Abstract
Objective
This analysis critically compares publications discussing complications and functional outcomes of plate fixation (PF) versus intramedullary fixation (IF) for midshaft clavicle fractures.
Methods
Relevant studies published between January 1990 and October 2014, without language restrictions, were identified in database searches of PubMed®, Medline®, Embase and the Chinese National Knowledge Infrastructure (CNKI). Studies that compared postoperative complications and functional outcomes between PF and IF for midshaft clavicle fractures, and provided sufficient data for analysis, were included in this meta-analysis.
Results
After strict evaluation, 12 studies were included in this meta-analysis. Studies encompassed 462 participants in the PF group and 440 in the IF group. Study participants were followed up for ≥1 year. Outcomes were superior with IF compared with PF in terms of shoulder constant score at 6-month follow-up, fewer symptomatic hardware complications, lower rate of refracture after hardware removal and less hypertrophic scarring. In other aspects, such as functional recovery at 12-months and 24-months, Disability of Arm, Shoulder and Hand (DASH) questionnaire results at 12-month follow-up, shoulder motion range, rates of superficial infection, temporary brachial plexus lesion, nonunion, malunion, delayed union, implant failure and need for major revision, both techniques were similar.
Conclusions
Findings of this meta-analysis suggest that, in many respects, IF was superior to PF for the management of midshaft clavicle fractures. This finding could aid surgeons in making decisions on the optimum internal fixation pattern for midshaft clavicular fractures.
Keywords: Midshaft clavicle fractures, intramedullary fixation, plate fixation, meta-analysis
Introduction
Clavicular fracture is a common injury, accounting for 2.6–10% of all fractures in adults.1–4 Approximately 80% of clavicular fractures involve the midshaft of the clavicle and >70% of midshaft clavicular fractures are displaced.4,5 Conservative treatment has been traditionally considered as ‘standard treatment’ for midshaft fractures even for displaced fractures, with the expectation that even severe radiographic malalignment would not influence functional results. However, a relatively high incidence (30%) of postoperative complications and deficits in functional recovery of the shoulder has been reported in patients originally treated with conservative regimens.6–8 With advancements in techniques and implants for fracture fixing, internal fixation is generally considered a better choice for these fractures than conservative treatment. Substantial controversy among surgeons regarding the optimal fixation pattern (plate fixation [PF] or intramedullary fixation [IF]) of these injuries exists and further research on better treatment options is needed.
To date, multiple forms of plating and intramedullary devices have been used to fix midshaft clavicle fractures, including precontoured dynamic compression plates (DCP), use of a reconstruction plate for PF and Knowles pinning, elastic stable intramedullary nailing with a Rockwood clavicle pin and an Acumed clavicle rod for IF9–12. PF is a popular technique providing a rigid fix, allowing early rehabilitation protocols.13 A precontoured plate, designed to parallel the S-shaped curve of the clavicle, has become a popular PF pattern. However, extensive soft-tissue dissection, implant prominence, postoperative infection, scarring, hardware failure and refracture after the removal of the plate are all negative factors for PF.14–17 With IF, the soft tissue envelope, periosteum and vascular integrity can be preserved,18,19 early hardware migration appears to be solved by an improved locked intramedullary device, but the issue of low biomechanical stability remains.20
Barlow et al.21 and Houwert et al.22 have conducted relevant systematic reviews comparing IF and PF methods of midshaft clavicle fracture repair, but with qualitative and equivocal conclusions. Duan et al.23 conducted a meta-analysis of randomized control trials (RCT), but only two studies were included comparing complications and functional outcomes between methods. Several original studies comparing different methods have since been published,15,24–28 which prompted this updated meta-analysis. Accordingly, the present analysis aimed to evaluate whether IF is better than PF in terms of postoperative complications and functional outcomes for the management of acute midshaft clavicle fractures.
Materials and methods
Search strategy
This meta-analysis was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (http://www.prisma-statement.org/statement.htm). An electronic literature search was performed in PubMed®, Medline®, Embase and the Chinese National Knowledge Infrastructure (CNKI), to identify relevant studies published between January 1990 and October 2014. The following keywords were used: ‘clavicular’ or ‘clavicle’ and ‘midshaft’ and ‘fracture’ and ‘intramedullary’ and ‘plate’ or ‘plating’ and ‘complications’ or ‘effectiveness’ or ‘results’ or ‘outcome’. A manual search of references in the included original articles or systematic reviews was also performed, to identify any potential additional studies.
Inclusion criteria
Two reviewers (H.G., T. Z.) independently evaluated the titles and abstracts of the identified papers. Only full text articles without language restriction were included in this meta-analysis. Disagreements were resolved through discussion; if they remained unresolved, a third reviewer was consulted. Inclusion criteria were RCTs or case–control or cohort studies comparing the outcomes of two methods for treating midshaft clavicular fractures, at least one set of results in each paper had to be original, the age of participants in both groups had to be <65 years (young, active participants), participants in studies were followed up for ≥12 months and sufficient data were provided to estimate the odds ratio (OR) or standardized mean difference (SMD) with 95% confidence intervals (CIs).
Quality assessment and data extraction
The quality of studies was evaluated by the tool recommended in the Cochrane Handbook 5.1.0: ‘The Cochrane collaboration’s tool for assessing risk of bias’, which was used by Fang et al.29 This scale includes six major potential sources of bias, including sequence generation, allocation concealment, blinding, incomplete data, selective outcome reporting and other outcomes reporting. Data were carefully and independently abstracted from eligible studies by the same two reviewers (H.G., T.Z.). The following basic characteristics were abstracted from each study: first author’s name; publication year; patients’ age and sex; follow-up duration; definition and numbers in each IF and PF group; the number of studies providing information for each surgical method.
