The United Kingdom is in the grip of a nationwide mumps epidemic with almost 5000 notifications in the first month of 2005 alone.1 Most patients are aged between 19 and 23, and there is now the threat of outbreaks among under-immunised children.
As a result of the measles, mumps, and rubella (MMR) vaccine, which was introduced in 1988, the current generation of practising doctors have little experience of mumps infection. Mumps may have permanent sequelae, and not all cases can be diagnosed clinically. Here we explain the basis of the current epidemic and review the epidemiology, clinical presentation, complications, laboratory confirmation, and treatment of mumps.
Methods
We searched Medline for evidence based information on the internet, using a range of search terms. Other internet based resources included the websites of the Health Protection Agency (HPA), the World Health Organization (WHO), and the US Centers for Disease Control (CDC). We also used various formal texts.
Mumps and its transmission
Mumps is an enveloped, single stranded RNA virus belonging to the family paramyxoviridae, which causes an acute infectious disease mainly in children and young adults.2 Transmission is by droplet spread, and humans are the only known host. Mumps is highly infectious and spreads rapidly in susceptible people living in close proximity. The number of secondary cases of infection expected to result from an index case of mumps in a fully susceptible population (R0 or basic reproduction number) is 10-12. By comparison, measles—a notoriously infectious virus—has an R0 of 15-17.3
The incubation period from infection to appearance of the characteristic swelling of the parotid glands is 15-24 days.4 The infectious period starts several days before the onset of parotitis and continues for several days afterwards.4 w1 Infection control guidance for schools and nurseries advises that children stay away from school for five days from the onset of swollen glands.4
The current UK epidemic
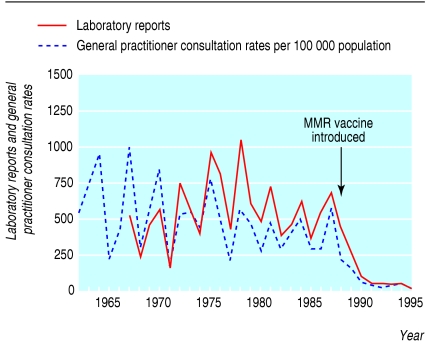
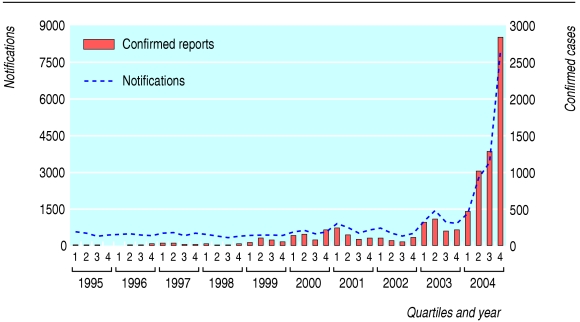
In the UK, mumps epidemics used to occur in the winter and spring months every few years.5 MMR vaccination of 1 year olds was started in 1988, coinciding with a preschool catch-up programme. Mumps became notifiable at that time, and its incidence fell drastically during the 1990s (fig 1). With little measles in circulation, unvaccinated children were not being exposed and remained susceptible. Small outbreaks of measles occurred in children at secondary school, threatening an epidemic and prompting the 1994 national catch-up campaign for 5-16 year olds. Instead of the MMR vaccine, they received a combined measles and rubella preparation.5 This was because of a shortage of mumps vaccine at the time, when sufficient quantities of MMR vaccine were not available. The recent outbreaks (fig 2) have particularly affected individuals born between 1982 and 1986 who have neither been previously exposed to natural infection (due to the reduction in circulating mumps) nor protected by vaccination. People born before 1982 are not susceptible, with up to 98% seropositivity rates, owing to early natural infection in the pre-MMR era.6
Fig 1.
Incidence of mumps and numbers of confirmed cases reported to the Communicable Disease Surveillance Centre, 1962-95
Fig 2.
