Abstract
Cognitive behavior therapy (CBT) is efficaciously and effectively used in the treatment of anxiety disorders; however, as CBT for anxiety routinely utilizes exposure components, clients often experience ambivalence about treatment and their clinicians often must deal with resistance. Motivational Interviewing (MI) is a therapeutic strategy that addresses ambivalence about change in clinical interventions. MI has been applied as an adjunct for treatments such as CBT in order to increase motivation for and commitment to the intervention, especially when components of the treatment may be challenging (e.g., exposure, cognitive restructuring). Though researchers have commented specifically on the use of MI as a supplement to CBT for anxiety disorders, no comprehensive review has systematically assessed the strengths and limitations of extant literature on the topic, nor across anxiety disorders. Findings are summarized from 6 case studies and uncontrolled trials and 11 randomized controlled trials published through March 2016. An integrated critique of this literature also is offered. Limitations and the preliminary nature of the work in this area notwithstanding, it appears that it is feasible to supplement or integrate CBT with MI and that doing so has the potential to improve treatment initiation and engagement, as well as clinical outcomes. A number of directions for future research are addressed, such as determining which MI approaches to implement, with whom, when, and in what contexts.
Keywords: Motivational Interviewing, CBT, anxiety, treatment outcomes, treatment onset
Anxiety disorders are prevalent and have detrimental impacts at both individual and societal levels (Goetzel, Hawkins, & Ozminkowski, 1999; Kessler et al., 2004; Kessler et al., 2012; Sanderson & Andrews, 2002). The evidence for cognitive behavior therapy (CBT) as a treatment of choice for mental disorders is strong, and particularly so for anxiety disorders (Butler, Chapman, Forman, & Beck, 2006; Hofmann et al., 2012). Exposure-related and cognitive restructuring methods are some of the most widely used and well-validated CBT intervention strategies for the treatment of anxiety disorders. Nevertheless, not all clients receiving CBT intervention for anxiety disorders achieve optimal treatment outcome (e.g., Hofmann et al., 2012; Olatunji, Cisler, & Deacon, 2010). By their very nature, CBT’s exposure and cognitive restructuring exercises can be distressing and difficult for clients, as contacting anxiety-provoking stimuli (physical and/or cognitive) and contingencies is required. Not surprisingly, noncompletion of exposure-related aspects of CBT often is cited as a significant barrier to clinical improvement (e.g., Cordioli et al., 2003; Maltby & Tolin, 2003; Purdon, Rowa, & Antony, 2004). Additionally, failure to seek treatment and premature termination of treatment are barriers to clinical improvement for clients with anxiety disorders generally (e.g., Abramowitz, Franklin, Zoellner, & DiBernardo, 2002; Demyttenaere et al., 2004; Grant et al., 2005; Wang et al., 2005). Dropout rates appear to be higher for the treatment of anxiety disorders as compared to other disorders such as major depressive disorder (e.g., Haby et al., 2005; Jacobson et al., 1996).
Given these barriers, strategies have been developed to improve client outcomes by bolstering rates of treatment utilization, completion of treatment, and engagement with critical components of treatment. One such strategy is increasing client/patient motivation (McNeil & Quentin, 2015), as low motivation frequently has been cited as the most common reason for treatment dropout and/or poor engagement with treatment (e.g., Bados, Balaguer, & Saldaña, 2007; Dugas et al., 2003). In addition to improving treatment engagement and rates of completion generally, increasing client motivation may reduce apprehension about challenging or intense exposure exercises, specifically (Maltby & Tolin, 2003), and/or cognitive restructuring exercises.
Motivational Interviewing (MI) was developed as a means to help clients resolve ambivalence about behavior change and to encourage and support motivation for and commitment to that change (Miller & Rollnick, 2013). The most current definition of MI indicates that it “is a collaborative, goal-oriented style of communication with particular attention to the language of change” and “is designed to strengthen personal motivation for change” (Miller & Rollnick, 2013, p. 29). Considered critical, the relational context of MI involves the following components: an attitude of collaboration rather than an authoritative style (i.e., “Partnership”), respect for the autonomy of the client/patient (i.e., “Acceptance”), promotion of the client’s welfare and prioritization of his/her needs (i.e., “Compassion”), and the evocation of the client/patient’s own motivation (versus the provision of this motivation from the therapist; i.e., “”Evocation”; Miller & Rollnick, 2013). Together, these four components make up “MI spirit.” In addition to operating under the umbrella of MI spirit, MI involves four processes: (a) engagement, or using person-centered, empathic listening; (b) focusing, or identifying a target for change that will be the primary subject of discussion in therapy (e.g., clarifying goals for treatment); (c) evoking, or supporting client motivation and eliciting change talk; and (d) planning, or using client expertise to implement change. Additionally, MI involves five core skills: (a) asking open-ended questions, (b) affirming, (c) reflective listenting, (d) summarizing, and (e) informing and advising. For a comprehensive description of MI, see Miller and Rollnick (2013).
A number of meta-analyses provide a strong indication that MI can yield moderate to large effects across a range of problem behaviors and health behavior change (e.g., Burke, Arkowitz, & Menchola, 2003; Burke, Dunn, Atkins, & Phelps, 2004; Hettema, Steele, & Miller, 2005; Lundahl, Kunz, Brownell, Tollefson, & Burke, 2010; Rubak, Sandbæk, Lauritzen, & Christensen, 2005). Though not all studies have demonstrated positive results, effect sizes as high as .75 and .77 have been observed for some MI-targeted behavior change, such as treatment compliance and risky behavior (e.g., substance abuse, unsafe sex practices) reduction, and across a variety of populations, including those that are medical, mental health, and/or predominantly comprised of racial and ethnic minority individuals.
MI can be applied to a wide variety of psychopathology and problem behaviors, partly because it can be complementary to other treatment strategies (Miller & Rose, 2009). Originally designed for the treatment of substance abuse (Miller, 1983), MI thereafter was applied to the treatment of other psychological disorders and health behavior problems (see Arkowitz, Westra, Miller, & Rollnick, 2015; McNeil, Hayes, & Randall, 2016; Rollnick, Miller, & Butler, 2008; and Westra & Arkowitz’s 2011 special issue in Cognitive and Behavioral Practice). Because it is grounded in theory (with relational and technical components; see Miller & Rose, 2009), offers specific strategies for improving motivation for change, and can be delivered in a relatively brief manner, MI also can be applied as an adjunct to, and in combination with, existing psychotherapeutic interventions such as CBT (e.g., Simpson & Zuckoff, 2011). MI, provided before or during anxiety treatment, may supplement and enhance CBT by increasing motivation for change and commitment to the intervention, ultimately improving clinical outcomes.
MI has, in fact, been utilized along with CBT for anxiety disorders, and a number of authors have provided a rationale for this integration and have suggested how to successfully combine the two treatment approaches (see Naar & Flynn, 2015; Slagle & Gray, 2007; Westra, Arkowitz, & Dozois, 2009; Westra, 2012; Westra & Dozois, 2008). Naar and Flynn (2015) suggested four major elements of CBT that are consistent with MI: (a) problem-oriented focus, (b) case formulation and treatment planning, (c) skills training and cognitive restructuring, and (d) behavioral activation. Slagle and Gray’s (2007) discussion of the utility of MI as an adjunct to exposure therapy for anxiety disorders includes a short review of literature demonstrating the efficacy of MI in anxiety disorder samples; they concluded that, given the few studies reviewed, utilizing MI with clients with anxiety disorders is beneficial. Likewise, Westra’s (2012) very brief summary of existing literature, and Westra, Aviram, and Doell’s (2011) concise review of similar literature are concluded with parallel statements: Preliminary research demonstrating the efficacy of using MI as an adjunct to CBT is promising. Though these summaries of extant literature are an important first step in integrating the available data on the use of MI as an adjunct to CBT for anxiety disorders, they do not systematically address the strengths and limitations of available empirical literature.
Purpose and Organization of the Critical Review
The purpose of this review is to offer a comprehensive summary and critical evaluation of currently available literature pertaining to the utilization of MI in combination with CBT for anxiety disorders. To amass the literature, Academic Search Complete, CINAHL, ERIC, Google Scholar, Medline, PsycARTICLES, and PyscINFO were searched. Search terms included “Motivational Interviewing” or “motivation enhancement (therapy)” and one of the following: “CBT,” “cognitive behavior therapy,” “exposure,” “exposure therapy,” “anxiety,” “Generalized Anxiety Disorder” (GAD), “Obsessive-Compulsive Disorder” (OCD), “Panic Disorder,” “Posttraumatic Stress Disorder” (PTSD), “Social Phobia,” “Social Anxiety Disorder” (SAD), and “Specific Phobia.” For the purposes of this review, only empirical articles published by the end of March 2016 in English and in peer-reviewed journals were included. More specifically, to be included, articles had to quantifiably assess treatment outcomes and/or engagement for participants who did or did not receive MI or similar motivation enhancement therapy in conjunction with standard CBT for an anxiety disorder as a principal diagnosis. To comprehensively evaluate this emerging literature, both uncontrolled and controlled clinical studies were included and no criteria were set for type of participant or intervention setting. Furthermore, studies were not excluded from this review based on how treatment outcomes and/or engagement were assessed, nor based on the time course of treatment or follow-up.
In total, 17 articles were reviewed (see Figure 1 for summary of article selection). Articles describe case studies or uncontrolled trials (n = 6) and randomized controlled trials (RCT; n = 11). First, study findings are presented independently, arranged by study design (i.e., uncontrolled or case studies versus controlled studies), participant sample type (i.e., diagnosis), and study outcome variable (i.e., treatment initiation/engagement versus clinical outcomes). Then, a critical analysis of study strengths and limitations across the literature is provided. Critiques cover conceptual and methodological issues that are directly relevant to understanding how MI may be applied along with CBT for anxiety disorders. The review integrates and defines broadly the state of extant literature, highlights the strengths and limitations of this body of work, and provides directions for future research.