Statistical analyses
Odds ratios and 95% CI were estimated and pooled across studies to assess for any differences between the two methods. A P-value < 0.05 was considered significant. Heterogeneity among studies was tested by Q-statistics, with significance set at P < 0.1030 and further measured by I2 statistics, with I2 > 50% indicating significant inconsistency. A random-effects model was used to calculate pooled ORs in the case of significant heterogeneity (P < 0.10 or I2 > 50%); otherwise, a fixed-effects model was used.31 The outcome of the meta-analysis for variables was summarized graphically using forest plots. Publication bias was assessed and presented using funnel plots. For any variable presenting with large heterogeneity, a sensitivity analysis, excluding outlier studies, was conducted to investigate the source of heterogeneity. All analyses were performed using Stata® software, version 11.0 (Stata Corp., College Station, TX, USA).
Results
Basic information
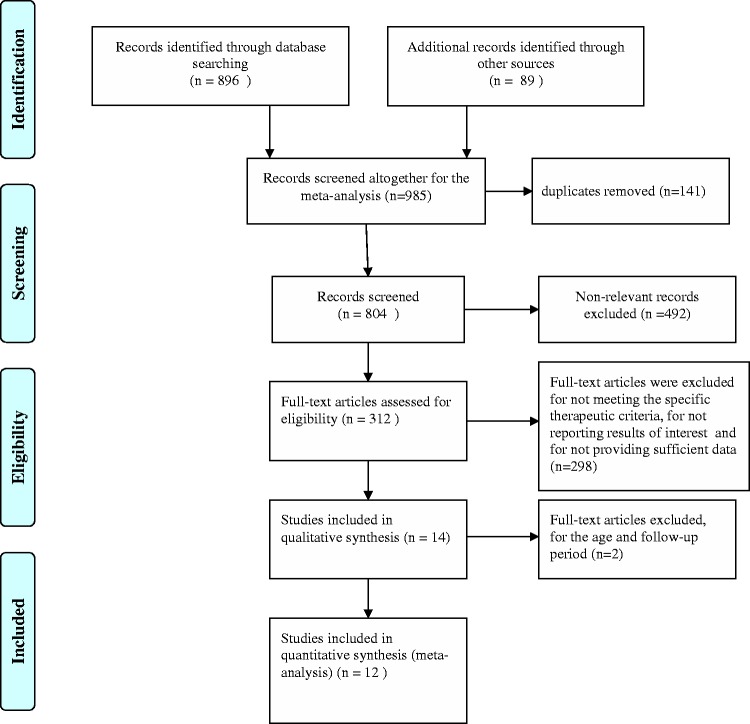
The initial database search yielded 985 papers: 673 were excluded as they were in an inappropriate format (e.g. abstracts, letters, meeting reports, same data reported at different time-points); 193 were excluded for not meeting the specific therapeutic methods according to the study criteria; 76 were excluded as the reported results were outside the interest of this study; 29 were excluded as they did not provide sufficient data for the meta-analysis; one study was excluded as its follow-up period was too short (mean of 5.9 months);32 one study was excluded as its participants were not within the specified age criteria.33 The remaining 12 studies were eligible and were included in this meta-analysis. The search procedure is presented in Figure 1.
Figure 1.
Flow diagram of literature search strategy to identify manuscripts to compare complications and functional outcomes of plate fixation (PF) or intramedullary fixation (IF) for midshaft clavicle fractures, according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
The 12 original articles included were published between 1999 and 2014. A total of 440 patients from these 12 studies had undergone IF; 462 had undergone PF. In each study, patients treated by each method were similar in terms of sex, side involved and injury mechanism. In two studies, patients treated with PF were significantly older than those treated with IF,28,34 whereas in the other included studies, the age between the two groups was similar. A summary of basic characteristics is listed in Table 1.
Table 1.
Basic characteristics of participants and details of the 12 studies included in a meta-analysis comparing intramedullary fixation (IF) with plate fixation (PF) for midshaft clavicle fracture.
| Author | Country, region | Publication year | IF n | PF n | IF age (range) | PF age (range) | IF, M/F | PF, M/F | Follow-up, months |
|---|---|---|---|---|---|---|---|---|---|
| Narsaria | India | 2014 | 33 | 32 | 38.9 ± 9.1 (20–62) | 40.2 ± 11.2 (18–64) | 24/9 | 26/6 | >24 |
| Liu35 | China, Taiwan | 2010 | 51 | 59 | 33.6 ± 13.5 | 31.7 ± 9.7 | 32/19 | 29/30 | >12 |
| Fu25 | China, Taiwan | 2012 | 53 | 50 | 35.2 ± 14.5 | 39.9 ± 14.8 | 38/15 | 33/17 | >12 |
| Ko36 | Republic of Korea | 1999 | 13 | 18 | 36.6 (23–68) | 43.3 (18–74) | NP | NP | >12 |
| Lee J26 | USA | 2014 | 43 | 67 | 27.6 (14–59) | 31.7 (16–68) | 29/5 | 63/4 | >15 |
| Wenninger27 | USA | 2013 | 33 | 29 | 25.2 (18–51) | 26.9 (20–49) | 32/1 | 26/3 | >12 |
| Assobhi34 | Egypt | 2011 | 19 | 19 | 30.3 ± 4.8 (24–45) | 32.6 ± 5.9 (26–49) | 16/3 | 17/2 | >12 |
| Wijdicks28 | The Netherlands | 2012 | 47 | 43 | 33.1 ± 15.6 | 39.4 ± 14.1 | 33/14 | 33/10 | >12 |
| Ferran43 | UK | 2010 | 17 | 15 | 23.8 (13–42) | 35.4 (16–53) | 14/3 | 13/2 | 12.4 (mean) |
| Kleweno39 | USA | 2011 | 18 | 14 | 35 (16–56) | 28 (16–46) | 15/3 | 10/4 | >12 |
| Chen15 | China | 2012 | 57 | 84 | 34.3 (20–59) | 36.5 (19–63) | 41/16 | 61/23 | >24 |
| Lee Y18 | China, Taiwan | 2008 | 56 | 32 | 40.1 | 38.2 | 37/19 | 20/12 | >12 |
PF, plate fixation; IF, intramedullary fixation; M, male patients; F, female patients.
