Abstract
Background
Neuropsychological evidence is not sufficient concerning whether there is cognitive impairment in patients with primary insomnia. Further study is needed in this regard.
Aims
To measure the changes in cognitive functioning in patients with primary insomnia.
Methods
40 patients with insomnia (insomnia group) and 48 normal sleepers (control group) were tested using the Pittsburgh Sleep Quality Index (PSQI), episodic memory test, and Montreal Cognitive Assessment (MoCA).
Results
The insomnia group had significantly lower scores than the control group in the naming (t=3.17, p=0.002), immediate memory (t=3.33, p=0.001), and delayed recall (t=6.05, p=0.001) sections of the MoCA, as well as a lower overall score on the MoCA (t=3.24, p=0.002). Participants with different degrees of insomnia also had significantly different scores in naming (F=7.56, p=0.001), language (F=3.22, p=0.045), total score (F=6.72, p=0.002), delayed memory (F=8.41, p=0.001), and delayed recall (F=22.67, p=0.001) sections of the MoCA. The age of primary insomnia patients was correlated to MoCA total score, immediate memory, delayed recall, and delayed recognition function, also with statistical significance. The years of education of primary insomnia patients was also significantly correlated to overall MoCA score, as well as visuospatial and executive function, naming, attention, language, and abstraction sections of the MoCA.
Conclusion
Primary insomnia patients have cognitive impairment. The more severe the insomnia is, the wider the range of and the more serious the degree of cognitive impairment is.
Key words: primary insomnia, cognitive function, episodic memory, influencing factors
Abstract
背景
原发性失眠患者是否存在认知功能损害, 其神 经心理学的证据仍不充分, 需要作进一步研究。
目的
探讨原发性失眠患者认知功能改变及其影响因 素。
方法
对40 例失眠患者(失眠组)和48 例正常睡 眠者(对照组)进行匹兹堡睡眠质量指数(Pittsburgh SleepQuality Index , PSQI)、 情景记忆测试和蒙特利尔 认知评估(Montreal cognitive assessment, MoCA)测验。
结果
失眠者MoCA 测试的总分(t=3.24, p=0.002)、 命名(t=3.17, p=0.002)成绩较对照组差, 即刻记忆 (t=3.33, p=0.001)、 延迟回忆(t=6.05, p=0.001) 成 绩较对照组差。 不同失眠程度的被试在命名(F=7.56, p=0.001)、 语言(F=3.22, p=0.045)、 总分(F=6.72, p=0.002)、 延迟记忆(F=8.41, p=0.001)、 延迟回忆(F=22.67, p=0.001) 差异显著。 且原发性失眠患者的年龄与MoCA 总分、 即刻记忆、 延迟回忆和延迟再认功能相关有统 计学意义, 受教育年限与 MoCA 总分、 视空间与执行 功能、 命名、 注意、 语言、 抽象等功能相关有统计学 意义。
结论
原发性失眠患者存在认知功能损害;且失眠程度越严重,认知功能损害范围越广,程度越重。
1. Introduction
Insomnia is a sleep disorder involving difficulty initiating or maintaining sleep. It leads to a lack of sleep time or poor sleep quality which cannot meet an individual’s physiological needs, and as a result significantly affects activities during the day.
According to the criteria of the Diagnostic and Statistical Manual of Mental Disorders-IV (DSM-IV), primary insomnia (PI) involves difficulty initiating and/or maintaining sleep, or suffering from nonrestorative sleep, for at least one month. It causes clinically significant distress or impairment in social, occupational, or other important areas of functioning. It excludes secondary insomnia caused by other types of sleep disorders, mental disorders, somatic diseases, alcohol abuse, medication, or general medical conditions.[1]
Cognition is one of the many kinds of psychological activities of human beings, which includes attention, execution and memory. Memory, as a psychological activity, consists of a series of process such as memorizing, maintaining information, recognition and recall. Memory function is mainly controlled by the frontal lobe and thalamus. Attention, a basic function of individual psychological activity, is the directivity and concentration towards a certain thing, which allows for the normal control of the psychological activities. Attention is a kind of psychological characteristic, similar to psychological processes such as sensation, perception, learning and memory, thinking, and association. Its basic characteristics are directivity and concentration.[2-3]
Previous studies[4-5] found that sleep contributed to the functional recovery of the central nervous system and the peripheral nervous system, and that getting enough rest was important for maintaining cognitive function. The test scores in patients with chronic primary insomnia were decreased in digit span, word fluency test, immediate memory, delayed recall, delayed recognition, and event based prospective memory test. Findley et al. performed comprehensive tests on cognitive functions, such as intelligence, attention, concentration, alertness, hand to eye coordination, complex problem solving ability, and immediate and short-term memory, in patients with Obstructive Sleep Apnea Hypopnea Syndrome (OSAHS), and found that the patients’ attention, concentration, ability to solve complex problems, and short-term memory were significantly impaired.[3]
In this paper, we explore the changes in cognitive function in patients with primary insomnia. Insomnia due to different factors could affect functioning in the cerebral cortex, resulting in cognitive impairment. Long-term insomnia can even lead to larger psychological problems.[6] Complaints of insomnia patients generally include low energy, lack of concentration, and poor memory. But these subjective feelings need to be further studied. The purpose of this study is to investigate cognitive functioning in patients with primary insomnia, to explore the relationship between the severity of insomnia and cognitive function, and factors that may influence the cognitive functioning of patients with PI.
