Abstract
Introduction
Sepsis with Bacillus anthracis infection has a very high mortality rate despite appropriate antibiotic and supportive therapies. Over the past 15 years, recent outbreaks in the US and in Europe, coupled with anthrax's bioterrorism weapon potential, have stimulated efforts to develop adjunctive therapies to improve clinical outcomes. Since lethal toxin and edema toxin (LT and ET) make central contributions to the pathogenesis of B. anthracis, these have been major targets in this effort.
Areas covered
Here, the authors review different investigative biopharmaceuticals that have been recently identified for their therapeutic potential as inhibitors of LT or ET. Among these inhibitors are two antibody preparations that have been included in the Strategic National Stockpile (SNS) and several more that have reached Phase I testing. Presently, however, many of these candidate agents have only been studied in vitro and very few tested in bacteria-challenged models.
Expert opinion
Although a large number of drugs have been identified as potential therapeutic inhibitors of LT and ET, in most cases their testing has been limited. The use of the two SNS antibody therapies during a large-scale exposure to B. anthracis will be difficult. Further testing and development of agents with oral bioavailability and relatively long shelf lives should be a focus for future research.
Keywords: anthrax, Bacillus anthracis, lethal and edema toxins, toxin-directed agents, treatment
1. Introduction
The 2001 US outbreak of Bacillus anthracis (anthrax) infection from spore-contaminated letters and the potential for this bacterium to be used for bioterrorism has heightened awareness to prospective risks [1-5]. This awareness has been further escalated by several isolated cases in the US and Europe over the last decade and an outbreak of injection anthrax among heroin users in Europe beginning in 2009 [4,6-10]. Unfortunately, in these anthrax outbreaks the development of septic shock has been associated with a particularly poor prognosis despite patients receiving aggressive conventional therapy with antibiotics and intensive care support. All patients with shock during the US 2001 outbreak died [2,5,11]. A review of 27 confirmed cases of infection from the outbreak in injection drug users in the UK noted that the mortality rate among patients requiring vasopressor therapy was close to 80% and substantially higher than other types of septic shock [4,12,13]. These findings emphasize the need to identify adjunctive therapies, which can be used with conventional ones to improve outcomes.
B. anthracis produces two toxins, lethal toxin and edema toxin (LT and ET), strongly implicated in its associated shock and lethality and which are likely targets for adjunctive therapies [1,14-16]. Over the past 10 – 15 years, there has been considerable progress identifying agents with the potential to therapeutically inhibit LT and ET. Here, we first briefly discuss the structure, actions and cardiovascular effects of LT and ET. We then describe the steps required for toxin uptake by host cells and in that context, discuss agents which have been identified with the potential to serve as or be developed into adjunctive therapies for anthrax.
2. B. anthracis toxin structure, function and potential cardiovascular effects
LT and ET are binary toxins comprised of protective antigen (PA), a protein that mediates the uptake of the toxins' toxic moieties: lethal factor (LF) for LT and edema factor (EF) for ET [17,18]. LF is a zinc-dependent metalloprotease which inactivates MAPKK 1 – 4 and 6 and essential stress kinase pathways [19]. LF also activates the Nlrp-1 inflammasome in macrophages and dendritic cells, resulting in caspase-1 activation, IL-1 and IL-18 production, and cell death [20]. EF has potent calmodulin-dependent adenyl cyclase activity and rapidly increases intracellular cAMP levels [21].
Data in in vivo and in vitro models suggest that LT can disrupt endothelial barrier function and produce hypotension in part through the extravasation of fluid [1,2]. Some studies have also suggested that LT, but not ET, may have direct myocardial depressant effects, while others have not [22]. Other studies have suggested that ET also has a direct effect on reducing endothelial barrier function and can produce intravascular volume losses [1,2]. On the one hand, this would be consistent with ET's known ability to produce localized tissue edema when injected subcutaneously in animals. Notably though, endothelial impairment is not consistent with EF's recognized action of potent adenyl cyclase activity since much research has shown that increased intracellular cAMP levels have potential endothelial-protective effects [23,24]. Alternatively, ET may produce shock by causing direct arterial and venous relaxation and dilation, changes very consistent with its adenyl cyclase activity [22,25].
3. Toxin uptake during infection
During B. anthracis infection, PA protomers with a molecular weight (MW) of 83 (PA83) bind to host cells via one of two receptors, tumor endothelial marker 8 (TEM8) or capillary morphogenesis gene-2 (CMG2) (Figure 1) [17,18,26-28]. Both receptors express an extracellular von Willebrand factor A (vWA) domain that binds to PA83 and are present in a wide variety of tissues. CMG2 may have a greater role in infection due to its higher affinity for PA. A third possible toxin receptor with a vWA domain has been implicated in toxin uptake but its pathogenic contribution is unclear [29]. Following host cell binding, the PA83 protomer undergoes furin cleavage into an active 63 kDa monomer and inactive 20 kDa monomer (PA63 and PA20) [30]. The small monomers are released while the PA63 monomers oligomerize into heptamers or octamers, termed prepores, which localize to lipid raft regions of the cell membrane. The formation of the prepore oligomers results in their activation and ability to bind three to four LF or EF molecules and to undergo endocytosis. As the endosome is internalized, decreasing intravesicular pH stimulates prepore incorporation into the endosomal membrane where it forms a cation-selective channel [31-33]. This channel or pore connects the inside of the endosome to the cell's cytosol. The transformed PA63 oligomer then mediates translocation of LF and EF into the cytosol along a proton gradient facilitated by specific amino acids within the passageway. Once in the cytosol, LF and EF exert their individual effects. Categorization of potential toxin-directed agents for anthrax can be done in the context of the steps required for toxin uptake by cells [26,27,30,34].
Figure 1.
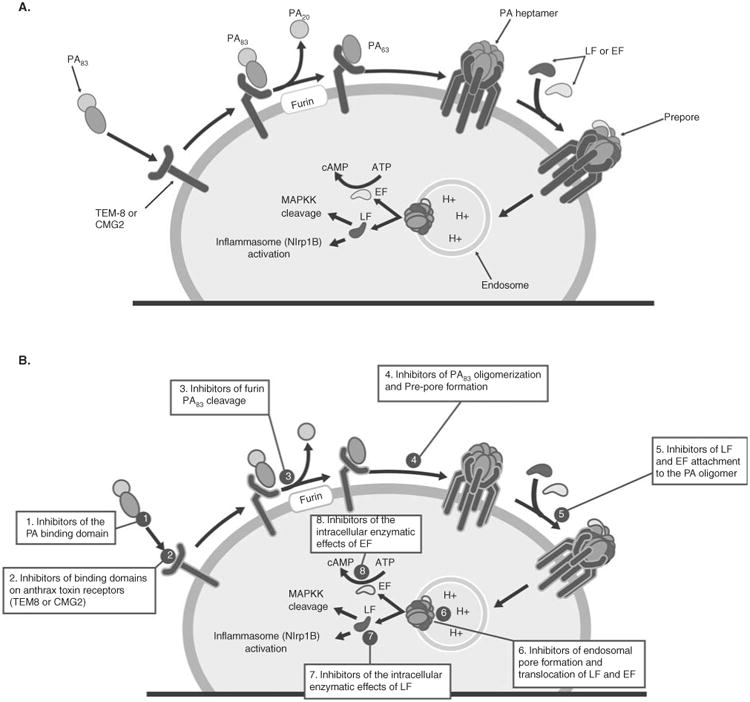
(A) Key events in the uptake of edema or lethal toxin by host cells as well as the potential effects of edema and lethal factor. During infection, circulating protective antigen (PA) protomer (PA83) binds to one of at least two host cellular receptors, termed anthrax toxin receptors (ATR), that are encoded by the tumor endothelial marker 8 (TEM8) gene or by the capillary morphogenesis gene 2 (CMG2), both of which are present on many tissues. The bound PA83 precursor molecule undergoes furin cleavage with release of an unbound subunit (PA20) and a retained bound subunit (PA63). Bound PA63 subunits then form either heptamers or octamers that one to three circulating lethal factor (LF) or edema factor (EF) proteins competitively bind to, forming the structure termed the prepore. This complex undergoes endocytosis, the prepore combines with the endosomal membrane and the toxic factors are then released into the cytoplasm. Edema factor has calmodulin-dependent adenyl cyclase activity and increases intracellular cAMP levels while LF inhibits mitogen-activated protein kinase 1 – 4, 6 and 7 and stimulates inflammasome formation. Based on the steps outlined in (A), (B) indicates where different categories of toxin-directed inhibitors have been designed to exert their effects. These categories, shown in the boxes in the figure and discussed in the text, include: inhibitors of the PA binding domain (1); inhibitors of binding domains on anthrax toxin receptors (TEM8 or CMG2) (2); inhibitors of furin PA83 cleavage (3); inhibitors of PA63 oligomerization and prepore formation (4); inhibitors of LF and EF attachment to the PA oligomer (5); inhibitors of endosomal pore formation and translocation of LF and EF (6); inhibitors of the intracellular enzymatic effects of LF (7); and inhibitors of the intracellular enzymatic effects of EF (8).
4. Toxin-directed therapies for the management of B. anthracis shock
When considering the potential of proposed agents, it is important to consider the degree to which their efficacy has been assessed. This assessment can be divided into several general stages. After a potential antitoxin agent has been identified, it is first determined whether it will protect against the cytotoxic effects of LT in a macrophage lysis assay, usually RAW264.7 or J774A.1 cells. For ET-directed agents, in vitro studies may test the agent's ability to inhibit cAMP production or a cAMP-mediated event. If effective in vitro, then the agent's effects are assessed in an LT (or sometimes ET)-challenged animal model, most frequently the highly sensitive Fisher 344 rat although other strains and species are sometimes used. If protective with an in vivo toxin challenge, then the agent is tested in vivo with a live B. anthracis challenge using either a fully virulent B. anthracis strain (e.g., Ames), or a less virulent one that still produces toxin (e.g., Sterne). Full in vivo assessment of the agent should include studies showing that it is effective when administered at some clinically relevant time point after B. anthracis challenge (e.g., 72 – 96 h after initiation of infection, upon detection of PA in the bloodstream or a rising temperature) and that it adds to the protective effects of antibiotics. Based on the animal rule, for FDA approval in the US, the agent has to have been tested in two relevant animal models [35]. For the only two antitoxin agents presently included in the Strategic National Stockpile (SNS, see below), this testing has included live B. anthracis challenge in ciprofloxacin- or levofloxacin-treated rabbit and cynomolgus monkey models. While a large number of potential anthrax toxin-directed agents have been identified, the degree to which their efficacy has been tested in relevant models varies considerably. Some agents which have shown particular promise in preclinical testing have undergone Phase I clinical testing (see below).