A detailed quality assessment of the included studies is presented in Table 2.
Table 2.
Methodological assessment of articles included in a meta-analysis comparing intramedullary fixation (IF) with plate fixation (PF) for midshaft clavicle fracture using the Cochrane collaboration tool for assessing risk of bias.
| Reference | Random sequence generation | Allocation concealment | Blinding | Incomplete outcome data | Free of selective reporting | Free of other bias |
|---|---|---|---|---|---|---|
| Narsaria, 201424 | Yes | Yes | Unclear | Yes | Yes | Yes |
| Liu, 201035 | No | Unclear | Yes | Yes | Yes | Unclear |
| Fu, 201225 | No | Unclear | Yes | Yes | Yes | Unclear |
| Ko, 199936 | Yes | Unclear | Unclear | Yes | Yes | No |
| Lee J, 201426 | Unclear | Yes | Unclear | Yes | Yes | Yes |
| Wenninger, 201327 | Yes | Unclear | Yes | Yes | Yes | Unclear |
| Assobhi, 201134 | No | Yes | Yes | Unclear | Yes | No |
| Wijdicks, 201228 | Yes | Yes | Yes | Yes | Yes | No |
| Ferran, 201043 | No | Unclear | Unclear | Yes | Yes | Yes |
| Kleweno, 201139 | Yes | Yes | Yes | Yes | Yes | No |
| Chen, 201215 | No | Unclear | Yes | Yes | Yes | No |
| Lee Y, 200818 | Yes | Yes | Unclear | Unclear | Yes | Yes |
Yes’, low risk of bias; ‘Unclear’, unclear risk of bias; ‘No’, high risk of bias.
Postoperative complications
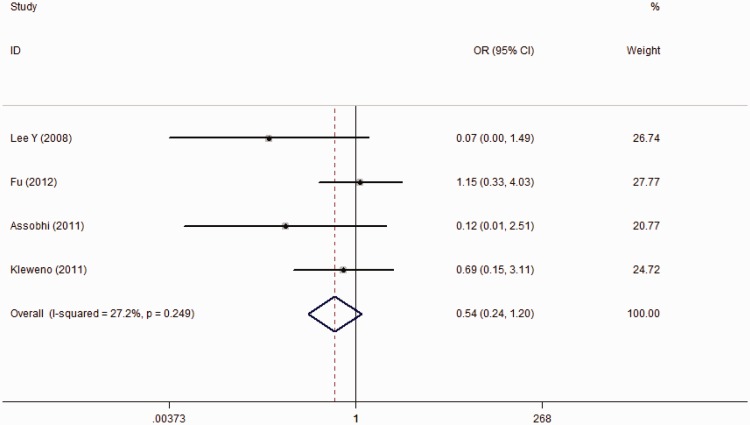
Total complications were reported in four studies involving 146 IF patients and 115 PF patients. The PF group yielded a slightly higher incidence of total complications than the IF group (13.9% versus 7.5%), but the combined result did not reach significance (OR 0.54; 95% CI 0.24, 1.20; Figure 2).
Figure 2.
Forest plot for total complications, reported in four studies involving 146 intramedullary fixation (IF) patients and 115 plate fixation (PF) patients with midshaft clavicle fractures; overall, I2 = 27.2%, P = not significant.
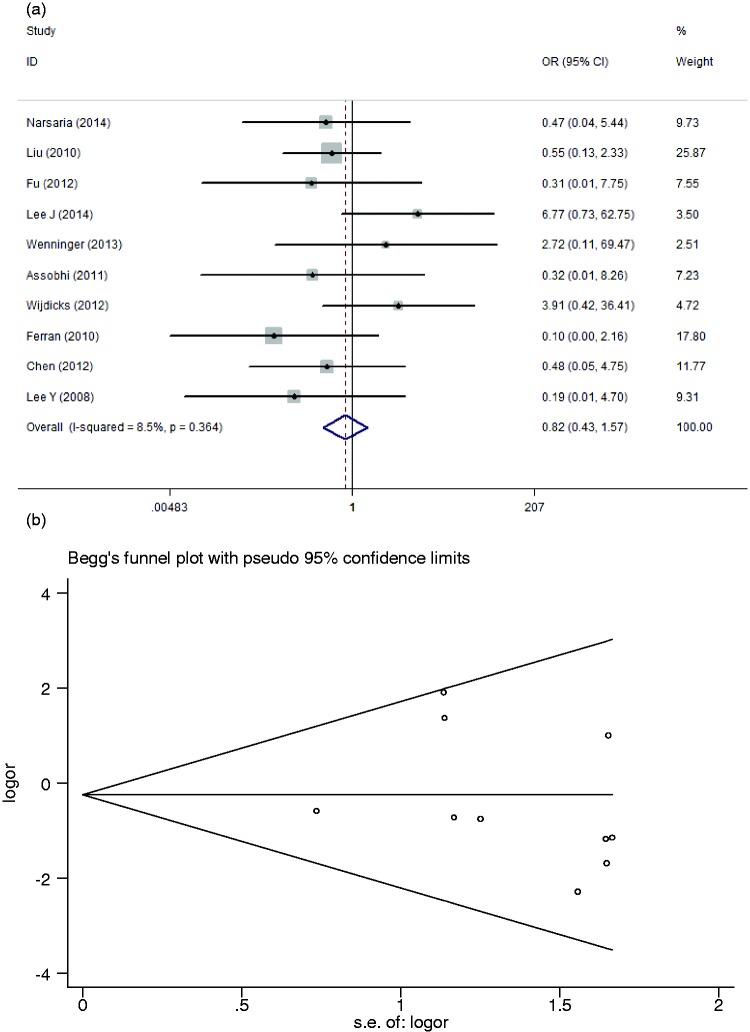
Postoperative superficial infection was reported in ten studies encompassing 409 IF patients and 430 PF patients; overall, 14 (3.4%) and 19 (4.4%) patients, respectively, were infected shortly after surgery. Analysis for a combined outcome found no significant difference between surgical methods (OR 0.82; 95% CI 0.43, 1.57; Figure 3A), with little heterogeneity (I2 = 8.5%). Begg’s test showed no publication bias for this variable (Figure 3B).
