Abstract
Hepatitis C virus is associated with several immune-mediated phenomena, presented usually as extra-hepatic hepatitis C manifestations. A predisposition to autoimmunity associated with the presence of baseline autoantibodies has been demonstrated in interferon mediated autoimmune diseases. We report a male patient, 34 years old, with genotype 1, chronic hepatitis C (hepatitis C viremia 1.432.463 UI/mL) and family history of psoriasis. He had high levels of transaminases and immunology showed positive antinuclear antibodies (1/320) and anti-smooth-muscle antibodies, with elevated immunoglobulin G (1740 mg/dL). Liver biopsy revealed a F1/2 Metavir score, histologic activity index of 3 and mild piecemeal necrosis. Antiviral treatment was started with peg-interferon α2a 180 mcg plus ribavirin 1200 mg, and the patient had rapid virologic response, normalization of transaminases, negativation of antinuclear antibodies positivity and decrease of immunoglobulin levels. However, at week 22, he developed psoriatic-like eczema and arthritis with functional limitation. Due to suspicion of latent psoriatic arthritis not previously diagnosed, he was started on methotrexate 10 mg/weekly with improvement of psoriatic plaques, arthritis and functional limitation. Patient achieved sustained virologic response, with normal transaminases and no significant changes in immunology. Post-treatment median hepatic elastography was 3.6 kPa. Autoimmunity in hepatitis C infection is not limited to surrogate autoantibody seropositivity, but may embrace the full spectrum of autoimmune disorders.
Keywords: Hepatitis C, Autoantibodies, Psoriasis, Interferons, Hepacivirus
Resumo
O vírus da hepatite C associa-se a diversos fenómenos de auto-imunidade, apresentando-se geralmente como manifestações extra-hepáticas da hepatite C. Uma predisposição para auto-imunidade associada à presença de auto-anticorpos foi demonstrada em doenças auto-imunes mediadas pelo Interferão. Descrevemos um doente do sexo masculino, 34 anos, com hepatite C crónica, genótipo 1 (viremia 1.432.463 UI/mL) e história familiar de psoríase. Apresentava transaminases elevadas e imunologia positiva para anticorpos antinucleares (1/320) e anti-musculo liso, com imunoglobulina G elevada (1740 mg/dL). A biópsia hepática revelou um score Metavir F1/2, índice de actividade histológica de 3 e necrose piecemeal ligeira. Foi iniciado tratamento antivírico com Interferão peguilado α-2a 180 mcg e Ribavirina 1200 mg, com resposta virológica rápida e normalização das transaminases, com negativação dos anticorpos antinucleares e diminuição dos níveis de imunoglobulina G. Contudo, à semana 22, apresentou eczema do tipo psoriático e artrite com limitação funcional. Devido à suspeita de artrite psoriática latente não diagnosticada previamente, iniciou tratamento com Metotrexato 10 mg/semana com melhoria das placas de psoríase, artrite e limitação funcional. O doente alcançou resposta virológica sustentada, com transaminases normais, sem alterações significativas da imunologia. A elastografia hepática mediana pós-tratamento foi de 3.6 kPa. A auto-imunidade na Hepatite C não está limitada à seropositividade dos auto-anticorpos, podendo abranger todo o espectro de doenças auto-imunes.
