Abstract
Surgical repair for large rotator cuff tear remains challenging due to tear size, altered muscle mechanical properties, and poor musculotendinous extensibility. Insufficient extensibility might lead to an incomplete reconstruction; moreover, excessive stresses after repair may result in repair failure without healing. Therefore, estimates of extensibility of cuff muscles can help in pre-surgical planning to prevent unexpected scenarios during surgery. The purpose of this study was to determine if quantified mechanical properties of the supraspinatus muscle using shear wave elastography (SWE) could be used to predict the extensibility of the musculotendionous unit on cadaveric specimens. Forty-five fresh-frozen cadaveric shoulders (25 intact and 20 with rotator cuff tear) were used for the study. Passive stiffness of 4 anatomical regions in the supraspinatus muscle was first measured using SWE. After detaching the distal edge of supraspinatus muscle from other cuff muscles, the detached muscle was axially pulled with the scapula fixed. The correlation between the SWE modulus and the extensibility of the muscle under 30 and 60 N loads was assessed. There was a significant negative correlation between SWE measurements and the experimental extensibility. SWE modulus for the anterior-deep region in the supraspinatus muscle showed the strongest correlation with extensibility under 30 N (r = 0.70, P < 0.001) and 60 N (r = 0.68, P < 0.001). Quantitative SWE assessment for the supraspinatus muscle was highly correlated with extensibility of musculotendinous unit on cadaveric shoulders. This technique may be used to predict the extensibility for rotator cuff tears for pre-surgical planning.
Keywords: Shear wave elastography, Rotator cuff tear, Supraspinatus muscle, Extensibility
INTRODUCTION
A rotator cuff tear is the most common cause of shoulder pain and disability of shoulder function, especially in the middle-aged and elderly population (Minagawa et al., 2013; Moosmayer et al., 2009; Tempelhof et al., 1999). Patients who failed conservative treatment may require surgery in order to restore shoulder function and/or to reduce pain (Caldwell et al., 1997; Gazielly et al., 1994; Harryman et al., 1991). Surgical options for rotator cuff tears are highly individualized, including debridement alone, direct repair of smaller defects, partial repair, augmentation with a patch or tendon transfer to cover the defect, or shoulder arthroplasty (Bedi et al., 2010).
As notable characteristics, a detached rotator cuff tendon can retract over time, increasing the size of the initial tear (Safran et al., 2011). Moreover, it may change cuff muscles properties. With a deteriorated length-tension relationship of the musculotendinous structure, intrinsic changes in muscle quality, fatty infiltration, and/or degeneration may occur, resulting in a decrease in extensibility and an increase in stiffness (Hersche and Gerber, 1998; Meyer et al., 2006; Safran et al., 2005). Consequently, large passive tensile loads are required to bring torn tendons onto the footprint region for repair (Berth et al., 2010; Ward et al., 2006). The subsequent excessive tensile stresses on the repaired tendon-bone structure, combined with abnormal tissue properties with poor extensibility, may cause repair failure with gap formation in the repair site, as reported in 17–57% of re-tear cases (Bartl et al., 2012; Iannotti et al.; Zumstein et al., 2008).
In the clinical setting, individualized assessment of biomechanical parameters for extensibility of rotator cuff structures, as well as morphological parameters are necessary to assist in pre-surgical planning and monitoring recovery throughout the rehabilitation process. Computed tomography (CT), magnetic resonance imaging (MRI) and ultrasound imaging techniques have been utilized for rotator cuff assessment in the past; however, mainly to assess gross muscle and tear size, and/or the presence/absence and extent of fatty infiltration (Bedi et al., 2010; Maman et al., 2009; Meyer et al., 2006; Yamaguchi et al., 2001). In this study, we aimed to develop a non-invasive tool to acquire the rotator cuff muscles’ extensibility for pre-surgical planning thus improving treatment outcome. To achieve this goal, we adopted a novel ultrasound technique, shear wave elastography (SWE). SWE can provide quantitative in-vivo measurements of soft tissue elasticity, or stiffness, by measuring shear wave propagation speed, which is inherently related to the elastic modulus (Garra, 2007). The technique is fast, convenient and applicable to a variety of clinical scenarios in which other approaches would potentially be inadequate; thus, it has been used successfully for breast cancers diagnosis (Athanasiou et al., 2010) and liver fibrosis staging (Ferraioli et al., 2014). In addition, quantitative assessments of the mechanical properties of skeletal muscles have also been investigated in in-vivo and in-vitro studies (Akagi et al., 2015; Hatta et al., 2016a; Hirata et al., 2015; Hug et al., 2013).