Figure 3.
(A) Forest plot for superficial infection reported in 10 studies encompassing 409 intramedullary fixation (IF) patients and 430 plate fixation (PF) patients with midshaft clavicle fractures; I2 = 8.5%, P = not significant. (B)Begg’s funnel plot to assess publication bias of the included studies comparing the level of superficial infection between intramedullary fixation (IF) and plate fixation (PF) for midshaft clavicle fractures (P = not significant).
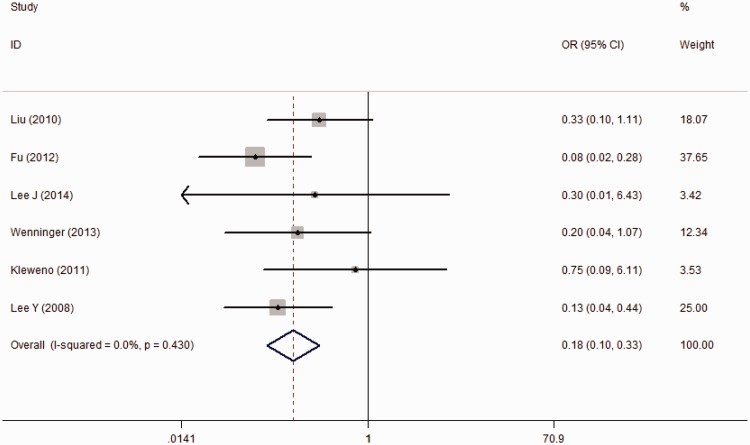
Six studies involving 251 IF patients and 254 PF patients reported postoperative symptomatic hardware, which was higher in the PF group (22.4%) than in the IF group (6.0%). This result was significant, without heterogeneity (OR 0.18; 95% CI 0.10, 0.33; Figure 4).
Figure 4.
Forest plot for six studies involving 251 intramedullary fixation (IF) patients and 254 plate fixation (PF) patients which reported postoperative symptomatic hardware during recovery from midshaft clavicle fracture; I2 = 0.0%, P = not significant.
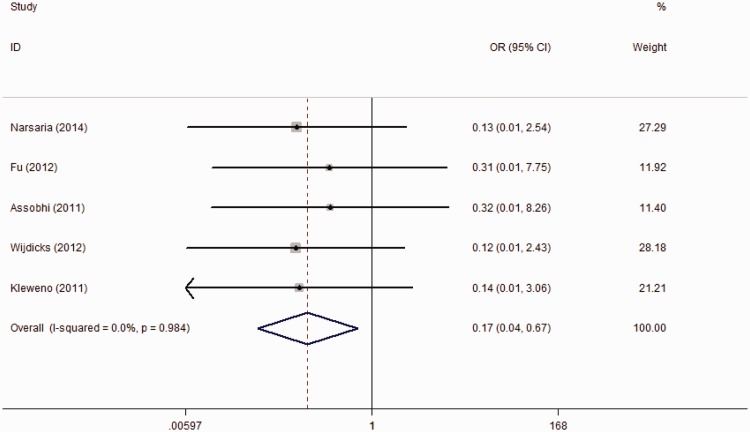
Five studies reported refracture incidence after implant removal, and found a lower incidence in IF patients compared with PF patients (0% versus 6.3%); the meta-analysis result was not significant (OR 0.17; 95% CI 0.04, 0.67; Figure 5).
Figure 5.
Forest plot for five studies which reported refracture incidence after implant removal in intramedullary fixation (IF) and plate fixation (PF) patients during recovery from midshaft clavicle fracture; I2 = 0.0%, P = not significant.
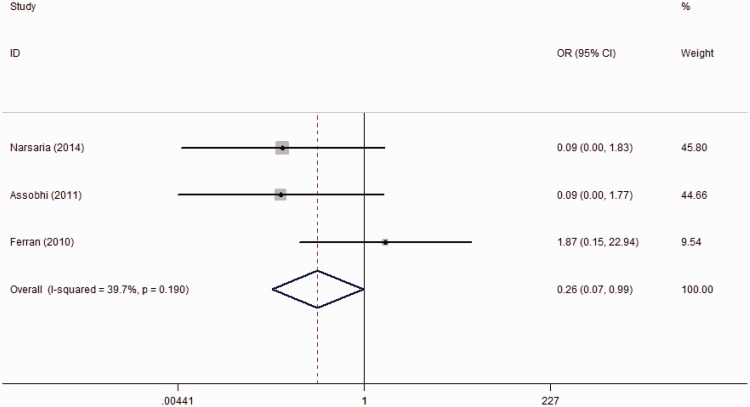
Development of hypertrophic scarring is an important complication that affects patients’ confidence in their appearance. Three studies reported postoperative hypertrophic scarring, with a higher incidence in PF patients (13.6%) than in IF patients (2.9%). The meta-analysis for combined results suggested a significant difference (OR 0.26; 95% CI 0.09, 0.99), with partial heterogeneity (I2 = 39.7%; Figure 6).
