Abstract
Racial and ethnic disparities have been reported in clinical trial/research participation, utilization of autologous and allogeneic BMT and availability of allogeneic donors. We performed a population-based cohort study to investigate adult hematologic malignancy referrals to a U.S tertiary cancer center, utilization of BMT and participation in clinical trials, survey and biospecimen research, by race. U.S. Census Data and the New York State Public Access Cancer Epidemiology Database identified the racial distribution of the general population and new hematologic malignancy cases in the primary catchment area. From 2005–2011, 1,106 patients aged 18–75 years were referred for BMT consultation; while the rate of BMT among hematologic malignancy referrals did not differ by race, the reasons for not receiving a BMT did. Participation in biospecimen research did not vary by race, however African-Americans and other minorities were significantly less likely to participate in survey research than European-Americans. While rates of hematologic malignancy referrals and use of BMT for minorities appear low (<10%), they closely reflect the race distribution of all hematologic malignancy cases and the Western New York population. African-Americans are equally likely as other races to participate in biospecimen banking, but further study is needed to understand reasons for lower participation in survey research.
Keywords: Blood and Marrow Transplantation, Referrals, Clinical Research, Race
INTRODUCTION
Autologous and allogeneic blood and marrow transplantation (BMT) are complex, intensive treatments usually performed in tertiary care centers. Patients are initially referred for BMT consultation and subsequently undergo a comprehensive medical work-up, psychological evaluation including compliance, social work evaluation including caregiver support, screening for insurance and financial support and, if applicable, an allogeneic donor search. Patients with co-morbidities can still be eligible for a BMT if the co-morbidities are controlled.1 These include coronary artery disease, prior myocardial infarction, depression, diabetes, and prior cancer. During the BMT evaluation process, which can take weeks to months, a patient and/or their physician may decide that the patient is not a suitable candidate and it is not in the patient’s best interest to have a BMT.
The under-utilization of both autologous and allogeneic BMT by race and gender has been previously reported on a national basis.2 A recent analysis of the allogeneic donor pool within the National Marrow Donor Program demonstrated that most BMT candidates will have a suitable 7/8 or 8/8 HLA matched allogeneic donor in the registry, however an optimal 8/8 HLA-matched donor is more likely to be found for European American (EA) patients (75% chance) than for African American (AA) (16–19% chance) or other minorities (27–52% chance).3 Autologous BMT does not require a donor, has fewer side effects than an allogeneic BMT, requires less follow-up and resources than an allogeneic BMT. Yet, autologous BMT for multiple myeloma is significantly more common in EA than AA, even though the incidence of multiple myeloma is twice as common in AAs as in EAs.2,4 This suggests that disparities in use of BMT by race cannot be attributed solely to donor availability and may be due to socioeconomic factors.
We investigated population based rates of hematologic malignancy cases, referrals for BMT consultation, utilization of BMT as therapy and participation in clinical trials, survey and biospecimen research by race in our U.S. center. We examined demographic factors that might influence referral for BMT consultation and which may impede a patient’s ability to undergo BMT. Identification of modifiable factors could lead to interventions to decrease disparities in BMT referrals and increase utilization of BMT by minorities. We also sought to investigate the rate of participation in clinical research by race, since studies to improve disparities in outcomes or utilization of BMT will be compromised by low participation rates in minority populations.
METHODS
Study Population
We conducted a population based analysis of the average annual new hematologic cancer cases (Acute and Chronic Leukemia, Hodgkin and Non-Hodgkin Lymphoma, and Multiple Myeloma) diagnosed 2005–2009 by race and age using the New York State (NYS) Department of Health (DOH) Cancer Registry. NYS Public Health Law, Article 24, Title 1, Section 2401 requires all NYS physicians, dentists, laboratories, and other health care providers to report every case of cancer or other malignant disease to the NYS DOH Cancer Registry.5 The NYS Public Access Cancer Epidemiology Data (NYSPACED) can be used to analyze cancer incidence and mortality data reported to the NYS DOH Cancer Registry.6
Roswell Park Cancer Institute (RPCI) is the only NCI-designated Comprehensive Cancer Center in NYS outside of New York City, with the nearest cancer hospital about 75 miles away. Therefore, the main catchment area for RPCI is the 8 counties (Allegany, Cattaraugus, Chautauqua, Erie, Genesee, Niagara, and Orleans, Wyoming) of Western New York (WNY), from which 75% of all RPCI BMT referrals originate. The RPCI BMT database prospectively collects patient information (demographic, disease, treatment and outcomes data) in real-time from initial BMT referral until death or last follow-up. Disposition of BMT referrals includes: 1) the patient had an autologous or allogeneic BMT, 2) the patient did not have a BMT and the reason why, or 3) the patient is still pending a decision (currently undergoing work-up, searching for a donor, undergoing active cancer therapy, collecting hematopoietic cells, pending insurance approval, etc.). The RPCI Clinical Research Services database tracks all research study participation including consent, enrollment and study outcomes by race, age and gender.
