Abstract
Objective
As independent trials have provided evidence for the efficacy and effectiveness of the dissonance-based Body Project eating disorder prevention program, the present trial tested whether clinicians produce the largest intervention effects, or whether delivery can be task-shifted to less expensive undergraduate peer educators or to Internet-delivery without effect size attenuation, focusing on acute effects.
Method
680 young women (M age = 22.2, SD = 7.1) recruited at colleges in 2 states were randomized to clinician-led Body Project groups, peer-led Body Project groups, the Internet-based eBody Project or an educational video control condition.
Results
Participants in all three variants of the Body Project intervention showed significantly greater reductions in eating disorder risk factors and symptoms than educational video controls. Participants in clinician-led and peer-led Body Project groups showed significantly greater reductions in risk factors than eBody Project participants, but effects for the two types of groups were similar. Eating disorder onset over 7-month follow-up was significantly lower for peer-led Body Project group participants versus eBody Project participants (2.2% vs. 8.4%), but did not differ significantly between other conditions.
Conclusions
The evidence that all three dissonance-based prevention programs outperformed an educational video condition, that both group-based interventions outperformed the Internet-based intervention in risk factor reductions, and that the peer-led groups showed lower eating disorder onset over follow-up than the Internet-based intervention is novel. These acute-effects data suggest that both group-based interventions produce superior eating disorder prevention effects than the Internet-based intervention and that delivery can be task-shifted to peer leaders.
Keywords: prevention, body dissatisfaction, eating disorder, dissonance, delivery
Eating disorders affect 13–15% of females and are marked by chronicity, relapse, distress, functional impairment, and increased risk for future obesity, depression, suicide, and mortality (Allen, Byrne, Oddy, & Crosby, 2013; Arcelus, Mitchell, Wales, & Nielsen, 2011; Stice, Marti, & Rohde, 2013). Because 80% of individuals with eating disorders do not receive treatment (Swanson, Crow, Le Grange, Swendsen, & Merikangas, 2011), a public health priority is to broadly implement effective eating disorder prevention programs.
Only three prevention programs have significantly reduced eating disorder symptom composite measures (Atkinson & Wade, 2014; Stice, Marti, Spoor, Presnell, & Shaw, 2008; Stice, Rohde, Shaw, & Marti, 2013) and only three have significantly reduced future onset of threshold or subthreshold eating disorders (Martinsen et al., 2014; Stice et al., 2008; Stice, Rohde, Shaw et al., 2013). However, only the Body Project has produced effects in multiple efficacy trials conducted by independent teams and produced significantly larger intervention effects than credible alternative interventions (Becker, Smith, & Ciao, 2005; Halliwell & Diedrichs, 2014; Mitchell, Mazzeo, Rausch, & Cooke, 2007; Serdar et al., 2014; Stice, Shaw, Burton, & Wade, 2006; Stice et al., 2008), the latter is critical because it provides evidence that the effects are not simply due to expectancies and demand characteristics inherent to randomized trials. Independent replication and evidence that a prevention program significantly outperforms credible alternative interventions are both essential to justify broad implementation. In the Body Project young women voluntarily critique the thin beauty ideal in verbal, written, and behavioral exercises, which theoretically generates dissonance that prompts participants to reduce their pursuit of this unrealistic ideal because people align their attitudes with their publically displayed behaviors. Reduced thin-ideal internalization putatively decreases body dissatisfaction, unhealthy dietary behaviors, negative affect, and eating disorder symptoms, as posited by the dual pathway model of eating disorder development (Stice, Mazotti, Weibel, & Agras, 2000). In support of the intervention theory, reductions in thin-ideal internalization mediate the effects of the Body Project on symptom reductions (Seidel, Presnell, & Rosenfield, 2009; Stice, Presnell, Gau, & Shaw, 2007) and high- versus low-dissonance versions of this program produce greater symptom reductions (Green, Scott, Diyankova, Gasser, & Pederson, 2005; McMillan, Stice, & Rohde, 2011). Further, the Body Project eliminated the adverse effects of exposure to thin models on adolescent girls (Halliwell & Diedrichs, 2014) and reduced objectively measured brain reward region responsivity to thin models (Stice, Yokum, & Waters, 2015). The latter effect is important because women with versus without eating disorders show greater reward region (nucleus accumbens, caudate, amygdala) response to thin models (Fladung et al., 2010; Vocks et al., 2010). Effectiveness trials confirm that the Body Project is effective when delivered by high school and college counselors under ecologically valid conditions (Stice, Butryn, Rohde, Shaw, & Marti, 2013; Stice, Rohde, Butryn, Shaw, & Marti, 2015; Stice, Rohde, Gau, & Shaw, 2009; Stice, Rohde, Shaw, & Gau, 2011) and when delivered by undergraduate peer educators (Becker, McDaniel, Bull, Powell, & McIntyre, 2012; Halliwell, Jarman, McNamara, Rison, & Jankowski, 2015; Stice, Rohde, Durant, Shaw, & Wade, 2013). Peer leaders have cost effectively delivered universal, selective, and indicated prevention programs (Mellanby, Rees, & Tripp, 2000). For certain interventions, peer leaders have been more effective than clinician leaders (Botvin, Baker, Renick, Filazzola, & Botvin, 1984; Leupaker, Johnson, Murray, & Pechacek, 1983; Rhee, Belyea, Hunt, & Brasch, 2011).
To facilitate broad delivery, we developed an unmoderated Internet version of the Body Project that reduced eating disorder risk factors and symptoms in a pilot trial (Stice, Durant, Rohde, & Shaw, 2014; Stice, Rohde, Durant, & Shaw, 2012). Another team found that an Internet version of this prevention program delivered with a synchronous moderator who coordinated on-line discussions among members assigned to virtual groups reduced body dissatisfaction, but not eating disorder symptoms (Serdar et al., 2014).
As independent efficacy and effectiveness trials provide support for the Body Project, and Internet versions of the Body Project have received preliminary support, the next step is to test whether clinicians produce the largest intervention effects or whether delivery can be task-shifted to more abundant and cost-effective undergraduate peer educators or to Internet-delivery without loss of effectiveness. The present trial evaluated the relative effectiveness of clinical-led Body Project groups, peer-led Body Project groups, and the Internet-delivered eBody Project in relation to an educational video control condition. Participants completed assessments of outcomes at pretest, posttest (4-weeks later), and at 6, 12, 24, and 36-month follow-ups. The present report focuses on acute effects at posttest and 6-month follow-up: the longer-term effects will be reported subsequently. We selected an educational video as a comparison condition because it is important to establish that a prevention program produces larger reductions in outcomes than observed in alternative interventions. The educational video comparison condition produced somewhat larger reductions in outcomes than observed in assessment-only controls (Stice et al., 2012), and it seemed more ethical to examine a comparison condition that produces some benefit for participants. Further, it seemed reasonable to strive to outperform a comparison intervention that could be very widely delivered at low cost. We focused on female college students because eating disorders often emerge during college (Stice, Marti et al., 2013), there are over 10 million female college students in the US (US Department of Education, 2008), and colleges typically have an infrastructure for delivering prevention programs. Our primary outcomes were reductions in eating disorder symptoms and eating disorder onset during follow-up; secondary outcomes were risk factors that have been found to predict future onset of eating disorders (Killen et al., 1996; Stice, Gau, Rohde, & Shaw, 2016), including thin-ideal internalization, body dissatisfaction, and negative affect.