Mumps notifications and confirmed cases, 1995-2004 by quarter
Summary points
A nationwide outbreak of mumps is occurring predominantly in 19-23 year olds in the UK
Cases are also occurring in susceptible children
Complications of mumps are not uncommon and can be severe
Salivary IgM testing is a useful seroepidemiological tool
No opportunity should be missed to ensure that all children and young adults have had two doses of the measles, mumps, and rubella (MMR) vaccine
Clinical presentation
Patients may have a fever in the prodromal period, with or without headache. Parotid swelling is present in 95% of symptomatic cases of mumps2 and is bilateral in 90% of these (fig 3).w2 Local tenderness, and occasionally earache, precedes parotid swelling. Normally the parotids are not readily discernible and are said to be swollen once clinically apparent. The parotitis is due to direct infection of ductal epithelium and local inflammation and may be accompanied by a rise in serum amylase concentrations.8 The orifice of the glandular duct (Stensen's duct) may become red and oedematous.2
Fig 3.

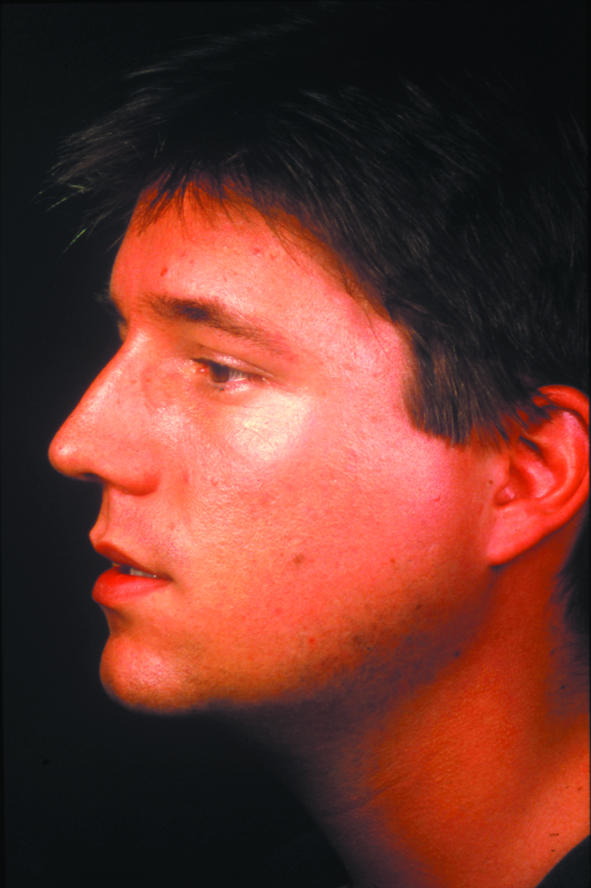
Bilateral parotid swelling in a young man with mumps
Thirty per cent of infections are subclinical,2 and other manifestations of mumps may occur without parotid swelling. Although the presentation is similar, clinical symptoms are usually more severe in adults and adolescents than children.
Differential diagnosis
In the presence of parotitis and particularly during an epidemic, the diagnosis of mumps is straightforward. Other causes of unilateral or bilateral parotitis warrant consideration however. Infectious aetiologies include other viral agents such as parainfluenza, coxsackievirus, influenza A, Epstein-Barr virus, adenovirus, and suppurative bacterial infection. Non-infectious causes include salivary calculi, tumours, sarcoid, Sjögren's syndrome, ingestion of starch or thiazides, and iodine sensitivity.8
Complications
Box 1 shows potential complications associated with mumps.
Before the introduction of MMR vaccination, mumps was the commonest cause of viral meningitis5 and one of the leading causes of hearing loss in children younger than 15 years of age in the UK.2 On the basis of cerebrospinal fluid pleocytosis at least half of all mumps infections involve the central nervous system.8 w3
Neurological complications such as meningitis and encephalitis can precede or follow parotitis; they can even occur in the absence of salivary gland enlargement in up to 50% of cases.8 w2 Young men seem to be at greatest risk of associated meningoencephalitis.w4 Seizures occur in 20-30% of children with neurological symptoms, although the electroencephalogram is usually normal.8 The relation of these seizures to febrile episodes is unclear from the literature.
