Abstract
Stigma related to sexual violence (SV) is associated with many negative physical and social outcomes. We sought to create a contextually relevant SV stigma measure for women in the Democratic Republic of Congo (DRC) and assess the scale's psychometrics and validity. Using baseline screening data from two randomized controlled trials of services for female SV survivors in eastern DRC (n=1,184), we conducted exploratory and confirmatory factor analyses to test the measurement model. Cronbach's alphas and Kuder-Richardson 20 statistics were used to evaluate internal consistency. Logistic and linear regressions of the stigma measures with related constructs were used to assess construct validity. Two distinct but related scales were developed based on factor analyses: a four-item scale of discrimination related stigma (i.e. enacted stigma) and an eight-item scale of combined perceived and internalized stigma (i.e. felt stigma). Both scales showed good internal consistency (KR-20=0.68; alpha=0.86). A higher felt stigma score was associated with significant increases in combined depression and anxiety and trauma symptoms, as well as functional impairment (p<0.001). Having a child as a result of SV was associated with both significantly higher enacted and felt stigma (p<0.001). Neither SV stigma scale was associated with medical care seeking. To address harmful ramifications of stigma among SV survivors, locally relevant quantitative measures are necessary to understand the nature and severity of stigma they experience. Our process of scale creation and evaluation can serve as an example for developing locally relevant SV-related stigma measures.
Keywords: stigma, sexual violence, psychometrics, scale development, Democratic Republic of Congo
Background
Sexual violence (SV), defined by the World Health Organization (WHO) as any actual or attempted coerced sexual act, is common globally (World Health Organization, 2013a). SV can be particularly pervasive in areas affected by conflict (Amowitz et al., 2002; Desai & Perry, 2004; Swiss et al., 1998) due to its use as a tool of war and the social and legal disruption caused by systemic violence (M. Marsh, Purdin, & Navani, 2006). In conflict-affected areas of eastern Democratic Republic of Congo (DRC), up to 40% of women report an experience of SV (Johnson et al., 2010). Many reported cases of SV are committed by combatants (Bartels et al., 2012), though civilian-perpetrated SV and intimate partner violence are also common and likely underreported (Bartels et al., 2011; Peterman, Palermo, & Bredenkamp, 2011). Multiple adverse health outcomes are associated with SV including pain, gynecological injuries, sexually transmitted infections (STIs), unwanted pregnancies, and mental distress (Decker et al., 2014; Dossa, Zunzunequi, Hatem, & Fraser, 2014; Ellsberg, Jansen, Heise, Watts, & Garcia-Moreno, 2008; Johnson et al., 2010; World Health Organization, 2013b).
Stigma, a frequent consequence of SV, is a complex construct and is often also directly associated with poor health and social outcomes. One type of stigma that is relevant to SV survivors is receiving negative reactions when disclosing SV experiences, which has been shown to predict poorer mental and physical health in survivors (Campbell, Ahrens, Sefl, Wasco, & Barnes, 2001; Ullman, Townsend, Filipas, & Starzynski, 2007). In some contexts, blame from community members can damage survivors' relationships and marriageability (Glass, Ramazani, Tosha, Mpanano, & Cinyabuguma, 2011; Kelly et al., 2012). Focus groups with SV survivors in DRC have revealed that survivors can face restricted access to income generation and farming activities (Kelly et al., 2012). Losing the ability to support one's family can contribute to further devaluing of survivors in a vicious cycle of marginalization and loss (Glass et al., 2011). This isolation can be extreme; a study in DRC found that 12.5% of SV survivors seeking medical services reported being forced from their home (Steiner et al., 2009).
Defining Stigma
Many theories seek to explain the generation and maintenance of stigma for health and social conditions. Erving Goffman (1963) described stigma as socially generated and possibly self-inflicted by a person who may feel maltreatment is deserved. Drawing on Goffman's ideas, Link & Phelan (2006) explained stigma as a process that unfolds in the presence of a power differential. In this process, a difference is identified, labeled, stereotyped, and used to socially distance, ultimately resulting in discrimination. Thornicroft, Rose, Kassam, & Sartorius (2007) described the stigma of mental disorders as due to a lack of knowledge and negative ideas regarding a condition as well as behaviors such as rejection. All these definitions indicate that stigma involves a dynamic interplay between thoughts, actions, and social identity perpetuated by the broader community, but internalized and lived by the target of stigma himself or herself.
Measuring Stigma
Drawing on multiple definitions, stigma has been explored widely in the fields of HIV/AIDS and mental health through the use of a variety of measures. Internalized, perceived, and enacted stigma are three common constructs underlying measures of stigma (Brohan, Slade, Clement, & Thornicroft, 2010). Internalized stigma scales assess the extent to which a group's negative perceptions of a person result in that individual feeling shame or changing his or her behaviors in a way that exacerbates feelings of being different; a scale of internalized stigma might include items on self-blame or guilt (see Simbayi et al., 2007). Perceived stigma measures ask respondents to report, from their own perspective, how others view or behave towards them (see Liu et al., 2011). Enacted stigma measures assess actual acts of discrimination (see Lasalvia et al., 2012; Thornicroft, Brohan, Rose, Sartorius, & Leese, 2009), for instance when someone refuses to interact with or provide services to someone with a stigmatized condition (Link & Phelan, 2006). Perceived stigma measures generally capture subjective thoughts and feelings of the SV survivor while enacted stigma measures involve reports as to whether or not a particular discriminatory act occurred.
The extent to which these three constructs are important in understanding SV-related stigma in low-income and conflict-affected populations has received limited attention. SV-related stigma has been assessed based on community attitudes towards rape survivors in diverse settings (Babalola, 2014; Lee, Kim, & Lim, 2010; Tavrow, Withers, Obbuyi, Omollo, & Wu, 2013; Ward, 1988). While community attitudes represent one aspect of the complex process of stigmatization, they exclude the actual and perceived experiences of the survivors themselves. Measures that assess stigma as experienced by SV survivors have been developed in high-resource settings (Campbell & Raja, 2005; Coffey, Leitenberg, Henning, Turner, & Bennett, 1996; Gibson & Leitenberg, 2001; Ullman, 2000; Ullman et al., 2007) often using samples of university-based women (Gibson & Leitenberg, 2001; Ullman, 2000; Ullman et al., 2007). These measures may not be appropriate in settings where there are different cultural norms related to gender, sexuality, and social roles. The appropriateness of using measures from such a different cultural context has been challenged in discussions on the stigmatization of other conditions (Keusch, Wilentz, & Kleinman, 2006), leading to the suggestion that SV-related stigma measures should also be developed based on local perspectives and context.