Method
Participants and Procedure
Participants were 680 women (M age = 22.2, SD = 7.1; M BMI [kg/m2] = 25.5, SD = 5.6) recruited from 3 universities in Oregon and Texas. An a priori power analysis indicated that with cell sizes of 160 we would have a power of .88 to detect a 9% reduction in the incidence of eating disorder onset over 3-year follow-up (a medium effect that translated into a hazard ratio of 2.5), which is the magnitude of the reduction in eating disorder onset over 3-year follow-up observed in Body Project participants versus assessment-only control participants in a large efficacy trial (Stice et al. 2008); we oversampled slightly to guard against effect size shrinkage. We powered this study for the most stringent analytic test, based on the logic that we would have ample power for less stringent tests. The sample was 60% White, 17% Latina, 14% Asian, 5% African American, 3% Native Americans, 1% Pacific Islander. Average parental education was 13% high school graduate, 16% some college, 34% college graduate, and 38% graduate or professional degree.
Participants were recruited between March 2013 – April 2015 using email messages and posters. Interested women (undergraduate students, graduate students, and university staff) were directed to an enrollment webpage that confirmed that they had body dissatisfaction (the sole inclusion criterion) and administered the Eating Disorder Diagnostic Scale (EDDS, Stice, Fisher, Martinez, 2004); individuals who endorsed diagnostic criteria for current DSM-IV anorexia nervosa, bulimia nervosa, and binge eating disorder, were not affiliated with the university, or were already participating in another trial evaluating an intervention (e.g., an obesity prevention trial) were excluded (the exclusion criteria). Eligible participants were randomly assigned to clinician-led Body Project groups (n = 173), peer-led Body Project groups (n = 162), the eBody Project (n = 184), or an educational video condition (n = 161) via a random number table. Undergraduate students, graduate students, and staff were assigned to the same groups.
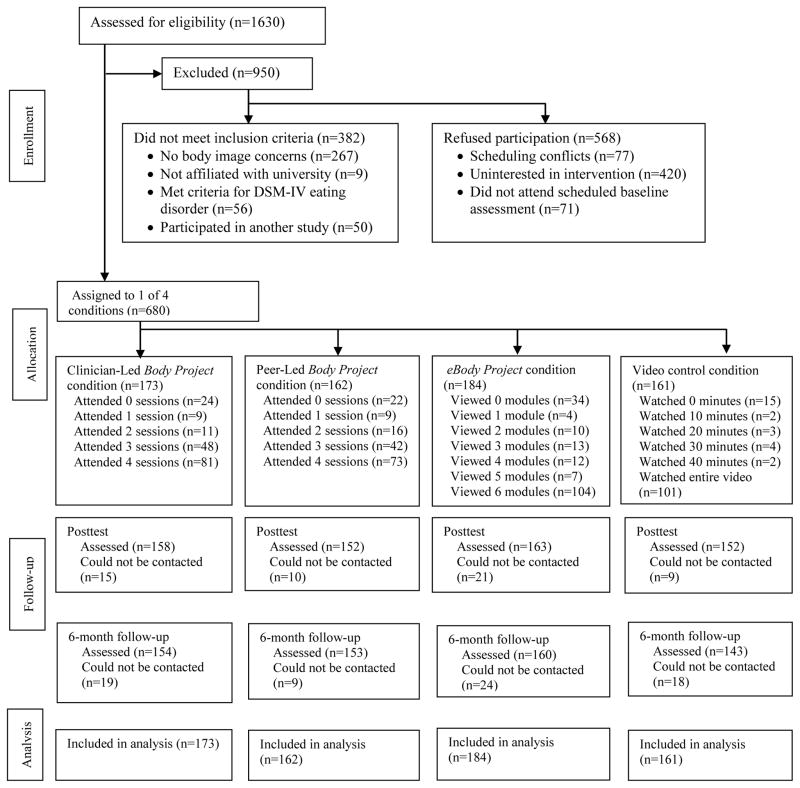
Figure 1 provides a participant flowchart. Participants were paid $15 for completing the baseline assessment, $30 for the posttest assessment, and $40 for the 6-month follow-up assessment. We attempted to collect data from all participants at each assessment, even if they did not provide data at an earlier assessment. Trained female assessors were masked to condition. Participants provided written informed consent after receiving a study description. The institutional review board at each university approved this project.
FIGURE 1.
Participant Flow throughout Study
Interventions
Body Project
The Body Project consisted of 4 weekly 1-hour group sessions with 5–9 participants delivered by either clinician or peer leaders using a scripted manual. Participants voluntarily engaged in verbal, written, and behavioral exercises in which they critiqued the beauty ideal during the sessions and in home exercises (see Stice, Butryn et al., 2013 for details regarding session content).
We approached clinicians responsible for providing mental health care to students at the student mental health clinic, psychology clinic, and counseling clinic on campuses to identify clinicians interested in providing Body Project groups. We worked with the 2–4 clinicians who voiced an interest (none were excluded). Nearly half of the clinicians were graduate students who provided mental health care as part of their training. We typically had to train replacement clinicians because of turnover. We approached peer educator programs on each campus to identify students interested in providing Body Project groups to fellow students. We trained 2–14 peer educators at each campus, due to variation in size of peer educator programs. We invited peer educators who exhibited the greatest competence in delivering the material during the training workshop (based on our observations) and who had greater availability to implement the Body Project. In total 17 clinician leaders (95% female; 82% White; 6% Hispanic; age M [SD] = 33.8 [10.1] years, range = 24 – 55) and 21 peer leaders (94% female; 81% White; 5% Hispanic; age M [SD] = 20.9 years [0.9], range = 19 – 22) were recruited. Pairs of facilitators delivered the intervention.
Facilitator training involved reading the manual and attending a training workshop that was 4 hrs for clinicians and 8 hrs for peer educators. During the workshops the conceptual theory for the Body Project was presented, the empirical support for the intervention was summarized, solutions to common challenges in implementing Body Project groups were discussed, and facilitators practiced implementing each session in role-plays, receiving feedback on their performance. The training was longer for peer educators to give them more practice delivering the sessions because they had less experience implementing scripted group-based interventions.
Drs. Rohde and Shaw reviewed video-recordings of facilitators’ first group and a randomly selected 50% of the remaining sessions. Facilitators were sent supervisory e-mail messages that praised them for positive behaviors and offered constructive suggestions. Key elements of each session were rated for degree of accurate presentation (10-point scale from 1 = No adherence; the section was skipped to 10 = Perfect; all material in the section was presented as written). Facilitator competence was rated with 12 items (e.g., leaders express ideas clearly and at an appropriate pace) using a 10-point scale with behavioral anchors for each item (e.g., 2 = Poor; leaders are difficult to follow and session proceeds at an uncomfortable pace, 10 = Superior; leaders are unusually articulate and express ideas in way that all group members understand; perfect pace). Drs. Rohde and Shaw independently coded a randomly selected 50% of sessions to assess inter-rater agreement for intervention fidelity and competence ratings; intraclass correlation coefficient (ICC) was .78 for fidelity and .84 for competence.
eBody Project
The eBody Project is an Internet-based version of this intervention that includes 6 40-minute modules (equal in time to the group intervention) involving user-driven self-education activities and games (e.g., texting role-plays), and also parallels the group program in that activities are voluntary and highly accountable (see Stice et al., 2012 for details regarding the intervention content).
Educational video condition
Participants were asked to view Dying to Be Thin (WGBH Video, 2000), a 55-min documentary on eating disorders, body dissatisfaction, and body acceptance. Participants were sent a link to a web page where they could view the video for free.
Measures
Thin-ideal internalization
Because participants are no longer responding to items from the Ideal-Body Stereotype Scale that refer to curvy and shapely bodies as reflecting the same appearance ideal that is captured by the rest of the items, which reduced internal consistency in recent studies (Stice et al., 2012), we rewrote several items to capture the following facets of the thin ideal: physical fitness, a shapely buttocks, and large breasts. The new scale, referred to as the Thin-Ideal Internalization Scale (TIIS), used a response format ranging from 1 = strongly disagree to 5 = strongly agree. Items were averaged for this scale and those described below. The TIIS showed a mean α = .75 across assessments in the present trial. The original scale, which shared most items, had shown 2-week test-retest reliability (r = .80), predictive validity for bulimic symptom onset, and sensitivity to detecting intervention effects (Stice et al., 2008).