2. Participants and methods
2.1 Participants
Inclusion criteria for the insomnia group: 1) aged 18-60 years old, male or female, 2) meeting DSM-IV criteria for primary insomnia, 3) PSQI score>7, 4) able to take the measurements and providing informed consent to participate in this study. Exclusion criteria: 1) having organic brain diseases or other major somatic diseases, which could cause cognitive impairment or inability to participate in this study, 2) in the prior month to this study, had taken medications/drugs that could affect brain cognitive function or reaction rate. (Not including medications for treatment of insomnia or taken as part of another clinical trial). 3) deemed unsuitable for participation in this study by their clinician.
The patient group under study consisted of outpatients from the sleep clinic of our hospital, including a total of 40 cases, (9 males and 31 females), with a mean (sd) age of 37.3 (9.1) years, mean (sd) length of education 10.8 (3.5) years, and mean (sd) PSQI score of 14.7(3.5).
Inclusion criteria for the control group were the following: 1) aged 18 to 60 years old, male or female, 2) good mental status, no self reported sleep disorder, 3) PSQI scale score<8, 4) able to take the measurements and providing informed consent to participate in this study. Exclusion criteria were the following: having organic brain disease or other major somatic disease, which could cause cognitive impairment or inability to cooperate with this study. A total of 48 cases were included in the control group, with 13 males and 35 females, mean (sd) age of 39.8(10.0) years, mean (sd) length of education 9.3(4.5) years, and mean (sd) PSQI score of 3.1(1.7). There were no significant differences in the mean age, gender, or years of education between the patient group and the control group. All subjects provided written informed consent to participate in this study. In order to further study the effects of age on cognitive impairment in primary insomnia, we divided participants into two groups: 18-44 years old as one group (62 cases, 30 cases in the control group, 32 cases in the insomnia group), and 45-60 years old as the second group (26 cases, 18 cases in the control group, 8 cases in the insomnia group).
2.2 Methods
2.2.1 Cognitive function rating scale
1) Episodic memory test consists of immediate memory, delayed recall and long delay recognition.
Immediate memory test: participants read out a set of object-related words at a moderate speed and finished in about a minute. Immediately afterwards participant would recall and say these words in two minutes. It was noted how many words were remembered by the participant. This processs was repeated with three word sets and relevant data was documented. Delayed recall test: After 5 minutes, participants would recall, without prompt, the set of words given previously, and the number of words remembered, inserted or repeated was recorded.
Delayed recognition: after about 20 minutes (with intermediate time for other tests), participants were given words, including those previously given and similar ones. Participants were to decide which words had been given and read already. Afterwards a score was calculated based on the number of recognized words minus words given mistakenly.
2) MoCA (Xiehe version) test includes visuospatial and executive function, naming, memory, attention, language, abstraction, delayed recall, and orientation, among which memory is not rated. MoCA (Xiehe version) test has a sensitivity of 0.93, specificity of 0.87, test-retest reliability coefficient of 0.92, and internal consistency Cronbach coefficient of 0.86.[7]
2.2.2 Insomnia Rating Scale
Pittsburgh Sleep Quality Index (PSQI) is mainly used to test the severity of insomnia. It includes 7 dimensions, (i.e. subjective sleep quality, sleep latency, length duration, habitual sleep efficiency, sleep disturbance, use of sleep medications, and daytime dysfunction), with a total score of 21 points. A PSQI total score less than or equal to 7 points indicates normal sleep, and a PSQI total score greater than 7 points may be determined as sleep disorder. The higher the score, the worse the sleep quality, and the more severe the insomnia.[8,9] Meanwhile, based on the study by Ma et al. [10], study subjects with a score of >7 were divided into two groups: mild insomnia group with scores of 8-14, and severe insomnia group with scores of 15-21.