When SV-related stigma research has been conducted among SV survivors in DRC, stigma has often been assessed by including one or two questions on survivors' perceptions of stigma (Johnson et al., 2010) or by asking about the survivors' experiences of rejection by their family (Steiner et al., 2009). Given the dynamic socio-cultural processes related to stigma (Nyblade, 2006), such brief measures likely leave out important aspects of stigma. An exception is a recent adaptation of the Everyday Discrimination Scale (Williams, Yu, Jackson, & Anderson, 1997) which included both enacted and perceived stigma items for adolescent SV survivors in DRC (Verelst, De Schryver, De Haene, Broekaert, & Derluyn, 2014). Without this kind of more comprehensive, valid, and reliable measures of SV-related stigma, it will be difficult to determine how stigma is related to adult survivors' well-being, understand how stigma is changing in a community, and assess the impact of interventions on reducing stigma. Our goal is to present a process for developing locally appropriate SV-related measures of stigma that we applied in the DRC with adult women and that can be replicated in other contexts.
Study Aims
In this study from the DRC, we had two aims:
To create contextually relevant scales of stigma using data collected as part of two randomized controlled trials of services for SV survivors.
To assess the validity and internal consistency of the created scales.
Methods
Design
This study used quantitative data collected as part of baseline eligibility screenings for two trials: one of Cognitive Processing Therapy (CPT) (Bass et al., 2013) and one of a Village Savings and Loan Associations (VSLA) intervention (Bass et al., 2014), both conducted with female survivors of SV with moderate to severe symptoms of mental distress living in South Kivu province in eastern DRC. The Johns Hopkins Bloomberg School of Public Health and Kinshasa School of Public Health Institutional Review Boards provided ethical approval for these trials.
Participants
For the CPT trial, 495 women were screened for eligibility in 15 study villages in December 2010. One woman was dropped from all study analyses due to a paperwork error that prevented her study ID from being verified, leaving a total baseline sample of 494 women. For the VSLA trial, 695 women were recruited from nine villages through word of mouth of community-based organizations and screened in February 2011. A full description of the recruitment and screening process can be found elsewhere (Bass et al., 2013). Across the two trials, 1,189 women were screened for eligibility. We excluded five women who reported an age under 18, and 440 women who reported witnessing, but not personally experiencing, SV for a total of 744 women included in the current study.
Measures
Trained local interviewers administered the study questionnaires in person to women in both trials. Relevant for this study, the study questionnaire included sections for symptoms of distress, functioning, and traumatic experiences as described below. All measures were adapted to the local context by using data from a previously conducted qualitative study and then translated into the five study languages (for a detailed description of the process refer to Applied Mental Health Research Group, 2013a, 2013b; Bass, Ryder, Lammers, Mukaba, & Bolton, 2008). The qualitative study consisted of free list interviews with women living in three communities with high rates of sexual violence in South Kivu and key informant interviews with men and women identified through snowball sampling from the same communities (report available upon request). These interviews were designed to understand the type and nature of problems experienced by sexual violence survivors as well as appropriate terminology and locally relevant expressions of distress.
Symptoms of distress
The Hopkins Symptoms Checklist (HSCL-25) (Hesbacher, Rickels, Morris, Newman, & Rosenfeld, 1980; Winokur, Winokur, Rickels, & Cox, 1984) was adapted to measure combined depression and anxiety and the Harvard Trauma Questionnaire (HTQ) (Mollica et al., 1992) for traumatic stress based on results of the qualitative study. For both measures, Likert response categories were used to assess how often a woman experienced each symptom in the previous four weeks, ranging from 0 (not at all) to 3 (a lot). These scales showed a high degree of internal consistency (Cronbach's alpha: HSCL 0.89, HTQ 0.88) (Bass et al., 2013). Sixteen additional symptoms generated from the brief qualitative study that were not represented in these standard measures were selected by staff from JHU and its in-country partner, International Rescue Committee (IRC), to be added to the questionnaire to create a locally relevant measure of distress, including such concepts as shame, thinking too much, rejection, and avoiding others.
Functioning
A 20-item assessment of functional impairment was developed using data from a preliminary qualitative study to measure a woman's ability to engage in tasks of daily living. Respondents rated each task using a Likert scale of 0 (no difficulty) to 4 (often unable to complete the task). Items included tasks related to caring for the family (e.g. cooking, looking after children), the community (e.g. socializing with others), and self (e.g. learning new skills) (see Bass et al. 2013 for a full description of this measure).
Traumatic event exposure
A measure of exposure to traumatic events was created to capture whether a woman witnessed murder and experienced or witnessed five other traumas: SV, violent attack, abduction, abandonment or being thrown out, and looting or burning of a home or other property. Sexual violence survivor for the purpose of this study was defined as any woman who self-reported yes to having personally experienced “sexual violence” which was translated locally as “rape.” Eleven yes or no questions were included about the characteristics and ramifications of the SV events: two questions were specific to women who indicated having a husband (“rejected by your husband as a result of SV” and “forced to live away from your husband”) and one question to women who indicated having children (“forced to live away from your children”). Two questions were also included in which survivors were asked to indicate whether they agreed, disagreed or were unsure about the following two statements: “the violence happened because of the way I acted,” and, “somebody else wouldn't have gotten in this situation.” For the current analysis, these last two questions were dichotomized to agree or disagree; a response of unsure was changed to missing.
Analysis
Measurement model exploration and testing
Using exploratory factory analysis (EFA), we first assessed the underlying factor structure of the 16 symptoms of distress that were identified during the qualitative study among all SV survivors (n=744). The rationale for first focusing on these 16 symptoms of distress (rather than all 55 items on the distress measure including the HSCL-25 and HTQ items) was that these symptoms were identified by members of the community as specifically relevant to SV survivors and thus we considered that they were a first glimpse at how members of the community perceived SV survivors. Six items that loaded strongly onto a factor that resembled a combination of the two types of stigma (internalized and perceived) were retained (results not presented). Although “thinking about hurting yourself”loaded onto the same factor, it was not included as it was considered to be a consequence of stigma based on conversations with IRC field staff.
To improve content validity, items from the HSCL-25, HTQ, and the traumatic event exposure scale were reviewed to identify those that appeared related to one of the constructs of stigma described earlier (internalized, perceived, or enacted). Nine items were identified that appeared related to the three stigma constructs: two from the HSCL-25 depression subscale, one from the HTQ measure, and six traumatic exposure items. We did not select items that represented generalized distress or traumas without a connection to one of the definitions of stigma (e.g. we included feeling guilty because of the inclusion of guilt in definitions of internalized stigma but did not include nightmares that can result from a traumatic experience).
A second EFA was performed on this combined set of 15 items. Both a Bartlett's Test of Sphericity p-value of <0.001 (Bartlett, 1950) and the Kaiser-Meyer Olkin Measure of Sampling Adequacy (Kaiser, 1970; Kaiser & Rice, 1974) value of 0.868 indicated that the data were suitable for factor analysis. The polychoric correlation matrix (available upon request) was first examined and then used in the EFA due to categorical item responses (Flora, Finkel, & Foshee, 2003). The decision on the number of factors extracted was based on principal components analysis results including percentage of variance explained and the number of eigenvalues over one. Iterated principal factor estimation was used and a promax rotation was performed. Items were retained based on high factor loadings (>0.4) and low uniqueness. The EFA was implemented using Stata 12 IC (StataCorp, 2011). As Stata uses complete case analysis, this EFA that included items with missing values was implemented among SV survivors with no missing data (n=418).
