Abstract
Objectives
The main objectives of this study were to describe in-hospital acute respiratory compromise among children (age < 18 years), and its association with cardiac arrest and in-hospital mortality.
Design
Observational study using prospectively collected data.
Setting
United States hospitals reporting data to the Get With The Guidelines® – Resuscitation registry.
Patients
Pediatric patients (age < 18 years) with acute respiratory compromise. Acute respiratory compromise was defined as absent, agonal, or inadequate respiration that required emergency assisted ventilation and elicited a hospital-wide or unit-based emergency response.
Interventions
None.
Measurements and Main Results
The primary outcome was in-hospital mortality. Cardiac arrest during the event was a secondary outcome. To assess the association between patient, event, and hospital characteristics and the outcomes, we created multivariable logistic regressions models accounting for within-hospital clustering. One thousand nine hundred and fifty two patients from 151 hospitals were included. Forty percent of the events occurred on the wards, 19% in the emergency department, 25% in the intensive care unit, and 16% in other locations. Two hundred eighty patients (14.6%) died before hospital discharge. Pre-existing hypotension (odds ratio: 3.26 [95%CI: 1.89, 5.62], p < 0.001) and septicemia (odds ratio: 2.46 [95%CI: 1.52, 3.97], p < 0.001) were associated with increased mortality. The acute respiratory compromise event was temporally associated with a cardiac arrest in 182 patients (9.3%), among whom 46.2% died. One thousand two hundred and eight patients (62%) required tracheal intubation during the event. In-hospital mortality among patients requiring tracheal intubation during the event was 18.6%.
Conclusion
In this large, multicenter study of acute respiratory compromise, 40% occurred in ward settings, 9.3% had an associated cardiac arrest, and overall in-hospital mortality was 14.6%. Pre-event hypotension and septicemia were associated with increased mortality rate.
Keywords: Intubation, pulmonary ventilation, heart arrest, epidemiology, hospitals
INTRODUCTION
In-hospital acute respiratory failure requiring assisted ventilation occurs frequently in children irrespective of the criteria used to define this condition.(1–7) Even though mortality varies substantially depending on the definitions used(1, 2), mortality may exceed 40% in severe cases.(3, 4) Although there are no published incidence estimates for all pediatric patients, ICD-9-data from a study performed in 2000 estimates the annual incidence at greater than 5,000 cases each year in the United States in children between 5 and 17 years.(5, 8) However, this may represent a substantial underestimation of all pediatric in-hospital acute respiratory failure, because it is particularly common among younger patient groups.(1–4)
Pediatric intubation has been extensively described in the intensive care unit (ICU)(9–16) and emergency department (ED) setting.(17, 18) However, to our knowledge, no large, multi-center study has described the landscape of in-hospital acute respiratory compromise events, defined as absent, agonal, or inadequate respiration requiring emergency assisted ventilation and eliciting a hospital-wide or unit-based emergency response. Likewise, specific data are lacking on children experiencing acute respiratory compromise outside the ICU or ED setting, although these patients are often included, along with other deteriorating children, in studies of early warning scores and implementation of rapid response teams.(7, 19–24)
This study represents the first report from a large, multicenter, prospective United States registry reporting the epidemiology of pediatric in-hospital acute respiratory compromise across hospital locations for children of all ages. The main objectives were to describe in-hospital acute respiratory compromise events, and assess key patient, event and hospital factors associated with cardiac arrest and in-hospital mortality.
MATERIALS AND METHODS
Study design and data source
This was an observational study using prospectively collected data from the Get With The Guidelines® – Resuscitation (GWTG-R) registry.(25) Based in the United States and sponsored by the American Heart Association, the GWTG-R is a quality improvement database of in-hospital cardiac arrest, medical emergency team responses, and acute respiratory compromise events. The registry includes both pediatric and adult patients. Trained personnel at each participating hospital collected data on all of these events according to standard definitions (see below). Certification of data entry personnel and the use of standardized software further improved data integrity.(26, 27) Additional hospital descriptive data were obtained from the American Hospital Association’s Annual Survey Database 2013.(28)
All participating hospitals are required to comply with local regulatory guidelines. Because data are used primarily at the local site for quality improvement, sites are granted a waiver of informed consent under the common rule. The Committee on Clinical Investigations at Beth Israel Deaconess Medical Center, Boston, USA confirmed that this is not considered human subjects research under the common law and therefor waived the need for informed consent.
Population and outcomes
The GWTG-R registry defines “acute respiratory compromise” as absent, agonal, or inadequate respiration that requires emergency assisted ventilation and elicits a hospital-wide or unit-based emergency response. This includes non-invasive (e.g., mouth-to-mouth, mouth-to-barrier device, bag-valve-mask, continuous positive airway pressure, or bi-level positive airway pressure) and invasive (e.g., endotracheal or tracheostomy tube, laryngeal mask airway) positive pressure ventilation. Elective intubations and out-of-hospital events are not part of the database.
For this study, we included index events in pediatric patients (age < 18 years) from January 2005 to December 2014. Events were excluded if they occurred in visitors, in the delivery room, newborn nursery, or in neonatal intensive care unit. Patients were also excluded if they had an invasive airway in place or received assisted ventilation immediately prior to the hospital-wide or unit-based emergency response activation. Finally, we excluded events if outcome data was missing, specifically data on cardiac arrest or in-hospital mortality.
The primary outcome was in-hospital mortality. Cardiac arrest during the acute respiratory compromise event was a secondary outcome.
Statistical analyses
We used descriptive statistics to summarize the study population. Survivors and non-survivors were first compared using unadjusted logistic regression. For categorical variables with more than two categories, the category with the largest sample size was chosen as the reference group. Next, we created a multivariable logistic regression model. We used generalized estimation equations with an exchangeable variance-covariance structure to account for correlation among patients within the same hospital. To avoid overfitting, we only included variables in the multivariable model that were different between survivors and non-survivors at a p-value < 0.10 in unadjusted analysis. We then performed backwards selection removing variables one-by-one according to the highest p-value until all variables were associated with the outcome at a p-value < 0.05. In the main multivariable analysis, we only included patients with no missing data.