2.3 Statistical methods
SPSS 17.0 software package was used for the statistical analysis of all data. Descriptive analysis with mean (standard deviation) was used for basic variables including age, education years, and the scores on PSQI, Hamilton Depression Scale (HAMD), and Hamilton Anxiety Scale (HAMA). Independent sample t-test was used for the comparison of cognitive function between the insomnia group and control group, and for the study of the effect of age on cognitive impairment in those with primary insomnia. One-Way ANOVA Tukey test was used to explore whether cognitive function had changed at different severeity levels for insomnia. Pearson linear correlation analysis was used for the analysis of relevant factors that affected cognitive function. Statistical significance was set as α=0.05.
3. Results
3.1 Demographic variables and clinical characteristics
After analyzing the demographic variables and clinical characteristics of the patient group and control group, it was found that there was no significant difference in gender, age, or years of education. (p=0.324, 0.230, 0.150).
However, the mean (sd) PSQI scores of the two groups were 3.1 (1.7) and 14.7 (3.5) respectively, with statistical value being 495.80. The mean (sd) HAMD scores of the two groups were 3.2 (2.9) and 14.8 (5.6) respectively, with statistical value being 155.53. The mean (sd) HAMA scores of the two groups were 3.3 (2.4) and 13.9 (4.4), respectively, with statistical value being 207.31. These three sets of scores had statistically significant differences. (see table 1)
Table 1.
Demographic and clinical characteristics of insomnia and comparison groups
| Item | Control n=48 | Insomnia n=40 | Statistical value (χ2/F) | P value |
|---|---|---|---|---|
| Gender(male/female) | 13/35 | 9/31 | 3.69 | 0.324 |
| mean(sd) age in years | 39.8(9.9) | 37.3(9.1) | 1.54 | 0.230 |
| mean(sd) years of education | 9.3(4.5) | 10.8(3.5) | 2.91 | 0.150 |
| mean(sd) PSQIa score | 3.1(1.7) | 14.7(3.5) | 495.80 | <0.001 |
| mean(sd) HAMDb score | 3.2(2.9) | 14.8(5.6) | 155.53 | <0.001 |
| mean(sd) HAMAc score | 3.3(2.4) | 13.9(4.4) | 207.31 | <0.001 |
a(PSQI) Pittsburg Sleep Quality Index;
b (HAMD) Hamilton Depression rating scale;
c (HAMA) Hamilton Anxiety rating scale
3.2 Results of the Montreal cognitive assessment test and episodic memory test
MoCA test results of the control group and insomnia group showed that the mean (sd) scores in naming for the control group and the insomnia group were 2.9 (0.2) and 2.6 (0.6) respectively, with a statistically significant difference. The mean (sd) scores of delayed recall were 3.0 (1.5) and 1.8 (1.4) respectively, with a statistically significant difference. There was no significant difference between the two groups in spatial and executive function, attention, language, abstraction, or orientation. However, there was a significant difference between the two groups in the MoCA total score, as shown in Table 2.
Table 2.
Comparison of MoCA test results between insomnia and comparison groups (mean [sd])
| Item | Control | Insomnia | t value | p value |
|---|---|---|---|---|
| Visuospatial and executive function | 4.2(1.0) | 4.0(1.1) | 1.23 | 0.221 |
| Naming | 2.9(0.2) | 2.6(0.6) | 2.97 | 0.005 |
| Attention | 5.5(0.9) | 5.4 (0.8) | 0.14 | 0.891 |
| Language | 2.4(0.85) | 2.1(0.8) | 1.81 | 0.073 |
| Abstraction | 1.3(0.7) | 1.2(0.7) | 1.07 | 0.288 |
| Delayed recall | 3.0(1.5) | 1.8(1.4) | 4.05 | 0.001 |
| Orientation | 6.0(0.0) | 6.0(0.2) | 1.00 | 0.323 |
| Total score | 26.0(3.3) | 23.6(2.9) | 3.58 | 0.001 |
The results of episodic memory test were the following: the mean (sd) immediate memory score of the control group was 28.0 (5.2), and that of the insomnia group was 24.0 (6.0). The difference was statistically significant (t=3.33, p=0.001). The mean (sd) scores of delayed recall were 11.6 (2.7) and 7.9 (3.1) for the control group and the insomnia group respectively, with a statistically significant difference (t=6.05, p=0.001). However, the mean (sd) scores of delayed recognition were 13.1 (1.9) and 12.7 (2.2) for the control group and the insomnia group respectively, without a statistically significant difference (t=1.01, p=0.315), as shown in table 3.