Confirmatory factor analyses (CFA) with a weighted least squares estimator and categorical indicators were then done among all survivors of SV (n=744) to test the hypothesized factor structure of the items retained based on the EFA results. We compared the fit statistics of a CFA with a three-factor solution (consistent with the results of the second EFA) and a two-factor solution. The CFAs were implemented using Mplus Version 7 (Muthen & Muthen, 2011) using full information maximum likelihood estimation with an expectation-maximization algorithm. Model coefficients were standardized using the variance of the latent variables (STD coefficients in Mplus).
Assessing internal consistency and external construct validity
Based on the final measurement model tested in the CFA, two scales were developed. A combined perceived and internalized stigma (defined as felt stigma) scale was created using eight of the distress symptoms. The felt stigma scale score was generated based on the average response to the eight symptoms, with scores ranging from 0 to 3; a score of three indicated a woman indicated experiencing all felt stigma items “a lot” in the past four weeks. There was no missing data for this scale. An enacted stigma scale was created by summing responses to four of the yes/no questions asking about rejection following the violence. The enacted stigma scale score was calculated for SV survivors who answered at least three of the four items on the scale (n=672, 90%), as answering only two items was seen as insufficient information. For the 153 (23%) of these women who answered only three items, there mean score was calculated based only on these three items. We did not multiply impute responses as the majority of missinginess was due to a question not being relevant to a participant (e.g. a woman who was not married did not indicate if she was “rejected by husband”). Enacted stigma scores ranged from a value of 0 to 4, with a score of 4 indicating a woman reported yes to having experienced all four acts of rejection.
A Kuder-Richardson 20 (KR-20) reliability coefficient and Cronbach's alpha coefficient were calculated to assess internal consistency of the enacted and felt stigma scales respectively. Logistic and linear regressions were performed to assess the associations of stigma scale scores with mental health symptom scales (combined depression/anxiety and trauma), functional impairment, and events following SV (receiving medical services for, telling someone about, and having a child due to the SV) to explore external construct validity. Due to the inclusion of two mental health symptom scale items on the felt stigma scale, combined depression and anxiety score was calculated without the item “feelings of worthlessness” and trauma score without “feeling detached or withdrawn.” Regressions were conducted using Stata 12 IC (StataCorp, 2011).
Sensitivity Analyses
To help discern the extent to which the stigma scales were distinct from broader distress experienced by women, we conducted an additional EFA with the final stigma scale items and all depression items from the HSCL-25 following the same procedures described above. In addition, we used regression to compare scores on the felt stigma scale between SV survivors (the 744 women in this study) and the 440 women assessed at baseline in the two RCTs but excluded from these analyses as they did not indicate personal SV experience. We did not compare enacted stigma scores as these items were only administered to women who indicated personally experiencing sexual violence.
Results
Study Participants
The women in this study had a mean age of 37 years and on average completed two years of formal education (Table 1). About half (47%) of the women were married and 11.5% of the married women reported not currently living with their spouse. The majority (76%) of women were living in the area (i.e. territory) where they were born. Mean household size was seven people and women reported caring for an average of four children. The participants were ethnically diverse. Approximately three quarters (72%) of the survivors reported telling someone about the sexual violence experience and 75% reported receiving medical attention. A fifth of SV survivors reported having a child due to the sexual violence they experienced.
Table 1. Characteristics of sexual violence survivors (n=744).
| Demographics | |
|
| |
| Age in years, mean (SD) | 37.12 (13.16) |
| Years of education completed, mean (SD) | 2.03 (3.03) |
| Number of people living in home | 7.13 (3.11) |
| Number of children responsible for | 4.14 (2.57) |
| Marital Status, No. (%) | |
| Single | 69 (9.27) |
| Married | 353 (47.45) |
| Divorced | 18 (2.42) |
| Separated | 134 (18.01) |
| Widowed | 170 (22.85) |
| Lives with husband if married, No. (%) | 277 (78.47) |
| Ethnicity, No. (%) | |
| Mushi | 307 (41.26) |
| Mufuliru | 155 (20.83) |
| Muhavu | 121 (16.26) |
| Mubembe | 51 (6.85) |
| Other | 110 (14.78) |
| Living in territory of origin, No. (%) | 569 (76.48) |
|
| |
| Sexual violence exposure and characteristics | |
|
| |
| Witnessed sexual violence, No. (%) | 556 (74.73) |
| Events post-sexual violence experience | |
| Received medical assistance after SV, No. (%) | 559 (75.13) |
| Had a child as a result of the SV, No. (%) | 156 (20.86) |
| Told someone about the SV, No. (%) | 536 (72.04) |
|
| |
| Mental health and functioning | |
|
| |
| Average HSCL-depression and anxiety score | 2.03 (0.56) |
| Average HTQ-trauma score | 1.97 (0.67) |
| Average functional impairment score | 1.89 (0.87) |
Measurement Model Exploration and Testing
Efa
In the set of 15 items chosen from the initial EFA of the locally relevant distress scale and review of other measures, seven items related to internalized stigma and four each related to perceived and enacted stigma (see Table 2). EFA results of these 15 items produced three eigenvalues substantially over one (range: 1.4-5.5) that together explained 60% of the variance. A three-factor EFA of these 15 items is presented in Table 2. Three items related to blame were included in the EFA. One of these items did not load strongly (>0.4) on any factor and had a high uniqueness. The other two loaded together on their own factor but one item had very high uniqueness.
Table 2. Exploratory factor analysis among survivors of sexual violence (n=418).
| Item1 | Factor 1 | Factor 2 | Factor 3 | Uniqueness |
|---|---|---|---|---|
|
| ||||
| Blaming self for things (D, I) | 0.31 | -0.08 | 0.25 | 0.82 |
| Feelings of worthlessness- no value (D, I) | 0.58 | 0.14 | -0.12 | 0.60 |
| Feeling detached or withdrawn from others (H, I) | 0.68 | 0.01 | 0.16 | 0.46 |
| Feeling badly treated by family members (Q, P) | 0.68 | 0.01 | -0.004 | 0.53 |
| Feeling badly treated by community members (Q, P) | 0.81 | -0.02 | -0.07 | 0.39 |
| Feeling shame (Q, I) | 0.63 | -0.04 | 0.12 | 0.53 |
| Feeling rejected by everybody (Q, P) | 0.88 | -0.05 | -0.03 | 0.27 |
| Feeling stigma (Q, P) | 0.75 | 0.001 | -0.01 | 0.43 |
| Wanting to avoid other people or hide (Q, I) | 0.71 | 0.01 | -0.10 | 0.52 |
| Abandoned/thrown out (T, E) | 0.01 | 0.84 | -0.02 | 0.30 |
| Rejected by family (T, E) | 0.13 | 0.63 | 0.06 | 0.50 |
| Rejected by your husband (T, E) | -0.10 | 0.98 | 0.01 | 0.10 |
| Forced to live away from your children (T, E) | 0.04 | 0.54 | 0.02 | 0.69 |
| The violence happened because of the way I acted (T, I) | -0.08 | 0.002 | 0.44 | 0.82 |
| Somebody else would not have gotten into this situation (T, I) | -0.04 | 0.03 | 0.77 | 0.42 |
|
| ||||
| Correlation factor 1 and factor 2 | 0.41 | |||
| Correlation factor 2 and factor 3 | 0.22 | |||
| Correlation factor 1 and factor 3 | 0.24 | |||
Items in bold were retained in the final CFA model.
