Abstract
Introduction:
The use of medicinal plants was a very spread therapeutic way. At present, several studies are moving toward this ancestral option, seen the emergence of several bacterial resistance and for the large number of side effects of some synthetic drugs.
Objective:
The objective of this study was to collect and evaluate information on medicinal plants commonly used in five Moroccan cities: Rabat, Salé, Témara, Khémisset, and Tiflet for the management of halitosis.
Methods:
This is a cross-sectional survey; conducted among 171 herbalists. The tool of the study was a questionnaire filled by herbalists. SPSS in its version 13 was used for statistical calculations. Quantitative variables were expressed as a mean and standard deviation. Categorical variables were expressed as numbers and percentage.
Results:
Analysis of the results of this study identified 23 plants that are used the most. The herbal knowledge herbalists prescribed on the toxicity of plants and their side effects were appreciated.
Conclusions:
Preliminary results presented in this work allow knowing the plants used by this population. This data could be the basis for experimental and clinical studies to promote the use of natural agents in the treatment of bad breath.
Keywords: Halitosis, medicinal plants, phytotherapy, traditional healers
BACKGROUND
Halitosis, also commonly known as “bad breath” is a condition characterized by unpleasant odors emanating timely from the oral cavity [1-3], and which affect more than 30% of the general population [4]. The etiology of halitosis involves many intra- and extra-oral factors such as gingivitis, periodontitis, nasal inflammation, chronic sinusitis, diabetes mellitus, liver insufficiency, cirrhosis, uremia, lung carcinoma, trimethylaminuria, and postnasal drip [5]. However, the most common source of halitosis is the oral cavity itself (90%) [6]. Indeed, bad breath derived from the mouth is mainly caused by volatile sulfur compounds including hydrogen sulfide, methyl mercaptan, and dimethyl sulfide, produced through the putrefaction activity of oral bacteria [7-9].
Managing the halitosis is based on one hand on good oral hygiene cleaning, that reduces by 25% the CSV rates present in the oral air [10,11], and on the other hand on the treatment of oral diseases when necessary. In some case, patients can also turn to “soft” medicine that offers a wide range of disciplines to treat bad breath; homeopathy, herbal medicine and aromatherapy as alternative treatments, or complementary to conventional medicine.
This traditional mode of treatment had always been used largely by Moroccans as Arabs and Africans. By its geographical and climate diversity, Morocco has a wide range of species of aromatic plants. There are about 800 species of medicinal and aromatic plants that are potentially exploitable. Taking into account this natural wealth, and especially for cultural and economic reasons, the use of medicinal plants is still widespread in the Moroccan society. According to the WHO 2003 statistics (World Health Organization [WHO]), in some developing countries in Asia, Africa, and Latin America, 80% of the population use traditional medicine to meet their needs for primary health care. WHO has established a list of herbal monograph classifying them into three categories: Plants whose use is supported by clinical data, those whose use is supported by pharmacopeia and traditional systems of medicine and those whose use is reported in the popular milieu, but not based by clinical and experimental studies [12].
The main objective of this study was to know the medicinal plants used by herbalists for treatment of halitosis.
METHODS
This is a cross-sectional study, conducted from November 2015 to May 2016, including all forms of traditional healers (TH) from five Moroccan cities: Rabat, Salé, Témara, Khémisset, and Tiflet.
The instrument used for this study was a questionnaire in which questions were either binary choice (yes/no) or multiple choices. The questionnaires were self-administered to TH to elicit information from them. Those TH who were unable to read or write were interviewed and their responses captured. Information elicited was demography of the TH, the local names of the medicinal plants/products used for the management of orofacial problems.
The questionnaire covers three parts: The first part treated the sociodemographic characteristics; the second part interested to the phytotherapeutic practices of patients; the third part concerned the names of prescribed medicinal plants used for the management of halitosis their routes of administration and methods of usage. The TH were also surveyed about their knowledge and practice regarding toxicities and contraindications of prescribed plants.
Herbalists were selected by convenience sampling. We asked all herbalists located in the five cities in their grocery stores, the first point of contact city officials was the herbalist’s representatives who communicate the contact details of all traditional practitioners.
The inclusion criteria were herbalists who prescribe herbs for dental and oral problems. The exclusion criteria were herbalists who are limited only to the sale of medicinal plants and herbalists who do not prescribe medicinal plants for oral pathologies.
Statistical Analysis
Data obtained were analyzed using the Statistical Package for Social Sciences (SPSS version 13.0, SPSS Inc., Chicago, IL, USA) and summarized using descriptive statistics and presented as frequencies and percentages.