Figure 1.
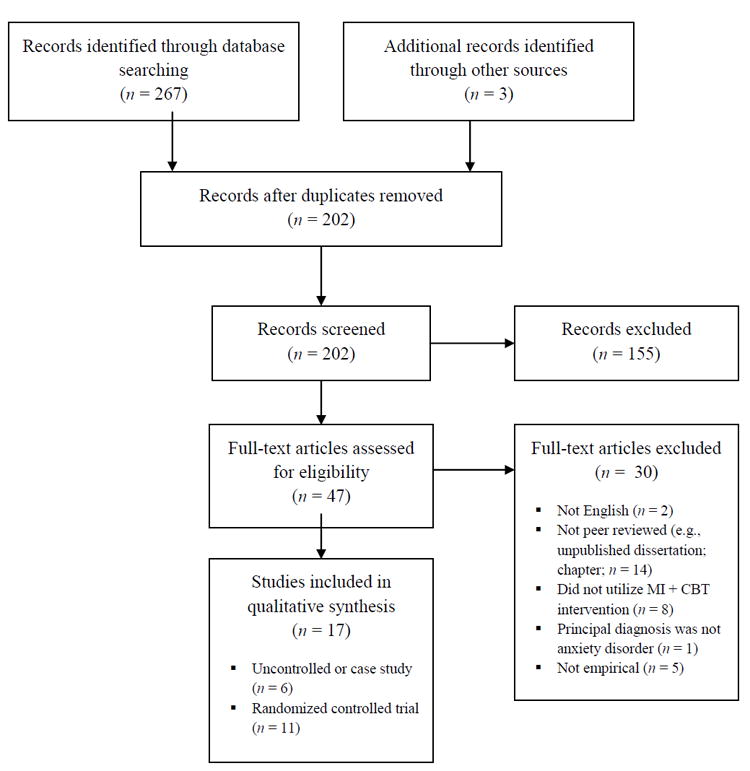
Selection of articles for the critical review
Review of the Literature
Case Studies and Uncontrolled Trials
Mixed Anxiety and Depression
Westra (2004) published the first known study on the application of MI to CBT for individuals with anxiety disorders. The paper is a collection of three case studies that highlight how MI, adapted for anxiety and depression, can increase motivation and target resistance to CBT for clients with mixed anxiety and depression. In the first case, a 5-session MI prelude to CBT for SAD, panic disorder with agoraphobia, and a major depressive episode was used to address a strong hesitancy to begin treatment. Following MI, the client agreed to initiate and subsequently completed 10 sessions of CBT in which she was fully engaged. Based on this case, Westra (2004) concluded that CBT, rather than MI alone, led to clinically significant change, and that pre-CBT MI may engage those who are initially wary to take an active approach to treatment. Westra (2004) presented two other cases, one of a client with GAD who previously did not respond well to CBT, and another of a client with SAD and major depressive disorder who previously demonstrated only a mild response to CBT. Drawing on the clinical outcomes of these clients following 4- or 5-session courses of MI, Westra (2004) suggested that MI may be a treatment option for clients who do not respond to standard CBT and that MI has the potential to serve as an adjunct to CBT when treatment response is only partial. Important clinically, Westra (2004) emphasizes that particular client states may necessitate a shift from CBT to MI so as to enhance motivation, such as when clients are reluctant to begin CBT or when CBT elicits insufficient treatment response.
Hypochondriasis
McKay and Bouman (2008) described three cases in which monosymptomatic hypochondriasis was treated with CBT, following a series of between 5 and 8 MI sessions. Each of the clients previously had received extensive psychotherapy (reportedly, mostly psychodynamic). For all three cases presented, once-weekly therapy sessions lasted 50 minutes each and the entire course of treatment ranged from 12 to 31 sessions. According to the authors, MI was intended to “weaken the strength of the belief in the presence of illness or disease” (McKay & Bouman, 2008, p. 157). Immediately following MI and CBT, scores on anxiety and depression measures were decreased for all three clients, and these reductions were maintained at 6-month follow-up. The authors concluded that “MI is promising as an adjunct to treatment for monosymptomatic hypochondriasis” (McKay & Bouman, 2008, p. 164). Of clinical importance is that in each of the presented cases, there was one “critical” session in which MI facilitated lowered belief conviction about health concerns, then allowing more intensive CBT.
OCD
Riccardi, Timpano, and Schmidt (2010) presented a clinical case study of a patient with OCD (with contamination obsessions and washing compulsions) who was treated with MI methods integrated into standard CBT. The 20 weekly 50- to 60-minute psychotherapy sessions were completed over the course of 6 months, and MI methods were infused into these sessions as necessary, particularly when hesitation about treatment, especially exposure exercises, was encountered. At the end of treatment, the client’s scores on measures of OCD symptomatology no longer were in the clinical range and daily time-in-shower had been decreased from approximately 325 minutes at intake to approximately 15 minutes. Treatment gains were maintained 6 months after treatment termination. The authors concluded that integrating MI into CBT for OCD may enhance the efficacy of standard treatment by increasing perseverance during exposure exercises (Riccardi et al., 2010).
Simpson, Zuckoff, Page, Franklin, and Foa (2008) described an open pilot trial in which six clients with a principal diagnosis of OCD and at least moderate OCD severity were treated with three MI sessions prior to initiating a 15-session course of CBT for OCD. Additionally, an MI module was available for integration into standard CBT in the event that resistance became a barrier to the patient’s treatment (used almost every session for one participant, “frequently” for three clients, and not required for use for two clients). Two clients previously had engaged in CBT. Clients’ OCD symptomatology was the primary outcome measure and was assessed at baseline, post-MI, midway through CBT, and at termination. Of the six clients, four completed the full course of treatment, with one dropping out at Session 4 due to refusal to complete exposure exercises, and another at Session 13 due to work-related responsibilities. Scores on measures of OCD symptomatology decreased across treatment, most notably from baseline to termination. At termination, only one treatment-completing patient demonstrated moderate OCD symptomatology; all others were in remission. OCD symptoms did not decrease following only MI sessions. The authors commented that firm conclusions could not be drawn from the pilot study, as it was an open trial that included only a small sample. Still, they suggested that it is feasible to utilize MI as an adjunct to standard CBT and that MI may need to be delivered more frequently for some clients, depending on their readiness to change.
Drawing from their preliminary data suggesting that MI could be added to CBT for OCD, Simpson and Zuckoff (2011) completed a series of case studies addressing whether MI could be used to facilitate initiation of an evidence-based treatment for OCD clients. There were six clients with histories of refusing evidence-based treatment for OCD who received four 1-hour sessions of MI. MI was intended to increase motivation for change for these clients so that they would subsequently initiate treatment for OCD. Symptom severity was measured by independent evaluators before and after the MI intervention, and initiation of treatment for OCD at 1-month follow-up was considered the primary outcome variable. Across the clients, scores on measures of OCD symptom scores did not change from pre- to post-MI assessment. None of the three clients whose OCD symptoms included compulsive hoarding reported initiating treatment following the MI intervention; however, all three others reported pursuing an evidence-based treatment for OCD at follow-up. Simpson and Zuckoff (2011) concluded that MI alone does not lead to reduction in OCD symptoms but may lead some treatment-refractory OCD clients to commit to evidence-based treatment.
Social Anxiety Disorder (Social Phobia)
Buckner (2009) presented a case description in which an intervention designed to increase motivation to engage in treatment was utilized to facilitate initiation of CBT. A client with SAD who never had received treatment for her social anxiety completed three MI-congruent sessions lasting 3.5 hours in total. The client’s ratings of her own confidence to change and her willingness to schedule a CBT appointment increased markedly. The client, at 1-month follow-up, had initiated CBT. Furthermore, the client attended all CBT sessions and demonstrated perfect homework compliance. Scores for one measure of social anxiety dropped from clinically significant at pretreatment to within normal range over the course of the MI sessions, while scores on similar measures did not reflect this trend. At 1-month follow-up, after CBT had been initiated, scores on all measures of social anxiety were near normal range. Buckner (2009) concluded that, in addition to increasing treatment engagement, MI may be useful for enhancing entry into CBT for individuals with social anxiety who have not previously sought treatment.
Randomized Controlled Trials
PTSD
In an RCT, Murphy, Thompson, Murray, Rainey, and Uddo (2009) assessed whether a 4-session (1.5 hours long each), group-based motivation enhancement intervention, based on MI, improved engagement of military veterans participating in a group-based CBT intervention for PTSD. Study participants were randomly assigned to receive either the motivation enhancement group or a control group that received psychoeducation. Motivation enhancement, which most notably included the creation of a decision-balance worksheet completed in MI spirit, or psychoeducation, occurred in the second month of the year-long PTSD intervention. Outcome variables included attendance and dropout data obtained from hospital charts for the 10 months following the motivation enhancement or control interventions, and ratings of problem-specific readiness to change. No significant differences emerged between the study groups on pretestposttest changes in some readiness to change scores; however, the motivation enhancement group participants, compared to those in the control group, changed a significantly higher percentage of self-listed problems from “might have” to “definitely have” on a problem identification form that was completed prior to treatment and revisited later during treatment. A large effect size was reported for this between-group difference (Cohen’s d = 0.86), suggesting that the motivation enhancement group participants were better able than control participants to resolve ambivalence by categorizing issues that were thought to potentially be problems (i.e., “might have”) as in fact present (i.e., “definitely have”) so they could be targeted in treatment. Most importantly, the motivation enhancement group participants also had higher attendance rates than their control group counterparts (Cohen’s d = 0.37) and participants in the treatment group remained in the CBT program for a longer period of time before dropping out than participants in the control group (Cohen’s d = 0.47). These findings, which were moderate to large in effect, led to the conclusion that there is support for inclusion of strategies that increase readiness to change in PTSD treatment, although noting the study was preliminary in nature.