Therefore, this ultrasound technique to quantify the mechanical properties of skeletal muscles structures may be used to predict the extensibility of the supraspinatus muscle. We hypothesized that the mechanical properties, measured by SWE, of the supraspinatus muscle could be correlated to the extensibility of the supraspinatus musculotendinous unit.
MATERIALS AND METHODS
Specimen Preparation
Forty-five fresh-frozen human cadaveric shoulders were harvested from 45 subjects after institutional review board approval from our institution. Twenty-four right shoulders and 21 left shoulders were used for this study. The specimens were kept frozen at −20°C until testing and thawed overnight at room temperature before the experiment. After disarticulating the scapula from the thorax and cutting the humerus at the level of the midshaft, the scapula and a fiberglass rod inserted into the humeral medullary canal were both secured in a custom-designed experimental device, as previously described (Hatta et al., 2015). Based on the International Society of Biomechanics (ISB) recommendation, the scapula was fixed at 0° of upward/downward rotation considered as a neutral position (Schwartz et al., 2014; Wu et al., 2005). All soft tissues including skin, subcutaneous fat, and muscles within the cut level were kept intact during this process.
Supraspinatus Muscle Passive Stiffness Measurements
Passive stiffness of the supraspinatus (SSP) muscle was assessed using a commercial ultrasound system (Aixplorer; Supersonic Imagine Ltd., Aix-en-Provence, France) with a linear array transducer (2–10 MHz; Supersonic Imagine, Ltd.). Mechanical properties of the SSP muscle were obtained using a built-in-software and measured in kilopascal (kPa). Placement of the ultrasound transducer and measurement regions of the SSP muscle had been established in previous studies (Hatta et al., 2015; Itoigawa et al., 2015). Briefly, the SSP muscle was divided into 4 regions according to the muscle fiber orientation; anterior deep (AD), anterior superficial (AS), posterior deep (PD), and posterior superficial (PS). SWE measurements for each region were assessed independently on the plane parallel to the muscle fibers (Fig. 1). Regions of interest (ROI), represented by circular areas including the whole thickness of each muscle region, were used to obtain quantitative SWE moduli. To minimize technical variation due to probe positioning or probe pressure, SWE measurement values were obtained repeatedly 9 times based on a previous study (Hatta et al., 2015). Mean SWE values were then calculated for each region.
Fig. 1.
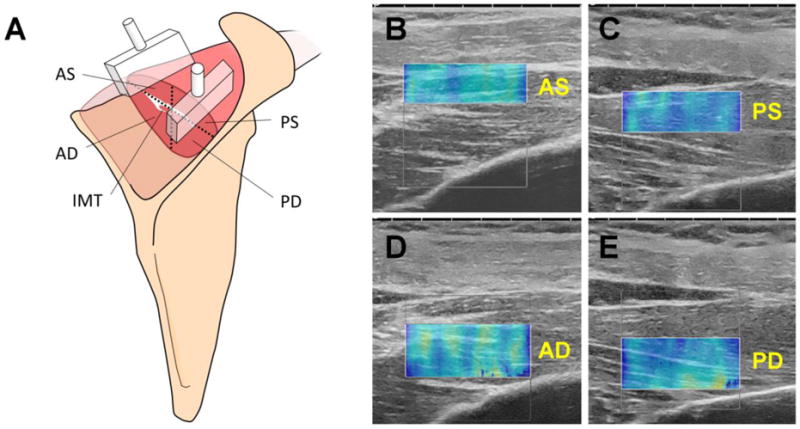
Quadrisected regions of the supraspinatus muscle for SWE measurements. A) Scheme of the placement of the ultrasound probe for the 4 muscular regions. SWE images for B) anterior-superficial (AS), C) posterior-superficial (PS), D) anterior-deep (AD), and E) posterior-deep (PD) muscular regions. IMT; intra-muscular tendon.