4.1 Inhibitors of the PA-binding domain
The majority of testing has been done with agents that directly inhibit PA binding. Anthrax Immune Globulin (AIG, Emergent Biosolutions, Winnipeg, Canada) is a polyclonal antibody derived from the plasma of humans previously vaccinated with Anthrax Vaccine Adsorbed [36,37] (AVA or BioTrax). It is presently one of only two adjunctive treatments for anthrax included in the SNS [38]. The vaccine employed (AVA) to generate AIG was produced by adsorbing filtered culture from an attenuated B. anthracis strain (V770-NP1-R) and which is comprised largely of PA. AIG improved survival in aerosolized B. anthracis (Ames)-challenged rabbits and cynomolgus monkeys when administered up to 24 h after challenge or upon detection of PA in blood [37] (close to 48 h). In spore-challenged rabbits, compared with levofloxacin treatment alone, AIG with levofloxacin administered at 96 h but not earlier (≤ 84 h) produced an increase in survival approaching significance (p = 0.13) [36]. Since the 2001 US outbreak, AIG is the only adjunctive therapy that has been used clinically for anthrax infection. It was administered to three isolated cases of inhalational disease and one GI case several days after each patient had presented [6-10] AIG accelerated declines in serum PA levels and reduced LF levels, and three patients survived [7,10]. In 27 confirmed cases of injection anthrax from the 2009 UK outbreak, 9 of 15 patients (60%) not receiving AIG survived compared with 7 of 12 (58.3%) that did. However, AIG patients may have been sicker than non-AIG ones [4].
The other adjunctive therapy now included in the SNS is raxibacumab (Abthrax, GlaxoSmithKline, Philadelphia, PA). Presently, it is the only agent that has received FDA approval. Raxibacumab is a humanized mAb that inhibits the PA-binding domain [39]. In rabbits and cynomolgus monkeys challenged with aerosolized B. anthracis (Ames strain), treatment with raxibacumab, either at initial detection of circulating PA or with an increase in body temperature, improved survival significantly [39]. Compared with antibiotic treatment alone in anthrax-challenged rabbits, post-exposure treatment with raxibacumab in combination with antibiotics increased survival in a trend approaching significance (p = 0.08) [40,41]. In LT-challenged canines, raxibacumab augmented the hemodynamic and survival benefits of standard hemodynamic support [42]. Finally, in a Phase I study in 438 subjects, raxibacumab was associated with only one serious adverse event and it was unclear whether this was a result of the therapy itself [39].
ETI-204 or Anthim (Elusys Therapeutics, Pine Brook, New Jersey, NJ) is a humanized, affinity-enhanced variation of a mouse mAb (14B7) [43]. In one study in rabbits challenged with aerosolized B. anthracis (Ames strain), compared with survival in controls (0 of 10 animals), survival was significantly increased with ETI-204 treatment 24 h (8 of 10 survived; p = 0.001 vs control) or 36 h (5 of 10; p = 0.04 vs control) but not 48 h (3 of 7; p = 0.42 vs control) after challenge. In another study in a similar rabbit model, compared with survival in non-treated control animals (0 of 4 animals), animals administered doxycycline when PA was first noted after bacteria challenge had increased survival (5 of 10 animals; reportedly p = 0.85 vs control) that was increased further when combined with ETI-204 (9 of 10; p = 0.005 vs control and p = 0.131 vs antibiotic alone) [44]. Three Phase I safety trials have reportedly been initiated with this agent [45]. IQNPA (IQ Corporation, Walnut, CA) directed against PA and an anti-LF mAb (IQNLF) are fully human mAbs (i.e., both Fab and Fc regions have been humanized) developed with hybridomas from lymphocytes isolated from individuals immunized with the UK licensed anthrax vaccine [46]. IQNPA pretreatment in A/J mice challenged with intraperitoneal (i.p.) B. anthracis (Sterne strain) provided 100% protection. W1-mAb is a chimpanzee/human chimeric mAb obtained from chimpanzees immunized with PA [47]. Post-treatment with W1-mAb increased survival significantly in Sprague-Dawley rats challenged with intravenous (i.v.) ET or LT and in C57BL/6J mice challenged with subcutaneous (s.c.) B. anthracis [48] (A35 strain). A recently reported mAb, PA6-Fab, constructed with the variable regions of a murine PA-directed mAb and constant region of human IgG was protective in LT-challenged J774A.1 macrophages and Fisher rats [49].
Non-antibody inhibitors of the PA-binding region have focused on soluble preparations of the two anthrax receptors, CMG2 and TEM8. Early studies suggested that a soluble form of CMG2 (sCMG2 or RD1) had greater potency than that of TEM8 (sATR/TEM8, sTEM8) in a cell culture system and in LT-challenged Fisher rats, this was protective with an antibody-resistant form of LT [50,51]. Other studies, however, suggested that sTEM8 and L56A, a PA-binding-affinity-elevated mutant of sTEM8, had better tissue penetration than sCMG2 and were as protective as sCMG2 in LT-challenged rats [52]. To increase the half-life of such receptor-based therapies, another group used plant technology to produce a fusion protein consisting of the extracellular domain of CMG2 and human IgG-Fc [53] (CMG2-Fc). CMG2-Fc was protective in RAW264.7 cells challenged with normal and PA antibody-resistant forms of LT. Post-exposure treatment with CMG-Fc protected Dutch belt (DB) rabbits challenged intranasally with B. anthracis (Ames strain). Another fusion protein employing the extracellular PA-binding VWA domain of TEM8 and CMG2 and IgG-Fc domain (VWA-Fc) was protective LT-challenged J774 cells [54]. In Fisher rats challenged with LT, compared with survival in controls (0%), survival with VWA-Fc treatment 1 h before or at the time of LT challenge increased survival (83%; p = 0.0051). VWA-Fc at the dose of 50 μg administered immediately before and 2 days after intratracheal (i.t.) B. anthracis (Sterne strain) challenge improved survival in DBA/2 mice (75% survival with VWA-Fc vs 0% survival with control, p < 0.05). No significant protection was observed with the lower dose of VWA-Fc (10 μg). Other studies have suggested though that sequestration of LF by another fusion protein (RDI-elIgG1) results in later release of the toxic moiety and loss of the fusion preparation's efficacy [55].
4.2 Inhibitors of binding domains on anthrax toxin receptors (TEM8 or CMG2)
Since therapies directed against epitopes on PA itself may be ineffective for B. anthracis strains which express mutant or deleted forms of the epitope, agents that directly block TEM8 and CMG2 have been identified. One group employed phage-display technology to identify 12- and 7-amino acid residues that combine with the TEM8- and CMG2-binding domains [56]. These residues were employed to construct polyvalent inhibitors which protected LT-challenged RAW264.7 cells. The most protective peptide improved survival in LT-challenged Fisher rats (6 of 6 animals survived with treatment vs 1 of 12 controls). Another group used a fluorescence resonance transfer (FRET) system to screen for compounds that interfered with PA–CMG2 or PA–TEM8 interactions [57,58]. With this technique, cisplatin inhibited both CMG2 and PA while tannic acid interacted with CMG2 alone and ebselen and thimersol inhibited PA and TEM8 interactions. Although this group did not test these agents with ET or LT, in prior experiments by another group, cisplatin was protective with LT challenge in vitro and in vivo [59]. Interestingly though, this latter study concluded that cisplatin's protective effects were related to inhibition of PA heptamer formation rather than to receptor inhibition. A recent study with interference RNA methodology showed that siRNAs to either CMG2 or TEM8 were protective in LT-challenged mouse and human macrophage assays and inhibited LT-induced MEK2 cleavage and ET-stimulated adenyl cyclase activity in human kidney cells [60].
4.3 Inhibitors of furin PA83 cleavage
One group isolated antibody-producing lymphocytes from an individual vaccinated against anthrax and then produced nine fully human mAbs with high specificity to PA [61]. Two of the mAbs (p6C01 and p6F01) neutralized LT in the RAW264.7 macrophage assay and protected A/J mice from LT challenge. Additional studies with one of these preparations (p6C01) showed that it blocked furin cleavage but not PA63 oligomerization. However, other studies by this same group have suggested that antibodies against the PA cleavage site were not as protective as ones against the binding site [62].
Non-antibody agents blocking furin cleavage have also been identified. Hexa-d-arginine (D6R), a poly-arginine, inhibited both LT-induced macrophage lysis and PA83 cleavage [63] D6R-protected Fisher rats and FVB and 129/SV mice from LT challenge. Lengthening and modifying the structure of such poly-arginines (D9R) increased their affinity for furin and potency in the LT macrophage lysis assay [64]. Combination of D6R with the LF inhibitor In-2-LF, a peptide hydroxamate, resulted in enhanced protection against LT in a macrophage lysis assay [65]. A peptide inhibitor (AO-RARRRKKRT), modeled from the active furin cleavage site of influenza A H5N1, inhibited both free and cell surface furin PA83 cleavage [66,67]. Post-treatment with this peptide inhibitor was protective in A/J mice challenged with i.p. B. anthracis (Sterne strain) both with and without ciprofloxacin treatment. Inter-α-inhibitor-p (IαIp) is a serine protease which inhibits several different proteases [68] (e.g., neutrophil, elastase and plasmin). IαIp blocked protein cleavage by recombinant furin and was protective in LT-challenged macrophages and BALB/c mice. In A/J mice receiving moxifloxacin post-treatment, IαIp treatment 1 h before or up to 24 h after i.p. B. anthracis (Sterne strain) challenge appeared protective [69]. Combination of the protease inhibitor eglin c with a peptidyl boronic acid inhibited cell surface processing of PA83 and macrophage lysis by LT [70]. Combination of this agent with chloroquine had additive effects in the macrophage lysis assay. Studies described below found that compounds targeting PA monomer oligomerization could also inhibit furin cleavage of PA [71].