Mixed Anxiety Sample
Westra and Dozois (2006) examined whether participants who received three sessions of MI prior to group CBT for anxiety disorders demonstrated greater treatment engagement and clinical gains over participants who received no pretreatment intervention. Participants in this pilot study had a principal diagnosis of panic disorder, SAD, or GAD. CBT completion rates did not differ between the treatment groups, nor did therapist-rated indices of homework completion. While both treatment groups demonstrated reductions in clinical outcome measures, the pre-CBT MI group showed significantly greater reductions than did the control group. Effect sizes for the difference between the pre-CBT MI and control groups were large for participants with GAD and panic disorder (Cohen’s d = 1.29 and Cohen’s d = 0.69, respectively), and moderate for participants with SAD (Cohen’s d = 0.44). Though 75% of the treatment group demonstrated clinically significant reductions in problems (i.e., no longer meeting diagnostic criteria, or scoring below a pre-identified cut score), only 50% of the control group demonstrated these reductions, a statistically significant group difference. At 6-month follow-up, gains were maintained equally by the treatment groups. Westra and Dozois (2006) concluded that there is strong but preliminary support for including a brief pre-CBT intervention to improve engagement in and response to CBT for clients with anxiety disorders; however, MI was not compared to other pretreatment interventions that could be just as efficacious at improving CBT outcomes.
GAD
Following the Westra and Dozois (2006) pilot study, Westra et al. (2009) completed a preliminary RCT to determine whether individuals who received a series of four, 50-minute sessions of MI prior to CBT for GAD differed in posttreatment measures of worry, compared to individuals in a 4-week waiting-list control group who completed only CBT. The eight sessions of individual CBT (six weekly 2-hour sessions, then two 1-hour sessions) were completed by therapists who were blind to participants’ pretreatment group. Participants receiving MI prior to CBT showed lower levels of worry post-CBT (Cohen’s d = 0.53), and a greater percentage of post-CBT worry levels in the nonclinical rage, than their counterparts in the control group. These between-group effects were not observed on other measures of psychopathology. Additionally, those receiving pre-CBT MI completed significantly more homework (Cohen’s d = 0.59) than those in the control group, which partially mediated the relation between treatment group and clinical outcome (i.e., worry reduction). The treatment group effect on worry reduction no longer was apparent at 6- and 12-month follow-up. The percentage of participants in each treatment group who met diagnostic criteria for GAD following treatment was not significantly different across the groups. The authors concluded that there may be some benefit in adding MI as a pretreatment adjunct to CBT for the reduction of worry symptoms. Westra and colleagues also pointed out that supplementing CBT with MI may be especially beneficial for individuals with high worry symptom severity.
In a follow-up to the 2009 study by Westra and colleagues, Aviram and Westra (2011) assessed whether participants with GAD who received pre-CBT MI demonstrated differences in resistance and homework compliance (both measured by standardized coder- or clinician-completed assessment tools) as compared to participants in a waiting-list control group. Significant differences emerged between treatment groups in resistance, with a large effect size (Cohen’s d = 1.45) and treatment group accounting for 36% of the variance in resistance. Pre-CBT MI was associated with reduced resistance, even when compared to decreases in resistance observed after the same number of CBT sessions in the control group. Contrary to the authors’ hypothesis, the effect of resistance on treatment outcome, as measured by worry measure scores, was direct and not mediated by homework compliance. Also, there was no direct effect of treatment group on homework compliance. Aviram and Westra (2011) ultimately concluded that, for GAD clients with severe worry behavior, receiving MI as a prelude to CBT for GAD is associated with reduced resistance and better treatment engagement, which in turn is associated with reduced worry behavior. This finding extends the results of earlier work to suggest that reduction in resistance and an enhancement in treatment engagement may be the mechanism by which pre-CBT MI improves treatment outcomes compared to CBT alone.
OCD
In the first known RCT addressing the addition of MI to CBT for OCD, Maltby and Tolin (2005) randomized clients who had refused exposure and response prevention (ERP) to either a 4-session treatment readiness intervention based on MI or a waiting-list control condition. Maltby and Tolin (2005) reported that the readiness intervention was associated with greater likelihood of CBT initiation (86%) as compared to the waitlist control group (20%), but did not yield changes in severity of OCD. Nevertheless, half of the participants who completed the readiness intervention prematurely dropped out of the CBT treatment; however, all of those participants who completed CBT demonstrated reductions in OCD behavior, ranging from those with mild to severe symptomatology. Maltby and Tolin (2005) concluded that there is initial support that a motivation-enhancing intervention delivered prior to CBT for OCD may increase rates of acceptance of ERP and, ultimately, treatment initiation.
Drawing on earlier open pilot trials described above, Simpson and colleagues (2010) completed an RCT in which participants with at least moderate OCD were assigned to receive 15 (90-minute, twice-weekly) ERP sessions following three standard introductory sessions, or the same treatment with three MI introductory sessions. For the group receiving the pre-CBT MI, a short MI module was available for use when resistance was encountered during exposure exercises, although frequency of use was not noted. There were no differences in dropout rate between the treatment groups. There also were no differences between treatment groups in the number of completed exposure exercises. Clients in both treatment groups demonstrated clinically significant decreases in OCD severity, and there was no significant difference in clinical outcome between the groups. Simpson and colleagues (2010) suggested that, even with these results, it still is premature to conclude that CBT treatment adherence for OCD clients cannot be improved by MI.
In another RCT, Meyer and colleagues (2010) treated participants with OCD with 12 weekly 2-hour group CBT sessions. Half of the participants were randomly assigned to receive two, 1-hour individual MI plus Thought Mapping (Lukefeld, Brown, Clark, Godlaski, & Hays, 2000) sessions prior to the group-CBT for OCD. (Thought Mapping is a structured approach to understanding the relations between thoughts and actions that involves the creation of visual aids.) The remaining participants received two, 1-hour individual therapy sessions that included psychoeducation related to smoking prevention and physical activity in order to control for therapist contact encountered by the treatment group. Following treatment, the mean reduction in OCD severity was significantly greater for the treatment group than for the control group, a finding that also was observed at 3-month follow-up. Additionally, a significantly greater number of participants in the treatment group experienced full remission, as compared to the control group. Meyers and colleagues (2010) concluded that there is initial support for adding MI and Thought Mapping to group CBT for OCD.
Merlo and colleagues (2010) also completed an RCT assessing the benefit of adding MI to CBT for OCD, but with a pediatric population (ages 6–17 years) who were randomly allocated to receive up to 14, 90-minute CBT sessions for anxiety, delivered over 3 weeks, following either three MI sessions or three psychoeducation sessions. MI and control sessions lasted approximately one-half hour and were completed immediately before CBT Sessions 1, 4, and 8. At posttreatment, symptom severity scores and change scores were not significantly different between the treatment and control groups, though the group receiving MI did show a more rapid decline in these scores earlier in treatment. There was a difference in number of therapy sessions attended across the treatment groups, with the group receiving MI attending significantly fewer sessions (though not terminating treatment against the advice of their therapist). The authors concluded that supplementing CBT for pediatric OCD with MI may accelerate treatment progress.
Social Anxiety Disorder (Social Phobia)
Buckner and Schmidt (2009) studied whether MI could be utilized to improve CBT initiation for individuals with social anxiety. In an RCT, participants were assigned to receive Motivation Enhancement Therapy, a 3-session (approximately 1.75 hours each) pre-CBT intervention, following a short psychoeducation session about CBT for social anxiety. Half of the participants were assigned to a control group that received only the brief psychoeducation session. Considerably more (58.3%) participants in the Motivation Enhancement Therapy group attended a CBT appointment, compared to only 13.3% of control participants, a statistically significant difference. Buckner and Schmidt (2009) suggested that a pre-CBT motivation enhancement based on MI may increase CBT utilization among socially anxious individuals.
In the only known RCT addressing the addition of MI-congruent motivational enhancement strategies to Internet-based CBT (iCBT), Titov and others (2010) studied a sample of participants with SAD. Half of the participants were randomly allocated to the iCBT (i.e., treatment as usual) group and the other half were randomly allocated to the iCBT plus motivational enhancement group. (iCBT for SAD is an Internet-based program that leads clients though self-guided psychoeducation, fear hierarchy development, graduated exposure exercises, and cognitive restructuring; Titov et al., 2010). Participants who received motivational enhancement strategies were given, prior to iCBT, MI-congruent questions to consider regarding their SAD and treatment. Controlling for pretreatment scores, the authors did not find significant differences between the treatment and control groups in posttreatment scores on measures of social anxiety; participants in both treatment (Cohen’s d = 1.16) and control groups (Cohen’s d = 1.15) demonstrated reduced anxiety symptoms. The lack of between-group differences continued at 3-month follow-up. Significantly more participants in the treatment group (75%) completed the program than did those in the control group (56%). Titov and colleagues (2010) concluded that there was no evidence that adding Internet-based motivational strategies to Internet-based CBT for SAD is beneficial compared to standard Internet-based CBT, but that the addition of MI-congruent strategies may improve treatment completion.