RESULTS
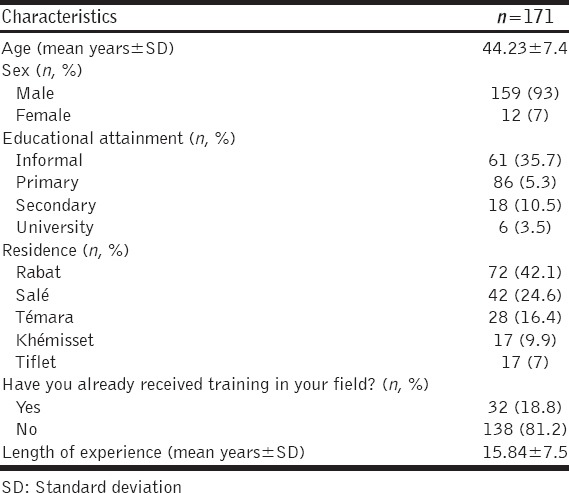
A total of 171 questionnaires conducted among herbalists, were recovered and exploited. The mean age was 44.23 ± 7.4 years. The majority 72 (42.1%) resided in Rabat. 159 (93%) were males. More than a half 86 (50.3%) had a primary school education, 61 (35.7%) informal, 18 (10.5%) secondary education, and 6 (3.5%) only university education. No statistical difference between age and educational level was found. The overage of years of experience in traditional therapeutics for TH was 15.84 ± 7.5 years. 138 (81.2%) reported that they had never received any training in their field [Table 1].
Table 1.
Sociodemographic characteristics and experience of the participants
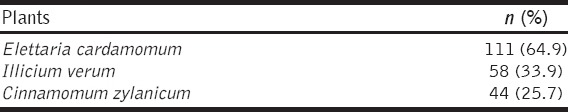
This study showed that 23 plants were used to treat bad breath [Table 2]. These plants were used alone or as a combination of two or more varieties in the same recipe [Table 3]. All TH have confirmed that patients use medicinal plants for the treatment of bad breath, and they have also quotes the most used plants by Moroccan patients [Table 4].
Table 2.
Medicinal plants used for the treatment of halitosis by traditional healers
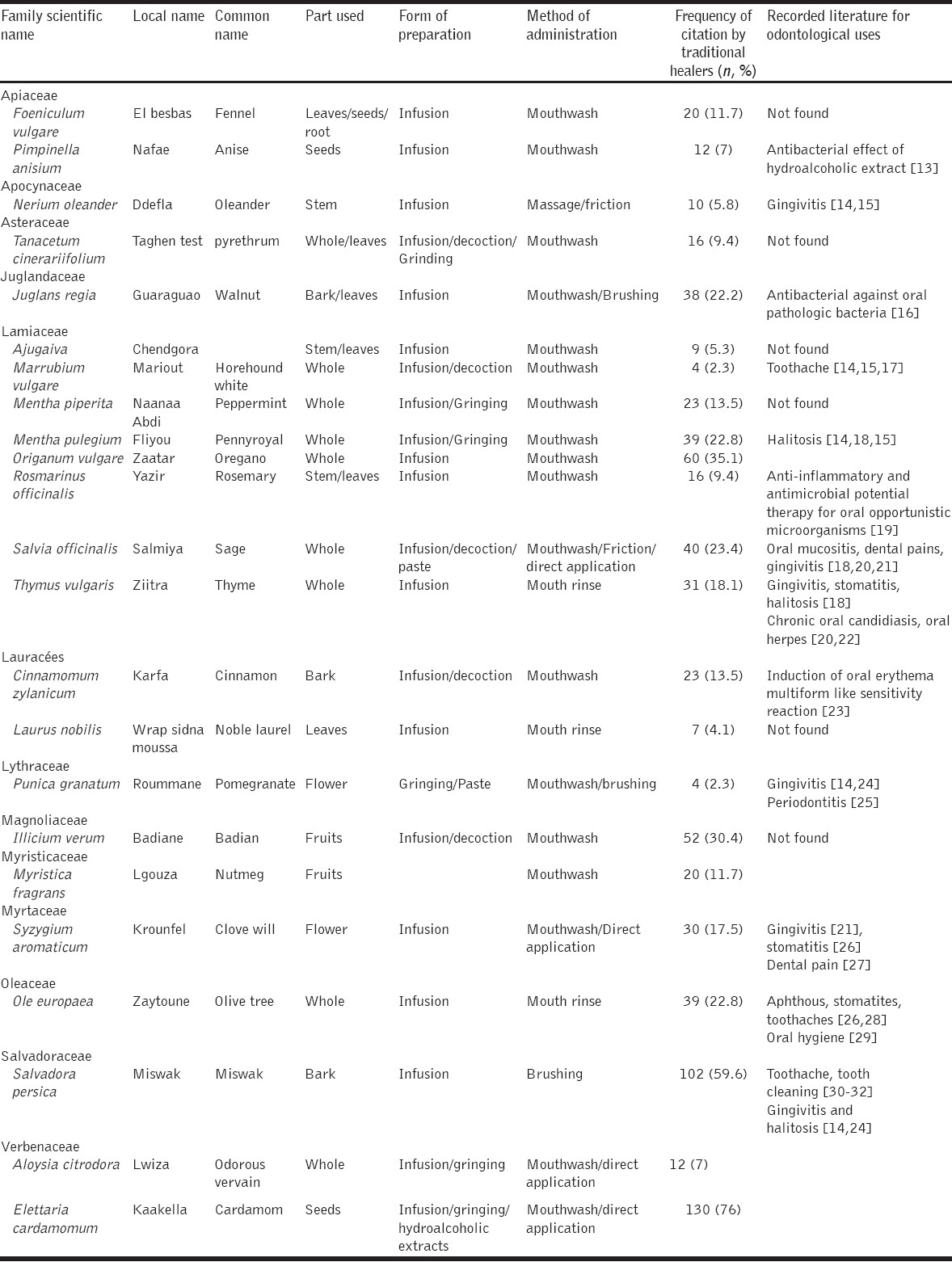
Table 3.