4.4 Inhibitors of PA63 oligomerization and prepore formation
Monoclonal antibodies with high affinity for PA83 were developed from lymphocytes of an individual vaccinated with AVA and hybridoma technology and two, AVP-21D9 and AVP-22G12, were protective in LT-challenged macrophages and Fisher rats [72]. The inhibitory effects of the mAbs were related primarily to interference with PA63 heptamer formation and not PA83 binding to host receptors or toxic moiety binding to the oligomer complex [73]. In subsequent studies in rabbits challenged with intranasally instilled or aerosolized B. anthracis (Ames strain), AVP-21D9 was protective when administered at the time of challenge but not 24 – 36 h after challenge [74]. In other studies in Swiss-Webster mice and guinea pigs, AVP-21D9 and a subtherapeutic dose of ciprofloxacin administered post-exposure had synergistic protective effects [75]. Post-exposure treatment with AVP-21D9 based on rising body temperature or the presence of positive serum PA levels in B. anthracis (Ames strain) challenged New Zealand rabbits or cynomolgus monkeys increased survival [76]. In a Phase I clinical trial in 50 patients, AVP-21D9 was not associated with increased adverse events [76].
Another group employed a humanized mouse strain (HC2/KCo7) to develop mAbs against PA, which were then engineered into a human IgG expression vector and produced from transfected Chinese hamster ovary (CHO) cells [77]. The engineered mAb (mAb-1303) improved survival when administered either in two doses 1 h and up to 96 h after aerosolized B. anthracis (Ames strain) challenge in rabbits and in one dose at the time of a similar challenge in cynomolgus monkeys. In rabbits receiving aerosolized B. anthracis (Ames strain), 8 of 10 animals receiving mAb-1303 treatment 24 h after challenge survived and this effect was comparable to prophylactic treatment. However, in this study, only three of seven animals receiving treatment at 48 h survived. Functional studies suggested that mAb-1303 interfered with oligomer formation since it did not alter PA83 binding to host receptor or toxic moiety binding to oligomer. A Phase I clinical trial of mAb-1303 was suspended due to an adverse event but an additional Phase I study was reportedly underway [78,79].
One group employing the macrophage lysis assay to screen for toxin-directed agents identified cisplatin as a candidate [59]. In vitro studies suggested that cisplatin blocked oligomer formation and subsequent PA-mediated intracellular translocation of toxin. Cisplatin protected BALB/cJ mice and Fisher rats when co-administered with an LT challenge, but not when administered 2 h before or after LT challenge. Another group employed ICMPocketFinder to identify pockets in the PA monomer interface necessary for oligomerization and then screened the Chem-bridge library for compounds predicted to bind with these sites [71]. Four compounds [5180717(17), 5181401(01), 5181385(85) and 5117235(35)] were identified that targeted a pocket close to the furin-binding site, protected against LT in the macrophage lysis assay and inhibited PA oligomerization in vitro. Another group employed CAVEAT to identify molecular scaffolds that could be modified to interfere with the binding sites necessary for PA heptamer formation [80]. Several candidate compounds were constructed which had modest protective effects in a macrophage lysis assay. Neither the compounds identified from the Chembridge library or with the CAVEAT methodology were tested in vivo.
4.5 Inhibitors of LF and EF attachment to the PA oligomer
Therapies designed to block LF or EF attachment to the PA oligomer can target either PA or the individual toxic moieties. Domains I of LF and EF, which mediate PA binding for each moiety, have substantial homology.
One group developed human single-chain variable fragments (scFvs) (SS87, SS70, SS73 and A8) directed against the LF- and EF-binding domain on PA [81,82]. All these scFvs inhibited LT in the macrophage lysis assay although their potencies varied. Other investigators used phage display analysis to define peptides capable of binding to the PA heptamer [83]. This and subsequent studies identified several 12 (e.g., HTSTYWWLDGAP) and then a 6 amino acid (TYWWLD) sequence that bound to the PA heptamer [84-88]. Although individually these amino acids were weak ligands, combination of multiple copies on polymer backbones with the proper spacing and density resulted in polyvalent compounds with high affinity for the PA heptamer and which inhibited LT in vitro and in vivo.
Murine monoclonal antibodies (10G3, 2E7, 10D4, 10G4 and 13D10) to LF capable of interfering with LF binding to PA were first reported in 1990 [89]. These antibodies were identified by their ability to neutralize LT's activity in a J774A.1 macrophage assay, and two (mAb 2E7 and 10G3) protected LT-challenged Fisher rats. Subsequent studies by differing groups have demonstrated other murine mAbs generated against LF which have inhibited binding of LF to PA and were protective in the LT macrophage lysis assay or with LT challenge in vivo [90-92]. A high affinity scFv (2LF) generated against LF in macaques and described as humanlike inhibited LF binding to PA63 and was protective in the macrophage lysis assay and in LT-challenged Fisher rats [93]. One group combined antibody-producing lymphocytes from individuals vaccinated with the UK anthrax vaccine with a human–mouse heteromyeloma cell line (CB-F7) and developed mAb to LF (hLF1-SAN) [94]. This mAb bound to peptide regions 121 – 150 and 451 – 470 of LF and was protective in an LT neutralization assay and in LT-challenged mice. One previously developed murine mAb (LF8) that blocked LT formation was employed to construct a human–murine chimeric Fab mAb (LF8-Fab) using LF8 variable regions combined with human constant regions which was protective pre- and post-exposure in LT-challenged J774A.1 cells [90,95]. Finally, a human mAb against LF (IQNLF) developed as noted above was shown to bind to domain I of LF (i.e., the PA-binding domain) [46]. IQNLF inhibited LT in the macrophage lysis assay and was protective in A/J mice when administered 2.5 h prior to an i.p. B. anthracis (Sterne strain) challenge. A Phase I clinical trial of IQNLF had been planned [96] (omicsonline.org/2157-2526/2157-2526-S1.006-004.pdf).
Early studies also defined murine mAbs (7G10 and 9F5) against amino acids in the PA-binding region of EF, one of which (9F5) inhibited ET activity in a CHO cell elongation assay [97]. More recently, a murine mAb generated against LF (H10) was shown to interfere with the PA-binding regions on both LF and EF and the adenyl cyclase activity of ET and macrophage cytotoxicity of LT [98]. In BALB/c mice, H10 pretreatment was protective against either ET or LT challenge. Four murine mAbs (1D4, 3F2, 4A6 and 7F10) directed against the PA-binding region of EF all inhibited ET-induced cAMP release from RAW264.7 cells and footpad edema formation in BALB/c mice but these effects were greatest for 7F10 [99]. At the highest dose tested, mAbs 3F2, 4A6 and 7F10 were protective in ET-challenged C57BL/6J mice, while all four mAbs reduced leg edema following B. anthracis (Sterne strain) s.c. foreleg injection. However, in mice challenged with lethal bacteria, a combination of 7F10, 3F2 and 4Ag, while prolonging survival did not change the proportion of animals surviving significantly.
4.6 Inhibitors of endosomal pore formation and translocation of LF and EF
One group developed a mouse–human chimeric mAb (cAb29), which was protective as a pretreatment in LT-challenged rats and B. anthracis spore challenged guinea pigs and rabbits [100,101]. While cAb29 did not inhibit PA-receptor binding, furin cleavage of PA83, PA63 oligomerization or LF binding to the prepore, it did interfere with the flexible loop in Domain 2 (2β2 – 2β3; residues 302 – 325) of the PA complex necessary for insertion of the prepore into the endosomal membrane and delivery of LF and EF.
Several groups have shown that dominant-negative (DN) mutants of the PA63 monomer, which can be incorporated along with wild-type monomers during oligomerization, prevent prepore to pore transformation [102-105]. These mutants have targeted residues necessary for prepore insertion into the endosomal membrane (e.g., 2β2 – 2β3 of domain 2) or ones necessary for translocation of LF and EF (e.g., F427). Treatment with DN mutants was protective in the LT macrophage lysis assay and in LT-challenged Fisher rats and BALB/c [103,104].
Since acidification of the endosomal vesicle is necessary for prepore to pore transformation, agents inhibiting this acidification process have been investigated. One such agent, chloroquine, was shown to be protective in the LT macrophage lysis assay and in LT-challenged BALB/c mice and in LT lymphocyte suppression testing [106-109]. However, other work has suggested that the protective effects of chloroquine and related agents actually relate to their binding and blockade of the barrel required for LF and EF translocation [110]. One group used a lipid bilayer system to investigate the binding and inhibitory effects of a group of chloroquine-related heterocyclic fused azinium salts on PA63 channels [111]. Three agents, HA1568, HA1495 and HA1383, were protective in a J774A.1 macrophage lysis assay, although this was most notable for HA1568. Another group investigated 500 potential small-molecule inhibitors of LT using a high-throughput RAW 264.7 cell-based assay [112]. This screen identified amiodarone and bepridil, two cardiac anti-arrhythmic agents, which interfered with LTs cytotoxic effects in concentrations comparable to ones used clinically. Both agents exerted their effects by inhibiting endosomal acidification, while amiodarone was protective in LT-challenged Fisher rats. Using high-throughput analysis, another group identified three agents, niclosamide, diphillin and a novel chromeno[4,3-c]pyrazol-4 (iH)-one (NCG00084148-01), which were protective in the macrophage lysis assay [113]. At low concentrations these agents interfered with endosomal acidification either via inhibition of vacuolar (H+)-ATPase (V-ATPase) or blocking of trafficking to endosomes with increased acidity.
Employing a structure-based analysis to define compounds with ring structures capable of inhibiting the heptameric PA prepore ring, investigators identified a group of β-cyclodextrin-based compounds [114-118]. They then constructed a compound [per-6-(3-aminopropylthio)-β-cyclodextrin or AmPrβCD)] which was shown by X-ray crystallography to bind to the pore barrel lumen. AmPrβCD blocked conductance through prepore structures inserted into lipid bilayers and was protective in LT-challenged macrophages and Fisher rats. Post-treatment at 24 h with a similar agent (14b) in mice challenged with B. anthracis (Sterne strain) and treated with ciprofloxacin improved survival compared with antibiotic alone [119].
One group developed a recombinant fusion protein which combined the domain I of LF lacking its initial 27 amino acids, with the N-terminus of EF [120] (ΔLFn-EFn). This fusion protein was protective in a macrophage lysis assay and in LT-challenged Fisher rats. Further studies in CHO cells suggested that this fusion protein interfered with translocation of the toxic moieties.
4.7 Inhibitors of the intracellular enzymatic effects of LF
Several antibodies developed against LF appear to target its enzymatic actions. For the murine mAb LF8, originally shown by electromobility shift assay to interfere with LF binding to PA, subsequent epitope studies showed that it associated with domain III which is necessary for LF's enzymatic activity [91]. Similar binding to domain III has been shown for mAbs 10G3, 5B13B1 and 3C16C3 [89,92].