The RPCI Data Bank and Biorepository (DBBR) is a comprehensive data and sample bank containing high quality pretreatment biological specimens and associated clinical and epidemiologic data.7 Briefly, all cancer referrals to RPCI are invited to participate. In addition, patients with benign diseases and healthy individuals (family/friends of patients and community volunteers) are also recruited to participate in the DBBR. After consent, blood samples are collected, and an epidemiologic questionnaire is given to the patient or healthy individual to complete and return by mail. The epidemiologic survey has 2 versions, one for males and one for females, which contain questions on reproductive history, family and personal history of cancer, vitamin and supplement use, diet, exercise, smoking history, alcohol history, medications and other drug use, education, marital status, and household income.
Study Design
To determine the proportions of race and ethnicity in the general population in the 8 counties of WNY (main catchment area), we used 2010 U.S. census data for people aged 18–75 years (based on published US census age categories). NYSPACED data from 2005–2009 was used to determine the race and ethnicity of all cases of hematologic malignancies aged 20–74 years (based on published NYSPACED age categories) diagnosed in the 8 counties of WNY. The RPCI BMT database captured all BMT referrals from January 2005 to August 2011. The BMT referral data were extended about 20 months after the end of the NYSPACED data collection period in order to account for a lag-time between diagnosis and referral. DBBR epidemiologic questionnaire data were available for BMT referrals who participated.
Study Definitions
Race and ethnicity are based on self-identification and self-report for U.S. Census Data. http://www.census.gov/topics/population/race.html Race and ethnicity data for NYSPACED are submitted by the medical provider reporting to the NYSDOH based on the patient’s medical record.6 Race and ethnicity for BMT referrals were documented in the medical record based on self-report at time of initial registration at RPCI. Adults were defined as: young 18–39 years, middle aged 40–64 years, or Medicare-eligible 65–75 years. Patients >75 years were not eligible for a BMT at RPCI during this time period. Disease risk was defined as low (first complete remission), intermediate (second or greater complete remission), or high (not in remission). Smoking status was coded as current, former, or never. Alcohol consumption was coded as never, social (≤1 drink/month), monthly (2–3 drinks/month), or weekly (4–8 drinks/week). Total household income was collected and analyzed as: <$25,000, $25,000–49,999, $50,000–74,999, and ≥$75,000. The median of each total household income category was divided by the total number of individuals within the household to create a variable estimating the amount of income support per person within a household. Patients with missing values or “I don’t know” responses on the DBBR questionnaire were coded in the lowest group for the following variables: education status (high-school or less) (N=7 missing), currently employed (no) (N=4 missing) and marital status (single, never married) (N=10 missing).
Statistical Analysis
We used NYSPACED to ascertain the average annual cases of leukemia, Hodgkin lymphoma, non-Hodgkin lymphoma, and multiple myeloma, aged 20–74 years and diagnosed 2005–2009 in the 8 counties of WNY. The proportion of EA and AA cases were available for Erie County and all of NYS (excluding New York City) for all ages. The proportion of each race (EA/AA) was applied to the average annual cases aged 20–74 for Erie County (using Erie County data) and the remaining 7 WNY counties (using the NYS, excluding NYC, data). We included BMT referrals over 6.7 year period, the average annual case rate was multiplied by 6.7 to estimate the new incident cases available for BMT referral.
Univariate comparisons of categorical variables used the Pearson chi-square test or ANOVA, as appropriate. Patients pending a decision regarding BMT were excluded from the analysis (N=45). Participants were not excluded from the analysis due to missing responses from the DBBR questionnaire. AA (N=12) and all other minorities (N=7) were combined as one group and compared with EAs due to the small number of minority patients. All statistical analyses were performed using SPSS Version 21 (2007, IBM). This study was reviewed and approved by the RPCI Institutional Review Board.
RESULTS
Population based analysis
Based on US census data from 2007–2011, the adult population aged 18–74 years in the 8 counties of WNY (the primary catchment area for RPCI) were 90% EA and 10% minorities (including 9.5% AA and <1% all other races/ethnicities) (Table 1). Based on US census data in the 8 counties of WNY, 59% of the Hispanic population and 48% of the AA population are less than 30 years old compared to 35% of the EA population. Since the minority populations in WNY are significantly younger than the EA population and younger than the median age of onset of hematologic malignancies, they have a low risk for developing hematologic malignancies or a rare need for BMT. This was confirmed in NYSPACED data demonstrating slightly less minorities (8% AAs, <1% all other races/ethnicities) among hematologic malignancy cases than in the general population.