Table 3.
Comparison of the episodic memory test results between insomnia and comparison groups
| Item | comparison group | Insomnia group | t value | p value |
|---|---|---|---|---|
| Immediate memory | ||||
| words correctly remembered in 3 repeats (mean[sd]) | 28.0(5.2) | 24.0(6.0) | 3.32 | 0.001 |
| Delayed recall | ||||
| words correctly remembered (mean[sd]) | 11.6(2.7) | 7.9(3.1) | 6.05 | 0.001 |
| Long delayed recognition Score (mean[sd]) | 13.1(1.9) | 12.7(2.2) | 1.01 | 0.315 |
3.3 Effects of severity of insomnia on the dimensions of the MoCA scale and episodic memory
Overall, the control group, mild insomnia group, and severe insomnia group had statistically significant differences in the four aspects of the MoCA scale: naming (F=7.56, p=0.001), language (F=3.22, p=0.045), delayed recall (F=9.17, p=0.001), and total score (F=6.72, p=0.002). Further pairwise comparisons showed that the severe insomnia group had lower scores than the control group in each of the four aspects, (i.e. naming, language, delayed recall, and total score) all with statistically significant differences. However there was no statistically significant difference in the score of each dimension, between the control group and the mild insomnia group, and between the mild insomnia group and the severe insomnia group, as shown in Table 4.
Table 4.
Variance analysis of dimensions of MoCA scale with degree of insomnia
| Item | Insomnia | p1 | p2 | p3 | Comparison results | ||
|---|---|---|---|---|---|---|---|
| Control ① | Mild ② | Severe ③ | |||||
| Visuospatial and executive function | 4.2(1.0) | 4.2(1.0) | 3.8(1.1) | 0.990 | 0.228 | 0.480 | |
| Naming | 2.9 (0.2) | 2.8(0.4) | 2.5(0.7) | 0.603 | 0.001 | 0.086 | ①, ②>③ |
| Attention | 5.5(0.9) | 5.4(0.9) | 5.5(0.8) | 0.965 | 1.000 | 0.972 | |
| Language | 2.4(0.8) | 2.3(0.7) | 1.9(0.8) | 0.981 | 0.040 | 0.193 | ①, ②>③ |
| Abstraction | 1.3 (0.7) | 1.2(0.8) | 1.1(0.7) | 0.817 | 0.548 | 0.960 | |
| Delayed recall | 3.0 (1.5) | 2.1(1.5) | 1.5(1.4) | 0.090 | <0.001 | 0.384 | ①, ②>③ |
| Orientation | 6.0(0.0) | 6.0(0.0) | 6.0(0.2) | 1.000 | 0.264 | 0.447 | |
| Total score | 26.0(3.3) | 24.6(2.4) | 22.958(3.1) | 0.245 | 0.001 | 0.256 | ①, ②>③ |
Note: p1 represents ①vs②, p2 represents ①vs③, and p3 represents ②vs③. Pairwise comparison uses One-Way ANOVA analysis with Tukey test.
With regard to the episodic memory scale, there were significant differences in the delayed memory (F=8.41, p=0.001) and delayed recall (F=22.67, p=0.001) scores among the control group, mild insomnia group and severe insomnia group. Further pairwise comparison suggested that the control group and mild insomnia group had higher immediate memory scores than the severe insomnia group, with a statistically significant difference. The mean (sd) scores of three groups were 28.0 (5.2), 26.4 (6.2), and 22.4 (5.4) respectively. With regard to the delayed recall score, the relationship of the scores of the three groups was: control group 11.6 (2.7) > mild insomnia group 9.3 (2.4) > severe insomnia group 7.0 (3.2), with a statistically significant difference. (see table 5)
Table 5.
