Abstract
The laryngeal mask airway (LMA) Protector™ is a second-generation perilaryngeal sealer type supraglottic airway device recently introduced into clinical practice. We describe our initial experiences with the use of the LMA Protector™ in three patients undergoing laparoscopic cholecystectomies. In all patients, we found the LMA Protector™ to have acceptable placements on the first attempt, adequate oropharyngeal leak pressures and ventilation adequacy.
Keywords: Airway management, case report, laparoscopic, laryngeal masks
INTRODUCTION
Supraglottic airway devices (SADs) have been widely popular in the past three decades ever since the prototypical laryngeal mask airway (LMA) Classic™ was described in 1983.[1] Many anaesthesiologists today are comfortable with the routine use of SADs for general anaesthesia, as well as advanced uses in selected surgeries such as laparoscopic cholecystectomy.[2] In this context, concerns exist regarding the risk of aspiration and inadequate ventilation from positive pressure ventilation with SADs.
The LMA Protector™ (Teleflex Medical, Co. Westmeath, Ireland) is a single-use second-generation SAD designed with a large volume conduit with gastric access and a fixed curved structure to facilitate insertion.[3] The medical grade silicon inflatable cuff has been constructed for a primary oropharyngeal seal and distal oesophageal seal, potentially improving the ability of the LMA Protector™ in providing positive pressure ventilation and preventing aspiration. An image with labels of the LMA Protector™ showcasing its essential features has been included [Figure 1].
Figure 1.
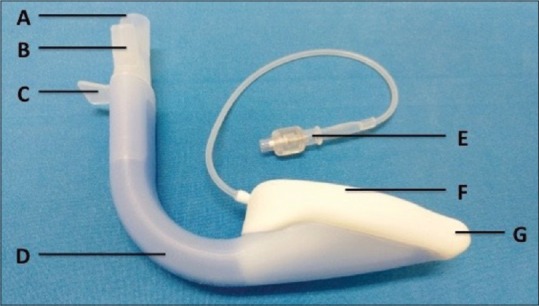
An image portraying the essential features of the laryngeal mask airway Protector™. A: Ventilation channel, B: Dual gastric channels, C: Securement tab, D: Preformed curvature, E: Inflation pilot balloon, F: Medical grade silicone cuff, G: Distal oesophageal seal
Currently, there is a paucity of literature detailing the use of the novel LMA Protector™ in the clinical domain, with only one published study at the time of writing.[4] The available literature does not address laparoscopic surgery at the time of this case report. In this report, we describe the successful use of the LMA Protector™ in three patients scheduled for elective laparoscopic cholecystectomy conducted in a tertiary hospital based in Singapore. Placement and performance tests were evaluated as per guidance provided by Timmermann et al.[5]
CASE REPORT
All three patients, American Society of Anesthesiologists Physical Status II with normal body mass indices (24.7–26.2 kg/m2) and no clinical features predictive of a difficult airway, underwent elective laparoscopic cholecystectomy. Written patient consent was obtained from all patients for publication of this case report.
Continuous electrocardiogram, non-invasive blood pressure, pulse oximeter, capnogram, temperature and train-of-four neuromuscular monitoring were placed for all patients. In all three patients, general anaesthesia and muscle relaxation were induced by weight-adjusted intravenous administration of propofol, fentanyl, midazolam, lignocaine and rocuronium. The LMA Protector™ was placed atraumatically after induction of anaesthesia on the first attempt in all patients by an experienced anaesthesiologist. Patient A received a size four LMA whereas patients B and C had size five LMAs. All three LMAs were inflated to 60 cmH2O intracuff pressure using manometers as outlined by a published randomised controlled trial.[6] Once the train-of-four ratio was 0, a size 4.0 mm flexible video endoscope was used to grade the laryngeal view through the LMA Protector™ and verify its correct placement in situ. In all three cases, a Cormack Lehane grade 2 (with partial downfolding of the epiglottis) equivalent laryngeal view was obtained [Figure 2]. Gastric tube insertions were successful on the first attempt for all patients with no resistance encountered.
