis, as opposed to a content analysis approach (Bell & Davison, 2012). The analytical process involved three phases: (a) Phase 1: an individual aesthetic analysis of each RP snapshot; (b) Phase 2: a cross-comparison of all RP snapshots complemented with their corresponding Preop, OR, and Postop snapshots; and (c) Phase 3: a consolidated team analysis. The first two phases were conducted by the research team and co-authors of this paper, whereas the third phase was conducted in collaboration with the participating surgeons.
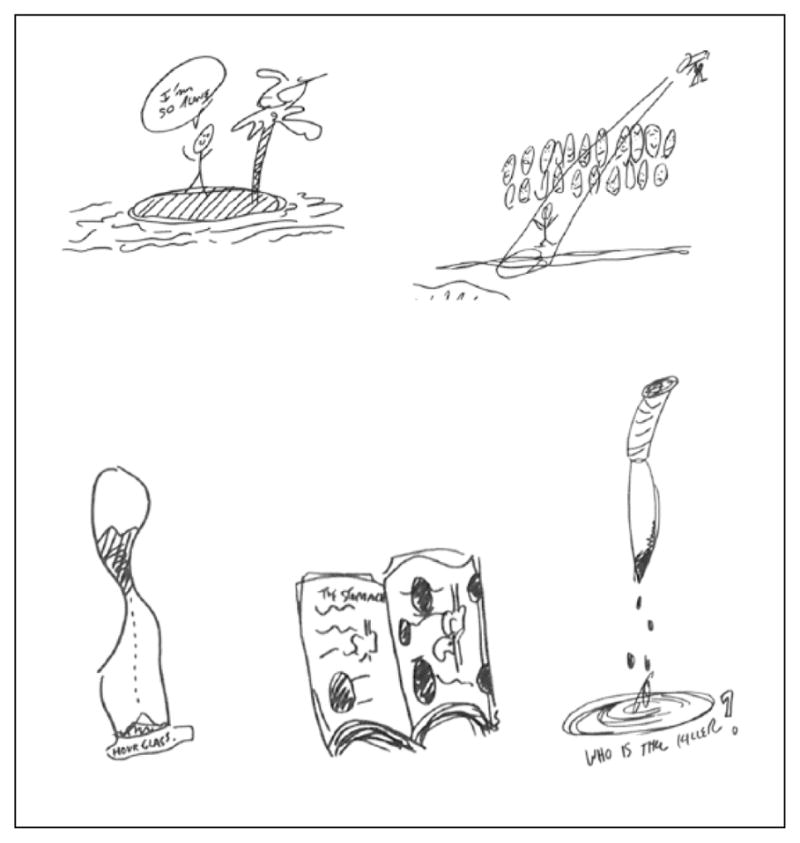
During the aesthetic analysis of individual RP snapshots, we engaged in a four-moment observational process of the rich pictures. These four moments of observation allowed us to build a bottom-to-top description of the RP snapshots. At the bottom, the focus was on the particular aesthetic features of the elements of the RP snapshot, including the identification and pictorial elements and how they were visually connected. Considerations of lines, shape, color, scale, focal point, emphasis, balance, motion, and space were taken into account. At the top, we considered the meaning of the motifs individually and in relation to others. We looked at the evolution of individual motifs when they were repeated in the same drawing at different positions, any groupings of motifs that would potentially carry out a story, and those elements that appeared to be foregrounded and backgrounded by those stories. At this point, we used the rest of the snapshots to help uncover those stories while remaining alert to their authenticity. We kept detailed documentation of the four moments of observation in the form of an audit trail; refer to Table 1 and Figure 1 for a sample of the audit trail.
Table 1.
Sample of the Audit Trail for the Aesthetic Analysis of Figure 3.
| Analysis | Interpretation | |||
|---|---|---|---|---|
| Motifs (See Figure 3) | Description of Motif | How have the motifs been arranged? How do they visually connect to each other? | Phase 1: What do we (the researchers) think the motifs mean individually and in relation to each other? | Phase 2: What did the surgeon say about his drawing and its meaning? |
| The castaway (stick figure person on an island, see figure 4) | A male stick figure stands next to a palm tree on an oval rock/island. The rock shape is drawn with diagonal lines, which gives it a bit of weight. Wavy lines around the island represent water. A speech bubble, above the figure’s head, reads, “I’m so alone.” The figure’s arms are up and it has a face. | The “lonely” upper-right corner motif, above the “cancer monster.” Stick figure person on an island Person in the spotlight |
The figure on the island and figure in the spotlight equal two ways of representing how the surgeon feels alone: alone in making decisions and alone in the face of judgment by peers. He is surrounded by people, but they are observing him/judging his decisions. |
In the upper right, there are two representations that I’ve tried to make of my concerns about operating on this person. They’re more about me, personally. They have nothing really to do with the patient. One is my feeble attempt to drawing a person standing on an island saying that they’re so alone, because when you’re in that situation you have to make these decisions. You have to read the consequences for your decisions and no one else is there, really, with you. And sometimes, patients and their families put you in that situation where they say. “What do you think he should do?” And I don’t really like to ever answer that question, because it’s not up to me; it’s up to them to decide. I see my job as giving them information, and they’re supposed to decide. But often families in this situation will put you on that island because they don’t want to be the ones responsible for making the decision |
| Person in the spotlight being watched, see figure 4 | Two horizontal rows of faces (happy and angry) are situated above a male stick figure, which is standing on the ground surrounded by an implied spotlight beam coming from a source on the upper right. | Located to the left of the island scene and just above and to the right of the tombstone and cloud. | See above. | The second is someone standing in the middle of a room with a spotlight on them, with a whole bunch of faces, that are somewhat disapproving, staring at them, which is my representation of morbidity and mortality rounds. Based on my decision making, I’m going to stand in the middle there, even though that doesn’t really happen, but that’s what it feels like. And people might be standing around saying, “Why did you even bother operating on this person? What were you thinking when you did this? This is ridiculous. You’ve created a problem where there was no problem.” |
| Hourglass, see figure 4 | Linear drawing of an hourglass that is labeled as such. The upper part of the glass is half full and the sand flowing down is represented by a dotted line. | Located to the upper left of the tombstone, between the book and the stomach. | The hourglass and the clock equal repetition of time motif on different places on the page with a different emphasis each time. There is also a clock on the clock tower of the building in the “surgeons’ face” grouping. The hourglass represents running out of time. He’s trying to find a way to fix the stomach. Also, in the face grouping: the pressure of time. | I tried to draw an hourglass, which isn’t a very good representation. But that, to me, represents the fact that he’s only got a certain amount of time anyway, and no matter what we did, the grains of sand are going to keep ticking down and he’s going to die at some point. So I guess that kind of fits with that feeling of futility, that no matter what we did, the grains of sand, we’re not going to turn that upside down; it’s still going to keep dropping. |