Figure 6.
Forest plot for three studies that reported hypertrophic scar incidence in intramedullary fixation (IF) and plate fixation (PF) patients during recovery from midshaft clavicle fracture; I2 = 39.7%, P = not significant.
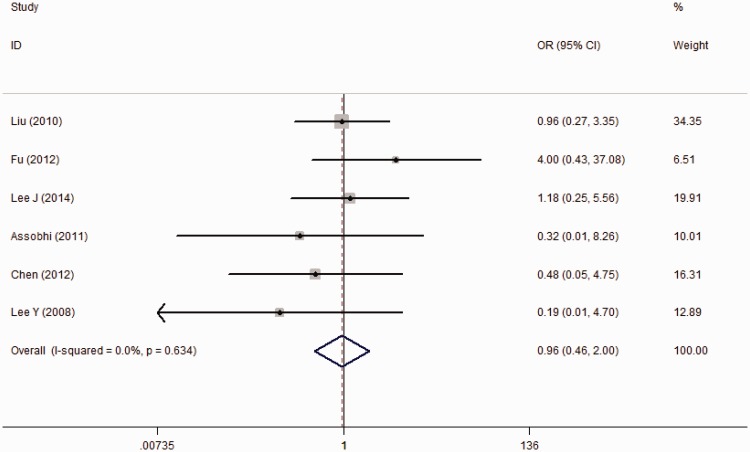
Nonunion is an important complication of this fracture, as it commonly necessitates a second operation for bone grafting and implant fixation. Six studies reported the incidence of nonunion, with slightly higher reports in PF patients than in IF patients (5.1% versus 4.7%). The meta-analysis result was not significant (OR 0.96; 95% CI 0.46, 2.00) without any heterogeneity (Figure 7).
Figure 7.
Forest plot for six studies reporting the incidence of nonunion in intramedullary fixation (IF) and plate fixation (PF) patients during recovery from midshaft clavicle fracture; I2 = 0.0%, P = not significant.
There were no significant differences in temporary brachial plexus lesion, nonunion, malunion, implant failure and the need for major revision between the fixation techniques. For these variables, there was no statistically significant heterogeneity when investigated using both Q- and I2 statistics (Table 3).
Table 3.
Comparative data for five variables of outcome in a meta-analysis comparing intramedullary fixation (IF) with plate fixation (PF) for midshaft clavicle fracture.
| Variable | Studies, n | Pooled OR or SMD | LL 95% CI | UL 95% CI | Statistical significancea | Q-statistic for heterogeneity P-value | I2 statistic % |
|---|---|---|---|---|---|---|---|
| Temporary brachial plexus lesion | 2 | 1.69 | 0.31 | 9.19 | NS | 0.343 | 0 |
| Nonunion | 6 | 0.96 | 0.46 | 2.00 | NS | 0.634 | 0 |
| Malunion | 3 | 1.78 | 0.66 | 4.79 | NS | 0.763 | 0 |
| Implant failure | 6 | 1.03 | 0.43 | 2.48 | NS | 0.320 | 14.8 |
| Major revision needed | 2 | 0.25 | 0.05 | 1.24 | NS | 0.532 | 0 |
Fixed-effects model.
I2 statistic defined as the proportion of heterogeneity not due to chance or random error.
SMD, standardized mean difference; OR, odds ratio; LL, lower limit; UL, upper limit; NS, not significantly different.
Functional outcome and motion range
Liu et al.35 and Ko et al.36 reported shoulder motion in their studies, including forward flexion, abduction, external rotation and internal rotation. There were no significant differences for these items between PF and IF in the current study, and heterogeneity was not observed for any item (Table 3).
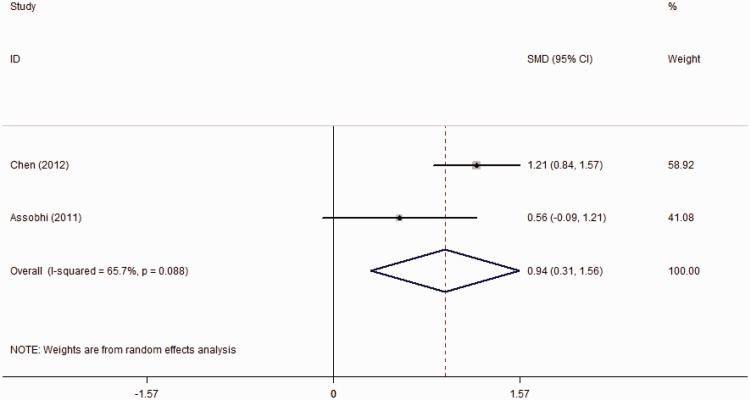
The shoulder constant score37 is used to assess the extent of functional recovery, with higher scores representing better rehabilitation. Constant scores at 6 months were reported by three studies, at 12 months by three studies and at 24-months follow-up by two studies. At 6-month follow-up, patients from the IF group had a higher constant score (92.6 versus 87.2) than those in the PF group: this finding was not significant by meta-analysis (SMD 0.94; 95% CI 0.31, 1.56) but there was significant heterogeneity (Figure 8). However, at the 12- and 24-month follow-up appointments, the results between groups were not significantly different (Table 3).
Figure 8.
Forest plot for the shoulder constant score reported in three studies at 12-month follow-up in intramedullary fixation (IF) and plate fixation (PF) patients during recovery from midshaft clavicle fracture; I2 = 65.7%, P = not significant.
