Abstract
Objective
Identify latent trajectories of executive functioning (EF) recovery overtime after childhood TBI and examine the predictive value of known risk factors within and across recovery trajectories using latent class growth modeling (LCGM).
Method
206 children between the ages of 3-7 years with a moderate to severe TBI or orthopedic injury (OI) were included. LCGM was applied to identify longitudinal trajectories of post-injury EF as assessed by the Behavior Rating Inventory of Executive Functioning General Executive Composite (GEC). Separate models were estimated for the TBI and OI groups.
Results
Two TBI trajectories: Normal Limits (70.8%) and Clinically Elevated (29.2%), and three OI trajectories: Normal Limits (20.9%), Subclinical (49.0%), and Clinically Elevated (30.17%) were identified. Baseline GEC was the only predictor of class membership for all models. Both TBI trajectories demonstrated an increase in GEC over time whereas only one of the three OI classes demonstrated this pattern. Family variables were associated with GEC across trajectories.
Conclusion
The lack of association of injury characteristics with trajectory class membership highlights the heterogeneity in recovery following pediatric TBI. Associations of EF trajectories with family factors underscores the importance of involving the family in interventions for children with traumatic injuries.
Traumatic brain injury (TBI) is a leading cause of acquired morbidity and mortality in children.1 Despite adequate characterization of resulting neurobehavioral impairments at the group level,2,3 individual long-term outcomes are notoriously heterogeneous and there exists substantial unexplained variability in neurobehavioral outcomes and trajectories of recovery.4-6 This unexplained variability following TBI is one of the most significant barriers to the development of individualized clinical prognostic tools and therapeutic interventions.7,8
Neurobehavioral outcomes following pediatric TBI are multiply determined.9,10 Injury severity, typically quantified using the Glasgow Coma Scale (GCS),11 is the most commonly used risk factor in predicting outcome. However, this factor accounts for a relatively small amount of variance in short-term neurobehavioral outcomes12,13 and appears to diminish in predictive value over time, with several studies noting no association with longer-term neurobehavioral function.14,15 Injury severity accounts for even less variance when trajectories of recovery over time are examined rather than outcome at a single time point.4,16 Demographic factors also account for a small proportion of variance in outcomes. Children from families of low socioeconomic status (SES) fare worse than children with higher SES and related access to resources.9,17 In addition, the effects of pediatric TBI are age-dependent. Children sustaining injuries at younger ages are particularly vulnerable, likely because of increased susceptibility to diffuse brain insult and its effects on post-injury skill development.6,16 Child premorbid functioning is another factor that predicts post-injury neurobehavioral functioning.16 Not only do children who sustain TBI show higher rates of premorbid attention difficulties than their non-injured peers,18,19 but their premorbid difficulties are also exacerbated by TBI.20 Finally, family environmental factors, such as parenting style and family functioning, account for additional variance in outcomes. The effects of TBI on neurobehavioral function are more pronounced in children from disadvantaged family environments and buffered by favorable family environments,4,21-23 although these associations appear to vary over time since injury.21 Despite the known contributions of injury, demographic, child, and family factors to neurobehavioral outcomes, models remain insufficient for clinical prediction of recovery trajectories for the individual patient. Examination of latent trajectories may shed light on factors that contribute to differing patterns of recovery over time.
The objectives of the present study were to identify latent trajectories of executive functioning (EF) over time following TBI sustained in early childhood and examine the predictive value of known risk factors within and across recovery trajectories. EF was selected as our neurobehavioral variable of interest given its high vulnerability to impairment following TBI,2,24 and associations with academic, social, and adaptive functioning,25-27 as well as because it was assessed longitudinally at all six time points throughout our study, including an assessment of retrospective premorbid functioning. The majority of extant longitudinal studies of neurobehavioral function following pediatric TBI have utilized a variable-centered approach in which the goal is to identify predictors of dependent variables and describe how a priori, observed independent variables—often injury severity quantified using GCS—and dependent variables are related3,28,29. Given the limited predictive value of injury severity, especially for longer-term neurobehavioral outcomes, the variable-centered approach may obscure recovery trajectories present in the data.
To address these concerns, we utilized a person-centered approach, latent class growth curve modeling, to classify individuals into distinct groups based on prototypical latent trajectories across time30. This approach is useful with longitudinal data for representing heterogeneity in developmental trajectories and considers patterns of intra-individual change30. We hypothesized that some individuals with TBI would demonstrate poorer outcomes than others and that these differences would be related to injury and environmental factors. Further, based on evidence suggestive of emerging deficits over time, we hypothesize that the TBI trajectories will demonstrate a worsening of EF symptoms over time. We also examined latent trajectories in a comparison group of children with orthopedic injuries (OI). We anticipated that this group would demonstrate greater longitudinal stability in EF over time but that associations of family factors with EF would be similar in the two groups.