Variance analysis of scores of the episodic memory scale with degree of insomnia
| Item | Insomnia | p1 | p2 | p3 | Comparison results | ||
|---|---|---|---|---|---|---|---|
| Control ① | Mild ② | Severe ③ | |||||
| Immediate memory | 28.0(5.2) | 26.4(6.2) | 22.4(5.4) | 0.575 | <0.001 | 0.064 | ①,②>③ |
| Delayed recall | 11.6(2.7) | 9.3(2.4) | 7.0(3.2) | 0.012 | <0.001 | 0.034 | ①>②>③ |
| Delayed recognition | 13.1(1.9) | 12.8(2.4) | 12.6(2.0) | 0.835 | 0.583 | 0.964 | |
Note: p1 represents ①vs②, p2 represents ①vs③, and p3 represents ②vs③. Pairwise comparison uses One-Way ANOVA analysis with Tukey test.
3.4 Analysis of influencing factors of cognitive function in patients with insomnia
Correlation analysis of plausible influencing factors, including age, education level, and emotional state, of cognitive and memory functions in patients with insomnia suggested that age was negatively correlated with MoCA total score (r=-0.330, p=0.043), and with immediate memory (r=-0.374, p=0.028), delayed recall (r=-0.340, p=0.032), and delayed recognition (r=-0.383, p=0.015) measured using episodic memory scale. Education level was positively correlated with visuospatial and executive function (r=0.564, p<0.001), naming (r=0.329, p=0.038), attention (r=0.338, p=0.033), language (r=0.603, p<0.001), abstraction (r=0.661, p<0.001), and total score (r=0.746, p<0.001) of the MoCA scale. There was a significantly negative correlation between naming and HAMA score (r=-0.330, p=0.037). No significant linear correlation was found among the remaining items. The analysis results are shown in Table 6.
Table 6.
Correlation between influencing factors and cognitive test indicators
| Item | Age | Education level | HAMD | HAMA | ||||
|---|---|---|---|---|---|---|---|---|
| r value | p value | r value | p value | r value | p value | r value | p value | |
| MoCA scale | ||||||||
| Visuospatial and executive function | -0.238 | 0.138 | 0.564 | <0.001 | -0.171 | 0.293 | -0.186 | 0.252 |
| Naming | -0.081 | 0.621 | 0.329 | 0.038 | -0.136 | 0.404 | -0.330 | 0.137 |
| Attention | -0.022 | 0.895 | 0.338 | 0.033 | -0.149 | 0.358 | 0.014 | 0.934 |
| Language | -0.280 | 0.080 | 0.603 | <0.001 | 0.055 | 0.738 | 0.240 | 0.135 |
| Abstraction | -0.152 | 0.348 | 0.661 | <0.001 | 0.000 | 0.998 | 0.195 | 0.227 |
| Delayed recall | -0.278 | 0.083 | 0.218 | 0.177 | 0.097 | 0.552 | 0.172 | 0.289 |
| Orientation | 0.005 | 0.976 | 0.127 | 0.434 | 0.024 | 0.884 | 0.107 | 0.511 |
| Total score | -0.330 | 0.043 | 0.746 | <0.001 | -0.070 | 0.666 | 0.053 | 0.745 |
| Episodic memory scale | ||||||||
| Immediate memory | -0.347 | 0.028 | 0.307 | 0.054 | -0.070 | 0.669 | 0.026 | 0.872 |
| Delayed recall | -0.340 | 0.032 | 0.268 | 0.095 | -0.109 | 0.504 | -0.100 | 0.950 |
| Delayed recognition | -0.383 | 0.015 | 0.199 | 0.219 | -0.094 | 0.563 | -0.047 | 0.773 |
3.5 Comparison of cognitive functions between control groups and patient groups belonging to different age groups
Comparison of subjects of different age groups suggested that in the age group of 18-44 years old, the mean (sd) scores of the insomnia group were lower than those of the control group in: naming 2.6 (0.6) vs. 2.9 (0.2), language 2.1(0.7) vs. 2.6(0.6), delayed recall of the MoCA 1.7 (1.3) vs. (1.4), MoCA total score 23.7(3.0) vs. 26.9(3.1), immediate memory 24.2 (5.8) vs. 28.9 (5.9) and delayed recall 8.0 (2.9) vs. 11.6 (3.0) of the episodic memory scale, with statistically significant differences (t=2.23, p=0.031; t=2.70, p=0.009; t=3.89, p<0.001; t=3.52, p=0.001; t=3.10, p=0.003; t=4.70 p<0.001). While in the age group of 45-60 years old, the insomnia group only had lower mean (sd) score than the control group in the delayed recall section of the episodic memory scale, with a statistically significant difference 7.2(3.7) vs 11.6(2.1) (t=3.81, p=0.001). Detailed results are shown in Table 7.
