ABSTRACT
Objective
The aim of this study from the European Network for the Investigation of Gender Incongruence is to investigate the status of all individuals who had applied for gender confirming interventions from 2007 to 2009, irrespective of whether they received treatment. The current article describes the study protocol, the effect of medical treatment on gender dysphoria and body image, and the predictive value of (pre)treatment factors on posttreatment outcomes.
Methods
Data were collected on medical interventions, transition status, gender dysphoria (Utrecht Gender Dysphoria Scale), and body image (Body Image Scale for transsexuals). In total, 201 people participated in the study (37% of the original cohort).
Results
At follow-up, 29 participants (14%) did not receive medical interventions, 36 hormones only (18%), and 136 hormones and surgery (68%). Most transwomen had undergone genital surgery, and most transmen chest surgery. Overall, the levels of gender dysphoria and body dissatisfaction were significantly lower at follow-up compared with clinical entry. Satisfaction with therapy responsive and unresponsive body characteristics both improved. High dissatisfaction at admission and lower psychological functioning at follow-up were associated with persistent body dissatisfaction.
Conclusions
Hormone-based interventions and surgery were followed by improvements in body satisfaction. The level of psychological symptoms and the degree of body satisfaction at baseline were significantly associated with body satisfaction at follow-up.
Key words/Abbreviations: body image, gender dysphoria, gender incongruence, hormone therapy, gender confirming surgery, BIS = Body Image Scale, GD = gender dysphoria, GID = Gender Identity Disorder, GSI = Global Severity Index, SCL = Symptoms Checklist, UGDS = Utrecht Gender Dysphoria Scale
INTRODUCTION
Body image is a complex multifaceted construct including physical characteristics, psychological traits, and societal norms (1). Body image can be studied through the assessment of body-related satisfaction, feelings, ideals, and quality of life. In people with gender dysphoria (GD), body dissatisfaction—resulting from the discrepancy between “assigned” sex at birth and experienced gender—often leads to seeking medical care. Earlier research from our group has shown that body dissatisfaction of people with GD at admission is high and often reaches beyond sex characteristics only (2,3). Because not all body parts are affected by treatment, it is uncertain whether medical transition can completely dissolve body dissatisfaction.
Clinical care for people with GD is mostly conducted in multidisciplinary healthcare teams following the Standards of Care (4). Medical interventions were shown to improve quality of life and alleviate feelings of GD significantly (5,6). With regard to body image, both hormonal therapy (7) and genital surgery (8,9) were found to reduce overall body dissatisfaction and improved feelings of attractiveness and self-confidence (10). Furthermore, individuals with GD who did not receive genital surgery reported higher levels of body uneasiness (i.e., body-related distress) compared with people with eating disorders, people with GD postsurgery, and control participants (11).
In three earlier studies, data from the European Network for the Investigation of Gender Incongruence (ENIGI) cohort on body image at clinical admission were analyzed (2,3,12). Before medical care, participants reported highest dissatisfaction with genitalia but also with body hair growth (transwomen) and body shape (transmen) (3). Similar patterns were found when using the Body Image Scale (BIS) for transsexuals. In addition, body satisfaction was associated with social transition and with clinicians' valuation of “passing” (2). The most recent analysis has shown that body dissatisfaction has a sex-specific composition, in which multiple clusters of body characteristics can be distinguished (12).
Despite the increasing attention regarding the body image of people with GD, few researchers have performed prospective follow-up studies (13). These studies only reported overall body satisfaction scores, and none of the studies described body image in people who experience GD at one point in time but did not receive medical interventions at follow-up.
Stice and Whitenton (14) performed a large longitudinal study on the risk factors of body dissatisfaction in adolescent cisgender girls (2002). Besides body mass index and perceived pressure to be thin, two major factors associated with body (dis)satisfaction at follow-up were the degree of psychological symptoms as well as the level of initial body (dis)satisfaction (14). As mentioned earlier, previous studies emphasized the importance of medical transition and social passing as the experienced gender; however, no prospective study has been performed regarding predictive value of psychological symptoms and body satisfaction at baseline.
Follow-Up of the European Network for the Investigation of Gender Incongruence
In the ENIGI initiative, four European gender identity clinics collaboratively follow a large cohort of people with GD applying for medical care (15). The main objective of follow-up on the cohort was to provide a description of the current status of all applicants after 4 to 6 years after clinical entry and describing participants with and without medical transition. Relating outcomes at follow-up to characteristics at clinical entry may help identify prognostic factors of undergoing, refraining from or dropping out of the medical trajectory. The present article will focus on GD and body image specifically.
Aims of the Study
The objective of the current study was to measure the effects of medical interventions on the level of GD and body satisfaction 6 years after entering a gender identity clinic. A second objective was to examine whether satisfaction with body characteristics that are or were not targeted directly by medical care has improved. In addition, the predicting effects of psychological symptoms and baseline body satisfaction on body satisfaction at follow-up were studied. Lastly, in the current article, we describe the study protocol of the ENIGI follow-up study. We expect the medical interventions to have a positive effect on the feelings of GD and body satisfaction. In addition, in line with cisgender studies, we expect that body satisfaction at baseline and the degree of psychological symptoms also influence body satisfaction at follow-up.
MATERIAL AND METHODS
Participants
A total of 546 people were invited to participate in the study of whom 201 people (37%) both consented and filled out the survey (Amsterdam n = 100, Ghent n = 61, Hamburg n = 40). Among the study participants were 135 natal males (119 living in the female role, 12 in the male role, 4 did not report their current gender role) and 66 natal females (60 living in the male role, 5 in the female role, 1 did not report a current gender role). Twenty-nine individuals (14%) did not receive any medical interventions at follow-up, 36 (18%) received hormonal therapy only, and 136 (68%) received both hormone therapy and surgery.
Procedure
This study concerns a follow-up survey of the European Initiative for the Investigation of Gender Incongruence (ENIGI) (15). In the ENIGI protocol, all people applying for gender confirming medical interventions in Amsterdam (the Netherlands), Ghent (Belgium), Hamburg (Germany), and Oslo (Norway) fill out a standard battery of questionnaires during their diagnostic procedure.