Method
Participants and Study Design
Institutional Review Boards of all institutions approved all procedures, and written informed consent was obtained from all participants. A concurrent cohort/prospective research design was used. Consecutive admissions of preschool children with TBI or orthopedic injury (OI) that did not involve the central nervous system were screened at three tertiary care children's hospitals and a general hospital in Ohio. Participants included children who sustained a TBI or OI between the ages of 3 and 7 years. Children with OI served as the comparison group to control for pre-injury child and family factors that increase the likelihood of sustaining an injury requiring hospitalization. Additional inclusion criteria included overnight hospitalization, accidental cause of injury, no history of pre-injury neurological problems or developmental delays, and English as the primary spoken language. Children were not excluded if they had a history of attention problems, oppositional behaviors, or associated symptoms. Assessments were completed at baseline (0-3 months post-injury), 6-, 12-, 18-months, 3.4 years, and 6.7 years post-injury. TBI severity was characterized using the lowest post resuscitation GCS. Severe TBI was defined as GCS score less than or equal to 8. Moderate TBI was defined as GCS score of 9-12 or 13-15 accompanied by abnormal brain imaging. The OI group included children who sustained a bone fracture (not including skull fractures), had an overnight stay in the hospital, and did not exhibit alterations in consciousness or other signs or symptoms of head trauma or brain injury.
A total of 221 participants were enrolled. Children with uncomplicated mild TBI (GCS> 13 with no neuroimaging findings) were excluded from the present sample (n=15). A total of 206 children were included in the present analyses: 87 children with TBI (23 severe, 64 moderate) and 119 with OI. The injury groups did not differ in terms of demographic variables or baseline EF scores (See Table 1). Percent of data missing at each of the visits post baseline are as follows: 6-month (12.6%), 12-month (21.4%), 18-month (22.8%), ∼3 year (30.1%), ∼7 year (36.4%). Those that completed all visits did not differ from those who did not complete the extended follow-up (∼7 year) in terms of demographic (injury type and severity, age at injury, sex, race, SES) or any of the outcome variables discussed below.
Table 1.
Demographics table. Injury groups did not differ with regards to any demographic variables or baseline executive functioning scores.
| OI (n=119) | Moderate TBI (n=64) | Severe TBI (n=23) | p | |
|---|---|---|---|---|
| Age at Injury (SD) | 4.96 (1.00) years | 5.06 (1.20) years | 5.12 (1.07) years | .80 |
| Gender (% male) | 16 (69.57) | 37 (57.81) | 69 (57.98) | .56 |
| Race (% White) | 16 (69.57) | 43(67.19) | 91(76.47) | .38 |
| Baseline GEC (SD) | 53.48 (14.90) | 49.63 (13.15) | 48.96 (12.27) | .34 |
| SES z-score | .17 (.95) | -.12 (1.10) | -.48 (.65) | .01 |
| Median income (SD) | $63,888 ($23,410) | $57,051 ($26,327) | $54,308 ($15,823) | - |
| Maternal Education (% at least HS graduate) | 15 (71.43%) | 53 (84.13%) | 107 (93.04%) | - |
Note: GEC = Behavior Rating Inventory of Executive Function General Executive Composite, OI = Orthopedic Injury, TBI = Traumatic Brain Injury. General linear models were used to examine injury group differences for age at injury, baseline GEC, and zSES. Chi square tests were used to examine group differences for gender and race.
Group comparisons revealed that the OI group had significantly greater SES z-score than the severe TBI group (p = .01). No other group comparisons were significant.
Measures
Executive functioning
Parents provided ratings of their child's executive functioning on the Behavior Rating Inventory of Executive Functioning (BRIEF)31 at each assessment. The BRIEF is a standardized rating scale with satisfactory reliability and validity32 on which parents report the frequency (never, sometimes, often) of behaviors reflective of their child's EF. Because we assessed children between the ages of 3 and 7, we used the age appropriate versions of the BRIEF (for either preschool or school-age children). T-scores on the General Executive Composite Scale (GEC) were used as the dependent variable. Higher T-scores indicate poorer EF behaviors, with T-scores 65 or greater indicating clinically elevated problems. At the baseline assessment, parents were asked to report on their child's behavior prior to their injury, whereas ratings at the subsequent five time points represented the child's current EF.
Time-invariant risk factors
Variables potentially related to outcomes of TBI (age at injury, sex, SES, and baseline EF as measured by the baseline GEC) were included in the model as predictors of trajectory class membership. Categorical injury severity (moderate TBI vs Severe TBI) was also included as a predictor of TBI trajectory class membership. SES was determined by using the average of the z-scores for maternal education and median income for the census tract in which the family resided.
Time-varying risk factors
The purpose of time-varying covariates is to investigate change in the dependent variable as a function of change in the time-varying covariate over time. These variables are modeled as predictors of the dependent variable (GEC) along with the time variable (time since injury) in a time-specific equation. Family burden of injury, general family functioning, and parenting style were collected at each of the post-baseline assessments, and included as time-varying covariates to help clarify the dynamic relationship between family environment and GEC over time.
The 12-item General Functioning scale from the McMaster Family Assessment Device (FAD-GF) was used as a summary measure of family functioning33. FAD-GF scores range from 1-4 with higher scores reflective of greater dysfunction. Perceived family burden was assessed using the Family Burden of Injury Interview (FBII)34, which has satisfactory reliability and validity34,35. The composite score representing the mean of the Child, Spouse, and Extended Family and Friends scales was used in analyses, with higher scores indicative of greater burden34. Parenting behaviors were assessed via the Parenting Practices Questionnaire (PPQ)36. The PPQ is a 62-item self-report questionnaire of parenting behaviors that produces three summary scores, representing authoritarian, authoritative, and permissive parenting styles. A more authoritative parenting style has been associated with fewer child behavior problems than authoritarian or permissive approaches 37.