Table 1.
Population based comparison of race distribution among adults aged 18–74 years residing in the main catchment area, hematologic malignancy cases diagnosed in the main catchment area, BMT referrals from the main catchment area, BMTs performed, participants in clinical trials, survey and/or biospecimen research
| European American | African American | Other | |
|---|---|---|---|
| US Census data 2007–2011, WNY | 90% | 9.5% | <1% |
| NYSPACED, 2005–2009 cases of acute and chronic leukemia, lymphoma and myeloma, WNY | 91% | 8% | <1% |
| Total Referrals to RPCI BMT program, 2005–2011, and resided in a WNY county | 90% | 8% | 2% |
| Total Referrals to RPCI BMT program, 2005–2011, regardless of residence | 90.5% | 7% | 2.5% |
| All patients who received a BMT at RPCI, 2005–2011 | 92% | 6% | 2% |
| Received a BMT at RPCI, 2005–2011, and resided in a WNY county | 91% | 7% | 2% |
| Proportion of BMT referrals who participated in biospecimen research, 2005–2011* | 95% | 95% | 88% |
| Proportion of BMT referrals who participated in survey research, 2005–2011* | 70% | 34% | 38% |
| Proportion of BMT referrals who participated in clinical trials, 2005–2011 | 62% | 57% | 43% |
NYSPACED: New York State Public Access Cancer Epidemiology Database (patients aged 20–74 years), RPCI: Roswell Park Cancer Institute, BMT: Blood or Marrow Transplant, WNY: Western New York State 8 counties of WNY includes: Erie, Niagara, Alleghany, Chautauqua, Cattaraugus, Cayuga, Genesee, Orleans and Wyoming.
Other: Asian, Native American, Hispanic
Proportion of those who were approached and consented
Source of RPCI BMT Referrals
All referrals of adults to RPCI for potential BMT, 2005–2011, who resided in one of the 8 counties of WNY, had the same proportion of AAs (8%) and slightly higher proportion of other races/ethnicities (2%) as the NYSPACED hematologic malignancy cases (Table 1). The total BMT referral population, regardless of primary residence, had slightly less AAs (7%) and slightly more other races/ethnicities (2.5%) than the NYSPACED hematologic malignancy cases. Referrals of WNY cases for BMT consultation differed by race and type of hematologic malignancy. The rates of referrals were higher for EAs compared to AAs for HL (23% vs.15%), NHL (16% vs 7%) and MM (40% vs 31%) but were lower for leukemia (35% vs. 40%).
Characteristics of RPCI BMT referrals
There were a total of 1,106 patients referred to the RPCI BMT program between January 2005 and August 2011 including 90.5% EAs, 7% AAs and 2.5% all other minorities (Table 1). About 75% of all referrals to the RPCI BMT program are from the 8 counties of WNY. The most common diagnoses among BMT referrals were leukemia, non-Hodgkin/Hodgkin lymphoma, and multiple myeloma (Table 2). There were more males in the EA referrals (58%), and more females in the AA (57%), and other minority (55%) referrals. More than half (62%) of EA and AA BMT referrals were between the ages of 40–64 years, whereas the majority (54%) of other minority groups were younger than 40 years (Table 2).
Table 2.