Applicants for medical interventions from Amsterdam, Ghent, and Hamburg (between 2007 and 2009) of 17 years or older at clinical entry were invited by their caregivers through mail and/or telephone to fill out an online survey. All people, regardless of whether they had received medical interventions or not, were asked to participate. After a month, all nonresponders received a reminder. Information on the medical procedures received was retrieved from patient records. Ethical approval was received by institutional boards in Amsterdam, Ghent, and Hamburg. Because no ethical approval to contact participants was received in Oslo, only three clinics participated in the follow-up study.
The survey was provided online through a secured server using Encrypting File System technology (http://www.unipark.com/en/survey-software/). After providing consent, respondents received a personalized link via e-mail from their clinic. Within the survey, participants were routed automatically to sex- and treatment-specific questions, on the basis of their answers (e.g., natal females who had transitioned to the male gender would fill out versions for males). Before the study started, the survey and routing were tested with several nonparticipating individuals with (previous) GD.
Measures Analyzed in Current Study
During the diagnostic phase at baseline, data were collected on sociodemographic characteristics, relationships, and gender development (15). The criteria of the gender identity disorder (GID, currently GD) diagnosis were scored by the clinician on a self-constructed form, on the basis of the DSM-IV-TR criteria at the end of the diagnostic phase. At the time of data collection, this DSM version was still used (16). If both core criteria of GID in childhood were fulfilled, individuals were categorized as early onset. If none of the core criteria were fulfilled in childhood, individuals were classified as late onset (17). People who could not be assigned to either of the groups (i.e., because they fulfilled only 1 core criterion in childhood), were considered as a “residual” group. During the diagnostic procedure at the clinic, the Physical Appearance Scale was filled out by the clinician as well. This scale scores an observer's appraisal of the masculinity/femininity of a person's physical appearance on 14 items, rated on a five-point scale, ranging from very feminine (1) to very masculine (5) (18). The scores are recoded per natal sex into “least congruent” to “most congruent” with the experienced gender. Higher scores represent a physical appearance that is considered less in line with the experienced gender (i.e., the person “passes” poorly). Any sum score higher than 42 can be regarded as an appearance more in line with the natal sex than the experienced gender.
Utrecht Gender Dysphoria Scale
The 12-item scale assesses the level of experienced GD. Respondents rate the level of dysphoria of different dimensions of gender (role) on a one to five-point Likert scale regarding sex-specific statements. The sum score ranges from 12 (minimal dysphoria) to 60 (maximal dysphoria) (19,20). At follow-up, participants received the sex-specific version based on their current gender role (nontransitioned men and transmen filled out the male version, and nontransitioned women and transwomen filled out the female version). Both at baseline and follow-up, the Utrecht Gender Dysphoria Scale (UGDS) showed better internal consistency in the male version (αbaseline = 0.84, αfollow-up = 0.76) compared with the female version (αbaseline = 0.56, αfollow-up = 0.54).
Body Image Scale
This measure consists of 30 items to determine satisfaction with various body characteristics, rated on a five-point scale of satisfaction, ranging from very satisfied (1) to very dissatisfied (5) (7). The BIS contains equivalent sex-specific genital body parts to enable comparisons between the natal sexes. Higher scores represent higher degrees of body dissatisfaction. The following subscales can be extracted: social and hair items, head and neck items, muscularity and posture, hip region, chest region, and genitals (12). Participants of the follow-up study received a modified version including preoperative genital items (e.g., penis) and postoperative items (e.g., neovagina), resulting in 32 items. The BIS showed excellent internal consistency in the present sample (α = 0.90).
Symptom Checklist 90
The Symptom Checklist 90 (SCL-90) is a 90-item survey assessing self-reported psychological burden on a five-point Likert scale, ranging from zero (no symptoms) to four (severe symptoms). The Global Severity Index (GSI) is calculated as the average of all completed items and indicates overall experienced psychological symptoms (21). The SCL-90 was distributed both at baseline and after 6 years and showed excellent internal consistency (α = 0.98).
Other Measures
At follow-up, background information was collected on sociodemographic characteristics, social contacts, sexual orientation, and relationships, as well as on satisfaction with transition and medical treatments. All background information and information regarding treatment and transition were collected via self-constructed questionnaires. Details on the medical interventions were retrieved from patient records (in Amsterdam and Ghent) or provided by the responsible psychologist or psychiatrist (in Hamburg).
In addition, well-being, sexuality, psychological functioning, and social support were assessed but will be reported elsewhere:
Subjective wellbeing: using the Satisfaction With Life Scale (22), the Subjective Happiness Scale (23), and the Cantril Ladder (24)
Sexuality: measured by means of the Multidimensional Sexuality Questionnaire (25)
Social support: by means of the Social Support Questionnaire (26).
For an overview of all measures taken at clinical entry, we refer to the description of the ENIGI initiative, provided by Kreukels et al. (15).
Statistical Analysis
Internal consistency of the provided scales was calculated using Crohnbach α. Sex differences in demographic characteristics, evaluation of physical appearance, and frequency of treatments received at follow-up were assessed by means of χ2 and t tests. The UGDS and SCL-90 scores were calculated as overall means or sum scores per participant. The means for the BIS measure were calculated as overall and subscale scores. All outcome data were normally distributed. Analysis of variance (ANOVA) repeated measures were used to compare mean BIS and UGDS scores between admission and follow-up, and one-way ANOVA tests were performed to assess differences in BIS and UGDS averages among the three follow-up groups (no treatment, hormones only, and hormones and surgery). All surgical procedures were compiled into one dichotomous variable to facilitate group comparisons. To assess individual satisfaction with breasts and genitals, surgical procedures for breasts and genitals were tested separately in addition. The association between overall GD (UGDS) and body dissatisfaction (BIS) and the correlation between age and BIS were assessed using Pearson correlations (r). Furthermore, to assess the predictive value of nontreatment factors on body dissatisfaction at follow-up, a linear regression was performed including natal sex, age, Physical Appearance Scale at baseline, social transition at follow-up, SCL-90 at baseline and follow-up, and BIS at baseline as determinants. Cases were excluded listwise. Effect size was calculated using Cohen d. Variance and colinearity were assessed (−0.4 < r < 0.4), and homoscedasticy, linearity of residuals, and errors were judged through (P–P) plots and histograms. All analyses were performed using SPSS for Windows 22.0 (SPSS Inc, Chicago, Ill).