Types of small-molecule inhibitors of LF activity, both competitive and noncompetitive and each with numerous candidate agents, have been reported on and reviewed [121-123]. These inhibitors have included hydroxymates, zinc-metallo-proteases, amino-glycosides, quinolone urea derivatives, heterocyclic zinc chelators, drug structure scaffolds, hydrazones, several natural products (e.g., catechins), host defensins, compounds with polyphenol motifs and phenylfuran, phenylpyrazole and phenylpyrrole carboxylic derivatives [121]. Very few of these agents have been studied in in vivo models though, making their potential clinical application unclear. The ones that have been tested in animal models are discussed here.
Work by several groups demonstrated the potential effectiveness of peptide hydroxymates as competitive inhibitors of LF [124,125]. Subsequent work by investigators at Merck Research laboratories produced the hydroxamate (2R)-2-[(4-fluro-3-methylphenyl)sulfonylamino]-N-hydroxy-2-(tetrahydro-2H-pyran-4-yl) acetamide or LFI [126,127]. X-ray crystallography showed that LFI bound in the groove at the interface of LF domains III and IV, adjacent to the catalytic center. It inhibited LF protease activity and was protective in LT-challenged J774A.1 macrophages and BALB/c mice. In live bacteria challenge studies, LFI was protective as: i.v. pretreatment in BALB/c mice receiving i.p. B. anthracis (Sterne strain); s.c. pretreatment in DB rabbits receiving s.c. B. anthracis (Ames strain); s.c. post-treatment in DB rabbits receiving s.c. B. anthracis (Ames strain); and s.c. post-exposure treatment in DB rabbits receiving s.c. B. anthracis (Ames strain) and ciprofloxacin. However, animal numbers were relatively small in these experiments and levels of significance not provided.
Modification of the original structure proposed by Merck produced two small-molecule LF inhibitors, PT-8420 and PT-8541, that were investigated in an in vivo spore-challenged mouse model [128-131]. In one set of experiments, compared with C57BL/6J mice challenged with s.c. B. anthracis (Ames strain) and treated with a subtherapeutic dose of ciprofloxacin, post-treatment with either of the two LF inhibitors combined with ciprofloxacin increased survival significantly. In the same model but without antibiotics, PT-8541 and a mAb against ET had additive survival benefits.
Screening drug structure scaffolds, one group identified an initial compound (BI-MFM3) with a rhodanine ring and its modifications (BI-11B1, BI-11B2 and BI-11B3) that were LF specific and protective in LT-challenged RAW264.7 cells [132]. In DBA2 mice challenged with i.p. B. anthracis (Sterne strain) spores, compounds BI-11B1 or BI-11B3 in combination with ciprofloxacin administered 24 h after challenge increased proportional survival compared with ciprofloxacin treatment alone.
One group noted that the human neutrophil protein 1 (HNP-1), an α defensin, not only protected RAW264.7 macrophages from spore challenge, but also inhibited LF enzymatic activity and protected RAW264.7 macrophages and BALB/c mice from LT challenge [133]. Another group reported that the catechin (-) epigallocatechin-3-gallate (EGCG)-blocked LF enzymatic activity was protective in the RAW264.7 assay and reduced symptoms related to LT challenge in Fisher rats [134]. In studies examining the N-end rule in LT-mediated death, one group showed that bestatin protected LT-challenged RAW264.7 macrophages and BALB/c mice [135].
4.8 Inhibitors of the intracellular enzymatic effects of EF
Compared with LF, there has been much less work directed at EF inhibitors. A group at the NIH identified several chimpanzee mAbs against EF (EF12A, EF13D, EF14H and EF15A) from which Fabs were converted into full-length chimeric IgG molecules with γ1 heavy chain constant regions [99,136]. Although all four showed binding specificity for EF, only EF13D inhibited cAMP production in ET-challenged RAW264.7 cells. This mAb bound amino acids in close proximity to the calmodulin-binding site of EF and not only prevented calmodulin binding but also displaced it from EF. EF13D was protective in C57BL/6J mice when administered 1 h before i.v. ET challenge and 18 and 1 h before s.c. B. anthracis (Ames 35 strain) challenge. Another group developed a murine IgM mAb to EF (9F3) which produced dose-dependent decreases in EF-stimulated cAMP release from CHO cells and a weak survival benefit in A/JCr mice when used in combination with a subtherapeutic dose of a PA-mAb prior to i.v. B. anthracis (Sterne strain) challenge [137].
As recently reviewed, several potential nucleotide and non-nucleotide small-molecule EF inhibitors have been proposed based on differing search strategies [138]. While none of these have yet been reported to improve survival in in vivo anthrax models, they provide a basis for further investigation. Adefovir dipivoxil {9-[2-{{bis[(pivaloyloxy) phosphinyl]methoxy] ethyl]adenine;bis-POM- PMEA}, an antiviral drug used for the treatment of viral hepatitis, bound to the catalytic site in EF with an affinity four times higher than ATP [139].
Adefovir inhibited EF-mediated cAMP production in CHO cells and morphological changes in Y1 mouse adreno-cortical cells and reversed EF inhibition of macrophage TNF production. Adefovir inhibited EF-stimulated cAMP production and its cardiovascular effects in perfused heart and aortic ring models [22,25]. Other agents shown to have the potential to inhibit EF's enzymatic activity include 4-[4-(4-nitrophenyl)-thiazolylamino]-benzene-sulfonamide [140,141], 3-{(9-oxo-9H-fluorene-1-carbonyl)-amino]-benzoic acid [142,143], and (M)Ant nucleotides [144-149] and allosteric inhibitors [150].
5. Conclusion
B. anthracis infection continues to be a health threat in both developing and developed regions of the world. While antibiotic therapy and, in severe cases, aggressive cardiopulmonary support are the mainstays of treatment, developing adjunctive agents capable of mitigating the detrimental effects of LT and ET is important. Over the past 10 – 15 years, there has been considerable research in this regard. At present, two agents (AIG and raxibacumab) are undergoing or have completed FDA review or approval respectively and have actually been included in the SNS (Table 1). Four other agents (ETI-204, IQNPA, AVP-21D9 and MDX 1303) have reportedly undergone or are about to undergo Phase I testing (Table 1). While a large number of other toxin-directed agents have also shown promise in laboratory studies, their further development and approval for definitive clinical use should be a priority. Whether any of these agents under development for the treatment of B. anthracis infection demonstrate actions (e.g., inhibition of pore formation and cAMP formation) that might have applicability for other medical conditions is a potential secondary gain from this large research effort.
Table 1. Bacillus anthracis toxin-directed agents available for or close to clinical use.
| Agent designation | Description | Manufacturer | Stage of development |
|---|---|---|---|
| AIG [37] | pAb Inhibits PA binding domain |
Emergent Biosolutions | Undergoing FDA review Included in SNS |
| Raxibacumab (Abthrax) [39] | Humanized mAb Inhibits PA binding domain |
GlaxoSmithKline | FDA approved Included in SNS |
| ETI-204 (Anthium) [43] | Humanized mAb Inhibits PA binding domain |
Elusys Therapeutics | Reportedly completed Phase I testing Fast-track and orphan drug status by the FDA |
| IQNPA [45] | Human mAb Inhibits PA binding domain and LF |
IQ Corporation | Reportedly undergoing Phase I testing |
| AVP-21D9 [71,73-75] | Human mAb Interferes with oligomer formation |
Avanir Pharmaceuticals | Reportedly completed Phase I testing Published data available |
| MDX 1303 (Valortim) [76-78] | Human mAb Interferes with oligomer formation |
Emergent Biosolutions | Reportedly completed Phase I testing Fast-track and orphan drug status by the FDA |
AIG: Anthrax Immune Globulin; AVA: anthrax vaccine adsorbed; FDA: Food and Drug Administration; LF: Lethal factor; PA: Protective antigen; pAb: Polyclonal antibody; SNS: Strategic National Stockpile.
6. Expert opinion
Although antibiotic therapy alone is usually sufficient for the treatment of B. anthracis infection when systemic disease is not in question, for systemic disease, adjunctive therapy with toxin-directed agents is now recommended (38). Over the past 10 – 15 years, a large number of agents have been identified with the potential to inhibit LT and ET. The extent to which these agents have been developed and tested for possible clinical use though varies considerably. This work is certainly slowed by the need for laboratories operating at a sufficient biosafety level (i.e., 3 or 4) to provide later stage in vivo testing with relevant virulent B. anthracis strains as well as the need for compliance with the FDA animal rule. While antibody-based agents have received the most extensive testing to date, only two of these (AIG and raxibacumab) have been studied sufficiently to permit their inclusion in the US SNS or approval by the US FDA. Of concern, while each of these agents produced trends in improved survival when administered post-exposure and combined with antibiotics in virulent B. anthracis-challenged animal models, neither of these results actually reached significance. Furthermore, whether AIG has actually improved outcome when used clinically is unclear, especially when its application in the 2009 outbreak of anthrax of injection drug users in the UK is considered. The only other antitoxin agents that have reached Phase I clinical testing are also antibody based. Direct comparisons in relevant animal models of AIG and raxibacumab, as well as other antibody preparation possibly close to approval would be informative. Nevertheless, at present, AIG and raxibacumab are the only adjunctive agents available for use for anthrax.
Current antibody therapies require intravenous administration. These therapies, if effective, will be most useful for the treatment of either isolated cases or small outbreaks of anthrax infection. In the event of a large-scale exposure, as might occur during a bioterrorist event, rapid administration of an intravenous antibody to a large number of infected individuals, while possible, will be very difficult. In this regard, the ideal adjunctive agent would be one that was orally bioavailable and could be dispensed quickly along with an oral antibiotic. In this context, the large number of small-molecule agents that have been investigated are encouraging. Unfortunately, many of these agents target either the protease activity of furin, the metalloprotease activity of LF or the adenyl cyclase activity of EF. These enzymatic activities overlap with those of many host enzymes. Thus, defining small molecule inhibitors with sufficient selectivity to target the pathogenic enzymatic activities of LT and ET without effecting essential host cell function will be an obstacle but will hopefully be overcome with further research. Small molecule inhibitors targeting aspects of toxin uptake or action, which do not overlap with host cell functions, might provide the best targets for therapy.
Possibly one of the most promising groups of agents for use as adjunctive therapies are drugs already approved for clinical use for other conditions (e.g., chloroquine, adefovir or amiodarone) and which show convincing toxin inhibition. Once again, however, these agents would ideally be orally bioavailable ones with limited toxicity. Importantly though they would have to be shown to add significantly to the beneficial effects of standard support in relevant in vivo models. Since many potential agents in this category may offer little commercial value to pharmaceutical companies, whether the funding would be available to adequately test them without strong governmental support is unclear.
Article highlights.
