Abstract
A 72-year-old woman with a history of malignant lymphoma was referred to our hospital for the treatment of a bronchial artery aneurysm. Computed tomography (CT) scan showed a round, 30 mm-diameter fusiform aneurysm with two tortuous inflow arteries. We deployed thoracic stent grafting to cover the orifice of the two inflow arteries without transcatheter bronchial arterial embolization. Postoperative CT scan revealed complete thrombosis of the aneurysm. Although further follow-up is mandatory, this may be considered a viable treatment option in cases wherein the bronchial artery aneurysm is anatomically difficult to treat.
Keywords: bronchial artery aneurysm (BAA), endovascular surgery, stent graft
Introduction
Bronchial artery aneurysm (BAA) is a very rare disease found in <1% of patients undergoing bronchial arteriography.1) Multiple etiologies are reported for BAA, including congenital, acquired, and others.
Two approaches are recommended for the treatment of BAA. The first approach is open surgical treatment, involving extirpation of BAA or ligation of the inflow artery through thoracotomy. The second approach is endovascular treatment, which includes transcatheter bronchial arterial embolization (TAE), aortic stent grafting, or a combination of both. In this report, we present a patient with BAA treated successfully using only an aortic stent graft.
Case Report
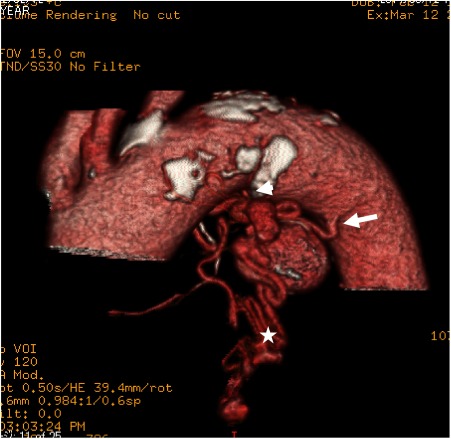
A 72-year-old woman was admitted to our hospital for the treatment of a BAA, which was incidentally detected during the observation of malignant lymphoma. She had a medical history of steroid use for rheumatoid arthritis for more than 20 years. At the age of 57, she underwent cerebral aneurysm clipping surgery due to a subarachnoid hemorrhage. She had no particular symptoms at the time of admission. Her general condition was poor, and she required wheelchair assistance due to moderate hemiplegia. An enhanced computed tomography (CT) angiogram revealed a round, 30 mm-diameter fusiform BAA adjacent to the distal aortic arch (Fig. 1). This aneurysm had two inflow arteries, one being the left bronchial artery and the other being a tortuous and thin artery branching from the lesser curvature of the aortic arch. Some indented outflow vessels drained into the pulmonary artery.
Fig. 1 An enhanced CT angiogram revealed a round, fusiform BAA adjacent to the distal aortic arch. This aneurysm had two inflow arteries, one is the left bronchial artery (arrow) and the other is a tortuous and thin artery branching from the lesser curvature of the aortic arch (arrowhead). Some indented outflow vessels drained to the pulmonary artery (asterisk).
Given the patient’s general status and frailty, conventional open chest surgery seemed to have a high operative risk. Therefore, we selected a less invasive endovascular approach. Because there were multiple, thin, and tortuous inflow arteries, coil embolization was considered technically demanding. Finally, we decided to use an aortic stent graft alone to block the blood flow into the aneurysm.
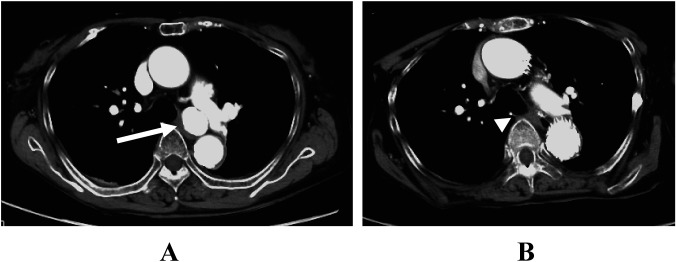
Under general anesthesia, the right common femoral artery was exposed, and a 6F sheath was inserted into the left femoral artery percutaneously. After heparin was administered, a 34 mm×157 mm thoracic aortic stent graft (Cook Zenith TX2, Cook Medical, Bloomington, IN, USA) was inserted from the left femoral artery. With fluoroscopic guidance, the stent graft was deployed at zone 3 across the orifice of the feeding artery and dilated with a balloon catheter (Cook Zenith Coda balloon). A post-procedure angiogram showed a small but not negligible type IA endoleak so we added a proximal extension device (Cook Zenith TX2 34 mm×77 mm) at zone 3 to cover the proximal portion of the device. After this procedure, blood flow into the aneurysm halted. The postoperative course was uneventful, and CT angiography at the time of hospital discharge demonstrated complete thrombosis of the aneurysm. Two years after the treatment, the patient was doing well. A repeat CT scan revealed no endoleakage, and the size of the aneurysm was reduced to 8 mm (Fig. 2).