We considered the following variables for entry into the model (see Table 1 for additional details): age, sex, illness category, pre-existing conditions (see eTable 1 in the supplemental material for definitions), location, time (time of day, day of week, year), whether the event was monitored (ECG, apnea monitor, apnea/bradycardia monitor, and/or pulse oximetry), whether a hospital-wide response was activated (as compared to a unit-wide response), the presence of vascular access, supplemental oxygen at the time of the event, the electrocardiographic rhythm, the breathing pattern and the patient’s consciousness at the beginning of the event. We also included hospital-level variables: type of hospital, number of beds, and teaching status. All variables were chosen a priori by the author team. We repeated the analysis for the secondary outcome cardiac arrest during the event. Results from the multivariable models are presented as odds ratios (OR) with 95% confidence intervals (95%CI). A predefined subgroup analysis was conducted in those who underwent tracheal intubation during the event.
Table 1.
| Characteristics | Main cohortc (n = 1952) | Cohort with imputed valuesd (n = 1952) |
|---|---|---|
| Demographics | ||
| Age | ||
| Neonate (< 1 month) | 470 (24) | 470 (24) |
| Infant (1 month up to 1 year) | 469 (24) | 469 (24) |
| Child (1 year to 12 year) | 712 (36) | 712 (36) |
| Adolescent (> 12 years) | 301 (15) | 301 (15) |
| Sex | ||
| Male | 1070 (55) | 1070 (55) |
| female | 882 (45) | 882 (45) |
| Illness category | ||
| Medical cardiac | 164 (8) | 164 (8) |
| Medical non-cardiac | 1096 (56) | 1101 (56) |
| Surgical cardiac | 136 (7) | 136 (7) |
| Surgical non-cardiace | 330 (17) | 332 (17) |
| Newbornf | 219 (11) | 219 (11) |
| Pre-existing conditionsg | ||
| Cyanotic cardiac malformation | 124 (7) | 146 (7) |
| Acyanotic cardiac malformation | 86 (5) | 96 (5) |
| Non-cardiac congenital malformation | 215 (13) | 236 (12) |
| CHF this admission | 54 (3) | 61 (3) |
| Hypotension | 112 (7) | 128 (7) |
| Acute stroke | 13 (1) | 18 (1) |
| Acute non-stroke neurological event | 244 (14) | 276 (14) |
| Pneumonia | 142 (8) | 157 (8) |
| Septicemia | 126 (7) | 146 (7) |
| Major trauma | 111 (7) | 121 (6) |
| None of the above | 721 (42) | 845 (43) |
| Location of the event | ||
| Emergency department | 368 (19) | 368 (19) |
| Floor with telemetry/step-down unit | 134 (7) | 134 (7) |
| Floor without telemetry | 653 (33) | 653 (33) |
| Intensive care unit | 493 (25) | 493 (25) |
| OR/PACU/procedural area | 175 (9) | 175 (9) |
| Other | 129 (7) | 129 (7) |
| Time of the event | ||
| Year | ||
| 2005 – 2006 | 430 (22) | 430 (22) |
| 2007 – 2008 | 339 (17) | 339 (17) |
| 2009 – 2010 | 473 (24) | 473 (24) |
| 2011 – 2012 | 403 (21) | 403 (21) |
| 2013 – 2014 | 307 (16) | 307 (16) |
| Time of week | ||
| Weekday (Monday – Friday) | 1461 (76) | 1461 (76) |
| Weekend (Saturday – Sunday) | 435 (24) | 435 (24) |
| Time of day | ||
| Day (7:00 am – 10:59 pm) | 1410 (76) | 1489 (76) |
| Night (11:00 pm – 6:59 am) | 435 (24) | 463 (24) |
| Event characteristics | ||
| Monitored | 1562 (80) | 1563 (80) |
| Hospital wide response activated | 1057 (54) | 1057 (54) |
| Vascular access in place | 1396 (72) | 1396 (72) |
| Supplemental oxygen in place | 922 (52) | 1018 (52) |
| Rhythm at start of event | ||
| Bradycardia | 298 (21) | 436 (22) |
| Sinus (including sinus tachycardia) | 1065 (76) | 1467 (75) |
| Other | 34 (2) | 50 (3) |
| Breathing pattern | ||
| Breathing | 1125 (61) | 1186 (61) |
| Not breathing | 481 (26) | 517 (26) |
| Agonal | 233 (13) | 250 (13) |
| Patient conscious | 993 (63) | 1225 (63) |
| Hospital characteristics | ||
| Hospital type | ||
| Primarily adult | 991 (52) | 1004 (51) |
| Primarily pediatric | 930 (48) | 948 (49) |
| Number of beds | ||
| < 250 | 206 (11) | 208 (11) |
| 250 – 499 | 1046 (54) | 1064 (54) |
| ≥ 500 | 669 (35) | 680 (35) |
| Teaching status | ||
| Non-teaching | 183 (10) | 184 (9) |
| Minor teaching | 418 (22) | 425 (22) |
| Major teaching | 1318 (67) | 1342 (69) |
CHF denotes chronic heart failure, OR operating room, PACU post-anesthesia care unit
All variables are reported as counts (frequencies)
Percentages indicate relative frequencies with non-missing values as the denominator
Values reflect “averaged” values over the 10 imputed data sets
Includes trauma and obstetric patients
I.e. being born on the current admission
See eTable 1 in the supplemental material for definitions
To account for missing data for included variables, we performed multiple imputations as a sensitivity analysis for the primary outcome in-hospital mortality. Missing values were imputed using the fully conditional specification method.(29) A total of 10 data sets were created. Analyses were then repeated taking into account the imputation.
All hypothesis tests were two-sided with a significance level of p < 0.05. No adjustments were made for multiple comparisons; therefore nominal significant p-values should be interpreted with caution. We conducted all statistical analyses with SAS software, version 9.4 (SAS Institute, Cary, NC, USA).
RESULTS
Patient inclusion, missing data, and characteristics
Four thousand five hundred and sixty pediatric acute respiratory compromise events were entered in the GWTG-R registry between January 2005 and December 2014 although the majority of hospitals reported cases for a shorter time period. For the current study, 1952 patients from 151 hospitals met all inclusion criteria and no exclusion criteria (Figure 1). Data was complete for all variables on 905 patients (46%) and 1657 patients (85%) had missing data on two or less variables. The median number of missing values was 1 (quartiles: 0, 1). Additional details on data missingness are provided in the eTable 2 (supplemental material).