Palavras-chave: Hepacivírus, Hepatite C, Interferons, Psoríase
1. Introduction
Approximately 3% of the world population is chronically infected with hepatitis C virus (HCV).1 It is associated with several immune-mediated phenomena; the association between serological findings suggestive of autoimmune disease and HCV is well known. Antinuclear antibodies (ANA), smooth-muscle antibodies (ASMA) and liver-kidney microssome 1 (LKM1) are detected in 25–30% of HCV patients.2 The mechanism responsible for seropositivity for these autoantibodies is not completely understood. Molecular mimicry of viral antigens by self-antigens, chronic stimulation of B cells, and a bystander effect are some proposed mechanisms for the development of autoimmune phenomena in hepatitis C.3
Patients with features of both autoimmune hepatitis (AIH) and HCV should be carefully evaluated, because immunosuppressive treatment may have deleterious effects on chronic hepatitis C (CHC). Conventional therapy of HCV consists of pegylated interferon-α (IFN-α) combined with ribavirin (RBV) and possibly a direct acting antiviral (DAA) agent depending on genotype.4 IFN-α has been reported to cause drug-induced AIH,5 however, it is unclear whether it unmasks, induces or simply causes liver injury with autoimmune features. HCV alone can trigger autoimmune processes; in addition, IFN-α exerts various immunomodulatory effects that may further facilitate this autoimmune phenomenon.6 Diagnosing AIH in patients with HCV is difficult on the basis of scoring systems because several serological and histological findings, which are incorporated in the diagnostic criteria, can also be observed in HCV.7 In HCV patients with AIH features, a definitive diagnosis of AIH should be made based on a combination of autoantibody profiles, histological findings, and therapy response and outcome.
An association between HCV and psoriasis has previously been reported and a recent epidemiological survey confirmed a higher prevalence of HCV infection in psoriatic patients. Psoriasis induction by IFN-α is a rare complication of HCV treatment, first noted in 1993.8 Since then, there have been 41 cases in the worldwide literature.
A predisposition to autoimmunity associated with the presence of baseline autoantibodies has been demonstrated in IFN-mediated autoimmune diseases9 and immunological alterations associated with HCV may constitute a predisposing factor in the onset of the disease in IFN-α treated patients.10 Besides that, there is still a question whether HCV itself can be one of the inducing factors for psoriasis.11 This case report tries to explore the difficulties in the differential diagnosis between HCV and AIH, as well as the clinical significance of autoantibodies in the development of autoimmune manifestations, like psoriasis.
2. Case report
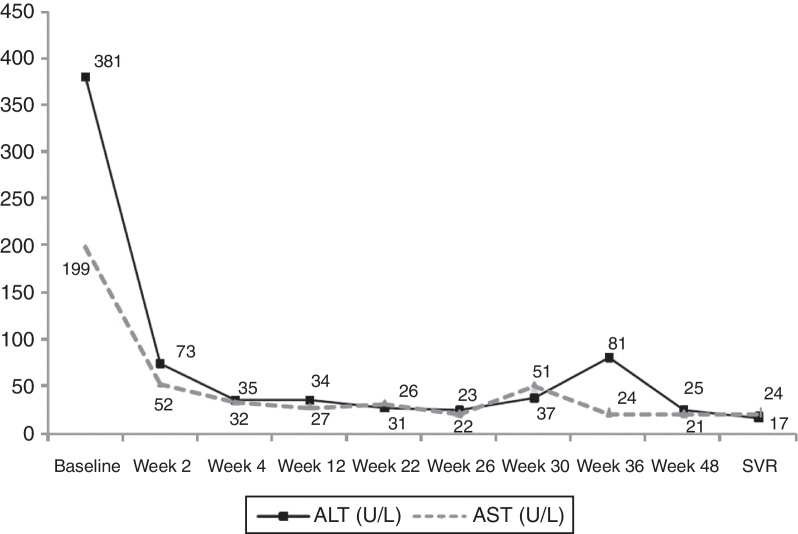