Invasive forms of Bacillus anthracis infection have occurred over the past decade with concerning frequency in the developed world and have been associated with a high mortality rate despite conventional antibiotic and intensive care unit support. This bacterium's ability to be weaponized remains a worldwide bioterrorist threat.
Production of lethal toxin and edema toxin (LT and ET, respectively) is important to the pathogenesis of B. anthracis infection and toxin inhibitors may serve as beneficial adjunctive therapies for patients with infection.
The multistep process required for the uptake and subsequent activity of LT and ET in host cells has provided a framework for the development of a broad range of differing toxin-directed agent treatments.
Over the past 10 – 15 years, a large number of candidate antitoxin agents have been identified. However, the development and preclinical testing of the majority of these agents in relevant diseased animal models has been slow with only a few reaching Phase I clinical testing.
While two antibody preparations directed against the toxins and with the potential to serve as adjunctive therapies have been included in the Strategic National Stockpile (SNS), orally bioavailable agents that can be administered rapidly and to large numbers of recipients in the event of a large outbreak of infection are needed.
This box summarizes key points contained in the article.
Acknowledgments
The authors are employees of the National Institutes of Health and are supported by the Intramural Program of the NIH, via the Clinical Center, Critical Care Medicine Department.
Footnotes
Declaration of interest: The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
Bibliography
Papers of special note have been highlighted as either of interest (•) or of considerable interest (••) to readers.
- 1.Remy KE, Qiu P, Li Y, et al. B. anthracis associated cardiovascular dysfunction and shock: the potential contribution of both non-toxin and toxin components. BMC Med. 2013;11:217. doi: 10.1186/1741-7015-11-217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sweeney DA, Hicks CW, Cui X, et al. Anthrax infection. Am J Respir Crit Care Med. 2011;184(12):1333–41. doi: 10.1164/rccm.201102-0209CI. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hicks CW, Sweeney DA, Cui X, et al. An overview of anthrax infection including the recently identified form of disease in injection drug users. Intensive Care Med. 2012;38(7):1092–104. doi: 10.1007/s00134-012-2541-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4•.Booth M, Donaldson L, Cui X, et al. Confirmed Bacillus anthracis infection among persons who inject drugs, Scotland, 2009-2010. Emerg Infect Dis. 2014;20(9):1452–63. doi: 10.3201/eid2009.131481. Review of 27 cases of Bacillus anthracis infection in injection drug users from the 2009 outbreak in the UK. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5•.Jernigan JA, Stephens DS, Ashford DA, et al. Bioterrorism-related inhalational anthrax: the first 10 cases reported in the United States. Emerg Infect Dis. 2001;7(6):933–44. doi: 10.3201/eid0706.010604. Review of 10 cases of inhalational B. anthracis infection from the 2001 outbreak in the US. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Walsh JJ, Pesik N, Quinn CP, et al. A case of naturally acquired inhalation anthrax: clinical care and analyses of anti-protective antigen immunoglobulin G and lethal factor. Clin Infect Dis. 2007;44(7):968–71. doi: 10.1086/512372. [DOI] [PubMed] [Google Scholar]
- 7.Anaraki S, Addiman S, Nixon G, et al. Investigations and control measures following a case of inhalation anthrax in East London in a drum maker and drummer, October 2008. Euro Surveill. 2008;13(51) [PubMed] [Google Scholar]
- 8.Klempner MS, Talbot EA, Lee SI, et al. Case records of the Massachusetts General Hospital. Case 25-2010. A 24-year-old woman with abdominal pain and shock. N Engl J Med. 2010;363(8):766–77. doi: 10.1056/NEJMcpc1003887. [DOI] [PubMed] [Google Scholar]
- 9•.Berger T, Kassirer M, Aran AA. Injectional anthrax – new presentation of an old disease. Euro Surveill. 2014;19(32) doi: 10.2807/1560-7917.es2014.19.32.20877. A summary of cases from the 2009 to 2011 outbreak of B. anthracis infection in injection drug users in the UK and Europe. [DOI] [PubMed] [Google Scholar]
- 10.Sprenkle MD, Griffith J, Marinelli W, et al. Lethal factor and anti-protective antigen IgG levels associated with inhalation anthrax, Minnesota, USA. Emerg Infect Dis. 2014;20(2):310–14. doi: 10.3201/eid2002.130245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sherer K, Li Y, Cui X, Eichacker PQ. Lethal and edema toxins in the pathogenesis of Bacillus anthracis septic shock: implications for therapy. Am J Respir Crit Care Med. 2007;175(3):211–21. doi: 10.1164/rccm.200608-1239CP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stevenson EK, Rubenstein AR, Radin GT, et al. Two decades of mortality trends among patients with severe sepsis: a comparative meta-analysis*. Crit Care Med. 2014;42(3):625–31. doi: 10.1097/CCM.0000000000000026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Angus DC, van der Poll T. Severe sepsis and septic shock. N Engl J Med. 2013;369(21):2063. doi: 10.1056/NEJMc1312359. [DOI] [PubMed] [Google Scholar]
- 14.Goldman DL, Casadevall A. Anthrax-associated shock. Front Biosci. 2008;13:4009–14. doi: 10.2741/2988. [DOI] [PubMed] [Google Scholar]
- 15.Golden HB, Watson LE, Lal H, et al. Anthrax toxin: pathologic effects on the cardiovascular system. Front Biosci. 2009;14:2335–57. doi: 10.2741/3382. [DOI] [PubMed] [Google Scholar]
- 16.Hicks CW, Cui X, Sweeney DA, et al. The potential contributions of lethal and edema toxins to the pathogenesis of anthrax associated shock. Toxins. 2011;3(9):1185–202. doi: 10.3390/toxins3091185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17•.Liu S, Moayeri M, Leppla SH. Anthrax lethal and edema toxins in anthrax pathogenesis. Trends Microbiol. 2014;22(6):317–25. doi: 10.1016/j.tim.2014.02.012. Excellent review of the pathophysiology of the anthrax toxins. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Young JA, Collier RJ. Anthrax toxin: receptor binding, internalization, pore formation, and translocation. Annu Rev Biochem. 2007;76:243–65. doi: 10.1146/annurev.biochem.75.103004.142728. [DOI] [PubMed] [Google Scholar]
- 19.Bromberg-White J, Lee CS, Duesbery N. Consequences and utility of the zinc-dependent metalloprotease activity of anthrax lethal toxin. Toxins. 2010;2(5):1038–53. doi: 10.3390/toxins2051038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moayeri M, Sastalla I, Leppla SH. Anthrax and the inflammasome. Microbes Infect. 2012;14(5):392–400. doi: 10.1016/j.micinf.2011.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tang WJ, Guo Q. The adenylyl cyclase activity of anthrax edema factor. Mol Aspects Med. 2009;30(6):423–30. doi: 10.1016/j.mam.2009.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hicks CW, Li Y, Okugawa S, et al. Anthrax edema toxin has cAMP-mediated stimulatory effects and high-dose lethal toxin has depressant effects in an isolated perfused rat heart model. Am J Physiol Heart Circ Physiol. 2011;300(3):H1108–18. doi: 10.1152/ajpheart.01128.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sayner SL. Emerging themes of cAMP regulation of the pulmonary endothelial barrier. Am J Physiol Lung Cell Mol Physiol. 2011;300(5):L667–78. doi: 10.1152/ajplung.00433.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guichard A, Nizet V, Bier E. New insights into the biological effects of anthrax toxins: linking cellular to organismal responses. Microbes Infect. 2012;14(2):97–118. doi: 10.1016/j.micinf.2011.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li Y, Cui X, Solomon SB, et al. B. anthracis edema toxin increases cAMP levels and inhibits phenylephrine-stimulated contraction in a rat aortic ring model. Am J Physiol Heart Circ Physiol. 2013;305(2):H238–50. doi: 10.1152/ajpheart.00185.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26•.Nestorovich EM, Bezrukov SM. Designing inhibitors of anthrax toxin. Expert Opin Drug Discov. 2014;9(3):299–318. doi: 10.1517/17460441.2014.877884. An excellent review on approaches to inhibiting the effects of anthrax toxin, structures of small molecule oligomer inhibitors provided. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bouzianas DG. Current and future medical approaches to combat the anthrax threat. J Med Chem. 2010;53(11):4305–31. doi: 10.1021/jm901024b. [DOI] [PubMed] [Google Scholar]
- 28.Van Der Goot G, Young JA. Receptors of anthrax toxin and cell entry. Mol Aspects Med. 2009;30(6):406–12. doi: 10.1016/j.mam.2009.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Martchenko M, Jeong SY, Cohen SN. Heterodimeric integrin complexes containing beta1-integrin promote internalization and lethality of anthrax toxin. Proc Natl Acad Sci USA. 2010;107(35):15583–8. doi: 10.1073/pnas.1010145107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Artenstein AW, Opal SM. Novel approaches to the treatment of systemic anthrax. Clin Infect Dis. 2012;54(8):1148–61. doi: 10.1093/cid/cis017. [DOI] [PubMed] [Google Scholar]
- 31.Thoren KL, Krantz BA. The unfolding story of anthrax toxin translocation. Mol Microbiol. 2011;80(3):588–95. doi: 10.1111/j.1365-2958.2011.07614.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Collier RJ. Membrane translocation by anthrax toxin. Mol Aspects Med. 2009;30(6):413–22. doi: 10.1016/j.mam.2009.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bann JG. Anthrax toxin protective antigen-insights into molecular switching from prepore to pore. Protein Sci. 2012;21(1):1–12. doi: 10.1002/pro.752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kumar BVS, Malik S, Grandhi P, et al. Anthrax lethal factor inhibitors as potential countermeasure of the infection. Curr Top Med Chem. 2014;14(17):1977–89. doi: 10.2174/1568026614666140929120231. [DOI] [PubMed] [Google Scholar]
- 35.Coate EA, Kocsis AG, Peters KN, et al. Remote monitoring of the progression of primary pneumonic plague in Brown Norway rats in high-capacity, high-containment housing. Pathog Dis. 2014;71(2):265–75. doi: 10.1111/2049-632X.12176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36•.Kammanadiminti S, Patnaikuni RK, Comer J, et al. Combination therapy with antibiotics and anthrax immune globulin intravenous (AIGIV) is potentially more effective than antibiotics alone in rabbit model of inhalational anthrax. PLoS One. 2014;9(9):e106393. doi: 10.1371/journal.pone.0106393. An important study testing the effects of post-treatment with AIG in an antibiotic-treated animal model. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mytle N, Hopkins RJ, Malkevich NV, et al. Evaluation of intravenous anthrax immune globulin for treatment of inhalation anthrax. Antimicrob Agents Chemother. 2013;57(11):5684–92. doi: 10.1128/AAC.00458-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38•.Hendricks KA, Wright ME, Shadomy SV, et al. Centers for disease control and prevention expert panel meetings on prevention and treatment of anthrax in adults. Emerg Infect Dis. 2014;20(2) doi: 10.3201/eid2002.130687. The latest recommendations from the CDC regarding the treatment of invasive anthrax infection, including the need to consider antitoxin adjunctive therapies. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Migone TS, Subramanian GM, Zhong J, et al. Raxibacumab for the treatment of inhalational anthrax. N Engl J Med. 2009;361(2):135–44. doi: 10.1056/NEJMoa0810603. [DOI] [PubMed] [Google Scholar]
- 40.Corey A, Migone TS, Bolmer S, et al. Bacillus anthracis protective antigen kinetics in inhalation spore-challenged untreated or levofloxacin/raxibacumab-treated New Zealand white rabbits. Toxins. 2013;5(1):120–38. doi: 10.3390/toxins5010120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41•.Migone TS, Bolmer S, Zhong J, et al. Added benefit of raxibacumab to antibiotic treatment of inhalational anthrax. Antimicrob Agents Chemother. 2015;59(2):1145–51. doi: 10.1128/AAC.04606-14. An important study testing the effects of post-treatment with raxibacumab in an antibiotic-treated animal model. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Barochia AV, Cui X, Sun J, et al. Protective antigen antibody augments hemodynamic support in anthrax lethal toxin shock in canines. J Infect Dis. 2012;205(5):818–29. doi: 10.1093/infdis/jir834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mohamed N, Clagett M, Li J, et al. A high-affinity monoclonal antibody to anthrax protective antigen passively protects rabbits before and after aerosolized Bacillus anthracis spore challenge. Infect Immun. 2005;73(2):795–802. doi: 10.1128/IAI.73.2.795-802.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Biron B, Beck K, Dyer D, et al. Efficacy of ETI-204 monoclonal antibody as an adjunct therapy in a New Zealand white rabbit partial survival model for inhalational anthrax. Antimicrob Agents Chemother. 2015;59(4):2206–14. doi: 10.1128/AAC.04593-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Anthium® – Investigational Aanthrax anti-toxin therapeutics. [Last accessed 02 November 2015]; Available from: www.elusys.com.