Figure 1. Patient inclusion/exclusion.
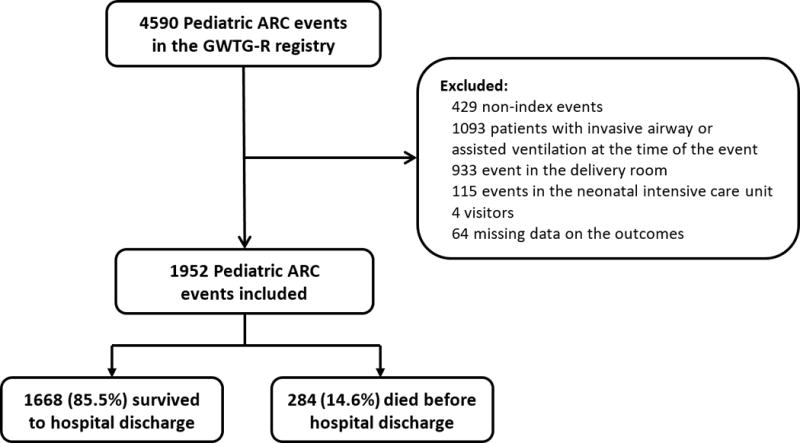
Of 4590 acute respiratory compromise (ARC) events in the registry, 1952 were included in this study. 284 (14.6%) died before hospital discharge.
Patient, event, and hospital characteristics are provided in Table 1 for both the non-imputed and imputed cohort. All age groups were represented and 45% were female. Forty percent of the events occurred on the wards, 19% in the emergency department, 25% in the intensive care unit, and 16% in other locations. Eighty percent of patients were monitored at the time of the acute respiratory compromise events; 76% with pulse oximetry, 67% with ECG, 14% with apnea monitor, and 20% with apnea/bradycardia monitor. The most common illness category was medical non-cardiac (56%) and the most common pre-existing conditions were non-cardiac congenital malformations (13%), acute non-stroke neurological events (14%), and pneumonia (8%). The majority of patients were spontaneously breathing (61%) and had a sinus rhythm (76%) at the beginning of the event. Patients were included from both primarily adult (51%) and pediatric (49%) hospitals with the majority of the hospitals being major teaching hospitals (69%). For 537 patients (28%) the event ended with unassisted return of spontaneous ventilation (i.e. spontaneous ventilation sustained for > 20 minutes).
Documented interventions during the acute respiratory compromise event are provided in Table 2. One thousand seven hundred and ten patients (88%) received bag-valve mask ventilation during the event, 1208 patients (62%) had tracheal intubations, and 288 patients (15%) received continuous or bi-level positive airway pressure ventilation. Other ventilation interventions were uncommon. The most common pharmacological interventions were administration of sedation/anesthetic agents (46%), neuromuscular blockade (34%), and an intravenous fluid bolus (22%).
Table 2.
| Characteristics | All patients (n = 1951) |
|---|---|
| Type of ventilation | |
| Bag-valve mask | 1710 (88) |
| Endotracheal tube | 1208 (62) |
| CPAP/BiPAP | 288 (15) |
| Other non-invasive ventilation | 46 (2) |
| Tracheostomy | 18 (1) |
| Laryngeal mask | 11 (1) |
| Mouth to barrier device | 9 (0) |
| Mouth to mouth | 3 (0) |
| Drugs given | |
| Sedation/Induction | 906 (46) |
| Neuromuscular blockade | 664 (34) |
| Intravenous fluid bolus | 432 (22) |
| Sodium bicarbonate | 101 (5) |
| Reversal agent | 83 (4) |
| Calcium chloride/gluconate | 49 (3) |
| Dextrose | 29 (1) |
| Bronchodilator | 18 (1) |
| Magnesium sulfate | 12 (1) |
| Prostaglandins | 4 (0) |
| Other | 517 (27) |
| None | 613 (31) |
Data was missing on one person. Variables were collected as “yes” vs. “no/not documented”
CPAP: continuous positive airway pressure, BiPAP: biphasic positive airway pressure
In-hospital mortality
Overall, 284 patients (14.6% [95%CI: 13.0%, 16.2%]) died before hospital discharge. Mortality according to year is presented in Figure 2 and according to location in eTable 3 (supplemental material). Patient, event, and hospital characteristics according to mortality is provided in Table 3 for the non-imputed cohort and in eTable 4 (supplemental material) for the imputed cohort.
Figure 2. Outcomes over time.
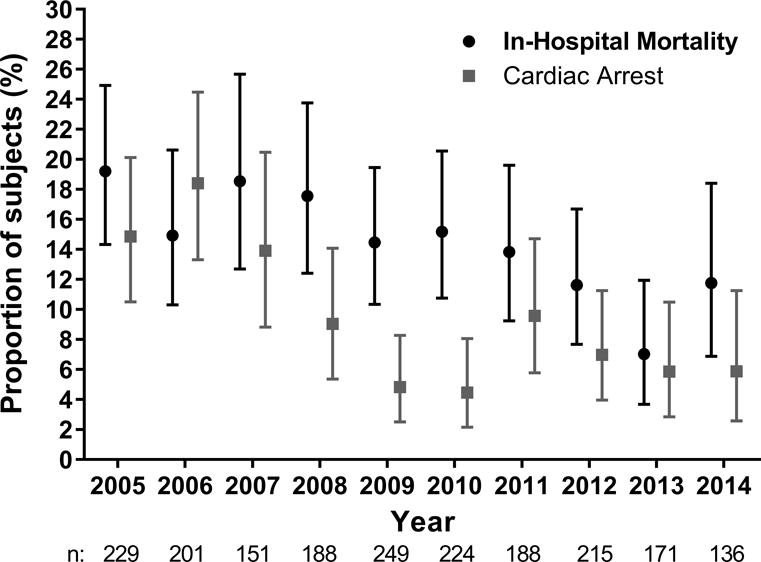
Proportion of patients dying (black circles) and progressing to cardiac arrest (grey squares) according to the year of the event. Error bars represent exact 95% confidence intervals. There was a significant unadjusted decreased in in-hospital mortality over time (OR per year 0.92 [95%CI: 0.88, 0.96]) that remained significant in multivariable analysis in the non-imputed cohort but not in the imputed cohort.