RESULTS
The characteristics of the study sample are displayed in Table 1. Compared with the natal females, natal male respondents were significantly older at admission and their physical appearance was evaluated less congruent with their experienced gender by the clinician. The natal female group consisted mostly of individuals with early onset of gender dysphoric feelings. In both at admission and follow-up, most of the respondents experienced low levels of psychological symptoms. In comparison with the eligible but nonparticipating individuals, the study participants were significantly older (36.4 [SD = 12.9] versus 31.9 [SD = 11.3] years old; t(540) = 4.27, p < .001) and more educated (33.8% versus 18.8% received high education at baseline; χ2(2) = 20.2, p <.001). Participants reported significantly higher baseline BIS scores (M = 3.33 [0.54]), compared with individuals who did not participate (M = 3.19 [0.61]; t(516) = 2.58, p = .01), which implies stronger body dissatisfaction among the study participants. The groups did not differ significantly in terms of fulfillment of the GID diagnosis.
TABLE 1.
Sample Characteristics
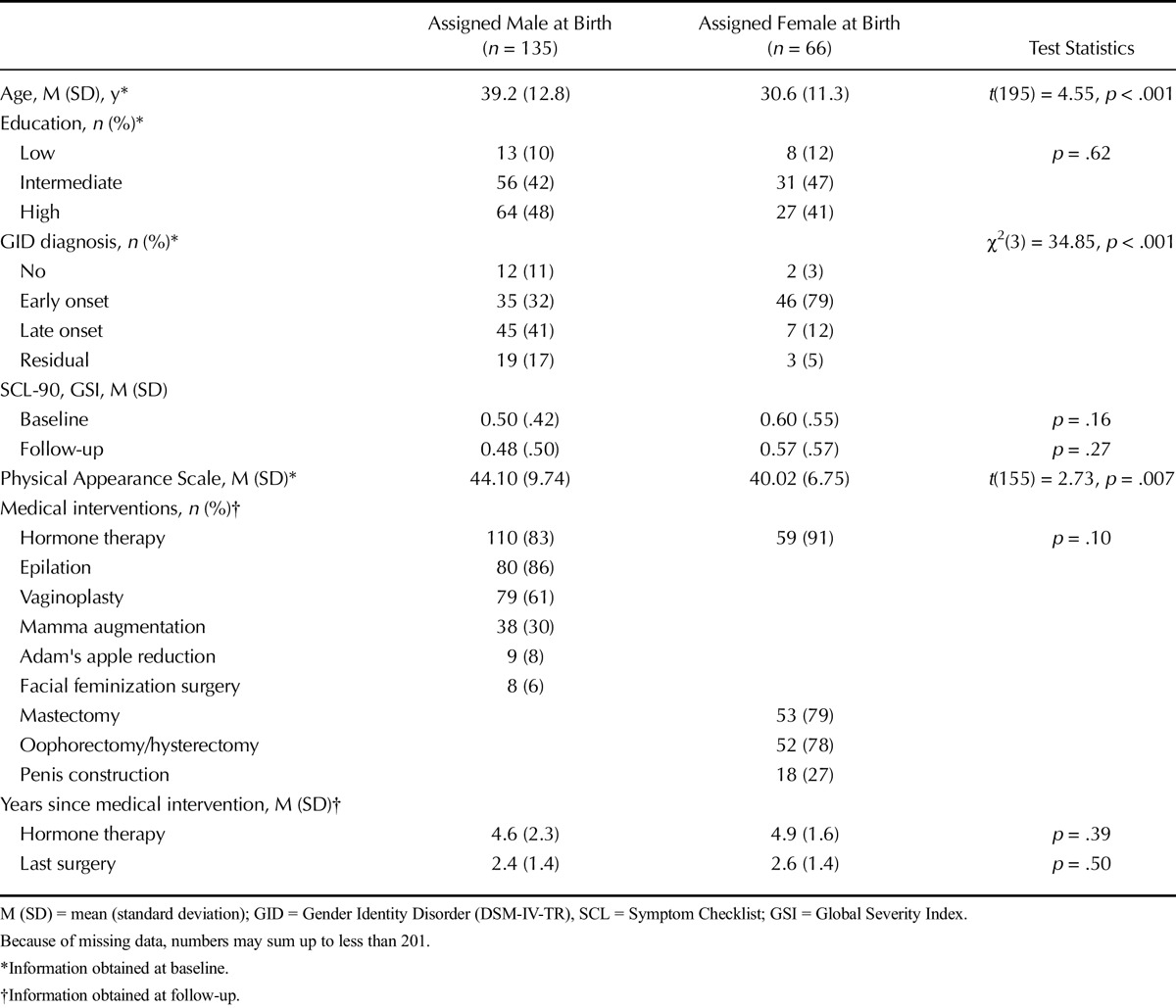
Medical Interventions
Ninety-one percent of the natal female (which includes mostly transmen) respondents had received cross-sex hormone therapy at follow-up, compared with 83% of the natal males (mostly transwomen). Most natal male participants had undergone epilation (86%) at follow-up. Surgical interventions, as a percentage of natal sex, are displayed in Table 1. There were no significant differences between the natal sexes regarding the average duration of hormone therapy or follow-up since surgery.
Gender Dysphoria
The average sum scores of GD were the following: UGDSadmission = 53.1 (SD = 6.7), UGDSno intervention = 20.2 (SD = 12.8), UGDShormones = 20.1 (SD = 8.8), and UGDShormones & surgery = 15.5 (SD = 4.3). The scores were significantly lower in all of the follow-up groups when compared with clinical admission, showing a decrease in GD (Fig. 1A). Within the follow-up groups, people who received both hormone therapy and surgery reported significantly less feelings of GD when compared with people without medical interventions. Such a difference was not found between the “hormones only” and “no intervention” groups. The baseline UGDS score of the “no interventions” group was significantly lower (Mno interventions [SD] = 48.4 [9.1]) than the other groups (Mhormones [SD] = 52.0 [5.4], Mhormones & surgery [SD] = 54.3 [5.8]; F(2,193) = 10.58, p < .001). Twenty-eight people did not fill out the UGDS (of whom 20 in the no interventions group), in some cases because participants ended the survey before finishing all instruments. In the no intervention group, all people who did not socially transition had missing data, which was the result of a programming error in the survey routing.