D- from HSCL depression scale; H- from HTQ trauma scale; Q- from locally-relevant distress measure (from qualitative findings and not on any other scale); T- from traumatic exposures questionnaire; I- selected as relevant to internalized stigma; P- selected as relevant to perceived stigma; E- selected as relevant to enacted stigma
Cfa
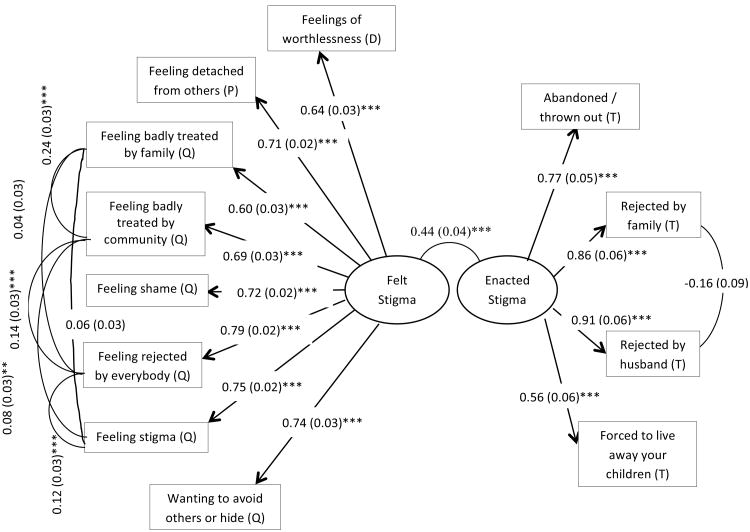
The two-factor CFA solution exhibited better model fit than the three-factor CFA solution. Further, consistent with EFA results, only two items significantly loaded onto the third factor. We therefore present the 12 item two-factor model tested with CFA (Figure 1). Due to similarity in wording, correlated errors were hypothesized to exist between four of the items: “feeling badly treated by family,” “feeling badly treated by the community,” “feeling rejected by everybody,” and “feeling stigma” and between the two items “rejected by family” and “rejected by husband.” Based on the items included in each factor, we identified the two factors as 1) a four-item enacted stigma factor and 2) an eight-item combination of perceived and internalized stigma factor (which we labeled felt stigma).
Figure 1. Confirmatory factor analysis of revised stigma scales (n=744).
*p-value <0.05, **p-value<0.01, *** p-value<0.001
D: from HSCL-25 depression subscale
P: from HTQ trauma scale
Q: from qualitative study (not on any other scale)
T: from traumatic exposures questionnaire
All eight felt stigma items were significantly (p <0.001) predicted by the latent factor with loadings ranging from 0.60 to 0.79. All four enacted items were significantly (p<0.001) predicted by the latent enacted factor, with loadings ranging from 0.56 to 0.91. Error terms for the felt stigma items were significantly correlated (p<0.05) with the exception of “feeling badly treated by family member” with “feeling stigma” (p=0.08) and with “feeling rejected by everybody” (p=0.19); the error terms of the enacted stigma items were not significantly associated (p=0.07). Correlations between error terms were overall low in magnitude (<0.3). The correlation between the two latent factors was 0.44 (p<0.05).
The Comparative Fit Index (CFI) (Bentler, 1990) and Tucker Lewis Index (TLI) (H. W. Marsh, Balla, & McDonald, 1988) were greater than 0.90 and 0.95 respectively, indicating good model fit (Table 3). The Root Mean Square Error of Approximation (RMSEA) was under 0.06 (at a value of 0.032) indicting very good fit (Hu & Bentler, 1999), and good fit was also supported by a Weighted Root Mean Square Residual (WRMR) (Muthen & Muthen, 2011) under 1.0 (at a value 0.759).
Table 3. Goodness of fit of CFA model (n=744).
| Fit Statistic | Value |
|---|---|
|
| |
| Χ2 p-value (saturated model) | 0.001 |
| CFI | 0.994 |
| TLI | 0.992 |
| RMSEA | 0.032 |
| WRMR | 0.759 |
Assessing Internal Consistency and External Construct Validity
For the results of the internal consistency analysis, the KR- 20 coefficient of reliability for the enacted stigma scale was 0.68, and the Cronbach's alpha for the felt stigma scale was 0.86. For the evaluation of external construct validity, the associations of the stigma scores with other constructs and variables are presented in Table 4. A one-unit increase in enacted stigma score was significantly associated with a small increase in combined depression and anxiety score (4.2%), trauma score (5.7%), and functional impairment (7.4%). An increase in felt stigma was associated with large increases in the combined depression and anxiety score (39.2%), trauma score (51%), and functional impairment (89.7%).
Table 4. Construct validity of stigma scales among survivors of SV1.
| Enacted Stigma (n=672) | Felt Stigma (n=744) | |||
|---|---|---|---|---|
|
| ||||
| Coefficient | Percentage Change | Coefficient | Percentage Change | |
| Linear Regression with Stigma as Predictor, β (SE) | ||||
| HSCL-Depression and Anxiety | 0.08 (0.02)*** | 4.2% | 0.47 (0.02)*** | 39.2% |
| HTQ Trauma | 0.10 (0.02)*** | 5.7% | 0.53 (0.02)*** | 51.4% |
| Functioning | 0.12 (0.02)*** | 7.4% | 0.66 (0.03)*** | 89.7% |
| Logistic Regression with Stigma as Predictor, OR (SE) | ||||
| Received Medical Services | 0.99 (0.07) | 0.95 (0.10) | ||
| Linear Regression with Stigma as Outcome β (SE) | ||||
| Told Someone about the SV | 0.31 (0.11)** | 21.2% | -0.01 (0.07) | 0.8% |
| Had a Child as a Result of SV | 0.85 (0.13)*** | 54.8% | 0.31 (0.07)*** | 18.2% |
p-value<0.05,
p-value < 0.01,
p-value<0.001
Neither felt (OR: 0.95; 95% CI: 0.77-1.17) nor enacted stigma (OR: 0.99; 95% CI: 0.87-1.12) was significantly related to having received medical services following SV, nor was felt stigma associated with telling someone about the experience of SV (β=-0.01; 95% CI: -0.14-0.11). Telling someone about the SV was associated with a significant (p=0.006) 21.2% increase in enacted stigma score. Having a child as a result of sexual violence was associated with significant (p<0.001) increases in both enacted (54.8%) and felt (18.2%) stigma scores.