Table 3.
Unadjusted comparison between survivors and non-survivorsa
| Characteristics | Non-survivorsb (n = 284) | Survivorsb (n = 1668) | Odds ratioc (95%CI) | p-value |
|---|---|---|---|---|
| Demographics | ||||
| Age | ||||
| Neonate (< 1 month) | 56 (20) | 414 (25) | 0.91 (0.64, 1.30) | 0.61 |
| Infant (1 month up to 1 year) | 79 (28) | 390 (23) | 1.37 (0.99, 1.89) | 0.06 |
| Child (1 year to 12 year) | 92 (32) | 620 (37) | Reference | – |
| Adolescent (> 12 years) | 57 (20) | 244 (15) | 1.57 (1.10, 2.26) | 0.01 |
| Sex | ||||
| Male | 144 (51) | 926 (56) | Reference | – |
| female | 140 (49) | 742 (44) | 1.21 (0.94, 1.56) | 0.13 |
| Illness category | ||||
| Medical cardiac | 47 (17) | 117 (7) | 2.57 (1.76, 3.76) | < 0.001 |
| Medical non-cardiac | 148 (52) | 948 (57) | Reference | – |
| Surgical cardiac | 27 (10) | 109 (7) | 1.59 (1.01, 2.50) | 0.05 |
| Surgical non-cardiac | 35 (12) | 295 (18) | 0.76 (0.51, 1.12) | 0.17 |
| Newborn | 26 (9) | 193 (12) | 0.86 (0.55, 1.35) | 0.52 |
| Pre-existing conditions | ||||
| Cyanotic cardiac malformation | 31 (13) | 93 (6) | 2.21 (1.44, 3.41) | < 0.001 |
| Acyanotic cardiac malformation | 15 (6) | 71 (5) | 1.32 (0.75, 2.35) | 0.34 |
| Non-cardiac congenital malformation | 34 (14) | 181 (12) | 1.18 (0.80, 1.76) | 0.40 |
| CHF this admission | 13 (5) | 41 (3) | 2.01 (1.06, 3.81) | 0.03 |
| Hypotension | 46 (19) | 66 (5) | 5.09 (3.39, 7.63) | < 0.001 |
| Acute stroke | 1 (0) | 12 (1) | 0.51 (0.07, 3.95) | 0.52 |
| Acute non-stroke neurological event | 24 (10) | 220 (15) | 0.64 (0.41, 0.99) | 0.05 |
| Pneumonia | 23 (10) | 119 (8) | 1.21 (0.76, 1.94) | 0.42 |
| Septicemia | 38 (16) | 88 (6) | 2.98 (1.98, 4.48) | < 0.001 |
| Major trauma | 13 (5) | 98 (7) | 0.81 (0.45, 1.46) | 0.48 |
| None of the above | 66 (28) | 655 (45) | 0.48 (0.35, 0.64) | < 0.001 |
| Location of the event | ||||
| Emergency department | 44 (15) | 324 (19) | 1.10 (0.74, 1.63) | 0.65 |
| Floor with telemetry/step-down unit | 19 (7) | 115 (7) | 1.33 (0.77, 2.30) | 0.30 |
| Floor without telemetry | 72 (25) | 581 (35) | Reference | – |
| Intensive care unit | 117 (41) | 376 (23) | 2.51 (1.82, 3.46) | < 0.001 |
| OR/PACU/procedural area | 14 (5) | 161 (10) | 0.70 (0.39, 1.28) | 0.25 |
| Other | 18 (6) | 11 (7) | 1.31 (0.75, 2.28) | 0.34 |
| Time of the event | ||||
| Year | 0.92d (0.88, 0.96) | < 0.001 | ||
| 2005 – 2006 | 74 (26) | 356 (21) | ||
| 2007 – 2008 | 61 (21) | 278 (17) | ||
| 2009 – 2010 | 70 (25) | 403 (24) | ||
| 2011 – 2012 | 51 (18) | 352 (21) | ||
| 2013 – 2014 | 28 (10) | 279 (17) | ||
| Time of week | ||||
| Weekday (Monday – Friday) | 220 (77) | 1241 (74) | Reference | – |
| Weekend (Saturday – Sunday) | 64 (23) | 427 (26) | 0.85 (0.63, 1.14) | 0.27 |
| Time of day | ||||
| Day (7:00am – 10:59 pm) | 192 (72) | 1218 (77) | Reference | – |
| Night (11pm – 6:59am) | 75 (28) | 360 (23) | 1.32 (0.99, 1.77) | 0.06 |
| Event characteristics | ||||
| Monitored | 241 (85) | 1321 (79) | 1.46 (1.03, 2.06) | 0.03 |
| Hospital wide response activated | 121 (43) | 936 (56) | 0.58 (0.45, 0.75) | < 0.001 |
| Vascular access in place | 214 (75) | 1182 (71) | 1.25 (0.94, 1.67) | 0.13 |
| Supplemental oxygen in place | 163 (63) | 759 (51) | 1.64 (1.25, 2.15) | < 0.001 |
| Rhythm at start of event | ||||
| Bradycardia | 64 (29) | 234 (20) | 1.70 (1.22, 2.35) | 0.002 |
| Sinus (including sinus tachycardia) | 148 (67) | 917 (78) | Reference | – |
| Other | 9 (4) | 25 (2) | 2.23 (1.02, 4.87) | 0.04 |
| Breathing pattern | ||||
| Breathing | 148 (57) | 977 (62) | Reference | – |
| Not breathing | 65 (25) | 416 (26) | 1.03 (0.75, 1.41) | 0.85 |
| Agonal | 47 (18) | 186 (12) | 1.67 (1.16, 2.40) | 0.006 |
| Patient conscious | 131 (57) | 862 (64) | 0.76 (0.57, 1.01) | 0.06 |
| Hospital characteristics | ||||
| Hospital type | ||||
| Primarily adult | 139 (50) | 852 (52) | Reference | – |
| Primarily pediatric | 138 (50) | 791 (48) | 1.08 (0.84, 1.39) | 0.57 |
| Number of beds | ||||
| < 250 | 15 (5) | 191 (12) | 0.48 (0.27, 0.83) | 0.009 |
| 250 – 499 | 148 (53) | 898 (55) | Reference | – |
| ≥ 500 | 115 (41) | 554 (34) | 1.26 (0.97, 1.64) | 0.09 |
| Teaching status | ||||
| Non-teaching | 12 (4) | 171 (10) | 0.35(0.19, 0.65) | < 0.001 |
| Minor teaching | 47 (17) | 371 (23) | 0.64 (0.46, 0.90) | 0.009 |
| Major teaching | 218 (79) | 1100 (67) | Reference | – |
CHF denotes chronic heart failure, OR operating room, PACU post-anesthesia care unit
All variables are reported as counts (frequencies)
Odds ratio for in-hospital mortality
Odds ratio per year
The results from the multivariable model for in-hospital mortality are presented in Table 4 for both the non-imputed and imputed cohort. The results were largely similar in the two cohorts. Compared to a medical non-cardiac illness category, a medical cardiac illness category was associated with increased mortality (OR: 2.86 [95%CI: 1.73, 4.71]). Pre-existing hypotension (OR: 3.26 [95%CI: 1.89, 5.62]) and septicemia (OR: 2.46 [95%CI: 1.52, 3.97]) were strongly associated with increased mortality. Events at non-teaching (OR: 0.28 [95%CI: 0.12, 0.65]) and minor teaching hospitals (OR: 0.43 [95%CI: 0.20, 0.90]) were associated with decreased mortality as compared to major teaching hospitals.