Body dissatisfaction
Items from the Satisfaction and Dissatisfaction with Body Parts Scale (Berscheid, Walster, & Bohrnstedt, 1973) assessed satisfaction with 9 body parts with a response scale ranging from 1 = extremely satisfied to 6 = extremely dissatisfied. It has shown internal consistency (α = .94), 3-week test-retest reliability (r = .90), predictive validity for bulimic symptom onset, and sensitivity to detecting intervention effects (Stice et al., 2008); mean α = .86.
Negative affect
The sadness, guilt, and fear/anxiety subscales from the Positive Affect and Negative Affect Scale-Revised (PANAS-X; Watson & Clark, 1992) assessed negative affect. Participants reported the extent to which they had felt various negative emotional states on scales ranging from 1 = very slightly or not at all to 5 = extremely. It has shown internal consistency (α = .95), 3-week test-retest reliability (r = .78), convergent validity, predictive validity for bulimic symptom onset, and sensitivity to detecting intervention effects (Stice et al., 2006; Watson & Clark, 1992); mean α = .94.
Eating disorder symptoms and diagnoses
The semi-structured Eating Disorder Diagnostic Interview (EDDI) assessed DSM-IV eating disorder symptoms. The following symptoms were assessed on a month-by-month basis during intervention delivery and follow-up: frequency of binge eating, vomiting, laxative/diuretic use, fasting, and excessive exercise; overvaluation of weight/shape and frequency of feeling fat and fear of weight gain were rated on 0–6 point scales. Participants who endorsed binge eating were asked about distress regarding binge eating, rapid eating, eating until uncomfortably full, eating large quantities of food when not hungry, eating alone because of embarrassment, feeling disgusted, depressed, or guilty after overeating, using yes or no ratings. Items assessing symptoms in the past month were summed to form a composite at pretest, posttest, and 6-month follow-up. This composite has shown internal consistency (α = .92), inter-rater agreement (ICC r = .93), 1-week test-retest reliability (ICC r = .95), predictive validity, and sensitivity to detecting intervention effects (Burton & Stice, 2006; Stice et al., 2009). The symptom composite showed internal consistency (mean α = .70), inter-rater agreement (ICC = .96; n = 116), and 1-week test-retest reliability (ICC = .96; n = 109). We used the monthly data on eating disorder symptoms to determine the month during which a participant first met criteria for threshold or subthreshold eating disorders, as operationalized in Table 1. EDDI eating disorder diagnoses have shown 1-week test-retest reliability (κ = .79) and inter-rater agreement (κ = .75), sensitivity to detecting intervention effects, and participants with versus without EDDI-diagnosed eating disorders show greater functional impairment, emotional distress, and mental health treatment (Stice et al., 2008, 2013).
TABLE 1.
Diagnostic Criteria for Threshold and Subthreshold Eating Disorders
| Subthreshold anorexia nervosa |
|
| Threshold anorexia nervosa |
|
| Subthreshold bulimia nervosa |
|
| Threshold bulimia nervosa |
|
| Subthreshold binge eating disorder |
|
| Threshold binge eating disorder |
|
| Purging disorder |
|
Note: A diagnosis of threshold or subthreshold AN took precedence over threshold and subthreshold diagnosis of BN and BED, and PD.
Statistical Methods
Model building
Intent-to-treat (ITT) analyses of condition effects were evaluated using a partially nested design (Baldwin, Bauer, Stice, & Rohde, 2011) to account for group variability where participants in two conditions were in clusters and participants in the other two conditions were not. Mixed effects growth models were fit with SAS 9.2 PROC MIXED (SAS/STAT, 2011). Individual variability in outcomes from posttest to 6-month follow-up was modeled as a function of condition, adjusting for pretest outcome values, to ensure that any differences in pretest levels of the outcome did not bias estimates of intervention effects. A condition X time interaction was included (coded in months since posttest) to test whether the reductions in outcomes were significantly stronger at posttest versus 6-month follow-up or vice versa. We first evaluated omnibus condition effects for each outcome followed by six planned comparisons, contrasting each condition pair, reporting the main effect (i.e., condition differences at posttest) and the condition differences at 6-months estimated from model implied least-square means derived from the time and condition X time interactions. Effect sizes are equivalent to Cohen’s d (Feingold, 2009). Missing data were imputed using IVEWare (Raghunathan, Solenberger, & Van Hoewyk, 2016) using baseline levels of the outcomes and demographic factors, with imputed data in 20 data sets analyzed separately; model parameters and standard errors were combined following Rubin (1987). Cox proportional hazard models, fit with the STATA software (StataCorp, 2007) tested whether the incidence of eating disorder onset over follow-up was significantly lower in each condition versus each other condition. Hazard ratios and number needed to treat (NNT; Altman & Andersen, 1999) are provided as measures of effect size. Because hazard models accommodate right censoring, we did not impute missing incidence data.
Results
Preliminary analyses
The outcomes approximated normal distributions, except eating disorder symptoms, which were normalized with a logarithmic transformation. Participants in the 4 conditions did not significantly differ on race, ethnicity, age, year in school, parental education or pretest measures of the outcomes. Table 2 provides means and SDs for outcomes at each assessment point across conditions. Table 3 provides the correlations of outcomes at baseline (correlations range from r = .14 to .45, mean r = .28). Attrition was 9% at posttest and 11% at 6-month follow-up. Attrition was not associated with condition (Cramer’s V = .09, p = .175), but was associated with elevated pretest eating disorder symptoms (d = .49). Models indicated no significant variability attributable to groups in the partially clustered models; but, significant variability attributable to site existed for eating disorder symptoms. Thus, all models were fit as two-level models in which assessment points were nested within individuals with the exception of symptoms, which contained a level-3 random effect for site.
TABLE 2.
Means and standard deviations for outcomes by condition at pretest, posttest, and 6-month follow-up
| Pretest | Posttest | 6-Month Follow-up | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Mean | SD | Mean | SD | Mean | SD | |
| Thin ideal internalization | ||||||
| Clinician-led groups | 3.86 | 0.42 | 3.41 | 0.48 | 3.44 | 0.61 |
| Peer-led groups | 3.86 | 0.44 | 3.43 | 0.57 | 3.45 | 0.51 |
| Internet-delivered | 3.85 | 0.45 | 3.53 | 0.57 | 3.56 | 0.48 |
| Educational video control | 3.87 | 0.42 | 3.73 | 0.41 | 3.68 | 0.50 |
| Body dissatisfaction | ||||||
| Clinician-led groups | 3.64 | 0.66 | 3.03 | 0.66 | 3.16 | 0.71 |
| Peer-led groups | 3.68 | 0.61 | 3.06 | 0.68 | 3.11 | 0.69 |
| Internet-delivered | 3.61 | 0.65 | 3.21 | 0.69 | 3.21 | 0.72 |
| Educational video control | 3.78 | 0.61 | 3.55 | 0.69 | 3.39 | 0.70 |
| Negative affect | ||||||
| Clinician-led groups | 2.33 | 0.83 | 1.81 | 0.67 | 1.88 | 0.71 |
| Peer-led groups | 2.32 | 0.74 | 1.84 | 0.62 | 1.90 | 0.73 |
| Internet-delivered | 2.30 | 0.79 | 1.92 | 0.68 | 1.96 | 0.75 |
| Educational video control | 2.35 | 0.78 | 2.13 | 0.76 | 2.05 | 0.81 |
| Eating disorder symptoms | ||||||
| Clinician-led groups | 17.60 | 12.16 | 8.51 | 7.62 | 8.85 | 8.31 |
| Peer-led groups | 16.70 | 11.89 | 9.38 | 9.02 | 8.87 | 8.83 |
| Internet-delivered | 18.16 | 13.03 | 10.48 | 9.77 | 11.08 | 12.03 |
| Educational video control | 17.05 | 10.90 | 12.89 | 10.48 | 12.55 | 12.44 |
SD = standard deviation.