Sensitivity Analyses
In an EFA of all stigma items with depression items from HSCL-25, all enacted stigma items loaded strongly onto one factor, all felt stigma items onto a second factor, and all depression items onto a third factor (results not shown). The one exception was the item “feelings of worthlessness.” This item, which was drawn from the HSCL-25 and included on the felt stigma scale, loaded onto both factors (loading=0.36 and =0.39 respectively). In a regression analysis, SV survivors on average had a stigma score that was 0.58 points higher (a 50% increase) than women who did not report experiencing SV (p-value<0.001)
Discussion
We developed two locally relevant sexual-violence related stigma scales using existing quantitative data from sexual violence survivors in eastern DRC and exploratory and confirmatory factor analyses. Of the two distinct but related scales, one measured internalized and perceived stigma while the other assessed enacted stigma. Both scales exhibited good internal consistency. Identification of our final CFA model with standard rules was not possible due to our inclusion of correlated errors. We removed these correlations to obtain an identified model and our findings were not substantially changed.
EFA analyses showed that items related to two types of stigma, internalized and perceived, loaded together onto one factor. This finding provided support to combine these types of stigma into a single construct which we labeled felt stigma, a term frequently used to refer to both internalized and perceived stigma (Deribe, Tomczyk, Mousley, Tamiru, & Davey, 2013; Hasan et al., 2012; Lekas, Siegel, & Leider, 2011). As used in studies of epilepsy, felt stigma refers to the actual or anticipated fear of being discriminated against, the perception that others view oneself negatively, and an accompanying sense of shame (Jacoby, 1994; Scambler & Hopkins, 1986). In our analyses, feelings of blame and guilt not specific to the SV event and feelings of responsibility for the SV event did not load strongly onto the felt stigma factor. This suggests that in eastern DRC blame and felt stigma may be distinct from one another, i.e. a woman may feel stigmatized even if she does not feel directly responsible. Although 60% indicated thinking that someone else would not have gotten into the SV situation, only 15% of SV survivors in this study indicated feeling that the violence happened because of how they acted. Scales of SV stigma in high income settings include and largely focus on blame and guilt as a part of stigma, which may limit their use in DRC and other conflict-affected areas.
Felt stigma has been explained as related to, but distinct from, enacted stigma; people may express felt stigma even when they cannot name an instance of discrimination (i.e. enacted stigma) (Brown, Macintyre, & Trujillo, 2003; Jacoby, 1994). We found support for this separation in the loading of enacted stigma items onto a separate factor. The content of the resulting enacted stigma scale is consistent with other studies from the region. Qualitative studies of women in DRC have indicated the magnitude of family rejection and abandonment among SV survivors (Glass et al., 2011; Kelly, Betancourt, Mukwege, Lipton, & Vanrooyen, 2011). In a recent study, the Everyday Discrimination Scale (Williams, Yu, Jackson, & Anderson, 1997) was adapted for use with adolescent SV survivors in DRC and included items on survivors' perception of their treatment relative to others and acts of rejection (Verelst, De Schryver, De Haene, Broekaert, & Derluyn, 2014). Items measuring discrimination were similar to those on our scale.
Survivors of SV who had a child as a result of sexual violence scored higher on both scales than survivors who did not have a child. Both felt and enacted stigma were associated with increases in a range of mental health symptoms and functional impairment as hypothesized, supporting external construct validity. While based on the literature we had hypothesized that stigma would be negatively associated with seeking health services after experiencing sexual violence (Abrahams & Jewkes, 2010; Bartels et al., 2012; Starzynski, Ullman, Filipas, & Townsend, 2005), neither felt nor enacted stigma was related to accessing post-SV medical care. There are several factors specific to the eastern DRC context and to this study that may affect the comparability of our results to previous literature. Women in this sample were recruited from local psychosocial service providers and community-based women's organizations in sites where the IRC had worked for several years to establish referral systems and train local groups in the referral and care of SV survivors. It may be in this context women accessed post-SV medical services regardless of any stigma they may have felt and experienced or stigma was associated with different patterns of care seeking that we did not measure (e.g. the type of care sought or the timing of seeking services).
Also contrary to our hypothesis, felt stigma was not associated with whether the survivor reported telling another person about the SV. For disclosure of sexual violence, our hypothesis was based on the idea that a woman could not be discriminated against for sexual violence if others did not have knowledge of the event. In eastern DRC, SV and its consequences can be public, giving the broader community knowledge of the event regardless of a woman's choice to disclose. Examples of public acts or effects include attacks on villages, abduction by armed groups, pregnancy from rape with no access to abortion, and severe physical injuries. Further, though our question on disclosure was general (“Did you tell anyone…”), in our sample where seeking services was common and women were recruited through grass roots women's associations and psychosocial assistants in the community, survivors may have been reporting disclosure to a trusted peer or community-based provider who may be less likely to discriminate against disclosing survivors compared to general community members. Our sampling strategy could explain finding no association between felt stigma and disclosure and make our results not generalizable to a broader community sample. It is also worth investigating the dynamics of family support and reactions to disclosure in future studies taking into account the profile of perpetrators and the circumstances of violence, as almost half of the survivors in this study indicated experiencing rejection by their family due to SV.
The felt stigma scale was made up of items taken from the overall measure of mental distress. Results from the EFA indicated that the items included in the felt stigma scale were distinct from other symptoms of distress (for example “anger in the heart” or “too many thoughts”) as evidenced by loadings on different factors. Stigma scores, as expected, were also higher among survivors as compared to non-survivors of SV. Additionally, a sensitivity analysis conducted to explore the extent to which the felt stigma items were expressions of generalized symptoms of depression suggested felt stigma to be a distinct construct.
One limitation of our study was that our study sample was largely connected to NGO service providers and community organizations. This strongly limits the generalizability of our findings to survivors who are more isolated with no opportunity to connect with others knowledgeable about sexual violence or other survivors. Rather, our findings are relevant for women who are known to be SV survivors and are seeking or receiving services. Additionally, women were not asked about the characteristics of the perpetrator(s) as a part of the baseline survey for either trial. We therefore were not able to separate out the stigma experience of women who may have undergone violence perpetrated by different types of individuals (e.g. combatant, intimate partner, or other civilian). Another limitation is the lack of men in our sample, though they are also targets of SV in DRC (Johnson et al., 2010). Stigma against male survivors may be different than for females due to norms and perceptions around sexuality and masculinity. Further, these scales were developed and tested in the same sample. Future research should independently validate the scales and their structure in a separate sample of survivors of sexual violence.
Our measure could be improved in several ways. As with any secondary data analysis, our original study was not designed to measure and analyze stigma. In particular, the enacted stigma scale included only acts of rejection made by individuals and some were only relevant to married women with children. There may be other important acts of discrimination, such as finger pointing and gossiping by members of the community that were left out (Kelly et al., 2011). We did not have measures of structural discrimination, which has been included in other mental illness related stigma studies (Link, Yang, Phelan, & Collins, 2004). An example of structural discrimination would be if a SV survivor could only sell goods in a less trafficked or profitable location within a market. Additionally, the collected information only had data on some of the negative ways people may change their behavior towards survivors of SV. We did not have data on possible ways local people might have treated SV survivors with pity for example, or on positive changes such as treating survivors with compassion (Link et al., 2004).