Fig. 2 (A) Preoperative axial CT image showed round mediastinal BAA (arrow). (B) Follow-up CT performed two years after treatment revealed no endoleak, and the size of the aneurysm was reduced to 8 mm (arrowhead).
Discussion
BAA is a very rare disease and is observed in <1% of patients who receive selective bronchial artery angiography.1) Although the cause of BAA is not clear, congenital (in the context of pulmonary sequestration or pulmonary agenesis) and acquired (as a result of arteriosclerosis or inflammatory lung disease, bronchiectasis, or trauma) have been reported as potential etiologies of BAA.1,2) In either case, the main mechanism of this disease is thought to be local weakness or damage to the arterial wall or an increase in bronchial artery blood flow. In this case, the cause of BAA may have been related to atherosclerosis because she had a history of hypertension for many years without trauma or lung disease.
Although BAA is often asymptomatic and diagnosed by chance, it may cause various symptoms. Symptoms vary depending on whether the site of BAA is intrapulmonary or mediastinal.1) The former case exhibits hemoptysis as the main symptom, while the latter shows various symptoms such as hemoptysis and others related to the compression or rupture of an adjacent organ. In cases involving rupture, the most frequent symptom is severe chest pain mimicking acute aortic dissection. Other symptoms such as hemothorax, hemomediastinum with superior vena cava syndrome, and hematemesis due to esophageal erosion have also been reported.
Some reports suggest no correlation between the risk of rupture and the size of aneurysm.1,8) Because of the high mortality associated with BAA rupture, it is recommended that BAA be treated when diagnosis is confirmed.1) BAA can be treated via either surgical or endovascular approach. In the surgical approach, resection of BAA and pulmonary lobectomy in case of bronchiectasis is performed through thoracotomy. Although it is possible to remove the lesion completely, this approach is invasive and currently limited to patients in whom endovascular treatment is contraindicated or has failed.3)
In the endovascular approach, TAE is an accepted first-line management owing to its low invasiveness. However, it is difficult to achieve complete embolization in cases where the vascular segment between the aneurysm and aorta is short.4) Revascularization of BAA is also reported by collateral vessels, incomplete embolization, and arterial re-canalization.1,4) In addition, in cases where the neck of BAA is branched from the anterior surface of the descending aorta, the possibility of distal embolization is significant.2)
Therefore, treatment with aortic stent grafts has been recently noted. It is possible to completely isolate the blood flow into the aneurysm by securely sealing the opening site of the feeding artery. To date, eight cases of BAA treated with aortic stent graft with or without TAE have been reported (Table 1). Since the retrograde blood flow to the aneurysm from the outflow vessel may remain, some authors recommended that TAE should be considered with the stent graft simultaneously.1,2,4) Although the follow-up period was short, Kasashima et al.6) and Arici et al.10) reported acceptable results using stent graft treatment alone. We also examined TAE in our case; it seemed too technically demanding because there are multiple, thin, and tortuous inflow arteries. Moreover, taking the patient’s status into consideration, we decided to treat with a stent graft alone. Takahashi et al. also commented that TAE is not necessary because the outflow artery finally returns to the pulmonary artery, which is the low-pressure system.8) In addition, even if the retrograde blood flow remained, transcatheter embolization of the outflow artery via the pulmonary artery may be considered. At present, stent grafting for BAA is not approved in Japan. If this procedure becomes covered by insurance in the future, treatment choices for BAA will increase for high-risk cases.