Characteristics of all patients referred for a BMT Consultation at RPCI between January 2005-August 2011, by Race
| European American (N=1000) n (%) |
African American (N=76) n (%) |
Other (N=30) n (%) |
P-Value | |
|---|---|---|---|---|
| Gender | 0.03 | |||
| Female | 423 (42) | 43 (57) | 16 (53) | |
| Male | 577 (58) | 33 (43) | 14 (47) | |
|
| ||||
| Age, years | 0.005 | |||
| <21 | 67 (7) | 6 (8) | 5 (17) | |
| 21–39 | 141 (17) | 13 (17) | 11 (37) | |
| 40–64 | 620 (62) | 47 (62) | 11 (37) | |
| 65–74 | 164 (16) | 9 (12) | 2 (7) | |
| ≥75 | 8 (1) | 1 (1) | 1 (3) | |
|
| ||||
| Diagnosis | 0.01 | |||
| Leukemia | 359 (40) | 26 (34) | 14 (47) | |
| NHL | 251 (25) | 8 (11) | 3 (10) | |
| MM | 166 (17) | 26 (34) | 5 (17) | |
| MDS | 72 (7) | 5 (7) | 1 (3) | |
| HL | 53 (5) | 4 (5) | 1 (3) | |
| MPN | 29 (3) | 1 (1) | 2 (7) | |
| Amyloidosis | 27 (3) | 1 (1) | 1 (3) | |
| Solid Tumor | 25 (3) | 1 (1) | 2 (7) | |
| Benign Hem. Disorder | 18 (2) | 4 (6) | 1 (3) | |
|
| ||||
| Received BMT | 0.05 | |||
| Yes - Total BMTs | 494 (49) | 31 (41) | 10 (33) | |
| Yes - Allo BMT | 270 (27) | 9 (12) | 6 (20) | |
| Yes - Auto BMT | 224 (22) | 22 (29) | 4 (13) | |
| No | 470 (47) | 38 (50) | 18 (60) | |
| Pending | 36 (4) | 7 (9) | 2 (7) | |
|
| ||||
| Participation in Research1 | <0.0001 | |||
| Yes | 430 (43) | 13 (17) | 6 (20) | |
| No | 570 (57) | 63 (83) | 24 (80) | |
Other: all other races/ethnicities, NHL: Non-Hodgkin lymphoma, MM: multiple myeloma, MDS: myelodysplastic syndrome, HL: Hodgkin lymphoma, MPN: myeloproliferative neoplasm, BMT: blood or marrow transplant
Includes survey research
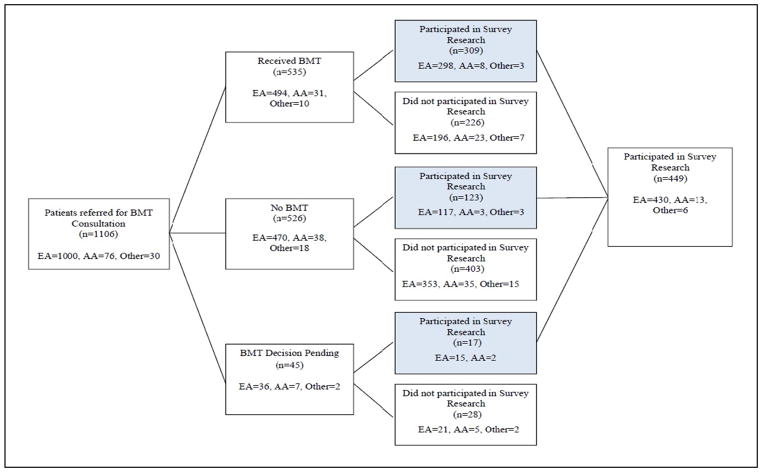
Overall, 535 (48%) patients received a BMT, however this varied by race (Table 2, Figure 1). Of all EA referrals, 49% received a BMT compared to 41% of all AA and 33% of all other minorities. Participation in survey research was highest among EA referrals (43%), with a small proportion of AA (17%) and other minorities (20%) participating in survey research. Participation in survey research was also higher for patients who had a BMT (58%) vs those who did not (23%).
Figure 1.
Patient Flow Chart
The reasons for not receiving a BMT are summarized in Table 3, and varied by race. Among EAs, the most common reasons for not receiving a BMT were patient decision/treatment reluctance (20%), stable disease not severe enough to warrant BMT (20%), death before BMT (19%) and disease progression (14%). Among AAs, the most common reason for not receiving a BMT was comorbidities/physician decision (29%), followed by death before BMT (16%), patient decision/treatment reluctance (13%), stable disease not severe enough to warrant BMT (13%) and transferred care to another center (13%). Other minorities’ most common reasons for not receiving a BMT were stable disease not severe enough to warrant BMT (22%), transferred care to another center (22%), death before BMT (17%), co-morbidities/physician decision (11%) and disease progression (11%). Importantly, in all races, failure to identify an allogeneic donor was a problem for only 4 EA and 2 AA patients.
Table 3.
Characteristics of all patients referred for a BMT consultation at Roswell Park Cancer Institute who did not receive a BMT, by Race
| Reason for not receiving a BMT | European American (N=470) | African American (N=38) | Other (N=18) |
|---|---|---|---|
| Patient Decision | 96 (20) | 5 (13) | 1 (6) |
| Stable Disease Not Requiring BMT | 94 (20) | 5 (13) | 4 (22) |
| Died before BMT | 88 (19) | 6 (16) | 3 (17) |
| Disease Progression before BMT | 67 (14) | 0 | 2 (11) |
| Co-Morbidities/Physician Decision | 55 (12) | 11 (29) | 2 (11) |
| Transferred care to another center | 41 (9) | 5 (13) | 4 (22) |
| Financial or Insurance Issues | 15 (3) | 0 | 0 |
| Psychosocial or compliance concerns | 9 (2) | 4 (11) | 0 |
| No Donor | 4 (<1) | 2 (5) | 0 |
| Age (too old for BMT) | 1 (<1) | 0 | 2 (11) |
BMT: Blood or Marrow Transplant, Other: all other races/ethnicities.