TABLE 3.
Correlations among Outcomes at Baseline.
| 1 | 2 | 3 | 4 | ||
|---|---|---|---|---|---|
| 1. | Thin-ideal internalization | 1.00 | |||
| 2. | Body dissatisfaction | .14 | 1.00 | ||
| 3. | Negative affect | .21 | .38 | 1.00 | |
| 4. | Eating disorder symptoms | .18 | .32 | .45 | 1.00 |
Among participants in clinician-led groups 47% attended all 4 sessions, 28% attended 3 sessions, 6% attended 2 sessions, 5% attended 1 session, and 14% attend no sessions; 31% completed at least 1 make-up session; participants completed an average of 71% of home exercises. Among participants in peer-led groups, 45% attended all 4 sessions, 26% attended 3 sessions, 9% attended 2 sessions, 6% attended 1 session, and 14% attend no sessions; 29% completed at least 1 make-up session; participants completed an average of 69% of home exercises. Clinician- and peer-led groups did not significantly differ on number of sessions attended (M [SD] = 2.9 [1.4] and 2.8 [1.4], respectively), number of make-up sessions, or percent of homework completed. Greater session attendance and homework completion correlated with larger outcome changes at posttest and follow-up (M r = −.13 and −.11 for clinician- and peer-led groups, respectively), providing evidence of dose-response relations. Ratings of fidelity (clinician-led M [SD] = 75.2 [5.1] vs. peer-led M [SD] = 70.2 [5.2]) and competence (clinician-led M [SD] = 71.7 [8.1] vs. peer-led M [SD] = 65.1 [8.6]) did not significantly differ for the two types of Body Project groups. Among eBody Project participants 57% completed all 6 modules, 10% completed 4–5 modules, 13% completed 2–3 modules, 2% completed 1 module, and 19% completed no modules. Among educational video control participants, 80% reported watching the entire 55-minute video, 8% reported watching only a portion of the video, and 12% reported not watching any of the video.
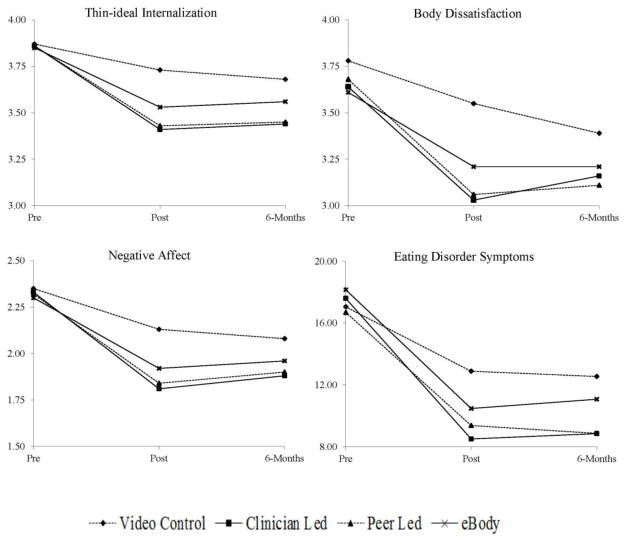
Continuous outcomes
Omnibus tests showed significant overall treatment effects for all three risk factors: thin-ideal internalization (p = .003), body dissatisfaction (p = .003), negative affect (p = .035), and for the primary continuous outcome of eating disorder symptoms (p = .011). The effect sizes and p-values of the tests of differential change for continuous outcomes across all pairs of conditions at posttest and at 6-month follow-up are shown in Table 4. Figure 2 graphs the mean scores at each assessment point across conditions. Clinician-led Body Project participants showed significantly greater reductions in all four continuous outcomes by posttest and 6-month follow-up compared to educational video controls (Figure 2). Clinician-led Body Project versus eBody Project participants showed significantly greater reductions in the three risk factors but not symptoms by posttest, and greater reductions in one risk factor (thin-ideal internalization) by 6-month follow-up. Clinician-led versus peer-led Body Project group participants did not show significantly greater reductions in any continuous outcome by posttest or 6-month follow-up.
TABLE 4.
Effect sizes (d) and Significance Levels for Condition Differences at Posttest and 6-Month Follow-up from Mixed Effects Growth Models
| Outcome Measure | ||||
|---|---|---|---|---|
| Comparison | Thin-ideal internalization | Body dissatisfaction | Negative affect | Eating disorder symptoms |
| Posttest | ||||
| Clinician-led vs. video control | −.56 (<.001) | −.70 (<.001) | −.38 (<.001) | −.52 (<.001) |
| Peer-led vs. video control | −.68 (<.001) | −.71 (<.001) | −.35 (<.001) | −.38 (<.001) |
| Internet vs. video control | −.45 (<.001) | −.34 (<.001) | −.23 (.005) | −.36 (.001) |
| Clinician-led vs. Internet | −.21 (.022) | −.30 (.002) | −.16 (.004) | −.18 (.089) |
| Peer-led vs. Internet | −.22 (.075) | −.31 (.002) | −.12 (.147) | −.02 (.830) |
| Clinician-led vs. Peer-led | −.06 (.478) | −.02 (.791) | −.05 (.553) | −.15 (.152) |
| 6-month follow-up | ||||
| Clinician-led vs. video control | −.39 (<.001) | −.26 (.023) | −.20 (.031) | −.43 (<.001) |
| Peer-led vs. video control | −.52 (<.001) | −.38 (.001) | −.17 (.093) | −.35 (.001) |
| Internet vs. video control | −.23 (.039) | −.09 (.395) | −.07 (.490) | −.26 (.020) |
| Clinician-led vs. Internet | −.22 (.026) | −.12 (.274) | −.13 (.140) | −.18 (.105) |
| Peer-led vs. Internet | −.28 (.014) | −.25 (.027) | −.10 (.314) | −.10 (.347) |
| Clinician-led vs. Peer-led | .00 (.999) | .11 (.355) | −.04 (.636) | −.07 (.513) |
Note. Effect sizes reported first followed by p-values in parentheses. Significant effects are shown in bold. For each comparison the first group is the reference group.
FIGURE 2.
Standardized mean outcomes over time by condition.
Peer-led Body Project group participants showed significantly greater reductions all four continuous outcomes by posttest and significantly greater reductions in all continuous outcomes except negative affect by 6-month follow-up compared to controls (Figure 2). Peer-led Body Project compared to eBody Project participants showed significantly greater reductions in body dissatisfaction by posttest and in thin-ideal internalization and body dissatisfaction by 6-month follow-up but differences on eating disorder symptoms were non-significant.
Finally, eBody Project participants showed significantly greater reductions in all four continuous outcomes by posttest compared to educational video controls (Figure 2). The effects for thin-ideal internalization and eating disorder symptoms were still significant by 6-month follow-up compared to educational video controls.