Table 7.
Comparison of cognitive functions between insomnia and comparison age groups
| Age group 18-44 years | Age group 45-60 years | |||||||
|---|---|---|---|---|---|---|---|---|
| Control | Insomnia | t value | p value | Control | Insomnia | t value | p value | |
| MoCA scale | ||||||||
| Visuospatial and executive function | 4.3(1.1) | 4.0(1.1) | 0.96 | 0.342 | 4.1(0.9) | 3.6(1.0) | 1.20 | 0.240 |
| Naming | 2.9(0.3) | 2.7(0.7) | 2.23 | 0.031 | 2.9(0.2) | 2.5(0.5) | 2.26 | 0.053 |
| Attention | 5.7(0.6) | 5.5(0.8) | 0.75 | 0.459 | 5.2(1.2) | 5.2(0.8) | -0.06 | 0.953 |
| Language | 2.6(0.6) | 2.1(0.8) | 2.70 | 0.009 | 1.9(0.9) | 1.7(0.8) | 0.52 | 0.606 |
| Abstraction | 1.2(0.7) | 1.1(0.7) | 0.58 | 0.566 | 1.3(0.6) | 1.1(0.6) | 1.01 | 0.325 |
| Delayed recall | 3.1(1.4) | 1.7(1.3) | 3.89 | 0.000 | 2.8(1.6) | 1.7(1.7) | 1.54 | 0.137 |
| Orientation | 6.0(0.0) | 5.9(0.1) | 1.00 | 0.325 | 6.0(0.0) | 6.0(0.0) | - | - |
| Total score | 26.5(3.1) | 23.7(3.0) | 3.52 | <0.001 | 25.1(3.6) | 22.8(2.4) | 1.63 | 0.115 |
| Episodic memory scale | ||||||||
| Immediate memory | 28.9(5.9) | 24.2(5.8) | 3.10 | 0.003 | 26.3(3.0) | 23.0(6.7) | 1.37 | 0.207 |
| Delayed recall | 11.6(3.0) | 8.0(2.9) | 4.70 | 0.000 | 11.6(2.1) | 7.2(3.7) | 3.81 | 0.001 |
| Delayed recognition | 13.0(2.1) | 12.8(2.0) | 0.23 | 0.816 | 13.2(1.2) | 11.7(1.5) | 1.58 | 0.149 |
4 Discussion
4.1 Main findings
4.1.1 Cognitive function changes in patients with insomnia
Contemporary neuroimaging studies have found decreased blood flow during the daytime in the prefrontal cortex of patients with chronic insomnia, a phenomena that could cause impairment to executive functions, such as abnormal functional connectivity between prefrontal cortex and hippocampus in PI patients. However, neuropsychological evidence is still insufficient regarding whether PI patients and chronic insomnia patients have executive function impairment.[11-12] Chen and Lan[13] found that chronic primary insomnia affected cognitive functions, using Wechsler Memory Test and Wisconsin Card Sorting Test (WCST) for the neuropsychological study of chronic primary insomnia patients. We found that there were significant differences in the immediate memory and in delayed recall between the insomnia group and the control group (p<0.01), as shown in Table 2. These suggest that the memory function in patients with primary insomnia may undergo great changes. Meanwhile, based on the MoCA scale, we could determine an individuals’ visuospatial and executive function, naming, attention, language, abstraction, delayed recall, and orientation. The results showed that patients with insomnia had differences in naming and delayed recall, and no obvious difference in other aspects. This suggests that insomnia could change an individual’s cognitive function to some extent.
4.1.2 Relationship between insomnia and impaired cognitive functions
Through the comparison of each indices of cognitive functioning between insomnia patients and healthy subjects, we found that the cognitive functions of insomnia patients were partially impaired, and that the degree of insomnia was plausibly associated with their cognitive functions. In order to further determine the difference of cognitive functions among different groups, the subjects were divided into three groups according to PSQI score, i.e., the control group, mild insomnia group (PSQT 8-14 points), and severe insomnia group (PSQI 15-21 points). Variance analysis was used for cognitive functions of subjects with different degrees of insomnia.
There were differences among the three groups in naming, language, and delayed recall in the MoCA scale, all of which were statistically significant. However the multiple-comparisons among these three groups (i.e. normal group and mild insomnia group, mild insomnia group and severe insomnia group) were not statistically significant. The control group and severe insomnia group were significantly different in the naming, language, delayed recall, and total score. These results showed that the extent and degree of cognitive impairment in patients with different degrees of insomnia were different.