| Book, see figure 4 | Drawing of an open book. The title page is the stomach. Circles are drawn in it like little illustrations and are filled in with scribbled lines to make them look black. There are also horizontal lines representing text and small drawings of stomachs. | Located between the knife and the book in the upper-left corner of the page. | A textbook? Looking for guidelines, rules? Not a textbook case? | There’s a textbook there that says the stomach, and then there’s a whole bunch of holes in it because that represents the fact that I had a lot of knowledge. But none of it was really applicable because the fact is that the problem we encountered, it didn’t really fit with anything that a textbook cancer would be. |
| Knife/Dagger, see figure 4 | A large vertical dagger is drawn pointing downwards. Teardrop shaped droplets fall from the dagger into an oval-shaped pool of blood. The tip of the knife is blackened with scribbled ink lines, as are the droplets. Underneath all of this are the words, “Who is the killer?” | Located in the upper-left corner of the page, to the left of the book. | Even though the patient has terminal cancer, this surgeon is wondering if he is just contributing to the patient’s death rather than trying to save his life. | The next thing beside it is very morbid, but I was trying to think of something that represented killing someone, and so it’s a knife with blood dripping off it, and the question is, “Who is the killer?” When you operate on these people, you don’t want to be the person that’s pushed them over the edge and kill them. They’re dying of a natural process: their cancer. That’s no one’s fault. No one caused that to them, no one did anything bad to them. It’s back luck, they just caught it and that’s the way the world works. But when you intervene and do something to someone, and operate on them, and cause them to die because of your intervention, or that process which is occurring, him dying has sped up, then sometimes you often think inside yourself that you actually killed someone, despite the fact you’re trying to help them. You might have made that process faster and they died. So that’s my morbid representation of those thoughts. |
Figure 1.
Story 1 (simplifying the description of events): “That sounds straightforward!”
In the second phase, we engaged in a cross-comparison of multiple RP snapshots. Our analysis focused on identifying common dimensions across different pictures and how those dimensions interrelated to each other. This analysis allowed us to expand on our preliminary understanding from Phase 1 of the individual stories that surgeons were depicting and to begin constructing an overall story of what seemed to be emerging out of the set of pictures. Our epistemological stance to visual analysis is one in which the visual is treated as a social construction that must be explored as a product of the encounter between researcher and research participant; therefore, Phase 3 was conducted in the form of a team analysis exercise.
We invited the participating surgeons to a “return-of-findings”1 session designed to explore their viewpoint on the analytical results from Phases 1 and 2. During this session, surgeons learned the aesthetic analysis process and had the opportunity to apply it to the RP snapshots of other participants. This educational activity was followed by a presentation of our viewpoints, and a team discussion focused on similarities and differences between viewpoints. From an SE perspective, there are several conceptual dimensions2 we could have used to approach our research question. We focused on the notion of surgical judgment as a multidimensional phenomenon, which relates to the concept of the system’s structure. Throughout the analysis, qualitative rigor criteria were used, including reciprocity, reflexivity, resonance, researcher and participant triangulation, and the formation of an audit trail of the analytical process (Flick, 2008; Harrison, MacGibbon, & Morton, 2001; Sandelowski, 1993).
In this section, we have provided the details of the overall analytical approach to orient the reader; however, it is not our intention with the present article to provide elaborate accounts of the results from the three analytical phases. Rather, we seek to uncover some advantages of using rich pictures as one of our data collection methods. With this is mind, the stories we describe next were derived from the first phase of the process; that is, individual aesthetic analysis of each RP snapshot.
Stories From our Research on Medical Expertise
We present three examples of instances from our research on medical expert judgment in which the use of rich pictures helped in the identification and understanding of unarticulated aspects of surgeons’ perspectives on challenging operations. These stories were chosen for their potential to illustrate the three main limitations of using interviews alone in research with experts: the tendency to simplify descriptions of complex situations, the tendency to focus on the procedural dimension of a situation, and verbalization barriers (Hoffman et al., 1995).
Story One (Simplifying the Description of Events): “That Sounds Straightforward!”