Data analysis
Latent class growth modeling (LCGM) analysis was conducted in SAS using PROC TRAJ. Separate models were run for TBI and OI groups as we hypothesized that the trajectory shapes would vary as a function of injury type (TBI versus OI). LCGM operates from the assumption that meaningful unobserved subpopulations exist within the larger sample, each having a distinct longitudinal dependent variable trajectory. Latent trajectory classes are extracted based on dependent variable patterns as well as time invariant risk factors and time-varying covariates. The probability of being assigned to each latent class is identified for each subject based upon their dependent variable scores over time, as well as on that subject's scores on time-invariant and time-varying covariates. Participants are assigned to one and only one latent class based on probabilistic estimation techniques. Next, the shape of each trajectory class over time is determined. The goal of the present analysis was to identify and characterize meaningful trajectory classes of individuals following similar patterns of EF recovery over time after early childhood traumatic injury.
Model selection involved the iterative estimation of the number of trajectory classes as well as the shape of each trajectory class. We considered a range of 1 to 5 classes, as well as flat (i.e., intercept-only), linear, quadratic and cubic trajectory shapes. The Bayesian information criterion statistic (BIC), model estimation convergence, percentage of population represented in each subgroup (>10%), minimization of the residual variance statistic (sigma), and examination of posterior subgroup classification probabilities were all factors in determining the best fitting model.
Results
Determining executive functioning trajectories
TBI models
LCGM analysis resulted in a final growth model with two TBI trajectory classes (Figure 1, Table 2). In both classes, the average probability of being assigned to the class was >90%, indicating good fit and suggesting that the model is appropriately grouping individuals with similar patterns over time and discriminating between individuals with dissimilar response patterns. The two trajectory classes (Figure 1) included a normal limits class with mean scores broadly within normal range (class 1; 70.8%) and a clinically elevated class (class 2; 29.2%). The parameter estimates are presented in Table 3 for the time invariant risk factors and in Table 4 for time-varying covariates. Baseline GEC was the only risk factor significantly associated with class membership (see Table 3); sex, SES and injury severity were not significantly associated with subgroup membership. It should be noted that age at injury was a trending predictor of class membership, with greater age at injury associated with membership to the clinically elevated class. The normal limits class displayed an increase in levels of GEC over the 7-year study period and was composed of 10 children with severe TBI (17.2%) and 48 children with moderate TBI (82.8%). This class represented 47.6% of the severe TBI sample and 80% of the moderate TBI sample. Within this trajectory class, higher family dysfunction, higher family burden of injury, and more permissive parenting were associated with a higher GEC (see Table 4).
Figure 1.
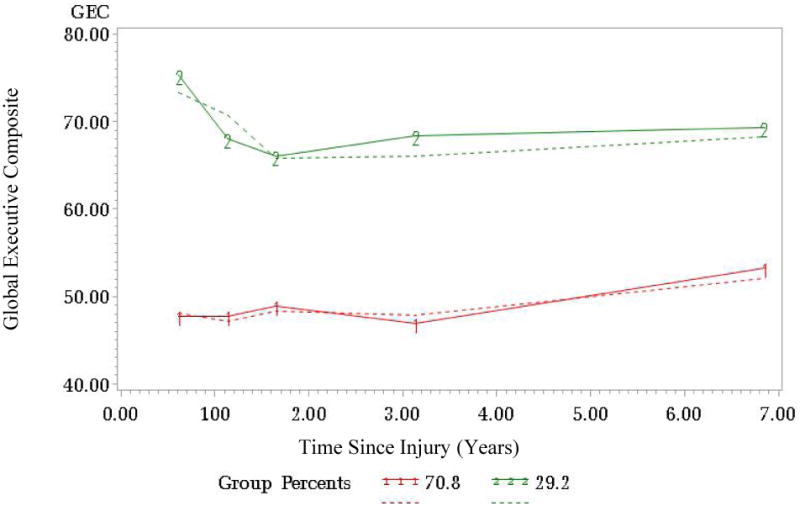
Executive functioning group trajectories for TBI group. Observed data trajectories are represented by dashed lines and model-based trajectories are represented by solid lines.
Table 2.
Final group based trajectory models. TBI and OI groups were modeled separately.
| TBI models | |||||
|---|---|---|---|---|---|
|
| |||||
| Group | Parameter | Estimate | Standard Error | t | p |
| Normal Limits | Intercept | 16.24 | 12.47 | 1.30 | .19 |
| Linear | 1.23 | .30 | 4.09 | .0001 | |
|
| |||||
| Clinically Elevated | Intercept | 70.70 | 16.50 | 4.28 | <.001 |
| Linear | -12.26 | 3.88 | -3.16 | .002 | |
| Quadratic | 2.61 | .97 | 2.68 | .008 | |
| Cubic | -.15 | .07 | -2.25 | .03 | |
|
| |||||
| OI Models | |||||
|
| |||||
| Normal Limits | Intercept | 23.80 | 12.18 | 1.95 | .05 |
| Linear | -2.85 | 1.71 | -1.67 | .10 | |
| Quadratic | .49 | .23 | 2.15 | .03 | |
|
| |||||
| Subclinical | Intercept | 44.07 | 9.12 | 4.83 | <.001 |
|
| |||||
| Clinically Elevated | Intercept | 36.67 | 10.14 | 3.62 | .0003 |
Table 3.