Musculotendinous Unit Extensibility Measurement
After SWE measurements were obtained, a 10cm incision was made parallel to the lateral border of the acromion. The deltoid muscle was detached from the acromion to observe the rotator cuff tendon. The presence/absence of a rotator cuff tear and its size (width and length) were recorded. The specimens were then divided into two groups based on the presence or absence of a cuff tear. The size of the tear was classified into small, medium, large, or massive, according to the classification established by Post et al. (Post et al., 1983). Load and muscle displacement data were used to measure extensibility at 30N and 60N in mm. Extensibility was considered as the measured displacement, or deformation, of the musculotendinous unit with the applied loads (Giambini et al., 2017). To assess the extensibility of SSP musculotendinous unit, the distal edge of the supraspinatus tendon was cut in specimens with intact cuff or small tears. This process was not required in specimens presenting medium size or large tears, since the distal edge of the tendon was already detached from the greater tuberosity. After removing all the soft tissues and acromion, the shoulders were placed in a custom-designed experimental device which allowed axial deformation of the SSP muscle and load/displacement recordings (Fig. 2). The scapulae were rigidly fixed to the fixture and the SSP muscles were pulled by suturing the tendon edge of the musculotendinous junction to a load cell. A linear potentiometer was attached to measure displacements. The muscles were axially pulled first to 30N and then 60N using a pneumatic system for three cycles each. The first cycle at each load was used to precondition the muscles and data from the two additional cycles were analyzed. Displacement data were obtained from both cycles at each load to determine the mean extensibility values. Experimental stiffness was evaluated from the linear region of the force/displacement curve.
Fig. 2.
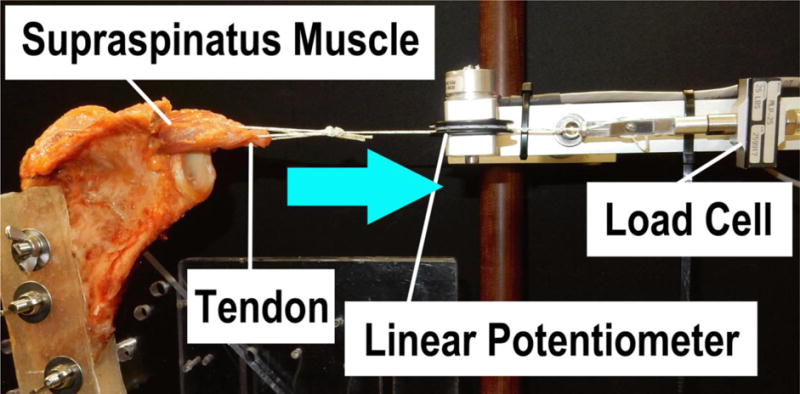
Custom-designed device used for the assessment of extensibility.
Statistical Analysis
Pearson correlation coefficient analysis and simple regression analysis were used to determine the correlation between SWE stiffness from each muscular region of the SSP muscle, and the extensibility and stiffness outcomes obtained experimentally. ICC (2,1) was used to determine the reproducibility of the extensibility data from the 2nd and 3rd cycles which followed the preconditioning of the muscle. The significance level was set to p < 0.05.
RESULTS
The specimens consisted of 25 intact shoulders and 20 shoulders with rotator cuff tears. The tear group included 6 small, 5 medium, 5 large and 4 massive tears based on a tear size classification system. Stiffness outcomes from SWE were successfully obtained in all 4 muscular regions. Experimental data was obtained for all shoulder when pulled to 30N. However, 4 specimens (1 intact and 3 from the tear group) ruptured at the muscle belly during the 60N load test. Therefore, extensibility under 60N loads was analyzed for a total of 41 specimens. Extensibility outcomes between the 2nd and 3rd cycles from these 41 specimens were reproducible and showed good correlations (30N: 0.889, 95% confidence interval [CI], 0.797–0.941; 60N: 0.847, 95% CI, 0.710–0.923).
There was a significant negative correlation between muscle stiffness measured with SWE for all regions and muscle extensibility under both 30N and 60N loads (Fig. 3A and 3B, respectively). Particularly, SWE stiffness on the anterior deep (AD) region of the SSP muscle showed the highest negative correlation with extensibility under 30N (r = 0.70, P < 0.001) and 60N (r = 0.68, P < 0.001). SWE stiffness showed a moderate significant positive correlation with experimental stiffness of the supraspinatus muscle (r = 0.57–0.63, P < 0.001 for all regions, Fig. 4). This positive correlation was observed on all muscular regions.
Fig. 3.