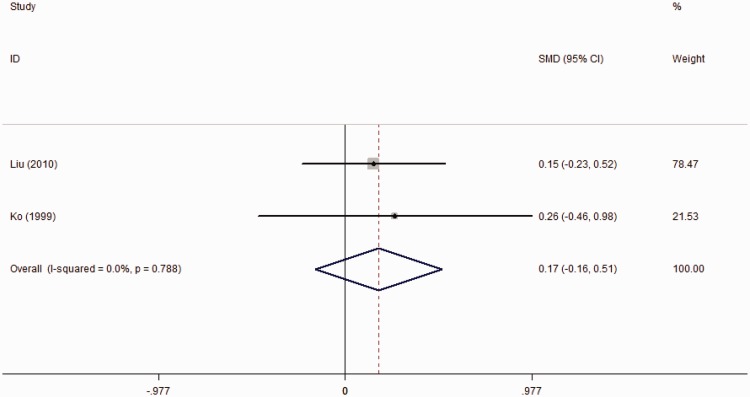
The Disability of Arm, Shoulder and Hand (DASH) questionnaire37 is a standardized 30-item measure evaluating patients’ subjective perception of their upper extremity health status, including impairments and activity limitations. Response options range between 1 and 5, based on the ability to perform activities (1, no difficulty; 2, mild difficulty; 3, moderate difficulty; 4, severe difficulty; 5, unable); the score ranges between 0 and 100, with 0 indicating no disability and 100 indicating complete disability. In this study, DASH score at the 6-month follow-up was reported in one study,15 where IF patients scored better than PF patients, with a significantly lower score (6.6 versus 15.0). The authors also reported the outcome of DASH at the 24-month follow-up, when no significant difference was observed. A further two studies35,36 reported that at the 12-month follow-up, the DASH score between IF and PF was not statistically different (SMD 0.17; 95% CI −0.16, 0.31); the meta-analysis showed no heterogeneity (Figure 9).
Figure 9.
Forest plot for the Disability of Arm, Shoulder and Hand (DASH) questionnaire37 scores at 12-month follow-up reported in two studies of intramedullary fixation (IF) and plate fixation (PF) patients during recovery from midshaft clavicle fracture; I2 = 0.0%, P = not significant.
Descriptive analysis
Union time was reported to be shorter with IF than with PF, but it was not possible to perform a meta-analysis on this variable due to significant heterogeneity and the different forms that the data were presented in the original studies. The American Shoulder and Elbow Surgeons (ASES) scale37 is a common tool to assess shoulder function recovery. Narsaria et al.24 reported that the ASES score at the 24-month postoperative follow-up was slightly higher in PF patients than in IF patients (99.4 versus 96.8), but this finding was not significantly different.
Discussion
Midshaft clavicle fracture has traditionally been treated conservatively, without surgery, but this method has a high rate of complications.6,8 Surgery appears to offer a better alternative for fractures of this type.38 However, there is controversy regarding whether IF or PF provides the optimum outcome for patients. In this study, a meta-analysis of 12 original studies was used to address this key issue. The results showed that IF outperformed PF, with a lower rate of symptomatic hardware, less hypertrophic scarring, fewer refractures after implant removal and better functional outcome at the 6-month follow-up. Other complications (including overall complications, implant failure, nonunion, malunion, delayed union, the need for major revision surgery, temporary brachial plexus lesion and reduced shoulder motion) showed no significant difference between the methods.
Surgeons commonly pay more attention to patients’ complications that might affect prognosis and functional recovery; severe complications may cause secondary surgery.18,27,28 A higher total complication incidence was more likely in the PF group than in the IF group18,39 (OR 2.97). The complications of acute midshaft clavicular fracture in active young patients were due to surgical procedures and the actual implant itself, and less associated with the patients’ underlying diseases. In this study, three implant-related complications: symptomatic hardware, hypertrophic scarring and refracture after implant removal were all more likely to occur in PF rather than IF groups. As PF generally requires a large incision, extensive exposure and soft tissue dissection, this technique is more likely to produce hypertrophic scarring, compared with IF. In a study by Kwak-Lee,26 16.4% of patients sustained symptomatic hardware or incision complications, which were attributed to intraoperative traction and/or stretching of the nerves over the plate. Refracture after hardware removal was reported to occur only in patients treated with plates, with an overall incidence of 6.3% (10/158)24,25,28,34,39 mostly occurring at the junction of the middle-third and outer-third regions of the clavicle. Implant removal after fracture healing reduces the mechanical strength of the clavicle, and the screw holes create weak spots in this thin bone, which together may initiate refracture.28,39
Implant failure is an important complication that affects operative success and causes over 80% of the revision surgery for midshaft clavicular fractures.28 In this analysis, the incidence of implant failure was similar in both techniques. In PF, implant failure was mainly triggered by excessive movement and often manifested as plate bending or loosening; in IF, lack of stability caused migration of the intramedullary device.40,41 Therefore, to prevent this complication, the stability of IF needs to be improved, and excessive movement, especially in the early stages of recovery from PF surgery, should be minimized.15,26,42
No significant difference was observed in shoulder motion range and functional recovery between IF and PF, except for the Constant Score at the 6-month follow-up. This suggests that IF is more likely than PF to yield a better early functional outcome, but there is no difference between the techniques at the bone union stage and the late stage of recovery. In some studies, rapid union has been confirmed with IF, which might be important in functional recovery and shoulder motion.24,26,34,39
The present study suffers from some weaknesses. Firstly, only four prospective RCTs were included in this meta-analysis, which might lower the power. Secondly, the types of fixations applied in the studies were varied and the follow-up periods of each study ranged widely. Thirdly, the age of patients in each group was not similar, except for one study. The choice of treatment was decided by the demands of each treatment, the surgeons’ experience and the patients underlying medical conditions. Advanced age generally has a negative effect on the level of function restored, and this aspect needs further future study.