The most important associations of medicinal plants used in the treatment of halitosis by traditional healers
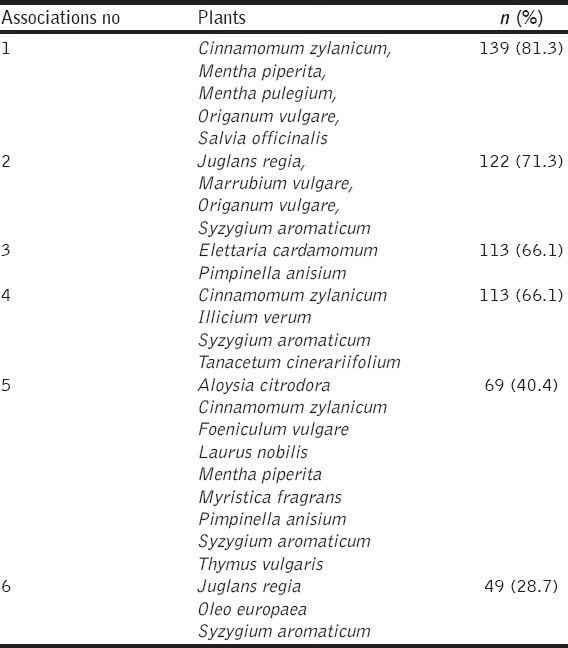
Table 4.
The most researched plants by Moroccan patients according to traditional healers
DISCUSSION
In this study, more than two-thirds of TH was older than 40 years. The most senior of them were illiterate, and <32% had formal training. It can be noticed that there was no significant difference between age and education level (P = 0.88). Furthermore, the training was not standardized, as most were trained by fathers, uncles, and other senior TH. The average duration of experience was 16 years depending on the ability of the apprentice. It can be suggested that because of their longer training, herbalists have good knowledge and skills to treat the patient by medicinal plants. There is a long and venerable history of the use of medicinal plants to treat wide varieties of oral diseases. Indeed, plants contain phytochemicals such as alkaloids, tannin, essential oils, and flavonoids that could have a high antimicrobial and anti-inflammatory efficacy.
The results of this survey revealed the use of 23 major plants belonging to 14 families in managing halitosis [Table 2].
Ethnobotany analysis of plant prescribed by herbalists and used by the patients in this study showed that they mainly belong to the family of Lamiaceae including eight species [Table 2]. This plant family is known for its wide global distribution, with over 7200 species across 240 genera [33]. In the studied region, “Kénitra-Rabat-Temara” it had been shown a predominance of species of the family Lamiaceae [34] which can explain its large use, as a local product, by the TH. However, when considered as a plant the most prescribed ones were; Elettaria cardamomum, Salvadora persica, Illicium verum, and Origanum vulgare.
E. cardamomum was widely used by TH (76%), and it was also the most researched plant by patients (64.9%) to treat halitosis. Although we did not found a literature data on its use in managing halitosis or oral diseases, we think that this plant could be useful as it has been proven to be active against many pathogenic Gram-positive and Gram-negative bacteria [35-37]. Its association with Pimpinella anisium was also prescribed by more than half of TH (66.1%). It was shown that hydroalcoholic extracts from P. anisium have an antibacterial effect on cariogenic bacteria [38].
S. persica (Miswak) was widely used (59.6%) to treat halitosis. This plant is known for its anti-inflammatory effect [39], it also contains vitamin C that helps in healing gingival edema and bleeding [14]. In a study comparing the Miswak (S. persica) with the effect of the conventional toothbrush on the periodontal health of users, Darout et al. 2003 [40] showed better results for this plant in the reduction of dental plaque and the resolution of gingivitis. Many studies showed the significant effect of Miswak as an antibacterial agent. The inhibitory role of this plant on both Gram-positive and Gram-negative bacteria and fungi residing in the oral cavity has been demonstrated both clinically and experimentally. It contains salvadorine and trimethylamine, that exhibit antibacterial effects on cariogenic bacteria such as Streptococcus mutans and that reduces the accumulation of biofilm supporting, therefore, periodontal health (Al-Bayaty et al., 2010) [41].