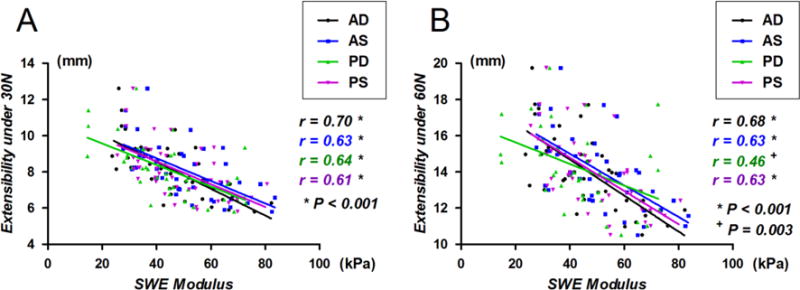
SWE moduli obtained from the 4 muscular regions of the supraspinatus muscle vs. extensibility under A) 30N and B) 60N loads.
Fig. 4.
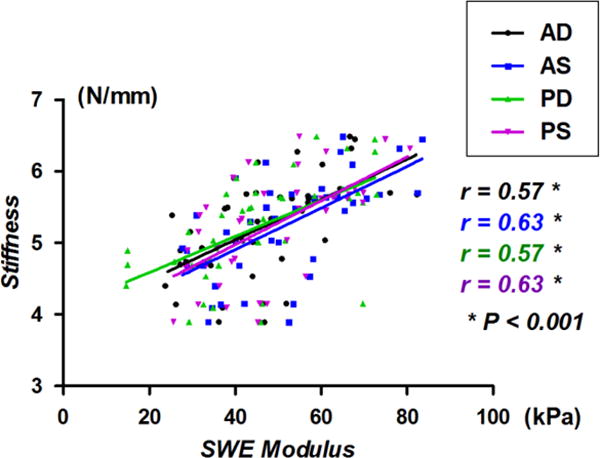
SWE moduli obtained from 4 muscular regions of supraspinatus muscle vs. stiffness.
Individual analysis of intact and tear shoulders showed similar outcomes, with the anterior deep (AD) compartment presenting the highest correlation between SWE stiffness and extensibility when compared among all 4 muscular regions (Table 1). Linear regression plots of the AD region for both the intact and tear shoulder specimens are shown in Fig. 5. SWE stiffness measurements at 30N and 60N loads negatively correlated with extensibility (Fig. 5A: 30N: r(intact) = 0.71, r(tear) = 0.77; Fig. 5B: 30N: r(intact) = 0.72, r(tear) = 0.78).
Table 1.
Correlation analysis summary of ultrasound SWE moduli and extensibility outcomes for the intact and tear shoulder specimens under 30N and 60N loads.
| Extensibility under 30 N loads | Intact (N = 25) Correlation |
P values | Tear (N = 20) Correlation |
P values |
|---|---|---|---|---|
| AD | r = 0.71 | < 0.001 | r = 0.77 | < 0.001 |
| AS | r = 0.64 | < 0.001 | r = 0.67 | 0.001 |
| PD | r = 0.60 | 0.002 | r = 0.67 | 0.001 |
| PS | r = 0.55 | 0.005 | r = 0.66 | 0.002 |
| Extensibility under 60 N loads | Intact (N = 24) Correlation |
P values | Tear (N = 17) Correlation |
P values |
|---|---|---|---|---|
| AD | r = 0.72 | < 0.001 | r = 0.78 | < 0.001 |
| AS | r = 0.67 | < 0.001 | r = 0.71 | 0.002 |
| PD | r = 0.68 | < 0.001 | r = 0.68 | 0.004 |
| PS | r = 0.62 | 0.001 | r = 0.68 | 0.004 |
Fig. 5.
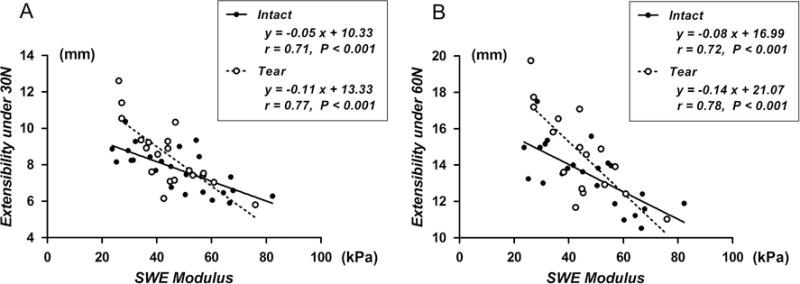
SWE moduli for the anterior-deep (AD) region vs. extensibility under A) 30N and B) 60N loads.