Assessment of Participation in Clinical Trials, Survey and Biospecimen Research by Race, among RPCI BMT Referrals
Table 1 shows the proportion of BMT referrals who participated in any therapeutic clinical trial, survey or biospecimen research, by race. For clinical trial participation, EA and AA rates were similar (62% and 57%, respectively) whereas other minority groups had a lower participation rate (13/30 or 43%). Table 5 summarizes the participation rates in survey and biospecimen research by race for all RPCI BMT referrals. While minority groups were approached more often (77% of AAs and 83% of other minorities) than EAs (75%), the rate of consent was lower among AAs (63% consented of those approached) and other minorities (64% consented/approached) than among EAs (81% consented/approached). Further drop-out occurred among AAs and other minorities since only 34% and 38% respectively of consented participants returned the survey (epidemiologic questionnaire) compared to a much higher rate of return for EAs (70%).A very high proportion of AAs provided a biospecimen (95%) which was identical to the EA rate, and higher than other minorities (88%).Only 19 minority patients participated in the survey and/or biospecimen research, therefore all minority groups are combined together.
Table 5.
Proportion of BMT referrals who were Approached, Consented and Participated in Survey or Biospecimen Research, by Race
| Patients Referred for BMT | EA N=1000 |
AA N=76 |
Other N=30 |
Total N=1106 |
|---|---|---|---|---|
| N (%) Approached by Research Staff of all BMT referrals | 747 (75%) |
60 (77%) |
25 (83%) |
832 (75%) |
| N (%) Consented of those Approached | 606 (81%) |
38 (63%) |
16 (64%) |
660 (79%) |
| N (%) Returned Survey of those Consented | 430 (70%) |
13 (34%) |
6 (38%) |
449 (68%) |
| N (%) Provided Blood Sample of those Consented | 575 (95%) |
36 (95%) |
14 (88%) |
625 (95%) |
| N (%) Returned Survey & Provided Blood Sample of those Consented | 410 (68%) |
13 (34%) |
10 (63%) |
433 (66%) |
EA: European American, AA: African American, Other: All other races/ethnicities
Characteristics of Patients who Did and Did Not Participate in Survey Research
Of the 430 EAs and the 19 minority patients who participated in survey research, there were significantly more minority than EA females (79% vs 44%, p=0.003). Age, highest level of education, smoking history and employment status did not differ by race. Minorities were more likely to have MM or amyloidosis (58% vs 26%, p>0.05), more likely to be single/never married (42% vs 13%, p=0.003), and never drinkers (63% vs 35%, p>0.05) than EAs. Minorities had a significantly lower number of people supported by their household income than EAs (42% vs 17% supporting only one person in household, p=0.01), which coincides with a higher rate of single/never married among minorities. Minority household incomes were significantly less than EA household incomes (42% minorities vs 15% EAs with <$25,000 annual income), which yields a median annual household income per person in the household of $10,417 for minority and $18,750 for EA households (p>0.05).
Table 6 compares the characteristics of the survey responders versus non-responders, by race. Among EA, the non-responders were more likely to be under 40 years and not undergo a BMT, with little difference by gender and underlying diagnosis. Among AA and other minority groups, non-responders were more likely to be male, under 40 years, have leukemia, and not undergo a BMT. The higher rate of responders among BMT patients is due to this protocol being part of the pre-BMT checklist to insure a high rate of patients approached to consider enrollment. Non-BMT hematologic malignancy services prioritize newly diagnosed patients be approached, with pre-treated patients having lower priority for enrolling in the survey and biospecimen repository.
Table 6.