- 46.Albrecht MT, Li H, Williamson ED, et al. Human monoclonal antibodies against anthrax lethal factor and protective antigen act independently to protect against Bacillus anthracis infection and enhance endogenous immunity to anthrax. Infect Immun. 2007;75(11):5425–33. doi: 10.1128/IAI.00261-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chen Z, Moayeri M, Zhou YH, et al. Efficient neutralization of anthrax toxin by chimpanzee monoclonal antibodies against protective antigen. J Infect Dis. 2006;193(5):625–33. doi: 10.1086/500148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Altaweel L, Chen Z, Moayeri M, et al. Delayed treatment with W1-mAb, a chimpanzee-derived monoclonal antibody against protective antigen, reduces mortality from challenges with anthrax edema or lethal toxin in rats and with anthrax spores in mice. Crit Care Med. 2011;39(6):1439–47. doi: 10.1097/CCM.0b013e3182120691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hao L, Zheng F, Xiong S, et al. Preparation and evaluation of human-murine chimeric antibody against protective antigen of Bacillus anthracis. Int J Mol Sci. 2014;15(10):18496–507. doi: 10.3390/ijms151018496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Scobie HM, Young JA. Interactions between anthrax toxin receptors and protective antigen. Curr Opin Microbiol. 2005;8(1):106–12. doi: 10.1016/j.mib.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 51.Sharma S, Thomas D, Marlett J, et al. Efficient neutralization of antibody-resistant forms of anthrax toxin by a soluble receptor decoy inhibitor. Antimicrob Agents Chemother. 2009;53(3):1210–12. doi: 10.1128/AAC.01294-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cai C, Che J, Xu L, et al. Tumor endothelium marker-8 based decoys exhibit superiority over capillary morphogenesis protein-2 based decoys as anthrax toxin inhibitors. PLoS One. 2011;6(6):e20646. doi: 10.1371/journal.pone.0020646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wycoff KL, Belle A, Deppe D, et al. Recombinant anthrax toxin receptor-Fc fusion proteins produced in plants protect rabbits against inhalational anthrax. Antimicrob Agents Chemother. 2011;55(1):132–9. doi: 10.1128/AAC.00592-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Vuyisich M, Gnanakaran S, Lovchik JA, et al. A dual-purpose protein ligand for effective therapy and sensitive diagnosis of anthrax. Protein J. 2008;27(5):292–302. doi: 10.1007/s10930-008-9137-0. [DOI] [PubMed] [Google Scholar]
- 55.Thomas D, Naughton J, Cote C, et al. Delayed toxicity associated with soluble anthrax toxin receptor decoy-Ig fusion protein treatment. PLoS One. 2012;7(4):e34611. doi: 10.1371/journal.pone.0034611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Basha S, Rai P, Poon V, et al. Polyvalent inhibitors of anthrax toxin that target host receptors. Proc Natl Acad Sci USA. 2006;103(36):13509–13. doi: 10.1073/pnas.0509870103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rogers MS, Cryan LM, Habeshian KA, et al. A FRET-based high throughput screening assay to identify inhibitors of anthrax protective antigen binding to capillary morphogenesis gene 2 protein. PLoS One. 2012;7(6):e39911. doi: 10.1371/journal.pone.0039911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cryan LM, Habeshian KA, Caldwell TP, et al. Identification of small molecules that inhibit the interaction of TEM8 with anthrax protective antigen using a FRET assay. J Biomol Screen. 2013;18(6):714–25. doi: 10.1177/1087057113478655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Moayeri M, Wiggins JF, Lindeman RE, Leppla SH. Cisplatin inhibition of anthrax lethal toxin. Antimicrob Agents Chemother. 2006;50(8):2658–65. doi: 10.1128/AAC.01412-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Arevalo MT, Navarro A, Arico CD, et al. Targeted silencing of anthrax toxin receptors protects against anthrax toxins. J Biol Chem. 2014;289(22):15730–8. doi: 10.1074/jbc.M113.538587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Smith K, Crowe SR, Garman L, et al. Human monoclonal antibodies generated following vaccination with AVA provide neutralization by blocking furin cleavage but not by preventing oligomerization. Vaccine. 2012;30(28):4276–83. doi: 10.1016/j.vaccine.2012.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Crowe SR, Ash LL, Engler RJ, et al. Select human anthrax protective antigen epitope-specific antibodies provide protection from lethal toxin challenge. J Infect Dis. 2010;202(2):251–60. doi: 10.1086/653495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sarac MS, Peinado JR, Leppla SH, Lindberg I. Protection against anthrax toxemia by hexa-D-arginine in vitro and in vivo. Infect Immun. 2004;72(1):602–5. doi: 10.1128/IAI.72.1.602-605.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kacprzak MM, Peinado JR, Than ME, et al. Inhibition of furin by polyarginine-containing peptides: nanomolar inhibition by nona-D-arginine. J Biol Chem. 2004;279(35):36788–94. doi: 10.1074/jbc.M400484200. [DOI] [PubMed] [Google Scholar]
- 65.Peinado JR, Kacprzak MM, Leppla SH, Lindberg I. Cross-inhibition between furin and lethal factor inhibitors. Biochem Biophys Res Commun. 2004;321(3):601–5. doi: 10.1016/j.bbrc.2004.07.012. [DOI] [PubMed] [Google Scholar]
- 66.Shiryaev SA, Remacle AG, Ratnikov BI, et al. Targeting host cell furin proprotein convertases as a therapeutic strategy against bacterial toxins and viral pathogens. J Biol Chem. 2007;282(29):20847–53. doi: 10.1074/jbc.M703847200. [DOI] [PubMed] [Google Scholar]
- 67•.Remacle AG, Gawlik K, Golubkov VS, et al. Selective and potent furin inhibitors protect cells from anthrax without significant toxicity. Int J Biochem Cell Biol. 2010;42(6):987–95. doi: 10.1016/j.biocel.2010.02.013. Molecular structure of inhibitors provided. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Opal SM, Artenstein AW, Cristofaro PA, et al. Inter-alpha-inhibitor proteins are endogenous furin inhibitors and provide protection against experimental anthrax intoxication. Infect Immun. 2005;73(8):5101–5. doi: 10.1128/IAI.73.8.5101-5105.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Opal SM, Lim YP, Cristofaro P, et al. Inter-alpha inhibitor proteins: a novel therapeutic strategy for experimental anthrax infection. Shock. 2011;35(1):42–4. doi: 10.1097/SHK.0b013e3181e83204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Komiyama T, Swanson JA, Fuller RS. Protection from anthrax toxin-mediated killing of macrophages by the combined effects of furin inhibitors and chloroquine. Antimicrob Agents Chemother. 2005;49(9):3875–82. doi: 10.1128/AAC.49.9.3875-3882.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wein AN, Williams BN, Liu S, et al. Small molecule inhibitors of Bacillus anthracis protective antigen proteolytic activation and oligomerization. J Med Chem. 2012;55(18):7998–8006. doi: 10.1021/jm300804e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sawada-Hirai R, Jiang I, Wang F, et al. Human anti-anthrax protective antigen neutralizing monoclonal antibodies derived from donors vaccinated with anthrax vaccine adsorbed. J Immune Based Ther Vaccines. 2004;2(1):5. doi: 10.1186/1476-8518-2-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wang F, Ruther P, Jiang I, et al. Human monoclonal antibodies that neutralize anthrax toxin by inhibiting heptamer assembly. Hum Antibodies. 2004;13(4):105–10. [PubMed] [Google Scholar]
- 74.Peterson JW, Comer JE, Baze WB, et al. Human monoclonal antibody AVP-21D9 to protective antigen reduces dissemination of the Bacillus anthracis Ames strain from the lungs in a rabbit model. Infect Immun. 2007;75(7):3414–24. doi: 10.1128/IAI.00352-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Peterson JW, Comer JE, Noffsinger DM, et al. Human monoclonal anti-protective antigen antibody completely protects rabbits and is synergistic with ciprofloxacin in protecting mice and guinea pigs against inhalation anthrax. Infect Immun. 2006;74(2):1016–24. doi: 10.1128/IAI.74.2.1016-1024.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Malkevich NV, Basu S, Rudge TL, et al. Effect of anthrax immune globulin on response to BioThrax (anthrax vaccine adsorbed) in New Zealand white rabbits. Antimicrob Agents Chemother. 2013;57(11):5693–6. doi: 10.1128/AAC.00460-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Vitale L, Blanset D, Lowy I, et al. Prophylaxis and therapy of inhalational anthrax by a novel monoclonal antibody to protective antigen that mimics vaccine-induced immunity. Infect Immun. 2006;74(10):5840–7. doi: 10.1128/IAI.00712-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Riddle V, Leese P, Blanset D, et al. Phase I study evaluating the safety and pharmacokinetics of MDX-1303, a fully human monoclonal antibody against Bacillus anthracis protective antigen, in healthy volunteers. Clin Vaccine Immunol. 2011;18(12):2136–42. doi: 10.1128/CVI.05059-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79•.Froude JW, II, Thullier P, Pelat T. Antibodies against anthrax: mechanisms of action and clinical applications. Toxins. 2011;3(11):1433–52. doi: 10.3390/toxins3111433. An excellent review on the potential for antibody therapies in the treatment of anthrax. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80•.Rubert Pérez C, López-Pérez D, Chmielewski J, Lipton M. Small molecule inhibitors of anthrax toxin–induced cytotoxicity targeted against protective antigen. Chem Biol Drug Des. 2012;79(3):260–9. doi: 10.1111/j.1747-0285.2011.01285.x. An excellent review. [DOI] [PubMed] [Google Scholar]