Clinical case definition of mumps (definition from the Centers for Disease Control and Prevention7)
“An illness with acute onset of unilateral or bilateral tender, self-limited swelling of the parotid or other salivary gland, lasting greater than or equal to 2 days, and without other apparent cause”
Box 1: Complications
Complications of mumps can be serious and include the following2,8,9,10 w1 w2
Orchitis (usually unilateral) in 20% of postpubertal young men
Oophoritis in 5% of postpubertal young women
Aseptic meningitis in 15%
Encephalitis in 1 in 6000
Permanent unilateral deafness in 1 in 15 000
Pancreatitis in up to 5%
Arthritis, thyroiditis, myocarditis, and, very rarely, hepatitis
Increased risk of miscarriage in the first 12 weeks of pregnancy
The outcome of disease of the central nervous system is usually good, although rare permanent sequelae may include obstructive hydrocephalus, unilateral deafness, myelitis, and cerebellar ataxia.8 The fatality rate of involvement of the central nervous system is around 1% and can be due to acute or post-infectious encephalomyelitis.w5 We did not identify any predictors of poor outcome in meningoencephalitis in the published literature.
Orchitis is a common complication occurring in 20% of adult men with mumps.2,9 Infection of the parenchyma leads to testicular atrophy in 40-70% of cases with orchitis. Usually only one testis is affected, but disease is bilateral in 15-30% of patients with mumps orchitis, and of these 13% result in hypofertility.9
Pancreatitis usually presents with epigastric pain, and can be confirmed by detection of increased levels of lipase or pancreatic amylase isoenzyme in the serum. Evidence for the aetiological role of mumps pancreatitis in type 1 diabetes is controversial.w6 w7
Laboratory tests
Box 2 shows the laboratory criteria for diagnosing mumps.
Routine blood testing may show a leucopenia with a relative lymphocytosis or sometimes a neutrophil leucocytosis. Raised C reactive protein and erythrocyte sedimentation rate may also be seen.2
Box 2: Laboratory diagnostic criteria
Isolation of mumps virus or nucleic acid from clinical specimen, or
Significant rise in mumps specific immunoglobulin titres between acute and convalescent serum samples by any standard serological assay, or
Positive serological test for mumps IgM in serum or saliva
Only 10% of suspected mumps cases were laboratory confirmed in England and Wales between 1989 and 1999,w1 highlighting the weakness of clinical diagnosis during a period of low transmission. In the absence of clinically apparent parotitis, a laboratory diagnosis is required even in the context of an epidemic.
Mumps specific IgM is detectable in serum as early as 11 days after exposure and is almost always present by the time of clinical illness. In the UK, mumps can conveniently be confirmed by detection of specific IgM antibody in salivary samples. This method is acceptable to children and parents and forms the basis for case confirmation by the Health Protection Agency.11 The specificity, as determined by analysis of blood donor samples, is greater than 98%.12 In the first week of illness the sensitivity is 75%, increasing to 100% after the first week.12 When salivary IgM is negative, reverse transcription-polymerase chain reaction can be used to detect mumps RNA in saliva.13 This sensitive and rapid method facilitates sequencing and subsequent genotyping for epidemiological purposes and is largely superseding viral isolation in animal cell lines. Viral culture or nucleic acid detection from urine (owing to replication in the kidney) is also possible for up to two weeks after symptoms begin.8
Where mumps is a cause of meningoencephalitis, cerebrospinal fluid typically shows a lymphocytosis averaging 250 cells/mm3, raised protein in 60-70% of cases, and a normal opening pressure.8 The glucose in cerebrospinal fluid is less than 50% of the serum value in up to a quarter of patients.8 Mumps virus nucleic acid can be detected in the cerebrospinal fluid of up to 96% of cases of mumps meningoencephalitis by reverse transcription-polymerase chain reaction and has been found up to two years later.14 Mumps specific IgM can also be found in cerebrospinal fluid in half of cases and IgG in a third,15 sometimes persisting for a year or more with pleocytosis. Such persistent abnormalities of cerebrospinal fluid have not been correlated with long term sequelae.