Comparison of Survey responders versus non-responders by race
| Patient Characteristic | EA | AA | Other | |||
|---|---|---|---|---|---|---|
|
| ||||||
| Responder N=430 | Non- Responder N=570 | Responder N=13 | Non- Responder N=63 | Responder N=6 | Non- Responder N=24 | |
| Male | 239 (56%) | 338 (59%) | 3 (23%) | 30 (48%) | 1 (17%) | 13 (54%) |
| Age, years | ||||||
| <21 | 7 (2%) | 60 (11%) | 0 | 6 (10%) | 0 | 5 (21%) |
| 21–39 | 54 (13%) | 87 (15%) | 1 (8%) | 12 (19%) | 0 | 11 (46%) |
| 40–64 | 295 (69%) | 325 (57%) | 10 (77%) | 37 (59%) | 4 (67%) | 7 (29%) |
| 65–74 | 71 (17%) | 93 (16%) | 2 (15%) | 7 (11%) | 2 (33%) | 0 |
| ≥75 | 3 (1%) | 5 (1%) | 0 | 1 (2%) | 0 | 1 (4%) |
| Diagnosis | ||||||
| Leukemia | 139 (32%) | 220 (39%) | 1 (8%) | 25 (40%) | 3 (50%) | 11 (46%) |
| NHL | 106 (25%) | 145 (25%) | 1 (8%) | 7 (11%) | 0 | 3 (13%) |
| MM | 98 (23%) | 68 (12%) | 8 (62%) | 18 (29%) | 3 (50%) | 2 (8%) |
| MDS | 33 (8%) | 39 (7%) | 2 (15%) | 3 (5%) | 0 | 1 (4%) |
| HL | 19 (4%) | 34 (6%) | 1 (8%) | 3 (5%) | 0 | 1 (4%) |
| MPN | 10 (2%) | 19 (3%) | 0 | 1 (2%) | 0 | 2 (8%) |
| Amyloidosis | 13 (3%) | 14 (2%) | 0 | 1 (2%) | 0 | 1 (4%) |
| Solid Tumor | 6 (1%) | 19 (3%) | 0 | 1 (2%) | 0 | 2 (8%) |
| BHD | 6 (1%) | 12 (2%) | 0 | 4 (6%) | 0 | 1 (4%) |
| Decision Regarding BMT | ||||||
| Yes | 298 (69%) | 196 (34%) | 8 (62%) | 23 (37%) | 3 (50%) | 7 (29%) |
| No | 117 (27%) | 353 (62%) | 3 (23%) | 35 (56%) | 3 (50%) | 15 (63%) |
| Pending | 15 (3%) | 21 (4%) | 2 (15%) | 5 (8%) | 0 | 2 (8%) |
EA: European American, AA: African American, Other: All other races/ethnicities
DISCUSSION
The seemingly low rate of BMT referrals and utilization of BMT among minorities reflects the underlying distribution of minorities in the hematologic malignancy cases in the primary catchment area, indicating little to no disparity in referrals for transplant consultation. The higher proportion of people younger than 30 years old among minorities in the general population compared to EAs infers that as the population ages, the number of cancer cases in these minority groups should increase. However, prior research has demonstrated disparities in outcomes after BMT for minority patients,8–14 thus efforts should focus on identifying causes of worse outcomes in minorities and interventions to reduce them.
Our findings are in contrast to a prior national study using SEER incidence rates applied to US census data to calculate the annual number of new hematologic malignancy cases and CIBMTR data which captures approximately 55% of autologous, 50% of related allogeneic and >90% of unrelated allogeneic BMT to estimate the number of autologous and allogeneic BMTs performed in the US.2 While this study by Joshua, et al. reported significantly fewer BMTs for AAs and women, we found that the proportion of AAs who received a BMT was similar to the proportion of AAs diagnosed with a hematologic malignancy and the general adult population in the catchment area. While our study was confined to a smaller geographic area, we captured >95% of hematologic malignancy cases, 100% of BMT referrals and 100% of BMTs performed in this area. It is unknown if the difference in results between these 2 studies is due to 1) our catchment area being different from the rest of the US, 2) we had complete ascertainment of referrals and BMTs, 3) we restricted our study to adults while Joshua, et al.2 included pediatric cases and BMTs or 4) our study is more contemporaneous (2005–2011) than Joshua, et al. (1997–2002) 2 and racial disparities have decreased recently.
We found results similar to others,15 that EAs are more likely than AAs to participate in survey research, however to our knowledge this is the first report of similar rates of participation for biospecimen research by race. The low participation rate in survey research could be due to how a patient is approached and consented, a racial (mis)match between consenter and patient, or how often a patient is approached to participate. In addition, the structure and length of our survey (45–47 pages) may deter patients from participating in or comprehending the survey itself. However, we have no information on patients who did not participate or return the survey to understand causes of the differential participation rate.
There are several limitations to our population based study design. Three independent sources of data (US census, NYSPACED and RPCI BMT database) are not harmonized in the reporting of age groups (US census ≥18 years and NYSPACED ≥20 years) and race/ethnicity (self-report vs medical record). While 75% of our referrals derive from a limited geographic area (8 contiguous counties), the remainder are distributed across a wider catchment area making it difficult to measure referral rates by race/ethnicity from those regions. It is disappointing that less than half of our referrals participated in survey or biospecimen research, and we are unable to determine reasons why most declined participation (actively or passively).
Prior publications have described 4 factors that have demonstrated improvement in minority recruitment and retention in health-related research including: targeted/tailored sampling approach and identification of eligible participants, community involvement and timing of contact, incentives and logistical issues, and cultural adaptations for research participation.15–17 Thus, a more targeted approach to recruitment of minority subjects in survey research may yield a better response rate.