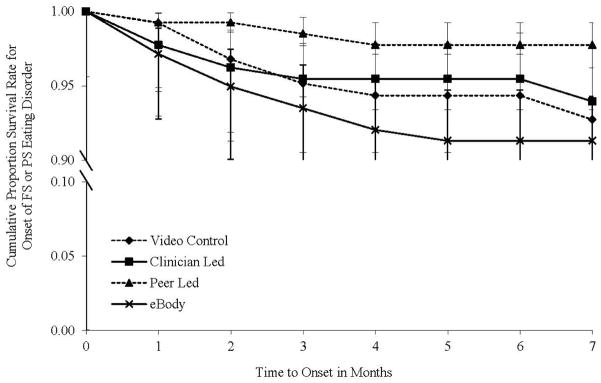
Eating disorder onset
The incidence of eating disorder onset during the 7-month post-baseline follow-up was 7 (5.1%) for clinician-led group participants (subthreshold bulimia nervosa [sBN] = 2, subthreshold binge eating disorder [sBED] = 3, purging disorder = 2 [PD]); 3 (2.2%) for peer-led group participants (sBN = 1, sBED = 2); 12 (8.4%) for eBody Project participants (sBN = 10, sBED = 1, PD = 2 [1 participant exhibited more than 1 eating disorder during follow-up]); and 8 (6.1%) for educational video controls (BN = 1, sBN = 6, BED=1, sBED = 3, PD = 1 [4 exhibited more than 1 eating disorder during follow-up]). Figure 3 shows the cumulative survival rates for onset of any eating disorder in each condition among participants free of these disorders at pretest. The difference in eating disorder onset did not reach statistical significance for clinician-led Body Project versus peer-led Body Project participants (hazard ratio [HR] [95% CI] = 2.39 [0.62–9.24], p = .207, NNT = 26), eBody Project participants (HR [95% CI] = 0.60 [0.24–1.53], p = .291, NNT =38), or educational video participants (HR [95% CI] = 0.83 [0.30–2.30], p = .723, NNT = 81). Eating disorder onset was significantly lower among peer-led Body Project versus eBody Project participants (HR [95% CI] = 0.25 [0.07–0.89], p = .033, NNT = 15). The HR of .25, a large effect, translates into a 74% reduction in eating disorder onset for peer-led Body Project versus eBody Project participants ([8.4 – 2.2]/8.4). Yet, the difference in eating disorder onset did not reach statistical significance for peer-led Body Project versus educational video participants (HR [95% CI] = 0.34 [0.09–1.30], p = .115, NNT = 20) or for eBody Project versus educational video participants (HR [95% CI] = 1.38 [0.56–3.37, p = .483, NNT = 70).
FIGURE 3.
Cumulative survival rates for onset of any threshold or subthreshold DSM-IV eating disorder by condition
Discussion
This report on the acute effects of this effectiveness trial produced several important findings. First, the evidence that clinician-led Body Project groups produced greater reductions in all of the risk factors and in the primary outcome of eating disorder symptoms, than educational video controls, with effects persisting through 6-month follow-up, is novel because the video is an alternative intervention. Likewise, the evidence that peer-led Body Project groups produced greater reductions in both risk factor and eating disorder symptom continuous outcomes than educational video controls, with all but one of the risk factor effects persisting through 6-month follow-up, is also novel for the same reason. The average effect size across the three continuous risk factor outcomes was a d = .42 for clinician-led and d = .47 for peer-led groups, both of which are medium effect sizes. Similarly, the average effect size across follow-up assessments for eating disorder symptoms was d = .48 for clinician-led and d = .36 for peer-led groups, which represent medium and medium-small effect sizes, respectively. When interpreting effects relative to the educational video condition it is critical to note that the average effect size for this educational video relative to an educational brochure control condition was d = .25 (Stice et al., 2012), making this a rigorous comparison condition because it produces a small clinical benefit. Indeed, the fact that a free 55-minute educational video produced an average effect size that is comparable to the average effect size (d = .26) for all eating disorder prevention programs evaluated in a meta-analyses (Stice, Shaw, & Marti, 2007) suggests that future prevention trials should use this video as a minimal-intervention comparison condition, rather than the typical assessment-only control condition. This is because the educational video comparison condition would ensure that participants in all conditions show at least some benefit, would better equate intervention versus control condition on expectancies and demand characteristics, and it seems laudable to strive to outperform such an easy and inexpensive intervention. However, it would also be useful to compare any new eating disorder prevention program to the extant prevention program with the strongest evidence-base, as this would accelerate identification of even more effective prevention programs. Only a handful of trials have compared eating disorder prevention programs to other efficacious programs. Reducing thin-ideal internalization, body dissatisfaction, and negative affect is important because each has been found to increase risk for future onset of eating disorders (e.g., Killen et al., 1996; Stice et al., 2016). It will be important to determine wherther these effects, and those reported below, persist over longer-term follow-up.
Second, the finding that clinician-led Body Project groups produced greater reductions in the three risk factors than the eBody Project is a novel contribution both because this too is a credible alternative intervention and more importantly because it contains similar content to the group-based Body Project. However, there were no significant effects for the clinician-led versus internet-delivered interventions for eating disorder symptoms and only one of the risk factor effects persisted through 6-month follow-up. The Body Project has now produced significantly larger effects for both eating disorder risk factors and symptoms than seven alternative interventions, including an educational video, expressive writing, a media advocacy prevention program, a psychoeducational prevention program, a healthy weight prevention program, a low-dissonance versions of the Body Project, and now an Internet-delivered version of the Body Project. The fact that the Body Project has produced greater reductions in certain outcomes than credible comparison conditions reduces the possibility that expectations or demand characteristics are responsible for the reductions in outcomes observed among Body Project participants. Nonetheless, the fact that the Body Project has not produced greater reductions in all core outcomes relative to all of these alternative interventions implies that non-specific factors, such as expectancies and demand characteristics, may contribute to some of the reductions in outcomes observed among Body Project participants. Further, the fact that the group-based Body Project produced larger posttest reductions in risk factor outcomes than the Internet eBody Project, which has similar content implies that the group-based nature of the Body Project contributes to intervention effects, potentially due to the social support participants provide to each other (Shaw, Rohde, & Stice, 2016) or because it changes perceptions regarding peer norms (i.e., whether most undergraduates reject the thin ideal as an appearance goal; Cruwys, Haslam, Fox, & McMahon, 2015). However, the Body Project produced greater reductions in outcomes relative to other group-based interventions, including the Healthy Weight prevention program, suggesting that the specific content significantly contributes to the effects, rather than being solely driven by non-specific factors that are present in most group-based interventions. It is important to note that Healthy Weight has emerged as an effective eating disorder prevention program and is the only program to have significantly reduced eating disorder onset over long-term follow-up in multiple trials (Stice et al., 2008, 2013).
Third, it was noteworthy that the average effects were similar for clinician-led and peer-led Body Project groups versus educational video participants (d = .43 vs. .44) and eBody Project participants (d = .19 vs. .18), and that clinician-led groups did not produce significantly larger intervention effects than peer-led groups for any of the continuous outcomes; the average d effect size for the comparisons between the two group conditions was only .04. It was also noteworthy that the fidelity and competence ratings were only slightly lower for peer-led versus clinician-led groups, and that acceptability of the two types of groups was also similar, as indexed by attendance and homework completion. These findings are unique because no fully powered trial has compared clinician-led to peer-led eating disorder prevention interventions.
Fourth, the finding that eBody Project participants showed significantly larger reductions in all of the risk factors and eating disorder symptoms than educational video controls was also novel, as to our knowledge, no other Internet-based eating disorder prevention program has significantly outperformed an alternative intervention. Indeed, to our knowledge other Internet-based eating disorder prevention programs have not significantly reduced eating disorder symptom composite measures relative to any type of control condition. However, the eBody Project effects showed limited persistence over follow-up and the average effect size across all continuous outcomes was only a d = .25, which is a small effect. The smaller effects for the eBody Project did not appear to be due to low acceptability, because the proportion of participants who completed all eBody Project modules (57%) was higher than the proportion who completed all Body Project group sessions when delivered by clinicians (47%) or peer-leaders (45%). Interestingly, despite the fact that completion was higher for the eBody Project than for the Body Project groups, the average effect sizes were larger for the groups (M d = .43 and .44 for clinician-led and peer-led groups, respectively) implying that although participants may prefer completing the Internet-delivered intervention to attending groups on campus, the group-based interventions produced larger effects with a smaller dose. Yet the percentage of participants who did not complete any of the eBody Project modules (19%) was higher than the percentage of participants who did not attend any group sessions (14% for both clinician- and peer-led groups), implying that acceptability of Internet-based interventions may be lower than group-based interventions. It is also noteworthy that the eBody Project produced larger intervention effects for a broader range of outcomes than the Internet-delivered version of the Body Project implemented with a synchronous moderator who coordinated on-line discussions among members assigned to a virtual group (Serdar et al., 2014). This pattern of findings implies that implementing the Body Project in virtual groups that are moderated synchronously may not result in larger effects.