Treatment
No antiviral treatment for mumps exists. Treatment is supportive and may include the use of anticonvulsants or even ventilatory support in more severe neurological cases.
Mumps in pregnancy and in immunocompromised hosts
Mumps in pregnancy has not been associated with congenital malformations,16 although the risk of miscarriage with mumps infection is increased in the first trimester.10
No cases of mumps in patients who have had a transplant or are HIV positive have been published, although a small study of mumps in children with acute lymphoblastic leukaemia showed a mild course.17 Little is known about mumps in immunocompromised patients, but current practice includes optimisation of immune status before transplantation (with re-vaccination if necessary), and continued monitoring of antibody status.
Although MMR is generally contraindicated in immunocompromised patients, including recipients of organ transplants, current evidence shows that the vaccine can be safely given to recipients of bone marrow transplants two years after transplantation in the absence of graft versus host disease.18,19 MMR vaccination is recommended for asymptomatic HIV positive children without evidence of severe immunosuppression, with the first dose at 12 months and the second as soon as 28 days later.7,20 Earlier administration may be appropriate in children at risk of exposure to measles.7 Although antibody related protection can be inferred in immunocompetent people, it is not known whether seropositivity confers adequate protection in immunocompromised patients.
Susceptible household and other close contacts of immunocompromised individuals should be fully protected. Recipients do not transmit the MMR vaccine viruses and do not therefore pose a risk to contacts.5,7
Mumps control and prevention
No postexposure prophylaxis for mumps is available. Passive immunisation with immune globulin does not seem to be useful in outbreak control.8 Vaccination of exposed individuals does not prevent progression to infection. Isolation of cases together with mass vaccination of susceptible people is likely to be the most effective course of action in controlling epidemics.
MMR vaccine coverage
WHO recommends immunisation coverage of 90% to prevent outbreaks of mumps.w8 But uptake of the MMR vaccine among 2 year olds in the UK fell from around92% in early 1995 to around 80% in 2003-4.w1 In some areas of London, as few as 60% of 2 year olds had received a first dose of MMR.21 This would account for our recent experience with mumps in younger children.
Additional educational resources
Health Protection Agency website (www.hpa.org.uk/infections/topics_az/mumps/menu.htm)—Provides up to date statistics on disease incidence and vaccine coverage
Communicable Disease Report Weekly (www.hpa.org.uk/cdr/default.htm)—Weekly electronic bulletin with surveillance data and outbreak reports
US Centers for Disease Control and Prevention (CDC, www.cdc.gov)—Government agency that serves as the national focus for developing and applying disease prevention and control, environmental health, and health promotion and education activities designed to improve the health of the people of the United States
Information for patients
Mumps information (http://health.allrefer.com/health/mumps-info.html)—American based resource for patients that provides visual as well as text based explanations regarding mumps illness
MMR information
NHS Immunisation Information. MMR—the facts. www.mmrthefacts.nhs.uk (accessed 19 Apr 2005)
Patient UK. MMR immunisation. www.patient.co.uk/showdoc/23068781 (accessed 19 Apr 2005)
Information on mumps and pregnancy
Perinatology.com. Infections during pregnancy. Mumps virus. www.perinatology.com/exposures/Infection/Mumps.htm (accessed 19 Apr 2005)
Birth.com. Mumps during pregnancy. www.birth.com.au/class.asp?class=6622&page=1 (accessed 19 Apr 2005)
Is one dose of MMR adequate for mumps prevention?