Early in October, Dr. X alerted us to a potentially challenging case of a patient who required a “redo” (repeated surgery) because of severe aortic stenosis. Two days after the operation, we conducted a postsurgery interview in which we initially asked Dr. X to describe his perspective on how the situation evolved and what made the situation challenging that day:
We got in safely. The redo sternotomy part, we were very careful. It took about twenty-five, thirty minutes to reopen. It was stuck but we cauterized it off, nothing bled, nothing fibrillated. We said, “Oh, not so bad,” so we put the retractor in and then everything was just completely sundown. The redo sternotomy part, which is always the most fear and trepidation—that was easy. It took about an hour to get rid of all these adhesions….So that was a bit of a challenge. And the other challenge was her aorta was calcified. So when we dissected all the adhesions and got in there, she almost had what we call porceline aorta. So that meant that we had to avoid that area, which then introduced downstream complexities. The tube for the heart–lung machine went in much more beyond that area, like in the distal aortic arch, and then we had to place the ascending aortic clamp much lower than normal….So then we did the job, we cannulated, we went on the heart–lung machine, we stopped the heart, and then we took out the severely calcified aortic valve leaflets and put in a new valve. Finally, when the valve was in, the valve was working fine and the time comes to close the aorta….I think it worked well. I mean, there was that initial negativity because the individual who did the surgical checklist had never met the person before, so actually said, “We’re going to take out the mitral valve,” which was working fine. The patient said, “No, I’m here for an aortic valve replacement.” Yeah, except for that, everything worked reasonably well.
Even though as interviewers we could infer the degree of difficulty that each of the steps described by Dr. X implied, it still felt to us as a stepwise description. Moreover, from our field notes, we were aware that this operation had an additional layer of complexity derived from an external event that took place at the start of the operation. Such an event was minimized in Dr. X’s verbal description.
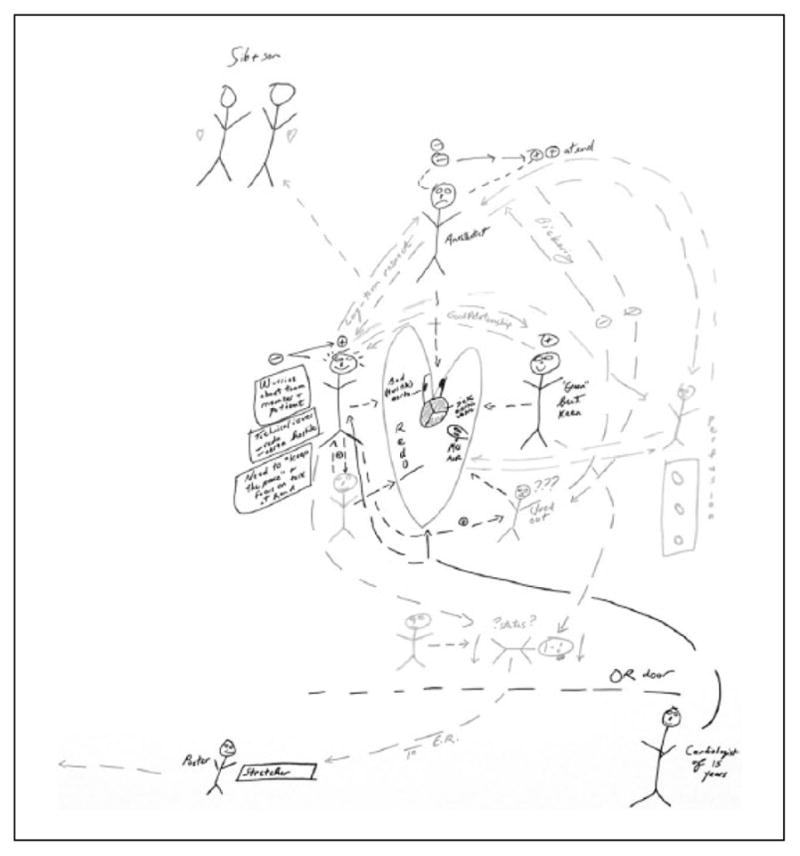
We next asked the surgeon to draw a rich picture for the same situation (see Figure 2), and removed ourselves from the room and allowed Dr. X to take as much time as desired to complete his drawing. Half an hour later, Dr. X invited us back into the room. To our surprise, we found that the initial stepwise description, which sounded like a linear process, was visually represented as an interrelated network of interactions among the team members:
I started with the patient in the center. I wrote inside the heart the technical issues that were applicable here. It’s a redo situation, so I put that within the heart. There’s a sick aortic valve with all the calcium showing in red, and then, there’s this black tube coming out of that valve with the bad or hostile aorta, so that’s just all within the heart. The day started with negative gestalt, so you see the anesthetist, above the patient, looks very unhappy. There’s a double negative, which thankfully does go to a double positive at the end. And then, what happened is there’s a second assistant over here, who’s not the most clued-in individual on the best of days. That individual, unfortunately, clued out this morning, and because I was delayed getting to the operating room, started the surgical checklist, which bore no relationship to the issue at hand. For instance, the operation that this individual said we planned was a redo mitral valve replacement, which the mitral valve was fine; it was the aortic valve that was the issue.
That then led to some very negative interactions between this second assistant and the anesthetist, who have fought in the past, so of course it’s never just a one-off; there’s always a preamble. And then, added to the mix, our illustrious team member, a research team member fell….And then, with the negative gestalt at the beginning for a multiplicity of reasons, there was need to keep the peace and get people focused into a complex surgery….Even though the surgeon might not admit it, the surgeon is always sweating, either literally or figuratively. Initially they’re so worried about the team member who dropped, and the patient, and then the technical issues, and then the need to keep everybody on the same page and have a positive gestalt instead of a negative gestalt….If there’s anything at all positive in terms of a team member going down and smacking their face, it’s that the bickering stopped.
This one [rich picture] is very much about relationships. Those arrows circulating around the patient really gives you that sense of what’s going on around them. They’re in the middle; there’s that operation, but this one is particularly about these relationships, everything that’s happening around the patient. It’s a good way of describing what’s going on…and that’s how I sort of perceived it. Fortunately, the patient did well and has had an uneventful post-op [postoperative] course.
Figure 2.
Story 2 (focus on the procedural dimension): “I wouldn’t have thought of mentioning that!”