Fifth, it was noteworthy that although all three variants of the Body Project intervention produced superior reductions in the primary continuous outcome of eating disorder symptoms compared to educational video at both posttest and 6-month follow-up, none of the pairwise comparisons between different methods of delivering the Body Project content produced significantly different amounts of symptom reduction. This pattern contrasts with the risk factor outcomes, where the group-based delivery methods produced significantly greater improvements in thin-ideal internalization and body dissatisfaction that persisted through 6-month follow-up. Though the pattern of results was consistent with the expectation that group-based interventions would be more effective than a stand-alone Internet program, differences in the primary continuous outcome measure failed to be significant in this large, well-powered trial.
Sixth, peer-led Body Project group participants showed a significant 74% reduction in onset of threshold or subthreshold eating disorder over 6-month follow-up compared to eBody Project participants, which was our second primary outcome. Only 2 other eating disorder prevention programs have produced this critical intervention effect (Martinsen et al., 2014; Stice et al., 2008, Stice, Rohde, Shaw et al., 2013), this effect has never been documented for peer-led Body Project groups, and this is the first time that an eating disorder prevention program produced significantly lower eating disorder onset than a credible alternative intervention. Although an NNT of 15 might be considered high for an expensive and potentially iatrogenic treatment, the Body Project is a 4-hr prevention program delivered by unpaid college students. Plus, it does not seem wasteful or onerous for 15 participants to have to complete the Body Project to prevent onset of one eating disorder, as most participants will exhibit improved body satisfaction, negative affect, and eating disorder symptoms. It is also important to note that this is an indicated prevention program that targets youth at high-risk for eating disorders, so reductions in these outcomes is equally important from a prevention standpoint. Nonetheless, it will be vital to determine whether this effect persists over longer follow-up. Further, we acknowledge that the 64% reduction in eating disorder onset observed in the peer-led Body Project condition versus educational video condition did not reach statistical significance (p value = .115). We also acknowledge that the 39% reduction in eating disorder onset for the clinician-led groups versus eBody Project participants and the 16% reduction in eating disorder onset observed in clinician-led groups versus educational video controls did not reach significance. Although these latter three effects were in the hypothesized direction, and two appear to be clinically meaningful, they were not significant, in part because of the low incidence of eating disorder onset in the sample through 7-month follow-up. It is possible that once the 3-year follow-up data are collected for this trial that some of these other contrasts will reach significance for our primary dichotomous outcome. It was also noteworthy that the only full threshold cases of eating disorders (bulimia nervosa and binge eating disorder) emerged in the educational video condition, though this could be due to chance.
When conducting randomized trials it is important to balance risk for false positive findings and risk for false negative findings. As we had 4 continuous outcomes and 1 dichotomous outcome, it is possible that some effects emerged by chance because we used a p-value of .05. However, 100% of the effects for clinician-led Body Project groups versus the educational video control condition and 88% of the effects for peer-led Body Project groups versus educational video control condition were significant, which is considerably higher than the 5% that would be anticipated based on chance alone, suggesting it is unlikely that we are reporting false positive findings. Moreover, most of these significant results represented medium magnitude effects. Putting the present results in a broader context, 47 of the 50 tests of the intervention effects for the core outcomes (94%) from the 10 past trials by our team that evaluated the Body Project were significant, which also suggests that these effects are not chance findings (only 2.5 would be expected based on chance; Linville et al., 2015; McMillian et al., 2011; Stice et al., 2000, 2003, 2006, 2009, 2012a, 2013a, 2013b). Further, 34 of the 47 tests for the core intervention effects (72%) from another 11 trials conducted by independent teams that used similar control or comparison conditions were significant, providing additional evidence that these effects are not chance findings (only 2.4 would have been expected based on chance; Becker et al, 2005, 2012; Ciao, Latner, Brown, Ebneter, & Becker, 2015; Green et al., 2005; Halliwell & Diedrichs, 2014; Halliwell et al., 2015; Kilpela et al., 2016; Matusek, Wendt, & Wiseman, 2004; Mitchell et al., 2007; Seidel et al., 2009; Serdar et al., 2014). In sum, the fact that the effects for the core outcomes for the Body Project that we report have replicated in 88% of the tests in 22 controlled trials conducted by independent teams suggest that the effects are reproducible.
Limitations
First, the follow-up period for this report on the acute effects from this trial was only 7-months post-baseline. It will be critical to examine the persistence of effects, and more importantly the true preventive impact, of the various delivery modalities of this eating disorder prevention program. Second, despite use of state-of-the-art procedures for handling missing data, the moderate attrition might have biased the results. The fact that participants with initial higher eating disorder symptoms were more likely to drop out is concerning because they are presumably most in need of an eating disorder prevention program. Third, the outcomes were based on self-report data, raising the possibility that expectances and demand characteristics inherent to randomized trials contributed to the observed effects. Future trials should thus incorporate biological and objective outcomes (e.g., brain imaging). In this context, it should be noted that participants who completed the Body Project showed significantly lower onset of objectively measured obesity over 1-year follow-up compared to participants in an assessment-only control condition and an alternative intervention in a previous trial (Stice et al., 2006). Fourth, although the Body Project has produced significantly larger reductions in outcomes than other group-based credible alternative interventions (e.g., Stice et al., 2006), the use of an educational video control condition in the present trial does not permit us to isolate the effects of the content of the Body Project from non-specific effects. Fifth, the low incidence of eating disorder onset during the 7-month follow-up limited sensitivity to detecting reductions in future onset of eating disorders.
Conclusions and Directions for Future Research
Collectively, findings suggest that over short-term follow-up both clinician-led and peer-led Body Project groups produced replicable and clinically meaningful reductions in eating disorder risk factors and symptoms, and the latter significantly reduced future eating disorder onset relative to a credible alternative intervention. Further, results suggest that Body Project delivery can be task shifted to peer leaders without a reduction in effects for the continuous outcomes (M d = .43 versus .44). This is important knowledge because whereas masters- or doctoral-level clinicians are relatively expensive interventionists, the peer-leaders delivered the Body Project groups for free as part of their college coursework. Further, peer leaders are abundant because 80% of colleges have peer educator programs (Hong, Robertson, Catanzarite, & McCall, 2011). Thus, implementing the group-based Body Project with undergraduate peer educators appears to represent a cost-effective delivery modality. In contrast, results revealed shifting from clinician-delivered groups to the Internet-delivered version of the Body Project attenuated effect sizes (M d = .43 versus .25). This finding, taken in conjunction with the evidence that participants who completed both clinician-led and peer-led Body Project groups showed greater reductions on several of the continuous risk factor outcomes than eBody Project participants, as well as the higher eating disorder onset observed among eBody Project versus peer-led Body Project group participants, imply that it would be better to implement the group-version of this prevention program than the Internet-version. However, in instances where this is unfeasible, because of a lack of infrastructure or in remote regions, it might be useful to encourage completion of the eBody Project, which did not significantly differ from either group-delivered version of the Body Project in terms of symptom reduction and is available for anyone to complete for free.
