Abstract
Individuals experiencing homelessness in the United States are aging; little is known about chronic pain in this population. In a cross-sectional, population-based study, we interviewed 350 homeless individuals aged 50 and older to describe pain experienced by older persons experiencing homelessness and to assess factors associated with chronic moderate to severe pain, defined as pain lasting ≥3 months, with a past week average severity score of 5–10 (scale 0–10). The median age of participants was 58 years. Participants were predominantly African American (79.6%) and male (77.3%). Overall, 46.8% reported chronic moderate to severe pain. Almost half of participants reported a diagnosis of arthritis (44.3%) and one-third reported symptoms consistent with post-traumatic stress disorder (PTSD, 32.8%). Three-quarters (75.3%) endorsed a personal history of abuse. In multivariate analyses, PTSD (AOR: 2.2, CI 1.4–3.7), arthritis (AOR: 4.8, CI 3.0–7.8), and history of experiencing abuse (AOR: 2.4, CI 1.3–4.3) were associated with chronic moderate to severe pain. HIV status, diabetes, depressive symptoms, and substance use were not associated with pain. Clinicians should consider the management of associated mental health conditions and the sequelae of experiencing abuse in the treatment of chronic pain in older adults experiencing homelessness.
Keywords: chronic pain, homeless persons, post-traumatic stress disorders
Introduction
More than 500,000 individuals in the United States are homeless at any time and approximately 3 million experience homelessness over the course of a year.43 The median age of adults experiencing homelessness has risen and is now approximately 50 years.21 Homelessness is a risk factor for many adverse health conditions, including aging-related conditions.6, 12, 35 Individuals experiencing homelessness have an earlier onset of age-related problems than the general population. In their 50s and 60s, they have a similar prevalence of geriatric conditions as housed adults in their 70s and 80s.14 Due to high prevalence of functional and cognitive impairments, researchers and practitioners consider homeless adults “older” at age 50.13, 14
Pain is a common and challenging symptom, and the risk factors, severity, and duration of pain are well studied in the general population.30 Chronic non-cancer pain, defined as pain lasting for longer than 3 months not attributable to malignancy, is common.85 While studies have examined chronic pain among older adults or homeless individuals, little is known about the risk factors for chronic pain in older adults experiencing homelessness.19, 28, 37, 45, 71 Compared with the general population, people who experience homelessness are more likely to report conditions associated with an increased prevalence and severity of chronic pain, including chronic physical and mental health disorders, substance use disorders, tobacco dependence, and histories of childhood physical or sexual abuse.5, 93 In addition, people who are homeless experience challenging physical environments (e.g., exposure to the elements, violence, overcrowded shelters, the requirement to walk long distances, a lack of bedding) which may worsen pain.51, 66, 87
Improving our understanding of chronic pain in older adults experiencing homelessness may aid efforts to identify effective ways to treat and relieve their suffering. In this study, we describe the severity and duration of pain and its association with demographic and clinical characteristics in a community-recruited sample of homeless adults aged 50 and older. We hypothesized a high prevalence of chronic moderate to severe pain. We explored factors associated with chronic pain, including: gender, race, age, physical environment, history of abuse, substance use, mental health problems, and physical health.
Methods
During July 2013 to June 2014, we enrolled a population-based sample of 350 homeless adults from overnight shelters, homeless encampments, meal programs, and a recycling center in Oakland, California.15 Based on the estimates of the number of unique individuals who used each site annually, we approached potential participants in a random order and assessed for interest and preliminary eligibility. Following an eligibility interview, study staff recruited individuals meeting the following criteria: (1) homeless as defined by the Homeless Emergency Assistance and Rapid Transition to Housing (HEARTH) Act, (2) English-speaking, (3) aged 50 or over, and (4) able to provide informed consent as verified by using a teach-back mechanism.8, 17 The HEARTH Act includes both individuals who lack a fixed residence or reside in a place not typically used for sleeping and individuals who are at imminent risk of losing housing within fourteen days. It acknowledges that people who are homeless reside in a variety of environments.42 We conducted study interviews at a community-based center that provided social services for low-income older adults. Participants did not have to be eligible for, or receive services at the Center. Trained study staff members administered the questionnaires. Participants received gift cards valued at $5 and $20 for the eligibility and baseline interviews, respectively. The Institutional Review Board of the University of California, San Francisco approved the study. Participants provided written informed consent for participation.
Dependent Variables
We assessed the prevalence, severity, and duration of pain using questions from the Brief Pain Inventory (BPI).3, 54, 62, 74 We asked participants whether they had experienced pain or taken medicine for pain in the past week. Next, we asked participants to rate their average pain over the past week on a 0–10 numeric rating scale, where 0 was ‘no pain’ and 10 was ‘pain as bad as you can imagine’. We categorized average pain ratings as no to mild (0–4), moderate (5–7), and severe (8–10) pain.62 If individuals indicated in response to the first question that they had not experienced pain in the past week, we classified their pain as ‘zero’. We asked participants with pain how long they had experienced their pain. We categorized these answers as ‘less than 3 months’, ‘3 months to 5 years’, and ‘more than 5 years’. We categorized participants with moderate to severe pain lasting over 3 months as experiencing chronic pain.85
We asked participants to rate how their pain interfered with their enjoyment of life and general activity on a scale of 0 (does not interfere) to 10 (completely interferes).3 We categorized these responses as mild (0–4), moderate (5–7), and severe interference (8–10).
Independent Variables
Demographics
We collected demographic information including age, sex, and race/ethnicity (categorized as African American/non-African American), and highest educational attainment (dichotomized as having graduated from high school, including general educational development (GED), versus having not graduated from high school).88
Housing
Using a follow-back residential calendar, we asked participants to report the location and duration of their living environments, by night, over the past 6 months.86 Living locations included: homeless shelters, unsheltered places, housing belonging to family/friends, transitional housing, hotels or single room occupancy units, rented rooms or apartments, owned homes, medical facilities, drug treatment facilities, and jail or prison.
Substance Use
We administered the Alcohol Use Disorders Identification Test (AUDIT) with a shortened timeframe of the previous 6 months to assess current risk and severity of alcohol use symptoms.23, 31 The AUDIT has been shown to correlate with alcohol use disorder as defined in the DSM IV.56 We categorized scores of ≥8 as indicative of moderate to high severity alcohol use.40
To assess use of illicit substances (cannabis, cocaine, amphetamine, inhalants, sedatives, hallucinogens, and opioids), we administered the Alcohol, Smoking and Substance Involvement Screening Test (ASSIST)49, 77 for each illicit substance using a 6 month timeframe, classifying current substance use as low (score 0–3) or moderate to high risk (≥4).40
Mental Health and Adverse Experiences
To assess the prevalence of depressive symptomatology, we administered the Center for Epidemiologic Studies Depression Scale (CES-D).55, 96 We used the standard threshold CES-D score of ≥16 to indicate depressive symptoms.92 To assess for potential post-traumatic stress disorder, we administered the Primary Care PTSD Screen (PC-PTSD).67, 68 We considered a score of ≥3 to indicate likely PTSD.68, 89 We adapted questions from the National Survey of Homeless Assistance Providers and Clients (NSHAPC) and the Addiction Severity Index (ASI) to inquire whether participants had ever had a significant period during which they experienced anxiety that was not a direct result of drug or alcohol use.61 Then, we asked how recently they had experienced this anxiety and dichotomized responses according to whether they experienced anxiety during the previous 30 days.