Despite these limitations, we found support for the validity of two stigma scales and the structure of the scales were similar to discussions of stigma in the HIV and mental health literature. Incorporating measures of stigma into intervention research could provide valuable information on how interventions for survivors of SV impact their experience of stigma, and how highly stigmatized women may respond differently to services. It is common for unanticipated factors to emerge as important in the process of conducting research. Our process of scale creation and assessing validity could also be used to evaluate stigma measures in other low-resource and conflict-affected contexts. For eastern DRC, this process has helped to characterize and measure stigma associated with SV, which can help inform future programs to address this problem.
References
- Abrahams N, Jewkes R. Barriers to post exposure prophylaxis (PEP) completion after rape: a South African qualitative study. Culture, Health & Sexuality. 2010;12(5):471–484. doi: 10.1080/13691050903556316. http://doi.org/10.1080/13691050903556316. [DOI] [PubMed] [Google Scholar]
- Amowitz LL, Reis C, Lyons KH, Vann B, Mansaray B, Akinsulure-Smith AM, et al. Iacopino V. Prevalence of war-related sexual violence and other human rights abuses among internally displaced persons in Sierra Leone. JAMA: The Journal of the American Medical Association. 2002;287(4):513–521. doi: 10.1001/jama.287.4.513. http://doi.org/10.1001/jama.287.4.513. [DOI] [PubMed] [Google Scholar]
- Applied Mental Health Research Group. Johns Hopkins University Bloomberg School of Public Health; 2013a. Design, implementation monitoring, and evaluation of mental health and psychosocial assistance programs for trauma survivors in low resource countries: a user's manual for researchers and program implementers (Adult version), Module 1: Qualitative Assessment. Retrieved from http://www.jhsph.edu/research/centers-and-institutes/center-for-refugee-and-disaster-response/response_service/AMHR/dime/VOT_DIME_MODULE1_FINAL.pdf. [Google Scholar]
- Applied Mental Health Research Group. Johns Hopkins University Bloomberg School of Public Health; 2013b. Design, implementation monitoring, and evaluation of mental health and psychosocial assistance programs for trauma survivors in low resource countries: a user's manual for researchers and program implementers (Adult version), Module 2: Developing quantitative tools. Retrieved from http://www.jhsph.edu/research/centers-and-institutes/center-for-refugee-and-disaster-response/response_service/AMHR/dime/VOT_DIME_MODULE2_FINAL.pdf. [Google Scholar]
- Babalola SO. Dimensions and correlates of negative attitudes toward female survivors of sexual violence in Eastern DRC. Journal of Interpersonal Violence. 2014;29(9):1679–1697. doi: 10.1177/0886260513511531. http://doi.org/10.1177/0886260513511531. [DOI] [PubMed] [Google Scholar]
- Bartels SA, Scott JA, Leaning J, Kelly JT, Joyce NR, Mukwege D, VanRooyen MJ. Demographics and care-seeking behaviors of sexual violence survivors in South Kivu Province, Democratic Republic of Congo. Disaster Medicine and Public Health Preparedness. 2012;6(04):393–401. doi: 10.1001/dmp.2012.66. http://doi.org/10.1001/dmp.2012.66. [DOI] [PubMed] [Google Scholar]
- Bartels SA, Scott JA, Leaning J, Kelly JT, Mukwege D, Joyce NR, VanRooyen MJ. Sexual violence trends between 2004 and 2008 in South Kivu, Democratic Republic of Congo. Prehospital and Disaster Medicine. 2011;26(6):408–413. doi: 10.1017/S1049023X12000179. http://doi.org/10.1017/S1049023X12000179. [DOI] [PubMed] [Google Scholar]
- Bartels S, Kelly J, Scott J, Leaning J, Mukwege D, Joyce N, Vanrooyen M. Militarized sexual violence in South Kivu, Democratic Republic of Congo. Journal of Interpersonal Violence. 2012 doi: 10.1177/0886260512454742. http://doi.org/10.1177/0886260512454742. [DOI] [PubMed]
- Bass J, Bolton P, Murray S, Cole G, Robinette K, Poulton C, et al. Annan J. Report by the International Rescue Committee (IRC) and the Applied Mental Health Research Group (AMHR) at Johns Hopkins Bloomberg School of Public Health (JHBSPH) Washington, D.C: World Bank; 2014. Study of effectiveness of a social-economic intervention for sexual violence survivors in Eastern DRC. Retrieved from http://www.logica-wb.org/PDFs/LOGICA_StudySeries_VSLA.pdf. [Google Scholar]
- Bass JK, Annan J, McIvor Murray S, Kaysen D, Griffiths S, Cetinoglu T, et al. Bolton PA. Controlled trial of psychotherapy for Congolese survivors of sexual violence. New England Journal of Medicine. 2013;368(23):2182–2191. doi: 10.1056/NEJMoa1211853. http://doi.org/10.1056/NEJMoa1211853. [DOI] [PubMed] [Google Scholar]
- Bass JK, Ryder RW, Lammers M, Mukaba TN, Bolton PA. Post-partum depression in Kinshasa, Democratic Republic of Congo: validation of a concept using a mixed-methods cross-cultural approach. Tropical Medicine & International Health: TM & IH. 2008;13(12):1534–1542. doi: 10.1111/j.1365-3156.2008.02160.x. http://doi.org/10.1111/j.1365-3156.2008.02160.x. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107(2):238–246. doi: 10.1037/0033-2909.107.2.238. http://dx.doi.org/10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Brohan E, Slade M, Clement S, Thornicroft G. Experiences of mental illness stigma, prejudice and discrimination: a review of measures. BMC Health Services Research. 2010;10:80. doi: 10.1186/1472-6963-10-80. http://doi.org/10.1186/1472-6963-10-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown L, Macintyre K, Trujillo L. Interventions to reduce HIV/AIDS stigma: what have we learned? AIDS Education & Prevention. 2003;15(1):49–69. doi: 10.1521/aeap.15.1.49.23844. http://doi.org/10.1521/aeap.15.1.49.23844. [DOI] [PubMed] [Google Scholar]
- Campbell R, Ahrens CE, Sefl T, Wasco SM, Barnes HE. Social reactions to rape victims: healing and hurtful effects on psychological and physical health outcomes. Violence and Victims. 2001;16(3):287–302. [PubMed] [Google Scholar]
- Campbell R, Raja S. The sexual assault and secondary victimization of female veterans: help-seeking experiences with military and civilian social systems. Psychology of Women Quarterly. 2005;29(1):97–106. http://doi.org/10.1111/j.1471-6402.2005.00171.x. [Google Scholar]