DISCUSSION
The current in-vitro study established a novel, non-invasive ultrasound technique to predict the biomechanically-measured extensibility of a rotator cuff muscle. We showed a significant correlation between the extensibility and ultrasound shear wave elastography (SWE) stiffness measurements of the supraspinatus muscle. Using the techniques described in this study, SWE could offer a non-invasive method to predict rotator cuff extensibility during the preoperative planning phase for a rotator cuff repair. Future applications for SWE in the clinic in the setting of rotator cuff repairs may include patient-specific determination of optimal treatment modality based on the predictive extensibility of a torn rotator cuff. In addition to the current qualitative assessment of tear size, preoperative knowledge of quantitative extensibility outcomes might predefine whether the torn edge of the cuff could be successfully pulled and repaired onto its original insertion, or a partial defect would still remain after repair. Additionally, in patients in which the estimated extensibility is poor, patch augmentation, tendon transfer, or shoulder arthroplasty could be considered preoperatively.
SWE has been previously used to quantify the mechanical properties of various soft tissues. Eby et al. (Eby et al., 2013) reported that the SWE modulus obtained from the swine brachialis muscle was significantly related to the Young’s modulus of the muscle during axial loading. Because the skeletal muscle may be considered transversely isotropic with its longitudinal axis (Morrow et al., 2010), with the probe aligned longitudinally with the underlying muscle fibers, the shear modulus can be estimated from the ultrasound shear wave speed (Eby et al., 2013). Based on this concept and on the supraspinatus muscles’ fiber orientation, a methodology using SWE has been reliably and feasibly established to quantify the mechanical properties, such as the passive stiffness (Hatta et al.; Itoigawa et al., 2015). Therefore, we have assessed whether SWE could be used to predict the extensibility of the supraspinatus muscle.
SWE stiffness outcomes of the anterior-deep muscular region yielded a stronger correlation with the extensibility of the supraspinatus musculotendinous unit compared to the other muscular compartments. Anatomical studies have shown that the anterior muscle region is approximately 2.5 times larger in its physiological cross-sectional area than the posterior muscle regions (Roh et al., 2000). Moreover, studies have demonstrated that the tensile stress of the supraspinatus muscle was highly correlated to its anatomical cross-sectional area (Gerber et al., 2007). Based on these and the outcomes of the current study, therefore, the anterior musculotendinous region, encompassing the largest volume within the supraspinatus muscle, could be responsible for the overall muscle stiffness and the resistance to muscle extensibility, compared to the posterior region. The supraspinatus muscle consists of multidirectional circum-pennated muscle fiber structures, not only in the antero-posterior regions but also in the deep-superficial directions (Itoigawa et al., 2015; Kim et al., 2013). Results from the current study indicate that the extensibility of the retracted supraspinatus muscle into the humeral insertion may depend on the biomechanical characteristics of specific muscle regions, such as the antero-deep region, rather than the whole-muscle. Consequently, localized muscle properties of the anterior-deep region could be assessed to determine and predict the extensibility in patients with longitudinally retracted rotator cuff tears.
In this study, we found a significant correlation between the SWE modulus on the anterior-deep (AD) region and the experimentally-measured extensibility in specimens with intact and torn rotator cuff tendons. SWE outcomes in specimens with rotator cuff tears reflected the extensibility of the detached SSP muscle. On the other hand, in the intact specimens, the tendons had to be artificially detached from the footprint. This pathological and potentially chronic deterioration of the mechanical properties in the muscles with rotator cuff tear, compared to the artificial detachment of the tendon edge in intact specimens, might have led to the differences observed in the slopes of the regression lines between these two groups. Therefore, SWE could potentially be more sensitive to predictions of extensibility in shoulders with chronic rotator cuff tear than acute pathologies.
The current study has several limitations. First, SWE moduli for the supraspinatus muscles were obtained from cadaveric shoulders. It is important to note that fresh-frozen shoulders might present a different muscular response to elongation in comparison with in-vivo subjects. Four of the specimens ruptured at the muscle belly during the 60N load. Although this load has been previously implemented as a safe limit to avoid damaging the tendon or the muscle (Meyer et al., 2006), the four specimens might have potentially presented with an underlying disease or disuse, that might have eventually affected their mechanical properties. However, there was no information available from the specimens that could confirm any abnormal condition. Additionally, we should note that the applied load was not prescribed, rather, manually ramped using the pneumatic system. This manual loading could have potentially induced micro-architectural deterioration, such as in the sarcomeres, leading to muscle failure.