Figure 2.
Laryngeal views of each patient obtained using flexible bronchoscopy. In all patients, a Grade 2 equivalent laryngeal view was obtained
Maintenance of anaesthesia was achieved through inhalational sevoflurane. Multimodal analgesia was administered including intravenous acetaminophen and parecoxib at the start of surgery and titrated doses of intravenous morphine intraoperatively. Prophylactic anti-emetics such as dexamethasone and ondansetron were administered. Abdominal insufflation pressures and gas flows were maintained, using carbon dioxide, at 14–20 mmHg and 200–400 mL/min, respectively. Surgery proceeded uneventfully in all three cases, with each case lasting approximately 1–1.5 h.
Intraoperatively, peak pressures were 22, 19 and 21 cmH2O for patients A, B and C, respectively, with a minimal leak in the system of <50 mL. At the end of surgery, neuromuscular blockade was reversed with titrated doses of neostigmine and atropine administered intravenously. The patients were then transferred asleep and with the LMA Protector™ in situ to the post-anaesthesia care unit. After adequately responding to verbal commands, the LMA Protector™ was removed. Subsequently, all patients were discharged to the general ward for further management.
DISCUSSION
The LMA Protector™ is a second-generation perilaryngeal-sealer type SAD recently introduced into clinical practice. It has design features mooted to improve patient safety. Minimal published data currently exist regarding the safety and utility of the novel device for advanced indications of the LMA Protector™. We describe the successful use of the LMA Protector™ in three cases of laparoscopic cholecystectomies and report placement and performance test data.
Placement and performance tests are important parameters for the evaluation of SADs. These tests give the clinician the reassurance in mitigating the risks of aspiration and ensuring the success of positive pressure ventilation through the airway device to maintain normocapnia. In our preliminary assessment, the LMA Protector™ possessed oropharyngeal leak pressures and maximum minute ventilation of ranges 27–31 cmH2O and 15.1–21.8 L/min, respectively. These are above the thresholds of 25 cmH2O for oropharyngeal leak pressure and 12 L/min for maximum minute ventilation considered to reflect adequate clinical efficacy.[5] These values were comparable to those in Sng et al.'s preliminary assessment of the LMA Protector™ in 26 patients who had undergone minor gynaecological procedures requiring general anaesthesia and use of a SAD.[4] From previously published studies investigating the safety and efficacy of similar airway devices, the LMA Supreme™ had mean oropharyngeal leak pressures of 21 ± 5 cm H2O versus the LMA ProSeal™ of 25 ± 6 cm H2O (P < 0.001).[7]
In all three patients, the LMA Protector™ was successfully placed on the first attempt, and the subsequent insertion of gastric tube was performed with minimal difficulty. The correct placement of the device was later verified by the gastric tube ‘bubble’ test and flexible bronchoscopies as seen in Figure 2. The first time insertion success rates of the LMA Protector™ in this study are consistent with previous studies, further supporting the efficacious use of the LMA Protector™.[4] This device is, therefore, a promising alternative to the LMA Supreme™ and the LMA ProSeal™ - with 98% and 88% success rates on first-attempt insertions, respectively.[7] Our experience with the LMA Protector™ concurs with the study by Maltby et al. where they found that the LMA ProSeal™ provided equally effective oxygenation and ventilation when compared with tracheal intubation in a prospective randomised controlled trial of non-obese patients scheduled for laparoscopic cholecystectomies.[8] Between the LMA Protector™ and LMA ProSeal™, we opined that the LMA Protector™ is superior given that the trachea can be intubated directly using the bronchoscope without the need for intermediary devices such as the Aintree Intubation Catheter. The preformed curvature of the LMA Protector™ allows easier intubation, the presence of a reservoir with dual suction ports leads to greater prophylaxis against gastric aspiration, and the similar, if not higher, oropharyngeal leak pressures of the LMA Protector™ ensure better lung ventilation in laparoscopic surgeries. Nevertheless, we recognise the limitations of our case report where the sample size is small, and the patients are without risk factors such as difficult airway and obesity. However, we hope that this case report of our initial experience may highlight the utility of the LMA Protector™ as an alternative to other SADs and motivate future research.