- Coffey P, Leitenberg H, Henning K, Turner T, Bennett RT. Mediators of the long-term impact of child sexual abuse: perceived stigma, betrayal, powerlessness, and self-blame. Child Abuse & Neglect. 1996;20(5):447–455. doi: 10.1016/0145-2134(96)00019-1. [DOI] [PubMed] [Google Scholar]
- Decker MR, Peitzmeier S, Olumide A, Acharya R, Ojengbede O, Covarrubias L, et al. Brahmbhatt H. Prevalence and health impact of intimate partner violence and non-partner sexual violence among female adolescents aged 15–19 years in vulnerable urban environments: A multi-country study. Journal of Adolescent Health. 2014;55(6, Supplement):S58–S67. doi: 10.1016/j.jadohealth.2014.08.022. http://doi.org/10.1016/j.jadohealth.2014.08.022. [DOI] [PubMed] [Google Scholar]
- Deribe K, Tomczyk S, Mousley E, Tamiru A, Davey G. Stigma towards a neglected tropical disease: Felt and enacted stigma scores among podoconiosis patients in Northern Ethiopia. BMC Public Health. 2013;131178(1) doi: 10.1186/1471-2458-13-1178. http://doi.org/10.1186/1471-2458-13-1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desai S, Perry MJ. Tracking gender-based human rights violations in postwar Kosovo. American Journal of Public Health. 2004;94(8):1304–1307. doi: 10.2105/ajph.94.8.1304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dossa NI, Zunzunegui MV, Hatem M, Fraser WD. Mental health disorders among women victims of conflict-related sexual violence in the Democratic Republic of Congo. Journal of Interpersonal Violence. 2014 doi: 10.1177/0886260514552447. http://doi.org/10.1177/0886260514552447. [DOI] [PubMed]
- Ellsberg M, Jansen HA, Heise L, Watts CH, Garcia-Moreno C. Intimate partner violence and women's physical and mental health in the WHO multi-country study on women's health and domestic violence: an observational study. Lancet. 2008;371(9619):1165–1172. doi: 10.1016/S0140-6736(08)60522-X. http://doi.org/10.1016/S0140-6736(08)60522-X. [DOI] [PubMed] [Google Scholar]
- Flora DB, Finkel EJ, Foshee VA. Higher order factor structure of a self-control test: Evidence from confirmatory factor analysis with polychoric correlations. Educational and Psychological Measurement. 2003;63(1):112–127. http://doi.org/10.1177/0013164402239320. [Google Scholar]
- Gibson LE, Leitenberg H. The impact of child sexual abuse and stigma on methods of coping with sexual assault among undergraduate women. Child Abuse & Neglect. 2001;25(10):1343–1361. doi: 10.1016/s0145-2134(01)00279-4. http://doi.org/10.1016/S0145-2134(01)00279-4. [DOI] [PubMed] [Google Scholar]
- Glass N, Ramazani P, Tosha M, Mpanano M, Cinyabuguma M. A Congolese-US participatory action research partnership to rebuild the lives of rape survivors and their families in eastern Democratic Republic of Congo. Global Public Health. 2011:1–12. doi: 10.1080/17441692.2011.594449. http://doi.org/10.1080/17441692.2011.594449. [DOI] [PubMed]
- Goffman E. Stigma: Notes on the Management of Spoiled Identity. Englewood Cliffs, NJ: Prentice Hall; 1963. [Google Scholar]
- Hasan MT, Nath SR, Khan NS, Akram O, Gomes TM, Rashid SF. Internalized HIV/AIDS-related stigma in a sample of HIV-positive people in Bangladesh. Journal of Health, Population, and Nutrition. 2012;30(1):22–30. doi: 10.3329/jhpn.v30i1.11272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hesbacher PT, Rickels K, Morris RJ, Newman H, Rosenfeld H. Psychiatric illness in family practice. The Journal of Clinical Psychiatry. 1980;41(1):6–10. [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. http://doi.org/10.1080/10705519909540118. [Google Scholar]
- Jacoby A. Felt versus enacted stigma: a concept revisited. Evidence from a study of people with epilepsy in remission. Social Science & Medicine. 1994;1982;38(2):269–274. doi: 10.1016/0277-9536(94)90396-4. [DOI] [PubMed] [Google Scholar]
- Johnson K, Scott J, Rughita B, Kisielewski M, Asher J, Ong R, Lawry L. Association of sexual violence and human rights violations with physical and mental health in territories of the Eastern Democratic Republic of the Congo. JAMA: The Journal of the American Medical Association. 2010;304(5):553–562. doi: 10.1001/jama.2010.1086. http://doi.org/10.1001/jama.2010.1086. [DOI] [PubMed] [Google Scholar]
- Kelly J, Kabanga J, Cragin W, Alcayna-Stevens L, Haider S, Vanrooyen MJ. If your husband doesn't humiliate you, other people won't’: gendered attitudes towards sexual violence in eastern Democratic Republic of Congo. Global Public Health. 2012;7(3):285–298. doi: 10.1080/17441692.2011.585344. http://doi.org/10.1080/17441692.2011.585344. [DOI] [PubMed] [Google Scholar]
- Kelly JT, Betancourt TS, Mukwege D, Lipton RI, Vanrooyen MJ. Experiences of female survivors of sexual violence in eastern Democratic Republic of the Congo: a mixed-methods study. Conflict and Health. 2011;5(1):25. doi: 10.1186/1752-1505-5-25. http://doi.org/10.1186/1752-1505-5-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keusch GT, Wilentz J, Kleinman A. Stigma and global health: developing a research agenda. Lancet. 2006;367(9509):525–527. doi: 10.1016/S0140-6736(06)68183-X. http://doi.org/10.1016/S0140-6736(06)68183-X. [DOI] [PubMed] [Google Scholar]
- Lasalvia A, Zoppei S, Van Bortel T, Bonetto C, Cristofalo D, Wahlbeck K, et al. Thornicroft G. Global pattern of experienced and anticipated discrimination reported by people with major depressive disorder: a cross-sectional survey. Lancet. 2012 doi: 10.1016/S0140-6736(12)61379-8. http://doi.org/10.1016/S0140-6736(12)61379-8. [DOI] [PubMed]
- Lee J, Kim J, Lim H. Rape myth acceptance among Korean college students: the roles of gender, attitudes toward women, and sexual double standard. Journal of Interpersonal Violence. 2010;25(7):1200–1223. doi: 10.1177/0886260509340536. http://doi.org/10.1177/0886260509340536. [DOI] [PubMed] [Google Scholar]
- Lekas HM, Siegel K, Leider J. Felt and enacted stigma among HIV/HCV-coinfected adults: the impact of stigma layering. Qualitative Health Research. 2011;21(9):1205–1219. doi: 10.1177/1049732311405684. http://doi.org/10.1177/1049732311405684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link BG, Phelan JC. Stigma and its public health implications. Lancet. 2006;367(9509):528–529. doi: 10.1016/S0140-6736(06)68184-1. http://doi.org/10.1016/S0140-6736(06)68184-1. [DOI] [PubMed] [Google Scholar]
- Link BG, Yang LH, Phelan JC, Collins PY. Measuring mental illness stigma. Schizophrenia Bulletin. 2004;30(3):511–541. doi: 10.1093/oxfordjournals.schbul.a007098. [DOI] [PubMed] [Google Scholar]