Anxiety in Traumatic Brain Injury (TBI) Patients
Hsieh (2012) and colleagues completed a pilot RCT to assess whether addition of pretreatment MI to CBT for anxiety would improve clinical outcomes over standard CBT for TBI patients with an anxiety disorder. Participants in the treatment group received three weekly individual MI sessions before beginning individual CBT for anxiety (MI + CBT). Participants in a nondirective counseling group received three weekly sessions of supportive therapy to establish rapport prior to beginning individual CBT for anxiety (NDC + CBT); this group was included to control for therapeutic attention received by the treatment group. Lastly, a control group received treatment as usual, which did not include CBT but may have included occupational therapy or neuropsychological assessment and rehabilitation. Both the MI + CBT and the NDC + CBT groups showed significant reductions on one measure of anxiety from baseline to post-CBT, with a larger effect size observed for the MI + CBT group (Cohen’s d = 0.50) than for the NDC + CBT group (Cohen’s d = 0.24). The authors concluded that adding MI to CBT for anxiety in TBI clients may result in improved outcomes.
Critique of the Literature
Experimental Issues
Sampling Considerations
Table 1 provides an overview of selected sample characteristics, as well as other study features, for the included literature. Many of the studies include community samples with participants of a range of reported ages (e.g., Aviram & Westra, 2011; Maltby & Tolin, 2005; Simpson et al., 2010), although 2 of the 17 studies (Westra, 2004; Westra & Dozois, 2006) did not explicitly report participant ages. With regard to gender, a few studies oversampled women (Buckner & Schmidt, 209; Meyer et al., 2010; Westra & Dozois, 2006), although that may reflect the gender distribution of many anxiety disorders. Two studies oversampled men (Hsieh et al., 2012; Murphy et al., 2009), likely a function of the disorder being targeted (i.e., PTSD in veterans, anxiety in brain injury patients).
Table 1.
Summary of Studies Included in the Critical Review and Key Conclusions
| Study Author(s) | Study Type | n | Age M (SD) | % or # Female | Sample | Experimental Treatment | Main Outcome Variable(s) | Key Conclusion(s) |
|---|---|---|---|---|---|---|---|---|
| Aviram & Westra (2011)* | RCT | 35 | 40.73 (11.41) | 80% | GAD | Pre-CBT MI | Resistance in CBT; Homework compliance | Pre-CBT MI is associated with reduced resistance in treatment and better treatment engagement |
| Buckner (2009) | Case study | 1 | 19 | 1 | Social Anxiety Disorder | Pre-CBT MI | CBT initiation; Remission of symptoms | MI increases CBT treatment engagement; MI may be useful for improving the utilization of CBT for individuals not actively seeking treatment |
| Buckner & Schmidt (2009) | RCT | 27 | 18.8 (0.8) | 63% | Social Anxiety Disorder | Pre-CBT MI | Interest in pursuing CBT; CBT initiation | Pre-CBT motivation enhancement may increase CBT utilization among socially anxious people who have not sought treatment |
| Hsieh et al. (2012) | RCT | 27 | 38.0 (13.2) | 22.2% | TBI patients with at least one anxiety disorder | Pre-CBT MI | Anxiety symptomatology; Stress; Non-productive coping | Adding MI to CBT for anxiety may result in improved clinical outcomes |
| Maltby & Tolin (2005) | RCT | 12 | 38.8 (12.8) | 48.6% | OCD | Pre-CBT MI | CBT initiation; OCD symptomatology; CBT drop-out | Pre-CBT motivation enhancement may increase rates of acceptance of ERP and treatment (i.e., CBT) initiation |
| McKay & Bouman (2008) | Case study | 3 | 37.7 | 2 | Monosymptomatic Hypochondriasis | Pre-CBT MI | Anxiety and depression symptomatology; Belief conviction | MI is a promising as an addition to standard treatment for hypochondriasis |
| Merlo et al. (2010) | RCT | 16 | 13.3 (3.0) | 37.5% | Pediatric OCD | Integrated MI/CBT | OCD symptomatology | Supplementing CBT for pediatric OCD with MI may accelerate |
| Meyer et al. (2010) | RCT | 93 | 38.6 (12.5) | 75.3% | OCD | Integrated MI and Thought Mapping | OCD symptomatology | There is initial support for adding MI to group CBT for OCD to produce greater reductions in OCD symptomatology and to enhance remission |
| Murphy et al. (2009) | RCT | 114 | 56.2 (6.7) | 0% | PTSD | Pre-CBT MI | Treatment engagement; CBT dropout | There is support of the inclusion of strategies that increase readiness to change in CBT for PTSD |
| Riccardi et al. (2010) | Case study | 1 | 39 | 0 | OCD | Integrated MI/CBT | OCD symptomatology | Integration of MI into CBT may enhance efficacy of treatment for OCD |
| Simpson & Zuckoff (2011) | Case study | 6 | 51.2 | 4 | OCD | Pre-CBT MI | Treatment (CBT or medication) initiation | MI alone does not result in reduction of OCD symptoms, but may lead some OCD clients to commit to evidence-based treatment (CBT) |
| Simpson et al. (2010) | RCT | 30 | 39.9 (13.4) | 47% | OCD | Pre-CBT MI + 1 integrated MI/CBT session | Patient adherence to CBT; OCD symptomatology | Though pre-CBT MI did not yield better outcomes than MI alone, it is premature to conclude that CBT treatment adherence cannot be improved by MI |
| Simpson et al. (2008) | Case study | 6 | 40.2 | 4 | OCD | Pre-CBT MI + 1 integrated MI/CBT session | OCD symptomatology | It is feasible to utilize MI as an adjunct to standard CBT; MI may need to be delivered more frequently for some clients than for others |
| Titov et al. (2010) | RCT | 113 | 43.6 (14.6) | 47% | Social Anxiety Disorder | Pre-CBT MI (Internetbased | Internet-based CBT completion rates; Social Anxiety Disorder symptomatology | Adding motivational strategies to Internet-based CBT for SAD may not improve CBT outcomes but may improve treatment completion |
| Westra (2004) | Case study | 3 | NA | 3 | Mixed anxiety and depression | Pre-CBT MI | CBT initiation; Anxiety and depression symptomatology | MI is a treatment option for clients who do not respond to standard CBT; MI can serve as adjunct to CBT when treatment response is only partial |
| Westra et al. (2009) | RCT | 76 | 41.9 (12.4) | 67% | GAD | Pre-CBT MI | GAD symptomatology (worry); CBT homework completion | Pre-CBT MI may increase efficacy of CBT for anxiety disorders, especially for more severe cases |
| Westra & Dozois (2006) | RCT | 55 | 38.0 (11.0) | 70% | Panic Disorder; Social Anxiety Disorder; GAD | Pre-CBT MI | Anxiety symptomatology; CBT homework completion | Brief pre-CBT MI interventions may improve engagement in and response to CBT for anxiety disorders |
Notes:
Secondary data analysis of Westra et al. (2009) study data; RCT = randomized controlled trial; NR = not reported; GAD = Generalized Anxiety Disorder; OCD = Obsessive-Compulsive Disorder; CBT = Cognitive Behavior Therapy; MI = Motivational Interviewing.
Ethnicity/race of study participants was not reported in just under half of the articles reviewed (Hsieh et al., 2012; Maltby & Tolin, 2005; McKay & Bouman, 2008; Meyer et al., 2010; Titov et al., 2010; Westra, 2004; Westra & Dozois, 2006). Considering race and ethnicity is important for establishing the external validity and applicability of clinical research (Morales & Norcross, 2010). Socioeconomic status, or a proxy for it, was reported for participants of a number of the included studies, though eight failed to report this important demographic variable (Maltby & Tolin, 2005; McKay & Bouman, 2008; Merlo et al., 2010; Meyer et al., 2010; Murphy et al., 2009; Riccardi et al., 2010; Titov et al., 2010; Westra, 2004).
As most of the studies presented in this review are preliminary in nature, they contain samples that are rather homogeneous with regard to patient population and Diagnostic and Statistical Manual of Mental Disorders diagnoses (currently in 5th edition, though included studies used earlier editions; DSM-5; American Psychiatric Association, 2013). This homogeneity is a strength in terms of drawing conclusions about treatment efficacy, but may hinder external validity and inferences that can be drawn about effectiveness (Kazdin, 2003). Six of the reviewed studies did not report whether participants had comorbid psychological problems (Maltby & Tolin, 2005; McKay & Bouman, 2008; Merlo et al., 2010; Murphy et al., 2009; Simpson et al., 2011; Titov et al., 2010). For the studies that did report comorbidities, depression, dysthymia, and anxiety disorders were the most common additional diagnoses. As comorbid conditions have the potential to greatly impact treatment response (Steele & Roberts, 2005), lack of reporting makes it difficult to completely appreciate the implications for effectiveness (and generalizability) of some of the reviewed studies. Participant history effects (i.e., prior contact with treatment) also can impact treatment response and should therefore be reported in clinical research (Finger & Rand, 2005; Kazdin, 2003). The studies reviewed varied in whether included samples were naïve to treatment or had a history of treatment; however, a few articles did not report whether participants had past psychological treatment, a notable limitation (Aviram & Westra, 2011; Merlo et al., 2010; Meyer et al., 2010; Murphy et al., 2009). Current use of psychotropic medication or concurrent behavioral treatment was reported by most of the study authors; however, three articles also failed to report this information (Maltby & Tolin, 2005; McKay & Bouman, 2008; Titov et al., 2010).