Model results for stable risk factor variables for TBI and OI models. Bolded items indicate statistically significant predictors of class membership.
| TBI Models | |||||
|---|---|---|---|---|---|
|
| |||||
| Group | Parameter | Estimate | Standard Error | t | p |
| Normal Limits | Constant | - | - | - | - |
|
| |||||
| Clinically Elevated | age at injury | 0.81 | .42 | 1.94 | .054 |
| sex | .64 | .83 | .77 | .443 | |
| ses | -.32 | .44 | -.72 | .474 | |
| injury severity | -1.45 | .85 | -1.71 | .087 | |
| Baseline GEC | .13 | .04 | 2.98 | .003 | |
|
| |||||
| OI Models | |||||
|
| |||||
| Group | Parameter | Estimate | Standard Error | t | p |
|
| |||||
| Normal Limits | Constant | - | - | - | - |
|
| |||||
| Subclinical | Age at injury | -.31 | .53 | -.58 | .56 |
| Sex | -1.11 | 1.24 | -.89 | .37 | |
| SES | -.25 | .57 | -.44 | .66 | |
| Baseline GEC | .53 | .20 | 2.63 | <.01 | |
|
| |||||
| Clinically Elevated | Age at injury | -.20 | .61 | -.33 | .74 |
| Sex | -2.06 | 1.41 | -1.47 | .14 | |
| SES | -.25 | .67 | -.37 | .71 | |
| Baseline GEC | .69 | .21 | 3.33 | <.001 | |
Note: Injury severity was modeled categorically (moderate vs. severe TBI). Significant positive parameter estimates indicate more/greater instances of a variable in that trajectory group compared to the comparison (normal limits) group, whereas negative parameter estimates indicate fewer/less instances of that variable in the trajectory group compared to the comparison (normal limits) group. GEC = Behavior Rating Inventory of Executive Function General Executive Composite
Table 4.
Results for time varying covariates for TBI and OI models. Bolded items indicate items with significant association with GEC.
| TBI Model | |||||
|---|---|---|---|---|---|
|
| |||||
| Group | Parameter | Estimate | Standard Error | t | p |
| Normal Limits | FBII | 5.76 | 1.30 | 4.45 | .000 |
| FAD | 5.32 | 1.63 | 3.26 | .001 | |
| Authoritative | -.03 | .08 | -.32 | .747 | |
| Authoritarian | .16 | .09 | 1.72 | .087 | |
| Permissive | .51 | .11 | 4.80 | .000 | |
|
| |||||
| Clinically Elevated | FBII | 6.55 | 1.56 | 4.20 | <.001 |
| FAD | -3.51 | 2.37 | -1.48 | .14 | |
| Authoritative | -.05 | .12 | -.46 | .65 | |
| Authoritarian | .01 | .14 | .07 | .94 | |
| Permissive | .52 | .16 | 3.27 | .001 | |
|
| |||||
| OI Model | |||||
|
| |||||
| Group | Parameter | Estimate | Standard Error | t | p |
|
| |||||
| Normal Limits | FBII | 1.07 | 2.08 | .52 | .607 |
| FAD | 3.17 | 1.94 | 1.63 | .104 | |
| Authoritative | .01 | .07 | .18 | .860 | |
| Authoritarian | .10 | .13 | .77 | .442 | |
| Permissive | .25 | .13 | 1.88 | .061 | |
|
| |||||
| Subclinical | FBII | 4.71 | 1.48 | 3.19 | .002 |
| FAD | 2.28 | 1.64 | 1.39 | .165 | |
| Authoritative | -.10 | .06 | -1.74 | .083 | |
| Authoritarian | .02 | .09 | .26 | .792 | |
| Permissive | .30 | .11 | 2.84 | .005 | |
|
| |||||
| Clinically Elevated | FBII | 10.37 | 1.82 | 5.70 | <.001 |
| FAD | 1.70 | 1.62 | 1.05 | .294 | |
| Authoritative | .01 | .07 | .20 | .845 | |
| Authoritarian | .14 | .09 | 1.60 | .110 | |
| Permissive | .32 | .12 | 2.71 | .007 | |
Note: Significant positive parameter estimate indicates that greater scores on that factor are associated with greater GEC within that trajectory. GEC = Behavior Rating Inventory of Executive Function General Executive Composite, FBII = Family Burden of Injury Interview, FAD = Family Assessment Device
The clinically elevated class demonstrated a cubic trajectory, involving two points of improvement during the first 2 years post-injury, followed by a consistently worsening GEC from approximately 3 years post-injury through the end of the study period. This class was made up of 11 children with severe TBI (47.8%) and 12 with moderate TBI (52.5%), representing 52.4% of the severe TBI sample and 20% of the moderate TBI sample. Poorer baseline GEC score was associated with a higher probability of membership to the clinically elevated class relative to the normal limits class (p = .003, see Table 3). Within this trajectory class, higher family burden of injury and more permissive parenting were associated with a higher GEC (see Table 4).