A male patient, 34 year-old, was referred to the Hepatology outpatient clinic due to positive serology against HCV (anti-HCV). He had a past medical history of intravenous drug addiction between 1994 and 1998, pulmonary tuberculosis (treated) in 1997, and alcohol consumption (less than 20 g/day). The patient was asymptomatic and there was a family history (grandfather) of psoriasis. Laboratory analysis showed increased aspartate aminotransferase (AST) 5 times upper limit of normal (ULN) and alanine aminotransferase (ALT) 10 times ULN. HCV-RNA detected by polymerase chain reaction (PCR) was 1.432.463 UI/mL. HCV genotype was 1, with undetermined subtype. Immunology showed positive ANA (1/320) and ASMA, with elevated immunoglobulin G (IgG) (1.2 times ULN). Anti-mitochondrial antibody, anti-liver kidney microsomal antibody and anti-neutrophil cytoplasmic antibody were negative. Tests for iron, copper metabolic disorders, alpha1 antitrypsin and complement were normal. Thyroid function tests were also normal. The abdominal ultrasound was normal. A liver biopsy was performed for differential diagnosis with AIH. Trabecular architecture was preserved with mild to moderate portal fibrosis with focal fibrous septa. There was portal inflammatory infiltrate, predominantly mononucleate with lymphoid aggregates, mild piecemeal necrosis and moderate intra-lobular necro-inflammatory activity with no other significant changes (Fig. 1). AIH score without treatment was 3 (probable if > or = 10) and simplified score was 5 (probable if > or = 6). Treatment was started with peg-IFN α2a 180 mcg plus RBV 1200 mg, under close monitoring of liver biochemistry during the initial weeks. The patient achieved a fast normalization of transaminases, rapid virologic response (RVR), negativation of ANA positivity and decrease of IgG levels. At week 22, he sought his clinician due to a psoriatic-like eczema and arthritis (Fig. 2) with functional limitation. Due to suspicion of latent psoriatic arthritis not previously diagnosed, the patient was evaluated by Rheumatology and started methotrexate (MTX) 10 mg/weekly plus calcipotriol hydrate and bethametasone dipropionate with dose reduction of peg-IFN to 135 mcg. At week 28, patient referred partial improvement of psoriatic plaques, arthritis and functional limitation, with dose intensification of MTX to 15 mg/weekly and complete improvement of symptomatology. At week 30, there was an increase of transaminases to 2 times ULN. As HCV viremia remained negative, and there was no evidence of immunological flare, MTX dose was decreased to the initial scheme, with normalization of transaminases, and the patient managed to complete 48 weeks of antiviral therapy. The patient achieved sustained virologic response (SVR), with no significant changes in immunology and normal transaminases (Fig. 3). Post-treatment median hepatic elastography fibroscan was 3.6 kPa. The patient is asymptomatic without relapse of psoriasis even after suspension of MTX and topic therapy.
Figure 1.
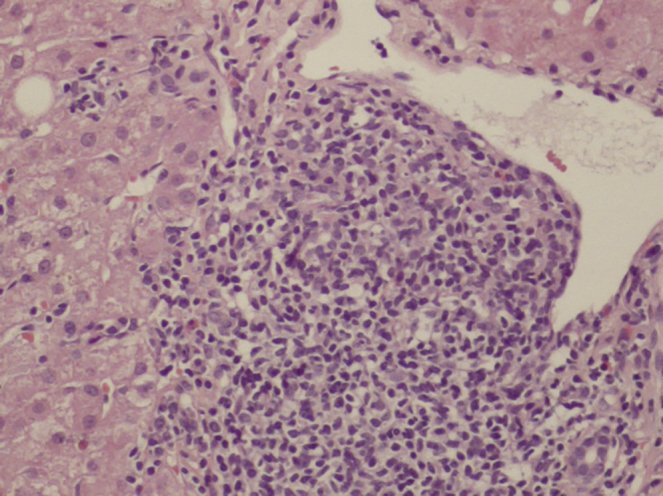
Liver histology showed portal inflammatory infiltrate, predominantly mononucleate with lymphoid aggregates, mild piecemeal necrosis and moderate intra-lobular necro-inflammatory activity.
Figure 2.

Hands of the patient with psoriatic-like eczema and arthritis.
Figure 3.
Evolution of aspartate aminotransferases (AST) and alanine aminotransferases (ALT) during 48 weeks of hepatitis C treatment with peg-interferon plus ribavirin; methotrexate was started at week 22, with dose intensification at week 28; at week 30, methotrexate dose was decreased to the initial scheme.