Although this study had limitations that were unavoidable, it still has merit. First, the search style using both the computer and manual searching ensures a complete inclusion of relevant studies. Secondly, no significant heterogeneity was observed in most variables, except for active external rotation. This heterogeneity was diminished by sensitivity analysis, without altering the result. Lastly, but most importantly, this is the first quantitative meta-analysis to date to give a definitive preference to one of the two methods for treating complex fractures of the proximal humerus, reflecting the current status of this issue.
In conclusion, based on present evidence, IF appears to be superior to PF for the management of midshaft clavicle fractures. Compared with PF, IF provides a better shoulder constant score at 6 months and fewer incidences of symptomatic hardware, refracture after hardware removal and hypertrophic scarring. This could aid surgeons in making decisions for fixing midshaft clavicular fractures.
Acknowledgements
We are grateful to J Lu and Y Chen of the Department of Orthopaedics of the Second Hospital of Hebei Medical University, Shijiazhuang, China, and to X Zhang of the Department of Statistics and Applications of Hebei Medical University, Shijiazhuang, China, for their kind assistance.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Robinson CM. Fractures of the clavicle in the adult. Epidemiology and classification. J Bone Joint Surg Br 1998; 80: 476–484. [DOI] [PubMed] [Google Scholar]
- 2.Zhang YZ. Clavicle Fractures. Clinical epidemiology of orthopedic trauma, First edition Stuttgart & New York: Thieme, 2012, pp. 564–580. [Google Scholar]
- 3.Khan LA, Bradnock TJ, Scott C, et al. Fractures of the clavicle. J Bone Joint Surg Am 2009; 91: 447–460. [DOI] [PubMed] [Google Scholar]
- 4.Postacchini F, Gumina S, De Santis P, et al. Epidemiology of clavicle fractures. J Shoulder Elbow Surg 2002; 11: 452–456. [DOI] [PubMed] [Google Scholar]
- 5.Nordqvist A, Petersson C. The incidence of fractures of the clavicle. Clin Orthop Relat Res 1994; 300: 127–132. [PubMed] [Google Scholar]
- 6.Robinson CM, Court-Brown CM, McQueen MM, et al. Estimating the risk of non-union following nonoperative treatment of a clavicular fracture. J Bone Joint Surg Am 2004; 86: 1359–1365. [DOI] [PubMed] [Google Scholar]
- 7.Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. A multicenter, randomized clinical trial. J Bone Joint Surg Am 2007; 89: 1–10. [DOI] [PubMed] [Google Scholar]
- 8.Zlowodzki M, Zelle BA, Cole PA, et al. Treatment of acute midshaft clavicle fractures: systematic review of 2144 fractures: on behalf of the Evidence-Based Orthopaedic Trauma Working Group. J Orthop Trauma 2005; 19: 504–507. [DOI] [PubMed] [Google Scholar]
- 9.Grechenig W, Heidari N, Leitgoeb O, et al. Is plating of mid-shaft clavicular fractures possible with a conventional straight 3.5 millimeter locking compression plate? Acta Orthop Traumatol Turc 2011; 45: 115–119. [DOI] [PubMed] [Google Scholar]
- 10.Shen JW, Tong PJ, Qu HB. A three-dimensional reconstruction plate for displaced midshaft fractures of the clavicle. J Bone Joint Surg Br 2008; 90: 1495–1498. [DOI] [PubMed] [Google Scholar]
- 11.Mueller M, Rangger C, Striepens N, et al. Minimally invasive intramedullary nailing of midshaft clavicular fractures using titanium elastic nails. J Trauma 2008; 64: 1528–1534. [DOI] [PubMed] [Google Scholar]
- 12.Mudd CD, Quigley KJ, Gross LB. Excessive complications of open intramedullary nailing of midshaft clavicle fractures with the Rockwood clavicle pin. Clin Orthop Relat Res 2011; 469: 3364–3370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smekal V, Irenberger A, Struve P, et al. Elastic stable intramedullary nailing versus nonoperative treatment of displaced midshaft clavicular fractures-a randomized, controlled, clinical trial. J Orthop Trauma 2009; 23: 106–112. [DOI] [PubMed] [Google Scholar]
- 14.Collinge C, Devinney S, Herscovici D, et al. Anterior-inferior plate fixation of middle-third fractures and nonunions of the clavicle. J Orthop Trauma 2006; 20: 680–686. [DOI] [PubMed] [Google Scholar]
- 15.Chen YF, Wei HF, Zhang C, et al. Retrospective comparison of titanium elastic nail (TEN) and reconstruction plate repair of displaced midshaft clavicular fractures. J Shoulder Elbow Surg 2012; 21: 495–501. [DOI] [PubMed] [Google Scholar]
- 16.Verborgt O, Pittoors K, Van Glabbeek F, et al. Plate fixation of middle-third fractures of the clavicle in the semi-professional athlete. Acta Orthop Belg 2005; 71: 17–21. [PubMed] [Google Scholar]
- 17.Böstman O, Manninen M, Pihlajamäki H. Complications of plate fixation in fresh displaced midclavicular fractures. J Trauma 1997; 43: 778–483. [DOI] [PubMed] [Google Scholar]
- 18.Lee YS, Huang HL, Lo TY, et al. Surgical treatment of midclavicular fractures: a prospective comparison of Knowles pinning and plate fixation. Int Orthop 2008; 32: 541–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nakayama M, Gika M, Fukuda H, et al. Migration of a Kirschner wire from the clavicle into the intrathoracic trachea. Ann Thorac Surg 2009; 88: 653–654. [DOI] [PubMed] [Google Scholar]