FIGURE 1.
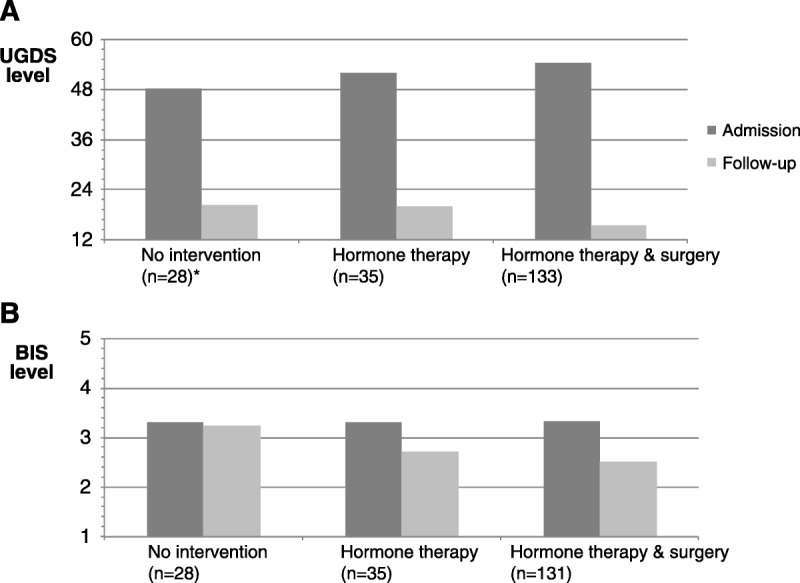
A, GD at clinical entry and follow-up displayed per treatments received. UGDS = Utrecht Gender Dysphoria Scale (12 = least dysphoric, 60 = most dysphoric). Baseline and follow-up levels of GD are displayed for the groups without and with hormonal and surgical therapy at follow-up; hormone therapy is mostly cross-sex hormones, surgery includes facial, chest, and/or genital surgery; the displayed n values report the available data per measure; SDno intervention admission = 9.2, SDno intervention follow-up = 12.8, SDhormone therapy admission = 5.4, SDhormone therapy follow-up = 8.8, SDsurgery admission = 5.8, SDsurgery follow-up = 4.3. *Due to a programming error, the follow-up UGDS data were available of nine participants only. B, Body dissatisfaction at clinical entry and follow-up displayed per treatments received. BIS = body image scale (1 = very satisfied, 5 = very dissatisfied). Baseline and follow-up levels of body dissatisfaction are displayed for the groups without and with hormonal and surgical therapy at follow-up; the displayed n values report the available data per measure; hormone therapy is mostly cross-sex hormones, surgery includes facial, chest, and/or genital surgery; SDno intervention admission = 0.59, SDno intervention follow-up = 0.64, SDhormone therapy admission = 0.61, SDhormone therapy follow-up = 0.73, SDsurgery admission = 0.51, SDsurgery follow-up = 0.58. Baseline versus follow-up; UGDS: F(1,168) = 13,668.37, p < .001; BIS: F(1,183) = 202.85, p < .001. Among follow-up groups; UGDS: F(2,170) = 9.54, p < .001; BIS: F(2,187) = 14.02, p < .001. GD = gender dysphoria; SD = standard deviation.
Body Image
Overall Body Satisfaction
Comparable with UGDS scores, respondents reported significantly higher overall body dissatisfaction at admission (BISadmission = 3.34 [SD = 0.52]) when compared with follow-up (Fig. 1B). At follow-up, people without medical interventions (BISno intervention = 3.24 [SD = 0.64]) were significantly more dissatisfied with their body than the people who did receive hormone therapy with(out) surgery (BIShormones = 2.72 [SD = 0.73], BIShormones & surgery = 2.51 [SD = 0.58]). Overall body dissatisfaction and GD were not found to be significantly correlated, neither at baseline nor at follow-up, implying that the degree of overall body (dis)satisfaction did not necessarily relate to the degree of GD. At baseline, however, the level of GD was moderately positively correlated to the level of genital dissatisfaction (r(183) = 0.39, p < .001). This association was not found at follow-up (r = 0.05).
Body Area Satisfaction
The average overall and subscale scores of body satisfaction at admission and follow-up are displayed in Figure 2. On average, the respondents who did not receive medical interventions at follow-up had similar levels of body dissatisfaction at baseline and at follow-up. People who did receive hormone therapy with or without surgery reported lower body dissatisfaction compared with baseline levels. Dissatisfaction with genitals and breasts was highest in the no intervention group at follow-up.
FIGURE 2.
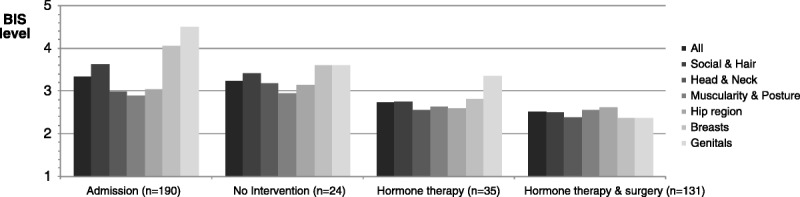
Dissatisfaction with body areas of all participants (at baseline) and per treatments received (at follow-up). BIS = Body Image Scale (1 = very satisfied, 5 = very dissatisfied). Baseline and follow-up levels of body area dissatisfaction are displayed of all participants at baseline (“admission”) and differentiated for the groups without and with hormonal and surgical therapy at follow-up; The displayed n values report the available data per measure; SDadmission all = 0.54, SDadmission social and hair = 0.72, SDadmission head and neck = 0.71, SDadmission muscularity and posture = 0.68, SDadmission hips = 0.76, SDadmission breasts = 0.82, SDadmission genitals = 0.72; SDno intervention all = 0.64, SDno intervention social and hair = 0.64, SDno intervention head and neck = 0.82, SDno intervention muscularity and posture = 0.77, SDno intervention hips = 0.77, SDno intervention breasts = 1.1, SDno intervention genitals = 1.1; SDhormones all = 0.73, SDhormones social and hair = 0.77, SDhormones head and neck = 1.0, SDhormones muscularity and posture = 0.76, SDhormones hips = 0.80, SDhormones breasts = 1.2, SDhormones genitals = 1.0; SDsurgery all = 0.58, SDsurgery social and hair = 0.74, SDsurgery head and neck = 0.73, SDsurgery muscularity and posture = 0.65, SDsurgery hips = 0.75, SDsurgery breasts = 0.95, SDsurgery genitals = 1.2. SD = standard deviation.