The sample size used in this study was small, especially when considering the tear samples and the variability in tears. This small sample size prevented us from obtaining stiffness values according to their tear classification, and compare those outcomes to intact shoulder specimens. Nevertheless, using this methodology, future studies should investigate the material properties of the supraspinatus muscle including more samples in each tear classification, but more importantly in in-vivo subjects, defining definitive SWE patterns for predicting the extensibility. In addition, the existence of fatty infiltration was not evaluated. Further studies should investigate the relationship between muscle quality, such as stiffness and fatty infiltration, and the biomechanical characteristics of the muscle. The current study focused on the feasibility of SWE to quantitatively measure the mechanical properties of the SSP muscle and predict extensibility. However, SSP muscle thickness and/or cross-sectional area were not measured. Further studies should include these anatomical properties and evaluate their effect in muscle extensibility and SWE moduli. Finally, we exclusively evaluated the supraspinatus musculotendinous unit. If a torn tendon is repaired via the margin convergence technique (Burkhart et al., 1996; Hatta et al., 2016b) or partial repair technique (Bedi et al., 2010) especially in patients with massive rotator cuff tears, the extensibility of the infraspinatus musculotendinous unit may become equally important. An evaluation of the effectiveness of this technique on the infraspinatus muscle is also required and should be further evaluated.
CONCLUSION
In conclusion, our results demonstrated a quantitative assessment of the material properties of the supraspinatus muscle using SWE, and showed that these properties were highly correlated to the extensibility of the detached supraspinatus musculotendinous unit. Particularly, SWE measurements of the anterior-deep muscular region might be more prone to predicting the extensibility for patients with rotator cuff tears.
Acknowledgments
Research reported in this publication was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health under Award Number R21 AR065550. The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest statement
The authors confirm that there is no potential conflict of interest, including employment, consultancies, stock ownership, honoraria and paid expert testimony and patent applications, influencing this work.
References
- Akagi R, Yamashita Y, Ueyasu Y. Age-Related Differences in Muscle Shear Moduli in the Lower Extremity. Ultrasound Med Biol. 2015;41:2906–2912. doi: 10.1016/j.ultrasmedbio.2015.07.011. [DOI] [PubMed] [Google Scholar]
- Athanasiou A, Tardivon A, Tanter M, Sigal-Zafrani B, Bercoff J, Deffieux T, Gennisson JL, Fink M, Neuenschwander S. Breast lesions: quantitative elastography with supersonic shear imaging–preliminary results. Radiology. 2010;256:297–303. doi: 10.1148/radiol.10090385. [DOI] [PubMed] [Google Scholar]
- Bartl C, Kouloumentas P, Holzapfel K, Eichhorn S, Wortler K, Imhoff A, Salzmann GM. Long-term outcome and structural integrity following open repair of massive rotator cuff tears. Int J Shoulder Surg. 2012;6:1–8. doi: 10.4103/0973-6042.94304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bedi A, Dines J, Warren RF, Dines DM. Massive tears of the rotator cuff. J Bone Joint Surg Am. 2010;92:1894–1908. doi: 10.2106/JBJS.I.01531. [DOI] [PubMed] [Google Scholar]
- Berth A, Neumann W, Awiszus F, Pap G. Massive rotator cuff tears: functional outcome after debridement or arthroscopic partial repair. J Orthop Traumatol. 2010;11:13–20. doi: 10.1007/s10195-010-0084-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burkhart SS, Athanasiou KA, Wirth MA. Margin convergence: a method of reducing strain in massive rotator cuff tears. Arthroscopy. 1996;12:335–338. doi: 10.1016/s0749-8063(96)90070-5. [DOI] [PubMed] [Google Scholar]