The procedural aspects still remained the same with the representation of the valve replacement at the center, but they appeared to be overshadowed by a layer of arrows connecting people in the room and were labeled with positive and negative signs. By using the rich picture and having the time to himself while drawing it, Dr. X began to describe his thoughts and feelings about how those interactions had deeply affected the mood of the operating room. Moreover, he was able to visually register a key event not described in the interview—the fainting of one of the observers—as the breaking point in the chain of events that allowed him to regain the focus of the team.
Story Two (Focus on the Procedural Dimension): “I Wouldn’t Have Thought of Mentioning That!”
In vascular surgery, abdominal aortic aneurysms are not uncommon, but these become even more challenging with peculiarly unhealthy patients. Many concerns were worrying Dr. Y as he scheduled a patient for surgery. He opted for an image-guided operation to insert an endovascular stent graft to address an abdominal aortic aneurysm. Dr. Y was aware of the patient’s delicate condition, including being a heart transplant recipient, having significant lung disease, and having only one kidney. He knew there was much room for error and therefore he took plenty of time during the interview to organize and describe his decision-making process to us:
With his comorbidities, with the fact that he’s had a heart transplant, with the fact that he has significant lung disease, it’s better to do the smaller operation. However, his anatomy, the short distance to the one kidney, would make it actually better to do the larger operation. However, I don’t think he would survive the larger operation, so we’ve had to, I don’t want to say compromise, but accept some of those factors and choose one route. Now, once we choose that route, in the decision making we have to choose the device or the graft that goes in, and that’s based on the patient’s anatomy and some measurements. I sit down at a computer screen with a CT [Computer Tomography] scan. It usually takes maybe twenty, twenty-five minutes to do the measurements that are required to choose the right device or stent graft. If you choose the wrong one then there are a lot of things that could happen. First of all, it might not adequately repair the aneurysm. It might cover blood vessels that you don’t want to cover, like the blood vessels to the kidney, in this case.
There’s a number of things that could go wrong if you choose the wrong graft. There’s a number of small decisions that have to be made preoperatively. I tell the residents it’s one of those operations where at the end of it, for people who don’t understand the operation, it can look very easy, but there are probably a thousand steps in that operation where you could kill the patient, to put it bluntly. And, at the end of it, if everything looked easy, then great, you made all those decisions correctly…and the operation went very well. Some of the key technical steps where there was very little room for error went well. We succeeded with what we wanted to do, which was at the end of the case, fixing the aneurysm through a minimally invasive approach and dealing with a specific concern, which was the blood supply to the kidney. So, the end result was quite good and the patient did very well after the surgery. He was out of hospital in two days and did well. I was quite happy with the way it went.
While we listened to Dr. Y’s verbal account, we could feel how much he was concerned about making sure that procedural decisions were made correctly.
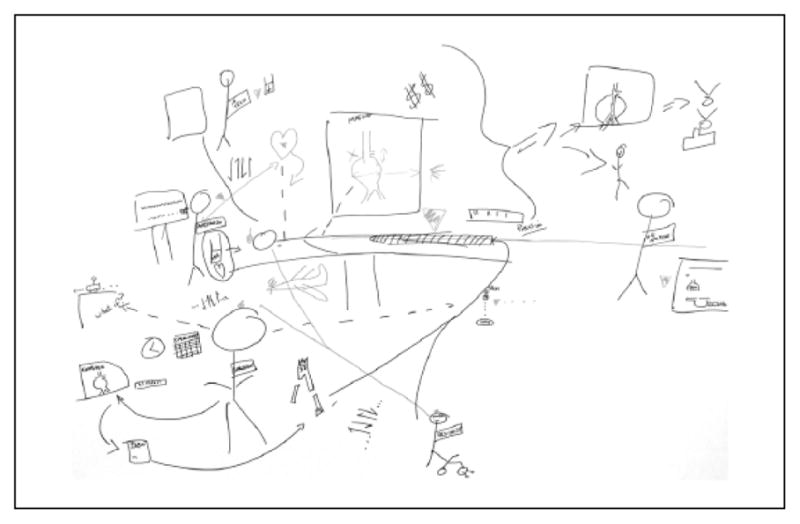
Even though we did not notice any outstanding external events affecting the operation, we began to wonder whether it was just the procedural dimension that made the situation challenging for Dr. Y, or whether there might have been something else overshadowing the procedural dimension, as we had seen in our previous experiences with other surgeons. As one of the most senior surgeons in our study, Dr. Y might have been concerned about another dimension that contributed to his perception of this episode as a challenging event. We kept those concerns in mind as we engaged Dr. Y in drawing a rich picture (see Figure 3).
Figure 3.
Story 3 (verbalization barriers to elucidate tacit knowledge): “I know it’s there, but it’s hard to describe it!”
After half an hour of quiet drawing, Dr. Y invited us into the room with the promise that he had made a discovery:
I think before drawing the picture, the trust thing, I wouldn’t have told you that that would have been one of the themes. But then as I was going through, I was thinking well, the interplay between surgeon and resident, sure it’s the technical aspect, and he comes in and the technical aspect comes together, and the communication, and that’s fine. But how do you depict the trust when you say to the resident, “Okay, you’re going to do this step.” The resident is never going to say, or rarely going say, “No, I can’t do it.” If you say, “Can you do this?” they’ll say yes, whether they can or not. There’s got to be a level of trust based on previous experience, previous interactions. It’s a dynamic….It’s hard sometimes. But I wouldn’t have told you that trust was a theme before I drew the picture [in the form of a William Tell analogy: apples on the heads of the surgeon, the patient, and the resident, joined by red arrows]. As I was thinking about it, I was thinking it is. It’s not just there. It’s trust with anesthesia and trust with the nurses.