- 20.Golish SR, Oliviero JA, Francke EI, et al. A biomechanical study of plate versus intramedullary devices for midshaft clavicle fixation. J Orthop Surg Res 2008; 3: 28–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barlow T, Beazley J, Barlow D. A systematic review of plate versus intramedullary fixation in the treatment of midshaft clavicle fractures. Scott Med J 2013; 58: 163–167. [DOI] [PubMed] [Google Scholar]
- 22.Houwert RM, Wijdicks FJ, Steins Bisschop C, et al. Plate fixation versus intramedullary fixation for displaced mid-shaft clavicle fractures: a systematic review. Int Orthop 2012; 36: 579–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Duan X, Zhong G, Cen S, et al. Plating versus intramedullary pin or conservative treatment for midshaft fracture of clavicle: a meta-analysis of randomized controlled trials. J Shoulder Elbow Surg 2011; 20: 1008–1015. [DOI] [PubMed] [Google Scholar]
- 24.Narsaria N, Singh AK, Arun GR, et al. Surgical fixation of displaced midshaft clavicle fractures: elastic intramedullary nailing versus precontoured plating. J Orthop Traumatol 2014; 15: 165–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fu TH, Tan BL, Liu HC, et al. Anatomical reduction for treatment of displaced midshaft clavicular fractures: Knowles pinning vs. reconstruction plating. Orthopedics 2012; 35: e23–e30. [DOI] [PubMed] [Google Scholar]
- 26.Kwak-Lee J, Ahlmann ER, Wang L, et al. Analysis of contoured anatomic plate fixation versus intramedullary rod fixation for acute midshaft clavicle fractures. Advances in Orthopedic Surgery 2014; 2014: 1–7. [Google Scholar]
- 27.Wenninger JJ, Jr., Dannenbaum JH, Branstetter JG, et al. Comparison of complication rates of intramedullary pin fixation versus plating of midshaft clavicle fractures in an active duty military population. J Surg Orthop Adv 2013; 22: 77–81. [DOI] [PubMed] [Google Scholar]
- 28.Wijdicks FJ, Houwert M, Dijkgraaf M, et al. Complications after plate fixation and elastic stable intramedullary nailing of dislocated midshaft clavicle fractures: a retrospective comparison. Int Orthop 2012; 36: 2139–2145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fang X, Jiang L, Wang Y, et al. Treatment of Gustilo grade III tibial fractures with unreamed intramedullary nailing versus external fixator: a meta-analysis. Med Sci Monit 2012; 18: RA49–RA56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lau J, Ioannidis JP, Schmid CH. Quantitative synthesis in systematic reviews. Ann Intern Med 1997; 127: 820–826. [DOI] [PubMed] [Google Scholar]
- 31.Wei J, Yang TB, Luo W, et al. Complications following dorsal versus volar plate fixation of distal radius fracture: a meta-analysis. J Int Med Res 2013; 41: 265–275. [DOI] [PubMed] [Google Scholar]
- 32.Thyagarajan D S, Day M, Dent C, et al. Treatment of mid-shaft clavicle fractures: a comparative study. Int J Shoulder Surg 2009; 3: 23–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lee YS, Lin CC, Huang CR, et al. Operative treatment of midclavicular fractures in 62 elderly patients: knowles pin versus plate. Orthopedics 2007; 30: 959–964. [DOI] [PubMed] [Google Scholar]
- 34.Assobhi JE. Reconstruction plate versus minimal invasive retrograde titanium elastic nail fixation for displaced midclavicular fractures. J Orthop Traumatol 2011; 12: 185–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liu HH, Chang CH, Chia WT, et al. Comparison of plates versus intramedullary nails for fixation of displaced midshaft clavicular fractures. J Trauma 2010; 69: E82–E87. [DOI] [PubMed] [Google Scholar]
- 36.Ko Y, Park C, Shon O, et al. Comparison of plate versus threaded k-wire for fixation of midshaft clavicular fractures. J Korean Fract Soc 2012; 25: 123–128. [Google Scholar]
- 37.Angst F, Schwyzer HK, Aeschlimann A, et al. Measures of adult shoulder function: Disabilities of the Arm, Shoulder, and Hand Questionnaire (DASH) and its short version (QuickDASH), Shoulder Pain and Disability Index (SPADI), American Shoulder and Elbow Surgeons (ASES) Society standardized shoulder assessment form, Constant (Murley) Score (CS), Simple Shoulder Test (SST), Oxford Shoulder Score (OSS), Shoulder Disability Questionnaire (SDQ), and Western Ontario Shoulder Instability Index (WOSI). Arthritis Care Res (Hoboken) 2012Suppl 11): S174–S188. [DOI] [PubMed] [Google Scholar]
- 38.Alshameeri ZA, Katam K, Alsamaq M, et al. The outcome of surgical fixation of mid shaft clavicle fractures; looking at patient satisfaction and comparing surgical approaches. Int J Shoulder Surg 2012; 6: 76–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kleweno CP, Jawa A, Wells JH, et al. Midshaft clavicular fractures: Comparison of intramedullary pin and plate fixation. J Shoulder Elbow Surg 2011; 20: 1114–1147. [DOI] [PubMed] [Google Scholar]
- 40.Poigenfürst J, Rappold G, Fischer W. Plating of fresh clavicular fractures: results of 122 operations. Injury 1992; 23: 237–241. [DOI] [PubMed] [Google Scholar]
- 41.Shen WJ, Liu TJ, Shen YS. Plate fixation of fresh displaced midshaft clavicle fractures. Injury 1999; 30: 497–500. [DOI] [PubMed] [Google Scholar]
- 42.Harnroongroj T, Jeerathanyasakun Y. Intramedullary pin fixation in clavicular fractures: a study comparing the use of small and large pins. J Orthop Surg (Hong Kong) 2000; 8: 7–11. [DOI] [PubMed] [Google Scholar]
- 43.Ferran NA, Hodgson P, Vannet N, et al. Locked intramedullary fixation vs plating for displaced and shortened mid-shaft clavicle fractures: a randomized clinical trial. J Shoulder Elbow Surg 2010; 19: 783–789. [DOI] [PubMed] [Google Scholar]