- Caldwell GL, Warner JP, Miller MD, Boardman D, Towers J, Debski R. Strength of fixation with transosseous sutures in rotator cuff repair. J Bone Joint Surg Am. 1997;79:1064–1068. doi: 10.2106/00004623-199707000-00013. [DOI] [PubMed] [Google Scholar]
- Eby SF, Song P, Chen S, Chen Q, Greenleaf JF, An KN. Validation of shear wave elastography in skeletal muscle. J Biomech. 2013;46:2381–2387. doi: 10.1016/j.jbiomech.2013.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferraioli G, Parekh P, Levitov AB, Filice C. Shear wave elastography for evaluation of liver fibrosis. J Ultrasound Med. 2014;33:197–203. doi: 10.7863/ultra.33.2.197. [DOI] [PubMed] [Google Scholar]
- Garra BS. Imaging and estimation of tissue elasticity by ultrasound. Ultrasound Q. 2007;23:255–268. doi: 10.1097/ruq.0b013e31815b7ed6. [DOI] [PubMed] [Google Scholar]
- Gazielly DF, Gleyze P, Montagnon C. Functional and anatomical results after rotator cuff repair. Clin Orthop Relat Res. 1994:43–53. [PubMed] [Google Scholar]
- Gerber C, Schneeberger AG, Hoppeler H, Meyer DC. Correlation of atrophy and fatty infiltration on strength and integrity of rotator cuff repairs: a study in thirteen patients. J Shoulder Elbow Surg. 2007;16:691–696. doi: 10.1016/j.jse.2007.02.122. [DOI] [PubMed] [Google Scholar]
- Giambini H, Hatta T, Krzysztof GR, Widholm P, Karlsson A, Leinhard OD, Adkins MC, Zhao C, An KN. Intramuscular fat infiltration evaluated by magnetic resonance imaging predicts the extensibility of the supraspinatus muscle. Muscle Nerve. 2017 doi: 10.1002/mus.25673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harryman DT, 2nd, Mack LA, Wang KY, Jackins SE, Richardson ML, Matsen FA., 3rd Repairs of the rotator cuff. Correlation of functional results with integrity of the cuff. J Bone Joint Surg Am. 1991;73:982–989. [PubMed] [Google Scholar]
- Hatta T, Giambini H, Sukegawa K, Yamanaka Y, Sperling JW, Steinmann SP, Itoi E, An KN. Quantified Mechanical Properties of the Deltoid Muscle Using the Shear Wave Elastography: Potential Implications for Reverse Shoulder Arthroplasty. PLoS One. 2016a;11:e0155102. doi: 10.1371/journal.pone.0155102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatta T, Giambini H, Uehara K, Okamoto S, Chen S, Sperling JW, Itoi E, An KN. Quantitative assessment of rotator cuff muscle elasticity: Reliability and feasibility of shear wave elastography. J Biomech. 2015;48:3853–3858. doi: 10.1016/j.jbiomech.2015.09.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatta T, Giambini H, Zhao C, Sperling JW, Steinmann SP, Itoi E, An KN. Biomechanical Effect of Margin Convergence Techniques: Quantitative Assessment of Supraspinatus Muscle Stiffness. PLoS One. 2016b;11:e0162110. doi: 10.1371/journal.pone.0162110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hersche O, Gerber C. Passive tension in the supraspinatus musculotendinous unit after long-standing rupture of its tendon: a preliminary report. J Shoulder Elbow Surg. 1998;7:393–396. doi: 10.1016/s1058-2746(98)90030-1. [DOI] [PubMed] [Google Scholar]
- Hirata K, Kanehisa H, Miyamoto-Mikami E, Miyamoto N. Evidence for intermuscle difference in slack angle in human triceps surae. J Biomech. 2015;48:1210–1213. doi: 10.1016/j.jbiomech.2015.01.039. [DOI] [PubMed] [Google Scholar]
- Hug F, Lacourpaille L, Maisetti O, Nordez A. Slack length of gastrocnemius medialis and Achilles tendon occurs at different ankle angles. J Biomech. 2013;46:2534–2538. doi: 10.1016/j.jbiomech.2013.07.015. [DOI] [PubMed] [Google Scholar]
- Iannotti JP, Deutsch A, Green A, Rudicel S, Christensen J, Marraffino S, Rodeo S. Time to failure after rotator cuff repair: a prospective imaging study. J Bone Joint Surg Am. 2013;95:965–971. doi: 10.2106/JBJS.L.00708. [DOI] [PubMed] [Google Scholar]
- Itoigawa Y, Sperling JW, Steinmann SP, Chen Q, Song P, Chen S, Itoi E, Hatta T, An KN. Feasibility assessment of shear wave elastography to rotator cuff muscle. Clin Anat. 2015;28:213–218. doi: 10.1002/ca.22498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim SY, Bleakney RR, Rindlisbacher T, Ravichandiran K, Rosser BW, Boynton E. Musculotendinous architecture of pathological supraspinatus: a pilot in vivo ultrasonography study. Clin Anat. 2013;26:228–235. doi: 10.1002/ca.22065. [DOI] [PubMed] [Google Scholar]