Future research should continue to examine cost-effective methods of broadly delivering evidence-based eating disorder prevention programs to groups at risk for these pernicious mental health problems. It would also be useful to test whether the reductions in the continuous risk factor outcomes, especially thin-ideal internalization and body dissatisfaction partially mediate the effects of this prevention program on reductions in eating disorder onset. Moreover, future research should examine moderators that determine whether particular individuals show larger intervention effects from the various delivery modalities for this prevention program, as such a personalized prevention approach may improve the overall yield of prevention efforts. Further, it will be important to conduct cost effectiveness analyses of the various methods of delivering evidence-based eating disorder prevention programs. Finally, it will be critical to examine factors that influence adoption and implementation of evidence-based eating disorder prevention programs, as well as factors that predict fidelity, competence, and sustainability of intervention delivery.
Public Health Significance Statement.
Clinician- and peer-led Body Project groups and the Internet-based eBody Project eating disorder prevention programs produced greater reductions in eating disorder risk factors and symptoms than an educational video comparison condition over short-term follow-up.
Both group-based versions of the Body Project eating disorder prevention program produced larger risk factor reductions than the Internet-based eBody Project.
Delivery of the Body Project can be task shifted to delivery by more abundant and cost-effective undergraduate peer educators without loss of efficacy over short-term follow-up.
Acknowledgments
A grant MH097720 from the National Institute of Mental Health supported this research. We thank David Drum for assistance with supervision, Amber Borcyk, Victoria Perko, Julie Pope, Katharine Menke, and Caitlin Klossner for being exemplary project coordinators, and the students from the University of Oregon, Oregon State University, and The University of Texas at Austin who participated in this study. ClinicalTrials.gov Identifier: NCT01949649.
References
- Allen KL, Byrne SM, Oddy WH, Crosby RD. DSM-IV-TR and DSM-5 eating disorders in adolescents: prevalence, stability, and psychosocial correlates in a population-based sample of male and female adolescents. Journal of Abnormal Psychology. 2013;122:720–732. doi: 10.1037/a0034004. [DOI] [PubMed] [Google Scholar]
- Altman DG, Andersen P. Calculating the number needed to treat for trials where the outcome is time to an event. BMJ. 1999;(319):1492–1495. doi: 10.1136/bmj.319.7223.1492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arcelus J, Mitchell A, Wales J, Nielsen S. Mortality rates in patients with anorexia nervosa and other eating disorders: A meta-analysis of 36 studies. Archives of General Psychiatry. 2011;68:724–731. doi: 10.1001/archgenpsychiatry.2011.74. [DOI] [PubMed] [Google Scholar]
- Atkinson M, Wade T. Does mindfulness have potential in eating disorder prevention? A preliminary controlled trial with young adult women. Early Intervention in Psychiatry. 2014 doi: 10.1111/eip.12160. [DOI] [PubMed] [Google Scholar]
- Baldwin SA, Bauer DJ, Stice E, Rohde P. Evaluating models for partially clustered designs. Psychological Methods. 2011;16:149–165. doi: 10.1037/a0023464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker C, McDaniel L, Bull S, Powell M, McIntyre K. Can we reduce eating disorder risk factors in female college athletes? A randomized exploratory investigation of two peer-led interventions. Body Image. 2012;9:31–42. doi: 10.1016/j.bodyim.2011.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker C, Smith L, Ciao A. Reducing eating disorder risk factors in sorority members: A randomized trial. Behavior Therapy. 2005;36:245–254. doi: 10.1016/S0005-7894(05)80073-5. [DOI] [Google Scholar]
- Berscheid E, Walster E, Bohrnstedt G. The happy American body: A survey report. Psychology Today. 1973;7:119–131. [Google Scholar]
- Botvin G, Baker E, Renick N, Filazzola A, Botvin E. A cognitive-behavioral approach to substance abuse prevention. Addictive Behaviors. 1984;9:137–147. doi: 10.1016/0306-4603(84)90051-0. [DOI] [PubMed] [Google Scholar]
- Ciao A, Latner J, Brown K, Ebneter D, Becker C. Effectiveness of a peer-delivered dissonance-based program in reducing eating disorder risk factors in high school girls. International Journal of Eating Disorders. 2015;48:779–784. doi: 10.1002/eat.22418. [DOI] [PubMed] [Google Scholar]
- Cruwys T, Haslam A, Fox N, McMahon H. “That’s not what we do”: Evidence that normative change is a mechanism of action in group interventions. Behaviour Research and Therapy. 2015;65:11–17. doi: 10.1016/j.brat.2014.12.003. [DOI] [PubMed] [Google Scholar]
- Feingold A. Effect sizes for growth-modeling analysis for controlled clinical trials in the same metric as for classical analysis. Psychological Methods. 2009;14:43–53. doi: 10.1037/a0014699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fladung A, Gron G, Grammer K, Herrnberger B, Schilly E, Grasteit S, et al. A neural signature of anorexia nervosa in the ventral striatal reward system. American Journal of Psychiatry. 2010;167:206–212. doi: 10.1176/appi.ajp.2009.09010071. [DOI] [PubMed] [Google Scholar]
- Green M, Scott N, Diyankova I, Gasser C, Pederson E. Eating disorder prevention: An experimental comparison of high level dissonance, low level dissonance, and no-treatment control. Eating Disorders. 2005;13:157–169. doi: 10.1037/a0024351. [DOI] [PubMed] [Google Scholar]
- Halliwell E, Diedrichs P. Testing a dissonance body image intervention among young girls. Healthy Psychology. 2014;33:201–204. doi: 10.1037/a0032585. [DOI] [PubMed] [Google Scholar]
- Halliwell E, Jarman H, McNamara A, Risdon H, Jankowski G. Dissemination of evidence-based body image interventions: A pilot study into the effectiveness of using undergraduate students as interventionists in secondary schools. Body Image. 2015;14:1–4. doi: 10.1016/j.bodyim.2015.02.002. [DOI] [PubMed] [Google Scholar]
- Hong L, Robertson J, Catanzarite J, McCall L. Peer health education: Concepts and content. San Diego: University Readers; 2011. [Google Scholar]
- Killen J, Taylor C, Hayward C, Haydel K, Wilson D, Hammer L, et al. Weight concerns influence the development of eating disorders: a 4-year prospective study. Journal of Consulting and Clinical Psychology. 1996;64:936–940. doi: 10.1037//0022-006x.64.5.936. [DOI] [PubMed] [Google Scholar]
- Kilpela L, Blomquist K, Verzijl C, Wilfred S, Beyl R, Becker C. The Body Project 4 All: A pilot randomized controlled trial of a mixed-gender dissonance-based body image program. International Journal of Eating Disorders. 2016 doi: 10.1002/eat.22562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leupaker R, Johnson C, Murray D, Pechacek T. Prevention of cigarette smoking: Three year follow-up of an education program for youth. American Journal of Public Health. 1983;71:1320–1324. [Google Scholar]
- Linville D, Cobb E, Lenee-Bluhm T, Lopez-Zeron G, Gau J, Stice E. The effectiveness of an eating disorder prevention intervention in primary care medical settings. Behaviour Research and Therapy. 2015;75:32–39. doi: 10.1016/j.brat.2015.10.004. [DOI] [PubMed] [Google Scholar]
- Martinsen M, Bahr R, Borresen R, Holme I, Pensgaard A, Sundgot-Borden J. Preventing eating disorders among young elite athletes: A randomized controlled trial. Medicine and Science in Sports & Exercise. 2014;46:435–447. doi: 10.1249/MSS.0b013e3182a702fc. [DOI] [PubMed] [Google Scholar]
- Matusek JA, Wendt SJ, Wiseman CV. Dissonance thin-ideal and didactic healthy behavior eating disorder prevention programs: Results from a controlled trial. International Journal of Eating Disorders. 2004;36:376–388. doi: 10.1002/eat.20059. [DOI] [PubMed] [Google Scholar]