Dr. Y used four colors in his rich picture: black, red, yellow, and green. With black he depicted the conduit of the operation from the preplanning to the insertion of the graft. Then he used red, yellow, and green to overlay other aspects that were playing in his mind but were not observable in the room. The one that surprised him (and us) the most was his realization that trusting trainees (drawn in red) was a very important but tacit consideration in his mind. Dr. Y seemed to specifically use the three colors of a traffic light to indicate the level of concern in the negotiation of trust: yellow to describe not only the steps in which careful caution was necessary, but also who in the room should exercise caution and where this caution should be applied; and green to depict the success of the operation as a healthy artery.
Story Three (Verbalization Barriers to Elucidate Tacit Knowledge): “I Know it’s There, But it’s Hard to Describe it!”
On a Sunday at midnight, we received a phone call from Dr. Z advising us to drive to the hospital as soon as possible. A terminal cancer patient had been admitted to the emergency room with a perforation of his viscus. While the perforation presented with challenges itself, the fact that Dr. Z was not familiar with the terminal situation of the patient preoperatively complicated things further. Once we arrived in the operating room, Dr. Z explained why he thought this was a potentially challenging operation. The reaction of the family was emotional on learning that the cancer was terminal, because they apparently were not aware of this situation prior to their arrival at the emergency room. This translated into high expectations from the family about the ability of the surgeon to solve the problem. Being tired, having to talk multiple times to the family, and not having full support from the surgical team on his decision to proceed with the surgery created a personal dilemma that the surgeon found difficult to describe:
If someone has a noncurative tumor and you know from the outset that it’s noncurative, then you have to have that difficult discussion with family and patients about, do we do anything at all?—just let you die from your disease process, this is the end—versus do something. And, so that piece of information is, if you will, it’s kind of like the background in a landscape painting. It’s there, and it’s going to influence your interpretation of what’s going on, whether the sky’s blue or grey is going to change your feel of the painting. So, that is what was going on, kind of overarching everything is this idea that this situation is somewhat palliative….So, my thought process was, well, we can try this. If it works, it will improve his quality of life quite substantially, because he’ll be able to continue with his treatment, and eat and drink and go home. If it doesn’t work, he’s going to die, and he’s going to die anyway, so I might as well try something that’s going to provide him with a good quality of life, rather than something that might be easier for me but not provide good quality of life for him. So, I think that was probably the process that was going on in my brain, although I don’t know that I would say I thought of all those things specifically.
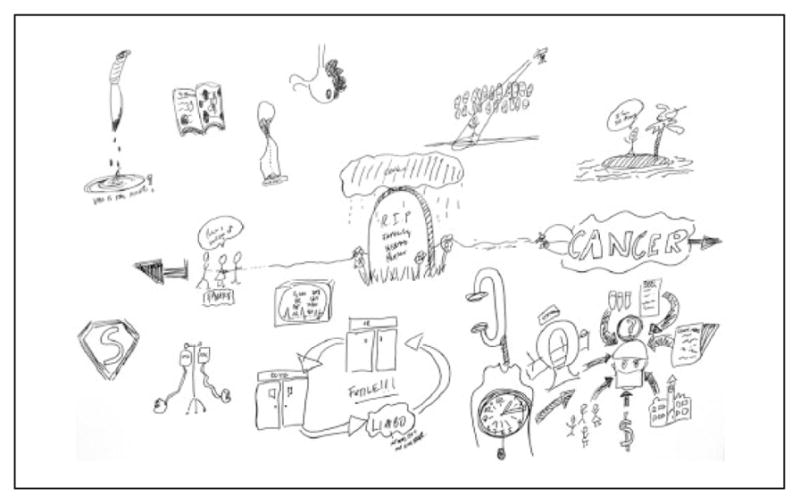
As the interview progressed, it was evident from some of his responses that this case had an emotional effect on the surgeon, although he clearly was having a difficult time trying to express it in words. During the rich picture session (see Figure 4), that emotional aspect became clearer as Dr. Z drew multiple visual metaphors that spoke to feelings of loneliness, frustration, and even guilt:
These are representations that I’ve tried to make of my concerns about operating on this person. They’re more about me, personally. They have nothing really to do with the patient. One is my feeble attempt to drawing a person standing on an island saying that they’re so alone, because when you’re in that situation you have to make these decisions. You have to read the consequences for your decisions and no one else is there, really, with you. And sometimes, patients and their families put you in that situation where they say, “What do you think he should do?” And I don’t really like to ever answer that question because it’s not up to me; it’s up to them to decide. I see my job as giving them information and they’re supposed to decide. But often families in this situation will put you on that island because they don’t want to be the ones responsible for making the decision.
The second is someone standing in the middle of a room with a spotlight on them, with a whole bunch of faces, that are somewhat disapproving, staring at them, which is my representation of morbidity and mortality rounds. Based on my decision making, I’m going to stand in the middle there, even though that doesn’t really happen, but that’s what it feels like. And people might be standing around saying, “Why did you even bother operating on this person? What were you thinking when you did this? This is ridiculous.” You’ve created a problem where there was no problem….I tried to draw an hour glass that, to me, represents the fact that he’s only got a certain amount of time anyway, and no matter what we did, the grains of sand are going to keep ticking down and he’s going to die at some point. So I guess that kind of fits with that feeling of futility, that no matter what we did, the grains of sand are still going to keep dropping. . . .
There’s a textbook there that says the stomach, and then there’s a whole bunch of holes in it because that represents the fact that I had a lot of knowledge. But none of it was really applicable because the fact is that the problem we encountered, it didn’t really fit with anything that a textbook cancer would be….The next thing beside it is very morbid, but I was trying to think of something that represented killing someone, and so it’s a knife with blood dripping off it and the question is, “Who is the killer?” When you operate on these people, you don’t want to be the person that’s pushed them over the edge and kill them. They’re dying of a natural process: their cancer. That’s no one’s fault. But when you intervene and do something and cause them to die because of your intervention, then sometimes you often think inside yourself that you actually killedsomeone, despite the fact you’re trying to help them. You might have made that process faster and they died. So that’s my morbid representation of those thoughts.
