Abstract
Objective: To evaluate the relationship between varicose veins and heart failure, both of which cause edema of lower extremities.
Materials and Methods: We enrolled 150 patients who underwent intervention for varicose veins of lower extremities between December 2012 and October 2015, and perioperative data were retrospectively investigated.
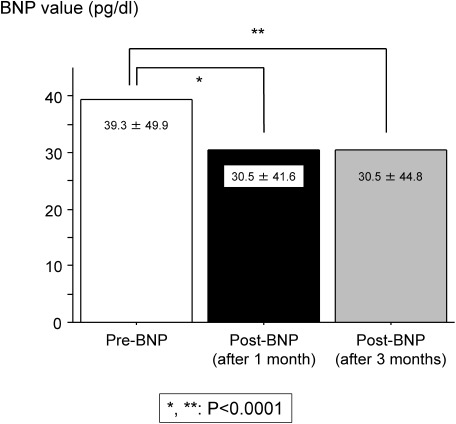
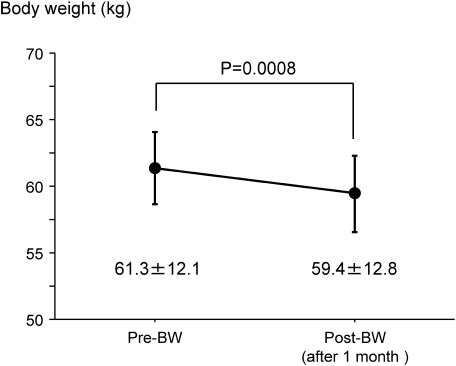
Results: Of the 150 patients, 104 (69.3%) were females. The mean age was 66.8±10.6 years (27–85 years). Eighty (53.3%) patients had varicose veins in both legs. In all patients, the postoperative (brain natriuretic peptide (BNP) value was significantly lower than the preoperative BNP value (pre : post=39.3 : 30.5 pg/dl, P<0.0001). In patients with higher BNP values (>100 pg/dl), the postoperative BNP values were significantly lower than the preoperative BNP values (pre : post=192.7 : 166.1 pg/dl, P<0.0001). Body weights of the patients decreased differently between pre- and post-operation (pre : post=61.3 : 59.4 kg, P=0.0008).
Conclusion: Intervention for varicose veins of lower extremities might be considered clinically useful for the improvement of cardiac function.
Keywords: varicose vein, brain natriuretic peptide, heart failure
Introduction
Varicose veins (VV) are frequent causes of discomfort, loss of productivity, and deterioration in the quality of life. The rate of occurrence is very high, affecting approximately 20–73% females and 15–56% males.1–5) The initial treatment for VV is elastic compression stockings. Anti-platelet and/or anticoagulation drugs are helpful for patients with few symptoms. In addition, sclerosing injections are effective. As a radical treatment, surgical stripping, endovascular ablation, or radiofrequency ablation (RFA) is typically the treatment of choice.
VV is also one of the causes of edema in the lower extremities. The mechanism behind this is chronic venous insufficiency.6) Perceptible change in the volume of fluid in the skin and subcutaneous structure are characteristically indented with pressure. Venous edema usually occurs in the ankle region but may extend to the lower leg and foot.
Limb edema appears as a symptom of many disorders. Renal dysfunction, liver cirrhosis, and particularly, heart failure cause edema of lower extremities in many patients. However, the relationship between VV and heart failure is unknown. The aim of this study was to investigate whether treatment for VV improved heart failure.
Materials and Methods
This retrospective study was approved by the institutional review board, and a written informed consent was obtained from all patients.
Overall, 194 patients underwent surgical interventions for VV in our institution between December 2012 and October 2015. Patients treated for small saphenous veins were excluded from this study. Thus, only 150 patients were enrolled.
In our institution, all patients with VV of the lower extremities underwent both ultrasound and magnetic resonance venography (MRV).7) We performed short stripping of saphenous veins (SS) or RFA as a surgical intervention for VV. We have performed RFA since May 2015; therefore, all patients before April 2015 underwent SS. After May 2015, patients with large saphenous veins (diameter >10 mm) underwent SS too.
The following characteristics were analyzed at the time of diagnosis: demographic features, predisposing family history and past personal history, clinical features, treatment, and outcome. Pre- and postoperative (1 month after surgical intervention) examinations included echocardiographic studies, radiologic images, and results of routine laboratory tests (including hematological value, lipid parameter, liver and renal function, and inflammatory parameters). The normal brain natriuretic peptide (BNP) value was ≤18.4 pg/dl in our hospital. The BNP value was examined thrice (once preoperatively and at 1 and 3 months after surgical interventions).