- 81.Steiniger SC, Altobell LJ, III, Zhou B, Janda KD. Selection of human antibodies against cell surface-associated oligomeric anthrax protective antigen. Mol Immunol. 2007;44(10):2749–55. doi: 10.1016/j.molimm.2006.11.011. [DOI] [PubMed] [Google Scholar]
- 82.Zhou B, Carney C, Janda KD. Selection and characterization of human antibodies neutralizing Bacillus anthracis toxin. Bioorg Med Chem. 2008;16(4):1903–13. doi: 10.1016/j.bmc.2007.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Mourez M, Kane RS, Mogridge J, et al. Designing a polyvalent inhibitor of anthrax toxin. Nat Biotechnol. 2001;19(10):958–61. doi: 10.1038/nbt1001-958. [DOI] [PubMed] [Google Scholar]
- 84.Gujraty K, Sadacharan S, Frost M, et al. Functional characterization of peptide-based anthrax toxin inhibitors. Mol Pharm. 2005;2(5):367–72. doi: 10.1021/mp050040f. [DOI] [PubMed] [Google Scholar]
- 85.Gujraty KV, Joshi A, Saraph A, et al. Synthesis of polyvalent inhibitors of controlled molecular weight: structure-activity relationship for inhibitors of anthrax toxin. Biomacromolecules. 2006;7(7):2082–5. doi: 10.1021/bm060210p. [DOI] [PubMed] [Google Scholar]
- 86.Rai PR, Saraph A, Ashton R, et al. Raftlike polyvalent inhibitors of the anthrax toxin: modulating inhibitory potency by formation of lipid microdomains. Angew Chem. 2007;46(13):2207–9. doi: 10.1002/anie.200604317. [DOI] [PubMed] [Google Scholar]
- 87.Gujraty KV, Yanjarappa MJ, Saraph A, et al. Synthesis of homopolymers and copolymers containing an active ester of acrylic acid by RAFT: scaffolds for controlling polyvalent ligand display. J Polym Sci A Polym Chem. 2008;46(21):7246–57. doi: 10.1002/pola.23031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88•.Joshi A, Kate S, Poon V, et al. Structure-based design of a heptavalent anthrax toxin inhibitor. Biomacromolecules. 2011;12(3):791–6. doi: 10.1021/bm101396u. Structure-based design of heptavalent anthrax toxin inhibitor included. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89•.Little SF, Leppla SH, Friedlander AM. Production and characterization of monoclonal antibodies against the lethal factor component of Bacillus anthracis lethal toxin. Infect Immun. 1990;58(6):1606–13. doi: 10.21236/ada216203. One of the first reports on the use of monoclonal antibodies directed against lethal toxin. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zhao P, Liang X, Kalbfleisch J, et al. Neutralizing monoclonal antibody against anthrax lethal factor inhibits intoxication in a mouse model. Hum Antibodies. 2003;12(4):129–35. [PubMed] [Google Scholar]
- 91.Nguyen ML, Terzyan S, Ballard JD, et al. The major neutralizing antibody responses to recombinant anthrax lethal and edema factors are directed to non-cross-reactive epitopes. Infect Immun. 2009;77(11):4714–23. doi: 10.1128/IAI.00749-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Lim NK, Kim JH, Oh MS, et al. An anthrax lethal factor-neutralizing monoclonal antibody protects rats before and after challenge with anthrax toxin. Infect Immun. 2005;73(10):6547–51. doi: 10.1128/IAI.73.10.6547-6551.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Pelat T, Hust M, Laffly E, et al. High-affinity, human antibody-like antibody fragment (single-chain variable fragment)neutralizing the lethal factor (LF) of Bacillus anthracis by inhibiting protective antigen-LF complex formation. Antimicrob Agents Chemother. 2007;51(8):2758–64. doi: 10.1128/AAC.01528-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Vor dem Esche U, Huber M, Zgaga-Griesz A, et al. Passive vaccination with a human monoclonal antibody: Generation of antibodies and studies for efficacy in Bacillus anthracis infections. Immunobiology. 2011;216(7):847–53. doi: 10.1016/j.imbio.2010.12.001. [DOI] [PubMed] [Google Scholar]
- 95.Ding G, Chen X, Zhu J, et al. A human/murine chimeric fab antibody neutralizes anthrax lethal toxin in vitro. Clin Dev immunol. 2013;2013:475809. doi: 10.1155/2013/475809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Stienstra S. The use of anthrax and orthopox therapeutic antibodies from human origin in biodefense. [Last accessed 02 October 2015];J Bioterr Biodef. 2012 3:3. Available from: http://dx.doi.org/10.4172/2157-2526.S1.006. [Google Scholar]
- 97.Little SF, Leppla SH, Burnett JW, Friedlander AM. Structure-function analysis of Bacillus anthracis edema factor by using monoclonal antibodies. Biochem Biophys Res Commun. 1994;199(2):676–82. doi: 10.1006/bbrc.1994.1281. [DOI] [PubMed] [Google Scholar]
- 98.Kulshreshtha P, Bhatnagar R. Inhibition of anthrax toxins with a bispecific monoclonal antibody that cross reacts with edema factor as well as lethal factor of Bacillus anthracis. Mol Immunol. 2011;48(15-16):1958–65. doi: 10.1016/j.molimm.2011.05.024. [DOI] [PubMed] [Google Scholar]
- 99.Leysath CE, Chen KH, Moayeri M, et al. Mouse monoclonal antibodies to anthrax edema factor protect against infection. Infect Immun. 2011;79(11):4609–16. doi: 10.1128/IAI.05314-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Rosenfeld R, Marcus H, Ben-Arie E, et al. Isolation and chimerization of a highly neutralizing antibody conferring passive protection against lethal Bacillus anthracis infection. PLoS One. 2009;4(7):e6351. doi: 10.1371/journal.pone.0006351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Mechaly A, Levy H, Epstein E, et al. A novel mechanism for antibody-based anthrax toxin neutralization: inhibition of prepore-to-pore conversion. J Biol Chem. 2012;287(39):32665–73. doi: 10.1074/jbc.M112.400473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Sellman BR, Mourez M, Collier RJ. Dominant-negative mutants of a toxin subunit: an approach to therapy of anthrax. Science. 2001;292(5517):695–7. doi: 10.1126/science.109563. [DOI] [PubMed] [Google Scholar]
- 103.Singh Y, Khanna H, Chopra AP, Mehra V. A dominant negative mutant of Bacillus anthracis protective antigen inhibits anthrax toxin action in vivo. J Biol Chem. 2001;276(25):22090–4. doi: 10.1074/jbc.M010222200. [DOI] [PubMed] [Google Scholar]
- 104.Cao S, Guo A, Liu Z, et al. Investigation of new dominant-negative inhibitors of anthrax protective antigen mutants for use in therapy and vaccination. Infect Immun. 2009;77(10):4679–87. doi: 10.1128/IAI.00264-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Wu G, Feng C, Cao S, et al. Identification of new dominant-negative mutants of anthrax protective antigen using directed evolution. Appl Biochem Biotechnol. 2012;168(5):1302–10. doi: 10.1007/s12010-012-9858-6. [DOI] [PubMed] [Google Scholar]
- 106.Friedlander AM. Macrophages are sensitive to anthrax lethal toxin through an acid-dependent process. J Biol Chem. 1986;261(16):7123–6. [PubMed] [Google Scholar]
- 107.Artenstein AW, Opal SM, Cristofaro P, et al. Chloroquine enhances survival in Bacillus anthracis intoxication. J Infect Dis. 2004;190(9):1655–60. doi: 10.1086/424853. [DOI] [PubMed] [Google Scholar]
- 108.Hirsh MI, Cohen V. Chloroquine prevents T lymphocyte suppression induced by anthrax lethal toxin. J Infect Dis. 2006;194(7):1003–7. doi: 10.1086/507311. [DOI] [PubMed] [Google Scholar]
- 109.Hirsh MI, Manov I, Cohen-Kaplan V, Iancu TC. Ultrastructural features of lymphocyte suppression induced by anthrax lethal toxin and treated with chloroquine. Lab Invest. 2007;87(2):182–8. doi: 10.1038/labinvest.3700505. [DOI] [PubMed] [Google Scholar]
- 110.Orlik F, Schiffler B, Benz R. Anthrax toxin protective antigen: inhibition of channel function by chloroquine and related compounds and study of binding kinetics using the current noise analysis. Biophys J. 2005;88(3):1715–24. doi: 10.1529/biophysj.104.050336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Beitzinger C, Bronnhuber A, Duscha K, et al. Designed azolopyridinium salts block protective antigen pores in vitro and protect cells from anthrax toxin. PLoS One. 2013;8(6):e66099. doi: 10.1371/journal.pone.0066099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112•.Sanchez AM, Thomas D, Gillespie EJ, et al. Amiodarone and bepridil inhibit anthrax toxin entry into host cells. Antimicrob Agents Chemother. 2007;51(7):2403–11. doi: 10.1128/AAC.01184-06. Structure of small molecules that inhibiting LF provided. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Zhu PJ, Hobson JP, Southall N, et al. Quantitative high-throughput screening identifies inhibitors of anthrax-induced cell death. Bioorg Med Chem. 2009;17(14):5139–45. doi: 10.1016/j.bmc.2009.05.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Karginov VA. Cyclodextrin derivatives as anti-infectives. Curr Opin Pharmacol. 2013;13(5):717–25. doi: 10.1016/j.coph.2013.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115•.Karginov VA, Yohannes A, Robinson TM, et al. β-Cyclodextrin derivatives that inhibit anthrax lethal toxin. Bioorg Med Chem. 2006;14(1):33–40. doi: 10.1016/j.bmc.2005.07.054. Structure of molecules that inhibit pore formation provided. [DOI] [PubMed] [Google Scholar]