Figure 4.
Motifs corresponding to Table 1.
It was a very informative rich picture session from our position as researchers. We sat and mostly listened to an elaborate description of a moral and emotional battle that we suspected beforehand was a major influence in the situation, but we never imagined its extent.
Discussion
Neither a visual nor a verbal representation can offer a complete construction of a situation. The three stories presented in this article have shown the ways in which visual methods, particularly rich pictures, can capture and elucidate potentially hidden aspects of the influence of the context on the judgment of surgical experts during challenging operations.
Recent work, specifically on patients’ perceptions in understanding illness, has demonstrated the usefulness of drawing to explore the multiplicity and complexity of human experience (Guillemin, 2004). We are expanding the applicability of drawings as a research method to include the human experience of practicing in high-stakes professions such as surgery. The ability to examine both the picture content and the motivations behind making a picture adds a new vantage point from which to describe how experts see a challenging situation in their professional practice; however, it is the reciprocity between participants and researchers during the interpretation of the pictures that has allowed us to uncover social, cultural, and personal dimensions that play a role in the complexity of challenging surgical operations. This reciprocity was more effectively achieved when the participants engaged in two different forms of expression, which were the interviews and the drawings. For example, Dr. Y realized that in his mind there was more than the technical dimension and the communication dimension playing a role in the operation. It was not until he had the opportunity to sit down and draw for half an hour that he was able to find a way to represent additional dimensions.
We acknowledge that given the nature of the participants—surgeons with a very busy clinical agenda—the required amount of engagement time with the study might have prevented some surgeons from participating. However, as SE scholars contend, exploring complexity requires both a detailed and a contextually sensitive exploratory approach (Gharajedaghi, 2011; Johnson, 2006; Rouse, 2003). Such an approach therefore requires a progressively deeper engagement with the situation by researchers and participants to foster a coconstructed understanding of the situation as it evolves. These requirements impose limitations that researchers need to be cognizant of when designing the scale of the studies when using visual methods, such as rich pictures.
As researchers, the process of moving the participants from the interview as a verbal form of expression to using rich pictures as a pictorial form helped us to realize that we also needed to adapt the ways such reciprocity is developed. During the interviews, we acted primarily as recipients of information, sometimes to the extent of feeling taught. During the drawing sessions, we noticed how participants, at times, invited our input to support their construction of the meaning of the pictures. The latter likely comes from the fact that we were present at each of those operations. For instance, Dr. X’s attempt to depict the fainting researcher was carefully considered in conversation with the affected individual. We therefore found that using both interviews and rich pictures was a strength of our study. Both types of data uncovered different aspects of the topic under investigation; however, it was the order in which they occurred, beginning with the interview and then drawing in a separate session, that allowed for deeper reflexivity.
Interviews served to open the door into the surgeons’ perspectives while they tried to satisfy the researchers’ curiosity. Drawing was perceived as a more personal experience as they tried to satisfy their own curiosity. Although surgeons frequently apologized for their imperfect artwork and the challenge of being taken out of their comfort zone by drawing, all participants commented on the feeling of having time to themselves to think and draw as a liberating experience. Sharing their pictures with us was perceived by the surgeons to be their opportunity to disclose their feelings about what was really important to them. These benefits to the researchers also translate into benefits for the participants. According to the surgeons, the interview constituted the recollection of events, whereas the drawing constituted on opportunity to reflect on the overall situation and on new things they encountered or learned that would shape how they understand other complex situations in the future. As one surgeon commented, “Drawing is an opportunity to reflect on what happened, rather than to just list step one, step two, step three.”
Research conducted using other visual methods, such as the Pictor Technique (King et al., 2013), has also recently demonstrated the capability of participant-generated visual data to more reflectively engage health professionals in the interpretation of their experiences. Similar to the Pictor Technique, rich pictures are used to elicit more reflective participation in the interviewing process. From the descriptions of the Pictor Technique (King et al.), it seems that the analytical emphasis is on the interviews. Rich pictures constitute another source of data, in addition to the interviews, which are analyzed separately from the interviews. The ability to offer participants an additional and less-structured avenue to visually represent their perspectives on complex issues adds to the depth of the analytical interpretation by allowing participants and researchers to engage more actively in the coconstruction of meaning. During the aesthetic analysis, researchers have the opportunity to share their interpretations of the motifs chosen by the participants, and conversely, participants have the opportunity to further reflect on those choices.
Using visual methods to design research in which the goal is to capture complexity might constitute an analytical advantage because it confers the opportunity to produce information that would not otherwise be accessed. The use of drawings has been confined to research with children; however, recent work has begun to show the potential of using drawings in research with adults (Guillemin, 2004; Martin, 1994, as cited in Guillemin, 2004; Victora & Knauth, 2001 as cited in Guillemin, 2004). In our research on medical expertise, experts were given the opportunity to decide how to portray their perspectives, which produced an abundance of visual metaphors that not only facilitated the elucidation of tacit knowledge but which also stimulated more meaningful researcher–participant interactions.