Premarketing serological response rates of 95% to mumps vaccine were reported, although estimates since have ranged from 60% to 90%.22 The discrepancy is explained by a 15% seronegativity rate after one year in children initially responding to vaccination,23 and data showing very low concentrations of mumps antibody in around a quarter of children two to four years later.24 In light of this, outbreaks in schools with high single dose MMR coveragew9 are not altogether surprising.
A second dose of MMR increases the mumps seropositivity rate to 95% and leads to higher sustained antibody concentrations.25 A second MMR dose was introduced into the routine immunisation schedule in the UK in 1996.9 Although a catch-up programme was conducted at this time, people born before 1990 may have had only one dose of MMR vaccine, therefore expanding the pool of susceptible people in the current epidemic.
Conclusions
The initial success of MMR vaccination in controlling mumps has been compromised in recent years with sporadic outbreaks. Since 2004 the number of reported and confirmed cases of mumps has increased, culminating in the current epidemic. As a result, doctors once again need to include mumps in the differential diagnosis of a broad range of conditions in adults and children. This epidemic underlines the importance of ensuring that all children and young adults have received two doses of MMR.
Supplementary Material
 Additional references w1-w9 are on bmj.com
Additional references w1-w9 are on bmj.com
We thank Rachel Heathcock, consultant in communicable disease control, South East London Local Health Protection Unit, for her critical review of this paper. Thanks also to Alice Gem for secretarial assistance with the manuscript.
Competing interests: EMM has received sponsorship from Aventis Pasteur MSD and SmithKlineBeecham towards conference attendance in the past five years.
References
- 1.Health Protection Agency. National increase in mumps cases continues. Press release 4 February 2005. www.hpa.org.uk/hpa/news/articles/press_releases/2005/050204_mumps.htm (accessed 7 Apr 2005).
- 2.Leinikki P. Mumps. In: Zuckerman AJ, Banatvala JE, Pattison JR, Griffiths PD, Schoub BD, eds. Principles and practice of clinical virology. 4th ed. Chichester: Wiley, 2004: 459-66.
- 3.Anderson RM, May RM. Modern vaccines: immunisation and herd immunity. Lancet 1990;335: 641-5. [DOI] [PubMed] [Google Scholar]
- 4.Richardson M, Elliman D, Maguire H, Simpson J, Nicoll A. Evidence base of incubation periods, periods of infectiousness and exclusion policies for the control of communicable diseases in schools and preschools. Paediatr Infect Dis J 2001;20: 380-91. [DOI] [PubMed] [Google Scholar]
- 5.Department of Health, Welsh Office, Scottish Office Department of Health, DHSS (Northern Ireland), Measles/mumps/rubella (MMR). In: Salisbury DM, Begg NT, eds. Immunisation against infectious disease. London: HMSO, 1996: 125-46.
- 6.Best JM, Palmer SJ, Hesketh L, Morgan-Capner P, Mathers K. Immunity to viral infections among medical students in London. BMJ 1994;309: 876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Infection. Measles, mumps, and rubella—vaccine use and strategies for elimination of measles, rubella, and congenital rubella syndrome and control of mumps: recommendations of the Advisory Committee on Immunization Practices (ACIP). Morb Mortal Wkly Rep MMWR 1998;47:RR-8:1-48. www.cdc.gov/nip/vaccine/MMR/default.htm (accessed 7 Apr 2005). [PubMed]
- 8.Carbone KM, Wolinsky JS. Mumps virus. In: Knipe D, Howley P, eds. Fields virology. 4th ed. Vol 1. Philadelphia: Lippincott, Williams and Wilkins, 2001: 1381-400. [Google Scholar]