Continuous variables were expressed as median±SD with ranges when appropriate. Categorical variables were expressed as numbers (%) and were compared with continuous variables using Student’s t test. Examinations of parametric data were used with contingency tables, with Fisher’s exact test. Differences were considered significant at P<0.05. Stat View for Windows version 6.0 (SAS Institute Inc., Cary, NC, USA) software program was used for all calculations.
Results
Table 1 shows that 104 out of 150 patients (69.3%) were female. The mean age was 66.8±10.6 years (27–85 years). VV in both legs occurred in 80 patients (53.3%). Overall, 130 patients (86.7%) underwent SS, and the other 20 patients (13.3%) underwent RFA.
Table 1 Demographic characteristics of all patients before intervention.
| n (%) | |
|---|---|
| Age (year) | 66.8±10.6 |
| Sex (female) | 104 (69.3%) |
| DM | 25 (16.7%) |
| AF | 3 (2.0%) |
| Bilateral VV | 80 (53.3%) |
| CEAP classification | |
| C2 and C3 | 133 (88.7%) |
| C4, C5, and C6 | 17 (11.3%) |
| BNP >100 pg/dl | 7 (4.7%) |
| Surgical intervention | |
| SS | 130 (86.7%) |
| RFA | 20 (13.3%) |
DM: diabetes mellitus; AF: atrial fibrillation; VV: varicose veins; CEAP: clinical etiology anatomy pathophysiology; BNP: brain natriuretic peptide; SS: short stripping of saphenous veins; RFA: radiofrequency ablation
Amongst all patients, 25 patients (16.7%) had diabetes mellitus, and 3 patients (2.0%) had atrial fibrillation (Table 1). No patient received hemodialysis (data not shown).
In this study, we investigated every test preoperatively and postoperatively (1 month after surgical interventions). Table 2 shows that postoperative albumin was significantly lower than preoperative albumin (pre : post=4.30±0.20 : 4.17±0.50 g/dl, P=0.0003). However, postoperative BNP values were significantly lower than preoperative BNP values (pre : post=39.3±49.9 : 30.5±41.6 pg/dl, P<0.0001). At 3 months after surgical intervention, the BNP value had remained low, similar to that of 1 month after intervention (Fig. 1). Additionally, postoperative BNP values were significantly lower than preoperative BNP values in patients with higher preoperative BNP values (>100 pg/dl) (pre : post=192.7±110.5 : 166.1±101.1 pg/dl, P<0.0001). There were no significant differences between pre- and post-operation creatinine levels (pre : post=0.70±0.17 : 0.74±0.40 mg/dl, P=0.2494), ejection fraction (pre : post=69.2±5.2 : 68.4±8.4%, P=0.7570), and tricuspid valve regurgitation grade in cardiac ultrasound cardiography (UCG) (pre : post=1.29±0.90 : 1.15±0.99 g/dl, P=0.5884).
Table 2 Perioperative laboratory data.
| Preoperative | Postoperative (after 1 month) | P Value | |
|---|---|---|---|
| Albumin (g/dl) | 4.30±0.20 | 4.17±0.50 | 0.0003 |
| Creatinine (mg/dl) | 0.70±0.17 | 0.74±0.40 | 0.2494 |
| BNP value (pg/dl) | 39.30±49.90 | 30.50±41.60 | <0.0001 |
| UCG | |||
| EF (%) | 69.2±5.2 | 68.4±8.4 | 0.7570 |
| TR grade | 1.29±0.90 | 1.15±0.99 | 0.5884 |
| Only high preoperative BNP (>100 pg/dl) | 192.7±110.5 | 166.1±101.1 | <0.0001 |
BNP: brain natriuretic peptide; UCG: ultrasound cardiography; EF: ejection fraction; TR: tricuspid regurgitation
Fig. 1 Perioperative BNP changes. BNP: brain natriuretic peptide.
Figure 2 shows that body weight (BW) of the patients decreased differently between pre- and postoperative intervention (pre : post=61.3±12.1 : 59.4±12.8 kg, P=0.0008). Preoperative edema of lower extremities improved in all patients (data not shown).
Fig. 2 Perioperative body weight changes. BW: body weight.
Between the SS group (n=130) and the RFA group (n=20), there were no significant differences in the perioperative BNP value (Table 3). Moreover, postoperative BNP values significantly decreased more than preoperative BNP values in both the groups (SS group: P=0.0184, RFA group: P<0.0001).