Within the groups who underwent medical interventions, satisfaction with both therapy responsive and nonresponsive body characteristics improved, when compared with clinical entry. At follow-up, people who have gone through medical interventions reported body satisfaction generally between two (satisfied) and three (neutral). No significant differences on most of the BIS subscales were found between respondents who had received hormones only and the respondents who also received surgery. The exception to this was genital dissatisfaction, which was significantly lower in the group that had surgery (M = 2.36 [SD = 1.21]), compared with the hormones only group (M = 3.36 [SD = 1.43]; t(160) = 4.13, p < .001). In transwomen, satisfaction with breasts was higher in the group who received breast enlargement (M = 1.90 [SD= .72]) in comparison with the group who received other surgeries than breast enlargement (M = 2.48 [SD = 1.00]), as well as people on hormones only (M = 2.70 [SD = 1.10]; F(2,105) = 4.89, p = .009). Within the “hormones only” group, different scores were observed between the people who planned (n = 14) and did not plan (n = 21) to undergo genital surgery in the future with regard to overall body satisfaction (Mplanned [SD] = 3.29 [0.61], Mnot planned [SD] = 2.35 [0.54]; t(33) = 4.75, p < .001) as well as for genital body satisfaction (Mplanned = 4.76 [SD = 0.40], Mnot planned [SD] = 2.42 [1.03]; t(33) = 8.07, p < .001).
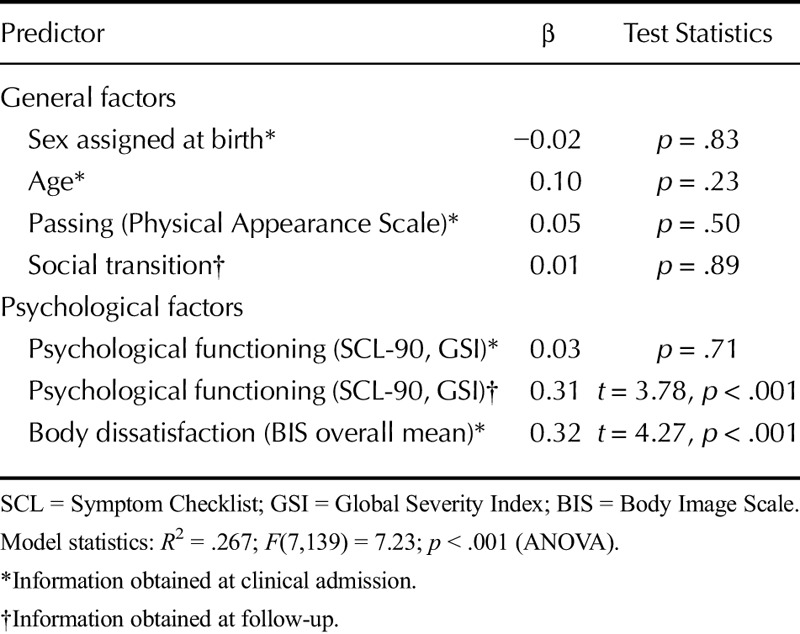
Nontreatment Predictors of Body Satisfaction
To assess the effects of nontreatment factors—both general and psychological—on body (dis)satisfaction at follow-up, a linear regression was performed (Table 2). The model assumptions were met (see the notes hereinafter the table). None of the general characteristics were found to be of predictive value, including natal sex, age, physical passing at admission, and social transition status at follow-up. Body dissatisfaction at admission was a significant predictor of body dissatisfaction at follow-up. This implies that a higher degree of overall body dissatisfaction before medical interventions predicts a higher degree of (persisting) body dissatisfaction after medical interventions. Moreover, psychological symptoms at follow-up (SCL-90 GSI score) were associated with body dissatisfaction at follow-up, which means that people with more psychological symptoms at follow-up were more dissatisfied with their bodies after medical interventions. Body dissatisfaction at follow-up was not predicted by psychological symptoms at baseline.
TABLE 2.
Linear Regression Model of Body Dissatisfaction at Follow-Up
Respondents Without Medical Intervention
Twenty-nine respondents had not received medical interventions at follow-up, of whom 23 natal males and six natal females. Some of them (5 natal males and 4 natal females) reported that this was their voluntary choice, whereas others mentioned different reasons. Among the motivations not to receive medical care were anxiety (n = 4: 3 natal males and 1 natal female), social circumstances (e.g., children; n = 3: all natal males), postponing the decision (n = 2: both natal females), benefit from psychological counseling (n = 1: natal female), and high age (n = 1: natal male).
More than 60% of the nonmedically treated group, regardless of the clinic, received psychological counseling, mostly outside of the participating clinics. Twelve participants dropped out the diagnostic procedure before a diagnosis could be made. Among the others, seven participants without medical interventions fulfilled the GID criteria according to their clinician, one was diagnosed with fetishistic transvestism, one with GID not otherwise specified, and for one participant data on the diagnosis were missing. Figure 3 displays the social (de)transitioning of the people without medical interventions. Five respondents did not provide information on their current gender role. On the question whether the respondent was planning to (re)apply for medical interventions in the future, most people said no (n = 9) or were unsure (n = 8), six people were planning to apply for medical care, and the other six did not respond to this question. There was no significant difference in the percentage of respondents without medical interventions between the three clinics.
FIGURE 3.