Procedural Considerations
In treatment studies such as those reviewed here, treatment fidelity is essential to both the internal and external validity of the findings as well as to the reproducibility of results (Kazdin, 2003). Essentially all of the studies critiqued reported that MI or MI-consistent therapeutic methods were utilized; therefore, it is important to evaluate these studies on their measurement and/or reporting of MI-related treatment fidelity. For interventions such as those described in the reviewed studies, treatment fidelity can be supported through a number of techniques, including use of standardized training manuals and structured practice (via role-play or standardized clients), ongoing training or regular training booster sessions, involvement of trainees who have trained as trainers (in the Motivational Interviewing Network of Trainers [MINT; www.motivationaltraining.org]), ongoing weekly supervision with provision of opportunities for consultation, and regular observation of psychotherapeutic interactions, and/or systematic coding of those interactions to confirm adherence to treatment protocol (see guidelines from the Treatment Fidelity Workgroup of the NIH Behavior Change Consortium; Bellg et al., 2004). Only 6 of the 17 included studies reported that treatment fidelity was measured for the experimental treatment, MI, via regular observation with coding of the psychotherapeutic interaction (Aviram & Westra, 2011; Buckner & Schmidt, 2009; Hsieh et al., 2012; Simpson et al., 2010; Simpson & Zuckoff, 2011; Westra et al., 2009). In all but one of these cases (Hsieh et al., 2012), researchers relied on the Motivational Interviewing Treatment Integrity Code 2.0 (MITI; Moyers, Martin, Manuel, Hendrickson, & Miller, 2005) or 3.0 (Moyers, Martin, Manuel, Miller & Ernst, 2007), a widely used and well-validated system for formally coding and assessing MI treatment fidelity. Two studies (Simpson et al., 2008; Westra & Dozois, 2006) reported on the extensive training of MI therapists, including trainers’ association with MINT.
Of the 17 reviewed studies, 10 indicated that the experimental MI intervention was manualized and that MI therapists followed a script (e.g., Murphy et al., 2009; Simpson et al., 2010; most often, the Westra & Dozois, 2003, manual—or an adaptation of that manual—was utilized). This practice improves treatment integrity and thus internal validity (Finger & Rand, 2005). It should be noted that, though manualization of treatments typically can strengthen study design, a rigid standardization of MI protocols can decrease the efficacy of the intervention. A meta-analysis indicated that effect sizes of MI are lower when the intervention is manualdirected (Hettema et al., 2005). Improvements in treatment integrity and internal validity that come with treatment manualization must be weighed against potential reductions in treatment effect in the context of research on MI. Given the most contemporary literature, it is likely that much of the increase in treatment integrity that comes with utilizing manual-guided MI is overshadowed by associated reductions in treatment effect size. The use of strictly and intensively scripted protocols can be a limitation in MI research.
Consideration of the manner in which study treatments are implemented from a procedural standpoint also is warranted, as the delivery of treatment in experimental work impacts the external validity and generalizability of study findings (Finger & Rand, 2005). With regard to MI or MI-like interventions completed in the reviewed studies, not all experimental interventions were created equally. For example, “dose” of MI received by study participants varied, with participants of some studies receiving four or five MI sessions (e.g., Murphy et al., 2009; Westra, 2004) and the participants of others receiving only two MI sessions (e.g., Meyer et al., 2010). Similarly, participants of some studies received significantly longer MI sessions than did participants of other studies. For example, Merlo and colleagues (2010) reported that MI sessions lasted between 20 and 30 minutes, while Buckner and Schmidt (2009) and Simpson and colleagues (2010) reported providing MI sessions lasting at least 90 minutes. Looking across studies, these large differences in experimental treatment delivery certainly limit overarching conclusions that can be drawn, as treatment dose-response is a critical consideration impacting construct and ecological validity (Kazdin, 2003).
Likewise, other aspects of treatment implementation, such as format of the intervention, can impact construct validity and generalizability of study findings. To be sure, the studies reviewed here differed fairly widely in experimental treatment implementation. For instance, 10 of the 17 studies utilized a pre-CBT MI intervention (e.g., Westra & Dozois, 2006) while three utilized an integrated MI intervention (e.g., Meyer et al., 2010), and four utilized a combination of pre-CBT MI and integrated MI (e.g., Simpson et al., 2010). None of the four studies that used a combination of pre-CBT MI with an optional integrated MI module explicitly reported whether and/or how often the optional MI module was utilized across all participants. Reporting this information would clarify treatment implementation, enumerate treatment dose, speak to the potential importance of such a module, and allow for replication of study findings in future research and clinical application. A few studies involved delivery of the experimental MI intervention in a group format (e.g., Meyer et al., 2010; Murphy et al., 2009), while others utilized an individual therapy strategy (e.g., Buckner & Schmidt, 2009; McKay & Bouman, 2008). Lastly, CBT interventions may have included MI methods that were not accounted for by researchers (e.g., permission asking, evoking change talk), further impacting construct validity. Only two studies noted that care was taken to account for this potential experimental contaminant (Simpson et al., 2010; Westra, 2004).
Experimental Design Considerations
To begin, though they differed across studies, exclusionary criteria were explicitly reported for all of the included RCTs, a strength of the literature. Common exclusionary criteria included psychosis, bipolar disorder, impaired cognitive ability, or inability to participate in therapy (e.g., not being able to regularly attend sessions) due to logistical issues. These exclusionary criteria can, in some ways, limit generalizability, but also limit selection bias interactions, thus bolstering external validity (Finger & Rand, 2005). Second, truly random assignment is a critical aspect of RCT designs, as it limits selection bias (Kazdin, 2003). Each of the RCTs critiqued for this review reported that, after randomization, experimental comparison groups did not differ on demographic or other key variables. One study (Westra & Dozois, 2006) reported that, by chance, experimental groups differed on one minor, secondary variable, which was controlled for in data analysis. Several of the reviewed studies (Buckner & Schmidt, 2009; Hsieh et al., 2012; Meyer et al., 2010; Murphy et al, 2009; Simpson et al., 2010; Westra et al., 2009) provided specific information about how participants were randomly assigned to experimental groups, a strength of these articles.
For the RCTs, the control group treatment is another critical experimental design consideration. Several of the RCTs included in this review (Hsieh et al., 2012; Merlo et al., 2010; Meyer et al., 2010; Simpson et al., 2010; Titov et al., 2010) utilized double-blind, nonspecific (i.e., “attention-placebo”) or standard treatment control groups in order to experimentally control for amount of therapist/treatment contact, limiting threats to internal and construct validity (Kazdin, 2003). Two other studies (Buckner & Schmidt, 2009; Murphy et al., 2009) utilized nonspecific treatment control groups; however, these groups did not receive the same amount of therapist contact as experimental treatment groups. Four studies (Aviram & Westra, 2011; Matlby & Tolin, 2005; Westra & Dozois, 2006; Westra et al., 2009) utilized only a waiting-list control, reducing construct validity.
A final experimental design issue that is intimately related to external validity and the generalizability of study findings involves therapist assignment to study cases. Clinical outcome studies that involve only one therapist may have reduced external validity, as therapist variables, not treatment variables, may account for much of the variance observed in study findings (Finger & Rand, 2005; Kazdin, 2003). Reviewed studies that utilized multiple MI and CBT therapists are considered to have appropriately addressed this experimental design concern (Buckner & Schmidt, 2009; Hsieh et al., 2012; Simpson et al., 2010; Westra et al., 2009). All studies included in this review apparently occurred at a single study site, which limits external validity and generalizability.
Measurement and Data Analytic Issues
Measurement Considerations
An important consideration in treatment studies such as those reviewed here is measurement of symptomology for diagnoses. For preliminary studies, as many of those reviewed are, an accurate diagnosis of psychopathology is critical for external validity and related generalizability (Finger & Rand, 2005). All but one (McKay & Bouman, 2008) of the reviewed studies utilized some structured method to diagnose anxiety disorders for study participants. Structured interviews often are considered the gold standard for diagnosing participants of treatment studies (Joiner & Pettit, 2005). Particularly strong studies (6 of 16) not only completed formal assessment of diagnosis, but also utilized some mechanism checking the reliability of that diagnosis, such as reviewing tapes of diagnostic interviews or employing an independent evaluator to confirm the diagnosis (Aviram & Westra, 2011; Buckner & Schmidt, 2009; Merlo et al., 2010; Simpson et al., 2010; Westra & Dozois, 2006; Westra et al., 2009).
In order to measure outcome variables, the majority of studies reviewed utilized widely used and well-validated instruments that are known to be reliable and otherwise psychometrically sound. Still, some studies utilized their own measures, which do not have data confirming their psychometric quality (Buckner & Schmidt, 2009; Maltby & Tolin, 2005; Murphy et al., 2009; Westra & Dozois, 2006). Only one of these studies (Westra & Dozois, 2006) presented psychometric data (i.e., measures of internal consistency) for their novel scale. A few studies (e.g., Simpson & Zuckoff, 2011; Simpson et al., 2008) reported completing psychosocial assessment tools using independent evaluators, and are consequently considered to be stronger with respect to accounting for interviewing bias (Finger & Rand, 2005).
In treatment research, demonstrating both statistical and clinical significance is important (Kazdin, 2003). The majority of reviewed studies (16 of 17) drew conclusions based on clinically significant results rather than simply statistically significant results. Still, one study (McKay & Bouman, 2008) did not report the meaning of clinical outcome measures, and reported only change scores or statistically significant outcomes.
Lastly, and related to clinical significance, the manner in which treatment gains are assessed is an important measurement issue. To be sure, the goal of any treatment is to yield remission that persists as long as possible. Treatment studies that measure clinical improvement only immediately after treatment termination (or only very soon after) risk drawing limited conclusions about the ultimate clinical utility of a particular treatment. In reviewing the included studies, two stood out as exceptional with regard to long-term follow-up of clinical outcome assessment, measuring study variables at 12-month posttreatment (Murphy et al., 2009; Westra et al., 2009). Seven of the included studies included follow-up assessment only 1 month posttreatment, or not at all, and conclusions regarding long-term clinical outcomes therefore are limited (Buckner, 2009; Buckner & Schmidt, 2009; Hsieh et al., 2012; Maltby & Tolin, 2005; Merlo et al., 2010; Simpson et al., 2008; Simpson et al., 2010).