We asked participants if they experienced verbal, physical, or sexual abuse, either in childhood or adulthood.33 We created a single composite variable (history of abuse ever versus never).
Physical Health
We inquired about health conditions that are prevalent in this population and likely associated with pain, including arthritis, human immunodeficiency virus (HIV), diabetes, and traumatic brain injury (TBI).5, 6, 20 To assess for HIV infection, we asked participants whether they had ever been tested and if so, for the result of the test. We asked participants whether a clinician had ever told them that they had diabetes or arthritis. To evaluate for a history of likely TBI, we asked participants whether they had ever been hit in the head, and if so, whether any of the three most severe head injuries resulted in loss of consciousness.83 We categorized responses as TBI if any head injury resulted in loss of consciousness.
Geriatric Conditions
To assess cognitive functioning, we administered the Modified Mini-Mental State (3MS) Examination.9 We categorized participants scoring 1.5 standard deviations below the reference mean (below the 7th percentile) as having cognitive impairment.11 To assess functional status, we asked participants to report if they had difficulty performing any of 5 activities of daily living (ADLs; bathing, dressing, eating, transferring, or toileting)46 and 6 instrumental activities of daily living (IADLs; taking transportation, managing medications, managing money, applying for benefits, setting up a job interview, or finding a lawyer).78 We defined ADL impairment as having difficulty performing ≥ 1 ADL; we defined IADL impairment as difficulty performing ≥ 1 IADL.
Statistical Analyses
To assess the association of chronic pain with living environment, we used participants’ self-report of the places where they had stayed for the prior 6 months. We performed a cluster analysis to create a classification of living environments.53 We used Ward’s linkage to minimize the sum-of-square differences within groups. We performed visual analysis of a dendrogram representing the structure of the data to select the optimum number of clusters. Using bivariate matrices, we confirmed that we could identify natural groupings. We used k-medians cluster methodology to verify cluster classifications.16
We performed chi-square tests of significance for differences in the independent variables representing the domains we hypothesized to be associated with chronic moderate to severe pain. These results informed a multivariate logistic regression analysis in which we included all hypothesized variables that were associated at a p<0.2 level in the bivariate analyses. Then, we used backward selection to define our final, reduced model. We performed a sensitivity analysis to evaluate missing data in our final model by assuming that missing dichotomous variables were either positive or negative and measuring their effects on the observed odds ratios and confidence intervals. We performed all analyses with SAS 9.4 (SAS Institute, Cary, North Carolina).
Results
Demographic and clinical characteristics
A total of 350 participants completed the enrollment interview (Figure 1).14, 53 Two people did not provide information on pain, leaving a sample of 348. The cohort was 77.3% male, 79.6% African American, and 74.4% high school-educated (including GED). The median age was 58 years, with a range from 50–80 years. Almost half (43.6%) of participants first experienced homelessness after turning 50. Almost half (44.3%) of participants reported being diagnosed with arthritis. Three-quarters (75.3%) endorsed a personal history of abuse. Nearly a third (32.8%) reported symptoms consistent with PTSD and over a third (34.3%) reported recent anxiety. Symptoms of depression and substance use problems were common (Table 1).
Figure 1. Flow-chart of recruitment of 350 older homeless adults.
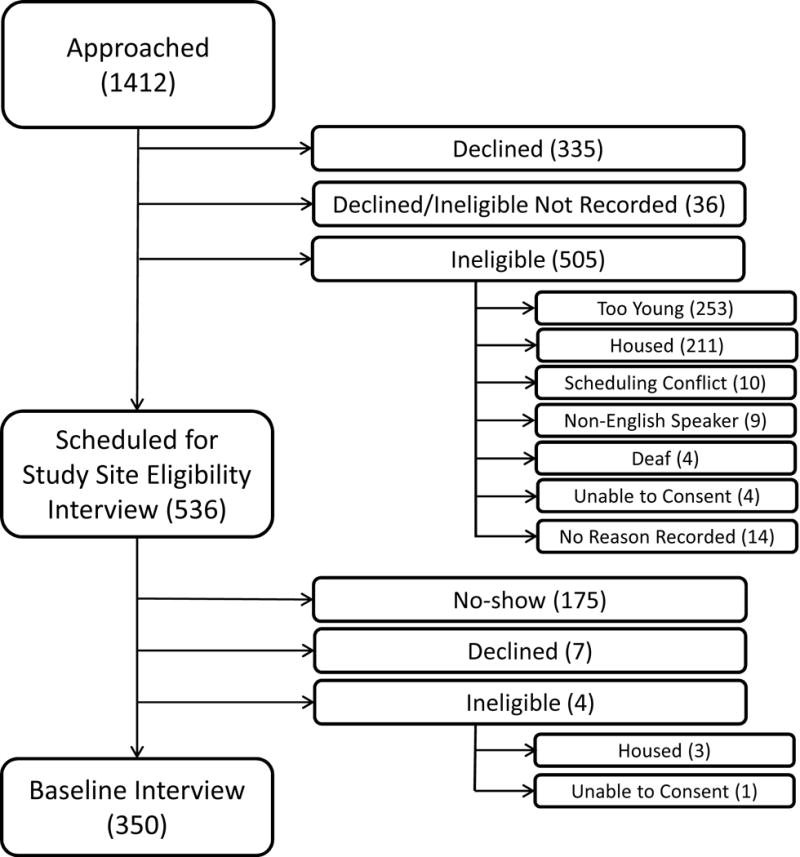
This figure shows the number of individuals approached, assessed for eligibility, and enrolled in the study, noting specific reasons for inability to enroll. Values represent the number of individuals in each group. Participants who declined after being approached (335) declined before being assessed for eligibility. Therefore, the number of participants who were ineligible for the study may have been higher than the numbers presented in this figure.
Table 1.
Baseline characteristics and life course experiences of 348 older homeless adults by chronic pain status
| Characteristic, no (%) | Total (n=348) | No Chronic Pain (n=185) | Chronic Paina (n=163) | P value |
|---|---|---|---|---|
| Sociodemographics | ||||
| Male | 269 (77.3) | 146 (78.9) | 123 (75.5) | 0.44 |
| Black | 277 (79.6) | 143 (77.3) | 134 (82.2) | 0.26 |
| Age | 0.04 | |||
| 50–54 | 102 (29.3) | 55 (29.7) | 47 (28.8) | |
| 55–59 | 115 (33.0) | 51 (27.6) | 64 (39.3) | |
| 60–64 | 89 (25.6) | 50 (27.0) | 39 (23.9) | |
| 65+ | 42 (12.1) | 29 (15.7) | 13 (8.0) | |
| Less Than High School Education or GEDb | 89 (25.6) | 46 (25.0) | 43 (26.4) | 0.77 |
| Housing Group | 0.52 | |||
| Cohabitersc | 57 (16.4) | 26 (14.1) | 31 (19.0) | |
| Multiple Institution Usersd | 87 (25.0) | 47 (25.4) | 40 (24.5) | |
| Recently Homelesse | 43 (12.4) | 26 (14.1) | 17 (10.4) | |
| Unshelteredf | 161 (46.3) | 86 (46.5) | 75 (46.0) | |
| History of Abuseg | 262 (75.3) | 126 (68.1) | 136 (83.4) | <0.001 |
| Health History | ||||
| HIVh | 19 (6.0) | 8 (4.8) | 11 (7.2) | 0.38 |
| Diabetesi | 49 (14.1) | 24 (13.0) | 25 (15.3) | 0.54 |
| Arthritisj | 154 (44.3) | 50 (27.0) | 104 (63.8) | <0.001 |
| Traumatic Brain Injuryk | 130 (38.2) | 59 (32.6) | 71 (44.7) | 0.02 |
| Post-Traumatic Stress Disorderl | 114 (32.8) | 42 (22.7) | 72 (44.2) | <0.001 |
| Depressive Symptomsm | 185 (53.5) | 86 (46.5) | 99 (61.5) | 0.005 |
| Anxietyn | 118 (34.3) | 47 (25.7) | 71 (44.1) | <0.001 |
| Substance Abuse Problem | ||||
| Alcoholo | 89 (25.6) | 46 (24.9) | 43 (26.4) | 0.75 |
| Any illicit drug except cannibisp | 177 (50.9) | 89 (48.1) | 88 (54.0) | 0.27 |
| Cannabisq | 135 (38.8) | 68 (36.8) | 67 (41.1) | 0.41 |
| Geriatric Conditions | ||||
| Cognitive Impairmentr | 89 (25.6) | 52 (28.3) | 37 (22.7) | 0.24 |
| ADL Impairments | 135 (38.8) | 46 (24.9) | 89 (54.6) | <0.001 |
| IADL Impairmentt | 171 (49.1) | 90 (48.6) | 81 (49.7) | 0.61 |
Chronic Pain defined as Brief Pain Inventory self-rated pain (1 to 10) score of ≥5 lasting over 3 months.