Table 4.
Characteristics of all patients referred for a BMT consultation who participated in Survey Research
| EA (N=430) | Other (N=19) | P-Value | |
|---|---|---|---|
| n (%) | n (%) | ||
| Gender | 0.003 | ||
| Female | 191 (44) | 15 (79) | |
| Male | 239 (56) | 4 (21) | |
|
| |||
| Age, years | NS | ||
| ≤ 20 | 7 (2) | 0 (0) | |
| 21–39 | 54 (13) | 1 (5) | |
| 40–64 | 295 (69) | 14 (74) | |
| 65–74 | 71 (17) | 4 (21) | |
| ≥ 75 | 3 (1) | 0 (0) | |
|
| |||
| Diagnosis | NS | ||
| CLL /NHL | 121 (28) | 2 (11) | |
| ALL/AML | 113 (27) | 2 (11) | |
| MM/Amyloidosis | 111 (26) | 11 (58) | |
| CML/MDS/MPN | 54 (13) | 3 (15) | |
| HL | 19 (4) | 1 (5) | |
| Benign Hem. Disorder | 6 (1) | 0 (0) | |
| Solid Tumor | 6 (1) | 0 (0) | |
|
| |||
| Received BMT | NS | ||
| Yes | 298 (69) | 11 (58) | |
| No | 117 (27) | 6 (32) | |
| Pending | 15 (3) | 2 (11) | |
|
| |||
| Smoking Status | NS | ||
| Current | 33 (8) | 1 (5) | |
| Former | 202 (47) | 8 (42) | |
| Never | 195 (45) | 10 (53) | |
|
| |||
| Alcohol Consumption | NS | ||
| Social | 97 (23) | 2 (11) | |
| Monthly | 82 (19) | 3 (16) | |
| Weekly | 102 (24) | 2 (11) | |
| Never | 149 (35) | 12 (63) | |
|
| |||
| Education Level | NS | ||
| High school or less | 146 (34) | 6 (32) | |
| Some College | 140 (33) | 7 (37) | |
| College Graduate or more | 144 (34) | 6 (32) | |
|
| |||
| Currently Employed | NS | ||
| No | 246 (57) | 12 (63) | |
| Yes | 184 (43) | 7 (37) | |
|
| |||
| Employment Status | NS | ||
| Full Time | 57 (13) | 3 (16) | |
| Part Time | 127 (30) | 4 (21) | |
| Unemployed | 246 (57) | 12 (63) | |
|
| |||
| Number of People in Household Support by Income | |||
| 1 | 73 (17) | 8 (42) | 0.01 |
| 2 | 189 (44) | 5 (26) | |
| ≥3 | 153 (36) | 4 (21) | |
| Missing | 15 (3) | 2 (11) | |
|
| |||
| Total Household Annual Income | 0.01 | ||
| <$25,000 | 65 (15) | 8 (42) | |
| $25–49,000 | 108 (25) | 6 (32) | |
| $50–75,000 | 99 (23) | 2 (11) | |
| >$75,000 | 101 (24) | 0 | |
| Unknown | 57 (13) | 3 (16) | |
|
| |||
| Median (range) Household | |||
| Income per person in household | $18,750 | $10,417 | NS |
| ($714–$75,000) | ($1,250–$37,500) | ||
|
| |||
| Marital Status | 0.003 | ||
| Married | 306 (71) | 8 (42) | |
| Separated/Divorced | 52 (12) | 2 (11) | |
| Single | 54 (13) | 8 (42) | |
| Widowed | 18 (4) | 1 (5) | |
EA: European American, Other: all other races/ethnicities, BMT: Blood and Marrow Transplant; CLL: chronic lymphocytic leukemia, NHL: non-Hodgkin lymphoma, ALL: acute lymphoblastic leukemia, AML: acute myeloid leukemia, MM: multiple myeloma, CML: chronic myeloid leukemia, MDS: myelodysplastic syndrome, MPN: myeloproliferative disorder, HL: Hodgkin lymphoma, NS: Not significant P>0.05
Highlights.
Hematologic malignancy referrals reflect the race distribution in the catchment area
BMT referrals had slightly less AAs but were enriched for other minority races
Participation in biospecimen research was high (>95%) and did not vary by race
Participation in survey research was significantly lower in minorities than whites
Acknowledgments
The Roswell Park Cancer Institute DataBank and Biorepository (DBBR) is a shared resource with partial funding provided by a Cancer Center Support Grant from the NIH (P30 CA016056).