- McMillan W, Stice E, Rohde P. High- and low-level dissonance-based eating disorder prevention programs with young women with body image concerns: An experimental trial. Journal of Consulting and Clinical Psychology. 2011;79:129–134. doi: 10.1037/a0022143. [DOI] [PubMed] [Google Scholar]
- Mellanby A, Rees J, Tripp J. Peer-led and adult-led school health education: A critical review of available comparative research. Health Education Research. 2000;15:533–545. doi: 10.1093/her/15.5.533. [DOI] [PubMed] [Google Scholar]
- Mitchell K, Mazzeo S, Rausch S, Cooke K. Innovative interventions for disordered eating: Evaluating dissonance-based and yoga interventions. International Journal of Eating Disorders. 2007;40:120–128. doi: 10.1002/eat.20282. [DOI] [PubMed] [Google Scholar]
- Raghunathan T, Solenberger P, Van Hoewyk J. IVEware: imputation and variance estimation software. University of Michigan; Ann Arbor, MI: Institute for Social Research; 2016. [Google Scholar]
- Rhee H, Belyea M, Hunt J, Brasch J. Effects of a peer-led asthma self-management program for adolescents. Archives of Pediatrics and Adolescent Medicine. 2011;165:513–519. doi: 10.1001/archpediatrics.2011.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York: John Wiley & Sons, Inc; 1987. [Google Scholar]
- SAS/STAT. User’s Guide 9.2. Cary, NC: SAS Institute Inc; 2011. [Google Scholar]
- Seidel A, Presnell K, Rosenfield D. Mediators in the dissonance eating disorder prevention program. Behaviour Research and Therapy. 2009;47:645–653. doi: 10.1016/j.brat.2009.04.007. [DOI] [PubMed] [Google Scholar]
- Serdar K, Kelly N, Palmberg A, Lydecker J, Thornton L, Tully C, Mazzeo A. Comparing online and face-to-face dissonance-based eating disorder prevention. Eating Disorders. 2014;22:244–260. doi: 10.1080/10640266.2013.874824. [DOI] [PubMed] [Google Scholar]
- Shaw H, Rohde P, Stice E. Participant feedback from peer-led, clinician-led, and Internet-delivered eating disorder prevention interventions. International Journal of Eating Disorders. doi: 10.1002/eat.22605. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stata Statistical Software. College Station, TX: StataCorp LP; 2007. [Google Scholar]
- Stice E, Butryn M, Rohde P, Shaw H, Marti N. An effectiveness trial of a new enhanced dissonance eating disorder prevention program among female college students. Behaviour Research and Therapy. 2013;51:862–871. doi: 10.1016/j.brat.2013.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Durant S, Rohde P, Shaw H. Effects of a prototype Internet dissonance-based eating disorder prevention program at 1- and 2-year follow-up. Health Psychology. 2014;33:1558–1567. doi: 10.1037/hea0000090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Fisher M, Martinez E. Eating disorder diagnostic scale: Additional evidence of reliability and validity. Psychological Assessment. 2004;16:60–71. doi: 10.1037/1040-3590.16.1.60. [DOI] [PubMed] [Google Scholar]
- Stice E, Gau J, Rohde P, Shaw H. Risk factors that predict future onset of each DSM-5 eating disorder: Predictive specificity in high-risk adolescent females. Journal of Abnormal Psychology. 2016 doi: 10.1037/abn0000219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Marti C, Rohde P. Prevalence, incidence, impairment, and course of the proposed DSM-5 eating disorder diagnoses in an 8-year prospective community study of young women. Journal of Abnormal Psychology. 2013;122:445–457. doi: 10.1037/a0030679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Marti C, Spoor S, Presnell K, Shaw H. Dissonance and healthy weight eating disorder prevention programs: Long-term effects from a randomized efficacy trial. Journal of Consulting and Clinical Psychology. 2008;76:329–340. doi: 10.1037/0022-006X.76.2.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Mazotti L, Weibel D, Agras WS. Dissonance prevention program decreases thin-ideal internalization, body dissatisfaction, dieting, negative affect, and bulimic symptoms: A preliminary experiment. International Journal of Eating Disorders. 2000;27:206–217. doi: 10.1002/(sici)1098-108x(200003)27:2<206::aid-eat9>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- Stice E, Presnell K, Gau J, Shaw H. Testing mediators of intervention effects in randomized controlled trials: An evaluation of two eating disorder prevention programs. Journal of Consulting and Clinical Psychology. 2007;75:20–32. doi: 10.1037/0022-006X.75.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Rohde P, Butryn ML, Shaw H, Marti CN. Effectiveness trial of a selective dissonance-based eating disorder prevention program with female college students: Effects at 2- and 3-year follow-up. Behaviour Research and Therapy. 2015;71:20–26. doi: 10.1016/j.brat.2015.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Rohde P, Durant S, Shaw H. A preliminary trial of a prototype Internet dissonance-based eating disorder prevention program for young women with body image concerns. Journal of Consulting and Clinical Psychology. 2012;80:907–916. doi: 10.1037/a0028016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Rohde P, Durant S, Shaw H, Wade E. Effectiveness of peer-led dissonance eating disorder prevention groups: Results from two randomized trials. Behaviour Research and Therapy. 2013;51:197–206. doi: 10.1016/j.brat.2013.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Rohde P, Gau J, Shaw H. An effectiveness trial of a dissonance-based eating disorder prevention program for high-risk adolescent girls. Journal of Consulting and Clinical Psychology. 2009;77:825–834. doi: 10.1037/a0016132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Rohde P, Shaw H, Gau J. An effectiveness trial of a selected dissonance-based eating disorder prevention program for female high school students: Long-term effects. Journal of Consulting and Clinical Psychology. 2011;79:500–508. doi: 10.1037/a0024351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Rohde P, Shaw H, Marti N. Efficacy trial of a selective prevention program targeting both eating disorders and obesity among female college students: 1- and 2-year follow-up effects. Journal of Consulting and Clinical Psychology. 2013;81:183–189. doi: 10.1037/a0031235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Shaw H, Burton E, Wade E. Dissonance and healthy weight eating disorder prevention programs: A randomized efficacy trial. Journal of Consulting and Clinical Psychology. 2006;74:263–275. doi: 10.1037/0022-006X.74.2.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Shaw H, Marti CN. A meta-analytic review of eating disorder prevention programs: Encouraging Findings. Annual Review of Clinical Psychology. 2007;3:233–257. doi: 10.1146/annurev.clinpsy.3.022806.091447. [DOI] [PubMed] [Google Scholar]
- Stice E, Yokum S, Waters A. Dissonance-based eating disorder prevention program reduces reward region response to thin models: How actions shape valuation. PLoS One. 2015;10:e0144530. doi: 10.1371/journal.pone.0144530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swanson S, Crow S, Le Grange D, Swendsen J, Merikangas K. Prevalence and correlates of eating disorders in adolescents: Results from the national comorbidity survey replication adolescent supplement. Archives of General Psychiatry. 2011;68:714–723. doi: 10.1001/archgenpsychiatry.2011.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Education. Digest of Educational Statistics, 2007. National Center for Education Statistics; 2008. [Google Scholar]
- Vocks S, Busch M, Gronemeyer D, Schulte D, Herpertz S, Suchan B. Neural correlates of viewing photographs of one’s own body and another woman’s body in anorexia nervosa and bulimia nervosa: An fMRI study. Journal of Psychiatry and Neuroscience. 2010;35:163–176. doi: 10.1503/jpn.090048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Clark LA. Affects separable and inseparable: On the hierarchical arrangement of the negative affects. Journal of Personality Social Psychology. 1992;62:489–505. [Google Scholar]
- WGBH Video. Twin Cities Public Television. Saint Paul, MN: WGBH Educational Foundation; 2000. Dying to be thin. [Google Scholar]