GED, General Educational Development
Cohabiters spent the majority of days staying with friends or family
Multiple Institution Users spent the majority of days in shelters, jail, transitional housing, and other institutions
Renters spent the majority of days in rented rooms or apartments
Unsheltered cluster spent the majority of days unsheltered (on the street or other place not ordinarily used as sleeping accommodations)
History of Abuse defined as experiencing emotional abuse, physical abuse, or sexual abuse at any age
HIV defined as self-report of a positive test for Human Immunodeficiency Virus
Diabetes defined as self-report of a past diagnosis of diabetes by a medical provider
Arthritis defined as self-report of a past diagnosis of arthritis by a medical provider
Traumatic brain injury defined as self-report of head injury leading to loss of consciousness
Post-Traumatic Stress Disorder defined as Primary Care PTSD Screen (PC-PTSD) score of ≥3
Moderate to Severe Depressive Symptoms defined as Center for Epidemiologic Studies-Depression Scale (CES-D) score of ≥16
Anxiety defined as self-report of having ever experienced serious anxiety
Alcohol Use Problem defined as Alcohol Use Disorders Identification Test (AUDIT) score of ≥8
Drug Use Problem, Any Illicit Except Cannabis defined as Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) score of ≥4 for Use of Cocaine, Opioids, Amphetamines, Sedatives, Hallucinogens, or Inhalants
Drug Use Problem, Cannabis defined as Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) score of ≥4 for Use of Cannabis
Cognitive impairment defined as Modified Mini-Mental State Examination score below the 7th percentile (1.5 standard deviations below the age- and education-adjusted reference mean)
ADL impairment defined as difficulty performing ≥1 activities of daily living (ADLs)
IADL impairment defined as difficulty performing ≥1 instrumental activities of daily living (IADLs)
Pain characteristics
In the overall cohort, 17.2% reported moderate pain and 39.4% reported severe pain over the past week. Approximately half of participants (46.8%) reported experiencing chronic moderate to severe pain. The majority (79.9%) of participants experiencing pain reported chronic pain (lasting longer than 3 months). The median duration of both moderate and severe pain was 5 years (IQR for moderate pain 9.2 years; IQR for severe pain 11.4 years). Most individuals with pain reported that it interfered with both general activity and life enjoyment. Participants with severe pain reported the most interference (Table 2).
Table 2.
Pain experiences of 348 older homeless adults by current pain severity
| Characteristic, no (%) | No to Mild Pain, 0–4a (n=151) | Moderate Pain, 5–7a (n=60) | Severe Pain, 8–10a (n=137) | |
|---|---|---|---|---|
| Median Years of Pain, years (IQR) | 0 (0–0) | 5 (0.8–10.0) | 5 (0.6–12.0) | <0.001 b |
| Duration of Pain, n (%) | ||||
| Less than 3 months | 135 (89.4) | 9 (15.0) | 25 (18.3) | <0.001c |
| 3 months to 5 years | 10 (6.6) | 22 (36.7) | 49 (35.8) | |
| More than 5 years | 6 (4.0) | 29 (48.3) | 63 (46.0) | |
| Pain Interference with General Activity (0–10 scale) | ||||
| Mild (0–3), n (%) | 147 (97.4) | 19 (31.7) | 20 (14.6) | <0.001c |
| Moderate (4–7), n (%) | 4 (2.6) | 27 (45.0) | 22 (16.1) | |
| Severe (8–10), n (%) | 0 (0.0) | 14 (23.3) | 95 (69.3) | |
| Median score (IQR) | 0.0 (0–0) | 6.0 (3.5–7.0) | 8.0 (7.0–10.0) | <0.001 b |
| Pain Interference with Enjoyment of Life (0–10 scale) | ||||
| Mild (0–3), n (%) | 149 (98.7) | 17 (28.3) | 14 (10.3) | <0.001c |
| Moderate (4–7), n (%) | 2 (1.3) | 30 (50.0) | 25 (18.4) | |
| Severe (8–10), n (%) | 0 (0.0) | 13 (21.7) | 97 (71.3) | |
| Median score (IQR) | 0.0 (0–0) | 6.0 (4.0–7.0) | 9.0 (7.0–10.0) | <0.001b |
Pain severity assessed by Brief Pain Inventory self-rated pain (score 1 to 10)
Kruskal-Wallis non-parametric test
Chi-square test
We derived four categories of participants based on their current living environments: unsheltered (46.3%), cohabiters (16.3%), multiple institution users (25.1%), and recently homeless (renters) (12.3%). Participants in the unsheltered group spent a large portion (average 154 days) of the prior 6 months in unsheltered locations; cohabiters spent a large portion of their time (average 128 days) staying with friends and family; multiple institution users stayed in multiple locations including shelters, transitional housing, motels, and jails (average 126 days); and renters, who had recently become homeless, spent a large portion of their time (average 144 days) in rental housing.53
Factors associated with chronic pain
In the bivariate analyses, compared with the no to mild pain group, participants with chronic moderate to severe pain described significantly more depressive symptoms, PTSD, recent anxiety, arthritis, histories of traumatic brain injury, and histories of abuse (Table 1). We did not find an association with living environment, gender, race, or substance use. We included significant variables as well as those that met the pre-specified criterion of p<0.2 in our full multivariate model. In our reduced multivariate model, we found significant associations between PTSD (AOR 2.2 [1.4–3.7]), arthritis (AOR 4.8, [3.0–7.8]), and a history of abuse (AOR 2.4 [1.3–4.3]) with chronic pain (Table 3). Depressive symptoms were not significant in the reduced multivariate model.
Table 3.