I. verum (Badian) was prescribed by 52% by TH and used by 58% of patients to treat halitosis. It had been shown that this plant possesses a potent antimicrobial property due to the presence of anethole. Studies with isolated anethole from I. verum indicated that it is effective against bacteria, yeast, and fungal strains (Ferng et al., 2010) [42]. It had been reported also, that this plant seems to have a good activity against Eikenella corrodens, but less active against Porphyromonas gingivalis, Porphyromonas asaccharolityca, Prevotella melaninogenica, Prevotella intermedia, Fusobacterium nucleatum, Capnocytophaga gingivalis, Veillonella parvula, E. corrodens, Peptostreptococcus micros, and Actinomyces odontolitycus (Iauk et al., 2003) [43].
O. vulgare was prescribed by 35.1% of TH. This plant is widely studied for its antibacterial effect in many systemic diseases, and more recently Khan et al. (2017) [44] reported its effect on cariogenic bacteria because of the presence of carvaccrol and thymol.
TH also prescribed Thymus vulgaris (Thyme) 31% and Syzygium aromaticum (Clove) 17.5%. These prescriptions are consistent with the literature data. Indeed, in a survey of students from the Faculty of Pharmacy, Lamendin et al. 2009 [45] showed that S. aromaticum (Clove) and T. vulgaris (Thyme) were most used for diseases of the oral mucosa. S. aromaticum (Clove) being an anti-infective, antiseptic, analgesic, [39] and anti-inflammatory [46], has its indication in all oral disease including gingivitis [9,14,15,47]. Furthermore, T. vulgaris (Thyme), through its various antiseptic and antioxidant properties [48,49], is widely reported in gingivitis, stomatitis, and bad breath [6].
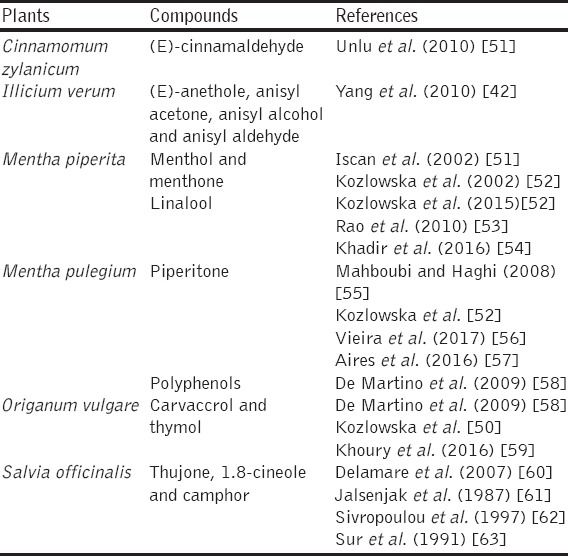
As halitosis is in most cases caused by bacteria colonizing mouth, thus using the above plants as antiseptics in treatment of oral diseases can help on resolving oral malodor. Indeed, the majority of the most used plants in this study exhibit some chemical compounds that can explain their effects [Table 5].
Table 5.
Isolated compound of the most used plants by traditional healers that have been identified as antibacterial agent
We asked TH also if they have knowledge about toxicity and counter-indications, less than 6% were aware of the related toxicity to the improper use of plants and a less than 10% were aware of against indications. Nevertheless, they insist especially on the dosage for children and elderly person; and exclude pregnant women.
Some plants like oleander had significant levels of toxicity at high doses [15]. Other herbs such as sage, thyme, pennyroyal, clove, pomegranate can also be toxic, and/or cause side effects of varying intensities (allergic reactions, gastric disorders…) following prolonged or inappropriate use. Thyme (T. vulgaris), used as a mouthwash, can cause allergic reactions as reported by Newal et al. 1996 [64]. Clove (S. aromaticum) can also cause allergy through eugenol [65], it may generates ulcers, tissue necrosis and delayed healing, or the evolution, and spread of untreated periodontal infection. Indeed, few are bibliographic data regarding the adverse effects of natural agents used in dentistry [66,67].
Herbal medicine can be dangerous, toxic and even lethal [36,68,69]. The toxicity may result from deterioration or accidental contamination of vegetation produced by other toxic substances (lead, mercury, cadmium, pesticides, and microorganisms…) or accidental substitution of parts of plants, when preparing the medicinal recipes. This toxicity can result from fraudulent practices of replacing the right plants with others of lesser value [69,70]. All this can give rise to toxic reactions as well. It is important to note that long-term users, as well as consumers of large amounts of medicinal plants and all patients using a wide variety of these plants, should be aware regarding the side effect and adverse effect of this product [71].