Table 4.
Multivariable model for mortality
| Non-imputed cohort (n = 905) | Imputed cohort (n = 1952) | |||
|---|---|---|---|---|
| Characteristics | Odds ratio (95%CI) | p-value | Odds ratio (95%CI) | p-value |
| Illness category | ||||
| Medical cardiac | 2.86 (1.73, 4.71) | < 0.001 | 2.20 (1.47, 3.30) | < 0.001 |
| Medical non-cardiac | Reference | – | Reference | – |
| Surgical cardiac | 1.68 (0.90, 3.15) | 0.11 | 1.23 (0.83, 1.81) | 0.30 |
| Surgical non-cardiac | 0.69 (0.37, 1.28) | 0.24 | 0.78 (0.52, 1.17) | 0.23 |
| Newborn | 1.43 (0.67, 3.07) | 0.35 | 1.15 (0.61, 2.16) | 0.67 |
| Pre-existing conditions | ||||
| Hypotension | 3.26 (1.89, 5.62) | < 0.001 | 3.92 (2.73, 5.63) | < 0.001 |
| Septicemia | 2.46 (1.52, 3.97) | < 0.001 | 2.53 (1.61, 3.98) | < 0.001 |
| Time of the event | ||||
| Year per year | 0.92 (0.85, 1.00) | 0.04 | – | – |
| Event characteristics | ||||
| Monitored | 0.51 (0.30, 0.87) | 0.01 | – | – |
| Hospital wide response activated | 0.42 (0.27,0.67) | < 0.001 | 0.63 (0.43, 0.92) | 0.02 |
| Supplemental oxygen in place | 1.93 (1.14, 3.27) | 0.01 | 1.57 (1.14, 2.17) | 0.006 |
| Breathing pattern | ||||
| Breathing | Reference | – | Reference | – |
| Not breathing | 1.59 (0.99, 2.54) | 0.05 | 1.43 (1.01, 2.02) | 0.04 |
| Agonal | 2.94 (1.67, 5.18) | < 0.001 | 2.05 (1.26, 3.34) | 0.004 |
| Hospital characteristics | ||||
| Teaching status | ||||
| Non-teaching | 0.28 (0.12, 0.65) | 0.003 | 0.30 (0.15, 0.59) | < 0.001 |
| Minor teaching | 0.43 (0.20, 0.90) | 0.03 | 0.57 (0.36, 0.92) | 0.02 |
| Major teaching | Reference | – | Reference | – |
Cardiac arrest during the event
The acute respiratory compromise event was temporally associated with a cardiac arrest in 182 patients (9.3% [95%CI: 8.1%, 10.7%]). For these patients, the in-hospital mortality was 46.2% (95%CI: 38.8%, 53.7%) compared to 11.3% (95%CI: 9.9%, 12.9%) in those without an acute respiratory compromise-associated cardiac arrest (p < 0.001). The proportion of patients with a cardiac arrest during the event per year is provided in Figure 2 and according to location in eTable 3 (supplemental material). The median time to cardiac arrest from the beginning of the event was 7 minutes (quartiles: 3, 16), see eFigure 1 in the supplemental material. This information was missing on 9% of the patients.
The results of the univariate analyses regarding cardiac arrest during the event are presented in eTable 5 (supplemental material) and the results of the multivariable analysis are presented in Table 5. Neonates and patients with an acute non-stroke neurological event had decreased odds of cardiac arrest during the event. Having an event on an inpatient floor, compared to an ICU, ED or other location was also associated with decreased odds of cardiac arrest.
Table 5.