Conclusion
The use of visual methods, in this case rich pictures, allowed us to capture experts’ perspectives on the multiple dimensions of challenging situations. In the domain of surgery, visual methods helped address three issues that commonly surface in interview-only research with experts: the tendency to simplify descriptions of complex situations, the tendency to focus on the procedural dimension of a situation, and verbalization barriers. The use of visual metaphors constituted a powerful language that surgeons found helpful in depicting the real complexity of the situation; therefore, the three issues were greatly reduced. Furthermore, visual methods seemed to increase engagement between researchers and participants, allowing for a more comfortable environment in which experts used the drawing activity as an opportunity to coconstruct their experiences by regarding researchers as meaningful participants. As a qualitative study, this process promoted reciprocity, reflexivity, and trustworthiness as markers of rigor (Harrison et al., 2001). From our experience with expert surgeons, we suggest that combining interviews with visual data will facilitate a more thorough understanding of and the generation of richer theoretical accounts of complex phenomena.
Acknowledgments
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Canadian Institutes of Health Sciences (CIHR), Royal College of Physicians and Surgeons of Canada (RCPSC).
Biographies
Sayra Cristancho, PhD, is an assistant professor, Department of Surgery, and a scientist, Centre for Education Research & Innovation, Western University, London, Ontario, Canada.
Susan Bidinosti, AOCA, is a research associate, Centre for Education Research & Innovation, Western University, London, Ontario, Canada.
Lorelei Lingard, PhD, is a professor, Department of Medicine, and director and scientist, Centre for Education Research & Innovation, Western University, London, Ontario, Canada.
Richard Novick, MD, MSc, FRCSC, FACS, is a professor, Department of Surgery, Division of Cardiac Surgery, Western University, London, Ontario, Canada.
Michael Ott, MD, MSc, FRCSC, FACS, is an associate professor, Department of Surgery, Division of General Surgery, Western University, London, Ontario, Canada.
Tom Forbes, MD, FRCSC, FACS, is a professor and division chair/chief, Department of Surgery, Division of Vascular Surgery, Western University, London, Ontario, Canada.
Footnotes
“Return-of-finding” refers to follow-up meetings with participants in which preliminary findings are discussed to achieve consensus in the interpretation and analysis of the data.
Conceptual dimensions of systems engineering: System structure (nested systems, dimensions), system functions and purposes (intentions, contradictions, dilemmas), systems dynamics and evolution (feedback loops, flow, emergence), multiple-causality, simultaneity.
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Armson R. Systems thinking for messy situations. Axminster, United Kingdom: Triarchy Press; 2011. [Google Scholar]
- Bell E, Davison J. Visual management studies: Empirical and theoretical approaches. International Journal of Management Reviews. 2012;15(2):167–184. doi: 10.1111/j.1468-2370.2012.00342.x. [DOI] [Google Scholar]
- Boardman J, Sauser B. Systems thinking: Coping with 21st Century problems. Boca Raton, FL: CRC Press; 2008. [Google Scholar]
- Bornstein BH, Emler AC. Rationality in medical decision making: A review of the literature on doctors’ decision-making biases. Journal of Evaluation in Clinical Practice. 2001;7(2):97–107. doi: 10.1046/j.1365-2753.2001.00284.x. [DOI] [PubMed] [Google Scholar]
- Crandall B, Klein GA, Hoffman RR. Working minds: A practitioner’s guide to cognitive task analysis. Cambridge, MA: MIT Press; 2006. [Google Scholar]
- Cristancho S, Lingard L, Regehr G. Attending to the whole and its parts: Seeing expertise-in-context through the lens of systems engineering. 2014 Manuscript submitted for publication. [Google Scholar]
- Cristancho S, Vanstone M, Apramian T, Lingard L, Ott M, LeBel ME. When surgeons face intraoperative challenges: A naturalistic conceptualization. American Journal of Surgery. 2013;205(2):156–162. doi: 10.1016/j.amjsurg.2012.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cristancho S, Vanstone M, Apramian T, Ott M, Novick R, Lingard L. Implications of a theoretical model of intraoperative decision-making for surgical education. 2014 Manuscript submitted for publication. [Google Scholar]
- Dawson NV. Systematic errors in medical decision making. Journal of General Internal Medicine. 1987;2(3):183–187. doi: 10.1007/BF02596149. [DOI] [PubMed] [Google Scholar]
- Detmer DE, Fryback DG, Gassner K. Heuristics and biases in medical decision-making. Academic Medicine. 1978;53(8):682–683. doi: 10.1097/00001888-197808000-00012. Retrieved from http://journals.lww.com/academicmedicine/Abstract/1978/08000/Heuristics_and_biases_in_medical_decision_making.12.aspx. [DOI] [PubMed] [Google Scholar]
- Durning S, Artino AR, Pangaro L, van der Vleuten CP, Schuwirth L. Context and clinical reasoning: Understanding the perspective of the expert’s voice. Medical Education. 2011;45(9):927–938. doi: 10.1111/j.1365-2923.2011.04053.x. [DOI] [PubMed] [Google Scholar]
- Durning SJ, Artino AR. Situativity theory: A perspective on how participants and the environment can interact. AMEE Guide No. 52. Medical Teacher. 2011;33(3):188–199. doi: 10.3109/0142159X.2011.550965. [DOI] [PubMed] [Google Scholar]