Multivariate models of factors associated with chronic pain
| Characteristic | Adjusted Odds Ratio (AOR), full model (95% CI) | P-value, full model | AOR, reduced model (95% CI) | P-value, reduced model |
|---|---|---|---|---|
| Age | ||||
| 50–54 | Ref | — | Ref | — |
| 55–59 | 1.5 (0.8 – 2.9) | 0.17 | 1.5 (0.8 – 2.8) | 0.16a |
| 60–64 | 0.8 (0.4 – 1.6) | 0.50 | 0.9 (0.5 – 1.7) | 0.75 |
| 65+ | 0.5 (0.2 – 1.2) | 0.11 | 0.5 (0.2 – 1.1) | 0.07 |
| History of Abuseb | ||||
| No abuse (verbal, physical, sexual) | Ref | — | Ref | — |
| Abuse | 2.5 (1.4 – 4.7) | 0.003 | 2.4 (1.3 – 4.3) | 0.004 |
| Health History | ||||
| Traumatic Brain Injuryc | ||||
| No Traumatic Brain Injury | Ref | — | ||
| Traumatic Brain Injury | 1.3 (0.8 – 2.1) | 0.38 | ||
| Post-Traumatic Stress Disorderd | ||||
| No PTSD | Ref | — | Ref | — |
| PTSD | 2.0 (1.1 – 3.4) | 0.02 | 2.2 (1.4 – 3.7) | 0.002 |
| Depressione | ||||
| No Depressive Symptoms | Ref | — | ||
| Mild to Severe Depressive Symptoms | 0.9 (0.5 – 1.6) | 0.76 | ||
| Anxietyf | ||||
| No Anxiety | Ref | — | ||
| Anxiety | 1.6 (1.0 – 2.8) | 0.07 | ||
| Arthritisg | ||||
| No Arthritis | Ref | — | Ref | — |
| Arthritis | 4.6 (2.8 – 7.6) | <0.001 | 4.8 (3.0 – 7.8) | <0.001 |
Note: Chronic pain defined as Brief Pain Inventory self-rated pain (1 to 10) score of ≥5 lasting over 3 months.
Overall, Type 3 p-value for age = 0.03
History of Abuse defined as experiencing emotional abuse, physical abuse, or sexual abuse at any age
Traumatic Brain Injury defined as self-report of any past head injury resulting in loss of consciousness
Post-Traumatic Stress Disorder defined as Primary Care PTSD Screen (PC-PTSD) score of ≥3
Mild to Severe Depressive Symptoms defined as Center for Epidemiologic Studies-Depression Scale (CES-D) score of ≥16
Anxiety defined as self-report of having ever experienced serious anxiety
Arthritis defined as self-report of a past diagnosis of arthritis by a medical provider
Sensitivity analysis
Two participants did not provide sufficient information to define the chronic pain variable. In our sensitivity analysis, we found that assuming missing values to be either positive or negative did not change any reduced model AORs or confidence limits by more than 0.1.
Discussion
In a sample of adults 50 and older experiencing homelessness, almost half of the participants reported chronic moderate to severe pain. While definitions for chronic pain vary within the literature, the prevalence of chronic pain in the general population ranges from 2.0% to 40.0%.38, 47, 64, 90 Studies of pain in community living older adults found the prevalence of any pain to range from 28%–59%.60 Studies of pain in nursing home residents found the prevalence of pain to range between 32%–57%, with more than half of that reported to be moderate-severe pain.24, 95,81 Despite the younger age of our sample, we found a higher prevalence of chronic moderate-severe pain.
Participants reported their pain to be longstanding: three-quarters of those with moderate or severe pain reported that their pain had lasted for 5 years or more. Participants reported a high prevalence of pain interference, which suggests that, despite other barriers faced by homeless adults, pain plays a role in reducing self-efficacy and quality of life.28 Consistent with other research, we found an association between a personal history of victimization,,22 arthritis, and PTSD symptoms with chronic pain.2, 27 In contrast to other populations,7, 18, 37, 39 we did not find an association between either substance use, number of chronic medical conditions, nor depression and chronic pain.
Our study population experiences a higher burden of chronic disease, injuries, substance use, and mental health problems, than the general population. Despite a median age of 58, our participants had a higher prevalence of functional and cognitive impairments than the general population of older adults in their 70s and 80s.13 The high prevalence of these factors, as well as unique factors associated with homelessness may explain the high prevalence of chronic pain in our sample.18, 37, 39 Homeless adults experience harsh environmental conditions: approximately half spent almost all of their nights outdoors, without shelter. A significant minority spent many nights in group shelter situations, where individuals may sleep on floor mats or low quality mattresses. These conditions may contribute to the high prevalence of chronic pain. The lack of an association between substance use and chronic pain may be due to its overall high prevalence in our sample.
We found that PTSD was more prevalent than in the general population and that it was associated with chronic pain. More than 40% of those who experienced chronic moderate to severe pain and more than 20% of those who did not, had likely PTSD, compared to approximately 8% of the general population.48 These prevalence ratios are similar to those found in other studies of homeless populations.80, 84 PTSD is common in homeless populations, possibly due to a high prevalence of traumatic childhood experiences, high prevalence of experiencing interpersonal violence, exposure to violence while homeless, coexisting psychiatric disorders, and poor social support.51, 65, 79, 87 Unstable housing status may itself contribute to the development of PTSD.32 Existing research conceptualizes the relationships between chronic pain and PTSD to be one of mutual maintenance.75, 76 Mutual maintenance asserts that mental health and substance use disorders maintain or worsen existing pain, while pain worsens these underlying conditions. The effective management of both pain and mental health problems should incorporate treatment of pain and behavioral health conditions simultaneously and longitudinally.2, 82
We found a high prevalence of arthritis and a strong association between arthritis and chronic pain. In studies of primary care in the general population, older individuals are more likely than younger ones to attribute pain to arthritis. Approximately one-quarter of chronic pain in adults ≥55 years is attributed to arthritis.26 In a previous study of chronic pain in homeless adults of all ages, between 9% and 24% attributed their pain to arthritis.45 Homeless older adults may have fewer evidence-based treatment options for arthritis pain (i.e., physical therapy, weight loss or joint replacement surgery) than the general population, due to difficulties accessing regular medical care, low-impact exercise, and healthy food choices.5, 59, 94
Finally, our study found that victimization throughout the life course was associated with chronic pain. Similar associations were found in other populations.22 The increased recognition of the role of trauma in chronic pain and other clinical conditions has led to the development of “trauma informed care” as an approach to address patients’ experiences of trauma. Trauma informed care refers to the reorientation of systems of care to incorporate a fundamental understanding of the role that traumatic experiences play in the lives and symptoms of people seeking care. Although limited data exists as to its effectiveness, especially for the relief of somatic symptoms such as physical pain, data that do exist suggest that trauma informed care reduces PTSD and depressive symptoms.4, 69, 72, 91
While the efficacy of opioid analgesics for the treatment of chronic non-cancer pain is questioned,1, 97 their use for this condition remains widespread.50, 57, 70 While older adults may, counterintuitively, experience a lower risk of overdose than younger adults,10 the co-occurrence of substance use disorders and the chaotic conditions of homelessness limit the use of opioids in this population. While multiple consensus statements describe multidisciplinary care (i.e. medication, behavioral health treatment, physical reconditioning, and self-management education) as the best approach for the management of chronic pain, limited data are available to support its efficacy.34, 73 Most studies showed only a modest effect for a minority of participants with no or minimal benefits lasting after six months.29, 41 Even if this care were efficacious, homeless individuals face numerous barriers to engaging in longitudinal care, including their need to prioritize food and housing, lack of insurance or financial resources, inadequate transportation, and inability to communicate with clinicians between visits.36, 52, 94
The health care of patients experiencing homelessness and the challenges of managing chronic pain are both foci of increasing research interest,44, 58, 63 yet chronic pain remains largely understudied among homeless adults. Homeless individuals face many barriers to research participation, and in particular, few studies focused on the emerging population of older homeless individuals. Most existing studies of homeless populations recruit either from health care facilities or homeless shelters, which may not be representative. By using population-based sampling and focusing on older homeless adults, our study provides the first estimates of chronic pain in a high-risk, but poorly understood, group of individuals. Our data demonstrate that chronic pain is not only common, but that it has detrimental effects on life enjoyment and general activity in older homeless adults. By decreasing functioning, chronic pain presents yet another hurdle for marginalized and under-resourced individuals to receive much needed health care and social services. In addition to causing physical and emotional distress, chronic pain can hamper individuals’ abilities to obtain and retain employment and stable housing, let alone to manage other health problems.