Table 3 Perioperative BNP changes between surgical interventions.
| SS group (n=130) | RFA group (n=20) | P value | |
|---|---|---|---|
| Preoperative BNP value (pg/dl) | 39.71±51.52 | 32.22±22.97 | 0.5339 |
| Postoperative BNP value (pg/dl) (after 1 month) | 30.37±44.92 | 24.67±13.13 | 0.5840 |
| P value | 0.0184 | <0.0001 |
SS: short stripping of saphenous veins; RFA: radiofrequency ablation; BNP: brain natriuretic peptide
Discussion
In our investigation, interventions for varicose saphenous veins of the lower extremities decreased BNP values. Postoperative BNP value depression was observed in the patients with higher BNP values (BNP >100 pg/dl). Although the nutrition status was poor, cardiac and renal functions did not change perioperatively.
BNP is a hormone secreted from the ventricles or lower chambers of the heart, and it undergoes a reaction to an increase in pressure that occurs when cardiac failure develops and worsens. BNP values are used as a barometer of cardiac failure in clinical practice. The level of BNP in the blood increases when heart failure becomes advanced and decreases when the heart failure condition is stable. In a patient with heart failure, BNP values are much higher than in a patient with normal heart function.
BNP levels increase in diseases other than heart failure, for example, renal failure (particularly patients who underwent hemodialysis), liver cirrhosis, and hyperthyroidism. Although there was no report that VV caused an elevation in the production of BNP, 91 (60.7%) patients had higher preoperative BNP values in the present study (data not shown). These patients showed normal cardiac function in UCG (Table 2).
Patients with higher postoperative values decreased to 69 (46.0%), and postoperative BNP values were significantly lower than preoperative BNP values (Table 2). The reason behind the decreased BNP values after intervention is uncertain. Moreover, the BW significantly decreased after operation in Fig. 2. Additionally, preoperative edema of the lower extremities improved in all patients (data not shown). VV causes edema of the lower extremities, and congestion of the lower extremities could become a load on cardiac function. We consider that the mechanism behind leg edema reduction after VV operation is the improvement of calf muscle pump function, and the improvement of leg edema triggers BW reduction. Further, BW loss may decrease BNP values.
Generally, a high BNP value (>100 pg/ml) is suggestive of cardiac failure.8) In our study, there were 11 (7.3%) patients with preoperative high BNP values, but their postoperative BNP values decreased (data not shown). Surgical intervention for VV could reduce the load on heart failure. In this regard, there were no significant differences in pre- and postoperative BNP values between SS and RFA (Table 3).
The results of this study had certain limitations. The present study is a retrospective study. In addition, the result was limited by a relatively small number of patients included because it was a single-center study. Despite these limitations, our study shows the possibility that surgical intervention for VV improves cardiac function.
Conclusion
Intervention for varicose veins of lower extremities is clinically useful for the improvement of cardiac function.
Disclosure Statement
There is no conflict of interest for this article.
References
- 1).De Backer G. Epidemiology of chronic venous insufficiency. Angiology 1997; 48: 569-76. [DOI] [PubMed] [Google Scholar]
- 2).Carpentier P, Priollet P. Epidemiology of chronic venous insufficiency. Presse Med 1994; 23: 197-201. [PubMed] [Google Scholar]
- 3).Fowkes FG, Evans CJ, Lee AJ. Prevalence and risk factors of chronic venous insufficiency. Angiology 2001; 52 Suppl. 1: S5-15. [DOI] [PubMed] [Google Scholar]
- 4).Cesarone MR, Belcaro G, Nicolaides AN, et al. ‘Real’ epidemiology of varicose veins and chronic venous diseases: the San Valentino Vascular Screening Project. Angiology 2002; 53: 119-30. [DOI] [PubMed] [Google Scholar]
- 5).Uema RT, Dezotti NR, Joviliano EE, et al. A prospective study of venous hemodynamics and quality of live at least five years after varicose vein stripping. Acta Cir Bras 2013; 28: 794-9. [DOI] [PubMed] [Google Scholar]
- 6).Priollet P. Essential varicose veins and chronic venous insufficiency. Rev Prat 1994; 44: 739-44. [PubMed] [Google Scholar]
- 7).Tamura K, Nakahara H. MR venography for the assessment of deep vein thrombosis in lower extremities with varicose veins. Ann Vasc Dis 2014; 7: 399-403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8).Nakamura M, Endo H, Nasu M, et al. Value of plasma B type natriuretic peptide measurement for heart disease screening in a Japanese population. Heart 2002; 87: 131-5. [DOI] [PMC free article] [PubMed] [Google Scholar]