Multivariable model for cardiac arrest (n = 905)
| Characteristics | Odds ratio (95%CI) | p-value |
|---|---|---|
| Demographics | ||
| Age | ||
| Neonate (< 1 month) | 0.36 (0.16, 0.82) | 0.01 |
| Infant (1 month up to 1 year) | 0.99 (0.60, 1.65) | 0.98 |
| Child (1 year to 12 year) | Reference | – |
| Adolescent (> 12 years) | 0.73 (0.33, 1.63) | 0.44 |
| Pre-existing conditions | ||
| Acute non-stroke neurological event | 0.41 (0.18, 0.92) | 0.03 |
| Location of the event | ||
| Emergency department | 6.31 (2.21, 18.0) | < 0.001 |
| Floor with telemetry/step-down unit | 0.87 (0.17, 4.39) | 0.86 |
| Floor without telemetry | Reference | – |
| Intensive care unit | 4.93 (2.02, 12.1) | < 0.001 |
| OR/PACU/procedural area | 7.19 (2.08, 24.9) | 0.002 |
| Other | 3.06 (0.85, 11.1) | 0.09 |
| Event characteristics | ||
| Rhythm at start of event | ||
| Bradycardia | 3.05 (1.69, 5.48) | < 0.001 |
| Sinus (including sinus tachycardia) | Reference | – |
| Other | 1.30 (0.25, 6.88) | 0.76 |
| Breathing pattern | ||
| Breathing | Reference | – |
| Not breathing | 2.43 (1.28, 4.63) | 0.007 |
| Agonal | 2.73 (1.15, 6.45) | 0.02 |
| Hospital characteristics | ||
| Teaching status | ||
| Non-teaching | 0.16 (0.03, 0.78) | 0.02 |
| Minor teaching | 0.75 (0.34, 1.69) | 0.49 |
| Major teaching | Reference | – |
Intubated subgroup
One thousand two hundred and eight patients (62%) required tracheal intubation during the event. In-hospital mortality in this patient population was 18.6% (95%CI: 16.5%, 20.9%). One hundred thirty four of these 1208 patients (11.1% [95%CI: 9.4%, 13.0%]) had a cardiac arrest and these patients had an overall in-hospital mortality of 51.5% (95%CI: 39.8%, 57.3%). Characteristics according to mortality is presented in eTable 6 (supplemental material) and the results of the multivariable model are presented in eTable 7 (supplemental material). The results in this subgroup were largely similar to the full cohort. Medical cardiac illness category, pre-existing hypotension, and septicemia were strongly associated with increased mortality.
DISCUSSION
In this multicenter study of children having an acute respiratory compromise event that required emergency assisted ventilation and elicited a hospital-wide or unit-based emergency response, we found an overall mortality of approximately 15%. Forty percent occurred in a ward setting, 28% had unassisted return of spontaneous ventilation during the event, and 9% had an acute respiratory compromise-associated cardiac arrest. Patients with cardiac arrests had a much higher mortality rate of 46%. Medical cardiac illness category, pre-existing hypotension and septicemia were patient characteristics consistently and strongly associated with increased mortality, even when other potentially confounding patient, event and hospital factors were accounted for.
Among these 1951 children with acute respiratory compromise events, 28% of the events ended with unassisted return of spontaneous ventilation. Presumably, some of these events were due to acute reversible neurologic events (e.g., seizures, responses to medications) and some were due to reversible obstructive and/or central apnea. In contrast, 88% were treated with bag-valve-mask ventilation, 62% had tracheal intubations, and 15% received continuous or bi-level positive airway pressure ventilation.
The National Emergency Airway Registry for Children (“NEAR4KIDS”) has provided valuable information on the occurrence of adverse events from emergent and non-emergent tracheal intubation in the ICU setting.(9–16) In the pediatric ICU setting, severe adverse events occurred in approximately 6% of cases and less than 2% of patients progressed to cardiac arrest during the event.(11, 14) Similar, or slightly higher, cardiac arrest event rates have been described in the ED for pediatric(18) and adult(30, 31) patients in relation to emergency intubation. These estimates are lower than the 9.3% reported here. However, there are important differences in the included patient population that limits direct comparison. Specifically, the inclusion criteria for the acute respiratory compromise GWTG-R registry includes activation of a unit- or hospital-wide response during the event likely selecting a more acutely ill patient population for inclusion. The ICU mortality from the NEAR4KIDS registry is approximately 12%(12), which is more aligned with the in-hospital mortality rate of 15% we report here.
A number of patient characteristics were consistently associated with mortality in the primary analysis, the sensitivity analysis accounting for missing data, and in the subgroup of patients who received tracheal intubation during the event: medical cardiac illness category, pre-existing hypotension, and septicemia. The fact that hemodynamic instability (i.e. hypotension and septicemia) was associated with increased mortality is perhaps expected yet important. Nishisaki et al., using the NEAR4KIDS registry, found that a diagnostic category of sepsis/shock and unstable hemodynamics prior to the event were associated with increased risk of severe adverse events.(11) In adults, pre-event hemodynamic instability has been associated with cardiac arrest and/or in-hospital mortality in a number of studies in the ED, ICU, and on inpatient wards.(27, 31–33) Furthermore, hemodynamic instability is a predictor of mortality in pediatric patients with acute respiratory failure receiving mechanical ventilation.(2) Whether hemodynamic optimization before/during airway management could lead to improved outcomes remains to be determined. We also found that hospital characteristics such as non-teaching and minor teaching hospitals were associated with decreased mortality in the multivariable model. Although the reasons for these findings are unknown, we speculate that patients in major teaching hospitals are different and might constitute a generally sicker patient population.
A previous study from the GWTG-R registry found that survival has increased over the last decade for in-hospital pediatric cardiac arrest.(34) In the current study, we found a similar significant trend with decreasing mortality from 2005 (19%) to 2014 (12%) after acute respiratory compromise. This remained significant in multivariable analysis indicating that the decrease in mortality cannot be explained by temporal changes in patient characteristics as captured in the GWTG-R registry. This finding did not remain significant in our imputed cohort and should therefore be interpreted with caution. However, whether this potential decrease in mortality is driven by improved acute management of the acute respiratory compromise event, by better intensive care management after the event, by changes in uncaptured patient characteristics, or by something else remains to be determined. Notably, we did not find a decrease over time in the number of events progressing to cardiac arrest in multivariable analysis, perhaps indicating that any changes in mortality (if true) are driven more by post-event care.