OI models
LCGM analysis resulted in a final growth model with three trajectory classes (Figure 2, Table 2). In all classes, the average probability of being assigned to the identified class was >89%, indicating good fit and suggesting that the model is appropriately grouping individuals with similar patterns over time and discriminating between individuals with dissimilar response patterns. The three trajectory classes (Figure 2) included a normal limits class with mean scores that fell within the normal range (class 1; 20.9%), a sub-clinical class (class 2; 49%), and a clinically elevated class (class 3; 30.1%). The parameter estimates for the time invariant risk factors are presented in Table 3 and time-varying covariates in Table 4. Baseline GEC was the only risk factor significantly associated with class membership (see Table 3); age at injury, sex, and SES were not significantly related to class membership.
Figure 2.
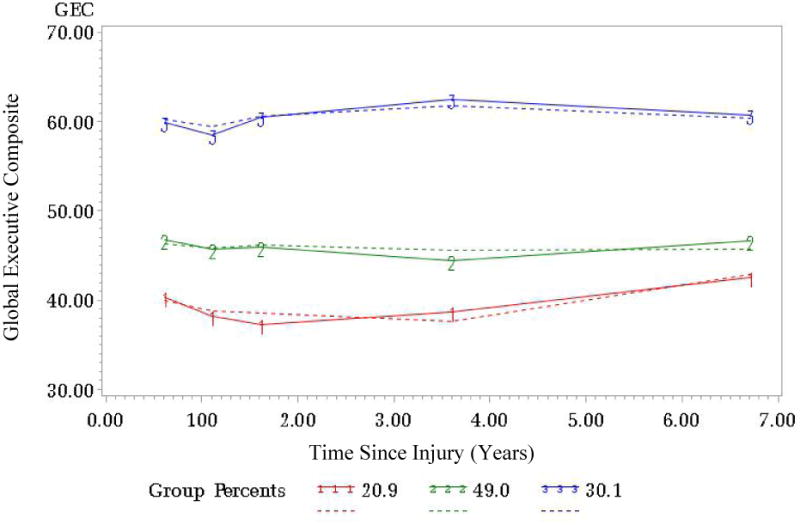
Executive functioning group trajectories for OI group. Observed data trajectories are represented by dashed lines and model-based trajectories are represented by solid lines.
The normal limits class demonstrated a quadratic trajectory, involving a decrease in GEC during the initial 3.5 years post-injury followed by an increase in GEC for the remainder of the study period. Environmental factors (family functioning, family burden of injury, and parenting styles) were not significantly associated with GEC within this group (Table 4).
The sub-clinical class demonstrated a flat trajectory with consistent levels of GEC throughout the study period. Poorer baseline GEC score was associated with a higher probability of membership to the sub-clinical class (p = .009, see Table 3). Within this trajectory, higher burden of injury and more permissive parenting were associated with a higher GEC (see Table 4).
The clinically elevated class also demonstrated a flat trajectory with consistent levels of GEC throughout the study period. Again, poorer baseline GEC score was associated with a higher probability of membership to the clinically elevated class (p = .0009, see Table 3). Within this trajectory class, higher burden of injury, and greater permissive parenting were associated with a higher GEC (see Table 4).
Discussion
Understanding the impact of child and family environmental factors on the recovery of EF following pediatric TBI is an important first step in identifying children and families most likely to require intervention, and provides valuable information regarding potential targets for treatment. Findings suggest that children with a history of early childhood TBI display two distinct EF recovery trajectories, whereas children with a history of early OI display three distinct EF trajectories. Baseline functioning (conceptualized as pre-injury functioning) was the only child factor associated with recovery in both TBI and OI models; however, environmental factors such as family burden, family functioning, and parenting styles had similar associations with EF within trajectory classes for both the TBI and OI groups. Surprisingly, injury severity did not predict class membership within the TBI models, and individuals with severe TBI were evenly distributed across both TBI trajectory classes. This finding highlights the heterogeneity of recovery after injury, particularly among those with severe TBI38. Further, at injury was a trending predictor of class membership in the TBI models with greater age associated with membership to the clinically elevated class. While this is in contrast to the literature suggesting an association between younger age of injury and greater impairment, the age range for the present study was limited (3-7 years), and may have influenced this finding.
Consistent with literature indicating early recovery from TBI10, children with greater EF impairment following injury demonstrated an initial improvement in EF during the first 1-2 years post injury, although still well above average. However both TBI trajectory classes demonstrated a worsening of EF over time, even in the class with EF scores within normal limits. This finding is consistent with the hypothesis that EF difficulties may surface or worsen as patients injured early in childhood face increasing EF demands with advancing age. Family factors also impacted both TBI trajectories. Specifically, greater family burden of injury and a more permissive parenting style were associated with increased EF impairment within both trajectory classes, whereas increased family dysfunction was associated with increased EF impairment in only the normal limits class. These findings are consistent with the literature suggesting that family and environmental factors do in fact impact EF recovery following pediatric TBI 4,21-23.