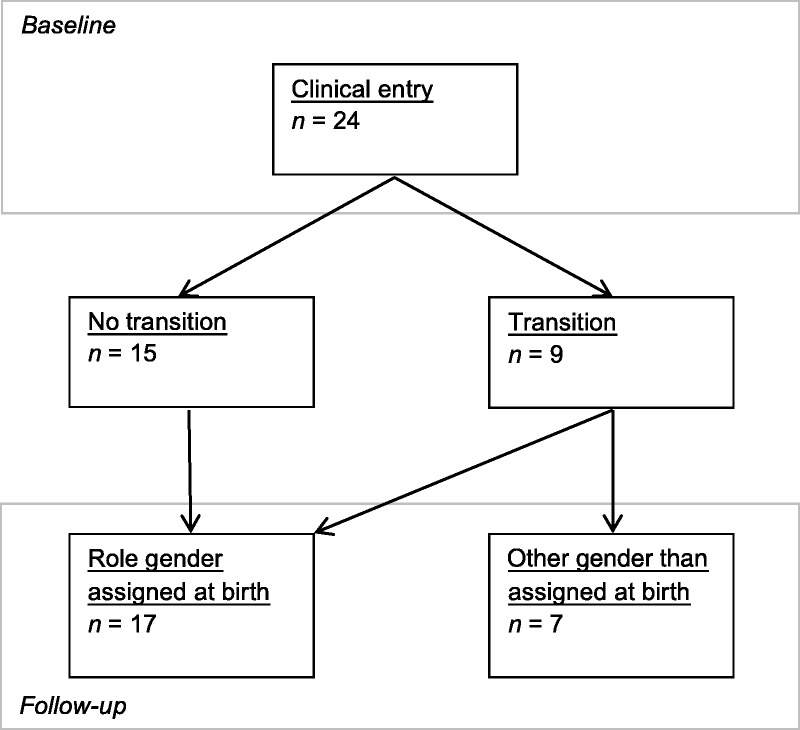
Social (de)transition of respondents without medical interventions. At/after clinical admission, some participants (had) transitioned to another gender role, of whom some had transitioned back to the role of their gender assigned at birth at follow-up.
DISCUSSION
When compared with clinical entry, experienced GD and body dissatisfaction were lower in follow-up groups with and without medical interventions. People who received both hormone therapy and surgery had more favorable body satisfaction scores compared with the people who used hormones only, both on therapy responsive and therapy unresponsive body characteristics. Genital satisfaction was particularly higher in the group who received surgery. In addition to the medical interventions, body dissatisfaction at baseline as well as psychological symptoms at follow-up was found to be associated with body dissatisfaction at follow-up.
Earlier studies have shown that medical transition alleviates most of the experienced GD in (young) adults (5,27,28). The baseline UGDS level in the current study (53.5) was similar to the levels reported in these studies, so were the postintervention levels, which were comparable with cisgender individuals (5,28). This decrease shows the effectiveness of medical interventions and social transition. Remarkably, feelings of GD of people without medical interventions also lowered. However, only seven of this group were thought to fulfill the GID criteria, whereas the others did not or dropped out of the diagnostic procedure before this could be assessed. At baseline, this group already showed lower UGDS scores indicating less severe GD. In addition, because of a programming error, in the “no interventions” group, only people who had socially transitioned received the UGDS. Living in the social role of the experienced gender may have decreased the level of GD already. Other explanations may be the positive effects of psychological counseling or prospect of future medical interventions, or people may have found alternative ways of living with their gender incongruence.
Follow-up studies on body image of people with GD are scarce (13). Smith et al. (5) and de Vries et al. (28) administered the BIS instrument before and after the start of medical transition (5,28). We found that people who were postoperative reported similar rates of body satisfaction compared with the earlier reported rates after surgery. Medical transition may increase body satisfaction and psychological wellbeing by improving the masculinity or femininity of body characteristics (e.g., voice deepening after testosterone or surgical creation of a vagina), making the body more congruent with the experienced gender identity, which positively influences the evaluation of the particular body characteristic and alleviates the level of GD. In addition, the altered body may be easier to “pass,” leading to more supportive social experiences. We have observed the influence of social passing on body satisfaction before (2). de Vries et al. (28), however, reported that body satisfaction with neutral characteristics (not primary or secondary) did not improve significantly after medical transition, possibly because all participants in that study had been on puberty blocking and were already relatively satisfied with these body parts. The present data show the biggest difference in body satisfaction between the groups with and without hormone therapy, although genital satisfaction was significantly higher in the group with surgery. In the follow-up group without medical interventions, the level of body dissatisfaction did not decrease as much as the level of GD. This may indicate that despite the lowered feelings of GD, there is still some body dissatisfaction (e.g., because someone socially transitioned without medical interventions). There is increasing discussion in the fields of psychosomatic and behavioral medicine about differences between biological sex versus gender roles in predicting disease risk factors and treatment outcomes (29,30). Although hormone and surgical treatments showed to improve psychological measures in our population, gender roles (29) and sexual orientation (31) have been described to directly affect mental health as well. In addition, the hormonal and surgical interventions in our participants may also be associated with consequences for medical outcomes such as cardiovascular diseases, although absolute risk increase was found to be low (32). The effects of medical interventions on outcomes and disease risk and their interaction with gender and sex deserve attention in future studies (30). None of the general characteristics significantly predicted overall body (dis)satisfaction at follow-up. Earlier studies found that body dissatisfaction at baseline was significantly higher in transwomen compared with transmen (2). This difference disappears after medical treatment or the study was underpowered to detect a difference (a small effect of sex was observed: d = 0.16). The same may be the case for the influence of age (a very weak correlation of r = 0.09 was found); previous research found that older transmen were less dissatisfied with their body, compared with their younger counterparts (33).
Psychological symptoms at follow-up were associated with body dissatisfaction at follow-up, which was found in earlier research (5,33). Lower body satisfaction may result from a lower overall satisfaction with life but can also be the consequence of a response bias in which both instruments were filled out negatively. Body dissatisfaction at baseline was another significant predictor of body dissatisfaction at follow-up, a finding that is in line with the results of Smith et al. (5) and studies in cisgender people (14). This suggests that people with a more severe body dissatisfaction are more likely to experience continued body dissatisfaction after medical transition. Nevertheless, a reverse relationship cannot be excluded (people with lower body satisfaction may “pass” less, experience more social difficulties and consequently more psychological symptoms). High treatment expectations can influence postoperative satisfaction as well; however, no data with regard to this topic were collected at baseline.