This study has several limitations. The analysis is cross-sectional, so we cannot identify causality. Only 12% of the study participants are aged 65 or over, reflecting, in part, premature mortality among homeless adults. While homeless populations are considered “older” by age 50,13, 14 the study population is younger than most studies of older adults. Study participants’ poor access to health care may lead to underreporting of chronic health conditions, limiting our ability to find associations. Due to the stigma associated with victimization, participants may have underreported experiences of verbal, physical, or sexual abuse. This misclassification would limit our ability to find an association between abuse and chronic pain, so our results could be interpreted as conservative. We did not assess pain-related diagnoses, such as back pain, sprains, strains, or fractures, or obtain participants’ understanding of the causes of their pain. We did not attain data on how they managed their pain or whether they had received treatment, including medication, for their pain. Prior research shows that individuals insured by Medicaid who have chronic pain diagnoses are more likely than those who are privately insured to receive opioid pain medication, and those with co-morbid mental health and substance use disorders are more likely to receive opioid treatment for chronic pain than those without such diagnoses.25 Determining the causes of chronic pain in this population, as well as the relationships between chronic pain, comorbid conditions, and the receipt of opiates are important directions for future research.
Chronic pain management is challenging due to the nature of the condition and the limited data on the efficacy of any treatment strategy. This challenge is especially true in a population with severe, chronic pain, poor access to longitudinal care, limitations in medications that can be used safely, and exposure to difficult environmental conditions. The high prevalence of chronic pain in people experiencing homelessness will require responses that address both pain and mental health problems that are adaptable to the needs of this growing population.
Perspective.
This article describes the prevalence and factors associated with chronic pain in older homeless adults. Almost half report chronic pain, which was associated with post-traumatic stress disorder, arthritis, and personal history of abuse. Clinicians should address chronic pain, trauma, and the associated mental health conditions in this high-risk population.
Highlights.
Half of older homeless adults report chronic moderate to severe pain.
Older homeless adults experienced moderate to severe pain for a median of 5 years.
Chronic moderate to severe pain was associated with arthritis, PTSD, and abuse.
Acknowledgments
We gratefully acknowledge our colleagues Pamela Olsen, Nina Fiellin, Tauni Marin, and Kenneth Perez for their invaluable contributions to the HOPE HOME study. We would like to acknowledge our colleague Angela Allen, who passed away in May of 2015, for her incredible contributions to the study. We thank the staff at St. Mary’s Center and the HOPE HOME Community Advisory Board for their guidance and partnership.
Disclosures: This study was funded by grants from the National Institute on Aging at the National Institutes of Health [K24AG046372, R01AG041860, P30AG044281]. These funding sources had no role in the preparation, review, or approval of the manuscript. M.B. Kushel is a member of the leadership board of Everyone Home, which seeks to end homelessness in Alameda County, CA. The authors report no other conflicts of interest or financial disclosures. This study was approved by the Institutional Review Board of the University of California San Francisco.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Arnér S, Meyerson BA. Lack of analgesic effect of opioids on neuropathic and idiopathic forms of pain. Pain. 1988;33:11–23. doi: 10.1016/0304-3959(88)90198-4. [DOI] [PubMed] [Google Scholar]
- 2.Asmundson GJG, Katz J. Understanding the Co-Occurrence of Anxiety Disorders and Chronic Pain: State-of-the-Art. Depress Anxiety. 2009;26:888–901. doi: 10.1002/da.20600. [DOI] [PubMed] [Google Scholar]
- 3.Atkinson TM, Rosenfeld BD, Sit L, Mendoza TR, Fruscione M, Lavene D, Shaw M, Li Y, Hay J, Cleeland CS, Scher HI, Breitbart WS, Basch E. Using confirmatory factor analysis to evaluate construct validity of the Brief Pain Inventory (BPI) J Pain Symptom Manage. 2011;41:558–565. doi: 10.1016/j.jpainsymman.2010.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Azeem MW, Aujla A, Rammerth M, Binsfeld G, Jones RB. Effectiveness of six core strategies based on trauma informed care in reducing seclusions and restraints at a child and adolescent psychiatric hospital. J Child Adolesc Psychiatr Nurs. 2011;24:11–15. doi: 10.1111/j.1744-6171.2010.00262.x. [DOI] [PubMed] [Google Scholar]
- 5.Baggett TP, Connell JJ, Singer DE, Rigotti NA. The unmet health care needs of homeless adults: a national study. Am J Public Health. 2010;100:1326–1333. doi: 10.2105/AJPH.2009.180109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baggett TP, Hwang SW, Connell JJ, Porneala BC, Stringfellow EJ, Orav EJ, Singer DE, Rigotti NA. Mortality among homeless adults in Boston: shifts in causes of death over a 15-year period. JAMA internal medicine. 2013;173:189–195. doi: 10.1001/jamainternmed.2013.1604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: a literature review. Arch Intern Med. 2003;163:2433–2445. doi: 10.1001/archinte.163.20.2433. [DOI] [PubMed] [Google Scholar]
- 8.Berg S. The HEARTH Act. Cityscape. 2013;15:317–323. [Google Scholar]
- 9.Bland RC, Newman SC. Mild dementia or cognitive impairment: the Modified Mini-Mental State examination (3MS) as a screen for dementia. Can J Psychiatry. 2001;46:506–510. doi: 10.1177/070674370104600604. [DOI] [PubMed] [Google Scholar]
- 10.Bohnert AS, Valenstein M, Bair MJ, Ganoczy D, McCarthy JF, Ilgen MA, Blow FC. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011;305:1315–1321. doi: 10.1001/jama.2011.370. [DOI] [PubMed] [Google Scholar]
- 11.Bravo G, Hebert R. Age- and education-specific reference values for the Mini-Mental and modified Mini-Mental State Examinations derived from a non-demented elderly population. Int J Geriatr Psychiatry. 1997;12:1008–1018. doi: 10.1002/(sici)1099-1166(199710)12:10<1008::aid-gps676>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 12.Breakey WR, Fischer PJ, Kramer M, Nestadt G, Romanoski AJ, Ross A, Royall RM, Stine OC. Health and mental health problems of homeless men and women in Baltimore. JAMA. 1989;262:1352–1357. [PubMed] [Google Scholar]