- Durning SJ, Artino AR, Boulet JR, Dorrance K, van der Vleuten C, Schuwirth L. The impact of selected contextual factors on experts’ clinical reasoning performance (does context impact clinical reasoning performance in experts?) Advances in Health Sciences Education. 2012;17(1):65–79. doi: 10.1007/s10459-011-9294-3. [DOI] [PubMed] [Google Scholar]
- Durning SJ, Artino AR, Jr, Pangaro LN, van der Vleuten C, Schuwirth L. Perspective: Redefining context in the clinical encounter: Implications for research and training in medical education. Academic Medicine. 2010;85(5):894–901. doi: 10.1097/ACM.0b013e31-81d7427c. [DOI] [PubMed] [Google Scholar]
- Ericsson KA. The influence of experience and deliberate practice on the development of superior expert performance. In: Ericsson KA, Charness N, Feltovich PJ, Hoffman RR, editors. The Cambridge handbook of expertise and expert performance. Cambridge, United Kingdom: Cambridge University Press; 2006a. pp. 683–703. [Google Scholar]
- Ericsson KA. Protocol analysis and expert thought: Concurrent verbalizations of thinking during experts’ performance on representative tasks. In: Ericsson KA, Charness N, Feltovich PJ, Hoffman RR, editors. The Cambridge handbook of expertise and expert performance. Cambridge, United Kingdom: Cambridge University Press; 2006b. pp. 223–242. [Google Scholar]
- Flick U. Managing quality in qualitative research. Thousand Oaks, CA: Sage; 2008. [Google Scholar]
- Gharajedaghi J. Systems thinking: Managing chaos and complexity: A platform for designing business architecture. Burlington, VT: Elsevier; 2011. [Google Scholar]
- Guillemin M. Understanding illness: Using drawings as a research method. Qualitative Health Research. 2004;14:272–289. doi: 10.1177/1049732303260445. [DOI] [PubMed] [Google Scholar]
- Harrison J, MacGibbon L, Morton M. Regimes of trustworthiness in qualitative research: The rigors of reciprocity. Qualitative Inquiry. 2001;7(3):323–345. doi: 10.11-77/107780040100700305. [DOI] [Google Scholar]
- Hoffman RR, Shadbolt NR, Burton AM, Klein G. Eliciting knowledge from experts: A methodological analysis. Organizational Behavior and Human Decision Processes. 1995;62(2):129–158. doi: 10.1006/obhd.1995.1039. [DOI] [Google Scholar]
- Johnson CW. What are emergent properties and how do they affect the engineering of complex systems? Reliability Engineering & System Safety. 2006;91(12):1475–1481. doi: 10.1016/j.ress.2006.01.008. [DOI] [Google Scholar]
- King N, Bravington A, Brooks J, Hardy B, Melvin J, Wilde D. The Pictor technique: A method for exploring the experience of collaborative working. Qualitative Health Research. 2013;23:1138–1152. doi: 10.1177/1049732313495326. [DOI] [PubMed] [Google Scholar]
- Klein G. The recognition-primed decision (RPD) model: Looking back, looking forward. Mahwah, NJ: Lawrence Erlbaum; 1997. [Google Scholar]
- Klein GA. Decision making in action: Models and methods. Norwood, NJ: Ablex; 1995. [Google Scholar]
- Klein GA, Orasanu JE, Calderwood RE, Zsambok CE. Decision making in action: Models and methods. Norwood, NJ: Ablex; 1993. [Google Scholar]
- Klein JG. Five pitfalls in decisions about diagnosis and prescribing. BMJ: British Medical Journal. 2005;330(7494):781. doi: 10.1136/bmj.330.7494.781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koens F, Mann KV, Custers EJ, Ten Cate OT. Analysing the concept of context in medical education. Medical Education. 2005;39(12):1243–1249. doi: 10.1111/j.1365-2929.2005.02338.x. [DOI] [PubMed] [Google Scholar]
- Moulton CA, Regehr G, Lingard L, Merritt C, MacRae H. Slowing down to stay out of trouble in the operating room: Remaining attentive in automaticity. Academic Medicine. 2010a;85(10):1571–1577. doi: 10.1097/ACM.0b013e3181f073dd. [DOI] [PubMed] [Google Scholar]
- Moulton CA, Regehr G, Lingard L, Merritt C, MacRae H. ‘Slowing down when you should’: Initiators and influences of the transition from the routine to the effortful. Journal of Gastrointestinal Surgery. 2010b;14(6):1019–1026. doi: 10.1007/s11605-010-1178-y. [DOI] [PubMed] [Google Scholar]
- Mylopoulos M, Regehr G. Cognitive metaphors of expertise and knowledge: Prospects and limitations for medical education. Medical Education. 2007;41(12):1159–1165. doi: 10.1111/j.1365-2923.2007.02912.x. [DOI] [PubMed] [Google Scholar]
- Mylopoulos M, Regehr G. Putting the expert together again. Medical Education. 2011;45(9):920–926. doi: 10.1111/j.1365-2923.2011.04032.x. [DOI] [PubMed] [Google Scholar]
- Norman G, Eva K, Brooks L, Hamstra S. Expertise in medicine and surgery. In: Ericsson KA, Charness N, Feltovich PJ, Hoffman RR, editors. The Cambridge handbook of expertise and expert performance. Cambridge, United Kingdom: Cambridge University Press; 2006. pp. 339–353. [Google Scholar]
- Pimmer C, Pachler N, Genewein U. Reframing clinical workplace learning using the theory of distributed cognition. Academic Medicine. 2013;88(9):1239–1245. doi: 10.1097/ACM.0b013e31829eec0a. [DOI] [PubMed] [Google Scholar]
- Rouse WB. Engineering complex systems: Implications for research in systems engineering. Systems, Man, and Cybernetics, Part C: Applications and Reviews, IEEE Transactions on. 2003;33(2):154–156. doi: 10.1109/TSMCC.2003.813335. [DOI] [Google Scholar]
- Sandelowski M. Rigor or rigor mortis: The problem of rigor in qualitative research revisited. Advances in Nursing Science. 1993;16(2):1–8. doi: 10.1097/00012272-199312000-00002. Retrieved from http://journals.lww.com/advancesinnursingscience/abstract/1993/12000/rigor_or_rigor_mortis__the_problem_of_rigor_in.2.aspx. [DOI] [PubMed] [Google Scholar]
- Tversky A, Kahneman D. The framing of decisions and the psychology of choice. In: Wright G, editor. Behavioral decision making. New York: Springer; 1985. pp. 25–41. [DOI] [PubMed] [Google Scholar]