Data Analytic and Statistical Considerations
Though case studies and small open trials are important preliminary steps understanding the potential benefits of novel treatment strategies, their inherently small sample sizes limit generalizability. Thus, each of the case studies and preliminary uncontrolled studies reviewed here is limited in the scale of the conclusions that can be drawn. As all but one of the RCT studies reviewed relied on a two-group design, a sample size of approximately 65 participants is recommended for essentially all of the studies presented here in order to detect a moderate effect with .80 power (G*Power 3.0; Faul, Erdfelder, Lang, & Buchner, 2007). Only four of the included studies (Meyer et al., 2010; Murphy et al., 2009; Titov et al., 2010; Westra et al., 2009) utilized samples large enough to be adequately powered. Though the reviewed studies are preliminary in nature and represent a first step in understanding how MI can be applied to CBT for anxiety disorders, most lack sufficient power to draw decisive conclusions as a result of small sample sizes and thus are susceptible to Type II error.
Three of the reviewed RCTs failed to report effect sizes altogether (Buckner & Schmidt, 2009; Maltby & Tolin, 2005), though two of those studies (Buckner & Schmidt, 2009; Simpson et al., 2010) did not present statistically significant results on topics within the scope of this review. Not reporting effect sizes limits conclusions that can be drawn from significant results, as it is difficult to ascertain the magnitude or meaning of group differences.
Type I error can be reduced a number of ways, including by defining a priori study hypotheses (Kazdin, 2003). Two studies (Merlo et al., 2010; Westra & Dozois, 2006) did not report a priori hypotheses, thus increasing the likelihood of identifying as significant group differences that truly are not. Another method of reducing Type I error is to avoid completing an abundance of between-group comparisons, especially when studies have small samples and are at risk for being underpowered (Kazdin, 2003). Given the number of participants in the majority of the reviewed studies, the likelihood of Type I error as a result of multiple comparisons without correction is high for all but a few studies. Only one of the remaining studies utilized a statistical correction for multiple comparisons (i.e., Buckner & Schmidt, 2009).
Not one of the included studies addressed how missing data were dealt with statistically, though a few did point out that there were missing data (e.g., Merlo et al., 2010; Simpson et al., 2008). Missing data can be prevalent in longer-term treatment studies (Kazdin, 2003) and appropriate handling of this concern is essential for making valid conclusions from study results (Allison, 2009; Schafer & Graham, 2002).
Conclusions
State of the Literature
There is a growing body of empirical literature addressing the utility of applying MI or MI-congruent processes to CBT for anxiety disorders to improve treatment initiation, treatment adherence, and, ultimately, treatment response. Table 1 summarizes key conclusions drawn by each of the reviewed studies. In total, the data presented in the summarized studies provide moderate support for the broad recommendation to include MI in CBT protocols. Although 5 of 11 RCTs did not demonstrate enhanced outcomes, findings must be understood in the context of the strengths and limitations of the work. In particular, power issues and floor effects must be considered when adding MI to an already effective treatment. It is noteworthy that there was no instance of the addition of MI to CBT resulting in less effective CBT, suggesting that using MI as an adjunct to CBT, at the very least, is equally as effective as CBT alone and, at best, better than CBT alone across a range of anxiety disorders.
Considering the available literature in its entirety, a few general conclusions can be drawn. First, as Simpson and colleagues (2008) noted, it appears feasible to utilize MI processes along with CBT. This conclusion is supported by each of the studies reviewed here and is an imperative for subsequent study and utilization of this potential adjunct to CBT. Second, available literature generally supports that adding MI to CBT may be a promising route for improving standard treatment outcomes, a finding that initially appears to be true across a number of anxiety disorders. Third, MI alone is not likely to produce changes in anxiety symptomatology in all clients. Fourth, treatment initiation and engagement can be improved by adding MI as an adjunct to CBT for anxiety disorders, with initial support suggesting this to be especially true for apprehensive treatment seekers.
A number of preliminary deductions also can be postulated, given the currently available science. There is early overarching support that MI may increase treatment utilization rates, enhance efficacy, and accelerate treatment progress for CBT for anxiety disorders. Though still premature, early evidence suggests these benefits may be the result of improving client/patient readiness to change, increasing treatment acceptance, reducing resistance, and/or increasing commitment to treatment, all of which may be especially useful for those who are less responsive to standard treatment. MI’s emphasis on client ambivalence and deciding about making a commitment to change likely is highly related to these outcomes (Miller & Rollnick, 2013). Of course, these interpretations are made with caution as many current findings are small in effect and there are many remaining questions to be addressed.
A host of overarching limitations elucidated in this critique should be noted. First, the body of available literature is relatively small and, therefore, has a relatively narrow focus, which limits generalizability of the findings. Similarly, the single-site studies with small sample sizes also limit generalizability. Given the current state of the literature, additional efficacy trials may be required before studies with a greater degree of generalizability are warranted and completed. Second, there is a good deal of variety in the quality of MI interventions administered and assessment/reporting of treatment fidelity across available studies, which impacts validity of conclusions drawn. Fidelity can be supported and verified in a number of ways (see Bellg et al., 2004), although the sine qua non is independent review and analysis of actual treatment sessions. Furthermore, fidelity methods must be reported so that validity can be established. Third, longterm follow-up data generally are lacking from this body of literature, making it difficult to discern durability of response vis-à-vis the benefit of combining MI and CBT for anxiety disorders. Fourth, currently available studies are more or less focused only on basic outcomes and not on the mechanisms underlying the phenomena of interest. Aviram and Westra’s (2011) path-analytic analyses addressing the role of resistance and homework compliance in the relation between treatment group and clinical outcomes, however, are particularly sophisticated and indicate a movement toward attempting to understand more causal and mechanistic phenomena.
Clinical and Scientific Implications
The case studies and small, uncontrolled studies reviewed here provide rich and insightful accounts of how MI can be utilized along with CBT for anxiety disorders. Further, the RCTs presented demonstrate promise that adding MI may be beneficial for a range of clients and across a range of anxiety diagnoses. Still, given the low-powered studies and sometimes neutral findings, it is too early to confidently suggest that therapists should routinely incorporate MI into CBT regimens for clients with anxiety disorders. That said, the current literature is trending in such a way that skilled clinicians who are well-trained in MI principles and processes, as well as expert in the delivery of CBT, may find the marrying of the two approaches useful for improving utilization of treatment, and outcomes for certain clients with anxiety disorders. Clinically, clients who seem reluctant, uncertain, or resistant about certain aspects of interventions, or treatment generally, may be the best candidates for inclusion of MI in CBT.
Future Directions
Melding MI and CBT is ripe with possibilities to improve practice and ultimately help clients with anxiety disorders. To begin, future research on the use of MI as an adjunct to CBT for anxiety disorders should consider the nature of the MI utilized with clients. Across reviewed studies, MI components varied from pretreatment adjuncts (e.g., Westra & Dozois, 2006), to integrated interventions (e.g., Merlo et al., 2010), to something in between (e.g., Simpson et al., 2010). Determining which approaches to implement, with whom, and how best to deliver MI interventions in the context of CBT for anxiety disorders should be a research priority. Along similar lines, studying the best manner to train therapists and whether/how to develop related treatment manuals also will serve the literature well. A few research groups already have manualized their pre-CBT MI interventions (e.g., Simpson et al., 2008; Westra & Dozois, 2003), and so these manuals ought to be utilized by other scientists to confirm the resulting MI fidelity, treatment utility, and relation to improved outcomes, among other factors. And still, future research that involves the training of therapists who utilize MI with CBT treatment for anxiety, and any related training or treatment manuals, should consider how best to incorporate MI spirit (Miller & Rollnick, 2013) and how to balance style and aspects of CBT and MI, which may be competing or complementary. Likewise, further work is needed to determine how best to achieve a full integration of MI and CBT when appropriate (Narr & Flynn, 2015). Additionally, determining how the manualization of MI impacts treatment effect sizes for CBT clients with anxiety disorders is important, as highly structured manual-guided treatment actually may limit treatment efficacy (Hettema et al., 2005).
Future research also should include an emphasis on understanding how MI may be used as an adjunct to pharmacotherapy or combined pharmacotherapy/CBT for anxiety disorders. Many of the reviewed studies indicated that participants were, in addition to receiving psychotherapeutic interventions, concurrently taking medication for anxiety symptoms. Thus, it will be necessary to understand the potential role(s) of MI in treatments involving pharmacotherapy, especially when pharmacotherapy occurs in conjunction with CBT (e.g., Balán, Moyers, & Lewis-Fernández, 2015).
Research in the area also will need to include larger and more diverse samples, including diversity of client age, as only one available study includes a sample of adolescents and none include older adults as a group. Greater attention should be given to amassing data across many diagnostic groups, too. Further, research related to non-treatment-seeking individuals who meet criteria for an anxiety disorder (which has been tried only minimally; e.g., Schmidt & Buckner, 2009) is critical, as these are the individuals who may benefit most from MI as an initial approach. In fact, including more nonseekers in future work may increase observed effects of intervention. Research that addresses in which settings and with which providers the MI plus CBT intervention is most effective also will be important moving forward, especially if such an approach is to be disseminated widely. Research in this area may prove fruitful by assessing acceptability, accessibility, and cost-effectiveness of treatment.
Of course, a key piece of addressing each of the aforementioned directions for future research is improving the understanding of the mechanism(s) in including both MI and CBT in treating anxiety disorders, whether it is melding, combining, or some other process. That is, a priority of future research should be identifying how the addition of MI to CBT for anxiety disorders improves treatment outcome. Some researchers (e.g., Aviram & Westra, 2011) already have attempted to elucidate how MI improves CBT outcomes; however, much more of this type of research is necessary. For example, is client-verbalized commitment to change the key issue targeted by MI? Is there something about MI, versus other pretreatment motivational strategies, which yields particularly high efficacy? Which aspects of MI are “doing the work?” Is MI serving as an opportunity for lower-level exposure that begins the process of extinction learning and promotes comfort with the CBT treatment? Research that answers these questions (related to the mechanisms of action of this exciting new treatment opportunity) is necessary if we are to understand the treatment fully and subsequently utilize it in the most beneficial ways. Just as MI and the transtheoretical model of change (i.e., stages of change) have been likened to “kissing cousins who never married” due to their compatibility and complementarity (p. 35, Miller & Rollnick, 2013), MI and CBT are like half-siblings who share one parent. Their partially shared theoretical backgrounds make the two approaches well suited to be paired.