- 13.Brown RT, Hemati K, Riley ED, Lee CT, Ponath C, Tieu L, Guzman D, Kushel MB. Geriatric Conditions in a Population-Based Sample of Older Homeless Adults. Gerontologist. 2016 Feb 26; doi: 10.1093/geront/gnw011. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brown RT, Kiely DK, Bharel M, Mitchell SL. Geriatric syndromes in older homeless adults. J Gen Intern Med. 2012;27:16–22. doi: 10.1007/s11606-011-1848-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Burnam MA, Koegel P. Methodology for Obtaining a Representative Sample of Homeless Persons The Los Angeles Skid Row Study. Evaluation Review. 1988 [Google Scholar]
- 16.Calinski T, Harabasz J. A dendrite method for cluster analysis. Communications in Statistics. 1974;3:1–27. [Google Scholar]
- 17.Carpenter WT, Gold JM, Lahti AC, Queern CA, Conley RR, Bartko JJ, Kovnick J, Appelbaum PS. Decisional capacity for informed consent in schizophrenia research. Arch Gen Psychiatry. 2000;57:533–538. doi: 10.1001/archpsyc.57.6.533. [DOI] [PubMed] [Google Scholar]
- 18.Cimmino MA, Ferrone C, Cutolo M. Epidemiology of chronic musculoskeletal pain. Best Pract Res Clin Rheumatol. 2011;25:173–183. doi: 10.1016/j.berh.2010.01.012. [DOI] [PubMed] [Google Scholar]
- 19.Conte M, Broder HL, Jenkins G, Reed R, Janal MN. Oral health, related behaviors and oral health impacts among homeless adults. J Public Health Dent. 2006;66:276–278. doi: 10.1111/j.1752-7325.2006.tb04082.x. [DOI] [PubMed] [Google Scholar]
- 20.Culhane DP, Gollub E, Kuhn R, Shpaner M. The co-occurrence of AIDS and homelessness: results from the integration of administrative databases for AIDS surveillance and public shelter utilisation in Philadelphia. J Epidemiol Community Health. 2001;55:515–520. doi: 10.1136/jech.55.7.515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Culhane DP, Metraux S, Byrne T, Stino M, Bainbridge J. The Age Structure of Contemporary Homelessness: Evidence and Implications For Public Policy. Analyses of Social Issues and Public Policy. 2013;13:228–244. [Google Scholar]
- 22.Davis DA, Luecken LJ, Zautra AJ. Are reports of childhood abuse related to the experience of chronic pain in adulthood? A meta-analytic review of the literature. Clin J Pain. 2005;21:398–405. doi: 10.1097/01.ajp.0000149795.08746.31. [DOI] [PubMed] [Google Scholar]
- 23.Dawson DA, Grant BF, Stinson FS, Zhou Y. Effectiveness of the derived Alcohol Use Disorders Identification Test (AUDIT-C) in screening for alcohol use disorders and risk drinking in the US general population. Alcohol Clin Exp Res. 2005;29:844–854. doi: 10.1097/01.alc.0000164374.32229.a2. [DOI] [PubMed] [Google Scholar]
- 24.Drager D, Budnick A, Kuhnert R, Kalinowski S, Konner F, Kreutz R. Pain management intervention targeting nursing staff and general practitioners: Pain intensity, consequences and clinical relevance for nursing home residents. Geriatr Gerontol Int. 2016 Dec 9; doi: 10.1111/ggi.12924. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 25.Edlund MJ, Martin BC, Devries A, Fan MY, Braden JB, Sullivan MD. Trends in use of opioids for chronic noncancer pain among individuals with mental health and substance use disorders: the TROUP study. Clin J Pain. 2010;26:1–8. doi: 10.1097/AJP.0b013e3181b99f35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Elliott AM, Smith BH, Penny KI, Smith WC, Chambers WA. The epidemiology of chronic pain in the community. Lancet. 1999;354:1248–1252. doi: 10.1016/s0140-6736(99)03057-3. [DOI] [PubMed] [Google Scholar]
- 27.Fishbain DA, Pulikal A, Lewis JE, Gao J. Chronic Pain Types Differ in Their Reported Prevalence of Post-Traumatic Stress Disorder (PTSD) and There Is Consistent Evidence That Chronic Pain Is Associated with PTSD: An Evidence-Based Structured Systematic Review. Pain Med. 2016 May 17; doi: 10.1093/pm/pnw065. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 28.Fisher R, Ewing J, Garrett A, Harrison EK, Lwin KK, Wheeler DW. The nature and prevalence of chronic pain in homeless persons: an observational study. F1000Res. 2013;2:164. doi: 10.12688/f1000research.2-164.v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fransen M, McConnell S, Harmer AR, Van der Esch M, Simic M, Bennell KL. Exercise for osteoarthritis of the knee. Cochrane Database Syst Rev. 2015 doi: 10.1002/14651858.CD004376.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gaskin DJ, Richard P. The Economic Costs of Pain in the United States. J Pain. 2012;13:715–724. doi: 10.1016/j.jpain.2012.03.009. [DOI] [PubMed] [Google Scholar]
- 31.Gomez A, Conde A, Santana JM, Jorrin A, Serrano IM, Medina R. The diagnostic usefulness of AUDIT and AUDIT-C for detecting hazardous drinkers in the elderly. Aging Mental Health. 2006;10:558–561. doi: 10.1080/13607860600637729. [DOI] [PubMed] [Google Scholar]
- 32.Goodman L, Saxe L, Harvey M. Homelessness as psychological trauma. Broadening perspectives. Am Psychol. 1991;46:1219–1225. doi: 10.1037//0003-066x.46.11.1219. [DOI] [PubMed] [Google Scholar]
- 33.Green HD, Jr, Tucker JS, Wenzel SL, Golinelli D, Kennedy DP, Ryan GW, Zhou AJ. Association of childhood abuse with homeless women’s social networks. Child Abuse Negl. 2012;36:21–31. doi: 10.1016/j.chiabu.2011.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Guzman J, Esmail R, Karjalainen K, Malmivaara A, Irvin E, Bombardier C. Multidisciplinary rehabilitation for chronic low back pain: systematic review. BMJ. 2001;322:1511–1516. doi: 10.1136/bmj.322.7301.1511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hahn JA, Kushel MB, Bangsberg DR, Riley E, Moss AR. BRIEF REPORT: the aging of the homeless population: fourteen-year trends in San Francisco. J Gen Intern Med. 2006;21:775–778. doi: 10.1111/j.1525-1497.2006.00493.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Han B, Wells BL. Inappropriate emergency department visits and use of the Health Care for the Homeless Program services by Homeless adults in the northeastern United States. J Public Health Manag Pract. 2003;9:530–537. doi: 10.1097/00124784-200311000-00014. [DOI] [PubMed] [Google Scholar]
- 37.Hanley O, Miner J, Rockswold E, Biros M. The relationship between chronic illness, chronic pain, and socioeconomic factors in the ED. Am J Emerg Med. 2011;29:286–292. doi: 10.1016/j.ajem.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 38.Hardt J, Jacobsen C, Goldberg J, Nickel R, Buchwald D. Prevalence of chronic pain in a representative sample in the United States. Pain Med. 2008;9:803–812. doi: 10.1111/j.1526-4637.2008.00425.x. [DOI] [PubMed] [Google Scholar]