CONCLUSION
Considering the growing interest of natural plant molecules as efficacious and safe substances for oral health care when properly used, the preliminary results of this work allow knowing the plants used in this population. This data could be the base for experimental and clinical studies promoting the use of natural agents in the treatment of bad breath.
ACKNOWLEDGMENTS
We acknowledge all the TH who kindly participated to this study.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Gokdogan O, Catli T, Ileri F. Halitosis in otorhinolaryngology practice. Iran J Otorhinolaryngol. 2015;27:145–53. [PMC free article] [PubMed] [Google Scholar]
- 2.Bollen CM, Beikler T. Halitosis: The multidisciplinary approach. Int J Oral Sci. 2012;4:55–63. doi: 10.1038/ijos.2012.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Basavaraj P, Nitin K. Halitosis: A review. Indian J Stomatol. 2011;2:183–6. [Google Scholar]
- 4.Hughes FJ, McNab R. Oral malodour--a review. Arch Oral Biol. 2008;53(Suppl 1):S1–7. doi: 10.1016/S0003-9969(08)70002-5. [DOI] [PubMed] [Google Scholar]
- 5.Nogueira-Filho GR, Duarte PM, Toledo S, Tabchoury CP, Cury JA. Effect of triclosan dentifrices on mouth volatile sulphur compounds and dental plaque trypsin-like activity during experimental gingivitis development. J Clin Periodontol. 2002;29:1059–64. doi: 10.1034/j.1600-051x.2002.291202.x. [DOI] [PubMed] [Google Scholar]
- 6.Tonzetich J. Oral malodour: An indicator of health status and oral cleanliness. Int Dent J. 1978;28:309–19. [PubMed] [Google Scholar]
- 7.Armstrong BL, Sensat ML, Stoltenberg JL. Halitosis: A review of current literature. J Dent Hyg. 2010;84:65–74. [PubMed] [Google Scholar]
- 8.Sopapornamorn P, Ueno M, Shinada K, Yanagishita M, Kawaguchi Y. Relationship between total salivary protein content and volatile sulfur compounds levels in malodor patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:655–60. doi: 10.1016/j.tripleo.2006.08.023. [DOI] [PubMed] [Google Scholar]
- 9.Sanz M, Roldán S, Herrera D. Fundamentals of breath malodour. J Contemp Dent Pract. 2001;2:1–17. [PubMed] [Google Scholar]
- 10.Aylikci BU, Colak H. Halitosis: From diagnosis to management. J Nat Sci Biol Med. 2013;4:14–23. doi: 10.4103/0976-9668.107255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van den Broek AM, Feenstra L, de Baat C. A review of the current literature on management of halitosis. Oral Dis. 2008;14:30–9. doi: 10.1111/j.1601-0825.2006.01350.x. [DOI] [PubMed] [Google Scholar]
- 12.Zeggwagh AA, Lahlou Y, Bousliman Y. Survey of toxicological aspects of herbal medicine used by a herbalist in Fes, Morocco. Pan Afr Med J. 2013;14:125. doi: 10.11604/pamj.2013.14.125.1746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kermanshah H, Kamangar SS, Arami S, Kamalinegad M, Karimi M, Mirsalehian A, et al. The effect of hydro alcoholic extract of seven plants on cariogenic bacteria - an in vitro evaluation. Oral Health Dent Manag. 2014;13:395–401. [PubMed] [Google Scholar]
- 14.Hmammouchi M. Utilisations, Biologie, Ecologie, Chimie, Pharmacologie, Toxicologie et Lexiques Ed. Imprimerie Fédala. Morocco: Rabat-Instituts; 1999. Les Plantes Médicinales et Aromatiques Marocaines; p. 450. [Google Scholar]
- 15.Valnet J. Phytothérapie Traitement Des Maladies Par Les Plantes. Paris: LGF/Livre de Poche; 2001. p. 459. [Google Scholar]
- 16.Zakavi F, Golpasand Hagh L, Daraeighadikolaei A, Farajzadeh Sheikh A, Daraeighadikolaei A, Leilavi Shooshtari Z. Antibacterial effect of Juglans regia bark against oral pathologic bacteria. Int J Dent. 2013;2013:854765. doi: 10.1155/2013/854765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Little JW. Complementary and alternative medicine: Impact on dentistry. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98:137–45. doi: 10.1016/j.tripleo.2004.05.011. [DOI] [PubMed] [Google Scholar]
- 18.Mutluay YE, Izgu N, Ozdemir L, Erdem SA, Kartal M. Sage tea-thyme-peppermint hydrosol oral rinse reduces chemotherapy-induced oral mucositis: A randomized controlled pilot study. Complement Ther Med. 2016;27:58–64. doi: 10.1016/j.ctim.2016.05.010. [DOI] [PubMed] [Google Scholar]