In contrast to other follow-up studies, the present study included all clinical applicants, irrespective of whether they decided to undergo medical treatment or not. However, at follow-up, most respondents had received hormone therapy with or without surgery, and only 29 participants received neither. The latter group reported different motives for not having gone through medical transition despite approaching a clinical facility, including their own choice, anxiety, social circumstances, and benefit from psychological counseling. At follow-up, most of them lived (again) in the social role of their natal sex. Previous studies reported “no intervention” rates of 22% and 32% at follow-up (5,34,35). Reasons included not being referred (yet) by the clinician, the severity of GD feelings, and psychological problems (5). The latter findings were confirmed in the current study: UGDS at baseline was lower in people without medical interventions, and one of the reported reasons among motivations not to undergo medical care was anxiety. Both lower levels of GD and anxiety can reduce the motivation to pursue obtaining medical treatments or prioritize alternative care (e.g., psychological counseling).
Limitations
The first limitation of the current study is that the Body Image Scale only measured body satisfaction as indicator of body image, leaving influential cognitions, feelings, and behavior out of scope. Furthermore, outcome measurement using sex-specific instruments is generally complicated when study participants medically transition. Because the UGDS instrument was initially not developed to make such intrapersonal cross-sex comparisons, statements on pre-post differences should be read prudently. Other methodological limitations include the fact that the compared groups were not matched, and therefore, other factors may have influenced the observed outcomes. The missing data on some measures may have had a similar effect. Group comparisons have been limited by the small sample size of the no intervention group, compared with the treated group. Some of the observed effect of medical treatments on the outcome variables may have been caused by regression to the mean in the different groups. In addition, physical outcome of medical transition is limited to a self-report measure only. In addition, because of the composition of the studied group and the response rate of 37%, insights on the body image of people with GD may be limitedly generalizable. The present study only describes the study responders, a group that was more educated than the nonresponders. Differences in body satisfaction may be possible between responding and nonresponding people. Because of a technical error, no conclusions can be drawn on the level of GD of people who neither received medical interventions nor socially transitioned.
CONCLUSIONS
The current study is the first comprehensive study to follow up on a larger group of people with GD applying for medical care in three gender identity clinics in Europe, regardless of the followed medical treatments. Medical care effectively reduced feelings of GD and improved body satisfaction. Hormone therapy decreased overall body dissatisfaction, whereas surgery contributed mostly to genital satisfaction. Analysis of predictors of persisting body dissatisfaction indicated that psychological mechanisms, next to medical interventions, contributed to body satisfaction. The concept of body image may assist clinicians and individuals with GD to develop treatment plans, which optimally improve psychological well-being. Especially, people with more profound and more overall body dissatisfaction could benefit from receiving additional counseling on this subject. Because current data suggest that a complete medical transition cannot dissolve all body dissatisfaction in some, psychotherapy may additionally offer guidance to accept the less than perfect body (aspects).
Acknowledgments
The authors thank all clinicians and research staff of the four clinics for their permanent support for the ENIGI research, and their contribution to the current follow-up study. The authors also thank Inga Becker for her valuable comments to a previous version of this article.
Source of Funding and Conflict of Interest: No funding was received for this study, neither did any of the authors receive external financial support. The authors report no conflicts of interest.
REFERENCES
- 1.Cash TF. Body image: past, present, and future. Body Image 2004;1:1–5. [DOI] [PubMed] [Google Scholar]
- 2.van de Grift TC, Cohen-Kettenis PT, Steensma TD, De Cuypere G, Richter-Appelt H, Haraldsen IR, Dikmans RE, Cerwenka SC, Kreukels BP. Body satisfaction and physical appearance in gender dysphoria. Arch Sex Behav 2016;45:575–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Becker I, Nieder TO, Cerwenka S, Briken P, Kreukels BP, Cohen-Kettenis PT, De Cuypere G, Haraldsen IR, Richter-Appelt H. Body image in young gender dysphoric adults: a European multi-center study. Arch Sex Behav 2016;45:559–574. [DOI] [PubMed] [Google Scholar]
- 4.Coleman E, Bockting W, Botzer M, Cohen-Kettenis P, DeCuypere G, Feldman J, Fraser L, Green J, Knudson G, Meyer WJ, Monstrey S, Adler RK, Brown GR, Devor AH, Ehrbar R, Ettner R, Eyler E, Garofalo R, Karasic DH, Lev AI, Mayer G, Meyer-Bahlburg H, Hall BP, Pfaefflin F, Rachlin K, Robinson B, Schechter LS, Tangpricha V, van Trotsenburg M, Vitale A, Winter S, Whittle S, Wylie KR, Zucker K. Standards of care for the health of transsexual, transgender, and gender-nonconforming people, version 7. Int J Transgend 2012;13:165–232. [Google Scholar]
- 5.Smith YL, van Goozen SH, Kuiper AJ, Cohen-Kettenis PT. Sex reassignment: outcomes and predictors of treatment for adolescent and adult transsexuals. Psychol Med 2005;35:89–99. [DOI] [PubMed] [Google Scholar]
- 6.Heylens G, Verroken C, De Cock S, T'Sjoen G, De Cuypere G. Effects of different steps in gender reassignment therapy on psychopathology: a prospective study of persons with a gender identity disorder. J Sex Med 2014;11:119–126. [DOI] [PubMed] [Google Scholar]
- 7.Lindgren TW, Pauly IB. A body image scale for evaluating transsexuals. Arch Sex Behav 1975;4:639–656. [DOI] [PubMed] [Google Scholar]
- 8.Fleming MZ, MacGowan BR, Robinson L, Spitz J, Salt P. The body image of the postoperative female-to-male transsexual. J Consult Clin Psychol 1982;50:461–462. [DOI] [PubMed] [Google Scholar]
- 9.Kuiper AJ, Cohen-Kettenis PT. Gender role reversal among postoperative transsexuals. Int J Transgend 1998;2. Available at: http://www.symposion.com/ijt/ijtc0502.htm. Accessed May 1, 2015.