3. Discussion
HCV infection is one of the main causes of chronic liver disease worldwide. Patients found to be anti-HCV positive, should have their HCV genotype and RNA level determined, and a liver biopsy should be considered to assess the degree of fibrosis. Validated, non invasive methods, as hepatic elastography, can be also used for staging, however, in the reported patient, liver biopsy was preferred due to the level of increase in ALT, which has been shown to overestimate liver stiffness. Biopsy was also done to exclude an autoimmune disorder that would contraindicate treatment. Treatment should be individualized and considered for all CHC patients. HCV infection tends to induce non-specific autoimmune reactions, as demonstrated by the high prevalence of various non-organ-specific autoantibodies, usually in low titers.12 Classic HCV infection generally is not characterized by prominent plasma cell infiltration on liver biopsy, a feature that is often prominent in AIH. In addition, patients with AIH may have marked elevations in serum IgG, a feature that is unusual in patients with HCV.13 The current guidelines recommend that the autoimmune profile namely ANA should be assessed in chronic HCV patients before the treatment decision with IFN and RBV and consider the presence of active autoimmune disorders as a contraindication for treatment. In our case, serum IgG was only mildly elevated and hepatic histology did not show a prominent plasma cell infiltration. Even though current guidelines recommend the association of conventional therapy with a NS3 protease inhibitor agent in genotype 1, there are no recommendations in patients with possible characteristics of autoimmunity, but it could be expected that a shorter duration of IFN-α would be beneficial.
Autoimmunity in HCV infection is not limited to autoantibody seropositivity, but embraces the full spectrum of autoimmune disorders.14 In previous reports of new onset or exacerbation of psoriasis after interferon therapy, it usually occurred 4 weeks after the initiation of treatment and cessation of medication was often needed. In most reported cases of IFN-α induced new onset or exacerbation of plaque-type psoriasis, cessation of IFN-α therapy has often been suggested,15 once dose reductions of IFN-α do not seem to help prevent such occurrences.16 Phototherapy is generally considered in these patients, however, there have been several reports of liver injury after PUVA therapy. MTX is not recommended for the treatment of psoriasis in patients with HCV due to an increased risk for hepatotoxicity. In our case, the patient manifested psoriatic arthritis at week 22; even though RVR was achieved, abbreviated treatment (24 weeks) could not be considered once he had high baseline HCV-RNA.4 Considering that, we chose to maintain treatment with a reduced dosage of peg-IFN (135 mcg/weekly), in an attempt to reduce the immunomodulatory effects exerted by IFN-α that may further facilitate this autoimmune phenomenon, even though there are no current recommendations. MTX was initiated, together with Rheumatology, and was well tolerated only with a transaminases flare 8 weeks after, that improved after MTX dose reduction. We chose to repeat the immune panel by the time of the transaminases elevation due to fear of an auto-immunity flare triggered by IFN-α, and also excluded HCV breakthrough due to reduced peg-IFN dosage and immunosupression.
Psoriasis is a rare complication of IFN-α treatment. A predisposition to autoimmunity associated with the presence of baseline autoantibodies has been demonstrated in previous studies. We report a case that tries to explore the difficulties in the differential diagnosis between HCV and AIH, as well as the clinical significance of autoantibodies in the development of autoimmune manifestations, like psoriasis. Numerous phase 2 and 3 studies are underway assessing the effectiveness and cutaneous side-effects of IFN-free regimens for the treatment of HCV infection. The incidence of psoriasis onset and worsening with IFN-free regimens is not yet available, but may be lower than the incidence with IFN-α treatment. Also, IFN-free regimens will probably avoid the potential of aggravating a real AIH associated with CHC. IFN-free regimens may become the preferred treatment for hepatitis C in patients with psoriasis and other autoimmune diseases.
Ethical disclosures
Protection of human and animal subjects
The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data
The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent
The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interest
The authors have no conflicts of interest to declare.