- 39.Heimer R, Zhan W, Grau LE. Prevalence and experience of chronic pain in suburban drug injectors. Drug Alcohol Depend. 2015;151:92–100. doi: 10.1016/j.drugalcdep.2015.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Henry-Edwards S, Monteiro MG, Humeniuk R, Ali R, Poznyak V. The Alcohol, Smoking and Substance involvement Screening Test (ASSIST): manual for use in primary care. Geneva: World Health Organization; 2010. [Google Scholar]
- 41.Henschke N, Ostelo RWJG, van Tulder MW, Vlaeyen JWS, Morley S, Assendelft WJJ, Main CJ. Behavioural treatment for chronic low-back pain. Cochrane Database Syst Rev. 2010 doi: 10.1002/14651858.CD002014.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Homeless E. Homeless Emergency Assistance and Rapid Transition to Housing: Defining “Homeless”. 24 CFR Parts 91, 582, and 283 [Docket No FR-5333-F-02] RIN 2506-AC26. 2010 [Google Scholar]
- 43.Housing and Urban Development. 2015 AHAR: Part 1 - PIT Estimates of Homelessness (508 Compliant Version) 2016:1–80. [Google Scholar]
- 44.Hwang SW, Tolomiczenko G, Kouyoumdjian FG, Garner RE. Interventions to improve the health of the homeless: a systematic review. Am J Prev Med. 2005;29:311–319. doi: 10.1016/j.amepre.2005.06.017. [DOI] [PubMed] [Google Scholar]
- 45.Hwang SW, Wilkins E, Chambers C, Estrabillo E, Berends J, MacDonald A. Chronic pain among homeless persons: characteristics, treatment, and barriers to management. BMC Fam Pract. 2011;12:73. doi: 10.1186/1471-2296-12-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Katz S. Assessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily living. J Am Geriatr Soc. 1983;31:721–727. doi: 10.1111/j.1532-5415.1983.tb03391.x. [DOI] [PubMed] [Google Scholar]
- 47.Kennedy J, Roll JM, Schraudner T, Murphy S, McPherson S. Prevalence of persistent pain in the U.S. adult population: new data from the 2010 national health interview survey. J Pain. 2014;15:979–984. doi: 10.1016/j.jpain.2014.05.009. [DOI] [PubMed] [Google Scholar]
- 48.Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- 49.Khan R, Chatton A, Thorens G, Achab S, Nallet A, Broers B, Calzada G, Poznyak V, Zullino D, Khazaal Y. Validation of the French version of the alcohol, smoking and substance involvement screening test (ASSIST) in the elderly. Subst Abuse Treat Prev Policy. 2012;7:14. doi: 10.1186/1747-597X-7-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kuehn BM. Prescription drug abuse rises globally. JAMA. 2007;297:1306. doi: 10.1001/jama.297.12.1306. [DOI] [PubMed] [Google Scholar]
- 51.Kushel MB, Evans JL, Perry S, Robertson MJ, Moss AR. No door to lock: victimization among homeless and marginally housed persons. Arch Intern Med. 2003;163:2492–2499. doi: 10.1001/archinte.163.20.2492. [DOI] [PubMed] [Google Scholar]
- 52.Kushel MB, Vittinghoff E, Haas JS. Factors associated with the health care utilization of homeless persons. JAMA. 2001;285:200–206. doi: 10.1001/jama.285.2.200. [DOI] [PubMed] [Google Scholar]
- 53.Lee CT, Guzman D, Ponath C, Tieu L, Riley E, Kushel M. Residential patterns in older homeless adults: Results of a cluster analysis. Soc Sci Med. 2016;153:131–140. doi: 10.1016/j.socscimed.2016.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Leveille SG, Jones RN, Kiely DK, Hausdorff JM, Shmerling RH, Guralnik JM, Kiel DP, Lipsitz LA, Bean JF. Chronic musculoskeletal pain and the occurrence of falls in an older population. JAMA. 2009;302:2214–2221. doi: 10.1001/jama.2009.1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lewinsohn PM, Seeley JR, Roberts RE, Allen NB. Center for Epidemiologic Studies Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychol Aging. 1997;12:277–287. doi: 10.1037//0882-7974.12.2.277. [DOI] [PubMed] [Google Scholar]
- 56.Lundin A, Hallgren M, Balliu N, Forsell Y. The use of alcohol use disorders identification test (AUDIT) in detecting alcohol use disorder and risk drinking in the general population: validation of AUDIT using schedules for clinical assessment in neuropsychiatry. Alcohol Clin Exp Res. 2015;39:158–165. doi: 10.1111/acer.12593. [DOI] [PubMed] [Google Scholar]
- 57.Manchikanti L, Singh A. Therapeutic opioids: a ten-year perspective on the complexities and complications of the escalating use, abuse, and nonmedical use of opioids. Pain Physician. 2008;11:S63–88. [PubMed] [Google Scholar]
- 58.Martens WH. A review of physical and mental health in homeless persons. Public Health Rev. 2001;29:13–33. [PubMed] [Google Scholar]
- 59.Martins DC, Gorman KS, Miller RJ, Murphy L, Sor S, Martins JC, Vecchiarelli ML. Assessment of Food Intake, Obesity, and Health Risk among the Homeless in Rhode Island. Public Health Nurs. 2015;32:453–461. doi: 10.1111/phn.12180. [DOI] [PubMed] [Google Scholar]
- 60.McCarthy LH, Bigal ME, Katz M, Derby C, Lipton RB. Chronic pain and obesity in elderly people: results from the Einstein aging study. J Am Geriatr Soc. 2009;57:115–119. doi: 10.1111/j.1532-5415.2008.02089.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, Pettinati H, Argeriou M. The Fifth Edition of the Addiction Severity Index. J Subst AbuseTreat. 1992;9:199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- 62.Miaskowski C, Penko JM, Guzman D, Mattson JE, Bangsberg DR, Kushel MB. Occurrence and characteristics of chronic pain in a community-based cohort of indigent adults living with HIV infection. J Pain. 2011;12:1004–1016. doi: 10.1016/j.jpain.2011.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mills S, Torrance N, Smith BH. Identification and Management of Chronic Pain in Primary Care: a Review. Curr Psychiatry Rep. 2016;18:22. doi: 10.1007/s11920-015-0659-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Nahin RL. Estimates of pain prevalence and severity in adults: United States, 2012. J Pain. 2015;16:769–780. doi: 10.1016/j.jpain.2015.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.North CS, Smith EM. Posttraumatic stress disorder among homeless men and women. Hosp Community Psychiatry. 1992;43:1010–1016. doi: 10.1176/ps.43.10.1010. [DOI] [PubMed] [Google Scholar]
- 66.Opening Doors: Federal Strategic Plan to Prevent and End Homelessness. United States Interagency Council on Homelessness; Washington, DC: 2015. [Google Scholar]
- 67.Ouimette P, Wade M, Prins A, Schohn M. Identifying PTSD in primary care: comparison of the Primary Care-PTSD screen (PC-PTSD) and the General Health Questionnaire-12 (GHQ) J Anxiety Disord. 2008;22:337–343. doi: 10.1016/j.janxdis.2007.02.010. [DOI] [PubMed] [Google Scholar]
- 68.Prins A, Ouimette P, Kimerling R, Cameron RP, Hugelshofer DS, Shaw-Hegwer J, Thrailkill A, Gusman FD, Sheikh JI. The primary care PTSD screen (PC-PTSD): development and operating characteristics. Prim Care Psychiatry. 2003;9:9–14. [Google Scholar]