- 19.Assaf AM, Amro BI, Mashallah S, Haddadin RN. Antimicrobial and anti-inflammatory potential therapy for opportunistic microorganisms. J Infect Dev Ctries. 2016;10:494–505. doi: 10.3855/jidc.7610. [DOI] [PubMed] [Google Scholar]
- 20.Taheri JB, Azimi S, Rafieian N, Zanjani HA. Herbs in dentistry. Int Dent J. 2011;61:287–96. doi: 10.1111/j.1875-595X.2011.00064.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kumar G, Jalaluddin M, Rout P, Mohanty R, Dileep CL. Emerging trends of herbal care in dentistry. J Clin Diagn Res. 2013;7:1827–9. doi: 10.7860/JCDR/2013/6339.3282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Koch C, Reichling J, Schneele J, Schnitzler P. Inhibitory effect of essential oils against herpes simplex virus Type 2. Phytomedicine. 2008;15:71–8. doi: 10.1016/j.phymed.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 23.Cohen DM, Bhattacharyya I. Cinnamon-induced oral erythema multiformelike sensitivity reaction. J Am Dent Assoc. 2000;131:929–34. doi: 10.14219/jada.archive.2000.0311. [DOI] [PubMed] [Google Scholar]
- 24.Chonco WZ. The African Bantu traditional practice of medicine: Some preliminary observations. Soc Sci Med. 1972;6:283–322. doi: 10.1016/0037-7856(72)90104-7. [DOI] [PubMed] [Google Scholar]
- 25.Ahuja S, Dodwad V, Kukreja BJ, Mehra P, Kukreja P. A comparative evaluation of efficacy of Punica granatum and chlorhexidine on plaque and gingivitis. J Int Clin Dent Res Organ. 2011;3:29–32. [Google Scholar]
- 26.Sastravaha G, Yotnuengnit P, Booncong P, Sangtherapitikul P. Adjunctive periodontal treatment with Centella asiatica and Punica granatum extracts. A preliminary study. J Int Acad Periodontol. 2003;5:106–15. [PubMed] [Google Scholar]
- 27.Sofrata A, Brito F, Al-Otaibi M, Gustafsson A. Short term clinical effect of active and inactive Salvadora persica miswak on dental plaque and gingivitis. J Ethnopharmacol. 2011;137:1130–4. doi: 10.1016/j.jep.2011.07.034. [DOI] [PubMed] [Google Scholar]
- 28.Raynaud J. Prescription et Conseil en Phytothérapie. Paris, France: Tec & Doc Lavoisier; 2005. p. 40. [Google Scholar]
- 29.Karygianni L, Cecere M, Skaltsounis AL, Argyropoulou A, Hellwig E, Aligiannis N, et al. High-level antimicrobial efficacy of representative Mediterranean natural plant extracts against oral microorganisms. Biomed Res Int. 2014;2014:839019. doi: 10.1155/2014/839019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bellakhdar J. La Pharmacopée Marocaine Traditionnelle: Médecine Arabe Ancienne et Savoirs Populaires. France: Ibis Press; 1997. [Google Scholar]
- 31.Alali F, Hudaib M, Aburjai T, Khairallah K, Al-Hadidi N. GC-MS analysis and antimicrobial activity of the essential oil from the stem of the Jordanian toothbrush tree Salvadora persica. Pharm Biol. 2004;42:577–80. [Google Scholar]
- 32.Khalessi AM, Pack AR, Thomson WM, Tompkins GR. An in vivo study of the plaque control efficacy of Persica: A commercially available herbal mouthwash containing extracts of Salvadora persica. Int Dent J. 2004;54:279–83. doi: 10.1111/j.1875-595x.2004.tb00294.x. [DOI] [PubMed] [Google Scholar]
- 33.Raina R, Kumar V, Krishna M, Raina S, Jaiswal A, Selvan A, et al. A comparison of antibacterial efficacy of 0.5% sodium fluoride impregnated miswak and plain miswak sticks on Streprococcus mutans - A randomized controlled trial. J Clin Diagn Res. 2017;11:ZC01–4. doi: 10.7860/JCDR/2017/21250.9165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.González-Tejero MR, Casares-Porcel M, Sánchez-Rojas CP, Ramiro-Gutiérrez JM, Molero-Mesa J, Pieroni A, et al. Medicinal plants in the Mediterranean area: Synthesis of the results of the project Rubia. J Ethnopharmacol. 2008;116:341–57. doi: 10.1016/j.jep.2007.11.045. [DOI] [PubMed] [Google Scholar]
- 35.Chow JW. Aminoglycoside resistance in enterococci. Clin Infect Dis. 2000;31:586–9. doi: 10.1086/313949. [DOI] [PubMed] [Google Scholar]