This study should be interpreted in the context of the study design and a number of limitations. Although the GWTG-R encourages inclusion of all events meeting all inclusion criteria and none of the exclusion criteria, we cannot guarantee that all eligible events are captured. As such, a selection bias might underestimate the actual incidence of acute respiratory compromise, but overestimate the incidence of acute respiratory compromise-associated cardiac arrest and mortality. Our analysis of outcomes over time is limited by the fact that hospitals participated in the registry for varying time periods. The sample size did not allow us to examine trends over time within individual hospitals. While the overall proportion of missing data was relatively low (median 1 [quartiles: 0, 1] out of 30 variables included), the proportion of missing data on a few specific variables (e.g., the rhythm at start of event and the level of consciousness) were relatively high. We tried to account for this by multiple imputation and these analyses gave largely similar results and conclusions. While this was a large multicenter study, the number of events was relatively low especially for the secondary outcome of cardiac arrest; therefore the multivariable model for this outcome should be interpreted with caution. Lastly, we were limited by the data and the data definitions included in the GWTG-R registry. For example, the definition of “septicemia” in the current study is different from prior and current definitions of sepsis. We were also unable to determine the specific cause of some of the pre-existing conditions such as “acute non-stroke neurological event” and the reasons for choice of ventilation or drugs given.
CONCLUSION
This is the first study from the GWTG-R registry describing acute respiratory compromise (i.e. absent, agonal, or inadequate respiration that requires emergency assisted ventilation) and elicits a hospital-wide or unit-based emergency response. We found that 40% occurred in ward settings, 28% had unassisted return of spontaneous ventilation during the event, and 9.3% progressed to cardiac arrest with a median time to cardiac arrest of 7 minutes. In-hospital mortality was 14.6%. Several patient and acute respiratory compromise event characteristics were consistently associated with mortality even after accounting for other potentially confounding patient, event, and hospital factors: an unmonitored event, medical cardiac illness category, pre-existing hypotension, and septicemia.
Supplementary Material
Acknowledgments
The authors would like to thank Francesca Montillo M.M. Emergency Department, Beth Israel Deaconess Medical Center, Boston, MA, USA for editorial assistance.
Funding:
This study was not funded.
Copyright form disclosure: Dr. Topijan received support for article research from the National Institutes of Health (NIH), and her institution received funding from the NIH. Dr. Donnino received support for article research from the NIH; he received funding from NIH K24 mentoring award; and he and his institution received funding from the American Heart Association for consulting.
Footnotes
No reprints will be ordered.
Financial Disclosure:
The authors have no financial relationships relevant to this article to disclose.
Conflicts of interest:
The authors have no conflicts of interest relevant to this article to disclose.
The remaining authors have disclosed that they do not have any potential conflicts of interest.
References
- 1.Randolph AG, Meert KL, O’Neil ME, et al. The feasibility of conducting clinical trials in infants and children with acute respiratory failure. Am J Respir Crit Care Med. 2003;167(10):1334–1340. doi: 10.1164/rccm.200210-1175OC. [DOI] [PubMed] [Google Scholar]
- 2.Leclerc F, Duhamel A, Deken V, et al. Nonrespiratory pediatric logistic organ dysfunction-2 score is a good predictor of mortality in children with acute respiratory failure. Pediatr Crit Care Med. 2014;15(7):590–593. doi: 10.1097/PCC.0000000000000184. [DOI] [PubMed] [Google Scholar]
- 3.Rivera RA, Butt W, Shann F. Predictors of mortality in children with respiratory failure: possible indications for ECMO. Anaesth Intensive Care. 1990;18(3):385–389. doi: 10.1177/0310057X9001800316. [DOI] [PubMed] [Google Scholar]
- 4.Timmons OD, Havens PL, Fackler JC. Predicting death in pediatric patients with acute respiratory failure. Pediatric Critical Care Study Group. Extracorporeal Life Support Organization. Chest. 1995;108(3):789–797. doi: 10.1378/chest.108.3.789. [DOI] [PubMed] [Google Scholar]
- 5.Behrendt CE. Acute respiratory failure in the United States: incidence and 31-day survival. Chest. 2000;118(4):1100–1105. doi: 10.1378/chest.118.4.1100. [DOI] [PubMed] [Google Scholar]
- 6.Karande S, Murkey R, Ahuja S, et al. Clinical profile and outcome of acute respiratory failure. Indian J Pediatr. 2003;70(11):865–869. doi: 10.1007/BF02730586. [DOI] [PubMed] [Google Scholar]
- 7.Raymond TT, Bonafide CP, Praestgaard A, et al. Pediatric Medical Emergency Team Events and Outcomes: A Report of 3647 Events From the American Heart Association’s Get With the Guidelines-Resuscitation Registry. Hosp Pediatr. 2016;6(2):57–64. doi: 10.1542/hpeds.2015-0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.United States Census Bureau. American Fact Finder. 2014 [cited 2016 1/12] Available from: https://www.census.gov/popest/data/national/asrh/2014/index.html.