- 10.Kraemer B, Delsignore A, Schnyder U, Hepp U. Body image and transsexualism. Psychopathology 2007;41:96–100. [DOI] [PubMed] [Google Scholar]
- 11.Bandini E, Fisher AD, Castellini G, Lo Sauro C, Lelli L, Meriggiola MC, Casale H, Benni L, Ferruccio N, Faravelli C, Dettore D, Maggi M, Ricca V. Gender identity disorder and eating disorders: similarities and differences in terms of body uneasiness. J Sex Med 2013;10:1012–1023. [DOI] [PubMed] [Google Scholar]
- 12.van de Grift TC, Cohen-Kettenis PT, Elaut E, De Cuypere G, Richter-Appelt H, Haraldsen IR, Kreukels BP. A network analysis of body satisfaction of people with gender dysphoria. Body Image;16:184–190. [DOI] [PubMed] [Google Scholar]
- 13.Jones BA, Haycraft E, Murjan S, Arcelus J. Body dissatisfaction and disordered eating in trans people: a systematic review of the literature. Int Rev Psychiatry 2016;1:81–94. [DOI] [PubMed] [Google Scholar]
- 14.Stice E, Whitenton K. Risk factors for body dissatisfaction in adolescent girls: a longitudinal investigation. Dev Psychol 2002;38:669–678. [DOI] [PubMed] [Google Scholar]
- 15.Kreukels BP, Haraldsen IR, De Cuypere G, Richter-Appelt H, Gijs L, Cohen-Kettenis PT. A European network for the investigation of gender incongruence: the ENIGI initiative. Eur Psychiatry 2012;27:445–450. [DOI] [PubMed] [Google Scholar]
- 16.American Psychiatric Association (APA). Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Arlington, VA: Amer Psychiatric Pub Inc; 1994. [Google Scholar]
- 17.Nieder TO, Herff M, Cerwenka S, Preuss WF, Cohen-Kettenis PT, De Cuypere G, Haraldsen IR, Richter-Appelt H. Age of onset and sexual orientation in transsexual males and females. J Sex Med 2011;8:783–791. [DOI] [PubMed] [Google Scholar]
- 18.Smith YL, van Goozen SH, Kuiper AJ, Cohen-Kettenis PT. Transsexual subtypes: clinical and theoretical significance. Psychiatry Res 2005;137:151–160. [DOI] [PubMed] [Google Scholar]
- 19.Cohen-Kettenis PT, Van Goozen SH. Sex reassignment of adolescent transsexuals: a follow-up study. J Am Acad Child Adolesc Psychiatry 1997;36:263–271. [DOI] [PubMed] [Google Scholar]
- 20.Schneider C, Cerwenka S, Nieder TO, Briken P, Cohen-Kettenis PT, De Cuypere G, Haraldsen IR, Kreukels BP, Richter-Appelt H. Measuring gender dysphoria: a multicenter examination and comparison of the utrecht gender dysphoria scale and the gender identity/gender dysphoria questionnaire for adolescents and adults. Arch Sex Behav 2016;45:551–558. [DOI] [PubMed] [Google Scholar]
- 21.Derogatis LR. SCL-90-R, administration, scoring and procedures manual-II for the R(evised) version and other instruments of the psychopathology rating scale series, Townson: Clinical Psychometric Res; 1992. [Google Scholar]
- 22.Diener E, Emmons RA, Larsen RJ, Griffin S. The satisfaction with life scale. J Pers Assess 1985;49:71–75. [DOI] [PubMed] [Google Scholar]
- 23.Lyubomirsky S, Lepper HS. A measure of subjective happiness: preliminary reliability and construct validation. Soc Indic Res 1999;46:137–155. [Google Scholar]
- 24.Cantril H. The Pattern of Human Concern, New Brunswick: Rutgers University; 1965. [Google Scholar]
- 25.Snell WE, Fisher TD, Walters AS. The Multidimensional Sexuality Questionnaire: an objective self-report measure of psychological tendencies associated with human sexuality. Ann Sex Res 1993;6:27–55. [Google Scholar]
- 26.Fydrich T, Sommer G, Brähler E. F-SOZU: Fragebogen zur sozialen Unterstützung, Göttingen: Hogrefe; 2007. [Google Scholar]
- 27.Murad MH, Elamin MB, Garcia MZ, Mullan RJ, Murad A, Erwin PJ, Montori VM. Hormonal therapy and sex reassignment: a systematic review and meta-analysis of quality of life and psychosocial outcomes. Clin Endocrinol (Oxf) 2010;72:214–231. [DOI] [PubMed] [Google Scholar]
- 28.de Vries AL, McGuire JK, Steensma TD, Wagenaar EC, Doreleijers TA, Cohen- Kettenis PT. Young adult psychological outcome after puberty suppression and gender reassignment. Pediatrics 2014;134:696–704. [DOI] [PubMed] [Google Scholar]
- 29.Juster RP, Pruessner JC, Desrochers AB, Bourdon O, Durand N, Wan N, Tourjman V, Kouassi E, Lesagne A, Lupien SJ. Sex and gender roles in relation to mental health and allostatic load. Psychosom Med 2016;78:788–804. [DOI] [PubMed] [Google Scholar]
- 30.Orth-Gomér K, Deter HC. Sex and gender issues in cardiovascular research. Psychosom Med 2015;77:1067–1068. [DOI] [PubMed] [Google Scholar]
- 31.Juster RP, Smith NG, Ouellet E, Sindi S, Lupien SJ. Sexual orientation and disclosure in relation to psychiatric symptoms, diurnal cortisol, and allostatic load. Psychosom Med 2013;75:103–116. [DOI] [PubMed] [Google Scholar]
- 32.Wierckx K, Elaut E, Declercq E, Heylens G, De Cuypere G, Taes Y, Kaufman JM, T'Sjoen G. Prevalence of cardiovascular disease and cancer during cross-sex hormone therapy in a large cohort of trans persons: a case-control study. Eur J Endocrinol 2013;169:471–478. [DOI] [PubMed] [Google Scholar]
- 33.Vocks S, Stahn C, Loenser K, Legenbauer T. Eating and body image disturbances in male-to-female and female-to-male transsexuals. Arch Sex Behav 2009;38:364–377. [DOI] [PubMed] [Google Scholar]
- 34.Lobato MI, Koff WJ, Manenti C, da Fonseca Seger D, Salvador J, da Graça Borges Fortes M, Petry AR, Silveira E, Henriques AA. Follow-up of sex reassignment surgery in transsexuals: a Brazilian cohort. Arch Sex Behav 2006;35:711–715. [DOI] [PubMed] [Google Scholar]
- 35.Johansson A, Sundbom E, Höjerback T, Bodlund O. A five-year follow-up study of Swedish adults with gender identity disorder. Arch Sex Behav 2010;39:1429–1437. [DOI] [PubMed] [Google Scholar]