In the episodic memory scale, immediate memory and delayed recall were significantly different among the three groups. Through pairwise comparison we also found that there was a significant difference in immediate memory between the normal control group and the severe insomnia group. There were significant differences in delayed recall between the normal group and the mild insomnia group, between the mild insomnia group and the severe insomnia group, and between the normal group and the severe insomnia group, respectively. These results showed that there was a substantial change in immediate memory and delayed recall in insomnia patients, and that the more severe the insomnia, the more obvious the impairment to memory functions.
4.1.3 Plausible factors affecting the cognitive functions of patients with insomnia
After analysis, we found that, in insomnia patients, age was correlated with episodic memory functions such as immediate memory, delayed recall, and delayed recognition, and with the total score on the MoCA, which suggests that age could be one of the causes of cognitive function impairment in patients with insomnia. In this experiment, the control group and insomnia group were divided into groups of those 18 to 44 years old and 45 to 60 years old. The results showed that after narrowing the age range, there were more indices with statistical differences. In the 18 to 44 years age group, the insomnia group had lower scores than the control group in naming, language, delayed recall and total score on the MoCA, and immediate memory and delayed recall of episodic memory. While in the 45 to 60 year old age group, there was only a statistically significant difference in delayed recall of episodic memory between the control group and the insomnia group, further suggesting that PI’s influence on cognitive functions was primarily due to the disease itself, rather than the age factor.
Meanwhile, we found that years of education was also significantly correlated with visuospatial and executive functioning, naming, attention, language, and abstraction on the MoCA scale, suggesting that education was an important factor affecting cognitive functions. Education may change our perception to some extent. However, there were no statistically significant correlations between HAMD, HAMA scores and cognitive sub-factors, indicating that the emotion was not the main factor influencing cognitive factors.
4.2 Limitations
This study has the following limitations:
1) Limited number of assessment scales for the evaluation of cognitive functions. This study only used the MoCA and the episodic memory scale to assess the cognitive status of participants. However, internationally there are many different cognitive function assessment scales emphasizing different aspects. Therefore, future work could use more scales to evaluate the cognitive functioning of participants more comprehensively.
2) A long history of chronic insomnia could be a major factor affecting cognitive functioning. In this study, illness duration was not divided into categories for comparative evaluation.
4.3 Implications
The results of this study indicate that PI could affect patients’ cognitive functions, mainly manifesting in naming, language, delayed recall, and immediate memory. PSQI scores were significantly lower in the 8-14 group compared to the 15-21 group, indicating that there was a plausible correlation between severity of sleep disorders and degree of cognitive impairment. However, for PI patients, age was in general negatively correlated with episodic memory, and education was positively correlated with visuospatial and executive function, naming, attention, language, and abstraction. With regard to depression and anxiety represented by the HAMD and HAMA scales, there was no significant correlation, except for the negative correlation between HAMD and naming.
Figure 1.
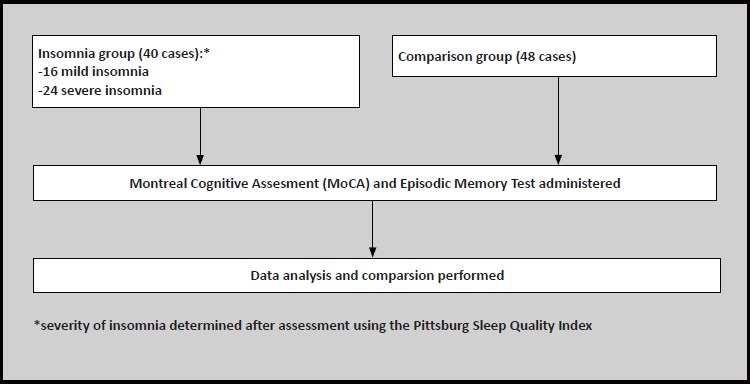
Flowchart of the study
Biography

Hui Guo graduated with a bachelor‘s degree from the Yangtze University School of Medicine in 2002. Since 2004, she has been working at the 7th People‘s Hospital in Wenzhou as deputy chief psychiatrist in the Department of Clinical Psychology, mainly engaged in clinical psychology and research work. Her achievements in clinical psychology and related fields include: participating in and presiding over more than twelve national, provincial, and municipal scientific research projects. She is the recepient of the Excellent Paper Award from the Chinese Association of Rehabilitation Medicine, Excellent Paper Award of The Ninth National Conference on Psychiatry, Wenzhou Science and Technology Progress Award, and has published fifteen academic papers.