In contrast to the TBI trajectories, two of the three of the OI classes did not display any changes in EF overtime. This coupled with the finding that baseline EF score was the only predictor of class membership supports the idea that EF in OI and remains consistent from the time of injury, and injury does not play a role in worsening EF over the study period, unlike the TBI trajectory classes which demonstrated increasing problems in EF over time. In contrast one of the three OI trajectory classes displayed some worsening in GEC over time; however, scores remain well below clinical levels throughout the study period and may be more reflective of regression to the mean than of clinical changes in EF. Associations of family factors with EF were also found in the OI group. While the normal limits OI class was not impacted by family factors, increased family burden of injury and permissive parenting were associated with an increase in EF impairment in both the subclinical and clinical OI trajectory classes. The results suggest long-term environmental influences on EF regardless of injury characteristics. This may be reflective of the idea that these environmental factors (family burden and permissive parenting) are important factors in child behavior regardless of injury status.
The differential impact of family environmental variables across trajectory classes further supports the notion that environmental factors exert a substantial influence on EF recovery after injury4,21-23 and indicate the need for professionals to explore the family environment in developing interventions for post-injury behavior problems. The negative impact of maladaptive parenting strategies was also apparent across groups. While authoritative strategies were not associated with EF (either positively or negatively) in any of the trajectory classes, permissive parenting was associated with greater EF deficits in both TBI classes as well as the subclinical and clinical OI classes. Findings related to parenting style again support the previously identified relationship between maladaptive parenting styles and child behavior problems21, and point to another target for intervention for those with EF difficulties.
Taken together, the current findings provide guidance in identifying youth at greatest risk for prolonged EF deficits over time following early childhood injury. Children with pre-injury EF difficulties within the context of increased family burden and maladaptive parenting styles are likely to exhibit prolonged EF difficulties, even years after the injury, regardless of the type or severity of injury. We cannot change the child's pre-injury functioning but we can address family burden and maladaptive parenting styles in hopes of improving EF over time.
Although the study adds to our understanding of EF recovery over time after pediatric TBI, it has a number of limitations. First, the sample was confined to children with traumatic injuries and may not generalize to the broader child population. In the absence of a healthy non-injured control group, we cannot assess the impact of environmental variables on EF within normal development. Children hospitalized for severe OI may have unique behavioral profiles that are not truly reflective of healthy development. Second, the analysis used in the present study takes a person-centered approach to examining longitudinal data, but is limited in that individuals must remain on the trajectory to which they are assigned over time. Future studies would benefit from using latent transition analysis, which allows for movement of individuals between trajectory groups and for the examination of the factors that contribute to movement between trajectories. Third, we do not know how these trajectories of recovery relate to functional or real world impairment. While greater deficits in EF on the BRIEF are associated with greater functional impairment39, the present study did not examine other important outcomes such as learning or socialization. Fourth, although relationships between risk factors and EF were found, the nature or direction of the relationships is unclear. Family factors may have contributed to weaknesses in EF, but EF difficulties may also have lead to more family burden or elicited more authoritarian or permissive parenting approaches. Future studies may benefit from analytic strategies such as cross lagged panel analyses, which would permit the examination of reciprocal interactions between variables over time. Additionally, the pre-injury GEC was obtained at the baseline visit that took place 0-3 months after injury. While data was collected as soon after injury as possible, it is possible that parental report of pre-injury functioning was biased by children's post-injury functioning. Finally, children with severe TBI were evenly distributed across trajectory groups, suggesting that additional factors are likely related to recovery. Future researchers may consider examining the role of additional factors associated with recovery, including engagement in rehabilitation programs and educational interventions as well as biological factors such as genetic influences and medical treatments.
Acknowledgments
Funding Source: This publication was supported by grant R01 HD42729 from the National Institute of Child Health and Human Development (NICHD) and Trauma Research grants from the State of Ohio Emergency Medical Services. Additional support was provided through Grant 8 UL1 TR000077 from the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NIH.