- Liu SH, Srikrishnan AK, Zelaya CE, Solomon S, Celentano DD, Sherman SG. Measuring perceived stigma in female sex workers in Chennai, India. AIDS Care. 2011;23(5):619–627. doi: 10.1080/09540121.2010.525606. http://doi.org/10.1080/09540121.2010.525606. [DOI] [PubMed] [Google Scholar]
- Marsh HW, Balla JR, McDonald RP. Goodness-of-fit indexes in confirmatory factor analysis: The effect of sample size. Psychological Bulletin. 1988;103(3):391–410. http://doi.org/10.1037/0033-2909.103.3.391. [Google Scholar]
- Marsh M, Purdin S, Navani S. Addressing sexual violence in humanitarian emergencies. Global Public Health. 2006;1(2):133–146. doi: 10.1080/17441690600652787. http://doi.org/10.1080/17441690600652787. [DOI] [PubMed] [Google Scholar]
- Mollica RF, Caspi-Yavin Y, Bollini P, Truong T, Tor S, Lavelle J. The Harvard Trauma Questionnaire. Validating a cross-cultural instrument for measuring torture, trauma, and posttraumatic stress disorder in Indochinese refugees. The Journal of Nervous and Mental Disease. 1992;180(2):111–116. [PubMed] [Google Scholar]
- Muthen LK, Muthen BO. Mplus user's guide (Version 7) Los Angeles, CA: Muthen & Muthen; 2011. [Google Scholar]
- Nyblade LC. Measuring HIV stigma: existing knowledge and gaps. Psychology, Health & Medicine. 2006;11(3):335–345. doi: 10.1080/13548500600595178. http://doi.org/10.1080/13548500600595178. [DOI] [PubMed] [Google Scholar]
- Peterman A, Palermo T, Bredenkamp C. Estimates and determinants of sexual violence against women in the Democratic Republic of Congo. American Journal of Public Health. 2011;101(6):1060–1067. doi: 10.2105/AJPH.2010.300070. http://doi.org/10.2105/AJPH.2010.300070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scambler G, Hopkins A. Being epileptic: coming to terms with stigma. Sociology of Health & Illness. 1986;8(1):26–43. http://doi.org/10.1111/1467-9566.ep11346455. [Google Scholar]
- Simbayi LC, Kalichman S, Strebel A, Cloete A, Henda N, Mqeketo A. Internalized stigma, discrimination, and depression among men and women living with HIV/AIDS in Cape Town, South Africa. Social Science & Medicine. 2007;64(9):1823–1831. doi: 10.1016/j.socscimed.2007.01.006. http://doi.org/10.1016/j.socscimed.2007.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starzynski LL, Ullman SE, Filipas HH, Townsend SM. Correlates of women's sexual assault disclosure to informal and formal support sources. Violence and Victims. 2005;20(4):417–432. http://dx.doi.org/10.1891/0886-6708.20.4.417. [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software: Release. Vol. 12. College Station, TX: StataCorp LP; 2011. [Google Scholar]
- Steiner B, Benner MT, Sondorp E, Schmitz KP, Mesmer U, Rosenberger S. Sexual violence in the protracted conflict of DRC programming for rape survivors in South Kivu. Conflict and Health. 2009;33(1) doi: 10.1186/1752-1505-3-3. http://doi.org/10.1186/1752-1505-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swiss S, Jennings PJ, Aryee GV, Brown GH, Jappah-Samukai RM, Kamara MS, et al. Turay-Kanneh RS. Violence against women during the Liberian civil conflict. JAMA: The Journal of the American Medical Association. 1998;279(8):625–629. doi: 10.1001/jama.279.8.625. [DOI] [PubMed] [Google Scholar]
- Tavrow P, Withers M, Obbuyi A, Omollo V, Wu E. Rape myth attitudes in rural Kenya: toward the development of a culturally relevant attitude scale and “blame index. Journal of Interpersonal Violence. 2013;28(10):2156–2178. doi: 10.1177/0886260512471086. http://doi.org/10.1177/0886260512471086. [DOI] [PubMed] [Google Scholar]
- Thornicroft G, Brohan E, Rose D, Sartorius N, Leese M. Global pattern of experienced and anticipated discrimination against people with schizophrenia: a cross-sectional survey. Lancet. 2009;373(9661):408–415. doi: 10.1016/S0140-6736(08)61817-6. http://doi.org/10.1016/S0140-6736(08)61817-6. [DOI] [PubMed] [Google Scholar]
- Thornicroft G, Rose D, Kassam A, Sartorius N. Stigma: ignorance, prejudice or discrimination? The British Journal of Psychiatry: The Journal of Mental Science. 2007;190:192–193. doi: 10.1192/bjp.bp.106.025791. http://doi.org/10.1192/bjp.bp.106.025791. [DOI] [PubMed] [Google Scholar]
- Ullman SE. Psychometric characteristics of the Social Reactions Questionnaire: A measure of reactions to sexual assault victims. Psychology of Women Quarterly. 2000;24(3):257–271. http://doi.org/10.1111/j.1471-6402.2000.tb00208.x. [Google Scholar]
- Ullman SE, Townsend SM, Filipas HH, Starzynski LL. Structural models of the relations of assault severity, social support, avoidance coping, self-blame, and PTSD among sexual assault survivors. Psychology of Women Quarterly. 2007;31(1):23–37. http://doi.org/10.1111/j.1471-6402.2007.00328.x. [Google Scholar]
- Verelst A, De Schryver M, De Haene L, Broekaert E, Derluyn I. The mediating role of stigmatization in the mental health of adolescent victims of sexual violence in Eastern Congo. Child Abuse & Neglect. 2014 doi: 10.1016/j.chiabu.2014.04.003. http://doi.org/10.1016/j.chiabu.2014.04.003. [DOI] [PubMed]
- Ward C. The attitudes toward rape victims scale. Psychology of Women Quarterly. 1988;12(2):127–146. http://doi.org/10.1111/j.1471-6402.1988.tb00932.x. [Google Scholar]
- Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health: Socio-economic status, stress and discrimination. Journal of Health Psychology. 1997;2(3):335–351. doi: 10.1177/135910539700200305. http://doi.org/10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- Winokur A, Winokur DF, Rickels K, Cox DS. Symptoms of emotional distress in a family planning service: stability over a four-week period. The British Journal of Psychiatry: The Journal of Mental Science. 1984;144:395–399. doi: 10.1192/bjp.144.4.395. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Geneva, Switzerland: World Health Organization; 2013a. Responding to intimate partner violence and sexual violence against women: WHO clinical and policy guidelines. Retrieved from http://apps.who.int/iris/bitstream/10665/85240/1/9789241548595_eng.pdf. [PubMed] [Google Scholar]
- World Health Organization. Geneva, Switzerland: World Health Organization; 2013b. Global and regional estimates of violence against women: prevalence and health effects of intimae partner violence and non-partner sexual violence. Retrieved from http://www.who.int/reproductivehealth/publications/violence/9789241564625/en/ [Google Scholar]