CONCLUSION
We report our experiences with the new second-generation perilaryngeal sealer LMA Protector™ in laparoscopic cholecystectomy, which was found to have acceptable placements on the first attempt, adequate oropharyngeal leak pressures and relatively high minute ventilation.
Financial support and sponsorship
Nil.
Conflicts of interest
Leng Zoo Tan was sponsored by Teleflex, a training trip to Germany to learn about the laryngeal mask airway Protector™ from Professor Friedrich Pühringer: Professor and Chairman of the Department of Anaesthesiology and Intensive Care Medicine at the Klinikum am Steinenberg in Reutlingen on 12th April 2016. Leng Zoo Tan has agreed to this arrangement to learn the correct usage of the laryngeal mask airway Protector™, which was a novel product at that point in time. The laryngeal mask airway Protector™ used for the case report was also provided free by Teleflex. This was necessary as the laryngeal mask airway Protector™ was not available for purchase at the point of the case report. Leng Zoo Tan did not, at any time, receive payment for any aspect of the submitted work.
REFERENCES
- 1.Brain AI. The laryngeal mask – A new concept in airway management. Br J Anaesth. 1983;55:801–5. doi: 10.1093/bja/55.8.801. [DOI] [PubMed] [Google Scholar]
- 2.Beleña JM, Ochoa EJ, Núñez M, Gilsanz C, Vidal A. Role of laryngeal mask airway in laparoscopic cholecystectomy. World J Gastrointest Surg. 2015;7:319–25. doi: 10.4240/wjgs.v7.i11.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Van Zundert AA, Skinner MW, Van Zundert TC, Luney SR, Pandit JJ. Value of knowing physical characteristics of the airway device before using it. Br J Anaesth. 2016;117:12–6. doi: 10.1093/bja/aew106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sng BL, Ithnin FB, Mathur D, Lew E, Han NR, Sia AT. Apreliminary assessment of the LMA protector™ in non-paralysed patients. BMC Anesthesiol. 2017;17:26. doi: 10.1186/s12871-017-0323-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Timmermann A, Bergner UA, Russo SG. Laryngeal mask airway indications: New frontiers for second-generation supraglottic airways. Curr Opin Anaesthesiol. 2015;28:717–26. doi: 10.1097/ACO.0000000000000262. [DOI] [PubMed] [Google Scholar]
- 6.Seet E, Yousaf F, Gupta S, Subramanyam R, Wong DT, Chung F. Use of manometry for laryngeal mask airway reduces postoperative pharyngolaryngeal adverse events: A prospective, randomized trial. Anesthesiology. 2010;112:652–7. doi: 10.1097/ALN.0b013e3181cf4346. [DOI] [PubMed] [Google Scholar]
- 7.Seet E, Rajeev S, Firoz T, Yousaf F, Wong J, Wong DT, et al. Safety and efficacy of laryngeal mask airway Supreme versus laryngeal mask airway ProSeal: A randomized controlled trial. Eur J Anaesthesiol. 2010;27:602–7. doi: 10.1097/eja.0b013e32833679e3. [DOI] [PubMed] [Google Scholar]
- 8.Maltby JR, Beriault MT, Watson NC, Liepert D, Fick GH. The LMA-ProSeal™ is an effective alternative to tracheal intubation for laparoscopic cholecystectomy. Can J Anaesth. 2002;49:857–62. doi: 10.1007/BF03017420. [DOI] [PubMed] [Google Scholar]