- 9.Nishisaki A, Ferry S, Colborn S, et al. Characterization of tracheal intubation process of care and safety outcomes in a tertiary pediatric intensive care unit. Pediatr Crit Care Med. 2012;13(1):e5–10. doi: 10.1097/PCC.0b013e3181fe472d. [DOI] [PubMed] [Google Scholar]
- 10.Sanders RC, Jr, Giuliano JS, Jr, Sullivan JE, et al. Level of trainee and tracheal intubation outcomes. Pediatrics. 2013;131(3):e821–828. doi: 10.1542/peds.2012-2127. [DOI] [PubMed] [Google Scholar]
- 11.Nishisaki A, Turner DA, Brown CA, 3rd, et al. A National Emergency Airway Registry for children: landscape of tracheal intubation in 15 PICUs. Crit Care Med. 2013;41(3):874–885. doi: 10.1097/CCM.0b013e3182746736. [DOI] [PubMed] [Google Scholar]
- 12.Graciano AL, Tamburro R, Thompson AE, et al. Incidence and associated factors of difficult tracheal intubations in pediatric ICUs: a report from National Emergency Airway Registry for Children: NEAR4KIDS. Intensive Care Med. 2014;40(11):1659–1669. doi: 10.1007/s00134-014-3407-4. [DOI] [PubMed] [Google Scholar]
- 13.Nett S, Emeriaud G, Jarvis JD, et al. Site-level variance for adverse tracheal intubation-associated events across 15 North American PICUs: a report from the national emergency airway registry for children*. Pediatr Crit Care Med. 2014;15(4):306–313. doi: 10.1097/PCC.0000000000000120. [DOI] [PubMed] [Google Scholar]
- 14.Tarquinio KM, Howell JD, Montgomery V, et al. Current medication practice and tracheal intubation safety outcomes from a prospective multicenter observational cohort study. Pediatr Crit Care Med. 2015;16(3):210–218. doi: 10.1097/PCC.0000000000000319. [DOI] [PubMed] [Google Scholar]
- 15.Rehder KJ, Giuliano JS, Jr, Napolitano N, et al. Increased Occurrence of Tracheal Intubation-Associated Events During Nights and Weekends in the PICU. Crit Care Med. 2015;43(12):2668–2674. doi: 10.1097/CCM.0000000000001313. [DOI] [PubMed] [Google Scholar]
- 16.Sanders RC, Jr, Nett ST, Davis KF, et al. Family Presence During Pediatric Tracheal Intubations. JAMA Pediatr. 2016;170(3):e154627. doi: 10.1001/jamapediatrics.2015.4627. [DOI] [PubMed] [Google Scholar]
- 17.Sagarin MJ, Chiang V, Sakles JC, et al. Rapid sequence intubation for pediatric emergency airway management. Pediatr Emerg Care. 2002;18(6):417–423. doi: 10.1097/00006565-200212000-00004. [DOI] [PubMed] [Google Scholar]
- 18.Pallin DJ, Dwyer RC, Walls RM, et al. Techniques and Trends, Success Rates, and Adverse Events in Emergency Department Pediatric Intubations: A Report From the National Emergency Airway Registry. Ann Emerg Med. 2016 doi: 10.1016/j.annemergmed.2015.12.006. [DOI] [PubMed] [Google Scholar]
- 19.Brilli RJ, Gibson R, Luria JW, et al. Implementation of a medical emergency team in a large pediatric teaching hospital prevents respiratory and cardiopulmonary arrests outside the intensive care unit. Pediatr Crit Care Med. 2007;8(3):236–246. doi: 10.1097/01.PCC.0000262947.72442.EA. quiz 247. [DOI] [PubMed] [Google Scholar]
- 20.Parshuram CS, Duncan HP, Joffe AR, et al. Multicentre validation of the bedside paediatric early warning system score: a severity of illness score to detect evolving critical illness in hospitalised children. Crit Care. 2011;15(4):R184. doi: 10.1186/cc10337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Parshuram CS, Hutchison J, Middaugh K. Development and initial validation of the Bedside Paediatric Early Warning System score. Crit Care. 2009;13(4):R135. doi: 10.1186/cc7998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Duncan H, Hutchison J, Parshuram CS. The Pediatric Early Warning System score: a severity of illness score to predict urgent medical need in hospitalized children. J Crit Care. 2006;21(3):271–278. doi: 10.1016/j.jcrc.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 23.Bonafide CP, Holmes JH, Nadkarni VM, et al. Development of a score to predict clinical deterioration in hospitalized children. J Hosp Med. 2012;7(4):345–349. doi: 10.1002/jhm.971. [DOI] [PubMed] [Google Scholar]
- 24.Bonafide CP, Localio AR, Roberts KE, et al. Impact of rapid response system implementation on critical deterioration events in children. JAMA Pediatr. 2014;168(1):25–33. doi: 10.1001/jamapediatrics.2013.3266. [DOI] [PubMed] [Google Scholar]
- 25.The American Heart Association. Get With The Guidelines Resuscitation web page. 2016 [cited 2016 1/11] Available from: http://www.heart.org/HEARTORG/HealthcareResearch/GetWithTheGuidelines/GetWithTheGuidelines-Resuscitation/Get-With-The-Guidelines-Resuscitation_UCM_314496_SubHomePage.jsp.
- 26.Peberdy MA, Kaye W, Ornato JP, et al. Cardiopulmonary resuscitation of adults in the hospital: a report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58(3):297–308. doi: 10.1016/s0300-9572(03)00215-6. [DOI] [PubMed] [Google Scholar]
- 27.Wang HE, Abella BS, Callaway CW, et al. Risk of cardiopulmonary arrest after acute respiratory compromise in hospitalized patients. Resuscitation. 2008;79(2):234–240. doi: 10.1016/j.resuscitation.2008.06.025. [DOI] [PubMed] [Google Scholar]
- 28.The American Hospital Association. AHA Annual Survey Database™ Fiscal Year 2013 web page. 2014 [cited 2016 1/11] Available from: http://www.ahadataviewer.com/book-cd-products/aha-survey/
- 29.van Buuren S. Multiple imputation of discrete and continuous data by fully conditional specification. Stat Methods Med Res. 2007;16(3):219–242. doi: 10.1177/0962280206074463. [DOI] [PubMed] [Google Scholar]
- 30.Heffner AC, Swords DS, Neale MN, et al. Incidence and factors associated with cardiac arrest complicating emergency airway management. Resuscitation. 2013;84(11):1500–1504. doi: 10.1016/j.resuscitation.2013.07.022. [DOI] [PubMed] [Google Scholar]
- 31.Kim WY, Kwak MK, Ko BS, et al. Factors associated with the occurrence of cardiac arrest after emergency tracheal intubation in the emergency department. PLoS One. 2014;9(11):e112779. doi: 10.1371/journal.pone.0112779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Andersen LW, Berg K, Chase M, et al. Acute Respiratory Compromise on Inpatient Wards in the United States: Incidence, Outcomes, and Factors Associated with In-Hospital Mortality. Resuscitation. 2016;105:123–129. doi: 10.1016/j.resuscitation.2016.05.014. [DOI] [PubMed] [Google Scholar]
- 33.Jaber S, Amraoui J, Lefrant JY, et al. Clinical practice and risk factors for immediate complications of endotracheal intubation in the intensive care unit: a prospective, multiple-center study. Crit Care Med. 2006;34(9):2355–2361. doi: 10.1097/01.CCM.0000233879.58720.87. [DOI] [PubMed] [Google Scholar]
- 34.Girotra S, Spertus JA, Li Y, et al. Survival trends in pediatric in-hospital cardiac arrests: an analysis from Get With the Guidelines-Resuscitation. Circ Cardiovasc Qual Outcomes. 2013;6(1):42–49. doi: 10.1161/CIRCOUTCOMES.112.967968. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