- 9.Dejucq N, Jegou B. Viruses in the mammalian male genital tract and their effects on the reproductive system. Microbiol Mol Biol Rev 2001;65: 208-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Siegel M, Fuerst HT, Peress NS. Comparative fetal mortality in maternal virus diseases: a prospective study on rubella, measles, mumps, chickenpox, and hepatitis. N Engl J Med 1966;274: 768. [DOI] [PubMed] [Google Scholar]
- 11.Gay N, Miller E, Hesketh P, Morgan-Capner P, Ramsay M, Cohen B, et al. Mumps surveillance in England and Wales supports introduction of two dose vaccination schedule. Commun Dis Rep Rev 1997;7: R21-6. [PubMed] [Google Scholar]
- 12.Perry KR, Brown DW, Parry JV, Panday S, Pipkin C, Richards A. Detection of measles, mumps and rubella antibodies in saliva using antibody capture radioimmunoassay. J Med Virol 1993;40: 235-40. [DOI] [PubMed] [Google Scholar]
- 13.Uchida K, Shinohara M, Shimada S, Segawa Y, Doi R, Gotoh A, et al. Rapid and sensitive detection of mumps virus RNA directly from clinical samples by real-time PCR. J Med Virol 2005;75: 470-4. [DOI] [PubMed] [Google Scholar]
- 14.Poggio GP, Rodriguez C, Cisterna D, Freire MC, Cello J. Nested PCR for rapid detection of mumps virus in cerebrospinal fluid from patients with neurological diseases. J Clin Microbiol 2000;38: 274-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Forsberg P, Fryden A, Link H, Orvell C. Viral IgM and IgG antibody synthesis within the central nervous system in mumps meningitis. Acta Neurol Scand 1986;73: 372-80. [DOI] [PubMed] [Google Scholar]
- 16.Siegel M. Congenital malformations following chickenpox, measles, mumps, and hepatitis. Results of a cohort study. JAMA 1973;226: 1521-4. [PubMed] [Google Scholar]
- 17.De Boer AW, de Vaan GA. Mild course of mumps in patients with acute lymphoblastic leukaemia. Eur J Pediatr 1989;148: 618-9. [DOI] [PubMed] [Google Scholar]
- 18.King SM, Saunders EF, Petric M, Gold R. Response to measles, mumps and rubella vaccine in paediatric bone marrow transplant recipients. Bone Marrow Transplant 1996;17: 633-6. [PubMed] [Google Scholar]
- 19.Ljungman P, Fridell E, Lonnqvist B, Bolme P, Bottiger M, Gahrton G, et al. Efficacy and safety of vaccination of transplant recipients with a live attenuated measles, mumps and rubella vaccine. J Infect Dis 1989;159: 610-5. [DOI] [PubMed] [Google Scholar]
- 20.Goon P, Cohen B, Jin L, Watkins R, Tudor-Williams G. MMR vaccine in HIV-infected children—potential hazards? Vaccine 2001;19: 3816-9. [DOI] [PubMed] [Google Scholar]
- 21.Kidd IM, Booth CJ, Rigden SP, Tong CY, MacMahon EM. Measles-associated encephalitis in children with renal transplants: a predictable effect of waning herd immunity? Lancet 2003;362: 832. [DOI] [PubMed] [Google Scholar]
- 22.Vandermeulen C, Roelants M, Vermoere M, Roseeuw K, Goubau P, Hoppenbrouwers K. Outbreak of mumps in a vaccinated child population: a question of vaccine failure? Vaccine 2004;22: 2713-6. [DOI] [PubMed] [Google Scholar]
- 23.Mitchell LA, Tingle AJ, Decarie D, Lajeunesse C. Serologic responses to measles, mumps, and rubella (MMR) vaccine in healthy infants: failure to respond to measles and mumps components may influence decisions on timing of the second dose of MMR. Can J Public Health 1998;89: 325-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pebody RG, Gay NJ, Hesketh LM, Vyse A, Morgan-Capner P, Brown D, et al. Immunogenicity of second dose measles-mumps-rubella (MMR) vaccine and implications for serosurveillance. Vaccine 2002;20: 1134-40. [DOI] [PubMed] [Google Scholar]
- 25.Davidkin I, Valle M, Julkunen I. Persistence of anti-mumps virus antibodies after a two-dose MMR vaccination. A nine-year follow-up. Vaccine 1995;13: 1617-22. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.