Highlights
-
•
PRMCs are very rare and they share macroscopical and histological similarity to ovarian cystadenomas.
-
•
It is important to rule out Echinococcosis specially in endemic regions such as South America.
-
•
Complete surgical excision of the PRMCs is recommended to eliminate the risk of infection, recurrence and malignant degeneration.
-
•
It is important to remember that cystic fluid spillage has to be prevented due to the uncertain pathology of the tumor in most of the cases.
Keywords: Cystic tumor, Retroperitoneum, Mucinous cystadenoma
Abstract
Mucinous cystadenomas and carcinomas of the ovary are well-established and common tumors. However, Primary retroperitoneal mucinous cystadenomas (PRMCs) are very rare. We present a 50-year-old woman referred to our institution with history of intermittent abdominal pain and palpable mass in her left flank. On CT-scan an unilocular cystic mass with thin wall measuring 171 × 155 × 108 mm in the retroperitoneum was shown. Patient underwent surgical excision of the tumor. The histopathology examination showed a cystic mass with a fibrous wall and an epithelium composed of a single layer of columnar cells with mucin vacuoles compatible with PRMC.
1. Introduction
Primary retroperitoneal mucinous cystadenomas (PRMCs) are observed more frequently in women with no specific symptoms. An accurate preoperative diagnosis in these cases is difficult because no effective methods have been established. Once diagnosed, complete excision is recommended because of the risk of infection or malignant degeneration, even though it behaves in a benign fashion with no recurrences in most of the cases.
The research work has been reported in line with the SCARE criteria [1].
2. Presentation of case
A 50-year-old woman was referred to our institution with a 2-month history of intermittent abdominal pain and palpable mass in her left flank. Her medical history was significant only for hypertension and a laparoscopic cholecystectomy. Physical examination revealed a painless, palpable mass in the left flank of her abdomen.
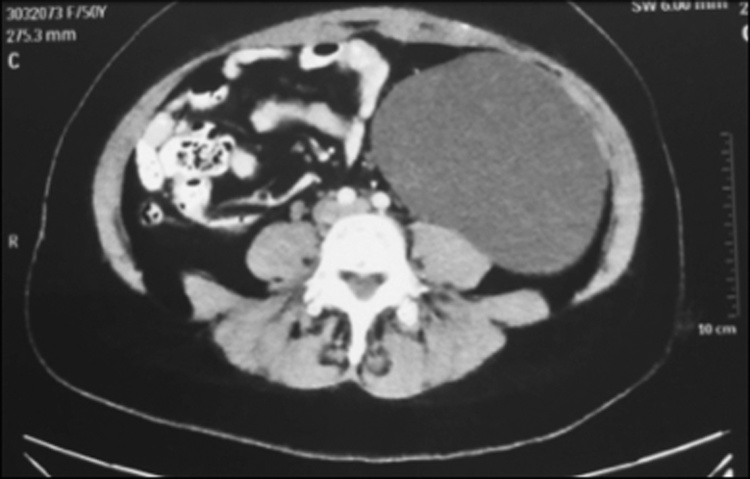
The patient was in good general status. Hormonal status and tumor markers, including CA 19-9, CA 125, beta-HCG, alpha-fetoprotein and CEA were within normal limits. Serology for E. granulosus was negative. Plain radiographs of the abdomen were normal. MRI and CT scan showed an unilocular cystic mass with thin walls measuring 171 × 155 × 108 mm in the retroperitoneum in the left flank of the abdomen (Fig. 1). It was in contact with the left kidney and separated from the left ovary.
Fig. 1.
CT-scan showing an unilocular cystic mass.
The patient underwent complete surgical excision of the tumor via a laparotomic approach due to its size. It was found to be located behind the posterior peritoneum of the descending colon and adhered to the organ and its posterior peritoneum.