Footnotes
Funding statement
Wenzhou social development and scientific research 2017Y0525
Informed consent
All participants provided written informed consent to participate in this study.
Conflict of interest statement
Authors declare no conflict of interest related to this manuscript.
Ethical approval
This study was approved by the Ethics Committee of the Wenzhou 7th People’s Hospital
Authors’ contributions
Hui Guo: completed the scale assessment, data collection, and article writing. Meijie Wei: completed the statistical analysis. Wantao Ding: provided study design, guidance, and article editing
References
- 1.Chen ML. [Study on Cognitive Function and Quality of Life in Patients with Primary Insomnia]. Suzhou: Suzhou University; 2015. p: 3-11. Chinese [Google Scholar]
- 2.Xu JT. [Effects of sleep on cognitive function]. Shen Jing Ji Bing Yu Jing Shen Wei Sheng. 2015; 15(4): 325-327. Chinese. doi: http://dx.chinadoi.cn/10.3969/j.issn.1009-6574.2015.04.001 [Google Scholar]
- 3.J Perrier, Chavoix C, Bocca ML. Functioning of the three attentional networks and vigilance in primary insomnia. Sleep Med. 2015; 16(12): 1569-1575. doi: http://dx.doi.org/10.1016/j.sleep.2015.06.025 [DOI] [PubMed] [Google Scholar]
- 4.Shekleton JA, Flynn-Evans EE, Miller B, Epstein LJ, Kirsch D, Brogna LA, et al. Neurobehavioral performance impairment in insomnia: relationships with self-reported sleep and daytime functioning. Sleep. 2014; 37(1): 107-116. doi:http://dx.doi.org/10.5665/sleep.3318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sutton EL. Psychiatric disorders and sleep issues. Med Clin North Am. 2014; 98(5):1124–1143. doi: http://dx.doi.org/10.1016/j.mcna.2014.06.009 [DOI] [PubMed] [Google Scholar]
- 6.Riemann D, Nissen C, Palagini L, Otte A, Perlis ML, Spiegelhalder K. The neurobiology, investigation, and treatment of chronic insomnia. Lancet Neurol. 2015; 14(5): 547-558. doi: http://dx.doi.org/10.1016/S1474-4422(15)00021-6 [DOI] [PubMed] [Google Scholar]
- 7.Wang QB, Shen Y. [The effect of Taijiquan Exercise on cognitive function in the elderly with mild cognitive impairment]. Zhongguo Kang Fu Li Lun Yu Shi Jian. 2016; 22(6): 645-649. Chinese. doi: 10.3969/j.issn.1006-9771.2016.06.005 [Google Scholar]
- 8.Littner M, Hirshkowitz M, Kramer M, Kapen S, Anderson WM, Bailey D, et al. Practice parameters for using polysomnography to evaluate insomnia: An update. Sleep. 2003; 26(6): 754-760 [DOI] [PubMed] [Google Scholar]
- 9.Roth T, Roehrs T, Pies R. Insomnia: Pathophysiology and implications for treatment. Sleep Med Rev. 2007; 11(1): 71-79. doi: http://dx.doi.org/10.1016/j.smrv.2006.06.002 [DOI] [PubMed] [Google Scholar]
- 10.Ma XL, He JC. [Neuropsychological Study of the Patients with Chronic Primary Insomnia]. Kunming: Ninth National Symposium on Neural Psychology and Behavior; 2014. p: 46-47. Chinese [Google Scholar]
- 11.Drummond SP, Walker M, Almklov E, Campos M, Anderson DE, Straus LD. Neural correlates of working memory performance in primary insomnia. Sleep. 2013; 36(9): 1307-1316. doi: http://dx.doi.org/10.5665/sleep.2952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huang Z, Liang P, Jia X, Zhan S, Li N, Ding Y, et al. Abnormal amygdala connectivity in patients with primary insomnia: Evidence from resting state fMRI. Eur J Radiol. 2012; 81(6): 1288-1295. doi: http://dx.doi.org/10.1016/j.ejrad.2011.03.029 [DOI] [PubMed] [Google Scholar]
- 13.Chen ML, Lan GH. [Study on cognitive function in patients with primary insomnia]. Lin Chuang Jing Shen Yi Xue Za Zhi. 2014; 6: 387-389. Chinese [Google Scholar]