- 116.Backer MV, Patel V, Jehning BT, et al. Inhibition of anthrax protective antigen outside and inside the cell. Antimicrob Agents Chemother. 2007;51(1):245–51. doi: 10.1128/AAC.00983-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Karginov VA, Nestorovich EM, Moayeri M, et al. Blocking anthrax lethal toxin at the protective antigen channel by using structure-inspired drug design. Proc Natl Acad Sci USA. 2005;102(42):15075–80. doi: 10.1073/pnas.0507488102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Karginov VA, Nestorovich EM, Yohannes A, et al. Search for cyclodextrin-based inhibitors of anthrax toxins: synthesis, structural features, and relative activities. Antimicrob Agents Chemother. 2006;50(11):3740–53. doi: 10.1128/AAC.00693-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Moayeri M, Robinson TM, Leppla SH, Karginov VA. In vivo efficacy of beta-cyclodextrin derivatives against anthrax lethal toxin. Antimicrob Agents Chemother. 2008;52(6):2239–41. doi: 10.1128/AAC.00009-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Kong Y, Guo Q, Yu C, et al. Fusion protein of Delta 27LFn and EFn has the potential as a novel anthrax toxin inhibitor. FEBS Lett. 2009;583(8):1257–6. doi: 10.1016/j.febslet.2009.03.053. [DOI] [PubMed] [Google Scholar]
- 121•.Dalkas GA, Papakyriakou A, Vlamis-Gardikas A, Spyroulias GA. Low molecular weight inhibitors of the protease anthrax lethal factor. Mini Rev Med Chem. 2008;8(3):290–306. doi: 10.2174/138955708783744083. Structures of small molecule inhibitors of LF provided. [DOI] [PubMed] [Google Scholar]
- 122.Turk BE. Discovery and development of anthrax lethal factor metalloproteinase inhibitors. Curr Pharm Biotechnol. 2008;9(1):24–33. doi: 10.2174/138920108783497604. [DOI] [PubMed] [Google Scholar]
- 123.Tonello F, Montecucco C. The anthrax lethal factor and its MAPK kinase-specific metalloprotease activity. Mol Aspects Med. 2009;30(6):431–8. doi: 10.1016/j.mam.2009.07.006. [DOI] [PubMed] [Google Scholar]
- 124.Tonello F, Seveso M, Marin O, et al. Screening inhibitors of anthrax lethal factor. Nature. 2002;418(6896):386. doi: 10.1038/418386a. [DOI] [PubMed] [Google Scholar]
- 125.Turk BE, Wong TY, Schwarzenbacher R, et al. The structural basis for substrate and inhibitor selectivity of the anthrax lethal factor. Nat Struct Mol Biol. 2004;11(1):60–6. doi: 10.1038/nsmb708. [DOI] [PubMed] [Google Scholar]
- 126.Xiong Y, Wiltsie J, Woods A, et al. The discovery of a potent and selective lethal factor inhibitor for adjunct therapy of anthrax infection. Bioorg Med Chem Lett. 2006;16(4):964–8. doi: 10.1016/j.bmcl.2005.10.088. [DOI] [PubMed] [Google Scholar]
- 127.Shoop WL, Xiong Y, Wiltsie J, et al. Anthrax lethal factor inhibition. Proc Natl Acad Sci USA. 2005;102(22):7958–63. doi: 10.1073/pnas.0502159102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Jiao GS, Kim S, Moayeri M, et al. Antidotes to anthrax lethal factor intoxication. Part 3: Evaluation of core structures and further modifications to the C2-side chain. Bioorg Med Chem Lett. 2012;22(6):2242–6. doi: 10.1016/j.bmcl.2012.01.095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Kim S, Jiao GS, Moayeri M, et al. Antidotes to anthrax lethal factor intoxication. Part 2: structural modifications leading to improved in vivo efficacy. Bioorg Med Chem Lett. 2011;21(7):2030–3. doi: 10.1016/j.bmcl.2011.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Jiao GS, Kim S, Moayeri M, et al. Antidotes to anthrax lethal factor intoxication. Part 1: Discovery of potent lethal factor inhibitors with in vivo efficacy. Bioorg Med Chem Lett. 2010;20(22):6850–3. doi: 10.1016/j.bmcl.2010.08.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Moayeri M, Crown D, Jiao GS, et al. Small-molecule inhibitors of lethal factor protease activity protect against anthrax infection. Antimicrob Agents Chemother. 2013;57(9):4139–45. doi: 10.1128/AAC.00941-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Forino M, Johnson S, Wong TY, et al. Efficient synthetic inhibitors of anthrax lethal factor. Proc Natl Acad Sci USA. 2005;102(27):9499–504. doi: 10.1073/pnas.0502733102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Kim C, Gajendran N, Mittrucker HW, et al. Human alpha-defensins neutralize anthrax lethal toxin and protect against its fatal consequences. Proc Natl Acad Sci USA. 2005;102(13):4830–5. doi: 10.1073/pnas.0500508102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Dell'Aica I, Dona M, Tonello F, et al. Potent inhibitors of anthrax lethal factor from green tea. EMBO Rep. 2004;5(4):418–22. doi: 10.1038/sj.embor.7400118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Wickliffe KE, Leppla SH, Moayeri M. Anthrax lethal toxin-induced inflammasome formation and caspase-1 activation are late events dependent on ion fluxes and the proteasome. Cell Microbiol. 2008;10(2):332–43. doi: 10.1111/j.1462-5822.2007.01044.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Chen Z, Moayeri M, Zhao H, et al. Potent neutralization of anthrax edema toxin by a humanized monoclonal antibody that competes with calmodulin for edema factor binding. Proc Natl Acad Sci USA. 2009;106(32):13487–92. doi: 10.1073/pnas.0906581106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Winterroth L, Rivera J, Nakouzi AS, et al. Neutralizing monoclonal antibody to edema toxin and its effect on murine anthrax. Infect Immun. 2010;78(6):2890–8. doi: 10.1128/IAI.01101-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138•.Seifert R, Dove S. Inhibitors of Bacillus anthracis edema factor. Pharmacol Ther. 2013;140(2):200–12. doi: 10.1016/j.pharmthera.2013.07.002. An excellent review on potential inhibitors of edema factor with molecular structures provided. [DOI] [PubMed] [Google Scholar]
- 139.Shen Y, Zhukovskaya NL, Zimmer MI, et al. Selective inhibition of anthrax edema factor by adefovir, a drug for chronic hepatitis B virus infection. Proc Natl Acad Sci USA. 2004;101(9):3242–7. doi: 10.1073/pnas.0306552101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Tang WJ, Guo Q. The adenylyl cyclase activity of anthrax edema factor. Mol Aspects Med. 2009;30(6):423–30. doi: 10.1016/j.mam.2009.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Lee YS, Bergson P, He WS, et al. Discovery of a small molecule that inhibits the interaction of anthrax edema factor with its cellular activator, calmodulin. Chem Biol. 2004;11(8):1139–46. doi: 10.1016/j.chembiol.2004.05.020. [DOI] [PubMed] [Google Scholar]
- 142.Schein CH, Chen D, Ma L, et al. Pharmacophore selection and redesign of non-nucleotide inhibitors of anthrax edema factor. Toxins. 2012;4(11):1288–300. doi: 10.3390/toxins4111288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Chen D, Misra M, Sower L, et al. Novel inhibitors of anthrax edema factor. Bioorg Med Chem. 2008;16(15):7225–33. doi: 10.1016/j.bmc.2008.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Suryanarayana S, Wang JL, Richter M, et al. Distinct interactions of 2′- and 3′-O-(N-methyl)anthraniloyl-isomers of ATP and GTP with the adenylyl cyclase toxin of Bacillus anthracis, edema factor. Biochem Pharmacol. 2009;78(3):224–30. doi: 10.1016/j.bcp.2009.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Taha HM, Schmidt J, Gottle M, et al. Molecular analysis of the interaction of anthrax adenylyl cyclase toxin, edema factor, with 2′(3′)-O-(N-(methyl) anthraniloyl)-substituted purine and pyrimidine nucleotides. Mol Pharmacol. 2009;75(3):693–703. doi: 10.1124/mol.108.052340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Pinto C, Lushington GH, Richter M, et al. Structure-activity relationships for the interactions of 2′- and 3′-(O)-(N-methyl)anthraniloyl-substituted purine and pyrimidine nucleotides with mammalian adenylyl cyclases. Biochem Pharmacol. 2011;82(4):358–70. doi: 10.1016/j.bcp.2011.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Taha H, Dove S, Geduhn J, et al. Inhibition of the adenylyl cyclase toxin, edema factor, from Bacillus anthracis by a series of 18 mono- and bis-(M)ANT-substituted nucleoside 5′-triphosphates. Naunyn Schmiedeberg's Arch Pharmacol. 2012;385(1):57–68. doi: 10.1007/s00210-011-0688-9. [DOI] [PubMed] [Google Scholar]
- 148.Geduhn J, Dove S, Shen Y, et al. Bis-halogen-anthraniloyl-substituted nucleoside 5′-triphosphates as potent and selective inhibitors of Bordetella pertussis adenylyl cyclase toxin. J Pharmacol Exp Ther. 2011;336(1):104–15. doi: 10.1124/jpet.110.174219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Gille A, Lushington GH, Mou TC, et al. Differential inhibition of adenylyl cyclase isoforms and soluble guanylyl cyclase by purine and pyrimidine nucleotides. J Biol Chem. 2004;279(19):19955–69. doi: 10.1074/jbc.M312560200. [DOI] [PubMed] [Google Scholar]
- 150.Laine E, Goncalves C, Karst JC, et al. Use of allostery to identify inhibitors of calmodulin-induced activation of Bacillus anthracis edema factor. Proc Natl Acad Sci USA. 2010;107(25):11277–82. doi: 10.1073/pnas.0914611107. [DOI] [PMC free article] [PubMed] [Google Scholar]