Table 1 Reported cases of bronchial artery aneurysm treated with stent graft in the English literature.
| Author (year) | Age | Sex | Rupture | Treatment | Outcome | Follow up |
|---|---|---|---|---|---|---|
| Sakai (1998)5) | 72 | M | No | TAE (coil)+SG | Complete thrombosis | 7 months |
| Kasashima (2003)6) | 79 | M | No | SG | Complete thrombosis | 18 months |
| Sanchez (2007)7) | 69 | F | No | TAE (fibrin sealant)+SG | Complete thrombosis | 3 days |
| Takahashi (2010)8) | 74 | M | No | TAE (coil)+SG | Complete thrombosis | 6 months |
| Hu (2011)2) | 67 | M | Yes | TAE (sodium polymannuronate, gelatin sponge)+SG | Complete thrombosis | 12 months |
| Guzzardi (2012)9) | 66 | M | No | TAE (coil)+SG | Complete thrombosis | 6 months |
| Arici (2013)10) | 64 | M | No | SG | Complete thrombosis | 30 days |
| Kim (2014)4) | 73 | F | No | TAE (PVA particles, gelfoam particle, coil)+SG | Complete resolution | 24 months |
| Our case | 72 | F | No | SG | Complete thrombosis | 24 months |
PVA: polyvinyl alcohol; SG: stent graft; TAE: transcatheter bronchial artery embolization
Conclusion
In conclusion, we report a rare case of BAA treated successfully with stent graft alone. Although further follow-up is mandatory, this may be considered a viable treatment option in cases where BAA is difficult to treat due to the anatomical reasons.
Disclosure Statement
All authors have no conflict of interest regarding the publication of this paper.
Author Contributions
Writing: TM
Critical review and revision: all authors
Final approval of the article: all authors
Accountability for all aspects of the work: all authors
References
- 1).Tanaka K, Ihaya A, Horiuci T, et al. Giant mediastinal bronchial artery aneurysm mimicking benign esophageal tumor: a case report and review of 26 cases from literature. J Vasc Surg 2003; 38: 1125-9. [DOI] [PubMed] [Google Scholar]
- 2).Hu C-X, Huang S, Xu Z-W, et al. Combination of aortic stent-graft and arterial embolization for ruptured bronchial artery aneurysm. Ann Thorac Surg 2011; 92: e19-21. [DOI] [PubMed] [Google Scholar]
- 3).Chatterjee A, Ghosh S, Salhiyyah K, et al. A rare presentation of ruptured bronchial artery aneurysm. Thorax 2004; 59: 912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4).Kim YK, Sung YM, Kim JH, et al. Aortic stent-graft for giant bronchial artery aneurysm with ultrashort neck. Ann Thorac Cardiovasc Surg 2014; 20 Suppl: 781-5. [DOI] [PubMed] [Google Scholar]
- 5).Sakai T, Razavi MK, Semba CP, et al. Percutaneous treatment of bronchial artery aneurysm with use of transcatheter coil embolization and thoracic aortic stent-graft placemen. J Vasc Interv Radiol 1998; 9: 1025-8. [DOI] [PubMed] [Google Scholar]
- 6).Kasashima F, Endo M, Kosugi I, et al. Mediastinal bronchial artery aneurysm treated with a stent-graft. J Endovasc Ther 2003; 10: 381-5. [DOI] [PubMed] [Google Scholar]
- 7).Sanchez E, Alados P, Zurera L, et al. Bronchial artery aneurysm treated with aortic stent graft and fibrin sealant. Ann Thorac Surg 2007; 83: 693-5. [DOI] [PubMed] [Google Scholar]
- 8).Takahashi Y, Tsutsumi Y, Monta O, et al. Stent grafting for giant bronchial artery aneurysm disguised as an aneurysm with multiple feeding artery. Ann Thorac Surg 2010; 89: 1652-4. [DOI] [PubMed] [Google Scholar]
- 9).Guzzardi G, Cerini P, Fossaceca R, et al. Endovascular treatment of bronchial artery aneurysm with aortic stent-graft placement and coil embolization. Ann Vasc Surg 2012; 26: 1013.e5-8. [DOI] [PubMed] [Google Scholar]
- 10).Arici V, Bozzani A, Odero A. Successful endovascular treatment of a bronchial artery aneurysm refractory to transcatheter embolization. Ann Vasc Surg 2013; 27: 802.e13-5. [DOI] [PubMed] [Google Scholar]