Summary
The addition, integration, or synergistic combination of MI and CBT is quite promising. MI very well may be a critical adjunct to CBT for certain individuals being treated for anxiety disorders, although it likely is not alone sufficient. Contemporary literature suggests that MI usefully can be applied as an adjunct to CBT for anxiety disorders in many instances and cases, and is very unlikely to be harmful. Furthermore, the available evidence is promising, as treatment initiation, engagement, and outcomes all initially seem to have the potential to be positively impacted by applying MI along with CBT. Given a number of limitations of the existing research, however, it is clear that additional work is necessary. Future research will expand upon encouraging preliminary findings, potentially changing some of the ways that CBT for anxiety disorders is delivered and ultimately improving outcomes for the clients who receive such treatment.
HIGHLIGHTS.
Motivational Interviewing (MI) appears efficacious as an adjunct to CBT for anxiety
Treatment initiation and engagement may be increased by adding MI to CBT
Preliminary literature suggests adding MI to CBT may improve treatment outcomes
Additional research is needed to identify how best to utilize MI with CBT
Acknowledgments
This article is based on the doctoral qualifying examination paper by the first author, supervised by the second author. The authors thank an anonymous reviewer and the Editor for helpful comments on an earlier draft of this manuscript. Preparation of this manuscript for publication was partially supported by a National Research Service Award from the National Institute for Dental and Craniofacial Research (National Institutes of Health), F31-DE023493.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abramowitz JS, Franklin ME, Zoellner LA, DiBernardo CL. Treatment compliance and outcome in obsessive-compulsive disorder. Behavior Modification. 2002;26:447–463. doi: 10.1177/0145445502026004001. [DOI] [PubMed] [Google Scholar]
- Allison PD. Missing data. In: Millsap RE, Maydeu-Olivares A, editors. The Sage handbook of quantitative methods in psychology. Thousand Oaks, CA: Sage Publications; 2009. pp. 72–89. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Arlington, VA: Author; 2013. [Google Scholar]
- Arkowitz H, Westra HA, Miller WR, Rollnick S, editors. Motivational Interviewing in the treatment of psychological problems. 2. New York: The Guilford Press; 2015. [Google Scholar]
- Aviram A, Westra HA. The impact of Motivational Interviewing on resistance in cognitive behavioural therapy for generalized anxiety disorder. Psychotherapy Research. 2011;21:698–708. doi: 10.1080/10503307.2011.610832. [DOI] [PubMed] [Google Scholar]
- Bados A, Balaguer G, Saldaña C. The efficacy of cognitive-behavioral therapy and the problem of drop-out. Journal of Clinical Psychology. 2007;63:585–592. doi: 10.1002/jclp.20368. [DOI] [PubMed] [Google Scholar]
- Balán IC, Moyers TB, Lewis-Fernández R. Motivational pharmacology: Combining Motivational Interviewing and antidepressant therapy to improve treatment outcomes. In: Arkowitz H, Miller WR, Rollnick S, editors. Motivational Interviewing in the treatment of psychological problems. 2. New York: The Guilford Press; 2015. pp. 219–248. [Google Scholar]
- Bellg AJ, Borrelli B, Resnick B, Hecht J, Minicucci DS, Ory M, Czaijkowski S, et al. Enhancing treatment fidelity in health behavior change studies: Best practices and recommendations from the NIH Behavior Change Consortium. Health Psychology. 2004;23:443–451. doi: 10.1037/0278-6133.23.5.443. [DOI] [PubMed] [Google Scholar]
- Buckner JD. Motivation enhancement therapy can increase utilization of cognitive-behavioral therapy: The case of social anxiety disorder. Journal of Clinical Psychology: In Session. 2009;65:1195–1206. doi: 10.1002/jclp.20641. [DOI] [PubMed] [Google Scholar]
- Buckner JD, Schmidt NB. A randomized pilot study of motivation enhancement therapy to increase utilization of cognitive-behavioral therapy for social anxiety. Behaviour Research and Therapy. 2009;47:710–715. doi: 10.1016/j.brat.2009.04.009. [DOI] [PubMed] [Google Scholar]
- Burke BL, Arkowitz H, Menchola M. The efficacy of Motivational Interviewing: A meta-analysis of controlled clinical trials. Journal of Consulting and Clinical Psychology. 2003;71:843–861. doi: 10.1037/0022-006X.71.5.843. [DOI] [PubMed] [Google Scholar]
- Burke BL, Dunn CW, Atkins DC, Phelps JS. The emerging evidence base for Motivational Interviewing: A meta-analytic and qualitative inquiry. Journal of Cognitive Psychotherapy. 2004;18:309–322. [Google Scholar]
- Butler AC, Chapman JE, Forman EM, Beck AT. The empirical status of cognitive-behavioral therapy: A review of meta-analyses. Clinical Psychology Review. 2006;26:17–31. doi: 10.1016/j.cpr.2005.07.003. [DOI] [PubMed] [Google Scholar]
- Cordioli AV, Heldt E, Bochi DB, Margis R, Sousa MB, Tonello JF, Manfro GG, Kapczinski F. Cognitive-behavioral group therapy in obsessive-compulsive disorder: A randomized clinical trial. Psychosomatic Psychotherapy. 2003;72:211–216. doi: 10.1159/000070785. [DOI] [PubMed] [Google Scholar]
- Demyttenaere K, Bruffaerts R, Posada-Villa J, Gasquet I, Kovess V, Lepine JP, Chatterji S, et al. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. Journal of the American Medical Association. 2004;291:2581–2590. doi: 10.1001/jama.291.21.2581. [DOI] [PubMed] [Google Scholar]
- Dugas MJ, Ladouceur R, Leger E, Freeston M, Langlois F, Provencher MD, Boisvert JM, et al. Journal of Consulting and Clinical Psychology. 2003;71:821–825. doi: 10.1037/0022-006x.71.4.821. [DOI] [PubMed] [Google Scholar]
- Faul F, Erdfelder E, Lang A-G, Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods. 2007;39:175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- Finger MS, Rand KL. Addressing validity concerns in clinical psychology research. In: Roberts MC, Illardi SS, editors. Handbook of research methods in clinical psychology. Malden, MA: Blackwell Publishing; 2005. pp. 13–30. [Google Scholar]
- Goetzel RZ, Hawkins K, Ozminkowski RJ. The health and productivity cost burden of the “top 10” physical and mental conditions affecting six large US employers in 1999. Journal of Occupational Environmental Medicine. 1999;45:5–14. doi: 10.1097/00043764-200301000-00007. [DOI] [PubMed] [Google Scholar]
- Grant BF, Hasin DS, Blanco C, Stinson FS, Chou SP, Goldstein RB, Huang B, et al. The epidemiology of social anxiety disorder in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2005;66:1351–1361. doi: 10.4088/jcp.v66n1102. [DOI] [PubMed] [Google Scholar]
- Haby MM, Donnelly M, Corry J, Vos T. Cognitive behavioural therapy for depression, panic disorder and generalized anxiety disorder: A meta-regression of factors that may predict outcome. Australian and New Zealand Journal of Psychiatry. 2005;40:9–19. doi: 10.1080/j.1440-1614.2006.01736.x. [DOI] [PubMed] [Google Scholar]
- Hettema J, Steele J, Miller WR. Motivational interviewing. Annual Review of Clinical Psychology. 2005;1:91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833. [DOI] [PubMed] [Google Scholar]
- Hsieh MY, Ponsford J, Wong D, Schonberger M, Taffe J, McKay A. Motivational Interviewing and cognitive behavior therapy for anxiety following traumatic brain injury: A pilot randomised controlled trial. Neuropsychological Rehabilitation. 2012;22:585–608. doi: 10.1080/09602011.2012.678860. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Asnaani A, Vonk IJJ, Sawyer AT, Fang A. The efficacy of cognitive behavioral therapy: A review of meata-analyses. Cognitive Therapy and Research. 2012;36:427–440. doi: 10.1007/s10608-012-9476-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Smits JAJ. Cognitive-behavioral therapy for adult anxiety disorders: A meta-analysis of randomized placebo-controlled trials. Journal of Clinical Psychiatry. 2008;69:621–632. doi: 10.4088/jcp.v69n0415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson NS, Dobson KS, Truax PA, Addis ME, Koerner K, Gollan J, Prince SE, et al. A component analysis of cognitive-behavioral treatment for depression. Journal of Consulting and Clinical Psychology. 1996;66:295–304. doi: 10.1037//0022-006x.64.2.295. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Pettit JW. Adult clinical assessment and diagnosis research: Current status and future directions. In: Roberts MC, Illardi SS, editors. Handbook of research methods in clinical psychology. Malden, MA: Blackwell Publishing; 2005. pp. 284–304. [Google Scholar]
- Kazdin AE. Research design in clinical psychology. 4. Boston, MA: Allyn & Bacon; 2003. [Google Scholar]
- Kessler RC, Berglund P, Chiu WT, Demler O, Heeringa S, Hiripi E, Jin R, Pennell BE, Walters EE, Zaslavsky A, Zheng H. The US National Comorbidity Survey Replication (NCS-R): design and field procedures. International Journal of Methods in Psychiatric Research. 2004;13:69–92. doi: 10.1002/mpr.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Petukhova M, Sampson NA, Zaslavsky AM, Wittchen H-U. Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. International Journal of Methods in Psychiatric Research. 2012;21(3):169–184. doi: 10.1002/mpr.1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundahl BW, Kunz C, Brownell C, Tollefson D, Burke BL. A meta-analysis of Motivational Interviewing: Twenty-five years of empirical studies. Research on Social Work Practice. 2010;20:137–160. [Google Scholar]