- 69.Quadara A. State of knowledge paper, Australia’s National Research Organisation for Women’s Safety. Sydney, NSW, Australia: 2015. Implementing trauma-informed systems of care in health settings: The WITH study. [Google Scholar]
- 70.Rosenblum A, Marsch LA, Joseph H, Portenoy RK. Opioids and the treatment of chronic pain: controversies, current status, and future directions. Exp Clin Psychopharmacol. 2008;16:405–416. doi: 10.1037/a0013628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Rustøen T, Wahl AK, Hanestad BR, Lerdal A, Paul S, Miaskowski C. Age and the experience of chronic pain: differences in health and quality of life among younger, middle-aged, and older adults. Clin J Pain. 2005;21:513–523. doi: 10.1097/01.ajp.0000146217.31780.ef. [DOI] [PubMed] [Google Scholar]
- 72.SAMHSA’s Concept of Trauma and Guidance for a Trauma-Informed Approach. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2014. (Vol HHS Publication No. (SMA) 14-4884). [Google Scholar]
- 73.Scascighini L, Toma V, Dober-Spielmann S, Sprott H. Multidisciplinary treatment for chronic pain: a systematic review of interventions and outcomes. Rheumatology. 2008;47:670–678. doi: 10.1093/rheumatology/ken021. [DOI] [PubMed] [Google Scholar]
- 74.Schepker CA, Leveille SG, Pedersen MM, Ward RE, Kurlinski LA, Grande L, Kiely DK, Bean JF. Effect of Pain and Mild Cognitive Impairment on Mobility. J Am Geriatr Soc. 2016;64:138–143. doi: 10.1111/jgs.13869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sharp TJ, Harvey AG. Chronic pain and posttraumatic stress disorder: mutual maintenance? Clinical Psychology Review. 2001;21:857–877. doi: 10.1016/s0272-7358(00)00071-4. [DOI] [PubMed] [Google Scholar]
- 76.Sherman KB, Goldberg M, Bell KR. Traumatic Brain Injury and Pain. Phys Med Rehabil Clin N Am. 2006;17:473–490. doi: 10.1016/j.pmr.2005.11.007. [DOI] [PubMed] [Google Scholar]
- 77.Stringfellow EJ, Kim TW, Gordon AJ, Pollio DE, Grucza RA, Austin EL, Johnson NK, Kertesz SG. Substance use among persons with homeless experience in primary care. Subst Abus. 2016;37:534–541. doi: 10.1080/08897077.2016.1145616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sullivan G, Dumenci L, Burnam A, Koegel P. Validation of the brief instrumental functioning scale in a homeless population. Psychiatr Serv. 2001;52:1097–1099. doi: 10.1176/appi.ps.52.8.1097. [DOI] [PubMed] [Google Scholar]
- 79.Tam TW, Zlotnick C, Robertson MJ. Longitudinal perspective: adverse childhood events, substance use, and labor force participation among homeless adults. Am J Drug Alcohol Abuse. 2003;29:829–846. doi: 10.1081/ada-120026263. [DOI] [PubMed] [Google Scholar]
- 80.Taylor KM, Sharpe L. Trauma and post-traumatic stress disorder among homeless adults in Sydney. Aust N Z J psychiatry. 2008;42:206–213. doi: 10.1080/00048670701827218. [DOI] [PubMed] [Google Scholar]
- 81.Teno JM, Weitzen S, Wetle T, Mor V. Persistent pain in nursing home residents. JAMA. 2001;285:2081. doi: 10.1001/jama.285.16.2081-a. [DOI] [PubMed] [Google Scholar]
- 82.The expert consensus guideline series. Treatment of Posttraumatic Stress Disorder. The Expert Consensus Panels for PTSD. 1999:3–76. [PubMed] [Google Scholar]
- 83.Thurman DJ, Alverson C, Browne D, Dunn KA. Traumatic brain injury in the United States: A report to Congress. 1999 doi: 10.1097/00001199-199912000-00009. [DOI] [PubMed] [Google Scholar]
- 84.Torchalla I, Strehlau V, Li K, Aube Linden I, Noel F, Krausz M. Posttraumatic stress disorder and substance use disorder comorbidity in homeless adults: Prevalence, correlates, and sex differences. Psychol Addict Behav. 2014;28:443–452. doi: 10.1037/a0033674. [DOI] [PubMed] [Google Scholar]
- 85.Treede RD, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, Cohen M, Evers S, Finnerup NB, First MB, Giamberardino MA, Kaasa S, Kosek E, Lavand’homme P, Nicholas M, Perrot S, Scholz J, Schug S, Smith BH, Svensson P, Vlaeyen JW, Wang SJ. A classification of chronic pain for ICD-11. Pain. 2015;156:1003–1007. doi: 10.1097/j.pain.0000000000000160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Tsemberis S, McHugo G, Williams V, Hanrahan P, Stefancic A. Measuring homelessness and residential stability: The residential time-line follow-back inventory. J Commun Psychology. 2006;35:29–42. [Google Scholar]
- 87.Tyler KA, Beal MR. The high-risk environment of homeless young adults: consequences for physical and sexual victimization. Violence Vic. 2010;25:101–115. doi: 10.1891/0886-6708.25.1.101. [DOI] [PubMed] [Google Scholar]
- 88.United States Census. 2009;2010:1–6. [Google Scholar]
- 89.van Dam D, Ehring T, Vedel E, Emmelkamp PMG. Validation of the Primary Care Posttraumatic Stress Disorder screening questionnaire (PC-PTSD) in civilian substance use disorder patients. J Subst Abuse Treat. 2010;39:105–113. doi: 10.1016/j.jsat.2010.05.005. [DOI] [PubMed] [Google Scholar]
- 90.Verhaak PF, Kerssens JJ, Dekker J, Sorbi MJ, Bensing JM. Prevalence of chronic benign pain disorder among adults: a review of the literature. Pain. 1998;77:231–239. doi: 10.1016/S0304-3959(98)00117-1. [DOI] [PubMed] [Google Scholar]
- 91.Warshaw C, Sullivan CM, Rivera EA. A Systematic Review of Trauma-Focused Interventions for Domestic Violence Survivors. National Center on Domestic Violence, Trauma & Mental Health. 2013 [Google Scholar]
- 92.Weissman MM, Sholomskas D, Pottenger M, Prusoff BA, Locke BZ. Assessing depressive symptoms in five psychiatric populations: a validation study. Am J Epidemiol. 1977;106:203–214. doi: 10.1093/oxfordjournals.aje.a112455. [DOI] [PubMed] [Google Scholar]
- 93.Weitzman BC, Knickman JR, Shinn M. Predictors of shelter use among low-income families: psychiatric history, substance abuse, and victimization. Am J Public Health. 1992;82:1547–1550. doi: 10.2105/ajph.82.11.1547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.White BM, Jones WJ, Moran WP, Simpson KN. Effect of the Economic Recession on Primary Care Access for the Homeless. J Health Care Poor Underserved. 2016;27:1577–1591. doi: 10.1353/hpu.2016.0104. [DOI] [PubMed] [Google Scholar]
- 95.Won AB, Lapane KL, Vallow S, Schein J, Morris JN, Lipsitz LA. Persistent nonmalignant pain and analgesic prescribing patterns in elderly nursing home residents. J Am Geriatr Soc. 2004;52:867–874. doi: 10.1111/j.1532-5415.2004.52251.x. [DOI] [PubMed] [Google Scholar]
- 96.Wong YL. Measurement properties of the Center for Epidemiologic Studies-Depression Scale in a homeless population. Psychol Assess. 2000;12:69–76. doi: 10.1037//1040-3590.12.1.69. [DOI] [PubMed] [Google Scholar]
- 97.Zenz M, Strumpf M, Tryba M. Long-term oral opioid therapy in patients with chronic nonmalignant pain. J Pain Symptom Manage. 1992;7:69–77. doi: 10.1016/0885-3924(92)90116-y. [DOI] [PubMed] [Google Scholar]