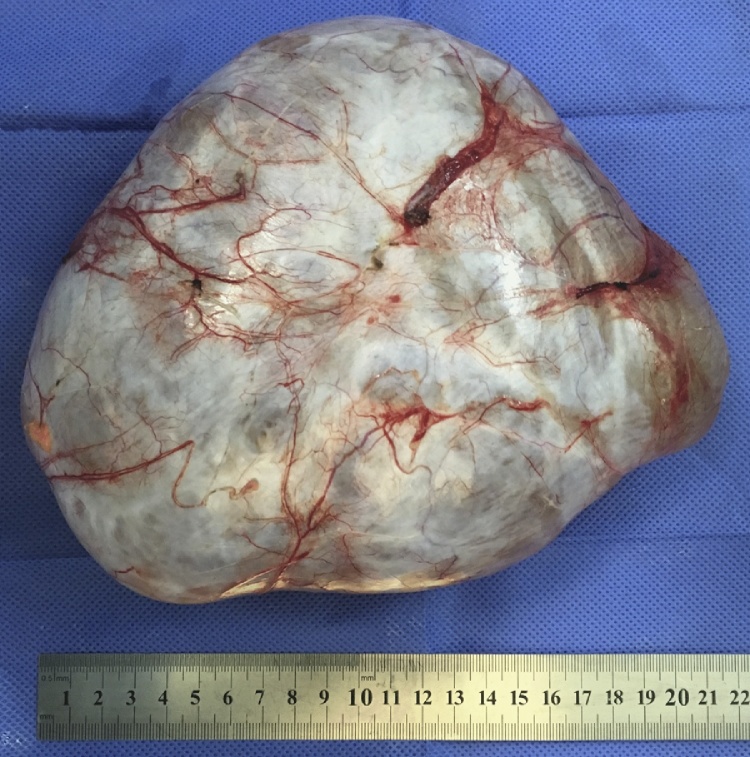
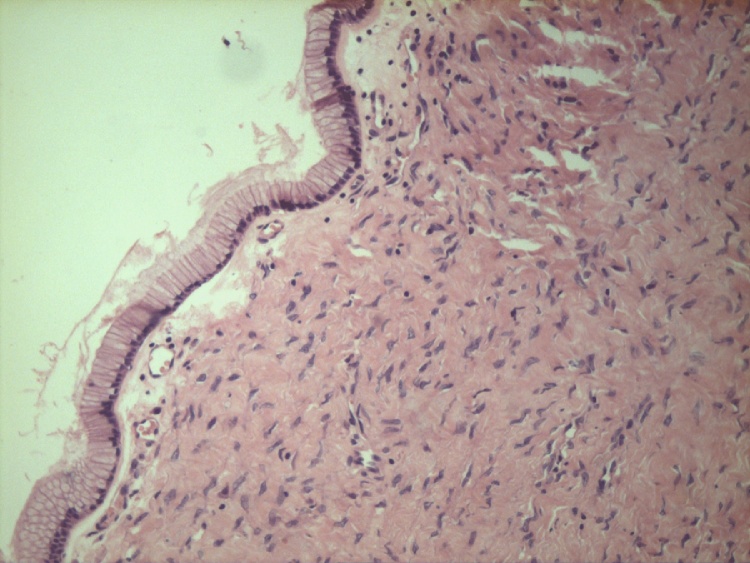
The surgical specimen consisted in a huge retroperitoneal cystic mass that measured 17 × 15 × 13 cm. It had thin vascularized walls and on opening, the cyst contained clear serous fluid (Fig. 2). Microscopic examination of the inner lining showed a single layer of columnar cells with abundant mucin vacuoles surrounded by dense fibrous tissue. Microcalcifications were also found (Fig. 3). Diagnosis of a PRMC was made.
Fig. 2.
Large cystic mass with thin vascularized walls.
Fig. 3.
Wall of fibrous tissue with single lining epithelium.
Postoperative course was uneventful being discharged on postoperative day 6.