Footnotes
This work was previously published as an abstract in Biol Blood Marrow Transplant 20: S110, 2014 (abstract #138) and presented as a poster at the Tandem BMT meeting in February 2014.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Deeg HJ, Sandmaier BM. Who is fit for allogeneic transplantation? Blood. 2010;116:4762–4770. doi: 10.1182/blood-2010-07-259358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Joshua TV, Rizzo JD, Zhang MJ, et al. Access to hematopoietic stem cell transplantation: effect of race and gender. Cancer. 2010;116:3469–76. doi: 10.1002/cncr.25297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gragert L, Eapen M, Williams E, Freeman J, Spellman S, Baitty R, Hartzman R, Rizzo JD, Horowitz M, Confer D, Maiers M. HLA match likelihoods for hematopoietic stem-cell grafts in the U.S. registry. New Engl J Med. 2014;371(4):339–348. doi: 10.1056/NEJMsa1311707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Landgren O, Gridley G, Turesson I, Caporaso NE, Goldin LR, Baris D, Fears TR, Hoover RN, Linet MS. Risk of monoclonal gammopathy of undetermined significance (MGUS) and subsequent multiple myeloma among African American and white veterans in the United States. Blood. 2006;107:904–906. doi: 10.1182/blood-2005-08-3449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cancer Reporting. Pursuant to New York State Public Health Law, Article 24, Title 1, Section 2401. [Accessed 2/1/2015];Cancer: duty to report. http://www.health.ny.gov/professionals/reportable_conditions/cancer/
- 6.Cancer Incidence - Public Use Data from 1996 to 2011, New York State Cancer Registry, New York State Department of Health, data as of November 2013. [Accessed 2/1/2015];About New York State Public Access Cancer Epidemiology Data (NYSPACED) https://www.health.ny.gov/statistics/cancer/registry/nyspaced/faq.htm#race.
- 7.Ambrosone CB, Nesline MK, Davis W. Establishing a cancer center data bank and biorepository for multidisciplinary research. Ca Epid Biomarker Prev. 2006;15:1575–77. doi: 10.1158/1055-9965.EPI-06-0628. [DOI] [PubMed] [Google Scholar]
- 8.Baker KS, Davies SM, Majhail NS, et al. Race and socioeconomic status influence outcomes of unrelated donor hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2009;15:1543–54. doi: 10.1016/j.bbmt.2009.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mielcarek M, Gooley T, Martin PF, et al. Effects of race on survival after stem cell transplantation. Biol Blood Marrow Transplant. 2005;11:231–239. doi: 10.1016/j.bbmt.2004.12.327. [DOI] [PubMed] [Google Scholar]
- 10.Savage D, Lindenbaum J, Van Ryzin J, Struening E, Garrett TJ. Race, poverty, and survival in multiple myeloma. Cancer. 1984;54:3085–3094. doi: 10.1002/1097-0142(19841215)54:12<3085::aid-cncr2820541246>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 11.Khaled Y, Abidi MH, Janakiraman N, et al. Outcomes after auto-SCT in African Americans with multiple myeloma. Bone Marrow Transplant. 2009;43:845–851. doi: 10.1038/bmt.2008.401. [DOI] [PubMed] [Google Scholar]
- 12.Hari PN, Majhail NS, Zhang MJ, et al. Race and outcomes of autologous hematopoietic cell transplantation for multiple myeloma. Biol Blood Marrow Transplant. 2010;16:395–402. doi: 10.1016/j.bbmt.2009.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Serna DS, Lee SJ, Zhang MJ, et al. Trends in survival after allogeneic hematopoietic stem cell transplantation for acute and chronic leukemia by ethnicity in the United States and Canada. J Clin Oncol. 2003;21:3754–60. doi: 10.1200/JCO.2003.03.133. [DOI] [PubMed] [Google Scholar]
- 14.Baker KS, Loberiza FR, Yu H, et al. Outcome of ethnic minorities with acute or chronic leukemia treated with hematopoietic stem cell transplantation in the United States. J Clin Oncol. 2005;23:7032–42. doi: 10.1200/JCO.2005.01.7269. [DOI] [PubMed] [Google Scholar]
- 15.Loberiza FR, Lee SJ, Freytes CO, et al. Methodological and logistical considerations to study design and data collection in racial/ethnic minority populations evaluating outcome disparity in hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2009;15:903–909. doi: 10.1016/j.bbmt.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yancey AK, Ortega AN, Kumanyika SK. Effective recruitment and retention of minority research participants. Ann Rev Public Health. 2006;27:1–28. doi: 10.1146/annurev.publhealth.27.021405.102113. [DOI] [PubMed] [Google Scholar]
- 17.Brown DR, Topcu M. Willingness to participate in clinical treatment research among older African Americans and Whites. Gerontologist. 2003;43:62–72. doi: 10.1093/geront/43.1.62. [DOI] [PubMed] [Google Scholar]