- 36.Mandal S, DebMandal M, Saha K, Pal NK. In vitro antibacterial activity of three Indian spices against methicillin-resistant Staphylococcus aureus. Oman Med J. 2011;26:319–23. doi: 10.5001/omj.2011.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ali SM, Khan AA, Ahmed I, Musaddiq M, Ahmed KS, Polasa H, et al. Antimicrobial activities of eugenol and cinnamaldehyde against the human gastric pathogen Helicobacter pylori. Ann Clin Microbiol Antimicrob. 2005;20:4–20. doi: 10.1186/1476-0711-4-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ahmad M, Imran H, Yaqeen Z, Rehman Z, Rahman A, Fatima N, et al. Pharmacological profile of Salvadora persica. Pak J Pharm Sci. 2011;24:323–30. [PubMed] [Google Scholar]
- 39.Rao NJ, Kumar KS, Subash KR. Phytotherapy in gingivitis; A review. Int J Periodontol. 2012;8:1–5. [Google Scholar]
- 40.Darout IA, Skaug N, Albandar JM. Subgingival microbiota levels and their associations with periodontal status at the sampled sites in an adult Sudanese population using miswak or toothbrush regularly. Acta Odontologica. 2003;61:115–22. doi: 10.1080/00016350310002784. [DOI] [PubMed] [Google Scholar]
- 41.Al-Bayaty FH, AI-Koubaisi AH, Ali NA, Abdulla MA. Effect of mouth wash extracted from Salvadora persica (miswak) on dental plaque formation: A clinical trial. J Med Plant Res. 2010;4:1446–54. [Google Scholar]
- 42.Yang JF, Yang CH, Chang HW, Yang CS, Wang SM, Hsieh MC, et al. Chemical composition and antibacterial activities of Illicium verum against antibiotic-resistant pathogens. J Med Food. 2010;13:1254–62. doi: 10.1089/jmf.2010.1086. [DOI] [PubMed] [Google Scholar]
- 43.Iauk L, Lo Bue AM, Milazzo I, Rapisarda A, Blandino G. Antibacterial activity of medicinal plant extracts against periodontopathic bacteria. Phytother Res. 2003;17:599–604. doi: 10.1002/ptr.1188. [DOI] [PubMed] [Google Scholar]
- 44.Khan ST, Khan M, Ahmad J, Wahab R, Abd-Elkader OH, Musarrat J, et al. Thymol and carvacrol induce autolysis, stress, growth inhibition and reduce the biofilm formation by Streptococcus mutans. AMB Express. 2017;7:49. doi: 10.1186/s13568-017-0344-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lamendin H, Toscano GB, Requirand P. Buccodental phytotherapy and aromatherapy. EMC Dent. 2004;1:179–92. [Google Scholar]
- 46.Kamatou GP, Vermaak I, Viljoen AM. Eugenol - from the remote Maluku Islands to the international market place: A review of a remarkable and versatile molecule. Molecules. 2012;17:6953–81. doi: 10.3390/molecules17066953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sijelmassi A. Les Plantes Médicinales du Maroc. Edition. Casablanca: Le fennec; 1996. [Google Scholar]
- 48.Imelouane B, Amhamdi H, Wathelet J, Ankit M, Kheded K, Elbachiri A. Chemical composition and antimicrobial activity of essential oil of thyme (Thymus vulgaris) from Eastern Morocco. Int J Agric Biol. 2009;11:205–8. [Google Scholar]
- 49.Stahl-Biskup E, Saez F. Thyme: The Genus Thymus. New York: CRC Press; 2002. p. 352. [Google Scholar]
- 50.Unlu M, Ergene E, Unlu GV, Zeytinoglu HS, Vural N. Composition, antimicrobial activity and in vitro cytotoxicity of essential oil from Cinnamomum zeylanicum Blume (Lauraceae) Food Chem Toxicol. 2010;48:3274–80. doi: 10.1016/j.fct.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 51.Iscan G, Kirimer N, Kürkcüoglu M, Baser KH, Demirci F. Antimicrobial screening of Mentha piperita essential oils. J Agric Food Chem. 2002;50:3943–6. doi: 10.1021/jf011476k. [DOI] [PubMed] [Google Scholar]
- 52.Kozlowska M, Laudy AE, Przybyl J, Ziarno M, Majewska E. Chemical composition and antibacterial activity of some medicinal plants from Lamiaceae family. Acta Pol Pharm. 2015;72:757–67. [PubMed] [Google Scholar]
- 53.Rao A, Zhang Y, Muend S, Rao R. Mechanism of antifungal activity of terpenoid phenols resembles calcium stress and inhibition of the TOR pathway. Antimicrob Agents Chemother. 2010;54:5062–9. doi: 10.1128/AAC.01050-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Khadir A, Sobeh M, Gad HA, Benbelaid F, Bendahou M, Peixoto H, et al. Chemical composition and biological activity of the essential oil from Thymus lanceolatus. Z Naturforsch C. 2016;71:155–63. doi: 10.1515/znc-2016-0005. [DOI] [PubMed] [Google Scholar]