- Lukefeld C, Brown C, Clark J, Godlaski T, Hays R. Behavioral therapy for ritual substance abusers. Lexington, KY: University of Kentucky Press; 2000. [Google Scholar]
- Maltby N, Tolin DF. Overview of treatments for OCD and spectrum conditions: Conceptualization, theory, and practice. Brief Treatment and Crisis Intervention. 2003;3:127–144. [Google Scholar]
- Maltby N, Tolin DF. A brief motivational intervention for treatment-refusing OCD patients. Cognitive Behaviour Therapy. 2005;34:176–184. doi: 10.1080/16506070510043741. [DOI] [PubMed] [Google Scholar]
- McKay D, Bouman TK. Enhancing cognitive-behavioral therapy for monosymptomatic hypochondriasis with Motivational Interviewing: Three case illustrations. Journal of Cognitive Psychotherapy. 2008;22:154–166. [Google Scholar]
- McNeil DW, Hayes SE, Randall CL. Oxford Handbooks Online. Oxford: Oxford University Press; 2016. Motivational Interviewing and motivational interaction for health behavior change and maintenance. [Google Scholar]
- McNeil DW, Quentin LL. Motivation in clinical interventions. In: Wright JD, editor. International Encyclopedia of Social and Behavioral Sciences. 2. Burlington, MA: Elsevier; 2015. [Google Scholar]
- Merlo LJ, Storch EA, Lehmkuhl HD, Jacob ML, Murphy TK, Goodman WK, Geffken GR. Cognitive behavioral therapy plus Motivational Interviewing improves outcome for pediatric obsessive-compulsive disorder: A preliminary study. Cognitive Behaviour Therapy. 2010;39:24–27. doi: 10.1080/16506070902831773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer E, Souza F, Heldt E, Knapp P, Cordioli A, Shavitt RG, Leukefeld C. A randomized clinical trial to examine enhancing cognitive-behavioral group therapy for obsessive-compulsive disorder with Motivational Interviewing and thought mapping. Behavioural and Cognitive Psychotherapy. 2010;38:319–336. doi: 10.1017/S1352465810000111. [DOI] [PubMed] [Google Scholar]
- Miller WR. Motivational interviewing with problem drinkers. Behavioral Psychotherapy. 1983;11:147–172. [Google Scholar]
- Miller W, Rollnick S. Motivational Interviewing: Helping people change. 3. New York: The Guilford Press; 2013. [Google Scholar]
- Miller WR, Rose GS. Toward a theory of Motivational Interviewing. American Psychologist. 2009;6:527–537. doi: 10.1037/a0016830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morales E, Norcross JC. Evidence-based practices with ethnic minorities: Strange bedfellows no more. Journal of Clinical Psychology: In Session. 2010;66:821–829. doi: 10.1002/jclp.20712. [DOI] [PubMed] [Google Scholar]
- Moyers TB, Martin T, Manuel JK, Hendrickson SML, Miller WR. Assessing competence in the use of Motivational Interviewing. Journal of Substance Abuse Treatment. 2005;28:19–26. doi: 10.1016/j.jsat.2004.11.001. [DOI] [PubMed] [Google Scholar]
- Moyers T, Martin T, Manuel JK, Miller WR, Ernst D. Revised global scales: Motivational Interviewing Treatment Integrity 3.0. 2007 Unpublished instrument. Retrieved from http://casaa.unm.edu/download/miti3.pdf.
- Murphy RT, Thompson KE, Murray M, Rainey Q, Uddo MM. Effect of a motivation enhancement intervention on verterans’ engagement in PTSD treatment. Psychological Services. 2009;6:264–278. [Google Scholar]
- Narr S, Flynn H. Motivational Interviewing and the treatment of depression. In: Arkowitz H, Miller WR, Rollnick S, editors. Motivational Interviewing in the treatment of psychological problems. 2. New York: The Guilford Press; 2015. pp. 170–192. [Google Scholar]
- Olatunji BO, Cisler JM, Deacon BJ. Efficacy of cognitive behavioral therapy for anxiety disorders: A review of meta-analytic findings. The Psychiatry Clinics of North America. 2010;33:557–577. doi: 10.1016/j.psc.2010.04.002. [DOI] [PubMed] [Google Scholar]
- Purdon C, Rowa K, Antony MM. Treatment fears in individuals awaiting treatment of OCD; Paper presented at the meeting of the Association for the Advancement of Behavior Therapy; New Orleans, LA. 2004. Nov, [Google Scholar]
- Riccardi CJ, Timpano KR, Schmidt NB. A case study perspective on the importance of motivation in the treatment of obsessive compulsive disorder. Clinical Case Studies. 2010;9:273–284. [Google Scholar]
- Rollnick S, Miller W. What is Motivational Interviewing? Behavioral and Cognitive Psychotherapy. 1995;23:325–334. doi: 10.1017/S1352465809005128. [DOI] [PubMed] [Google Scholar]
- Rollnick S, Miller WR, Butler CC. Motivational Interviewing in health care. New York: The Guilford Press; 2008. [Google Scholar]
- Rubak S, Sandbæk A, Lauritzen T, Christensen B. Motivational Interviewing: A systematic review and meta-analysis. British Journal of General Practice. 2005;55:305–312. [PMC free article] [PubMed] [Google Scholar]
- Sanderson K, Andrews G. Prevalence and severity of mental health disability and relationship to diagnosis. Psychiatric Services. 2002;53:80–86. doi: 10.1176/appi.ps.53.1.80. [DOI] [PubMed] [Google Scholar]
- Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychological Methods. 2002;7:147–77. [PubMed] [Google Scholar]
- Simpson HB, Zuckoff A. Using Motivational Interviewing to enhance treatment outcome in people with obsessive-compulsive disorder. Cognitive and Behavioral Practice. 2011;18:28–37. doi: 10.1016/j.cbpra.2009.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson HB, Zuckoff AM, Maher MJ, Page JR, Franklin ME, Foa EB, Schmidt AB, Wang Y. Challenges using Motivational Interviewing as an adjunct to exposure therapy for obsessive-compulsive disorder. Behaviour Research and Therapy. 2010;48:941–948. doi: 10.1016/j.brat.2010.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson HB, Zuckoff A, Page JR, Franklin ME, Foa EB. Adding Motivational Interviewing to exposure and ritual prevention for obsessive-compulsive disorder: An open pilot trial. Cognitive Behaviour Therapy. 2008;37:38–49. doi: 10.1080/16506070701743252. [DOI] [PubMed] [Google Scholar]
- Slagle DM, Gray MJ. The utility of Motivational Interviewing as an adjunct to exposure therapy in the treatment of anxiety disorders. Professional Psychology: Research and Practice. 2007;38:329–337. [Google Scholar]
- Steele RG, Roberts MC. Therapy and interventions research with children and adolescents. In: Roberts MC, Illardi SS, editors. Handbook of research methods in clinical psychology. Malden, MA: Blackwell Publishing; 2005. pp. 307–326. [Google Scholar]
- Titov N, Andrews G, Schwencke G, Robinson E, Peters L, Spence J. Randomized controlled trial of Internet cognitive behavioural treatment for social phobia with and without motional enhancement strategies. Australian and New Zealand Journal of Psychiatry. 2010;44:938–945. doi: 10.3109/00048674.2010.493859. [DOI] [PubMed] [Google Scholar]
- Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the United States. Archives of General Psychiatry. 2005;62:629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- Westra HA. Managing resistance in cognitive behavioural therapy: The application of Motivational Interviewing in mixed anxiety and depression. Cognitive Behaviour Therapy. 2004;33:161–175. doi: 10.1080/16506070410026426. [DOI] [PubMed] [Google Scholar]
- Westra HA. Motivational Interviewing in the treatment of anxiety. New York: The Guilford Press; 2012. [Google Scholar]
- Westra HA, Arkowitz H. Integrating motivational interviewing with cognitive behavioral therapy for a range of mental health problems. [Special issue] Cognitive and Behavioral Practice. 2011;18(1) doi: 10.1016/j.cbpra.2009.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westra HA, Arkowitz H, Dozois DJA. Adding a Motivational Interviewing pretreatment to cognitive behavioral therapy for generalized anxiety disorder: A preliminary randomized controlled trial. Journal of Anxiety Disorders. 2009;23:1106–1117. doi: 10.1016/j.janxdis.2009.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westra HA, Aviram A, Doell FK. Extending Motivational Interviewing to the treatment of major mental health problems: Current directions and evidence. The Canadian Journal of Psychiatry. 2011;56:643–650. doi: 10.1177/070674371105601102. [DOI] [PubMed] [Google Scholar]
- Westra HA, Dozois DJA. Motivational Interviewing adapted for anxiety/depression. 2003 Unpublished treatment manual. [Google Scholar]
- Westra HA, Dozois DJA. Preparing clients for cognitive behavioral therapy: A randomized pilot study of Motivational Interviewing for anxiety. Cognitive Therapy and Research. 2006;30:481–498. [Google Scholar]
- Westra HA, Dozois DJA. Integrating Motivational Interviewing into the treatment of anxiety. In: Arkowitz H, Westra HA, Miller WR, Rollnick S, editors. Motivational Interviewing in the treatment of psychological problems. New York: The Guilford Press; 2008. pp. 26–56. [Google Scholar]