References
- 1.Lavanchy D. The global burden of hepatitis C. Liver Int. 2009;29:74–81. doi: 10.1111/j.1478-3231.2008.01934.x. [DOI] [PubMed] [Google Scholar]
- 2.Bianchi F.B., Muratori P., Granito A., Pappas G., Ferri S., Muratori L. Hepatitis C and autoreactivity. Dig Liver Dis. 2007;39:S22–S24. doi: 10.1016/s1590-8658(07)80006-5. [DOI] [PubMed] [Google Scholar]
- 3.Ferri S., Muratori L., Lenzi M., Granito A., Bianchi F.B., Vergani D. HCV and autoimmunity. Curr Pharm Des. 2008;14:1678–1685. doi: 10.2174/138161208784746824. [DOI] [PubMed] [Google Scholar]
- 4.Ghany M.G., Nelson D.R., Strader D.B., Thomas D.L., Seeff L.B. An update on treatment of genotype 1 chronic hepatitis C virus infection: 2011 practice guideline by the American Association for the Study of Liver Diseases. Hepatology. 2011;54:1433–1444. doi: 10.1002/hep.24641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Krawitt E.L. Autoimmune hepatitis. N Engl J Med. 2006;354:54–66. doi: 10.1056/NEJMra050408. [DOI] [PubMed] [Google Scholar]
- 6.Kontorinis N., Agarwal K., Elhajj N., Fiel M.I., Schiano T.D. Pegylated interferoninduced immune-mediated hepatitis post-liver transplantation. Liver Transpl. 2006;12:827–830. doi: 10.1002/lt.20706. [DOI] [PubMed] [Google Scholar]
- 7.Mauss S., Berger F., Schober A., Moog G., Heyne R., John C. Screening for auto-antibodies in chronic hepatitis C patients has no effect on treatment initiation or outcome. J Viral Hepat. 2013;20:72–77. doi: 10.1111/jvh.12011. [DOI] [PubMed] [Google Scholar]
- 8.Garcia-Lora E. Interferon-induced psoriasis in a patient with chronic hepatitis C. Dermatology. 1993;187:280. doi: 10.1159/000247266. [DOI] [PubMed] [Google Scholar]
- 9.Conlon K.C., Urba W.J., Smith J.W., 2nd, Steis R.G., Longo D.L., Clark J.W. Exacerbation of symptoms of autoimmune disease in patients receiving alpha-interferon therapy. Cancer. 1990;65:2237. doi: 10.1002/1097-0142(19900515)65:10<2237::aid-cncr2820651013>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 10.Lombardini F., Taglione E., Riente L., Pasero G. Psoriatic arthritis with spinal involvement in a patient receiving alpha-interferon for chronic hepatitis C. Scand J Rheumatol. 1997;26:58–60. doi: 10.3109/03009749709065666. [DOI] [PubMed] [Google Scholar]
- 11.Palazzi C., Olivieri I., D’Amico E., D’Agostino L., Nicolucci A., Pennese E. virus infection in psoriatic arthritis. Arthritis Rheum. 2005;53(2):223–225. doi: 10.1002/art.21079. [DOI] [PubMed] [Google Scholar]
- 12.Cojocaru M., Cojocaru I., Iacob S. HCV infection-related autoimmunity. Mædica J Clin Med. 2007;2:230–236. [Google Scholar]
- 13.Cassani F., Cataleta M., Valentini P., Muratori P., Giostra F., Francesconi R. Serum autoantibodies in chronic hepatitis C: comparison with autoimmune hepatitis and impact on the disease profile. Hepatology. 1997;26:561. doi: 10.1002/hep.510260305. [DOI] [PubMed] [Google Scholar]
- 14.Peterson J.R., Hsu F.C., Simkin P.A., Wener M.H. Effect of tumor necrosis factor alpha antagonists on serum transaminases and viraemia in patients with rheumatoid arthritis and chronic hepatitis C infection. Ann Rheum Dis. 2003;62:1078–1082. doi: 10.1136/ard.62.11.1078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Horev A., Halevy S. New-onset psoriasis following treatment with pegylated interferon-alpha 2b and ribavirin for chronic hepatitis C. Isr Med Assoc J. 2009;11:760–761. [PubMed] [Google Scholar]
- 16.Georgetson M.J., Yarze J.C., Lalos A.T., Webster G.F., Martin P. Exacerbation of psoriasis due to interferon-alpha treatment of chronic active hepatitis. Am J Gastroenterol. 1993;88:1756–1758. [PubMed] [Google Scholar]