- Maman E, Harris C, White L, Tomlinson G, Shashank M, Boynton E. Outcome of nonoperative treatment of symptomatic rotator cuff tears monitored by magnetic resonance imaging. J Bone Joint Surg Am. 2009;91:1898–1906. doi: 10.2106/JBJS.G.01335. [DOI] [PubMed] [Google Scholar]
- Meyer DC, Lajtai G, von Rechenberg B, Pfirrmann CW, Gerber C. Tendon retracts more than muscle in experimental chronic tears of the rotator cuff. J Bone Joint Surg Br. 2006;88:1533–1538. doi: 10.1302/0301-620X.88B11.17791. [DOI] [PubMed] [Google Scholar]
- Minagawa H, Yamamoto N, Abe H, Fukuda M, Seki N, Kikuchi K, Kijima H, Itoi E. Prevalence of symptomatic and asymptomatic rotator cuff tears in the general population: From mass-screening in one village. J Orthop. 2013;10:8–12. doi: 10.1016/j.jor.2013.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moosmayer S, Smith HJ, Tariq R, Larmo A. Prevalence and characteristics of asymptomatic tears of the rotator cuff: an ultrasonographic and clinical study. J Bone Joint Surg Br. 2009;91:196–200. doi: 10.1302/0301-620X.91B2.21069. [DOI] [PubMed] [Google Scholar]
- Morrow DA, Haut Donahue TL, Odegard GM, Kaufman KR. Transversely isotropic tensile material properties of skeletal muscle tissue. J Mech Behav Biomed Mater. 2010;3:124–129. doi: 10.1016/j.jmbbm.2009.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Post M, Silver R, Singh M. Rotator cuff tear. Diagnosis and treatment. Clin Orthop Relat Res. 1983:78–91. [PubMed] [Google Scholar]
- Roh MS, Wang VM, April EW, Pollock RG, Bigliani LU, Flatow EL. Anterior and posterior musculotendinous anatomy of the supraspinatus. J Shoulder Elbow Surg. 2000;9:436–440. doi: 10.1067/mse.2000.108387. [DOI] [PubMed] [Google Scholar]
- Safran O, Derwin KA, Powell K, Iannotti JP. Changes in rotator cuff muscle volume, fat content, and passive mechanics after chronic detachment in a canine model. J Bone Joint Surg Am. 2005;87:2662–2670. doi: 10.2106/JBJS.D.02421. [DOI] [PubMed] [Google Scholar]
- Safran O, Schroeder J, Bloom R, Weil Y, Milgrom C. Natural history of nonoperatively treated symptomatic rotator cuff tears in patients 60 years old or younger. Am J Sports Med. 2011;39:710–714. doi: 10.1177/0363546510393944. [DOI] [PubMed] [Google Scholar]
- Schwartz C, Croisier JL, Rigaux E, Denoel V, Bruls O, Forthomme B. Dominance effect on scapula 3-dimensional posture and kinematics in healthy male and female populations. J Shoulder Elbow Surg. 2014;23:873–881. doi: 10.1016/j.jse.2013.08.020. [DOI] [PubMed] [Google Scholar]
- Tempelhof S, Rupp S, Seil R. Age-related prevalence of rotator cuff tears in asymptomatic shoulders. J Shoulder Elbow Surg. 1999;8:296–299. doi: 10.1016/s1058-2746(99)90148-9. [DOI] [PubMed] [Google Scholar]
- Ward SR, Hentzen ER, Smallwood LH, Eastlack RK, Burns KA, Fithian DC, Friden J, Lieber RL. Rotator cuff muscle architecture: implications for glenohumeral stability. Clin Orthop Relat Res. 2006;448:157–163. doi: 10.1097/01.blo.0000194680.94882.d3. [DOI] [PubMed] [Google Scholar]
- Wu G, van der Helm FC, Veeger HE, Makhsous M, Van Roy P, Anglin C, Nagels J, Karduna AR, McQuade K, Wang X, Werner FW, Buchholz B, International Society of, B. ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion–Part II: shoulder, elbow, wrist and hand. J Biomech. 2005;38:981–992. doi: 10.1016/j.jbiomech.2004.05.042. [DOI] [PubMed] [Google Scholar]
- Yamaguchi K, Tetro AM, Blam O, Evanoff BA, Teefey SA, Middleton WD. Natural history of asymptomatic rotator cuff tears: a longitudinal analysis of asymptomatic tears detected sonographically. J Shoulder Elbow Surg. 2001;10:199–203. doi: 10.1067/mse.2001.113086. [DOI] [PubMed] [Google Scholar]
- Zumstein MA, Jost B, Hempel J, Hodler J, Gerber C. The clinical and structural long-term results of open repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2008;90:2423–2431. doi: 10.2106/JBJS.G.00677. [DOI] [PubMed] [Google Scholar]