3. Discussion
Primary retroperitoneal mucinous cystadenomas (PRMCs) are very rare and they share macroscopical and histological similarity to ovarian cystadenomas. They can be found in any part of the retroperitoneum without attachment to the ovary.
Their origin is widely debated as there are no epithelial cells in the retroperitoneum. Two theories have been proposed to explain the histogenesis. The first theory is that they are thought to arise from heterotopic ovarian tissue due to its resemblance to ovarian mucinous cystadenomas. Estrogen receptor positivity in stromal cells of PRMCs has also been demonstrated [2]. The second theory is that these tumors arise from an invagination of multipotential mesothelium with subsequent mucinous metaplasia of the cells, giving rise to a mucinous tumor that enlarges to form a cyst [2], [3].
Based on a review of the cases reported in the literature, these tumors can be classified in three types. The most common type is the retroperitoneal mucinous cystadenoma. A large, unilocular or multilocular benign cystic tumor not associated with recurrence after resection. This was the type that our patient presented. In the second type, the cells of the inner lining presents with foci of epithelial proliferation. This type resembles the ovarian mucinous cystadenomas of low malignant potential. The third type is the mucinous cystadenocarcinoma [2], [3].
It is important to rule out Echinococcosis specially in endemic regions such as Southamerica. Serological tests were negative in our patient. They are useful in the diagnosis of the disease but the sensitivity is determined by the site and condition of the cyst [4], [5], [6]. Location of hydatid cysts in lungs, spleen or kidneys are associated with lower quantity of antigens and therefore a lower quantity of antibodies. This situation can lead to a false negative result [4]. Protoscolises and the characteristic sandy material of cyst fluid were not present in the tumor.
4. Conclusion
In conclusion, the complete surgical excision of the PRMCs is always recommended to eliminate the risk of infection, recurrence and malignant degeneration. An exploratory laparotomy with complete enucleation is the traditional treatment, although the laparoscopic excision has been reported. It is important to remember that cystic fluid spillage has to be prevented due to the uncertain pathology of the tumor in most of the cases.
Conflict of interest
None.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Consent
Written informed consent was obtained from the patient and there are no alterations that distort scientific meaning.
Authors contribution
Nardi: Operated and managed the patient. Study design.
Quildrian: Operated and managed the patient. Study design.
Dezanzo: Conducted the histopathologic examination of the specimen.
Guarantors
Nardi and Quildrian.
Contributor Information
Walter Sebastián Nardi, Email: nardi.ws@gmail.com.
Pablo Dezanzo, Email: pablodezanzo@aol.com.
Sergio Damián Quildrian, Email: squildrian@intramed.net.
References
- 1.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., the SCARE Group The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016 doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 2.Subramony C., Habibpour S., Hashimoto L.A. Retroperitoneal mucinous cystadenoma. Arch. Pathol. Lab. Med. 2001;125(May (5)):691–694. doi: 10.5858/2001-125-0691-RMC. [DOI] [PubMed] [Google Scholar]
- 3.Lee S.Y., Han W.C. Primary retroperitoneal mucinous cystadenoma. Ann. Coloproctol. 2016;32(February (1)):33–37. doi: 10.3393/ac.2016.32.1.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dionigi G., Carrafiello G., Recaldini C., Sessa F., Boni L., Rovera F. Laparoscopic resection of a primary hydatid cyst of the adrenal gland: a case report. J. Med. Case Rep. 2007;1:61. doi: 10.1186/1752-1947-1-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kumar S., Nanjappa B., Gowda K.K. Laparoscopic management of a hydatid cyst of the adrenal gland. Korean J. Urol. 2014;55:493–495. doi: 10.4111/kju.2014.55.7.493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nardi W., Buero A., Lozano S., Porto E.A. Laparoscopic resection of a bulky primary adrenal hydatid cyst. J. Minim. Access Surg. 2015;11(October–December (4)):279–281. doi: 10.4103/0972-9941.152103. [DOI] [PMC free article] [PubMed] [Google Scholar]