Contributor Information
Megan Narad, Cincinnati Children's Hospital Medical Center, Cincinnati, OH
Amery Treble-Barna, Cincinnati Children's Hospital Medical Center, Cincinnati, OH
James Peugh, Cincinnati Children's Hospital Medical Center, Cincinnati, OH
Keith Yeates, Department of Psychology, Alberta Children's Hospital Research Institute Hotchkiss Brain Institute, University of Calgary, Alberta, CA
H. Gerry Taylor, Case Western Reserve University, Rainbow Babies & Children's Hospital, University Hospitals Case Medical Center, Cleveland, OH
Terry Stancin, Case Western Reserve University, MetroHealth Medical Center, Cleveland, OH
Shari Wade, Cincinnati Children's Hospital Medical Center and The University of Cincinnati College of Medicine, Cincinnati, OH
References
- 1.Faul M, Xu L, Wald MM, Cornado VG. Traumatic brain injury in the United States: Emergency department visits, hospitalizations and deaths 2002-2006. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2010. [Google Scholar]
- 2.Beauchamp MH, Anderson V. Cognitive and psychopathological sequelae of pediatric traumatic brain injury. Handbook of clinical neurology. 2013;112:913–920. doi: 10.1016/B978-0-444-52910-7.00013-1. [DOI] [PubMed] [Google Scholar]
- 3.Gerrard-Morris A, Taylor HG, Yeates KO, et al. Cognitive development after traumatic brain injury in young children. J Int Neuropsych Soc. 2010 Jan;16(1):157–168. doi: 10.1017/S1355617709991135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yeates KO, Taylor HG, Drotar D, et al. Preinjury family environment as a determinant of recovery from traumatic brain injuries in school-age children. J Int Neuropsych Soc. 1997 Nov;3(6):617–630. [PubMed] [Google Scholar]
- 5.Catroppa C, Anderson VA, Morse SA, Haritou F, Rosenfeld JV. Outcome and predictors of functional recovery 5 years following pediatric traumatic brain injury (TBI) J Pediatric Psychol. 2008 Aug;33(7):707–718. doi: 10.1093/jpepsy/jsn006. [DOI] [PubMed] [Google Scholar]
- 6.Anderson V, Catroppa C, Morse S, Haritou F, Rosenfeld J. Functional plasticity or vulnerability after early brain injury? Pediatrics. 2005 Dec;116(6):1374–1382. doi: 10.1542/peds.2004-1728. [DOI] [PubMed] [Google Scholar]
- 7.Hawryluk GW, Manley GT. Classification of traumatic brain injury: past, present, and future. Handbook of clinical neurology. 2015;127:15–21. doi: 10.1016/B978-0-444-52892-6.00002-7. [DOI] [PubMed] [Google Scholar]
- 8.Forsyth RJ, Salorio CF, Christensen JR. Modelling early recovery patterns after paediatric traumatic brain injury. Arch Dis Child. 2010 Apr;95(4):266–270. doi: 10.1136/adc.2008.147926. [DOI] [PubMed] [Google Scholar]
- 9.Fletcher JM, Ewing-Cobbs L, Francis DJ, Levin HS. Variability in outcomes after traumatic brain injury in children: A developmental perspective. In: Broman S, Michel M, editors. Traumatic Head Injury in Children. New York: Oxford University Press; 1995. pp. 3–21. [Google Scholar]
- 10.Taylor HG, Yeates KO, Wade SL, Drotar D, Klein SK, Stancin T. Influences on first-year recovery from traumatic brain injury in children. Neuropsychology. 1999 Jan;13(1):76–89. doi: 10.1037//0894-4105.13.1.76. [DOI] [PubMed] [Google Scholar]
- 11.Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974 Jul 13;2(7872):81–84. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- 12.Taylor HG, Swartwout MD, Yeates KO, Walz NC, Stancin T, Wade SL. Traumatic brain injury in young children: postacute effects on cognitive and school readiness skills. J Int Neuropsych Soc. 2008 Sep;14(5):734–745. doi: 10.1017/S1355617708081150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Prasad MR, Ewing-Cobbs L, Swank PR, Kramer L. Predictors of outcome following traumatic brain injury in young children. Pediatr Neurosurg. 2002 Feb;36(2):64–74. doi: 10.1159/000048355. [DOI] [PubMed] [Google Scholar]
- 14.Crowe LM, Catroppa C, Babl FE, Anderson V. Intellectual, behavioral, and social outcomes of accidental traumatic brain injury in early childhood. Pediatrics. 2012 Feb;129(2):e262–268. doi: 10.1542/peds.2011-0438. [DOI] [PubMed] [Google Scholar]
- 15.Anderson V, Godfrey C, Rosenfeld JV, Catroppa C. Predictors of cognitive function and recovery 10 years after traumatic brain injury in young children. Pediatrics. 2012 Feb;129(2):e254–261. doi: 10.1542/peds.2011-0311. [DOI] [PubMed] [Google Scholar]
- 16.Anderson V, Le Brocque R, Iselin G, et al. Adaptive ability, behavior and quality of life pre and posttraumatic brain injury in childhood. Disabil Rehabil. 2012;34(19):1639–1647. doi: 10.3109/09638288.2012.656789. [DOI] [PubMed] [Google Scholar]
- 17.Anderson VA, Morse SA, Klug G, et al. Predicting recovery from head injury in young children: a prospective analysis. J Int Neuropsych Soc. 1997 Nov;3(6):568–580. [PubMed] [Google Scholar]
- 18.Bloom DR, Levin HS, Ewing-Cobbs L, et al. Lifetime and novel psychiatric disorders after pediatric traumatic brain injury. J Am Acad Child Psy. 2001 May;40(5):572–579. doi: 10.1097/00004583-200105000-00017. [DOI] [PubMed] [Google Scholar]