- 55.Mahboubi M, Haghi G. Antimicrobial activity and chemical composition of Mentha pulegium L. Essential oil. J Ethnopharmacol. 2008;119:325–7. doi: 10.1016/j.jep.2008.07.023. [DOI] [PubMed] [Google Scholar]
- 56.Vieira M, Bessa LJ, Martins MR, Arantes S, Teixeira AP, Mendes Â, et al. Chemical composition, antibacterial, antibiofilm and synergistic properties of essential oils from Eucalyptus globulus Labill. And seven mediterranean aromatic plants. Chem Biodivers. 2017 doi: 10.1002/cbdv.201700006. Doi:10.1002/cbdv.201700006. [DOI] [PubMed] [Google Scholar]
- 57.Aires A, Marrinhas E, Carvalho R, Dias C, Saavedra MJ. Phytochemical composition and antibacterial activity of hydroalcoholic extracts of Pterospartum tridentatum and Mentha pulegium against Staphylococcus aureus isolates. Biomed Res Int. 2016;2016:5201879. doi: 10.1155/2016/5201879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.De Martino L, De Feo V, Formisano C, Mignola E, Senatore F. Chemical composition and antimicrobial activity of the essential oils from three chemotypes of Origanum vulgare L. ssp. Hirtum (link) letswaart growing wild in Campania (Southern Italy) Molecules. 2009;14:2735–46. doi: 10.3390/molecules14082735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Khoury M, Stien D, Eparvier V, Ouaini N, El Beyrouthy M. Report on the medicinal use of eleven Lamiaceae species in lebanon and rationalization of their antimicrobial potential by examination of the chemical composition and antimicrobial activity of their essential oils. Evid Based Complement Alternat Med. 2016;2016:2547169. doi: 10.1155/2016/2547169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Delamare AP, Moschen-Pistorello I, Artico L, Atti-Serafini L, Echeverrigaray S. Antibacterial activity of the essential oils of Salvia officinalis L. and Salvia triloba L. Cultivated in South Brazil. J Food Chem. 2007;100:603–8. [Google Scholar]
- 61.Jalsenjak V, Peljnjak S, Kustrak D. Microcapsules of sage oil: Essential oils content and antimicrobial activity. Pharmazie. 1987;42:419–20. [PubMed] [Google Scholar]
- 62.Sivropoulou A, Nikolaou C, Papanikolaou E, Kokkini S, Lanaras T, Arsenakis M. Antimicrobial, cytotoxic, and antiviral activities of Salvia fruticose essential oil. J Agric Food Chem. 1997;45:3197–201. [Google Scholar]
- 63.Sur SV, Tuljupa F, Sur LI. Gas chromatographic determination of monoterpenes in essential oil medicinal plans. J Chromatogr. 1991;542:451–8. [Google Scholar]
- 64.Newall CA, Anderson LA, Phillipson JD. Herbal Medicines. A Guide for Health-Care Professionals. London: The Pharmaceutical Press; 1996. pp. 256–7. [Google Scholar]
- 65.Sarrami N, Pemberton MN, Thornhill MH, Theaker ED. Adverse reactions associated with the use of eugenol in dentistry. Br Dent J. 2002;193:257–9. doi: 10.1038/sj.bdj.4801539. [DOI] [PubMed] [Google Scholar]
- 66.Groppo FC, Bergamaschi Cde C, Cogo K, Franz-Montan M, Motta RH, de Andrade ED. Use of phytotherapy in dentistry. Phytother Res. 2008;22:993–8. doi: 10.1002/ptr.2471. [DOI] [PubMed] [Google Scholar]
- 67.Palombo EA. Traditional plant extracts and natural products with activity against oral bacteria: Potential application in the prevention and treatment of oral diseases. Evid Based Complement Alternat Med. 2011;1:1–15. doi: 10.1093/ecam/nep067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Chambial S, Bhardwaj P, Mahdi AA, Sharma P. Lead poisoning due to herbal medications. Indian J Clin Biochem. 2017;32:246–7. doi: 10.1007/s12291-016-0617-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Poivre M, Duez P. Biological activity and toxicity of the Chinese herb Magnolia officinalis Rehder & E. Wilson (Houpo) and its constituents. J Zhejiang Univ Sci B. 2017;18:194–214. doi: 10.1631/jzus.B1600299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Alempijevic T, Zec S, Milosavljevic T. Drug-induced liver injury: Do we know everything? World J Hepatol. 2017;9:491–502. doi: 10.4254/wjh.v9.i10.491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Conover EA. Herbal agents and over-the-counter medications in pregnancy. Best Pract Res Clin Endocrinol Metab. 2003;17:237–51. doi: 10.1016/s1521-690x(02)00102-1. [DOI] [PubMed] [Google Scholar]