- 19.Max JE, Lansing AE, Koele SL, et al. Attention deficit hyperactivity disorder in children and adolescents following traumatic brain injury. Dev Neuropsychol. 2004;25(1-2):159–177. doi: 10.1080/87565641.2004.9651926. [DOI] [PubMed] [Google Scholar]
- 20.Yeates KO, Armstrong K, Janusz J, et al. Long-term attention problems in children with traumatic brain injury. J Am Acad Child Psy. 2005 Jun;44(6):574–584. doi: 10.1097/01.chi.0000159947.50523.64. [DOI] [PubMed] [Google Scholar]
- 21.Yeates KO, Taylor HG, Walz NC, Stancin T, Wade SL. The family environment as a moderator of psychosocial outcomes following traumatic brain injury in young children. Neuropsychology. 2010 May;24(3):345–356. doi: 10.1037/a0018387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yeates KO, Taylor HG, Wade SL, Drotar D, Stancin T, Minich N. A prospective study of short- and long-term neuropsychological outcomes after traumatic brain injury in children. Neuropsychology. 2002 Oct;16(4):514–523. doi: 10.1037//0894-4105.16.4.514. [DOI] [PubMed] [Google Scholar]
- 23.Taylor HG, Yeates KO, Wade SL, Drotar D, Stancin T, Minich N. A prospective study of short- and long-term outcomes after traumatic brain injury in children: behavior and achievement. Neuropsychology. 2002 Jan;16(1):15–27. doi: 10.1037//0894-4105.16.1.15. [DOI] [PubMed] [Google Scholar]
- 24.Beauchamp M, Catroppa C, Godfrey C, Morse S, Rosenfeld JV, Anderson V. Selective changes in executive functioning ten years after severe childhood traumatic brain injury. Devel Neuropsychol. 2011;36(5):578–595. doi: 10.1080/87565641.2011.555572. [DOI] [PubMed] [Google Scholar]
- 25.Robinson KE, Fountain-Zaragoza S, Dennis M, et al. Executive functions and theory of mind as predictors of social adjustment in childhood traumatic brain injury. J Neurotram. 2014 Nov 15;31(22):1835–1842. doi: 10.1089/neu.2014.3422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Arnett AB, Peterson RL, Kirkwood MW, et al. Behavioral and cognitive predictors of educational outcomes in pediatric traumatic brain injury. J Int Neuropsych Soc. 2013 Sep;19(8):881–889. doi: 10.1017/S1355617713000635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fulton JB, Yeates KO, Taylor HG, Walz NC, Wade SL. Cognitive predictors of academic achievement in young children 1 year after traumatic brain injury. Neuropsychology. 2012 May;26(3):314–322. doi: 10.1037/a0027973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Anderson V, Catroppa C, Morse S, Haritou F, Rosenfeld JV. Intellectual outcome from preschool traumatic brain injury: a 5-year prospective, longitudinal study. Pediatrics. 2009 Dec;124(6):e1064–1071. doi: 10.1542/peds.2009-0365. [DOI] [PubMed] [Google Scholar]
- 29.Ewing-Cobbs L, Prasad MR, Kramer L, et al. Late intellectual and academic outcomes following traumatic brain injury sustained during early childhood. J Neurosurg. 2006 Oct;105(4 Suppl):287–296. doi: 10.3171/ped.2006.105.4.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nagin D. Group Based Modeling of Development. Cambridge, MA: Harvard University Press; 2005. [Google Scholar]
- 31.Gioia GA, Isquith PK, Guy SC, Kenworthy L. Behavior rating inventory of executive function. Odessa: Psychological Assessment Resources; 2000. [Google Scholar]
- 32.Gioia GA, Isquith PK. Ecological assessment of executive function in traumatic brain injury. Devel Neurpsych. 2004;25(1-2):135–158. doi: 10.1080/87565641.2004.9651925. [DOI] [PubMed] [Google Scholar]
- 33.Miller IW, Bishop DS, Epstein NB, Keitner GI. The McMaster Family Assessment Device: Reliability and validity. J Marital Fam Ther. 1985;11:345–356. [Google Scholar]
- 34.Burgess ES, Drotar D, Taylor HG, Wade S, Stancin T, Yeates KO. The family burden of injury interview: reliability and validity studies. J Head Trauma Rehab. 1999 Aug;14(4):394–405. doi: 10.1097/00001199-199908000-00008. [DOI] [PubMed] [Google Scholar]
- 35.Taylor HG, Yeates KO, Wade SL, Drotar D, Stancin T, Burant C. Bidirectional child-family influences on outcomes of traumatic brain injury in children. J Int Neuropsych Soc. 2001 Sep;7(6):755–767. doi: 10.1017/s1355617701766118. [DOI] [PubMed] [Google Scholar]
- 36.Robinson CC, Mandleco B, Olsen SF, Hart CH. Authoritative, Authoritarian, and Permissive Parenting Practices - Development of a New Measure. Psychol Rep. 1995 Dec;77(3):819–830. [Google Scholar]
- 37.Querido JG, Warner TD, Eyberg SM. Parenting styles and child behavior in African American families of preschool children. J Clin Child Adolesc. 2002 Jun;31(2):272–277. doi: 10.1207/S15374424JCCP3102_12. [DOI] [PubMed] [Google Scholar]
- 38.Babikian T, Asarnow R. Neurocognitive outcomes and recovery after pediatric TBI: meta-analytic review of the literature. Neuropsychology. 2009 May;23(3):283–296. doi: 10.1037/a0015268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mangeot S, Armstrong K, Colvin AN, Yeates KO, Taylor HG. Long-term executive function deficits in children with traumatic brain injuries: assessment using the Behavior Rating Inventory of Executive Function (BRIEF) Child Neuropsychol. 2002 Dec;8(4):271–284. doi: 10.1076/chin.8.4.271.13503. [DOI] [PubMed] [Google Scholar]


